Abstract
Health disparities are large and persistent gaps in the rates of disease and death between racial/ethnic and socioeconomic status subgroups in the population. Stress is a major pathway hypothesized to explain such disparities. The Eunice Kennedy Shriver National Institute of Child Health and Human Development formed a community/research collaborative—the Community Child Health Network—to investigate disparities in maternal and child health in five high-risk communities. Using community participation methods, we enrolled a large cohort of African American/Black, Latino/Hispanic, and non-Hispanic/White mothers and fathers of newborns at the time of birth and followed them over 2 years. A majority had household incomes near or below the federal poverty level. Home interviews yielded detailed information regarding multiple types of stress such as major life events and many forms of chronic stress including racism. Several forms of stress varied markedly by racial/ethnic group and income, with decreasing stress as income increased among Caucasians but not among African Americans; other forms of stress varied by race/ethnicity or poverty alone. We conclude that greater sophistication in studying the many forms of stress and community partnership is necessary to uncover the mechanisms underlying health disparities in poor and ethnic-minority families and to implement community health interventions.
Keywords: stress, health disparities, socioeconomic status (SES), ethnicity
Health disparities are the differences in rates of disease and early death among subgroups in the population. The phrase is often used to refer to the gaps in physical health between individuals of low and high socioeconomic status (SES) and between racial and ethnic groups. Health disparities are large in the United States, as they are in other countries, and, as a result, they are the subject of considerable research and policy attention (Adler & Stewart, 2010; Braveman, Cubbin, Egerter, Williams, & Pamuk, 2010; Chen, Martin, & Matthews, 2006; House & Williams, 2000; Koh, 2010). Particularly large disparities in birth and child outcomes exist in the United States between low-income women and women with more adequate financial resources (Blumenshine, Egerter, Barclay, Cubbin, & Braveman, 2010; Olson, Diekema, Elliott, & Renier, 2010) and between African American and non-Hispanic/White American women (Hauck, Tanabe, & Moon, 2011; Spong, Iams, Goldenberg, Hauck, & Willinger, 2011). For example, low birth weight, preterm birth, and infant mortality are all roughly twice as prevalent in African Americans as in non-Hispanic/ Whites (Martin et al., 2011; Minino, Murphy, Xu, & Kochaneck, 2011), whereas Hispanic women vary in these outcomes depending on income, nativity, acculturation, and other factors (Acevedo-Garcia, Soobader, & Berkman, 2007). Understanding these effects, especially the independent and interdependent effects of race/ethnicity and poverty, and addressing them are of paramount importance. The purpose of this article is to describe how a multidimensional approach to studying stress developed through community collaboration provides novel insights into the patterning of stress by SES and race/ethnicity.
Theory on Social Origins of Health Disparities
Research on health disparities has evolved from several scholarly roots. One root is the seminal body of work in which researchers document the positive gradient between adult SES and health (Adler et al., 1994) and seek to uncover the underlying mechanisms (Adler & Snibbe, 2005; Adler & Stewart, 2010). Similar to findings in adults, childhood SES and social position have negative effects on health over the lifespan (Chen et al., 2006; Chen, Matthews, & Boyce, 2002; Cohen, Janicki-Deverts, Chen, & Matthews, 2010). Another contribution to health disparities research is the equally ground-breaking body of work on race and health (Williams, Yu, Jackson, & Anderson, 1997) and on racism and discrimination as major sources of stress for African American individuals (Clark, Anderson, Clark, & Williams, 1999; Krieger, 2000). A third scholarly tradition is sociological theory and research on social origins of disparities, especially Pearlin's (1989) social structural analyses. In this tradition, researchers argue that stressful life events and conditions are rooted in the contexts in which people live and that most chronic and acute stressors arise from social stratification by SES, race, and gender. Stress processes are one major mechanism by which low SES and minority status are thought to translate into poorer health (House & Williams, 2000; Thoits, 2010; Turner, 2010). Those of low status are hypothesized to have higher stress, and stress is the intermediary process increasing risk of disease. For a simplified schematic of this pathway, see Figure 1. These theoretical premises are sometimes referred to as the stress hypothesis. Furthermore, the stress-generating effects of low income have been hypothesized to be greater among African American individuals than among non-Hispanic/Caucasian individuals because of the compounded effects of racial minority and low-income status (e.g., Geronimus, 1992), thus positing an interaction of the two status categories of SES and race/ethnicity.
Fig. 1.
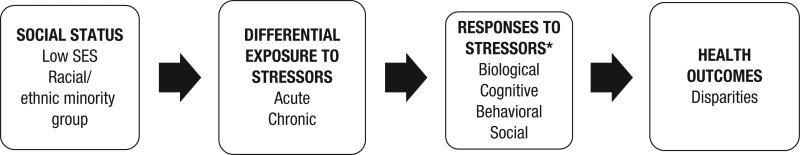
Simplified stress pathway to health disparities. The asterisk indicates that stress responses may or may not vary as a function of social status. SES = socioeconomic status.
Many authors have elaborated on exactly how health disparities could result from differential exposure to stress and heightened vulnerability to its effects in low-SES individuals (Gallo & Matthews, 2003; Taylor, Repetti, & Seeman, 1997). Many studies have resulted concerning the central question of how the social environment can “get under the skin.” Building on these, Myers (2009) developed a lifespan biopsychosocial model of cumulative diversity and minority health in which psychosocial adversities (including chronic daily stress, life events, stressors related to differential treatment on the basis of race and age, and community stressors) influence health indirectly via adverse effects on cognitive processing and emotion regulation and by depleting psychosocial reserve capacity (Gallo, de los Monteros, & Shivpuri, 2009). These mechanisms, in turn, are hypothesized to influence biological stress processes, health behaviors, and health care and to result in differences in health status. Of note, this formulation and several others dictate that many different forms of stress must be studied to explain health disparities in general and, for present purposes, disparities in maternal and child health (Thoits, 2010; Turner & Lloyd, 1999).
Among the various plausible explanations for health disparities, the stress pathway has attracted perhaps the most research attention. There is some evidence to support the role of the stress pathway in explaining health disparities (McLeod & Kessler, 1990; Turner & Avison, 2003; Williams, Neighbors, & Jackson, 2003), but the evidence is not conclusive (Dressler, 2005; Matthews et al., 2009; Turner, 2010). Researchers tend to examine single forms of stress, and the samples and research designs often pose limitations for definitively testing (a) whether stress is higher in lower status groups, (b) whether stress mediates effects of race or SES on health outcomes, and (c) interactions of race/ethnicity and SES. For example, researchers rarely sample people who are at the very bottom of the SES hierarchy because this poor population is particularly vulnerable and difficult to study. Furthermore, in studies on racial disparities, researchers typically compare only White and Black individuals. Research on stress and health disparities in Latino individuals has been scarce, despite the fact that Latino individuals are the fastest growing ethnic group in the United States. To summarize, stress is a central concept in contemporary theoretical formulations on health disparities, but existing evidence is not yet complete. Thus, there is a need to study multiple forms of stress in communities with a range of SES. Community partnership methods were devised to permit more ethical and higher quality studies of vulnerable populations and to provide a stronger basis for successful community interventions.
The Community Child Health Network (CCHN)
With maternal child health disparities as a priority, the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health established the CCHN in 2003 and added a data center in 2006. CCHN is a community-participatory, five-site research network. By design, the five sites varied in population demographics—three were urban, one was rural, and one was mixed urban/suburban—but all had high rates of adverse maternal and child outcomes. Each CCHN site was composed of community and academic partners engaged in an innovative methodological approach known as community-based participatory research (CBPR). CBPR involves full collaboration of scientists and community members in all stages of research from inception through publication and dissemination (Israel, Eng, Schulz, & Parker, 2005). The CCHN consortium included multidisciplinary expertise from psychology, medicine, public health, nursing/midwifery, social work, and sociology and was assisted by a data coordinating center (see the Acknowledgments for full membership). The network's specific aims were (a) to develop a conceptual framework for understanding maternal child health disparities, (b) to design and conduct a study through CBPR processes in order to test hypotheses concerning the underlying mechanisms that contribute to maternal child health disparities, and (c) to inform interventions to reduce such disparities.
Over the course of 2 years of planning, CCHN developed an integrative conceptual model that identified many pathways by which stress may contribute to maternal and child health outcomes (see Ramey et al., 2013). The network was informed in this work by a paradigm shift in health disparities research (Marmot, 2000; Smedley & Syme, 2000) involving an emphasis on multilevel and divergent influences on health. Multilevel approaches emphasize not only individuals but the context of their lives, including interdependent influences of partners, families, networks, neighborhoods or communities, social structures, and cultures. On the basis of the network's derived conceptual framework, CCHN conducted a prospective study of parents of three racial/ethnic groups who were recruited at the birth of a child and who were followed for 2 years at 6-month intervals. These groups were then further studied throughout any subsequent pregnancy, birth, and postpartum period. Our approach was both multilevel and multimethod, approximating Smedley and Syme's (2000) description. The multiple levels were individual, interpersonal, and community, representing many possible influences on physical and mental health, including stress. The multiple methods included quantitative and qualitative self-report interview measures, biomarker collection, medical record data, geographical community-level variables (i.e., geocoding for neighborhood characteristics), as well as pilot work on structured social observations (Laraia et al., 2006).
The primary research questions concerned the effects of parental stress and resilience resources on maternal allostatic load, defined as the cumulative biological burden of adaptation on major body systems (McEwen, 1998; McEwen & Seeman, 2001). Although stress has been studied widely with many different approaches (Cohen, Kessler, & Gordon, 1995; Contrada & Baum, 2010) in many different populations, comprehensive studies of stress in poor and minority communities are still lacking, especially studies of mothers and their partners, and no studies on allostatic load on this group existed at study onset. CCHN studied fathers as well as mothers so as to broaden the scope to include stress and resilience in the family and the larger social context. Community perspectives strongly affirmed that fathers are usually overlooked in maternal and child health research (Lu et al., 2010). CCHN's research project represents one of the largest and most comprehensive efforts to study stress in low- to middle-income fathers and mothers, and it is unprecedented in its focus on disparities within the context of a recent birth and postpartum period.
Conceptualization of Stress to Study Disparities
In general, stress is defined as demands that tax or exceed the resources of the individual (Cohen et al., 1995; Lazarus & Folkman, 1984). Stressors are the demands themselves and can be distinguished from stress responses, which refer to rapid biological and behavioral responses to acute stressors with fairly rapid return to equilibrium under normal conditions (Cohen et al., 1995; Kemeny, 2003). The term stress is often used imprecisely (Wheaton, 1994) to capture both of these as well as emotional responses (cf. Baum, 1990). In keeping with the conceptual framework of CCHN, stress was viewed as multifaceted and multilevel and as incorporating both acute and chronic demands.
Chronic stress refers to a vast array of life difficulties and conditions that vary in form and severity (Gottlieb, 1997). For our purposes, it was further defined as ongoing demands that threaten to exceed the resources of an individual in areas of life such as family, marriage, parenting, work, health, housing, and finances (Dunkel Schetter & Dolbier, 2011). Such stressors are typically not only in excess of the resources of the individuals but also of the families and communities that experience health disparities. Poor racial/ethnic minority populations tend to live in communities that are less economically vital and with fewer resources than the communities of poor White individuals (Brooks-Gunn, Duncan, & Aber, 1997). For those living in poverty, stressors tend to co-occur, accumulate, and persist. Chronic stressors that are more common among the poor include living in communities with crime; crowding; noise; air pollution; high household density; housing instability/frequent relocation; financial strain and food insecurity; long-term unemployment or underemployment; exposure to carcinogens and pathogens in air, water, buildings, and soil; and lack of adequate or good-quality health care (AHRQ, 2006; Busacker & Kasehagen, 2012; Coleman-Jensen, Nord, Andrews, & Carlson, 2011; Fleming, Baum, Davidson, Rectanus, & McArdle, 1987; Morello-Frosch, Zuk, Jerrett, Shamasunder, & Kyle, 2011; Ockenfels et al., 1995; Wheaton & Montazer, 2010).
In addition to stressors associated with low income, a major source of chronic stress for many people is discrimination or marginalization based on race, ethnicity, or other personal characteristics (Flores et al., 2008; Ong, Fuller-Rowell, & Burrow, 2009; Williams et al., 2003). Our community constituency in CCHN identified personal and structural racism and discrimination as major forms of chronic stress affecting individuals of color in their communities with implications for health and for understanding health disparities (Clark et al., 1999; Krieger, 2000; Pascoe & Richman, 2009; Rosenthal & Lobel, 2011; Williams et al., 2003). Many vivid descriptions of this toxic form of chronic stress were communicated by community partners in the planning phases. They also indicated that financial stress, relationship stress, and interpersonal violence (IPV) were important forms of chronic stress to study.
Acute stressors refer to events that have a discrete beginning and ending. Although their aftermath may continue for some time, they are hypothetically time-limited in their occurrence. Examples are sudden death of a loved one, residential relocation, auto accidents and injuries, physical assault, diagnosis of major illness, divorce, deportation, and community catastrophic events (such as floods, hurricanes, earthquakes, and terrorist attacks). Typically measured with life events inventories, major events—such as death of a loved one and divorce—have predicted higher disease morbidity and mortality in population studies (Mostofsky et al., 2012; Sbarra, Law, & Portley, 2011). Higher cumulative life event counts have been linked to greater risk of psychiatric disorders (Hammen, Davila, Brown, Ellicott, & Gitlin, 1992; Kessler, 1997; Turner & Wheaton, 1995), onset of chronic diseases (Renzaho et al., 2013), and adverse birth outcomes (Class, Lichtenstein, Langstrom, & D'Onofrio, 2011; Dole et al., 2003).
Community input from all sites affirmed that stress was a major contributor to health in the racially and ethnically diverse, primarily low-income communities of study, and community partners advocated for the study of many forms of stress. We identified the stressors that were prevalent in the lives of low-income, diverse parents in the communities of study in several ways, including review of the literature, community meetings, and a mixed-methods pilot study in one site (Los Angeles, California) that documented some of the many specific forms of stress that low-income community residents experienced (Abdou et al., 2010). The scientific literature has revealed that lower SES has been linked to higher exposure to some forms of stressors, such as work stress, in past research on the general population (Chandola & Marmot, 2011). Theory and past research further pointed to the high prevalence of chronic threats and challenges for low-SES individuals and families (Adler & Rehkopf, 2008; A. Baum, Garofalo, & Yali, 1999; Chen et al., 2006; Lantz, House, Mero, & Williams, 2005; Taylor et al., 1997). Nonetheless, few studies on chronic stress had been published on poor or ethnic minority parents, and none with CBPR methods that, in principle, enhance the validity and potential value of the findings. High chronic stress occurring prior to conception, during pregnancy, and following the birth of a child is likely to have serious repercussions for parent and child health through many behavioral and physiological pathways (Dunkel Schetter, 2011; Dunkel Schetter & Lobel, 2012; Hobel, Goldstein, & Barrett, 2008; Kramer, Hogue, Dunlop, & Menon, 2011; Lanzi, Ramey, & Bert, 2012).
Relevant past studies on differential exposure to stress and heightened vulnerability to the effects among low-SES and ethnic/racial minority populations can be characterized generally as limited in one or more of the following ways: (a) the samples have limited ethnic/racial diversity with typically only two groups; (b) sampling rarely includes individuals living in poverty; (c) participants are from a single, usually urban, geographic area (e.g., Detroit, Miami, and Toronto); (d) sample sizes restrict or prohibit testing interactions of SES and race; and (e) researchers fail to measure multiple forms of stress. In a few studies on mental health, researchers have measured more than one form of stress, sometimes with an eye to examining racial and SES disparities (e.g., Turner & Avison, 2003; Williams et al., 1997), but these have one or more of the earlier limitations, and none use community partnership at all stages of the research to enhance cultural appropriateness and community fit. Thus, our five-site collaborative network of approximately four dozen community partners and scientists engaged in CBPR processes focused on stress as a central concept involved in the mechanisms underlying disparities in maternal and child health in a large sample of participants drawn from three racial/ethnic groups with a large proportion living in poverty.
The CCHN Five-Site Study of Parents
To achieve our many goals and specific aims, CCHN designed and conducted a study of 2,448 mothers and 1,383 fathers residing in Washington, DC; Baltimore, Maryland; Los Angeles County, California; Lake County, Illinois; and seven counties in eastern North Carolina (Pitt, Greene, Washington, Tyrell, Martin, Bertie, and Edgecombe). Women in each specified catchment area were recruited in the hospital following birth of a baby, with the exception of one site (North Carolina), where participants were recruited during pregnancy or in postpartum clinics. Fathers were recruited if mothers gave permission. In our recruitment efforts, we oversampled on the basis of poverty status and risk for preterm delivery to identify an at-risk population.
Overall, the sample demographically represented fairly well the high-risk communities in which these mothers and fathers resided. A majority of participants were below or near the federal poverty level and identified as African American or Latino. Fathers tended to be of similar racial/ethnic background to their partners/spouses. Slightly more than half of the mothers identified as African American or Black, about one quarter identified as Latina or Hispanic, and the remainder identified as non-Hispanic or White.1 More than 90% of African American/Black and White individuals were born in the United States, whereas only 28% of Latino individuals were born in the United States. Among Latino mothers and fathers born outside the United States, a majority were born in Mexico. Nearly two thirds of mothers (61%) were cohabiting with the baby's father during the 1st year, whereas the remainder of the mothers—over one third of the sample—were not (39%). These figures diverge from many other studies of parents who are predominately or who are all married and who are less likely to be poor. For additional details on demographics of the sample, see Notes.2
Participants were categorized into one of three groups on the basis of 2009 federal poverty thresholds that take into account household income and size: (a) less than 100% federal poverty level (poor) characterized 43% of this sample, (b) 100%–200% federal poverty level (“nearly poor” or “near poverty”) characterized 28% of this sample, and (c) greater than 200% of the federal poverty level (“not poor”) characterized 29% of this sample. Of note, the not-poor group in the study was not affluent but rather was middle to lower middle class, with a mean income overall ranging from $18,000 to $39,000. Furthermore, race/ethnicity and SES are highly confounded in the U.S. population, posing difficulties for examining these factors jointly across racial/ethnic groups. However, the income distributions within each race/ethnic group of mothers and fathers in this study did not differ significantly, with the exception that in the not-poor or highest household income category, White individuals had statistically significantly higher household income than Black and Latino individuals by averages of $16,000–$18,000. Although not trivial, this is not a difference of the magnitude found in the U.S. population as a whole, and the gap in income among racial ethnic groups is not as large as in many study samples on disparities.
We followed parents at 1, 6, 12, 18, and 24 months after the birth of a child. Mothers and fathers were interviewed individually in their homes in the language of their choice (English or Spanish). Most of the interviews were conducted by community members who were experienced or trained in community research or clinical service delivery, and some were bilingual. For details of interviewer training, see the Notes.3
Measuring Multiple Forms or Types of Stress
A measurement goal was to study many forms of stress in these racially and ethnically diverse parents and to develop or adapt measures to be better attuned to these populations. In parallel, the network focused on conceptualizing and operationalizing many forms of resilience resources (Dunkel Schetter & Dolbier, 2011). To comprehensively operationalize stress in CCHN, community partners and scientists agreed on the concepts listed in Table 1: financial stress, pregnancy stress, life events, chronic life stress, perceived stress, IPV, perceived racism, and parenting stress. Interview measures of these concepts were contained in detailed structured protocols that were administered to study participants in their homes at 1, 6, and 12 months after a birth of a child. Biomarkers were also collected, and community level and geographical approaches to stress measurement were formulated as reported elsewhere.
Table 1.
CCHN Stress Measurement Framework and Timing of Assessment
| Forms of stress | Measure (Authors) | Time 1 (1 month) | Time 2 (6 months) | Time 3 (12 months) |
|---|---|---|---|---|
| Financial stress | CCHN developed from survey items | X | ||
| Pregnancy stress (retrospective) | Prenatal Psychosocial Profile (Curry, Burton, & Fields, 1998; Curry, Campbell, & Christian, 1994) | X | ||
| Life events | Life Events Inventory (Dominguez, Dunkel Schetter, Mancuso, Rini, & Hobel, 2005) | X | Xa | |
| Chronic stress | CCHN adaptation of the UCLA Life Stress Interview | X | ||
| Perceived stress | Perceived Stress Scale | X | X | Xa |
| Interpersonal violence | HITS | X | Xa | |
| Perceived racism | Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997) | X | Xa | |
| Parenting stress | Parenting Stress Index (Abidin, 1990, 1995) | X |
Note: An “X” indicates the time point at which each listed measure was administered. CCHN = Child Community Health Network; UCLA = University of California, Los Angeles; HITS = a four-item questionnaire in which respondents were asked how often their partner physically Hurt, Insulted, Threatened with harm, and Screamed at them. Measures administered at 18 and 24 months are not included in this report.
Results are not included in this article.
Interview measure development involved a close collaboration over a 2-year time frame between the CCHN Community Committee and the CCHN Measures Committee through weekly teleconferences and face-to-face network meetings. The process by which measures were nominated, vetted, and selected for use engaged CBPR processes extensively. For example, both community partners and scientists nominated measures of racism to review and discussed them in detail. Community partners critiqued existing stress measures as appropriate or inappropriate for their communities and evaluated wording to ensure understanding among the diverse groups under study. Community partners often guarded against the inclusion of scales or questions within them that would not be understood or would be confusing to men and women in their regions. Complex response scales or extremely long scales or instruments were sometimes rejected on the basis of community input. Community partners held meetings in the network sites of residents and reviewed the proposed measures as well. Pilot testing resulted in deletion of sets of items or shortening some interview instruments through CBPR dialogue.
Standardized scales with minimal changes were used to assess pregnancy stress (Misra, O'Campo, & Strobino, 2001), life events (Dominguez, Dunkel Schetter, Mancuso, Rini, & Hobel, 2005; Lobel, Dunkel Schetter, & Scrimshaw, 1992), perceived stress (Cohen, Kamarck, & Mermelstein, 1983; Cohen & Williamson, 1988), IPV (O'Campo, Caughy, & Nettles, 2010; Sherin, Sinacore, Li, Zitter, & Shakil, 1998), parenting stress (Abidin, 1990, 1995; Abidin & Brunner, 1995), and perceived racism (Williams et al., 1997). Complete details of these measures may be found in the Supplemental Material available online and in the Notes.4 The measures of financial stress and chronic stress were developed specifically for this study, and the measure of perceived racism was modified from its original form (full details available in the Supplemental Material). Of note, the chronic stress measure was a qualitative interview assessing chronic demands in three life domains—family, neighborhood, and partner relationship—that was based on an existing validated methodology, adapted for this study, and validated on a subsample (Stapleton, Dooley, Paek, Huynh, & Dunkel Schetter, 2013).
In addition to stress measures, interviews also contained demographic information on parent age, education, household income, number of persons in the household, place of birth, and self-identified race/ethnicity. Per capita household income was adjusted for cost of living in each site. Mother and father educational attainment variables were each scored as follows: less than high school, high school diploma or General Educational Development test, some college, and 4-year college degree or higher.
Variation in Stress by Poverty, Race/Ethnicity, and Related Factors
To examine the stress pathway to disparities, we tested whether there was significant variation by race/ethnicity and poverty with respect to each of the forms of stress and whether there were interactions of poverty by race/ethnicity. Specific details of analyses can be found in the Notes.5 In all, more than two thirds of the effects were significant or marginally significant (p < .05 or p < .10, respectively). Seven of 18 interaction effects were significant, and one was marginal. Thus, there was considerable evidence for effects of race/ethnicity and poverty on the various forms of stress and some evidence for interactions of these two social structural factors, as described further and summarized in Table 2. (Tables of means, confidence intervals, or significance levels for all stress measures for mothers and fathers are available in the Supplemental Material.)
Table 2.
Summary of Tests of Poverty and Race/Ethnicity in CCHN Sample of Mothers and Fathers
| Poverty effect |
Race/ethnicity effect |
Poverty × Race/Ethnicity effect |
||||
|---|---|---|---|---|---|---|
| Stress measure | Mothers | Fathers | Mothers | Fathers | Mothers | Fathers |
| Chronic stress | Poor > near poor > nonpoor | Poor > near poor, nonpoor | B > L, W | B > W | No | No |
| Parenting stress | Poor > near poor, nonpoor | Poor > near poor, nonpoor | L > B, W | L > B, W | No | No |
| Interpersonal violence | Poor > near poor > nonpoor | Not measured | No effect | Not measured | No | Not measured |
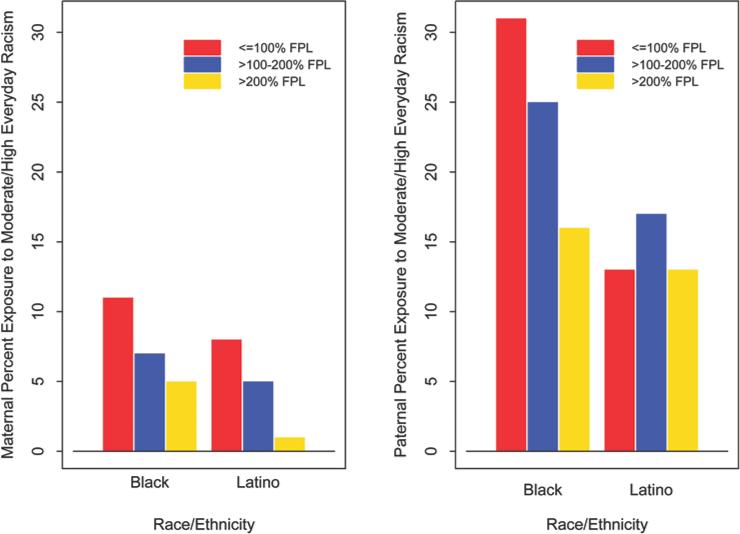
| Everyday racism | Marginal/QBI | Poor > near poor > nonpoor | B > L > W (see Figure 2) | B > L > W (see Figure 2) | Marginal | No |
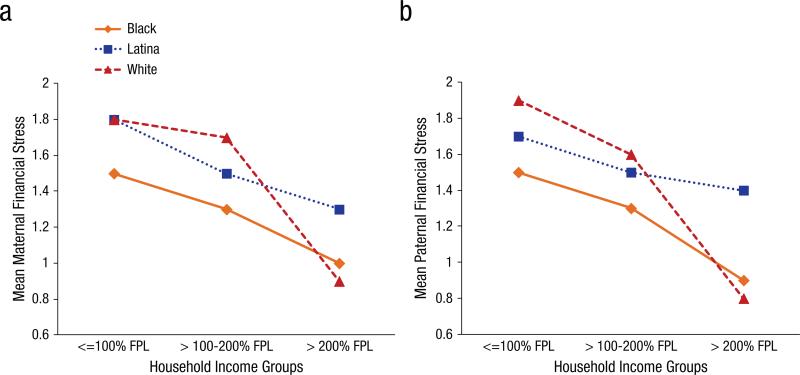
| Financial stress | ns/QBI | ns/QBI | ns/QBI | ns/QBI | Yes (see Figure 3) | Yes (see Figure 3) |
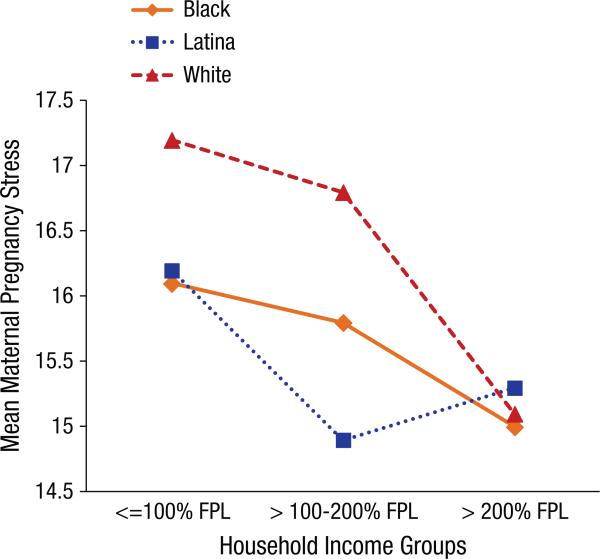
| Pregnancy stress | ns/QBI | Not measured | ns/QBI | Not measured | Yes (see Figure 4) | Not measured |
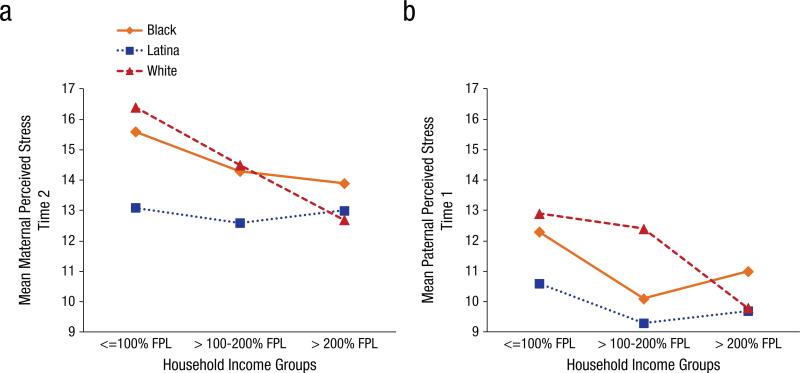
| PSS 1 month | Poor > near poor > nonpoor | ns/QBI | ns | ns/QBI | No | Yes (see Figure 5) |
| PSS 6 months | ns/QBI | Marginal | ns/QBI | B, W > L | Yes (see Figure 5) | No |
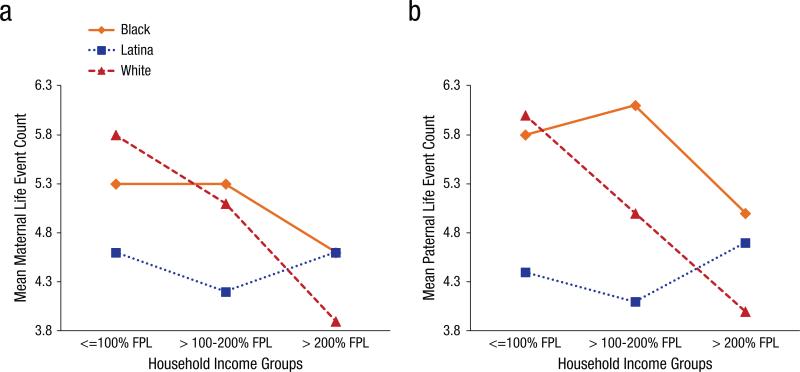
| Life event number | ns/QBI | ns/QBI | ns/QBI | ns/QBI | Yes (see Figure 6) | Yes (see Figure 6) |
| Life event impact | ns | ns | ns | ns | No | No |
Note: CCHN = Child Community Health Network; B = Black; L = Latina(o); W = White; QBI = qualified by interaction; PSS= Perceived Stress Scale.
Poverty and stress
There were effects of poverty (not qualified by interactions with race/ethnicity) for mothers and for fathers for two forms of stress (chronic stress and parenting stress) and two more either for fathers or mothers. Chronic stress, as measured at 6 months after birth by the qualitative interview, and parenting stress, as measured with a standardized scale at 1 year after birth, both varied significantly by poverty with graded effects such that poor parents were higher than those living near the poverty level who were higher than those who were not poor. IPV was also highest among poor mothers, was next highest among mothers near the poverty level, and was lowest in mothers who were not poor. Everyday racism also varied significantly by poverty for fathers (marginally for mothers), with 22% of fathers in the poor group scoring moderate to high compared with 17% in the near-poor group and 9% in the not-poor group. These findings parallel prior research showing that perceived stress is more prevalent in low-income populations (Chandola & Marmot, 2011; Cohen & Janicki-Deverts, 2012). Overall, they suggest powerful and consistent effects of poverty on stressors of many kinds occurring over the 1st year following a birth. Because the range of income was truncated, the results address the importance of variation at the low to middle range of the income spectrum and dramatically illustrate the numerous types of chronic exposures to demands that increase as a function of living in poverty or near poverty.
Race/ethnicity and stress
Chronic stress, parenting stress, and racism were the only forms of stress to show main effects of race/ethnicity among mothers and fathers without interactions with poverty status (see Table 2). The Life Stress Interview (LSI; Hammen et al., 1987) chronic stress scores that reflected family, partner, and neighborhood demands were highest among Black mothers and fathers. That is, Black mothers had significantly higher levels of chronic stress than both Latina and White mothers, who did not differ from each other, and Black fathers had significantly higher chronic stress than White fathers. These results are similar to those of Turner and Avison (2003) in their study of 899 adolescents in which African American youths were much higher in chronic stress than Caucasian youths, and that difference partially accounted for a disparity in depressive symptoms. Regarding parenting stress, Latino mothers and fathers in this study were higher in parenting stress than parents of other ethnicities. One further race/ethnic difference occurred among fathers: Perceived stress at 6 months after birth of a child was significantly higher in Black and White fathers compared with Latino fathers. In fact, across income levels, perceived stress was notably low in Latino fathers when unadjusted for foreign birth. In addition, there was a highly significant effect of race/ethnicity in reports of everyday racism for both mothers and fathers. African American/Black individuals reported the highest rates of everyday racism, especially Black fathers (see Figure 2). Among Black fathers, 24% scored moderate to high, versus 14% of Latino fathers and 2% of White fathers. Latino individuals were also significantly higher in everyday racism than White individuals.
Fig. 2.
Maternal and paternal moderate/high everyday racism by race/ethnicity and poverty group. FPL = federal poverty level.
Interactions of race/ethnicity by poverty
In its strongest form, the stress pathway to health disparities argues that race and ethnicity interact with low SES in generating higher stress for some individuals, which functions as a primary mechanism influencing their poorer health. As summarized in Table 2, there were significant interactions between poverty and race/ethnicity for mothers and fathers in effects on financial stress and life events, for mothers in effects on pregnancy stress and perceived stress at 6 months, and for fathers in effects on perceived stress at 1 month after the birth of a child. The patterns of results are depicted in Figures 3–6. In general, the patterns show steeper negative slopes for White individuals with increased income and flatter slopes for Black individuals. Latino individuals often paralleled Black individuals but not uniformly. These results are quite robust when repeated controlling for U.S. birth, marital status, and cohabitation with partner, although a few differences by foreign birth are noted.
Fig. 3.
Maternal and paternal financial stress at 1 month after birth by poverty group and race/ethnicity. FPL = federal poverty level.
Fig. 6.
Maternal and paternal life events preceding birth by poverty group and race/ethnicity. FPL = federal poverty level.
Financial stress
There was an inverse linear relation of financial stress and poverty group with the notable exception of Latino mothers and fathers, whose financial stress did not differ as much by poverty (see Figure 3). When examining simple effects, we find that both Black and White mothers decline significantly in financial stress from near poverty to not being poor (“nonpoor” group). In contrast, there were no significant differences by poverty status for Latino mothers or fathers. However, counter to expectations, White mothers who were poor or near poverty reported significantly higher financial stress than poor or near-poverty Black mothers (see Figure 3a). Poor Latina mothers also had significantly higher financial stress than poor Black mothers. This pattern may indicate differential responses to economic deprivation in the different ethnic/racial groups. For example, some researchers have hypothesized greater resilience, different forms of coping, and even more habituation to financial hardship among Black individuals, which may be evident here (Chen & Miller, 2012; Jackson, Knight, & Rafferty, 2010; McCubbin, Thompson, Thompson, & Futrell, 1998). Finally, among all fathers who were not poor, Latino fathers had significantly higher levels of financial stress than Black and White fathers (see Figure 3b).
Pregnancy stress and perceived stress at 6 months in mothers
Results among mothers for pregnancy stress (see Figure 4) and perceived stress at 6 months postpartum (see Figure 5a) also show a steeper slope in White individuals from near poverty to nonpoor compared with the other two race/ethnic groups. Simple effects show significantly higher pregnancy stress in poor and near-poverty White mothers compared with nonpoor White mothers and in poor Black mothers than in nonpoor Black mothers (see Figure 4). Within the near poverty group, White mothers were higher in pregnancy stress than Latina mothers. Latina mothers were also significantly lower in perceived stress at 6 months after birth than Black and White mothers but only among the poor (see the top panel of Figure 5). That is, among the poor women as a whole, simple effects revealed that Black and White mothers were significantly higher in perceived stress than Latina mothers, whereas near-poor or not-poor mothers did not differ by race/ethnicity. In fact, perceived stress at 6 months postpartum in Latina mothers was remarkably low regardless of income level, mirroring the results for financial stress.
Fig. 4.
Maternal pregnancy stress reported at 1 month postpartum by poverty group and race/ethnicity. FPL = federal poverty level.
Fig. 5.
Perceived stress for mothers at 6 months postpartum and fathers at 1 month after birth of child by poverty and race/ethnicity. FPL = federal poverty level.
Perceived stress at 1 month in fathers
Fathers had lower perceived stress overall compared with mothers even at 1 month after birth of a child with a newborn at home, and there was a significant interaction effect for perceived stress for fathers at 1 month after birth but not at 6 months after birth. Figure 5b depicts the pattern of means, but the significant simple effects were few; Black poor fathers had higher perceived stress compared with Black fathers who were near poverty (near poor), and White fathers who were poor had higher perceived stress compared with White fathers who were not poor (i.e., low to middle income).
Life events in mothers and fathers
Interaction patterns for effects of race/ethnicity by poverty status for life events look similar to the patterns of interactions for other variables in many ways. Life events decline with increased income for White mothers and fathers but not for Latino or Black mothers and fathers. Simple tests showed that White mothers and fathers who were poor reported significantly higher numbers of life events during the year preceding the birth compared with White mothers and fathers who were not poor (see Figure 6), whereas life events did not differ by poverty status within the other two racial/ethnic groups. Furthermore, among the poor, Latina mothers had significantly fewer life events than Black mothers. Similarly, within mothers who were near the poverty level, Latina mothers had significantly fewer life events than Black mothers. Finally, among those who were not poor, Black fathers had significantly more life events than White fathers. When cohabitation and marital status were controlled, Black and Latina mothers no longer differed significantly, indicating the importance of relationship status when examining ethnic differences in parenting stress.
Marital status, cohabitation, and parent stress
Although relationship status is not a recognized pathway to health disparities, perhaps it should be examined as one of the confluence of factors mediating effects of race/ethnicity and SES on health outcomes in adults. There were many significant effects of cohabitation on levels of stress in this sample, and, notably, no unique effects of marital status after cohabitation was adjusted. For both mothers and fathers, cohabitation was associated with fewer life events, less perceived stress at 1 month postpartum, and less (marginally less for fathers) chronic stress. For mothers, cohabitation was also associated with significantly less IPV, less pregnancy stress, less life event impact, and less parenting stress. Thus, the status of a parent relationship at birth seems to be a major determinant of stress during pregnancy and the year following birth for parents, especially for mothers. What mattered most in this sample was living together at the time of birth, not whether the couple was legally married at that time.
Foreign birth, acculturation, and stress
Although most of the multivariate effects remained significant when controlling for whether the mother or father was foreign versus U.S. born, some of the specific comparisons among Latino individuals and the other two ethnic/racial groups changed. To summarize, lower perceived stress among Latino fathers and fewer life events among Latino mothers and fathers were a function of lower rates in those of foreign birth compared with those of U.S. birth. These patterns are consistent with the Hispanic health paradox whereby immigrants have fewer health risks and better health outcomes than those of the same background living in the United States longer. In addition, adjustment for foreign birth attenuated the effects of poverty on financial stress for Latino individuals, reflecting higher incomes in the U.S.-born Latino individuals.
In addition to taking place of birth into account when examining ethnic/racial and SES disparities, the findings regarding foreign birth are of substantive interest as well. Foreign-born mothers and fathers experienced significantly more financial stress and racism but less chronic stress in family, neighborhood, and partner relationships when controlling for income, cohabitation, and marital status. Foreign-born mothers experienced more parenting stress and marginally more IPV but fewer life events when compared with those who were U.S. born. Foreign-born Latino fathers experienced lower perceived stress at 1 month after birth compared with those who were U.S. born and experienced marginally more perceived stress at 6 months.
To consider the associations of stress with acculturation further, we used a standardized scale measure of acculturation (Bidimensional Acculturation Scale; Marin & Gamba, 1996) and tested for associations with stress after controlling for household income (per capita adjusted for cost of living across sites). Higher English language orientation was associated with more of some key types of stress for both Latino mothers and fathers—namely, life events and chronic stress, and, for Latina mothers, more IPV but less financial stress. Perceived stress and life event impact also varied with acculturation for Latino fathers such that higher English orientation was associated with higher perceived stress at both 1 month and 6 months after birth and with greater life event impact. The one exception was financial stress, which was lower in those who were more acculturated, most likely because of higher rates of employment or higher income among those more acculturated. Revealed through multidimensional stress assessment, these findings provide a more complete picture of the complicated relationships of foreign birth and acculturation to stress among Latino individuals.
Advancing Knowledge of Stress Pathways to Disparities
Multiple and complex demands on families at risk
Clearly, there are multiple demands exceeding resources in communities where health disparities exist. Overall, levels of stress were similar to or higher when compared with other high-risk and representative national samples. In general, being poor or near the federal poverty level was associated with higher levels of almost every type of stress. Whether we tested household income and education as proxies for SES or the categories of poor (below federal poverty level), near poverty level, or not poor, the results are quite consistent6 and confirm the prevalence of stress as potent and potentially toxic for those of very low SES. These findings further verify the presence of several forms of chronic stress (e.g., parenting stress and financial stress) that may play important roles in the mechanisms contributing to health disparities among socioeconomic groups. Effect sizes are moderate overall, with the largest standardized effects for poverty (.60 or greater). These findings add to our understanding of poverty across various regions of the United States, even regarding differences between those who are poor and those who are just above the poverty level, as well as comparisons between those living in poverty and the middle class.
The effect of poverty on stress generation was especially pronounced among Black mothers and fathers and also among White mothers, and it was less pronounced for Latino parents and White fathers. For example, some forms of stress varied by race/ethnicity within each of the three poverty status groups. At the lowest income levels, White individuals had higher pregnancy stress than the other ethnic groups, Black individuals had lower financial stress, and Latino individuals had lower life events and perceived stress. Thus, among those who were poor, there was not one ethnic or racial group that was highest in all forms of stress, whereas ethnic/racial differences in stress were attenuated but did not disappear with higher household income. Moreover, these results do not appear to be attributable solely to differential income distribution within racial/ethnic groups, as is often the case. Because the income distribution in the sample is truncated, a more dramatic effect might be found if more affluent Americans were included for comparison.
Furthermore, for half of the stress measures, there were interactions of poverty by race/ethnicity, indicating that the gradients for Black, Latino, and White individuals differed significantly by poverty level. Greater income was not as strongly associated with lower levels of major life events, perceived stress, or some forms of chronic stress (financial, pregnancy) for Black individuals as for White individuals. For example, among White individuals, life events occurred more often if they were poor, whereas Black and Latino individuals experienced comparable numbers of life events regardless of poverty status. In short, Black individuals did not show the consistent, protective effects of increased income as did White individuals. Similarly, although educational attainment was fairly consistently associated with lower levels of most types of stress among mothers and fathers, the effects were weaker among Black and Latino individuals compared with White individuals. Although many theorists have hypothesized these interaction effects, very little or rather weak evidence exists in support of them. That the gradients across income and education differed for Black, Latino, and White individuals on several stress measures provides considerable support for the widely held theoretical argument that stress mechanisms explain racial health disparities and may partially explain their persistence when SES is controlled.
Stress in Latino individuals in the United States
Results also vary by place of birth, mainly as a function of Latino individuals, because there were very few foreign-born White individuals and because a few cases of foreign-born Black individuals were excluded from these analyses. We expected the stress patterns for Latino individuals to more closely parallel those of Black individuals than they did. That Latino mothers and fathers evidenced lower stress than other groups on several indicators even when they were poor fits with the Hispanic or Latino paradox, which involves paradoxically better health in low-income Latino individuals compared with other groups (Franzini, Ribble, & Keddie, 2001). Variations by place of birth (United States vs. foreign) and in acculturation weakened these patterns somewhat and are therefore critical to take into account beyond merely categorizing individuals by self-identification as Hispanic or not Hispanic. For example, Wilson (2008) found that acculturation of U.S. women of Mexican origin was associated with decreases in conception rates and in intentional pregnancies as well as less happiness about pregnancy. In the CCHN study, we learned that independent of the effects of income and education, many forms of stress were lower in Latino parents who were less acculturated and were higher among those who were more acculturated. These results also parallel closely other findings on the detrimental health effects of greater acculturation in the United States (an acculturation paradox so to speak) and the health-promoting effects of some traditional values, beliefs, and behaviors (Lara, Gamboa, Kahramanian, Morales, & Hayes Bautista, 2005).
Pregnancy and birth have been found to have somewhat different meanings in different ethnic/racial groups (e.g., Zambrana, Dunkel-Schetter, Collins, & Scrimshaw, 1999). Specific resilience factors among Latino individuals—such as familism, social support, and positive cultural values surrounding pregnancy—may mitigate effects of some of these stressors in the early months after the arrival of a new child (Campos, Dunkel-Schetter, Walsh, & Schenker, 2007). For example, extensive family and social network support following a birth may account for lower rates of some types of stress among poor Latino families. There is no question that understanding stress and health disparities in parents of Latin background requires meticulous attention to the complexities of nativity, language, acculturation, and cultural heritage. This poses a major challenge for multidisciplinary scientists in the future—one that community participation can help to address. We must address these issues more adequately in future studies in light of the fast growing population of Latino individuals in the United States.
Unique sources of stress for fathers
As one of the first studies of various sources of stress in a large and diverse group of fathers, there are a few important insights. Fathers of all backgrounds evidenced stress surrounding the time of a pregnancy and birth of similar levels to that of mothers. For instance, fathers experienced comparable degrees of financial, chronic, and parenting stress as mothers as well as comparable or higher numbers of life events. Black fathers were subjected to very high rates of unfair everyday treatment because of race, skin color, ancestry, and language, which pose additional potent sources of chronic stress that are generally not sufficiently recognized. There is much still to be learned about these fathers and their counterparts in high-risk communities. By studying them with CBPR processes and devoting intensive efforts to understanding participants’ concerns—such as reasons for nonparticipation, attrition, and mistrust of research—we had better success in recruitment, retention, and honesty with fathers as well as mothers than we might otherwise have had. The sources of stress for fathers, especially poor and minority fathers, may have consequences for parenting and family life that could provide insights into the best avenues for encouraging fathers’ involvement and skillful parenting.
The Many Forms of Stress
We utilized a more comprehensive approach to the study of stress than is typical and particularly in measuring many types of chronic stress. The collaborative measurement committee adopted some commonly used standardized scales to measure life events and perceived stress, for example, and supplemented them with new approaches derived from community engagement, such as interviewer ratings of chronic stress in various life domains and a new composite measure of financial stress. Thus, this work contributes to understanding a wider range of stress experiences during a critical time of life—following the birth of a child—in African American/Black, Latino, and non-Hispanic/White mothers and fathers, a majority of whom were living in poverty. For some of these mothers and fathers, the stress exposures were measured during the interval between births, which allows us to address further timely research questions regarding the effects of preconception stress on the fetus and later development of the next-born child.
This set of stress measures captured the underlying construct of “demands exceeding resources” quite well while simultaneously reflecting various independent aspects of stress. In future disparities studies, researchers should consider the different forms of stress more often within a single study. The dichotomy of acute versus chronic stress is insufficient given the richness and complexity of the sources of stress in the population, especially in the lives of those of low income. In general, all forms of chronic stress deserve further attention (e.g., racism and discrimination; IPV; and chronic neighborhood, family, parenting, and partner stress). Both the standardized and the newly adapted stress measures performed well in this study, indicating that they can be used with confidence in testing hypotheses in future studies of low-income and ethnically or racially diverse community populations, especially when brief assessments are needed. In the next section, we further highlight a few of the stress measures and findings.
Perceived stress
The Perceived Stress Scale (PSS; Cohen et al., 1983) is both a brief and powerful measure that reflects appraised stress, and it was fairly stable and high over 5 months in these new parents. In addition, the PSS was the measure most strongly associated with the other stress measures, thereby providing validation data for the full set of measures. However, the PSS does not identify the specific sources of stress that are valuable for some purposes, such as intervention planning. Life events inventories offer insight in this regard, as do other measures like those on IPV, perceived racism, financial stress, and parenting stress. The abbreviated and tailored CCHN version of the LSI was a good addition for gaining information on partner, family, neighborhood, and parenting stress, and it had the advantages that participants were able to speak in their own words to a community interviewer, often of the same ethnic or racial background, and it yielded more objective data. Both participants and interviewers responded favorably to this LSI format (Stapleton et al., 2013). In addition, the taped transcripts are proving to be a rich qualitative data source.
Chronic stress
As noted earlier, chronic stress is thought to be one of the most toxic forms of stress for physical and mental health. The absence of statistical interactions of poverty by race/ethnicity for two measures of chronic stress (the LSI and the PSS) is inconsistent with predictions of heightened exposure to chronic stress in Black individuals who are poor, as was the absence of interactions for a few other stress measures (parenting stress, IPV, racism). However, our not-poor group was not as advantaged economically as the high-income groups in many other studies and is unlikely to represent high-income individuals in the United States as a whole. Perhaps this aspect of our sample reduced the power to detect stronger interactions of race/ethnicity and income. In fact, the interactions of poverty by race/ethnicity that occurred for financial stress, pregnancy stress, and PSS 1 month and 6 months after birth are somewhat consistent with the premise of a chronic stress pathway explaining disparities in that the slopes differed between Black and White individuals in a predicted manner, although the results are not indicative that one racial/ethnic group experiences more chronic stress than others across the board. In contrast, the results are consistent with chronic stress as a potential mediator of effects of low SES on adverse health. To complete the analyses, we next turn to measures of allostatic load as our biological risk index and longer term outcomes, such as postpartum depression and birth outcomes in the next pregnancy.
Racism
Extensive attention has been devoted to the study of racism/discrimination and health in general (Jones, 2000; Krieger, 2000; Pascoe & Richman, 2009) and, to some extent, in maternal and child health in particular (Dominguez, 2008; Giscombé & Lobel, 2005). A plethora of measures appear in the literature (Kressin, Raymond, & Manze, 2008). Only through community participation in CCHN were we able to determine what aspects to study and how. CCHN's community partners provided strong expertise in the evaluation of many measures and their appropriateness. The instrument measuring everyday instances of unfair treatment was appealing to them because many reported experiencing everyday slights, prejudices, and discriminatory behaviors on a regular basis. Black individuals in this study reported the highest rates of everyday unfair treatment because of race/ethnicity, skin color, accent, or ancestry—especially Black fathers, who scored moderate to high on this index, whereas Latino and White fathers experienced far less of this treatment. Latino fathers were higher in everyday discrimination than White fathers, as in a prior study (Perez, Fortuna, & Alegria, 2008). Perceived everyday racism was not exacerbated by low income among fathers and was only marginal among mothers. In further analyses, we will consider several other forms of racism (e.g., lifetime racism) measured with additional scales. Nonetheless, the high prevalence of unfair treatment of men and women of color in everyday contexts in five areas of the United States, especially among Black men in general and poor Black women, underlines the national prevalence of this phenomenon and has significant implications for family health, public policy, and society.
IPV
IPV was highest among poor mothers, was next highest among mothers near the poverty level, and was lowest in mothers who were not poor, and there were no racial/ ethnic differences in IPV. These results differ from some findings in the literature. For example, Caetano, Field, Ramisetty-Mikler, and McGrath (2005), who used a different measure of IPV, found 2–3 times more IPV in Black and Hispanic individuals than in White individuals in a national sample. O'Campo et al. (2010), using the same measure as in this study, found IPV in Baltimore to be highest among White individuals. Although racial differences were not revealed in this study, the higher prevalence of IPV among the poor mothers in our study is consistent with the premise that poverty is a powerful factor in stress generation. IPV is an established risk factor in maternal, child, and family health (Campbell et al., 2002). Additional evidence on prevalence of IPV, variation by SES, and associations with other stressors is valuable in developing a full understanding of family violence.
How Is Future Research on Health Disparities Informed?
CCHN's contributions through the study of stress are complex and variegated in many ways, and they provide strong justification for conceptualizing and studying multiple types or forms of stress in the future—as some authors have advocated (Aldwyn, 2007; Thoits, 2010; Wheaton, 1994), but few researchers have done (cf. Turner & Avison, 2003; Vines et al., 2009; Williams et al., 1997). To test theories of stress as an explanation for health disparities, researchers need to take this next step, or they risk reaching incomplete or erroneous conclusions regarding stress as a possible explanation for health disparities. Using theories regarding effects of stress on physical health, researchers have pinpointed chronic stress as a very potent form, and the stress hypothesis regarding disparities suggests heightened exposure and vulnerability—but exposure to what in particular and for which subgroup? Are poor immigrant Latino individuals exposed to the same stressors as poor Black individuals? Are Black individuals of middle or high income vulnerable to the same chronic stresses as poor Black individuals? CCHN findings suggest that the answers are not obvious or simple and that a more nuanced approach to understanding stress as an explanation for health disparities is needed. Perhaps translational scientists should cease referring to stress as if it is a singular phenomenon. Furthermore, selection of stress measures can be sensitive not only to one's research goals and participant burden but also to the social and community contexts and racial, ethnic, and cultural groups to be studied. CBPR offers a valuable method for accomplishing this.
There are many additional potential influences on stress levels beyond income and race/ethnicity that were not addressed here, such as cultural values or community context. For example, in these analyses, we do not take into account structural community conditions—such as prevalence of crime, noise, or pollution—to be examined in the future in this work, and we do not consider additional indicators of socioeconomic position—such as occupational status, wealth, or assets—that are also presumably associated with stress. Of note, community input resulted in refraining from asking questions about wealth and assets because this low-income sample, which was studied during a major recession, might have been made uncomfortable being asked whether they owned or rented their home, had a retirement account, or had savings. We know that Black and White individuals at similar levels of SES are not comparable in social capital (Adler & Rehkopf, 2008; Williams, 1999). Understanding the multilevel mechanisms linking SES and health constitutes the “fourth era” in health disparities research across the lifespan (Adler & Stewart, 2010). Our network's findings thus far help to set the stage for this new era.
Conclusion
What have we learned using CBPR processes concerning stress in the lives of this large cohort of men and women of diverse ethnicity and SES from five communities who were studied as early as 1 month and 6 months after the birth of a child? The findings verify that these individuals face multiple, continual, and severe stressors that the typical study on stress does not capture. Increasing evidence suggests that some of them may contribute to disparities in maternal, child, and family health outcomes, but more sophisticated study is needed. Our multisite community sample of parents can be characterized by relatively high levels of stress of many different types and considerable variation by ethnicity and income depending on the type of stress. These are adverse conditions in which to bear and raise children. Increasing evidence on the health effects of early adversity supports an argument for addressing the root causes (Chen et al., 2002; Repetti, Taylor, & Seeman, 2002; Thoits, 2010). Our approach to studying stress is only one aspect of the work that CCHN undertook, yet because it was more comprehensive than most prior studies, it revealed potentially new and important insights into the lives of American parents of low income and of color. High exposures to and perceptions of stress, especially chronic stress, have been linked to premature death and disease in adults (e.g., Keller et al., 2012) and to disease mechanisms (McEwen & Seeman, 2001; Miller, Cohen, & Ritchey, 2002). These results point to the importance of studying many forms of chronic stress in maternal and child health and with greater precision. In particular, the relationship between stress and income among Black and Latino individuals in the United States diverges from the simple inverse relationship observed in White individuals, and this reality must be better understood if effective interventions to reduce health disparities are to be devised (Thoits, 2010).
Studying communities such as these in the absence of community collaboration is unlikely to yield a representative sample, sample retention, appropriate procedures and measures, full cooperation, complete and honest responses to questions, or a full understanding of the information gained. It is difficult to gain the trust and time of poor residents in urban and rural areas, and the history of research in these communities has not provided a strong basis for such trust. CBPR is a novel methodology for conducting research on disparities, and when it works well, it stands to yield more valid and reliable results. The purpose of our CBPR-founded network was to collaborate fully with these communities in an effort to do this work differently and, when possible, to give back. Our ongoing community meetings involve sharing and interpreting results to elucidate their full meaning and to generate solutions at all levels. It is a continual learning process for both community members and academics; studying people as psychological scientists do sometimes requires hands-on experience in the phenomena, and CBPR is one established method to engage in the process with personal, scientific, and community level education as a result. We refer those interested to other sources for more details on CBPR and suggest that even those disinclined to do a full CBPR study for reasons of time or funding might benefit from adopting pieces of the process, such as having a community panel to periodically review study plans and findings.
We note that there are also some clues to resilience in these communities. The parents we studied cannot be characterized overall as unable to cope but rather as continually trying valiantly to address and manage the stress in their lives. While high in general, levels of stress were not as high as might be expected under the adverse circumstances of the communities. Newer theoretical perspectives on how some low-SES children and adults cope with adversity by strategies involving “shift and persist” (Chen & Miller, 2012) may be helpful to understanding resilience in this population. Theory and research in psychological science—such as those regarding emotion regulation, cognitive adaptation, and the strategy of “broaden and build” to name a few examples—may shed light on sources of resilience in low income, diverse people and their communities.
Finally, CBPR is exceedingly challenging, but when scientists and communities studying health communicate their perspectives, a greater credibility can be achieved in the results. We look forward to learning more about the effects of these many forms of stress on maternal allo-static load and to incorporating resilience and community factors into a more complete picture; we also look forward to studying the subsequent pregnancies and children of this cohort. In addition, we have the ability to bring community in as a change agent and to be an integral part of the development of solutions to health disparities. Kurt Lewin (1946) once coined the term “action research” as an ambitious but worthy goal for behavioral scientists, and he said it took courage. It has, but working toward solutions regarding maternal child disparities is one of our primary collective goals in CCHN.
Supplementary Material
Acknowledgments
This article is designated as a “Core Paper” of the Child Community Health Network (CCHN) because it reflects major ideas and work considered central to our network. Accordingly, the last designated author is the network itself preceded by the names of those on the writing team who directly prepared this article listed in the order that the team judged best reflects their relative contributions. The CCHN is supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, and R03 HD59584) and the National Institute for Nursing Research (U NR008929). Members of each site are listed in the next paragraph (note that an asterisk indicates those members who participated in only the planning phase of the CCHN).
(1) Baltimore, Maryland: Baltimore City Healthy Start and Johns Hopkins University; Community principal investigator (PI): M. Vance; Academic PI: C. S. Minkovitz; Coinvestigators: P. O'Campo and P. Schafer; Project coordinators: N. Sankofa and K. Walton. (2) Lake County, Illinois: Lake County Health Department and Community Health Center, and the North Shore University Health System; Community PI: K. Wagenaar; Academic PI: M. Shalowitz; Coinvestigators: E. Adam, G. Duncan*, A. Schoua-Glusberg, C. McKinney, T. McDade, and C. Simon; Project coordinator: B. Clark-Kauffman. (3) Los Angeles, California: Healthy African American Families, Cedars-Sinai Medical Center, and University of California, Los Angeles; Community PI: L. Jones; Academic PI: C. Hobel; Coprincipal investigators: C. Dunkel Schetter and M. C. Lu; Coinvestigator: B. Chung; Project coordinators: F. Jones, D. Serafin, and D. Young. (4) North Carolina: East Carolina University, North Carolina Division of Public Health, North Carolina Eastern Baby Love Plus Consortium, and University of North Carolina, Chapel Hill; Community PIs: S. Evans, J. Ruffin, and R. Woolard; Academic PI: J. Thorp; Coinvestigators: J. DeClerque, C. Dolbier, and C. Lorenz; Project coordinators: L. S. Sahadeo and K. Salisbury. (5) Washington, DC: Virginia Tech Carilion Research Institute, Virginia Tech, Washington Hospital Center, and Developing Families Center; Community PI: L. Patchen; Academic PI: S. L. Ramey; Academic coprincipal investigator: R. Lanzi; Coinvestigators: L. V. Klerman, M. Miodovnik, C. T. Ramey, and L. Randolph; Project coordinator: N. Timraz; Community coordinator: R. German. (6) Data Coordination and Analysis Center (Pennsylvania State University); PI: V. M. Chinchilli; Coinvestigators: R. Belue, G. Brown Faulkner*, M. Hillemeier, I. Paul, and M. L. Shaffer; Project coordinator: G. Snyder; Biostatisticians: E. Lehman and C. Stetter; Data managers: J. Schmidt, K. Cerullo, and S. Whisler; Programmers: J. Fisher, J. Boyer, and M. Payton. (7) National Institutes of Health program scientists: V. J. Evans and T. N. K. Raju, Eunice Kennedy Shriver National Institute of Child Health and Human Development; L. Weglicki, National Institute of Nursing Research; Program officers: M. Spittel* and M. Willinger, Eunice Kennedy Shriver National Institute of Child Health and Human Development; Y. Bryan*, National Institute of Nursing Research. (8) Steering committee chairs: M. Phillippe (University of Vermont) and E. Fuentes-Afflick* (University of California—San Francisco School of Medicine).
Footnotes
The demographics for the sample of 2,448 mothers were as follows: the mean age was 26 years, and the mean education was 13 years; half of the mothers were having the first child; and 13% of the mothers had just given birth preterm (<37 weeks). Regarding ethnicity/racial identity, of the mothers, 54% identified as African American or Black, 24% identified as Latina or Hispanic, and 22% identified as non-Hispanic or White. The demographics for the sample of 1,383 fathers were as follows: the mean age was 29 years, and the mean education was 13 years. Regarding ethnicity/racial identity, of the fathers, 48% identified as African American or Black, 27% identified as Latino or Hispanic, and 25% identified as non-Hispanic or White. Regarding parent nativity, among Latino mothers and fathers born outside the United States, 65%–69% were born in Mexico, 15%–17% were born in El Salvador, 6% were born in Honduras, 5% were born in Guatemala, and 2% were born in Puerto Rico.
Terminology for race/ethnicity in the literature varies with no clear consensus; here, we refer to African American/Black individuals as “Black,” Latino/Hispanic individuals as “Latina” or “Latino,” and non-Hispanic/White individuals as “White.”
Prior to the study, we conducted intensive interviewer training coordinated across sites, after which they were certified in the key principles of the study. In the interviewer training, we utilized materials designed for the study by members of all sites to maintain consistency in the data collection and to ensure scientific integrity. CCHN community partners participated in and led some of the interviewer training sessions. Training materials included specifics on survey interviewing skills (e.g., professional conduct, how to build rapport, and how to ask questions). Interview specifications pertaining to the questions in each interview were fully documented for use in training. Training also covered any possible risks to interviewers and participants, such as how to handle participant distress and how to ensure their own safety when doing home visits. In addition, interviewers completed site-specific mandated training in the responsible conduct of research.
All indices were tested for internal consistency with Cronbach alpha coefficients and were found to be acceptable to good in both languages and for mothers and fathers: Perceived Stress Scale (Cohen et al, 1983) Time 1, α = .83 (mothers in English and Spanish), α = .81 (fathers in English), and α = .78 (fathers in Spanish); Perceived Stress Scale at Time 2, α = .85 (mothers in English), α = .79 (mothers in Spanish), α = .83 (fathers in English), and α = .81 (fathers in Spanish). For the Life Stress Interview (Hammen et al., 1987) measure of chronic stress (across the four domains), α = .65 (mothers in English), α = .70 (fathers in English), α = .59 (mothers in Spanish), and α = .68 (fathers in Spanish). For the financial stress index, α = .69 (mothers in English), α = .68 (mothers in Spanish), α = .68 (fathers in English), and α = .61 (fathers in Spanish). Everyday discrimination, when scored for any unfair treatment regardless of attribution, was α = .89 (mothers and fathers in English), α = .88 (mothers in Spanish), and α = .89 (fathers in Spanish). Parenting stress was α = .92 (mothers in English), α = .94 (mothers in Spanish), α = .93 (fathers in English), and α = .96 (fathers in Spanish). Only mothers completed the other two measures: the HITS measure (a four-item questionnaire in which respondents were asked how often their partner physically Hurt, Insulted, Threatened with harm, and Screamed at them; Sherin et al., 1998) of IPV (α = .74 in both languages) and the pregnancy stress inventory (α = .76 in English, and α = .75 in Spanish).
The following pertains to missing data: Data analysis involved data cleaning and treatment of missing data conducted by the Data Coordination and Analyses Center of the CCHN. Details on treatment of missing data are available from the authors. All the interview measures except the chronic stress scale had the largest percentage of partial data imputation, with 4.5% of the scale having items that were imputed for mothers and 6.4% for fathers. All other scales had <3% partial data imputation. The following pertains to analysis: As a preliminary step, we conducted analyses in which we compared the five CCHN sites using analyses of variance (ANOVAs) and controlled for race/ethnicity and poverty group. With race/ethnicity and poverty group controlled, there were significant effects in stress among sites but there were small effect sizes (results not shown). Therefore, in our analyses, we do not control for site. The general statistical approach to testing variation in these stress measures was a two-way ANOVA on the basis of three poverty categories crossed with three racial/ethnic categories. We examined histograms of the distributions of the scales prior to the analysis and observed that three scales (IPV, life event impact, and pregnancy stress) had highly skewed response distributions. Therefore, we log-transformed the data from these three scales prior to applying the analysis of variance. When reporting the descriptive statistics, however, we rely on the untransformed scores. If the Race × Income interactions were statistically significant, then one-way ANOVAs with a Bonferroni-corrected significance level of .0027 were applied for each of 18 pairwise comparisons. If the Racial/Ethnic Group × Poverty Group interaction was not significant, then a significance level of .0083 was used for each of the six pairwise comparisons (three pairwise comparisons of the race groups and three pairwise comparisons of the income groups). For the categorized everyday racism index, ordinal logistic regression was used. Associations of per capita household income and parental education with stress measures were examined via Pearson correlations for the continuous stress measures and Kendall's tau-b for the racism index. Given the large number of correlations computed, we used a higher significance level of p < .001 to interpret these results.
In addition to examining poverty as a contributor to stress, which this study was designed to do, we examined SES by per capita household income and parental educational attainment, which is a more conventional analysis (Kraus & Stephens, 2012). These analyses showed consistent inverse associations of the continuous measure of household income adjusted for cost of living with many forms of stress among mothers and fathers, similar to a prior study in which different stress measures in quite a different sample were used (Williams et al., 1997). Higher SES was associated with significantly lower reports by mothers and fathers of all ethnic/racial backgrounds of financial stress, chronic stress, perceived stress 1 month after birth, parenting stress, perceived racism, life events, and, among mothers, lower IPV. Repeating SES analyses within each of the three ethnic/racial groups revealed somewhat stronger effects for both household income and parental education among White mothers and fathers compared with the other two groups.
Declaration of Conflicting Interests
The authors declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Supplemental Material
Additional supporting information may be found at http://pps.sagepub.com/content/by/supplemental-data
References
- Abdou CM, Dunkel Schetter C, Jones F, Roubinov D, Tsai S, Jones L, Hobel C. Community perspectives: Mixed-methods investigation of culture, stress, resilience, and health. Ethnicity & Disease. 2010;20(2):41–48. [PMC free article] [PubMed] [Google Scholar]
- Abidin RR. Parenting Stress Index/Short form. Psychological Assessment Resources; Lutz, FL: 1990. [Google Scholar]
- Abidin RR. Parenting Stress Index, Short Form Third Edition: Professional manual. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Abidin RR, Brunner JF. Development of a parenting alliance inventory. Journal of Clinical and Child Psychology. 1995;24:31–40. [Google Scholar]
- Acevedo-Garcia D, Soobader M, Berkman L. Low birthweight among US Hispanic/Latino subgroups: The effect of maternal foreign-born status and education. Social Science & Medicine. 2007;65:2503–2516. doi: 10.1016/j.socscimed.2007.06.033. [DOI] [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–253. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2005;12:119–123. [Google Scholar]
- Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Science. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality . National health care disparities report. U.S. Department of Health and Human Services; Washington, DC: 2006. [Google Scholar]
- Aldwyn C. Stress, coping, and development: An integrative perspective. Guilford Press; New York, NY: 2007. [Google Scholar]
- Baum A. Stress, intrusive imagery, and chronic distress. Health Psychology. 1990;9:653–675. doi: 10.1037//0278-6133.9.6.653. [DOI] [PubMed] [Google Scholar]
- Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: Does stress account for SES effects on health? Annals of the New York Academy of Science. 1999;896:131–144. doi: 10.1111/j.1749-6632.1999.tb08111.x. [DOI] [PubMed] [Google Scholar]
- Blumenshine P, Egerter S, Barclay C, Cubbin C, Braveman P. Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine. 2010;39:263–272. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: What the patterns tell us. American Journal of Public Health. 2010;100(Suppl. 1):S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks-Gunn J, Duncan G, Aber J, editors. Neighborhood poverty (volume 1): Context and consequences for children. Russell Sage; New York, NY: 1997. [Google Scholar]
- Busacker A, Kasehagen L. Association of residential mobility with child health: An analysis of the 2007 National Survey of Children's Health. Maternal Child Health Journal. 2012;16:S78–S87. doi: 10.1007/s10995-012-0997-8. [DOI] [PubMed] [Google Scholar]
- Caetano R, Field CA, Ramisetty-Mikler S, McGrath C. The 5-year course of intimate partner violence among White, Black, and Hispanic couples in the United States. Journal of Interpersonal Violence. 2005;20:1039–1057. doi: 10.1177/0886260505277783. [DOI] [PubMed] [Google Scholar]
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O'Campo P, Wynne C. Intimate partner violence and physical health consequences. Archives of Internal Medicine. 2002;162:1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Campos B, Dunkel-Schetter C, Walsh JA, Schenker M. Sharpening the focus on acculturative change: ARSMA-II, stress, pregnancy anxiety, and infant birth-weight in recently immigrated Latinas. Hispanic Journal of Behavioral Sciences. 2007;29:209–224. [Google Scholar]
- Chandola T, Marmot MG. Socioeconomic status and stress. In: Contrada R, Baum A, editors. The handbook of stress science. Springer; New York, NY: 2011. pp. 185–193. [Google Scholar]
- Chen E, Martin AD, Matthews KA. Socioeconomic status and health: Do gradients differ within childhood and adolescence? Social Science & Medicine. 2006;62:2161–2170. doi: 10.1016/j.socscimed.2005.08.054. [DOI] [PubMed] [Google Scholar]
- Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children's health: How and why do these relationships change with age? Psychological Bulletin. 2002;128:295–329. doi: 10.1037/0033-2909.128.2.295. [DOI] [PubMed] [Google Scholar]
- Chen E, Miller GE. “Shift-and-persist” strategies: Why low socioeconomic status isn't always bad for health. Perspectives on Psychological Science. 2012;7:135–158. doi: 10.1177/1745691612436694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Class QA, Lichtenstein P, Langstrom N, D'Onofrio BM. Timing of prenatal maternal exposure to severe life events and adverse pregnancy outcomes: A population study of 2.6 million pregnancies. Psychosomatic Medicine. 2011;73:234–241. doi: 10.1097/PSY.0b013e31820a62ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology. 2012;42:1320–1334. [Google Scholar]
- Cohen S, Janicki-Deverts D, Chen E, Matthews KA. Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences. 2010;1186:37–55. doi: 10.1111/j.1749-6632.2009.05334.x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S, Kessler RC, Gordon LU. Strategies for measuring stress in studies of psychiatric and physical disorders. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: A guide for health and social scientists. Oxford University Press; New York, NY: 1995. pp. 3–26. [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample in the U.S. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont symposium on applied social psychology. SAGE; Newbury Park, CA: 1988. pp. 31–67. [Google Scholar]
- Coleman-Jensen A, Nord M, Andrews M, Carlson S. Household food security in the United States in 2010. U. S. Department of Agriculture; Washington, DC: 2011. pp. 8–15. [Google Scholar]
- Curry MA, Burton D, Fields J. The Prenatal Psychosocial Profile: A research and clinical tool. Research in Nursing & Health. 1998;21:211–219. doi: 10.1002/(sici)1098-240x(199806)21:3<211::aid-nur4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Curry MA, Campbell RA, Christian M. Validity and reliability testing of the Prenatal Psychosocial Profile. Research in Nursing & Health. 1994;17:127–135. doi: 10.1002/nur.4770170208. [DOI] [PubMed] [Google Scholar]
- Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. American Journal of Epidemiology. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- Dominguez TP. Race, racism, and racial disparities in adverse birth outcomes. Clinical Obstetrics and Gynecology. 2008;51:360–370. doi: 10.1097/GRF.0b013e31816f28de. [DOI] [PubMed] [Google Scholar]
- Dominguez TP, Dunkel Schetter C, Mancuso R, Rini C, Hobel C. Stress in African American pregnancies: Testing the roles of various stress concepts in prediction of birth outcomes. Annals of Behavioral Medicine. 2005;29(1):12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: Models to explain health disparities. Annual Review of Anthropology. 2005;34:231–252. [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C, Dolbier C. Resilience in the context of chronic stress and health in adults. Social & Personality Psychology Compass. 2011;5:634–652. doi: 10.1111/j.1751-9004.2011.00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, Lobel M. Pregnancy and birth outcomes: A multi-level analysis of prenatal stress and birth weight. In: Revenson TA, Baum A, Singer J, editors. Handbook of health psychology. 2nd ed. Psychology Press; London, England: 2012. pp. 431–464. [Google Scholar]
- Fleming I, Baum A, Davidson LM, Rectanus E, McArdle SS. Chronic stress as a factor in physiologic reactivity to challenge. Health Psychology. 1987;6:221–237. doi: 10.1037//0278-6133.6.3.221. [DOI] [PubMed] [Google Scholar]
- Flores E, Tschann J, Dimas J, Bachen E, Pasch L, de Groat C. Perceived discrimination, perceived stress, and mental and physical health among Mexican-Origin adults. Hispanic Journal of Behavioral Sciences. 2008;30:401–424. [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethnicity and Disease. 2001;11:496–518. [PubMed] [Google Scholar]
- Gallo LC, de los Monteros KE, Shivpuri S. Socioeconomic status and health: What is the role of reserve capacity? Current Directions in Psychological Science. 2009;18:269–274. doi: 10.1111/j.1467-8721.2009.01650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Geronimus AT. The weathering hypothesis and the health of African American women and infants: Evidence and speculations. Ethnicity & Disease. 1992;2:207–221. [PubMed] [Google Scholar]
- Giscombé CL, Lobel M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: The impact of stress, racism, and related factors in pregnancy. Psychological Bulletin. 2005;131:662–683. doi: 10.1037/0033-2909.131.5.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb B, editor. Coping with chronic stress. Plenum Press; New York, NY: 1997. [Google Scholar]
- Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D. Children of depressed mothers: Maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology. 1987;96:190–198. doi: 10.1037//0021-843x.96.3.190. [DOI] [PubMed] [Google Scholar]
- Hammen C, Davila J, Brown GW, Ellicott A, Gitlin M. Psychiatric history and stress: Predictors of severity of unipolar depression. Journal of Abnormal Psychology. 1992;101:45–52. doi: 10.1037//0021-843x.101.1.45. [DOI] [PubMed] [Google Scholar]
- Hauck F, Tanabe K, Moon R. Racial and ethnic disparities in infant mortality. Seminars in Perinatology. 2011;35:209–220. doi: 10.1053/j.semperi.2011.02.018. [DOI] [PubMed] [Google Scholar]
- Hobel C, Goldstein A, Barrett E. Psychosocial stress and pregnancy outcome. Clinical Obstetrics and Gynecology. 2008;51:338–348. doi: 10.1097/GRF.0b013e31816f2709. [DOI] [PubMed] [Google Scholar]
- House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, editors. Promoting health: Intervention strategies from social and behavioral research. National Academy Press; Washington, DC: 2000. pp. 81–124. [PubMed] [Google Scholar]
- Israel B, Eng E, Schulz A, Parker E, editors. Methods in community-based participatory research for health. Jossey-Bass; San Francisco, CA: 2005. [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP. Levels of racism: A theoretic framework and a gardener's tale. American Journal of Public Health. 2000;90:1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller A, Litzelman K, Wisk LE, Maddox T, Cheng ER, Creswell PD, Witt WP. Does the perception that stress affects health matter? The association with health and mortality. Health Psychology. 2012;31:677–684. doi: 10.1037/a0026743. doi:10.1037/a0026743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemeny M. The psychobiology of stress. Current Directions in Psychological Science. 2003;12:124–129. [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Review of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Koh HK. A 2020 vision for healthy people. New England Journal of Medicine. 2010;362:1653–1656. doi: 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- Kramer MR, Hogue CJ, Dunlop AL, Menon R. Preconceptional stress and racial disparities in preterm birth: An overview. Acta Obstetrica Gynecologica Scandinavica. 2011;90:1307–1313. doi: 10.1111/j.1600-0412.2011.01136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus MW, Stephens NM. A road map for an emerging psychology of social class. Social & Personality Psychology Compass. 2012;6:642–656. [Google Scholar]
- Kressin NR, Raymond KL, Manze M. Perceptions of race/ethnicity-based discrimination: A review of measures and evaluation of their usefulness for the health care setting. Journal of Health Care for the Poor and Underserved. 2008;19:697–730. doi: 10.1353/hpu.0.0041. doi:10.1353/hpu.0.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford University Press; Oxford, England: 2000. pp. 36–75. [Google Scholar]
- Lantz PM, House JS, Mero RP, Williams DR. Stress, life events, and socioeconomic disparities in health: Results from the Americans’ Changing Lives Study. Journal of Health and Social Behavior. 2005;46:274–288. doi: 10.1177/002214650504600305. [DOI] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanzi RG, Ramey SL, Bert SC. The parenting responsibility and emotional preparedness screening tool: A 3-item screen that identifies teen mothers at high risk for non-optimal parenting. Archives of Pediatrics and Adolescent Medicine. 2012;166(8):1–7. doi: 10.1001/archpediatrics.2012.143. [DOI] [PubMed] [Google Scholar]
- Laraia BA, Messer L, Kaufman JS, Dole N, Caughy M, O'Campo P, Savitz DA. Direct observation of neighborhood attributes in an urban area of the US south: Characterizing the social context of pregnancy. International Journal of Health Geographics. 2006;5:1–11. doi: 10.1186/1476-072X-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal and coping. Springer; New York, NY: 1984. [Google Scholar]
- Lewin K. Action research and minority problems. Journal of Social Issues. 1946;2(4):34–46. [Google Scholar]
- Lobel M, Dunkel Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: A prospective study of socioeconomically disadvantaged women. Health Psychology. 1992;11:32–40. doi: 10.1037//0278-6133.11.1.32. [DOI] [PubMed] [Google Scholar]
- Lu MC, Jones L, Bond MJ, Wright K, Pumpuang M, Maidenberg M, Rowley DL. Where is the F in MCH? Father involvement in African American families. Ethnicity and Disease. 2005;20:S2–49–S2-61. [PubMed] [Google Scholar]
- Marin GDL, Gamba RJ. A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS). Hispanic Journal of Behavioral Sciences. 1996;18:297–316. [Google Scholar]
- Marmot M. Multilevel approaches to understanding social determinants. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford University Press; Oxford, England: 2000. pp. 349–367. [Google Scholar]
- Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, Wilson EC. Births: Final data for 2009. National Vital Statistics Reports. 2011;60(1):1–72. [PubMed] [Google Scholar]
- Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology. 2011;62:501–530. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCubbin HI, Thompson EA, Thompson AI, Futrell JA, editors. Resiliency in African American families. SAGE; Beverly Hills, CA: 1998. [Google Scholar]
- McEwen BS. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Annals of the New York Academy of Sciences. 2001;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. Journal of Health and Social Behavior. 1990;31:162–172. [PubMed] [Google Scholar]
- Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid-resistance model. Health Psychology. 2002;21:531–541. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- Minino A, Murphy S, Xu J, Kochaneck K. Deaths: Final data for 2008. National Vital Statistics Reports. 2011;59(10):1–157. [PubMed] [Google Scholar]
- Misra DP, O'Campo P, Strobino D. Testing a sociomedical model for preterm delivery. Paediatric and Perinatal Epidemiology. 2001;15:110–122. doi: 10.1046/j.1365-3016.2001.00333.x. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. Understanding the cumulative impacts of inequalities in environmental health: Implications for policy. Health Affairs. 2011;30:879–887. doi: 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- Mostofsky E, Maclure M, Sherwood JB, Tofler GH, Muller JE, Mittleman MA. Risk of acute myocardial infarction after the death of a significant person in one's life: The determinants of Myocardial Infarction Onset Study. Circulation. 2012;125:491–496. doi: 10.1161/CIRCULATIONAHA.111.061770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers HF. Ethnicity- and socio-economic status-related stresses in context: An integrative review and conceptual model. Journal of Behavioral Medicine. 2009;32:9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- O'Campo P, Caughy MO, Nettles SM. Partner abuse or violence, parenting and neighborhood influences on children's behavioral problems. Social Science & Medicine. 2010;70:1404–1415. doi: 10.1016/j.socscimed.2009.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ockenfels MC, Porter L, Smyth J, Kirschbaum C, Hellhammer DH, Stone AA. Effect of chronic stress associated with unemployment on salivary cortisol: Overall cortisol levels, diurnal rhythm, and acute stress reactivity. Psychosomatic Medicine. 1995;57:460–467. doi: 10.1097/00006842-199509000-00008. [DOI] [PubMed] [Google Scholar]
- Olson M, Diekema D, Elliott B, Renier C. Impact of income and income inequality on infant health outcomes in the United States. Pediatrics. 2010;126:1165–1173. doi: 10.1542/peds.2009-3378. [DOI] [PubMed] [Google Scholar]
- Ong A, Fuller-Rowell T, Burrow A. Racial discrimination and the stress process. Journal of Personality and Social Psychology. 2009;96:1259–1271. doi: 10.1037/a0015335. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Richman LS. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI. The sociological study of stress. Journal of Health and Social Behavior. 1989;30:241–256. [PubMed] [Google Scholar]
- Perez DJ, Fortuna L, Alegria M. Prevalence and correlates of everyday discrimination among U.S. Latinos. Journal of Community Psychology. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramey SL, Schafer P, DeClerque J, Lanzi RG, Hobel C, Shalowitz M, Raju TN. The Community Child Health Network (CCHN): A transdisciplinary community-academic partnership reframes research on pre-conception health and child outcomes. 2013. Unpublished manuscript.
- Renzaho AM, Houng B, Oldroyd J, Nicholson JM, D'Esposito F, Oldenburg B. Stressful life events and the onset of chronic diseases among Australian adults: Findings from a longitudinal survey. European Journal of Public Health. 2013 doi: 10.1093/eurpub/ckt007. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social Science & Medicine. 2011;72:977–983. doi: 10.1016/j.socscimed.2011.01.013. [DOI] [PubMed] [Google Scholar]
- Sbarra DA, Law RW, Portley RM. Divorce and death: A meta-analysis and research agenda for clinical, social, and health psychology. Perspectives on Psychological Science. 2011;6:454–474. doi: 10.1177/1745691611414724. [DOI] [PubMed] [Google Scholar]
- Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: A short domestic violence screening tool for use in a family practice setting. Family Medicine. 1998;30:508–512. [PubMed] [Google Scholar]
- Smedley BD, Syme SL, editors. Promoting health: Intervention strategies from social and behavioral research. National Academy Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- Spong CY, Iams J, Goldenberg R, Hauck FR, Willinger M. Disparities in perinatal medicine: Preterm birth, stillbirth, and infant mortality. Obstetrics & Gynecology. 2011;117:948–955. doi: 10.1097/AOG.0b013e318211726f. [DOI] [PubMed] [Google Scholar]
- Stapleton L, Dooley L, Paek C, Huynh J, Dunkel Schetter C. Development and early validation findings for a brief Chronic Stress Interview Measure: The CCHN LSI Interview. 2013. Manuscript submitted for publication.
- Taylor SE, Repetti RL, Seeman T. Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress and health: Major findings and policy implications. Journal of Health and Social Behavior. 2010;51(1 Suppl.):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Turner RJ. Understanding health disparities: The promise of the stress process model. In: Avison WR, Aneshensel CS, Schieman S, Wheaton B, editors. Advances in the conceptualization of the stress process: Essays in honor of Leonard I. Pearlin. Springer; New York, NY: 2010. pp. 3–21. [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44:488–505. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Turner RJ, Wheaton B. Checklist measurement of life events. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: A guide for health and social scientists. Oxford University Press; New York, NY: 1995. pp. 29–58. [Google Scholar]
- Vines AI, Ta M, Esserman D, Baird DD. A comparison of the occurrence and perceived stress of major life events in black and white women. Women & Health. 2009;49:368–380. doi: 10.1080/03630240903238743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton B. Sampling the stress universe. In: Avison WR, Gotlib IH, editors. Stress and mental health. Plenum; New York City, NY: 1994. pp. 77–114. [Google Scholar]
- Wheaton B, Montazer S. Stressors, stress, and distress. In: Scheid TL, Brown TN, editors. A handbook for the study of mental health: Social contexts, theories, and systems. Cambridge University Press; Cambridge, England: 2010. pp. 171–199. [Google Scholar]
- Williams DR. Race, SES, and health: The added effects of racism and discrimination. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrialized nations: Social, psychological and biological pathways. New York Academy of Sciences; New York City, NY: 2009. pp. 173–188. [Google Scholar]
- Williams D, Yu Y, Jackson JS, Anderson N. Racial differences in physical and mental health. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EK. Acculturation and changes in the likelihood of pregnancy and feelings about pregnancy among women of Mexican origin. Women & Health. 2008;47:45–64. doi: 10.1300/J013v47n01_03. [DOI] [PubMed] [Google Scholar]
- Zambrana R, Dunkel-Schetter C, Collins N, Scrimshaw S. Mediators of ethnic-associated differences in infant birth weight. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 1999;76:102–116. doi: 10.1007/BF02344465. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.