Abstract
The use of alcohol and other drugs (AODs) is an important driver of gender disparities in HIV prevalence. Consequently, there is a need for women-specific HIV interventions that are conceptualized to address (1) women’s risk behavior, their roles in sexual relationships, and gender power dynamics, and (2) other issues commonly faced by women who use AODs, such as gender-based violence and victimization. This article presents the evolution of HIV prevention intervention research with women who use AODs. It looks at three generations of women-focused HIV research interventions, including first-generation projects that started in the 1990s, second-generation efforts where projects expanded in scope and included adaptions of evidence-based interventions for global relevance, and finally third-generation projects currently underway that combine biobehavioral methods and are being implemented in real-world settings. Because women who use AODs continue to report risk behaviors related to HIV, emphasis should be placed on training scientists to conduct gender-specific studies, increasing funding for new studies, and advocating to ensure that stigma-free services are available for these at-risk women.
Keywords: Gender disparity, women-focused HIV prevention, alcohol and other drug use, sex risk, women-specific HIV interventions
Introduction
The use of alcohol and other drugs (AODs) is an important driver of gender disparities in HIV prevalence. Research has shown that alcohol as well as other drug use among women leads to disinhibition and impaired judgment that may result in inconsistent condom use and other risky sex behaviors.1,2 AOD-using women may engage in unsafe sex practices, such as trading sex in exchange for AODs (or money to buy AODs) for themselves or their sex partners1,3–5 or they may use AODs to cope with sex trading.6,7 In such exchanges, women have limited agency to negotiate condom use and other preventive behaviors, especially if they are under the influence of AODs.6,8 This puts AOD-using women at high risk of contracting HIV and other sexually transmitted infections (STIs).9–13 Furthermore, women who inject drugs lack agency in negotiating safer injection practices with injecting sex partners, increasing the possibility of contracting HIV.14,15 Gender differences in injection practices also increases HIV risk among women who inject drugs. For example, women are more likely to use works (injection equipment) after men, which increases their chance of exposure to HIV.16
Women who use AODs are at especially high risk for heterosexual transmission of HIV, as they are often in sexual relationships with men who use AODs and who also participate in high-risk behaviors.17 In addition, compared with men, women are more biologically susceptible to HIV through sexual transmission.18 Accordingly, these intersecting risk behaviors associated with AOD use among women translate into greater gender disparities in HIV. Other contextual and structural factors also impact women’s risk for HIV. For instance, women who use AODs often have histories of abuse and experience intimate partner violence.3,6,19,20 There is strong evidence that experiences of partner abuse and gender-based violence are directly associated with HIV risk among women.21 Furthermore, women who use AODs and live in cultural contexts where men have all the decision-making power and are in control of the financial resources may lack the agency to negotiate protective behaviors, augmenting their risk for HIV and other diseases.22
Despite the significant need for women-specific preventive and reproductive healthcare among this highly vulnerable population, when women who use AODs seek health services they are often stigmatized, discriminated against, and treated poorly.23–26 In other instances, they are ignored, given incorrect information, and disrespected by staff, which discourages them from seeking services.27,28 Moreover, when women do seek services, many facilities do not offer childcare, clinic hours are inconvenient, and waiting times are long.29,30 All of these factors have been identified as barriers to seeking and initiating health and AOD treatment services.31,32 These barriers contribute to gender disparities in health outcomes among women who use AODs, with a recent study reporting substantially higher mortality rates among female drug users in Central Asia compared with their male counterparts.33
Despite these gender disparities in HIV risk and health outcomes, early HIV prevention intervention studies did not focus exclusively on AOD-using women and their unique needs, and it took a generation of HIV interventions before women-focused approaches to HIV prevention began to emerge.34,35 Whether all HIV prevention approaches for women who use AODs should be gender- and women-specific can be debated, given that policy, fiscal, cultural, and training resources can be a challenge and overall risk-reduction among both men and women must be considered foremost. Although the terms gender-specific and women-focused may have different meanings when speaking about single-sex interventions, they are used interchangeably in the literature. In this article, we focus on women-focused HIV interventions that are conceptualized to address (1) women’s risk behavior, roles in sexual relationships, and gender power dynamics, and (2) other issues commonly faced by many women, such as gender-based violence and victimization.
Substantial progress has occurred in the development of women-focused behavioral HIV prevention interventions over the past couple of decades, as National Institute on Drug Abuse (NIDA) sponsored intervention research has aimed to reach hard-to-reach and vulnerable AOD-using women at risk for HIV. In the past decade there has been an increasing emphasis on evidence-based approaches to behavioral prevention of HIV. However, there are still relatively few evidence-based HIV prevention interventions globally for women who use AODs.36 For example, out of 84 evidence-based behavioral risk-reduction interventions listed on the US Centers for Disease Control’s Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention, only three are specifically designed for women who use AODs,13,37,38 and one is listed for couples who use AODs.39 Nonetheless, women-focused interventions and their components have evolved as the science has advanced.
The evolution of women-focused HIV prevention interventions
Historically, there have been three generations of women-focused HIV prevention interventions (see Table 1). The first-generation HIV interventions, implemented in the 1990s, were pioneering in their efforts. All of the first-generation HIV interventions were conducted in the United States and have evolved over time. Most of the first-generation HIV prevention interventions for women targeted HIV/AIDS knowledge and increasing condom use, and only one was specifically for women of color.40 While these first-generation interventions addressed HIV risk, they did not address the other contextual factors that influence a woman’s ability to take protective action and reduce sex risk behavior, such as gender-based violence and female empowerment. Some of the early interventions funded by NIDA in the United States that targeted women who inject drugs, crack cocaine smokers, and sex partners of men who inject drugs did include components on negotiating condom use without risking partner and gender-based violence.41 These were usually delivered in a women-only session, but they did not occur in the context of a larger gender-specific intervention.
Table 1.
Characteristics of First-, Second-, and Third-Generation Women-focused Interventions for HIV Prevention among Women Who Use Alcohol and Other Drugs
| Components and outcomes | First Generation |
Second Generation |
Third Generation |
|---|---|---|---|
| Women’s group | • | • | • |
| Male condom use skills | • | • | • |
| Female condom use skills | • | • | • |
| Negotiation | • | • | • |
| US based | • | • | • |
| Assertiveness training | • | • | • |
| Sexual risk and drug use outcomes | • | • | • |
| One-on-one risk reduction | • | • | • |
| Cultural/ethnic tailoring | • | • | |
| Sex workers | • | • | |
| International focus and adaptations | • | • | |
| Comorbidity, HIV-positive, distress | • | • | |
| Focus on risks noninjecting | • | • | |
| Criminal justice | • | • | |
| Gender-based violence | • | • | |
| Contextual: homelessness, employment | • | • | |
| Health disparities and social determinants | • | • | |
| Stigma and accessing services | • | • | |
| Biomedical components(ART, microbicide, adherence) | • |
Note. ART=antiretroviral therapy
Beginning in 2000, a number of HIV interventions were expanded to contain culturally sensitive, women-specific content addressing contextual influences on risk behaviors or to include economic enhancement strategies, based on the recognition of the importance of interventions tailored for the unique needs of women.42,43 These second-generation HIV interventions advanced the first-generation interventions by also addressing a range of contextual factors (e.g., gender-based violence, homelessness, employment, female empowerment) that impede or facilitate women’s ability to implement HIV prevention strategies. Many of these second-generation interventions involved adaptations of the first-and second-generation interventions and several expanded to countries outside of the United States. They also began to focus on subgroups of vulnerable women, such as sex workers and currently or recently incarcerated women. Some had been adapted for couples who use AODs.
Around 2010, third-generation interventions emerged. These interventions added biomedical components to the behavioral intervention base of the second-generation interventions. For example, they provide antiretroviral therapy (ART) to women living with HIV to reduce infectiousness and pre-exposure prophylaxis (PrEP) to serodiscordant partners.
This article provides a historical review of each generation of women-focused HIV interventions, explores the challenges to delivering these interventions, and discusses directions in which these interventions need to develop to better prevent HIV among women who use AODs.
Methods
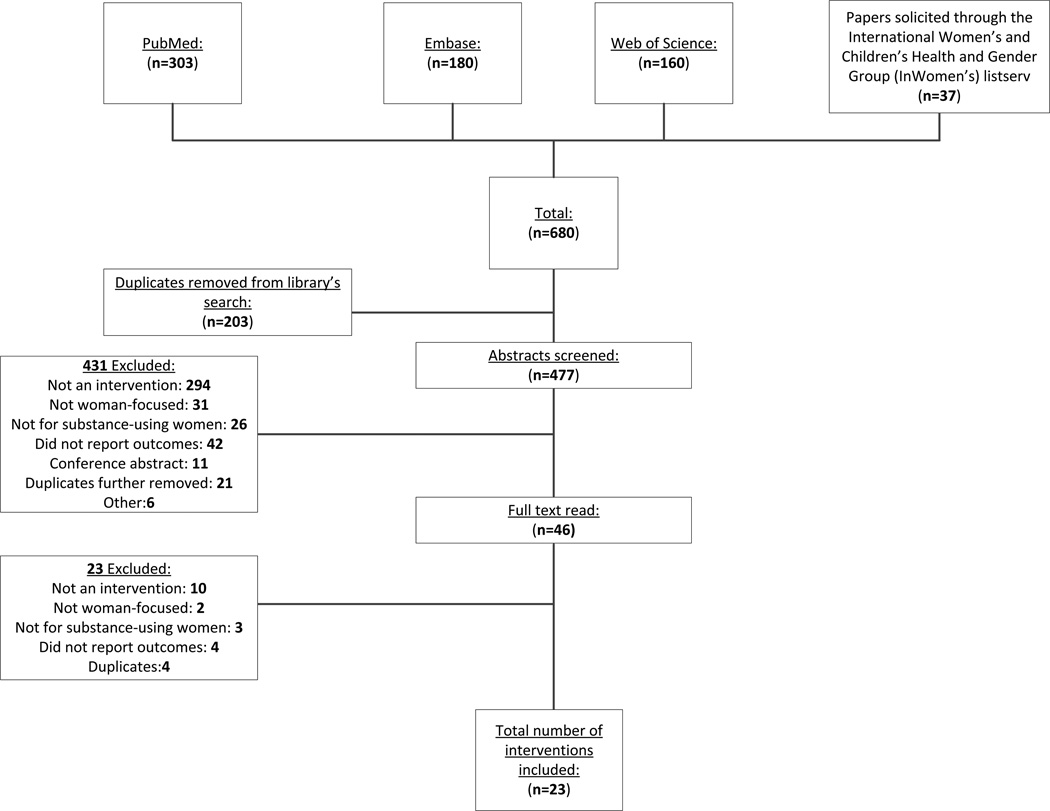
We worked with a professional reference librarian to develop a search strategy. Once we had a satisfactory search strategy, the librarian conducted searches on Medline via PubMed, Embase, and ISI Web of Science for articles and abstracts related to substance use and HIV prevention interventions for women that had been published since 1990. The search strategy is shown in Appendix 1. Searches were conducted between November 2014 and January 2015. All searches were limited to English-language articles only. We conducted separate searches for women-specific interventions and interventions for AOD-using heterosexual couples as gender-specific interventions involving women. To supplement this search strategy, we sent out a request for additional articles over the International Women’s and Children’s Health and Gender Group (InWomen’s) listserv.44 This group includes many of the researchers who conduct gender-specific HIV prevention intervention studies. Although we made our search as comprehensive as possible, we did not conduct a formal systematic review, which would have involved searching all conference abstracts and contacting authors of unpublished manuscripts. The combined searches returned 680 results, with 203 duplicated results.
To be included in this review, articles had to report on a randomized controlled trial of a women-focused HIV prevention intervention; target AOD-using women; and report on at least one of the following outcomes—(a) sex risk behaviors, including condom skills, (b) injection risk behaviors, (c) HIV incidence, or (d) AOD use. We reviewed the abstracts generated by the search and subsequently obtained copies of all manuscripts that clearly met the inclusion criteria. We also obtained manuscripts for all cases where the information in the abstract was insufficient to make a determination.
The most common reasons for exclusion were that the article did not report on an intervention (n=304), the intervention was not gender-specific (n=33), the intervention did not focus on women who use AODs (n=29), and the article did not report on our specified outcomes (n=46). A total of 23 studies met the inclusion criteria (see Appendix 2).
Results
Our search identified four first-generation interventions, all of which were conducted in the late 1980s and early 1990s. These interventions helped to establish the feasibility and acceptability of women-focused interventions for women who use AODs. All but one these interventions reported efficacy on at least one of the outcomes of interest. These studies also provided initial evidence that interventions may be efficacious in reducing HIV risk among vulnerable women. As such, these first-generation interventions laid the foundation for the next generation of interventions to follow.
We identified 19 interventions that met the criteria for second-generation women-focused interventions for women who use AODs, which also included couple-focused interventions for couples who used AODs. Among these 19 second-generation interventions, 11 were tested in studies conducted in the United States and 8 were tested in other countries, including Mexico, Mongolia, Russia, and South Africa. Sex risk reduction was a specific focus of 18 of the second-generation interventions; 14 included a focus on reducing AOD use; 4 included activities to reduce injection risk; and 6 included activities to reduce risk of victimization. All but two studies found efficacy in the women-focused arm. The second-generation interventions developed newer methods and innovations, such as computerized instrumentation, multimedia components and video storytelling, and microeconomics.45 A detailed description of these first- and second-generation interventions and their outcomes is presented in Tables 2 and 3, respectively.
Table 2.
Randomized Trial Results of First-Generation Women-Focused HIV Prevention Interventions for Women Who Use Alcohol and Other Drugs
| Intervention Characteristics | ||||||
|---|---|---|---|---|---|---|
| Gen | Study | Population/Setting | Aim | Description | Comparison Condition | Findings |
| 1st | Schilling et al., 199154 | New York, USA black and Hispanic women; n=91 | To compare intervention effects on AIDS knowledge, sexual risk behaviors, and drug use | AIDS education and skills building; five 2-hour sessions; information on AIDS transmission and prevention; visual and didactic exercises; condom use with models; assertiveness training; role-play | Information only control arm; one session of AIDS information routinely provided by the clinic | Increase in frequency of safer sex discussion in the intervention arm compared with control More frequent condom use in the intervention arm compared with control A significantly greater percentage of participants in the intervention arm reduced their sexual risk behavior compared with control |
| 1st | Nyamathi et al., 199340 | California, USA; African American and Latina women; n=858 | To compare intervention effects on cognitive, behavioral, and psychological factors in relation to HIV risk | Culturally specific; 2-hour program of AIDS education and HIV antibody counseling; individualized to group’s concerns; risk reducing behaviors; needle and syringe disinfection; enhancing self-esteem and control; video shown on risk behaviors associated with HIV | Traditional intervention; 1-hour small group format; video on risk behaviors, testing, and bleach kits | Pre-post improvements on most outcomes were reported by participants in both arms Overall participants in the control arm reported greater improvements on most outcomes than participants in the intervention arm |
| 1st | Kelly et al., 199455 | Wisconsin, USA; high-risk women 18–40; n=197 | To compare intervention effects on use of condoms and knowledge of HIV/STD risk | HIV/AIDS risk reduction intervention; 4-weekly 90-minute sessions; sessions on HIV risk and misconceptions; reducing risk, role-play discussion of condom use; condom demonstration; high-risk behavior triggers; peer support | Three 90-minute group sessions on topics unrelated to AIDS but relevant to low-income women; nutrition; meal preparation | Decrease in the frequency of unprotected sex in the intervention arm compared with control Higher increase in condom use in the intervention arm compared with control Greater increase in sexual negotiation and assertive communication skills in the intervention arm compared with control |
| 1st | Harris et al., 199856 | Eastern USA; Methadone-dependent African American women; n=204 | To compare intervention effects on high-risk behavior, self-esteem, and depressive affect | 16-week peer counseling and leadership training (PCLT); usual methadone maintenance activities; based on increasing self-esteem and control; sex and sexuality; implications for drug use and sexual behavior; concerns about AIDS; importance of disclosure | Usual methadone maintenance clinic activities; pre- and posttest only | Safer sex was significantly higher than in the control Participants in the intervention arm reported less depression following the training sessions compared with control |
Table 3.
Randomized Trial Results of Second-Generation Women-Focused HIV Prevention Interventions for Women Who Use Alcohol and Other Drugs
| Intervention Characteristics | ||||||
|---|---|---|---|---|---|---|
| gen | Study | Population/Setting | Aim | Description | Comparison Condition | Findings |
| 2nd | Van Devanter et al., 200257 | New York, Maryland, Washington, USA; women at high risk for HIV/STDs; n=604 | To compare intervention effects on risks associated with HIV/STDs among women with high-risk behaviors | Women in Group Support (WINGS); 6 weekly group sessions based on education, motivation, and behavioral skills; STD/HIV information, skills training; goal setting; female condom training | 1-hour session featuring a nutrition video on healthy food choices | Greater percentage of women tried the female condom in the WINGS arm compared with control Reported higher frequency of female condom use in the WINGS arm compared with control Significantly more positive attitudes toward the female condom in the WINGS arm compared with control Significantly greater skill in using the female condom on a model in the WINGS arm compared with control |
| 2nd | Sterk et al., 200358 | Georgia, USA; African American crack-cocaine using women; n=265 | To compare intervention effects on drug use and HIV sexual risk behaviors | The Health Intervention Project; two gender-specific interventions–4 sessions each and action plans: enhanced motivation reduce HIV risk, triggers for relapse; enhanced negotiation risk reduction and communication |
NIDA Standard Intervention* | Participants in the negotiation arm were more likely to increase the frequency of condom use with a steady partner than the control Participants in the negotiation arm reported a greater reduction in the number of times they had sex with a paying partner compared with the motivation arm and with the control |
| 2nd | Wechsberg et al., 200438 | North Carolina, USA; African-American crack-using women; n=620 | To compare intervention effects on sex risk behaviors, drug use, and employment and housing status | Women’s CoOp (WC); women-focused intervention; 4 modules; two 30- to 40-minute individual and two 60 to 90-minute group sessions over 6 weeks; HIV risk; drug use; risk reduction strategies; skills training; problem solving; focus on health; family; stress reduction, action plan | NIDA Standard Intervention* A delayed-treatment control arm |
Compared with participants in the control arm, WC participants reported significantly less crack use, sex trading, were less likely to be homeless and more likely to report full time employment at three month follow-up |
| 2nd | Wechsberg et al., 20066 | Pretoria, South Africa; women who reported recent substance use and sex trading; n=93 | To compare intervention effects on at-risk sex behaviors and AOD use by promoting condom use, and AOD education and skill | Women’s Health CoOp (WHC); adapted from US study; two one-on-one sessions held within 2 weeks for 1 hour each; addressed HIV/AIDs issues; assessment of drug and sexual risks; set goals to negotiate risk-reduction communication about condom use; violence prevention strategies; issues relevant to sex work; action plans | NIDA Standard Intervention* | Participants in the WHC intervention were half as likely to report daily alcohol use, less likely to report cocaine use, being victimized less, report unprotected sex, and condom use at last sex compared to standard participants at one-month follow-up |
| 2nd | Tross et al., 200837 | United States; women in methadone treatment; n=515 | To compare intervention effects on the number of unprotected sexual occasions among women in methadone or psychosocial treatment programs | HIV/STD safer sex skills building (SSB); five 90-minute sessions; risk reduction skills; designed to build skills for safer sexual decision making; active problem solving; role-play; peer feedback and support; negotiation | HIV/STD education; single 60-minute group session; HIV/STD definitions; testing and counseling |
Participants in the SSB arm had fewer unprotected sexual occasions (USOs) compared with control at six month follow-up |
| 2nd | Patterson et al., 200859 | Tijuana and Ciudad Juarez, Mexico; female sex workers; n=924 | To compare intervention effects on condom use negotiation and to ensure that condoms are consistently used during commercial sex transactions | Safe Woman Intervention (Mujer Segura);35-minute intervention; motivational interviewing; role-play to improve self-efficacy with clients; action plans; condom use; negotiating safer sex; social support | Didactic Control; face-to-face 35-minute intervention on materials from the US CDC guidelines for HIV counseling, testing, and referral | Significant increase in protected sex acts and percentage of times condoms were used in the Mujer Segura arm compared with control Significant decrease in unprotected sex acts used in the Mujer Segura arm compared with control Significant reduction in HIV and STI incidence used in the Mujer Segura arm compared with control |
| 2nd | Surratt & Inciardi, 201060 | Florida, USA; drug-using female sex workers; n=806 | To compare intervention effects on risky drug use and sexual behaviors among street-based women sex workers in Miami | Sex Worker-Focused (SWF) Intervention; two 1-hour sessions; issues relevant to sex workers; addressed violence prevention; barriers to safe sex; 5 elements: engagement, education, action, testing, referral | NIDA Standard Intervention* | Significantly more efficacious in reducing unprotected oral sex and sexual violence in the SWF arm compared with control at 6-month follow-up |
| 2nd | Wechsberg et al., 201061,62 | Pretoria, South Africa; women who reported recent substance use and sex trading; n=583 | To compare intervention effects on sex risk behaviors, substance use, experiences with violence, and condom use and sexual negotiation |
Women’s Health CoOp (WHC); 2 one-on-one sessions held within 2 weeks for approximately 1 hour each; addressed HIV/AIDS issues; assessment of drug and sexual risks; and skill-building exercises to negotiate risk-reduction communication; violence prevention strategies; action plans | NIDA Standard Intervention* | At 6-month follow-up, compared with participants in the control arm, participants in the WHC arm reported significantly higher condom use at last sex, and significantly less physical abuse by a main partner and drug use HIV+ women in the WHC arm were more likely to report condom use at last sex with a primary partner compared with control arm |
| 2nd | Witte et al., 201163 | Ulaanbaatar, Mongolia; alcohol-using female sex workers; n=166 | To compare intervention effects on sexual risk of HIV/STI and harmful alcohol use among female sex workers in Mongolia | Two interventions arms; HIV sexual risk reduction; one enhanced with two sessions of motivational interviewing; HIV-Sexual Risk Reduction four weekly relationship-based sessions; HIV-SSR + Motivational Interviewing (MI): same four weekly sessions; two wrap-around MI sessions; alcohol use and HIV risk |
Wellness Promotion; four weekly sessions on overall health and wellness knowledge and skills | No significant differences in effects were observed between conditions Compared to baseline Significant reductions in harmful alcohol use unprotected sex acts with paying partners were observed in all three arms |
| 2nd | El-Bassel et al., 201139 | New York, USA; HIV-negative drug-using couples; n=282 | To compare intervention effects on unprotected sex acts and STIs between couples compared with individual partners | Two intervention arms; Couples Risk Reduction; seven structured 2-hour sessions; social cognitive-theory; relationship-oriented ecological framework; sexual and drug reduction; modeling; role-play; technical condom use;Individual Risk Reduction; same material as covered in couples; delivered to either male or female partner | Couples Wellness Promotion; seven weekly 2-hour sessions; healthy diet; fitness; age-appropriate recommendations; stress reduction | Significant reduction in incidence rate of unprotected vaginal and anal sex acts and an increase in consistent condom use with the study partner in both risk reduction intervention arms compared with the control Significant reduction in the incidence rate of unprotected sex acts in the couples arm compared with the individuals arm |
| 2nd | Wechsberg et al., 201264 | St. Petersburg, Russia; injection drug-using women; n=100 | To compare intervention effects on injecting drug use and sex risk behaviors among female IDUs in drug treatment in St. Petersburg | Women’s CoOp (WC); two 1-hour one-on-one sessions; topics: injection drug use, sex-risk behaviors, HIV risks associated with AOD use and IDU; substance abuse treatment; HCV and skill-building; information on: STIs; harm reduction strategies; action plans | Nutrition intervention; two sessions; interactive discussion of healthy eating with limited resources | Significant reduction in unprotected vaginal sex acts, risk behaviors such as sharing equipment with a main partner, and frequency of partner impairment during sex in the past 30 days in the intervention arm compared with control |
| 2nd | Langhorst et al., 201230 | Virginia, USA; women with Alcohol-Use Disorders; n=36 | To compare intervention effects on the number and frequency of days of alcohol use and risk behavior | HIV/STD Safer Sex Skills Building + Alcohol (SSB+A); five 90-minute sessions; information plus skills building; female-male power issues; negotiation skills; assertiveness training for safer sex | Standard HIV/STD education; one 60-minute information only session; didactic format | Participants in the SSB+A arm had sex with condoms more frequently between 60- and 180-day post discharge compared with control |
| 2nd | Strathdee et al., 20138 | Tijuana and Ciudad Juarez; female sex workers; n=584 | To compare intervention effects on injection and sexual risk behaviors among sex workers who inject drugs | Safer Woman; three conditions, Groups; (B) interactive injection risk/didactic sexual risk intervention; (C) interactive sexual risk/didactic injection risk intervention condition;(D) interactive injection risk/interactive sexual risk intervention; 60 minutes each; equipment sharing; disinfected needles; risk behaviors; role-play; goal setting; counseling and referral information | Group A; didactic injection risk/didactic sexual risk intervention | Juarez participants in Group AC were significantly less likely to report receptive syringe sharing compared with Group BD HIV/STI incidence among participants in Juarez in Group C was significantly lower than Group A Tijuana participants in Group C and Group D had a lower HIV/STI incidence compared with Group A |
| 2nd | Wechsberg et al., 201365 | Cape Town, South Africa; drug-using African women 18–33; n=720 | To compare intervention effects on drug use and risk behaviors and knowledge of HIV, substance use, and empowerment | Women’s Health CoOp (WHC); HIV testing; four modules conducted over two sessions;1-hour each; information about drug use and risks; relationship power; communication and negotiation; myths about rape and violence; action plans | Nutrition control; delivered to groups of 4 to 6 women Standard HIV counseling and testing only (HCT) |
Greater percentage of participants in the WHC arm had negative urine drug screens compared with combined controls at 12-month follow-up Fewer participants in the WHC arm reported impairment at last sex than in combined controls at 6-month follow-up; this result was also observed between the WHC arm and the nutrition arm |
| 2nd | Surratt et al., 201466 | Florida; USA; drug-using African-American women; n=597 | To link underserved female sex workers (FSWs) with needed health services and to reduce risk behaviors for HIV | Two case management interventions; Strengths-Based/Professional-Only(PO);Strengths-Based/Professional-Peer (PP); approach on participant skills and assets; 5-structured Strengths-Based Case Management (SBCM) sessions over 8-weeks;relationship building; participant strengths; barrier identification | No control; compared multiple interventions |
Both women-focused No significant differences between intervention conditions Compared to baseline Both intervention groups displayed significant reductions in HIV risk behaviors, days of crack and alcohol use, male sexual partners over time, and significant increases in services utilization |
| 2nd | Knudsen et al., 201467 | Connecticut, Delaware, Kentucky, Rhode Island, USA; incarcerated drug-using women; n=444 | To compare intervention effects on HIV sexual risk behaviors among women with a history of drug use by addressing seven “thinking myths” about relationships as well as HIV transmission | HIV testing; Reducing Risky Relationships for HIV(RRR-HIV); 17-minute video on HIV and drug abuse; five prison-based group sessions; single booster delivered 30 days post release; addressed seven relationship myths linked to high-risk behaviors; sought to increase male condom use | 17-minute video on HIV and drug abuse | Significant difference in unprotected sexual behaviors with the RRR-HIV reporting fewer past-month occurrences than the control at 90-day follow-up |
| 2nd | El-Bassel et al., 201445 | New York, USA; drug-involved women under criminal justice community supervision; n=306 | To compare intervention effects on unprotected sex acts and condom use among drug-involved women under community supervision | Two intervention arms; Traditional WORTH (Women on the Road to Health); Four gender-specific 90- to 120-minute sessions; psycho-educational; HIV/STI knowledge; risk-reduction; skills-training; condom use; goal setting; Multimedia WORTH; identical sessions; interactive computerized games and visual enhancements; self-paced or group-based | Wellness Promotion; attention control; healthy diet; fitness; tobacco risks; exercise | Participants in the traditional and multimedia WORTH arms were significantly more likely to report an increase in the proportion of protected sex acts, consistent condom use during sex with a main partner, and a decrease in the number of unprotected sex acts compared with control |
| 2nd | McMahon et al., 201351 | New York, USA; sexually active substance-using women and their partners; n=330 couples | To compare intervention effects on drug-related and sexual risk behaviors among substance-using women and their primary partners | Two intervention arms; Couple-Based HIV-Counseling and Testing (CB-HIV-CT); tailored to the couple’s risk profile; HIV and STI information; mini-sessions to address risks; Woman-Only Relationship Focused HIV- Counseling and Testing(WRF-HIV-CT); mini-sessions focused on risk with partner; individual action plans | NIDA HIV-CT standard-of-care control | Significant reduction in HIV risk assessed using a composite measure of HIV risk in the CB-HIV-CT compared with the WRF-HIV-CT and control arms at 9-months Women in the CB-HIV-CT arm reported significantly less frequent receptive syringe sharing with primary partners than in other arms Lower frequency of unprotected anal intercourse among women in the CB-HIV-CT arm compared with other conditions |
| 2nd | El-Bassel et al., 201468 | Kazakhstan, Central Asia; drug-involved heterosexual couples; n=300 couples | To compare intervention effects on incidence of HIV, HCV, unprotected sex, STIs, unsafe injection among people who inject drugs and their partners | Project Renaissance; risk reduction intervention arm (RR); three single-gender group sessions for female and male partners followed by two couple sessions; strategies to reduce risk behaviors; encouraged disclosure; modeling; role-play; communication; technical skills; identifying risks for overdose | Wellness Promotion; five sessions; psychoeducational; healthy routines | Significantly lower incidence of HCV infection in the RR arm compared with control at 12-month follow-up Participants in the RR arm reported significantly fewer numbers of unprotected vaginal sex acts and more consistent condom use with their study partners compared with control over the entire follow-up |
The NIDA Standard Intervention is a 2-session HIV prevention intervention that is built around HIV counseling and testing. It originally focused on injecting drug users in the National AIDS Demonstration Research (NADR) Program. In the NIDA-funded Cooperative Agreement Program the intervention content was expanded to include risks associated with non-injecting drug use.
The emerging third-generation interventions are starting to take a combination prevention approach that incorporates a biomedical component in addition to the behavioral risk-reduction foundation.46 Several third-generation interventions are currently being tested, and while some of their research protocols are available, no outcomes have been published yet.46,47
Discussion
Although the first-generation HIV interventions for women who use AODs provided evidence of initial efficacy in reducing behavioral risks for HIV among women who use AODs, many women who received them continued to use AODs, engage in sex without a condom, and be exposed to gender-based violence. The second-generation interventions advanced to address additional contextual issues for risk-reduction strategies; however, risk behavior continued even with these advances. Other more recent second-generation interventions that address structural factors (e.g., organizational components) have the potential to overcome risk at multiple levels and additional barriers, which will empower women to further reduce their risk. The third-generation interventions, which include biomedical prevention strategies (e.g., ART and PrEP) have the potential to protect women from HIV even when they are unable to negotiate condom use.46
Globally, women who use AODs are still a key population at risk for HIV and they need to be reached for HIV prevention interventions using evidence-based, gender-specific programs. Second-generation efforts to prevent HIV among women in different regions have led to various intervention adaptations to ensure that they are culturally congruent (e.g., language, drug type) and that they target the most relevant risk behaviors (e.g., injecting vs. noninjecting risks). Throughout this evolutionary process, reducing sexual risks has been the centerpiece of interventions to help women reduce their risks for HIV.
Most behavioral interventions that work with individuals or small groups tend to emphasize risk elimination among participants. However, risk elimination is not necessary for an intervention to have a major impact at the population level. Predictive simulation models suggest that reducing transmission risk below a certain threshold can have a major impact on an HIV epidemic even in the context of continued risk at reduced levels.48,49 In most settings, women-focused interventions will be implemented as part of a comprehensive HIV prevention package. A variety of harm-reduction activities might include condom distribution, scaled-up HIV testing, HIV services, opiate substitution, and syringe exchanges (for injectors). As noted previously, AOD-using women contribute disproportionately to HIV epidemics, so women-focused interventions for AOD-using women must be included in comprehensive HIV prevention packages if these efforts are to achieve maximum success.
Harm reduction to reduce risk but not totally eliminate all risk represents important progress. The second-generation interventions expanded to incorporate the complex risk environments of women who use AODs; addressing gender roles, power dynamics in relationships, gender-based violence, and couple relationships.39,50,51 Our literature search, which spanned 25 years, only identified about two dozen gender-specific interventions for women who use AODs; with even fewer implemented in real-world settings. Yet globally, women bear an increasing proportion of the burden of HIV, which is disproportionately concentrated among women who use AODs. Consequently, capitalizing on these gains is essential.
Despite the scientific advances with gender-specific HIV interventions for women who use AODs, multiple challenges exist in real-world settings for facilitating broader implementation and ensuring sustainability. For example, there is a scarcity of resources for behavioral and biomedical gender-specific studies for populations that use AODs, and to test and implement interventions. Also, the limited number of women-focused and gender-specific studies indicates the low priority given to interventions for women, which may also reflect larger societal gender injustices. Furthermore, expanding efforts to develop women-specific and gender-specific HIV interventions will necessitate recruiting and training more investigators, especially with an international focus, who are committed to gender research. This will require additional funding resources for mentoring to increase understanding and empathy about the unique needs of vulnerable and at-risk women and the risk environment in which they live.52
Another resource challenge relates to the lack of funding for the combination of biomedical and behavioral interventions for women who use AODs. For example, it is important to test interventions that incorporate PrEP into behavioral interventions with serodiscordant couples who use AODs, which will require additional funding. More research is needed to examine service access as well the shortage of antiretrovirals and clinic staff in some regions. In many settings, the overall healthcare system is already overburdened, which reduces the likelihood of studying or implementing these efforts without additional funding.
As shown in this review, a number of women-focused interventions have demonstrated efficacy in reducing HIV risk among women who use AODs. Efforts are now needed to move these efficacious interventions into real-world practice settings and to make them even more efficacious and effective. In addition to the resource challenges described above, there are multiple challenges to implementation and service development, especially related to gender-specific programming. The Consolidated Framework for Implementation Research (CFIR), which examines characteristics of the interventions, the characteristics of the women themselves, the social setting, and the structural setting for service impact on intervention implementation,53 provides an approach to identifying potential challenges in implementing these interventions so that these can be addressed during the implementation process.
It is also important to note that we did not identify any interventions that addressed sociostructural barriers such as stigma, discrimination, and marginalization from health services that prevent AOD-using women from accessing HIV prevention and treatment services. Consequently, while the third-generation HIV interventions for women who use AODs can incorporate new biobehavioral advances in prevention, barriers to implementation of evidence-based programing as well as structural barriers to women’s utilization of these programs are likely to continue, and they must be studied and addressed to be fully beneficial for women who use AODs. Also, research must be coupled with advocacy to increase funding and implementation, and to bring needed changes in service delivery.
Limitations
Several limitations to this review should be noted. First, only randomized trials published in peer-reviewed journals were included. Consequently, women-focused studies that demonstrated efficacy but were only presented at conferences or appeared in the gray literature, for example, were not included. Second, more studies with null findings may have been conducted, but because of publication bias, they were not published and are not included in this review. Third, although we used a structured search strategy, we did not conduct a formal systematic review or meta-analysis, which limits some of our conclusions. Fourth, this review was limited to English-language articles.
Conclusions
A number of women-focused interventions have been found to be efficacious for reducing HIV-related risk and associated behaviors. The future of women-focused, gender-specific, and couples’ interventions lies in the ability to translate them to real-world settings and to populations where they are most needed using sustainable implementation strategies. Ensuring that research findings move to policy and practice and that efficacious programs are disseminated and maintained is a global challenge. To eradicate new HIV infections among women, we will need a universal commitment and sufficient resources to address gender and its relationship to the intersecting behaviors associated with HIV through AOD use and contextual disparities.
Supplementary Material
Acknowledgements
We thank the National Institute on Drug Abuse for ongoing support for women-focused studies for women who use AODs, the investigators committed to this field, and Jeffrey Novey for his editorial support. This work was supported in part by NIDA grant numbers R01DA032061 and P30DA011041.
Appendix 1. Search Strategy
| We searched Pubmed, Embase, and Web of Science using the following search terms. |
|---|
| (("HIV Infections/prevention and control"[Mesh] OR "Acquired Immunodeficiency Syndrome/prevention and control"[Mesh] OR HIV*[Title] OR "Acquired Immunodeficiency Syndrome"[Title] OR "Human Immunodeficiency Virus"[Title]) AND (("Female"[Mesh] NOT "Male"[Mesh]) OR "Women"[Mesh] OR "Women's Health"[Mesh] OR "Women's Health Services"[Mesh] OR female*[Title] OR girl*[Title] OR women*[Title] OR woman*[Title]) AND ("Substance-Related Disorders"[Mesh] OR "Street Drugs"[Mesh] OR "Alcohol Drinking"[Mesh] OR "Heroin"[Mesh] OR "Cocaine"[Mesh] OR "Designer Drugs"[Mesh] OR "Marijuana Smoking"[Mesh] OR "Alcoholic Beverages"[Mesh] OR substance abus*[Title] OR substance us*[Title] OR alcohol*[Title] OR "drinking"[Title] OR drug abus*[Title] OR drug us*[Title] OR illegal drug*[Title] OR "heroin"[Title] OR "cocaine"[Title] OR "marijuana"[Title]) AND ("Intervention Studies"[Mesh] OR "Risk Reduction Behavior"[Mesh:NoExp] OR "Health Education"[Mesh] OR "Health Promotion"[Mesh] OR "Program Evaluation"[Mesh] OR "Preventive Health Services"[Mesh] OR intervention*[Title] OR program*[Title] OR risk reduc*[Title] OR prevent*[Title] OR educat*[Title] OR "health promotion"[Title])) Publication date from 1990/01/01; English |
| OR |
| (("HIV Infections/prevention and control"[Mesh] OR "Acquired Immunodeficiency Syndrome/prevention and control"[Mesh] OR HIV*[Title] OR "Acquired Immunodeficiency Syndrome"[Title] OR "Human Immunodeficiency Virus"[Title]) AND ("Spouses"[Mesh] OR "Marriage"[Mesh] OR "Sexual Partners"[Majr] OR "couple"[Title] OR "couples"[Title] OR "partner"[Title] OR "partners"[Title] OR "married"[Title] OR marriage*[Title] OR significant other*[Title] OR husband*[Title] OR "wives"[Title] OR "wife"[Title] OR boyfriend*[Title] OR girlfriend*[Title] OR boy friend*[Title] OR girl friend*[Title] OR relationship*[Title] OR "dating"[Title] OR lover*[Title] OR spous*[Title] OR romantic*[Title]) AND ("Substance-Related Disorders"[Mesh] OR "Street Drugs"[Mesh] OR "Alcohol Drinking"[Mesh] OR "Heroin"[Mesh] OR "Cocaine"[Mesh] OR "Designer Drugs"[Mesh] OR "Marijuana Smoking"[Mesh] OR "Alcoholic Beverages"[Mesh] OR substance abus*[Title] OR substance us*[Title] OR alcohol*[Title] OR "drinking"[Title] OR drug abus*[Title] OR drug us*[Title] OR illegal drug*[Title] OR "heroin"[Title] OR "cocaine"[Title] OR "marijuana"[Title]) AND ("Intervention Studies"[Mesh] OR "Risk Reduction Behavior"[Mesh:NoExp] OR "Health Education"[Mesh] OR "Health Promotion"[Mesh] OR "Program Evaluation"[Mesh] OR "Preventive Health Services"[Mesh] OR intervention*[Title] OR program*[Title] OR risk reduc*[Title] OR prevent*[Title] OR educat*[Title] OR "health promotion"[Title])) Publication date from 1990/01/01; English |
Appendix 2. Search Results
References
- 1.Parry CD, Pithey AL. Risk behaviour and HIV among drug using populations in South Africa. Afr J Drug Alcohol Stud. 2006;5(2):140–157. [Google Scholar]
- 2.Kalichman SC, Simbayi LC, Cain D. HIV transmission risk behaviours among HIV seropositive sexually transmitted infection clinic patients in Cape Town, South Africa. European journal of public health. 2010;20(2):202–206. doi: 10.1093/eurpub/ckp127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wechsberg WM, Luseno WK, Lam WK. Violence against substance-abusing South African sex workers: intersection with culture and HIV risk. AIDS care. 2005;17(Suppl 1):S55–S64. doi: 10.1080/09540120500120419. [DOI] [PubMed] [Google Scholar]
- 4.Browne FA, Wechsberg WM. The intersecting risks of substance use and HIV risk among substance-using South African men and women. Current opinion in psychiatry. 2010;23(3):205–209. doi: 10.1097/YCO.0b013e32833864eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wechsberg WM, Jones HE, Zule WA, et al. Methamphetamine ("tik") use and its association with condom use among out-of-school females in Cape Town, South Africa. The American journal of drug and alcohol abuse. 2010;36(4):208–213. doi: 10.3109/00952990.2010.493592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wechsberg WM, Luseno WK, Lam WK, Parry CD, Morojele NK. Substance use, sexual risk, and violence: HIV prevention intervention with sex workers in Pretoria. AIDS and behavior. 2006;10(2):131–137. doi: 10.1007/s10461-005-9036-8. [DOI] [PubMed] [Google Scholar]
- 7.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Social science & medicine. 2004;59(8):1581–1592. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 8.Strathdee SA, Abramovitz D, Lozada R, et al. Reductions in HIV/STI incidence and sharing of injection equipment among female sex workers who inject drugs: results from a randomized controlled trial. PloS one. 2013;8(6):e65812. doi: 10.1371/journal.pone.0065812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amaro H, Raj A, Reed E. Women's sexual health: The need for feminist analyses in public health in the decade of behavior. Psychology of Women Quarterly. 2001;25(4):324–334. [Google Scholar]
- 10.Cohan D. Perinatal HIV: special considerations. Topics in HIV medicine : a publication of the International AIDS Society, USA. 2003;11(6):200–213. [PubMed] [Google Scholar]
- 11.Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sexually transmitted diseases. 2005;32(3):156–164. doi: 10.1097/01.olq.0000151418.03899.97. [DOI] [PubMed] [Google Scholar]
- 12.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7–8):637–660. [Google Scholar]
- 13.Sterk CE, Theall KP, Elifson KW, Kidder D. HIV risk reduction among African-American women who inject drugs: a randomized controlled trial. AIDS and behavior. 2003;7(1):73–86. doi: 10.1023/a:1022565524508. [DOI] [PubMed] [Google Scholar]
- 14.Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Hagan H. Are females who inject drugs at higher risk for HIV infection than males who inject drugs: an international systematic review of high seroprevalence areas. Drug and alcohol dependence. 2012;124(1–2):95–107. doi: 10.1016/j.drugalcdep.2011.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roberts A, Mathers B, Degenhardt L Use obotRGttUoHaID. Women who inject drugs: a review of their risks, experiences and needs. Sydney, Australia: National Drug and Alcohol Research Centre (NDARC), University of New South Wales; 2010. [Google Scholar]
- 16.Kirtadze I, Otiashvili D, O’Grady KE, et al. Women who inject drugs in the Republic of Georgia: in their own words. Journal of Psychoactive Drugs. doi: 10.1080/02791072.2014.990174. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abu-Raddad L, Akala FA, Semini I, Riedner G, Wilson D, Tawil O. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa. Characterizing the HIV/AIDS Epidemic in the Middle East and North Africa. 2010;1(1):1–282. [Google Scholar]
- 18.Adimora AA, Ramirez C, Auerbach JD, et al. Preventing HIV infection in women. Journal of acquired immune deficiency syndromes. 2013;63(Suppl 2):S168–S173. doi: 10.1097/QAI.0b013e318298a166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wechsberg WM, Lam WK, Zule W, Hall G, Middlesteadt R, Edwards J. Violence, homelessness, and HIV risk among crack-using African-American women. Substance use & misuse. 2003;38(3–6):669–700. doi: 10.1081/ja-120017389. [DOI] [PubMed] [Google Scholar]
- 20.Sawyer KM, Wechsberg WM, Myers BJ. Cultural similarities and differences between a sample of Black/African and colored women in South Africa: convergence of risk related to substance use, sexual behavior, and violence. Women & health. 2006;43(2):73–92. doi: 10.1300/J013v43n02_05. [DOI] [PubMed] [Google Scholar]
- 21.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 22.Wechsberg WM, Luseno W, Riehman K, Karg R, Browne F, Parry C. Substance use and sexual risk within the context of gender inequality in South Africa. Substance use & misuse. 2008;43(8–9):1186–1201. doi: 10.1080/10826080801918247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Otiashvili D, Kirtadze I, O’Grady KE, et al. Access to treatment for substance-using women in the Republic of Georgia: Socio-cultural and structural barriers. International Journal of Drug Policy. 2013;24(6):566–572. doi: 10.1016/j.drugpo.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padayachee A. The hidden health burden: alcohol-abusing women, misunderstood and mistreated. International Journal of Drug Policy. 1998;9(1):57–62. [Google Scholar]
- 25.Doherty MC, Garfein RS, Monterroso E, Brown D, Vlahov D. Correlates of HIV infection among young adult short-term injection drug users. Aids. 2000;14(6):717–726. doi: 10.1097/00002030-200004140-00011. [DOI] [PubMed] [Google Scholar]
- 26.Latkin CA, Mandell W, Knowlton AR, et al. Gender differences in injection-related behaviors among injection drug users in Baltimore, Maryland. AIDS education and prevention : official publication of the International Society for AIDS Education. 1998;10(3):257–263. [PubMed] [Google Scholar]
- 27.Rutman D, Callahan M, Lundquist A, Jackson S, Field B. Substance use and pregnancy: conceiving women in the policy-making process: Status of Women Canada Ottawa. 2000 [Google Scholar]
- 28.Blum LN, Nielsen NH, Riggs JA. Alcoholism and alcohol abuse among women: report of the Council on Scientific Affairs. American Medical Association. Journal of women's health / the official publication of the Society for the Advancement of Women's Health Research. 1998;7(7):861–871. doi: 10.1089/jwh.1998.7.861. [DOI] [PubMed] [Google Scholar]
- 29.Pinkham S, Malinowska-Sempruch K. Women, harm reduction, and HIV. International Harm Reduction Development Program of the Open Society Institute. 2007 [Google Scholar]
- 30.Langhorst DM, Choi YJ, Keyser-Marcus L, Svikis DS. Reducing Sexual Risk Behaviors for HIV/STDs in Women with Alcohol Use Disorders. Research on social work practice. 2012;22(4):367–379. doi: 10.1177/1049731512441683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Myers B, Louw J, Pasche S. Gender differences in barriers to alcohol and other drug treatment in Cape Town, South Africa: original. African Journal of psychiatry. 2011;14(2):146–153. doi: 10.4314/ajpsy.v14i2.7. [DOI] [PubMed] [Google Scholar]
- 32.Myers B, Kline TL, Doherty IA, Carney T, Wechsberg WM. Perceived need for substance use treatment among young women from disadvantaged communities in Cape Town, South Africa. BMC psychiatry. 2014;14:100. doi: 10.1186/1471-244X-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mravcik V, Zabransky T, Talu A, et al. Mortality of registered drug users in Central Asia. The International journal on drug policy. 2014 doi: 10.1016/j.drugpo.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Dennis ML, Wechsberg WM, McDermeit M, Campbell RS, Rasch RR. The correlates and predictive validity of HIV risk groups among drug users in a community-based sample: methodological findings from a multi-site cluster analysis. Eval Program Plann. 2001;24(2):187–206. doi: 10.1016/s0149-7189(01)00014-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wechsberg WM, Dennis ML, Stevens SJ. Cluster analysis of HIV intervention outcomes among substance-abusing women. Am J Drug Alcohol Ab. 1998;24(2):239–257. doi: 10.3109/00952999809001711. [DOI] [PubMed] [Google Scholar]
- 36.Shapoval A, Pinkham S. Women and harm reduction in central Asia. Tech Rep. 2011 Abt Associates(Quality Health Care Project in the Central Asian Republics). [Google Scholar]
- 37.Tross S, Campbell AN, Cohen LR, et al. Effectiveness of HIV/STD sexual risk reduction groups for women in substance abuse treatment programs: results of NIDA Clinical Trials Network Trial. Journal of acquired immune deficiency syndromes. 2008;48(5):581–589. doi: 10.1097/QAI.0b013e31817efb6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wechsberg WM, Lam WK, Zule WA, Bobashev G. Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. American journal of public health. 2004;94(7):1165–1173. doi: 10.2105/ajph.94.7.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.El-Bassel N, Gilbert L, Wu E, et al. Couple-based HIV prevention for low-income drug users from New York City: a randomized controlled trial to reduce dual risks. Journal of acquired immune deficiency syndromes. 2011;58(2):198–206. doi: 10.1097/QAI.0b013e318229eab1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nyamathi AM, Leake B, Flaskerud J, Lewis C, Bennett C. Outcomes of specialized and traditional AIDS counseling programs for impoverished women of color. Research in nursing & health. 1993;16(1):11–21. doi: 10.1002/nur.4770160104. [DOI] [PubMed] [Google Scholar]
- 41.Deren S, Tortu S, Davis WR. An AIDS risk reduction project with inner-city women. 1993 [Google Scholar]
- 42.Sherman SG, German D, Cheng Y, Marks M, Bailey-Kloche M. The evaluation of the JEWEL project: an innovative economic enhancement and HIV prevention intervention study targeting drug using women involved in prostitution. AIDS care. 2006;18(1):1–11. doi: 10.1080/09540120500101625. [DOI] [PubMed] [Google Scholar]
- 43.Jones HE, Kirtadze I, Otiashvili D, et al. Process and product in cross-cultural treatment research: development of a culturally sensitive women-centered substance use intervention in Georgia. Journal of addiction. 2014;2014:163603. doi: 10.1155/2014/163603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wechsberg WM. Promising international interventions and treatment for women who use and abuse drugs: focusing on the issues through the InWomen's Group. Substance abuse and rehabilitation. 2012;3(Suppl 1):1–4. doi: 10.2147/SAR.S21291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El-Bassel N, Gilbert L, Goddard-Eckrich D, et al. Efficacy of a Group-Based Multimedia HIV Prevention Intervention for Drug-Involved Women under Community Supervision: Project WORTH. PloS one. 2014;9(11):e111528. doi: 10.1371/journal.pone.0111528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wechsberg WM, Zule WA, Ndirangu J, et al. The biobehavioral Women's Health CoOp in Pretoria, South Africa: study protocol for a cluster-randomized design. BMC public health. 2014;14:1074. doi: 10.1186/1471-2458-14-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patterson TL, Semple SJ, Chavarin CV, et al. Implementation of an efficacious intervention for high risk women in Mexico: protocol for a multi-site randomized trial with a parallel study of organizational factors. Implementation science : IS. 2012;7:105. doi: 10.1186/1748-5908-7-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Strathdee SA, Hallett TB, Bobrova N, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bobashev G, Norton J, Wechsberg W, Toussova O. Are you HIV invincible? A probabilistic study of discordant couples in the context of HIV transmission. PloS one. 2014;9(5):e94799. doi: 10.1371/journal.pone.0094799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El-Bassel N, Wechsberg WM. Couple-based behavioral HIV interventions: Placing HIV risk-reduction responsibility and agency on the female and male dyad. Couple and Family Psychology: Research and Practice. 2012;1(2):94. [Google Scholar]
- 51.McMahon JM, Tortu S, Pouget ER, Torres L, Rodriguez W, Hamid R. Effectiveness of couple-based HIV Counseling and Testing for women substance users and their primary male partners: a randomized trial. Advances in preventive medicine. 2013;2013:286207. doi: 10.1155/2013/286207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Syvertsen JL, Bazzi AR, Scheibe A, Adebajo S, Strathdee SA, Wechsberg WM. The promise and peril of Pre-Exposure Prophylaxis (PrEP): using social science to inform PrEP interventions among female sex workers: review article. African Journal of Reproductive Health: Special Edition on HIV/AIDS: Special Edition 3. 2014;18:74–83. [PMC free article] [PubMed] [Google Scholar]
- 53.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science : IS. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schilling RF, El-Bassel N, Schinke SP, Gordon K, Nichols S. Building Skills of Recovering Women Drug Users to Reduce Heterosexual AIDS Transmission. Public Health Reports (1974-) 1991;106(3):297–304. [PMC free article] [PubMed] [Google Scholar]
- 55.Kelly JA, Murphy DA, Washington CD, et al. The effects of HIV/AIDS intervention groups for high-risk women in urban clinics. American journal of public health. 1994;84(12):1918–1922. doi: 10.2105/ajph.84.12.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harris RM, Bausell RB, Scott DE, Hetherington SE, Kavanagh KH. An intervention for changing high-risk HIV behaviors of African American drug-dependent women. Research in nursing & health. 1998;21(3):239–250. doi: 10.1002/(sici)1098-240x(199806)21:3<239::aid-nur7>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 57.Van Devanter N, Gonzales V, Merzel C, Parikh NS, Celantano D, Greenberg J. Effect of an STD/HIV behavioral intervention on women's use of the female condom. American journal of public health. 2002;92(1):109–115. doi: 10.2105/ajph.92.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sterk CE, Theall KP, Elifson KW. Effectiveness of a risk reduction intervention among African American women who use crack cocaine. AIDS education and prevention : official publication of the International Society for AIDS Education. 2003;15(1):15–32. doi: 10.1521/aeap.15.1.15.23843. [DOI] [PubMed] [Google Scholar]
- 59.Patterson TL, Mausbach B, Lozada R, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. American journal of public health. 2008;98(11):2051–2057. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Surratt HL, Inciardi JA. An effective HIV risk-reduction protocol for drug-using female sex workers. Journal of prevention & intervention in the community. 2010;38(2):118–131. doi: 10.1080/10852351003640732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wechsberg WM, Luseno WK, Kline TL, Browne FA, Zule WA. Preliminary findings of an adapted evidence-based woman-focused HIV intervention on condom use and negotiation among at-risk women in Pretoria, South Africa. Journal of prevention & intervention in the community. 2010;38(2):132–146. doi: 10.1080/10852351003640799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wechsberg WM, Zule WA, Luseno WK, et al. Effectiveness of an adapted evidence-based woman-focused intervention for sex workers and non-sex workers: The Women's Health Coop in South Africa. J Drug Issues. 2011;41(2):233–252. [Google Scholar]
- 63.Witte SS, Altantsetseg B, Aira T, et al. Reducing sexual HIV/STI risk and harmful alcohol use among female sex workers in Mongolia: a randomized clinical trial. AIDS and behavior. 2011;15(8):1785–1794. doi: 10.1007/s10461-011-9984-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wechsberg WM, Krupitsky E, Romanova T, et al. Double jeopardy--drug and sex risks among Russian women who inject drugs: initial feasibility and efficacy results of a small randomized controlled trial. Substance abuse treatment, prevention, and policy. 2012;7:1. doi: 10.1186/1747-597X-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wechsberg WM, Jewkes R, Novak SP, et al. A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the Women's Health CoOp. BMJ open. 2013;3(5) doi: 10.1136/bmjopen-2013-002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Surratt HL, O'Grady C, Kurtz SP, Levi-Minzi MA, Chen M. Outcomes of a behavioral intervention to reduce HIV risk among drug-involved female sex workers. AIDS and behavior. 2014;18(4):726–739. doi: 10.1007/s10461-014-0723-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Knudsen HK, Staton-Tindall M, Oser CB, Havens JR, Leukefeld CG. Reducing risky relationships: a multisite randomized trial of a prison-based intervention for reducing HIV sexual risk behaviors among women with a history of drug use. AIDS care. 2014;26(9):1071–1079. doi: 10.1080/09540121.2013.878779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.El-Bassel N, Gilbert L, Terlikbayeva A, et al. Effects of a couple-based intervention to reduce risks for HIV, HCV, and STIs among drug-involved heterosexual couples in Kazakhstan: a randomized controlled trial. Journal of acquired immune deficiency syndromes. 2014;67(2):196–203. doi: 10.1097/QAI.0000000000000277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.