Dear Editor,
The carotids are easily accessible with ultrasound. Since these vessels are superficial structures, high-quality images are obtainable in most patients. At respect, the proposal of Gassner et al. [1] regarding the Doppler ultrasonographic estimation of the cardiac output through the calculation of the volume flow at the common carotid artery (CCA-CO) is interesting, simple and attractive, and the authors’ efforts to promote their findings are commendable. Nevertheless, some technical points should be considered.
Volumetric blood flow measurement using ultrasound is obtained as follows:
Volume flow = Cross-sectional Area (A, not the diameter (D) as is stated in Gassner’s study) × Time-averaged velocity (TAV) [2, 3].
The A is obtained as π × radius2 (or its equivalent, D2 × 0.785), assuming that the vessel is circular in cross-section (e.g. arterial vessels).
TAV can be estimated from the intensity-weighted mean frequency (TAMEAN) or from the maximum frequency (TAMAX, also known as time-averaged peak velocity or TAP) over an integral number of cardiac cycles [4].
In the example provided in the Fig. 1 corresponding to Gassner’s study [1], the velocity used for calculation of volume flow is TAP (represented with a continuous yellow line delineating the maximum velocities of the Doppler spectrum occurring along the cardiac cycle). CCA diameter is 0.65 cm, derived A is 0.33 cm2, A × TAP (34.8 cm/s) is 11.54 cm3 or ml/s and finally volume flow in ml/min is obtained multiplying the last value by 60 (to convert seconds to minute), equal to 693 ml/min (the same value as in figure).
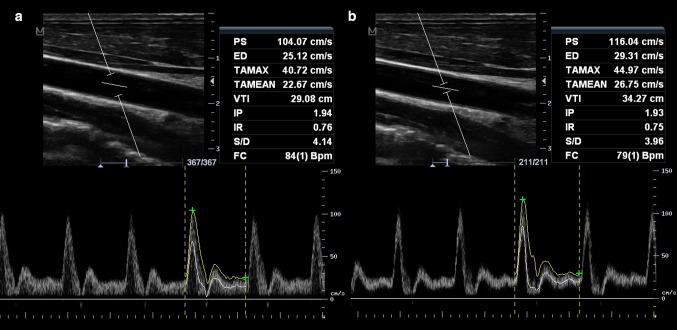
Fig. 1.
Spectral Doppler of the common carotid artery (CCA), obtained with pulsed-wave Doppler. Sample volume encompasses the whole vessel diameter. Time-averaged maximum velocity [TAMAX (also called TAP), represented with a continuous yellow line delineating the maximum velocities of the spectrum occurring along the cardiac cycle] and time-averaged mean velocity (TAMEAN, represented with a continuous white line delineating the mean velocities of the spectrum occurring along the cardiac cycle) were obtained. Of note, TAMAX and TAMEAN values are different, with TAMEAN lower than TAMAX. Cross-sectional area was estimated in 0.28 cm2, and the resultant volume flow measurements were 684 ml/min using TAMAX and 376 ml/min with TAMEAN
It is important to differentiate TAMAX versus TAMEAN since these are different averaged velocities and thus the resultant calculation of volume flow varies when one or the other is used [2, 4] (Fig. 1).
When blood is subjected to high acceleration, such as flow through valve orifices within the heart or aortic arch, the flow velocity profile is known as “plug or flat”, which means that velocities are uniform along the cross-section of the vessel or valve. In this case, velocities in the center of the vessel are nearly the same in comparison with the peripheral velocities, resulting in TAP similar to TAMEAN [2, 4].
In contrast, in parabolic flow profile, velocities are not constant along the cross-section of the vessel, with highest velocities in the center and lowest along the vessel walls. The net volume flow includes the averaging of all range of velocities. Thus, in parabolic flow, TAMEAN is not equal (is lower) than TAP [2, 4].
In real conditions, velocity profile in arteries (such as CCA) usually falls somewhere between parabolic and flat, with most of the flow during systole having a velocity profile more or less flat and then becoming parabolic at end-systole and diastole [4, 5].
In sum, TAP is derived from maximum or peak velocities (maximum Doppler shift along the cardiac cycle) and TAMEAN is obtained with all range velocities (mean Doppler shift along the cardiac cycle).
The practical conclusion is that at a constant cross-sectional area, the measurement of volume flow using TAP is higher in comparison with calculated blood flow using TAMEAN.
With respect to the effect of sample volume in determining the TAP and TAMEAN, in plug velocity profile, mean velocity measurements in a vessel will be of similar accuracy regardless of the sample volume dimensions. A parabolic profile, however, will overestimate the TAMEAN as the sample volume decreases below the size of the vessel, since faster velocities are found in the center. In this case, if gate is enlarged so that it encompasses the vessel from top to bottom, TAMEAN becomes representative of the net flow (all ranges of velocities) across the vessel [2, 3].
These theoretical notions indicate that accurate volumetric measurements of blood flow should be performed using the following principles:
The sample volume must include the whole internal diameter of the vessel and thus all ranges of velocities will be recorded; (Fig. 2)
Time-averaged mean velocity (TAMEAN) is preferable over maximal or peak (TAP or TAMAX).
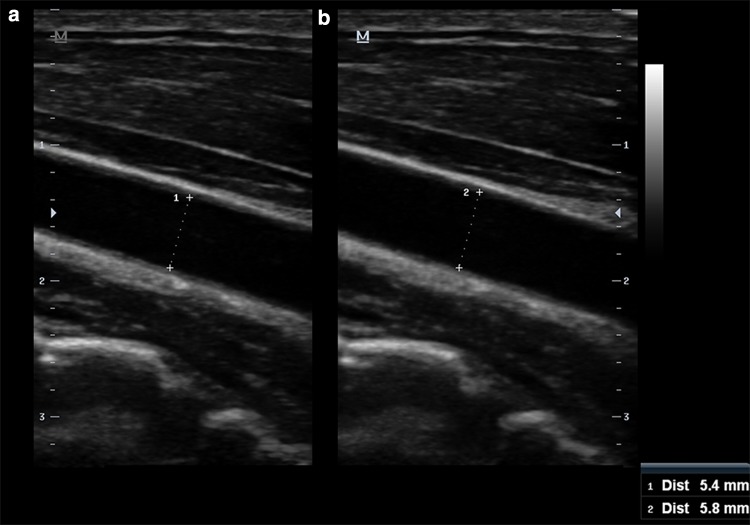
Fig. 2.
Doppler ultrasound of the CCA, with sample volume encompassing the whole diameter of the vessel (a) and with the sample volume in the center of the vessel (b). Broadening of the Doppler spectrum is demonstrated (a), indicating the recording of all range of velocities. TAMEAN is also lower in a as expected
Returning to the Gassner’s study, volume flows obtained in CCA are higher (315–1510 ml/min) in comparison with reference values in healthy patients also obtained with the Doppler method (around 420 ± 100 ml/min) [6, 7]. This discrepancy is probably explained due to the use of TAP in the authors’ study instead of TAMEAN for calculation of volume flow.
In concrete, differences in CO obtained with invasive measurements in comparison with CCA-CO are probably higher than expressed in Gassner’s study if TAMEAN is used in calculation of the volume flow. However, if volume flow calculated using TAP has good accuracy in estimating the CO, is TAP preferable over TAMEAN for this purpose? What will happen when comparing CCA-CO (TAP vs. TAMEAN) with other CO measuring techniques (e.g. echocardiography)? Did CCA-CO using TAP as well as invasive CO measurements overestimate the real CO? These are probably some reasons highlighting the need for further studies.
Another not irrelevant point of the Gassner’s study is the well-proposed standardization technique (important for intra- and inter-reproducibility of the technique) when measuring CCA velocities and CCA diameter at the level of the thyroid gland. However, at least of equal importance, the angle correction of beam insonation with respect to the vessel also needs standardization. It is well known that if beam-flow angle is made >60°, large error occurs in calculated velocities. Interestingly, when the Doppler angle is changed from 40° to 60°, the computed Doppler velocity increases by 42 or 2.1 % per degree [8]. This means a possible large variability in calculated velocities (and thus in calculated volume flow) when a different corrected angle is used, even if lower of 60°. For standardization purposes, the angle correction should better have a constant value, preferable at 60° (most actual ultrasound machines have this value as a standard). Instead of the constant 60° of angle correction, proper alignment between the vessel and beam must be correct; otherwise, disparities in calculated velocities also occur.
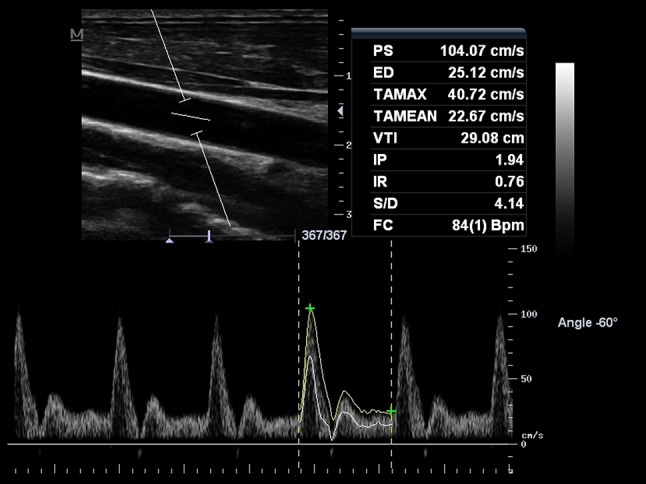
Finally, the cross-sectional area is calculated with the CCA diameter (D). The D of the CCA (and thus the CCA area) commonly changes along the cardiac cycle (systolic dimensions larger than diastolic) (Fig. 3). Observing the formula for calculation of A, small errors in measurement of the D result in large errors in A (squared), and thus in volume flow calculation. The measurement of D must be performed at largest CCA dimension (systole) and in possible exactly at the same site where the sample volume is placed, being D measurement guaranteed in longitudinal view.
Fig. 3.
Measurement of the diameter of the CCA. a Diastolic frame; b systolic frame. The systolic diameter is larger in comparison with the diastolic diameter. Note the effect in calculated area of 0.23 cm2 (a) and 0.26 cm2 (b)
Conflict of interest
The author has no conflict of interest to disclose.
Human and animal studies
The study described in this article does not contain studies with human or animal subjects performed by the author.
References
- 1.Gassner M, Killu K, Bauman Z, Coba V, Rosso K, Blyden D. Feasibility of common carotid artery point of care ultrasound in cardiac output measurements compared to invasive methods. J Ultrasound. 2014 doi: 10.1007/s40477-014-0139-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gill RW. Measurement of blood flow by ultrasound: accuracy and sources of error. Ultrasound Med Biol. 1985;11(4):625–641. doi: 10.1016/0301-5629(85)90035-3. [DOI] [PubMed] [Google Scholar]
- 3.Holland CK, Brown JM, Scoutt LM, Taylor KJ. Lower extremity volumetric arterial blood flow in normal subjects. Ultrasound Med Biol. 1998;24(8):1079–1086. doi: 10.1016/S0301-5629(98)00103-3. [DOI] [PubMed] [Google Scholar]
- 4.Li S, Hoskins PR, Anderson T, McDicken WN. Measurement of mean velocity during pulsatile flow using time-averaged maximum frequency of Doppler ultrasound waveforms. Ultrasound Med Biol. 1993;19(2):105–113. doi: 10.1016/0301-5629(93)90002-6. [DOI] [PubMed] [Google Scholar]
- 5.Daigle RJ. Arterial hemodynamics, anatomy and physiology. In: Daigle RJ, editor. Techniques in non-invasive vascular diagnosis: an encyclopedia of vascular testing. 3. Littleton: Summer Publishing; 2008. pp. 141–158. [Google Scholar]
- 6.Scheel P, Ruge C, Schöning M. Flow velocity and flow volume measurements in the extracranial carotid and vertebral arteries in healthy adults: reference data and the effects of age. Ultrasound Med Biol. 2000;26(8):1261–1266. doi: 10.1016/S0301-5629(00)00293-3. [DOI] [PubMed] [Google Scholar]
- 7.Yazici B, Erdoğmuş B, Tugay A. Cerebral blood flow measurements of the extracranial carotid and vertebral arteries with doppler ultrasonography in healthy adults. Diagn Interv Radiol. 2005;11(4):195–198. [PubMed] [Google Scholar]
- 8.Beach KW, Bergelin RO, Leotta DF, Primozich JF, Sevareid PM, Stutzman ET, Zierler RE. Standardized ultrasound evaluation of carotid stenosis for clinical trials: University of Washington Ultrasound Reading Center. Cardiovasc Ultrasound. 2010;8:39. doi: 10.1186/1476-7120-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]