Abstract
Purpose
The purpose of this study was to compare medication adherence rates and type 2 diabetes mellitus (T2DM) health outcomes in a sample of underserved patients with suboptimally controlled T2DM (HbA1C>7%) who had received pharmacist-directed medication therapy management (MTM) to those who had not received MTM.
Methods
A retrospective review of 100 patient records was conducted. For the MTM group, a pharmacist engaged patients in patient-centered services to optimize therapeutic outcomes. Non-MTM patients received usual care. Outcomes were HbA1C, medication adherence, blood pressure, lipids and creatinine. Group comparisons on clinical outcomes were analyzed before and after matching MTM and non-MTM patients on demographic characteristics.
Results
Before matching, the MTM group had a higher rate of medication adherence than the non-MTM group. Hemoglobin A1C levels were lower in the MTM group compared to the non-MTM group. Similarly, low density lipoprotein (LDL) cholesterol were lower in the MTM group compared to the non-MTM group. After matching, medication adherence rate remained higher in the MTM group than the non-MTM group. Similarly, HbA1C levels remained lower in the MTM group than the non-MTM group.
Conclusions
There is a paucity of research focused on behavioral interventions for improving health outcomes in underserved communities. Our results advance the existing literature by demonstrating a positive association between pharmacist-directed MTM, medication adherence, and glycemic control in a sample of underserved patients with suboptimally controlled T2DM. A prospective pharmacy intervention and examination of long-term effects of MTM on medication adherence and T2DM health outcomes in this population is warranted.
Introduction
Underserved populations are at increased risk for type 2 diabetes mellitus (T2DM) and other chronic health conditions.1,2 These vulnerable communities include persons who are underinsured/uninsured, and of lower socioeconomic status.1,3 Among individuals with T2DM, glycemic control is worse in the uninsured than the insured.4 Low-income populations are also more likely to experience T2DM-related health complications and early mortality than middle-income and high-income populations.2,5 Ethnoracial minorities, in particular African Americans and Hispanics, are also disproportionately affected by T2DM,6 and make up a large portion of these at-risk communities.7 Adherence to an anti-diabetes medication regimen is a major determinant of glycemic control 8 and T2DM-related health outcomes9,10 yet many patients with chronic health conditions experience difficulty adhering to their medication regimen.11 Finding an effective strategy to improve treatment adherence may help to address socioeconomic and racial disparities in T2DM disease outcomes.
There is an emerging initiative to discover effective ways to improve self-care behavior and T2DM health outcomes through interdisciplinary care teams. Pharmacist intervention models have shown promise as an effective strategy to manage T2DM and improve adherence to anti-diabetes medications.12 Medication therapy management (MTM),13 a range of patient-centered services tailored to a patient's needs provided by a pharmacist to optimize therapeutic outcomes, may be particularly useful in improving adherence to medication regimens and subsequent health outcomes. In order to determine the effectiveness of MTM intervention in a community health center, we compared medication adherence rates (i.e. prescription refills) between individuals with T2DM, who received pharmacist-directed MTM compared to those who had not received MTM. This study also examined group differences in T2DM-related health outcomes (HbA1C, blood pressure, lipids, and renal function). In order to control for confounding demographic factors, a second analysis after matching MTM and non-MTM patients on demographic characteristics (age, gender, race, and ethnicity). The study hypothesis was that MTM would be associated with lower HbA1C levels and better medication adherence. This study adds to the existing literature by examining how enhanced pharmacy care (i.e. MTM) relates to T2DM medication adherence and health outcomes in underserved communities. Findings from this study may inform the development of metrics to more systematically assess the effects of pharmacist-directed MTM on health outcomes.
Methods
Design and Collaborative Team
This study used a retrospective case-control design and was the product of a community-academic partnership. Retrospective case-control designs leverage existing data sources and are often implemented to generate hypotheses for future prospective research. Limitations of this type of design include dependence on existing documentation and causality cannot be determined. Key team members from the community partner organization, a community health center, included a clinical pharmacist and pharmacy personnel. The community partners provided expertise in MTM, identified patients for the study, abstracted data from medical records, obtained prescription refill data and participated in the interpretation of the data and dissemination of the findings. The community partners received training in data collection and management from the academic partners. The academic partners provided expertise in clinical and comparative effectiveness research, performed statistical analyses, and assisted with data interpretation and dissemination of study findings. Both the academic and community partners participated in the creation of data collection tools. This study was approved by the Vanderbilt University Institutional Review Board.
Study Population
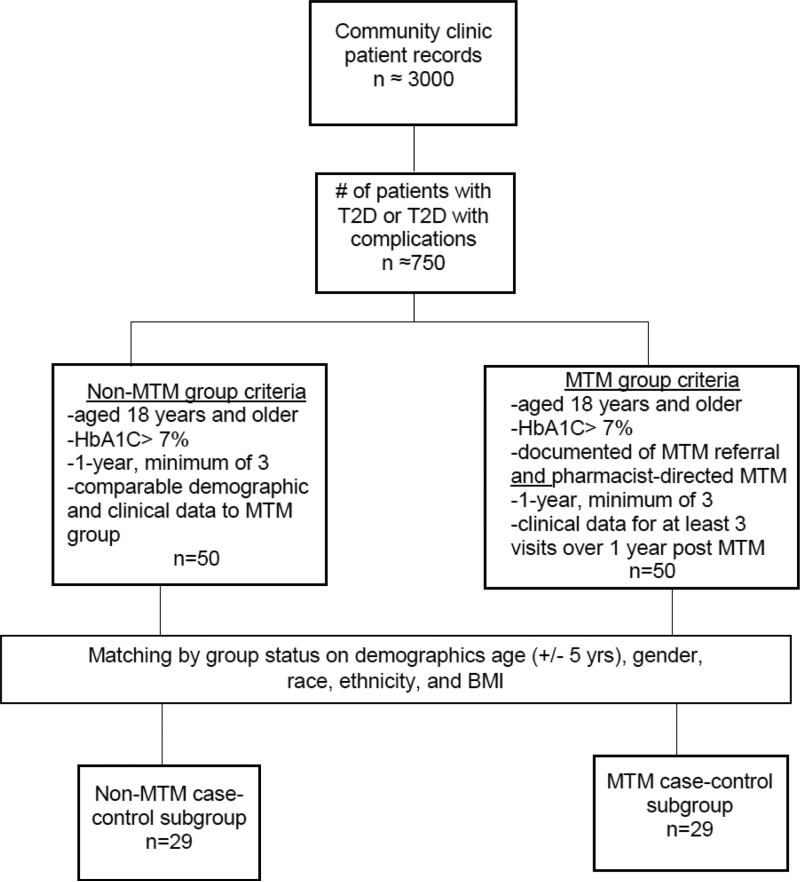
Patients from a community health clinic who were 18 years or older were identified through administrative medical record review using International Classification of Diseases (ICD-9) codes for T2DM (250.00, 250.02) and T2DM with disease complications (250.40, 250.42, 250.50, 250.52, 250.60, 250.62, 250.80, 250.82). Suboptimal control was defined as having at least one documented HbA1C value > 7%, which is the benchmark for glycemic control14 and a risk factor for disease-related microvascular complications.15 Patients in the non-MTM (control) group had no contact with the clinical pharmacist. Patients in the MTM group were referred to the pharmacist for MTM by their primary care provider (PCP) and had clinical data from at least 3 clinic visits during a consecutive 12-month period following the first MTM visit. Patients in this group were identified from medical record documentation noting contact with the clinical pharmacist and recorded information describing any instruction provided for optimizing therapeutic outcomes of anti-diabetes medication and T2DM disease management. Demographic variables (age, gender, race, and ethnicity) were used to select non-MTM patients. Patient record data was collected from clinic visits that occurred between the years of 2011 and 2013. A figure illustrating patient record selection is provided in Figure 1.
Figue 1.
Patient Record Selection Process
Measures
Clinical Outcomes
Clinical outcomes of interest included glycemic control (HbA1C), blood pressure, lipids (high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides), creatinine levels, and medication adherence. Medication adherence was determined by anti-diabetes prescription refill. Pharmacy personnel contacted retail pharmacies by phone to query patient prescription refill status. Refill percentage data was calculated from the ratio of the number of anti-diabetes medication refills dispense (from pharmacy record) to the number of medication refills prescribed. Patients were identified as adherent if they met their prescription refill a minimum of 85% of the time. Prescription refill is a common outcome measure in diabetes medication adherence research 16,17. Prescription refill data derived from pharmacy records circumvents issues of patient recall and social desirability bias. A caveat of refill data is that medication adherence cannot be assumed nor does refill data provide details on patient dosing errors. For patients in the MTM-group, prescription refill information was captured for a year post initial MTM consultation. For patients in the non-MTM group, prescription refill information was also captured for a year.
Intervention
Medication Therapy Management (MTM)
Medication therapy management refers to a group of analytical, educational, and monitoring services provided by the pharmacist to optimize therapeutic outcomes for the patient.13 For this study, the pharmacist used a patient-customized, semi-structured approach. The pharmacist reviewed the patient's T2DM medication regimen, provided verbal education and training on medication delivery and best administration sites and education on health-promoting behaviors (diet, exercise, smoking cessation). Patients were asked to “teach back” the information to confirm understanding. Frequency and duration data on MTM was not collected.
Statistical Analyses
Mann-Whitney tests for non-parametric data two-group comparisons were employed due to violations of normality in continuous dependent variables. For the first analysis, group differences in dependent variables were compared between the MTM group and non-MTM group. For the second analysis, a case-control design was used to match a sub-group of patients using demographic data. Patients were matched on key demographic factors including age (+/− 5 years), gender, race, ethnicity, and body mass index (BMI) (+/− 3 kg/m2). The matched sub-sample included 58 patients. Pearson chi-square test were used to determine group differences in categorical dependent variables. 2Sample size and power calculations were performed using data from a published study of MTM and diabetes, which had a difference in mean HbA1C between the matched pairs of 0.8% and a standard deviation of 2%.18, Using this mean for a study with 50 pairs of patients, we calculated that this sample size will provide of a power of 80% and a type 1 error rate of 0.05. Significance level was set a priori at p<0.05. SPSS version 22 (SPSS, Inc, Chicago, Illinois, USA) was used to analyze the data.
Results
Patient characteristics by group status, before and after matching are provided in Table 1. Patients in this study ranged in age from 24 to 77 years old (M= 53.7, years, SD=12.5) and were predominately female (58%). Prior to matching, patients in the MTM group were older (p<0.01) and had a higher body mass index, although the difference was not statistically significant (p=0.05 than the non-MTM group.
Table 1.
Sample Demographic Characteristics Before and After Matching
| Before Matching | After Matching | |||||
|---|---|---|---|---|---|---|
| MTM | Non-MTM | p-value | MTM | Non-MTM | p-value | |
| n=50 | n=50 | n=29 | n=29 | |||
| Age, years | 57 ± 9.8 | 50 ± 13.8 | <0.01 | 57.4±10.2 | 57.0±9.5 | 0.88 |
| Gender, % male | 28% | 56% | X2=0.008 | 14 [48.3%] | 14 [48.3%] | X2=1.00 |
| Race (n[%]) | X2=0.20 | X2=1.00 | ||||
| Caucasian | 29 [58%] | 20 [40%] | 15 [51.7%] | 15 [51.5%] | ||
| Black | 12 [24%] | 19 [38%] | 8 [27.6%] | 8 [27.6%] | ||
| Other | 9[18%] | 11 [22%] | 6 [ 20.7%] | 6 [20.7%] | ||
| Ethnicity (n[%]) | X2=0.07 | X2=1.00 | ||||
| Hispanic/Latino | 7 [14%] | 5 [10%] | 3 [10.3%] | 3 [10.3%] | ||
| Body Mass Index, kg/m2 | 36.2 ± 9.1 | 32.8 ± 8.1 | 0.05 | 37.2±10.1 | 34.3±8.6 | 0.25 |
Note: * p±0.05; Mean±SD; X2= Chi-square statistic
Medication Adherence
Prior to matching, medication adherence rates differed between the two groups. Results showed 64.6% of patients in the MTM group were medication adherent compared to 10% of patients in the non-MTM group, X2 (1) =27.13, p<0.001. After matching, these findings persisted, more patients in the MTM group (62%) were medication adherent than in the non-MTM group (7%), X2 (1) =18.51, p<0.001). Additional details are provided it Table 2.
Table 2.
Medication Adherence and Clinical Health Outcomes Before and After Matching
| Before Matching | After Matching | |||||
|---|---|---|---|---|---|---|
| MTM | Non-MTM | p-value | MTM | Non-MTM | p-value | |
| n=50 | n=50 | n=29 | n=29 | |||
| Medication Adherence (n[%]) | 31 [64.6%] | 4 [10%] | <0.001 | 18 [62.1%] | 2 [6.9%] | <0.001 |
| HbA1C (%) | 7.5 ± 0.42 | 10.6 ± 2.1 | <0.001 | 7.5± 0.38 | 10.8 ± 2.0 | <0.01 |
| Systolic Blood Pressure | 138.7 ± 22.0 | 139.2 ± 20.7 | 0.80 | 136.5±19.8 | 145.4±17.8 | 0.12 |
| Diastolic Blood Pressure | 73.3 ± 12.3 | 73.2 ± 13.7 | 0.71 | 72.7±10.3 | 73.8±14.7 | 0.63 |
| HDL | 47.6 ± 9.4 | 45.1 ± 13.0 | 0.07 | 48.2±10.3 | 45.2±12.9 | 0.17 |
| LDL | 89.2 ± 31.2 | 118.4 ± 82.5 | 0.02 | 92.7±36.4 | 110.8±65.7 | 0.16 |
| Triglycerides | 172.9 ± 75.0 | 209.8± 171.5 | 0.56 | 175.2±87.5 | 237.6±180.3 | 0.16 |
| Creatinine | 1.02 ± 0.7 | 1.08 ± 1.1 | 0.84 | 0.94±0.29 | 0.91±0.25 | 0.71 |
Note: * p±0.05; Mean±SD; X2= Chi-square statistic; HbA1C= glycated hemoglobin; HDL=high density lipoprotein; LDL= low density lipoprotein
Clinical Outcomes
Prior to matching, a significant difference in glycemic control between the MTM and non-MTM group was observed. Patients in the MTM-group (M rank= 27.62, n=50) had lower HbA1C levels than patients in the non-MTM group (M rank=73.38, n=50), z (160) =−7.89, p<0.0001. Significant differences in LDL levels were also observed. Patients in the MTM group (M rank=40.80, n=50) had lower LDL levels than patients in the non-MTM group (M rank=53.00, n=50), z (774.0) =−2.18, p=0.02. There was no significant difference in blood pressure, HDL, triglycerides, or creatinine between the groups. . After matching a significant difference in glycemic control remained, with the MTM group having lower HbA1C levels than the non-MTM group (p<0.001). After matching, the groups did not differ on any other clinical outcomes (all p-values>0.05). Group means and standard deviations are presented in Table 2.
Discussion
This study found pharmacist-directed MTM in a community health center was associated with better medication adherence and lower HbA1C compared to patients who did not receive MTM. These findings are aligned with previous reports demonstrating a positive association between pharmacy interventions and improved T2DM medication adherence.12,8, 19 This study's results differ from that of Odegard and colleagues who reported no effect of a 6-month pharmacist intervention on T2DM medication adherence.20 Differences in study findings may be attributed to differences in how medication adherence was defined. Participants in the two studies may also have experienced different barriers related to medication adherence. It is important to note, among published studies examining the association between pharmacist interventions and T2DM medication adherence, definitions of adherence vary widely (e.g. self-report, prescription refill, proxy reports) and this may pose a challenge in harmonizing findings from this growing area of research. Therefore, future work is needed to develop a systematic definition of medication adherence. Nevertheless, these results do suggest enhanced pharmacy care is a potentially valuable tool to increase medication adherence in individuals with T2DM.
Glycemic control is strongly associated with medication adherence, 21 therefore results in this study are expected. Prior to matching, cholesterol levels, in this study were also lower in the MTM group than the non-MTM group. These results are similar to other reports demonstrating a favorable association between pharmacy care and health indices associated with T2DM.22,23,24 The current study enhances the existing literature in several important ways. First, this study collected information on medication adherence and modifiable markers of T2D that are responsive to MTM in a high-risk, vulnerable population, often underrepresented in clinical research. Second, implementation of this study in a community health center settings sheds light on the potential benefits of MTM as an effective tool to treat chronic disease and address ethnoracial and socioeconomic health disparities. Third, the design of this study may serve as a model for community and academic institutional partnerships for the implementation of community-based research studies. Through a collaborative process, both partners participated in the pre-implementation and execution of this study. Results from this study advanced both partners understanding of community health and the role of pharmacy care. Finally, preliminary data from this study will set the foundation for developing a standardized MTM data recording tool that can be used in diverse healthcare settings. This tool will allow for the replication of our study findings and a more rigorous examination of effective MTM strategies to increase medication adherence and improve disease outcomes.
There are limitations to this study that should be highlighted. Findings may not be generalizable because of the small sample number of patient health records utilized in this study. Information on the number of clinic visit was not collected in this study. It is possible study findings may be in part, related to group differences in the number of clinic visits. The retrospective case-control cohort design used in this study can only determine associations between participation in the MTM intervention, medication adherence and T2DM outcomes. An alternative quasi-experimental study design to the one implemented in the current study is a pre-post study design. However, this design could not be implemented due to logistical restraints associated with obtaining patient data. A prospective randomized control design is needed to determine whether MTM has a positive causal effect on medication adherence and T2DM health outcomes. Finally, the MTM model used in this study was semi-structured and derived from medical record documentation.
Implications for Practice
Pharmacists are uniquely and ideally positioned to provide patient education, counseling on medication and disease, provide information about health-related community resources, and encourage health-promoting behavior.23 These skills in a community health center, where vulnerable populations often receive care, may be particularly valuable in improving health outcomes for high-risk populations. The results of this study show that a pharmacist-directed MTM is positively associated with medication adherence and disease outcomes in patients with suboptimally controlled T2DM. These findings in a community health clinic population has broad implications for improving health care delivery and health outcomes in community-based settings. Underserved populations are vulnerable to T2DM and other chronic conditions; furthermore their limited access to recommended healthcare likely makes this segment of the population the most in need of supportive chronic disease management services.
Acknowledgements
The authors wish to acknowledge Andrew Keller and the Vanderbilt Community Engagement Research Core
Funding: This project has been funded in whole or in part with Federal funds from the National Center for Research Resources and NCATS, National Institutes of Health, through the Clinical and Translational Science Awards Program (CTSA) under the following award numbers: UL1 TR000445 and U54 MD007593.
References
- 1.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87(2):443–494. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 3.Chin MH. Quality improvement implementation and disparities: the case of the health disparities collaboratives. Med Care. 2010;48(8):668–675. doi: 10.1097/MLR.0b013e3181e3585c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Card D, Dobkin C, Maestas N. The impact of nearly universal insurance coverage on health care utilization and health: Evidence from Medicare. Am Econ Rev. 2004;98(5):2242–2258. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Med Care. 2008;46(10):1023–1032. doi: 10.1097/MLR.0b013e318185c913. [DOI] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention National Diabetes Statistics Report, 2014. [September 29, 2014];Publications - Diabetes DDT. http://www.cdc.gov/diabetes/pubs/statsreport14.htm.
- 7.National Association of Community Health Centers [February 10, 2014];A sketch of Community Health Centers Chart Book 2014. www.nachc.com.
- 8.Chung WW, Chua SS, Lai PSM, Chan SP. Effects of a pharmaceutical care model on medication adherence and glycemic control of people with type 2 diabetes. Patient Prefer Adherence. 2014;8:1185–1194. doi: 10.2147/PPA.S66619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horswell RL, Wascom CK, Cerise FP, Besse JA, Johnson JK. Diabetes mellitus medication assistance program: relationship of effectiveness to adherence. J Health Care Poor Underserved. 2008;19(3):677–686. doi: 10.1353/hpu.0.0062. [DOI] [PubMed] [Google Scholar]
- 10.Chua S, Chan S. Medication adherence and achievement of glycaemic targets in ambulatory type 2 diabetic patients. J Appl Pharm Sci. 2011;01(04):55–59. [Google Scholar]
- 11.Cramer JA. A Systematic Review of Adherence With Medications for Diabetes. Diabetes Care. 2004;27(5):1218–1224. doi: 10.2337/diacare.27.5.1218. doi:10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- 12.Lindenmeyer A, Hearnshaw H, Vermeire E, Van Royen P, Wens J, Biot Y. Interventions to improve adherence to medication in people with type 2 diabetes mellitus: a review of the literature on the role of pharmacists. J Clin Pharm Ther. 2006;31(5):409–419. doi: 10.1111/j.1365-2710.2006.00759.x. [DOI] [PubMed] [Google Scholar]
- 13.Bluml BM. Definition of Medication Therapy Management: Development of Professionwide Consensus. J Am Pharm Assoc (2003) 2003;45(5):566–572. doi: 10.1331/1544345055001274. [DOI] [PubMed] [Google Scholar]
- 14.American Diabetes Association Standards of medical care in diabetes--2011. Diabetes Care. 2011;34(Suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Executive summary: standards of medical care in diabetes--2014. Diabetes Care. 2014;37(Suppl 1):S5–S13. doi: 10.2337/dc14-S005. [DOI] [PubMed] [Google Scholar]
- 16.Grant R, Adams AS, Trinacty CM, et al. Relationship between patient medication adherence and subsequent clinical inertia in type 2 diabetes glycemic management. Diabetes Care. 2007;30(4):807–812. doi: 10.2337/dc06-2170. [DOI] [PubMed] [Google Scholar]
- 17.Adams AS, Trinacty CM, Zhang F, et al. Medication adherence and racial differences in A1C control. Diabetes Care. 2008;31(5):916–921. doi: 10.2337/dc07-1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davidson MB, Karlan VJ, Hair TL. Effect of a pharmacist-managed diabetes care program in a free medical clinic. Am J Med Qual. 15(4):137–142. doi: 10.1177/106286060001500403. [DOI] [PubMed] [Google Scholar]
- 19.Skaer TL, Sclar DA, Markowski DJ, Won JK. Effect of value-added utilities on prescription refill compliance and Medicaid health care expenditures--a study of patients with non-insulin-dependent diabetes mellitus. J Clin Pharm Ther. 1993;18(4):295–299. doi: 10.1111/j.1365-2710.1993.tb00591.x. [DOI] [PubMed] [Google Scholar]
- 20.Odegard PS, Goo A, Hummel J, Williams KL, Gray SL. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Ann Pharmacother. 2005;39(3):433–440. doi: 10.1345/aph.1E438. [DOI] [PubMed] [Google Scholar]
- 21.Rhee MK, Slocum W, Ziemer DC, et al. Patient adherence improves glycemic control. Diabetes Educ. 31(2):240–250. doi: 10.1177/0145721705274927. [DOI] [PubMed] [Google Scholar]
- 22.Bluml BM, Watson LL, Skelton JB, Manolakis PG, Brock KA. Improving outcomes for diverse populations disproportionately affected by diabetes: Final results of Project IMPACT: Diabetes. J Am Pharm Assoc (2003) 2014;54(5):477–485. doi: 10.1331/JAPhA.2014.13240. [DOI] [PubMed] [Google Scholar]
- 23.Iyer R, Coderre P, McKelvey T, et al. An employer-based, pharmacist intervention model for patients with type 2 diabetes. Am J Health Syst Pharm. 2010;67(4):312–316. doi: 10.2146/ajhp090047. [DOI] [PubMed] [Google Scholar]
- 24.Garrett DG, Bluml BM. Patient self-management program for diabetes: first-year clinical, humanistic, and economic outcomes. J Am Pharm Assoc. 2003;45(2):130–137. doi: 10.1331/1544345053623492. [DOI] [PubMed] [Google Scholar]