Abstract
Cesarean scar implantation represents a rare, though growing subset of potentially life-threatening ectopic pregnancy. Because of the global increase in cesarean sections as well as the improved diagnostic abilities of transvaginal ultrasound, incidence rates have continued to rise since the first reported case in 1978. Uterine rupture and catastrophic hemorrhage can ensue when diagnosis is delayed. Additionally, a higher rate of concurrent trophoblastic myometrial invasion may increase the incidence of retained products of conception or post procedural bleeding. Endovaginal ultrasound has a reported sensitivity of 85 % for detection. In difficult cases, magnetic resonance imaging is often useful as a problem solving exam in confirming diagnostic suspicions and guiding therapeutic decisions. We present a series of five illustrative cases illustrating the range of clinical and imaging findings.
Keywords: Ectopic, Cesarean section, Pregnancy, Ultrasound
Sommario
La cicatrice da taglio cesareo rappresenta nella gravidanza ectopica una rara seppur crescente concausa potenzialmente pericolosa per la vita. L’aumento su scala globale della pratica del taglio cesareo, nonostante il supporto dell’applicazione dell’ecografia trans-vaginale sempre più precisa, ha visto crescere i tassi di incidenza a partire dal primo caso riportato nel 1978. Quando la diagnosi è tardiva ne può derivare la rottura dell’utero con conseguente grave emorragia. Inoltre, il verificarsi concomitante di invasione trofoblastica a livello del miometrio potrebbe aumentare l’incidenza dei residui da concepimento o delle emorragie post intervento. L’ecografia trans vaginale ha una capacità diagnostica dell’85 %. Nei casi più difficili, la RM è spesso utile come esame risolutore nel confermare i sospetti diagnostici e guidare quindi verso la terapia appropriata. Vi presentiamo 5 casi esemplificativi che illustrano la varietà di dati clinici ed imaging.
Introduction
Representing only 6 % of all ectopic pregnancies in women who have had a prior cesarean section, scar implantations are relatively uncommon, though thought to be increasing in incidence due to the increasing worldwide rate of c-sections [1–3]. The estimated incidence is 1/2,000 pregnancies or 0.15 % in women who have had at least one prior cesarean delivery [4]. Adenomyosis, in vitro fertilization, prior dilation and curettage and prior manual placental evacuation are additional risk factors [5]. The clinical presentation varies with at least 40 % of detected cases being asymptomatic [6]. Uterine rupture and potentially catastrophic bleeding however can occur with delayed detection. TVUS is the mainstay of diagnosis, with a reported sensitivity of 85 % [4, 7]. The presence of an empty endometrial canal with a low lying, anteriorly positioned gestational sac demonstrating trophoblastic vascularity and a thinned overlying myometrium are key features. Magnetic resonance imaging (MRI) can be a useful adjunctive study in confirming the diagnosis and estimating the extent of potential trans-serosal invasive placentation when present. Therapeutic options include suction evacuation, systemic or local injection of methotrexate or other embryocidal agents with or without uterine artery embolization, versus surgical wedge resection or hysterectomy when necessitated by delayed presentation and need for control of emergent hemorrhage [3, 8, 9].
Case reports
Case 1
A 28-year-old female presented with heavy vaginal bleeding and pain; surgical history was notable for two prior c-sections. Transabdominal and endovaginal ultrasound performed in the emergency room (ER) demonstrated a retroverted uterus with a low lying eccentrically positioned gestational sac and internal fetal pole at the level of the former c-section scar compatible with ectopic implantation. Cardiac activity was observed and fetal age was estimated to be 7 weeks 4 days by crown rump length. Mean sac diameter was 4.5 cm (Figs. 1, 2). Due to the size of the pregnancy and the urgent presentation, emergent laparoscopic hysterotomy and wedge resection was elected and successfully performed. A five-cm bulge in the lower uterine wall was observed on initial laparoscopic inspection corresponding to the sonographic findings of scar implantation. Post-surgical adhesions at the site of the prior bladder flap were noted with no evidence of invasive placentation. The patient tolerated the procedure well. Post-operative recovery was uneventful.
Fig. 1.

Transverse transabdominal ultrasound image shows asymmetric bulging of the lower uterine anterior wall with a vaguely visualized central sonolucency
Fig. 2.
Sagittal transvaginal ultrasound (TVUS) demonstrates a cystic structure eccentrically anterior and low in position in relation to the endometrial canal. Other images better demonstrated a single internal live internal fetal pole with a crown rump length corresponding to 7 weeks 4 days estimated gestational age (EGA). Overlying myometrium appears to be maintained
Case 2
A 35-year-old gravida 3 para 2 (G3P2) female was presented to the ER with intermittent vaginal bleeding. Surgical history notable for prior c-section beta-HCG levels was positive. Transabdominal and endovaginal ultrasound scanning subsequently performed, though limited by body habitus, demonstrated a small 8.5-mm complex cystic structure in the lower uterine wall (Fig. 3). Decidual reaction in the endometrial canal was observed. A questionable yolk sac was observed internally without a definitive fetal pole. Findings were felt suggestive of an early c-section scar ectopic implantation. The patient underwent medical management. Two cycles of intramuscular (IM) methotrexate were given and beta-HCG follow up was performed until normalization.
Fig. 3.
Sagittal TVUS demonstrates an elongated sub-centimeter sonolucency in the lower anterior uterine wall, eccentric in position to the endometrial stripe complex. Internal heterogeneity was noted. No demonstrable fetal pole was seen
Case 3
A 37-year-old G5P4 female, status post 4 prior c-sections, was presented to the ER with complaints of lower abdominal pain and heavy vaginal bleeding. Initial endovaginal exam demonstrated a complex cystic structure with a mean sac diameter of roughly 17 mm in the lower anterior uterine wall. No demonstrable fetal pole or yolk sac could be identified (Figs. 4, 5). Sonographic findings and clinical symptoms persisted without marked decline in quantitative beta-HCG levels despite three cycles of IM methotrexate. Due to failure of medical management, laparoscopic hysterotomy was subsequently performed with successful excision of non-viable ectopic pregnancy and surrounding trophoblastic tissue. Post-operative course was uneventful.
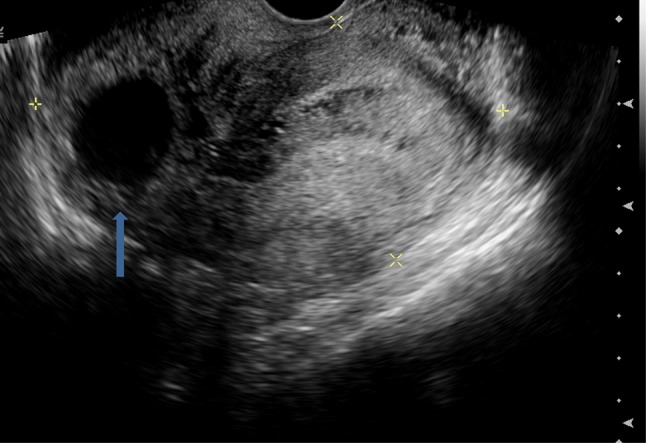
Fig. 4.
Sagittal TVUS at time of presentation demonstrates a 2-cm complex cyst with a central sac-like structure in the lower anterior uterine wall, anterior in position to the endometrial canal
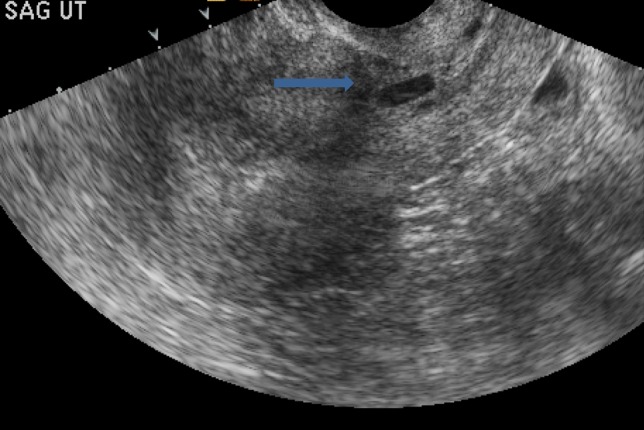
Fig. 5.
Sagittal TVUS with Color Doppler demonstrates surrounding marginal flow
Case 4
A 35-year-old G5P5 female was presented to the ER with a 4 days history of colicky lower abdominal pain and cramping without associated vaginal bleeding or discharge. Surgical history was notable for prior c-section. Endovaginal ultrasound demonstrated a presumed scar ectopic pregnancy at the level of the lower uterine body with a 12 weeks 2 days internal viable fetus (Fig. 6). Because of poor visualization of overlying myometrium sonographically, pelvic MRI was subsequently done to evaluate possible invasive placentation (Fig. 7). No definitive myometrium was observed at the site of the anterior sac margin compatible with placental percreta with mixed low and high T2 signal corresponding to trophoblastic tissue at the site of the prior bladder flap. There was no gross evidence of frank bladder invasion. After pre-operative discussion with the patient, a modified radical hysterectomy was elected and successfully performed. Placental tissue was noted to be protruding through the lower uterine incision with vascularized adhesions extending to the posterior bladder serosa. No frank bladder wall invasion was found. After a slightly prolonged post-operative course complicated by the extent of blood loss at the time of surgery, the patient was discharged in satisfactory condition.
Fig. 6.

Transabdominal ultrasound demonstrates a large gestational sac projecting anteriorly and superior to the demarcated cervical canal and internal os. An internal embryo is partially visualized. The overlying myometrium is markedly thinned with indeterminate integrity prompting subsequent further evaluation with pelvic MRI
Fig. 7.
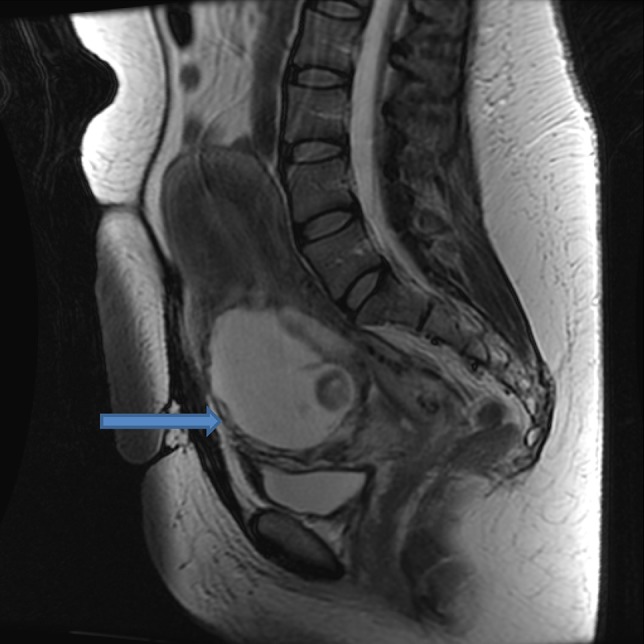
Sagittal fast spin echo (FSE) T2 weighted MRI demonstrates absence of overlying myometrial tissue and band-like areas of low and high T2 signal between the ectopic gestational sac and the bladder suggesting placenta percreta. No gross invasion of the bladder was observed
Case 5
A 33-year-old G3P2 female status post 2 prior c-sections, was presented to the ER with a multi-day history of lower pelvic pain, cramping and intermittent vaginal bleeding. Endovaginal ultrasound showed a 9 weeks 5 days single live pregnancy within the lower anterior uterine body eccentric in position to the endometrial canal. The uterine myometrium was thinned to absent at the site of the anterior sac margin, raising concerns for possible placenta percreta (Fig. 8). Subsequent pelvic MRI demonstrated similar findings with loss of myometrial covering extending over roughly 1 cm. No macroscopic trophoblastic tissue extension was seen into the area of the former bladder flap (Fig. 9). The adjacent bladder wall was unremarkable. After discussion, the patient was admitted for high dose methotrexate therapy with folinic acid rescue. Intracardiac fetal injection of potassium chloride (KCl) was also performed due to the size and age of the ectopic. Clinical recovery was uneventful.
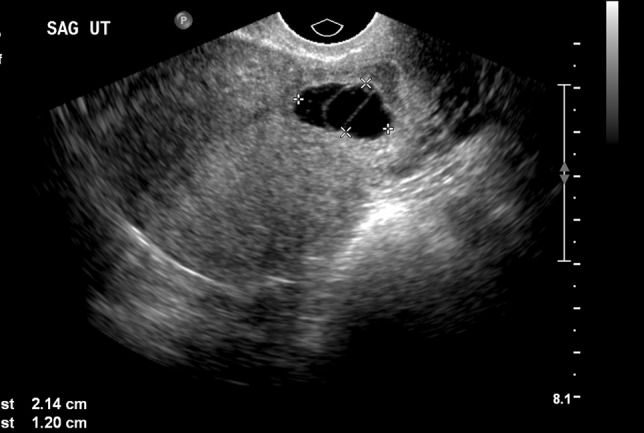
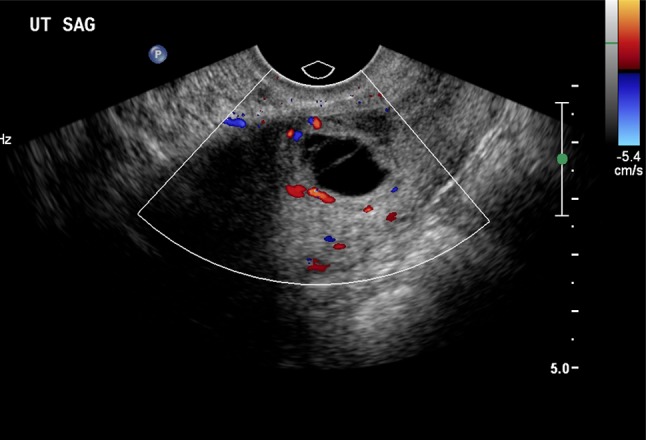
Fig. 8.

Sagittal TVUS image demonstrates a retroflexed uterus with an anterior and inferiorly positioned gestational sac and partially visualized fetal pole. There is severe thinning of the overlying myometrium at the site of the anterior sac margin
Fig. 9.
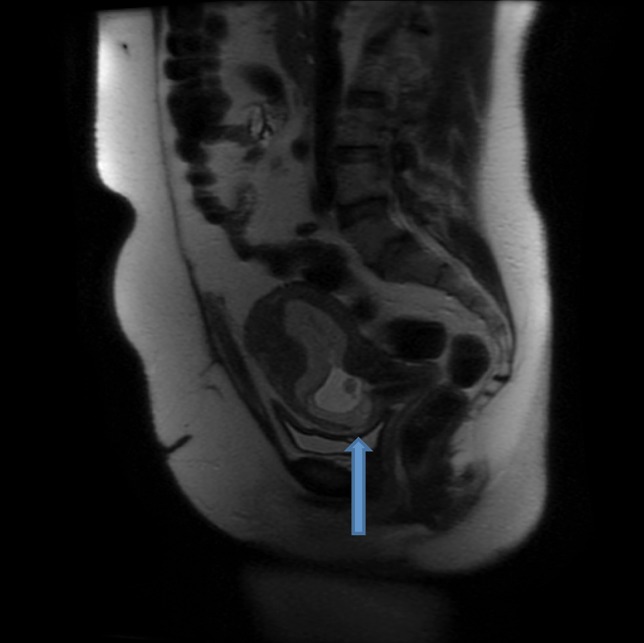
Sagittal FSE T2 weighted MRI demonstrates the inferiorly positioned gestational sac to be bulging anteriorly into the site of the former c-section scar. The overlying low signal myometrium is partially absent approximately 2 cm from the internal cervical os suggesting early placental percreta. No macroscopic trans-serosal extension into the area of the posterior bladder wall was seen
Discussion
Since the first reported case of cesarean scar implantation in 1978, the incidence of this relatively rare form of ectopic pregnancy has been consistently on the rise [1–3]. The overall incidence is now estimated at slightly less than one in every 2,000 pregnancies, with scar implantations representing approximately 6 % of all ectopic pregnancies in women status post at least one prior c-section [1].
Clinical presentation, aside from incidental detection in approximately 40 % of cases, ranges from vaginal bleeding and pelvic pain to uterine rupture and hemodynamic instability. Almost all cases are detected in the first trimester with an average range of 5–12 weeks [10]. In addition to prior c-sections, clinical risk factors also include adenomyosis, in vitro fertilization, prior dilation and curettage and prior manual placental evacuation [5].
Endovaginal ultrasound has a reported sensitivity of 85 % for detection [7]. Diagnosis hinges on the visualization of a gestational sac which is low and anterior in position in relation to the endometrial stripe complex with attenuated overlying myometrium typically measuring five mm or less in thickness. In one recent series of 77 patients, the average distance measured sonographically between the uterine serosa and the anterior trophoblastic border was 1.6 mm [11]. Color Doppler can be useful in detecting trophoblastic flow surrounding a viable gestational sac in contrast to the more avascular misshapen sac seen in conjunction with a low lying abortion in progress [12]. Differential diagnostic considerations include a diverticulum of entrapped physiologic fluid within a partially dehiscent c-section or post myomectomy scar.
Pelvic MRI has shown utility anecdotally as an adjunctive tool in problem cases not only in confirming initial imaging suspicions but also in further delineating possible extension of placental tissue beyond the uterine serosa. Sagittal and axial T2 weighted images best show preservation or absence of the low signal overlying outer myometrium and serosa in relation to the hyperintense sac and decidual tissue. Band-like fibrous areas of low T2 signal have also been described within the T2 hyperintense invasive trophoblastic tissue [6].
Several treatment options including both medical and surgical approaches exist for scar ectopics. Systemic or local injection of methotrexate or other embryocidal agents such as KCl or hyperosmolar glucose has been commonly used. Systemic methotrexate is most efficacious when used during the first 6 weeks of gestational age when beta-HCG levels are still lesser than 5,000 mIU/ml [10]. Surgical treatments include suction aspiration of the sac, dilation and curettage, hysteroscopy, or, in more advanced/urgent cases, wedge resection or hysterectomy [6]. More recently, in one study of 66 patients desiring to maintain fertility, uterine artery embolization used in conjunction with local methotrexate administration, were found to have the highest success rate with a lower chance for treatment failure and urgent hysterectomy [13].
In conclusion, scar implantations represent a rare, though increasing, subset of ectopic pregnancies of which it behooves the vigilant sonologist to be cognizant. Endovaginal ultrasound imaging affords a reliable and sensitive means of detecting the abnormally positioned sac. Color Doppler can aid in delineating the increased vascularity of the trophoblastic tissue. When necessary, MRI may prove a useful adjunct in confirming the initial impression and potentially delineating trans-serosal extension of invasive placentation.
Conflict of interest
The authors, M Rheinboldt, Z Delproposto, and D Osborn, declare that they have no conflicts of interest.
Ethical standard
All data was collected retrospectively in accordance with the laws of the United States for patient confidentiality and current 2015 Health and Insurance Portability and Accountability Act Standards (HIPAA) and also met with 2015 Henry Ford Hospital internal review board ethical standards and compliance and approval.
References
- 1.Ash A, Smith A, Maxwell D. Caesarean scar pregnancy. BJOG. 2007;114(3):253–263. doi: 10.1111/j.1471-0528.2006.01237.x. [DOI] [PubMed] [Google Scholar]
- 2.Maymon R, Halpern R, Mendlovik S, et al. Ectopic pregnancies caesarean section scars: the 8 year experience of one medical centre. Hum Reprod. 2004;19(2):278–284. doi: 10.1093/humrep/deh060. [DOI] [PubMed] [Google Scholar]
- 3.Maymon R, Halpern R, Mendlovik S, et al. Ectopic pregnancies in a ceasarean scar: review of the medical approach to an iatrogenic complication. Hum Reprod. 2004;10(6):515–523. doi: 10.1093/humupd/dmh042. [DOI] [PubMed] [Google Scholar]
- 4.Rotas M, Haberman S, Levgur M. Caesarean scar ectopic pregnancies: etiology, diagnosis, and management. Obstet Gynecol. 2006;107(6):1373–1381. doi: 10.1097/01.AOG.0000218690.24494.ce. [DOI] [PubMed] [Google Scholar]
- 5.Vial Y, Petignat P, Hohlfeld P. Pregnancy in a caesarean scar. Ultrasound Obstet Gynecol. 2000;16(6):592–593. doi: 10.1046/j.1469-0705.2000.00300-2.x. [DOI] [PubMed] [Google Scholar]
- 6.Wu R, Klein M, Mahboob S, Gupta M, et al. Magnetic resonance imaging as an adjunct to ultrasound in evaluating cesarean scar ectopic pregnancy. J Clin Imaging Sci. 2013;3:16. doi: 10.4103/2156-7514.109758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fylstra D. Ectopic pregnancy within a cesarean scar: a review. Obstet Gynecol Surv. 2002;57:537–543. doi: 10.1097/00006254-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Lee C, Wang C, Chao A, Yen C. Laparoscopic management of an ectopic pregnancy in a previous caesarean section scar. Hum Reprod. 1999;14(5):1234–1236. doi: 10.1093/humrep/14.5.1234. [DOI] [PubMed] [Google Scholar]
- 9.Graesslin O, Dedecker F, Quereuz C, et al. Conservative management of ectopic pregnancy in a cesarean scar. Obstet Gynecol. 2005;105(4):869–871. doi: 10.1097/01.AOG.0000141569.75297.44. [DOI] [PubMed] [Google Scholar]
- 10.Seow K, Huang L, Lin Y, et al. Cesarean scar pregnancy: issues in management. Ultrasound Obstet Gynecol. 2004;23(3):247–253. doi: 10.1002/uog.974. [DOI] [PubMed] [Google Scholar]
- 11.Moschos E, Wells C, Twickler D. Biometric sonographic findings of abnormally adherent trophoblastic implantations on cesarean delivery scars. J Ultrasound Med. 2014;33(3):475–481. doi: 10.7863/ultra.33.3.475. [DOI] [PubMed] [Google Scholar]
- 12.Jurkovic D, Jauniaux E, Kurjak A, et al. Transvaginal color doppler assessment of the uteroplacental circulation in early pregnancy. Obstet Gynecol. 1991;77:365–369. [PubMed] [Google Scholar]
- 13.Yang X, Yu H, Li K, et al. Uterine artery embolization combined with local methotrexate for treatment of caesarean scar pregnancy. BJOG. 2010;117:990–996. doi: 10.1111/j.1471-0528.2010.02578.x. [DOI] [PubMed] [Google Scholar]


