Abstract
By mimicking the variable resolution of the human eye, a newly designed foveated endomicroscopic objective shows the potential to improve current endoscopic based techniques of identifying abnormal tissue in the esophagus and colon. The prototype miniature foveated objective is imaged with a confocal microscope to provide large field of view images combined with a high resolution central region to rapidly observe morphological structures associated with cancer development in a mouse model.
OCIS codes: (170.2150) Endoscopic imaging, (350.3950) Micro-optics, (170.3880) Medical and biological imaging, (170.3890) Medical optics instrumentation, (170.1790) Confocal microscopy
1. Introduction
Accounting for approximately 28 percent of the deaths due to cancer in the United States, gastrointestinal carcinomas result in more deaths around than the world than all other malignancies [1]. Gastrointestinal cancers affect the entire GI tract, including the esophagus, stomach, pancreas, liver, gallbladder, colon and the anus. Esophageal adenocarcinoma (EAC) is a particularly devastating form of GI cancer due to a very dismal five-year survival prognosis of less than 10%. The incidence of developing EAC has increased at a greater rate than any other cancerous tumor type in the United States since 1975 [2]. Thus, there is a vital need for early detection and treatment of EAC and the preconditions associated with the malignancy [3]. A common precursor to EAC, Barrett’s Esophagus (BE) is defined as the replacement of normal squamous epithelium of the esophagus above the gastroesophageal junction by columnar epithelium often due to the long-term exposure of gastric acid reflux from gastroesophageal reflux disease (GERD) [4]. When stratified squamous epithelium is replaced by metaplastic intestinal columnar epithelium with goblet cells, BE becomes a much greater risk factor (30 to 50 times) to EAC development [5]. Monitoring the development and progression of BE is crucial for early detection and treatment of EAC.
The gold standard for screening high grade dysplasia (the typical intermediate stage as metaplastic epithelium progresses to cancer) in BE is the Seattle Protocol - an upper endoscopy biopsy procedure that uses traditional endoscopic surveillance to visually locate suspicious lesions that are then biopsied every 1 cm of the Barrett’s segment for histological analysis by a pathologist. Although somewhat systematic, the expensive and time-intensive quadrant biopsies miss 40-60% of focal dysplasia and cancer within large Barrett’s segments, which are often up to 20 cm in length [6]. Optical biopsy methods are a particularly promising solution to improve upon the inaccuracies and imprecision of the Seattle Protocol.
Current generation endoscopes typically utilize high-definition white-light endoscopy (HD-WLE) in combination with a variation of Narrow Band Imaging (NBI), a technique that aids in diagnosis by enhancing the visualization of microvasculature [7]. Other methods including chromoendoscopy, autofluorescence and multispectral imaging have also been investigated to aid in the visualization of diagnostically relevant architectural and molecular changes. However, a significant increase in sensitivity for detecting neoplasia over HD-WLE and biopsy has not been observed [8]. A recent study suggested that a combination of HD-WLE with NBI or some other visual enhancement technique with a higher optical resolution imaging modality such as confocal imaging could improve sensitivity of detection by resolving the adequate spatial details to identify neoplastic progression [9]. Confocal laser endomicroscopy (CLE) utilizes miniature optics and a spatial filter to significantly improve contrast and axial and lateral resolution. Due to diffraction effects and a fixed detector size of CLEs, the field of view (FOV) is limited to only a few hundred micrometers (as defined by the optical or Lagrange invariant), minimizing the usefulness of the device when navigating a long segment of BE.
In order to improve upon the deficiencies of current optical biopsy techniques, a single miniature system needs to combine high resolution imaging with the broad screening capabilities of enhanced visualization techniques. We have addressed these concerns through the development of a multimodal foveated endomicroscope system. By mimicking the human eye, a miniature custom foveated objective can provide a large FOV of several millimeters with micron level resolution in the central of the field. The output of the objective, integrated with an image guide, can then be divided into a broad surveillance mode of in vivo tissue through techniques like multi-spectral imaging, NBI or other visual enhancement method (to map biochemical signatures) in order to locate suspicious lesions that can then be further inspected through a confocal mode to observe morphological structures. The work presented here is focused on the design, fabrication and validation of the foveated endomicroscope objective integrated with a confocal microscope.
2. Foveated miniature objective
Several attempts have been made to produce an imaging system that balances achievable resolution with large FOV by emulating the human eye [10–16]. Through the human eye, we observe a drop off in imaging performance from the center of the FOV to the edge as most of the spatial detail is sampled in the center due to a higher concentration of rods and cones in the fovea centralis. By mimicking this separation of resolution regions through optical design, the traditional expected relationship between FOV, probe size, and resolution can be overcome, resulting in a large FOV with high resolution at the center of the optical axis. The resulting image contains distinct regions, with a lower resolution area providing “red-flag” surveillance to direct the high-resolution region towards the area of interest in order to inspect with greater detail. Attempted techniques for replicating the foveated phenomenon have included the use of mirrors, spatially tunable phase elements, sensor array manipulation, and high distortion inducing optics [10–14]. Most of these devices however, have been limited by bulky components, further limiting the adoption by clinicians.
In a prior publication, Hagen et al were able to demonstrate the initial concept of a foveated endomicroscope [10]. The objective that was fabricated utilizing a combination of custom built aspheric lenses and an off the shelf glass lens produced foveated images with resolution of 7-8 μm on axis and an overall FOV of 4.6 mm. While an elegant solution, the design was not without faults. Due to very tight machining tolerances that could not be trivially met, the prototype had to be built on large 38 mm disks, much too large to be considered an endomicroscope. Additionally, the use of large 3D printed holders was needed for precise alignment of the individual optical components. With this precision alignment it was possible to produce full field images, however damage to the lenses reduced the achievable resolution. Ultimately, this proof of concept objective did not exhibit resolution necessary for BE imaging and could not be assembled in a small format compatible with standard endoscopes.
2.1. Optical design of foveated objective
The major design guidelines for the foveated endomicroscope objective are as follows: a completely integrated miniature objective with outer diameter less than 2.8 mm to fit the standard tool channel of an upper endoscope, the ability to resolve between 2 to 3 μm in order to visualize cellular changes associated with dysplasia, and a large enough field of view (~5 mm) to provide sufficient context of the surrounding areas. To meet these design requirements, a new foveated endomicroscope was designed in the optical design software ZEMAX (Radiant Zemax, LLC., Redmond, Washington). The objective is loosely based off of a design from our previously published work [10]. Specific changes included removing the off the shelf glass lens and switching to three custom lenses. Additionally, the total length and clear aperture of the objective were reduced and machine tolerances were more accurately accounted for. Finally, the three elements were fabricated to include physical spacers, simplifying the assembly process in order to improve build reliability.
In order to provide both a large FOV and the ability to resolve fine features, the objective utilizes a large amount of negative distortion in order to decrease the numerical aperture and magnification as distance from the optical axis increases. The layout of this foveated objective is shown in Fig. 1.
Fig. 1.
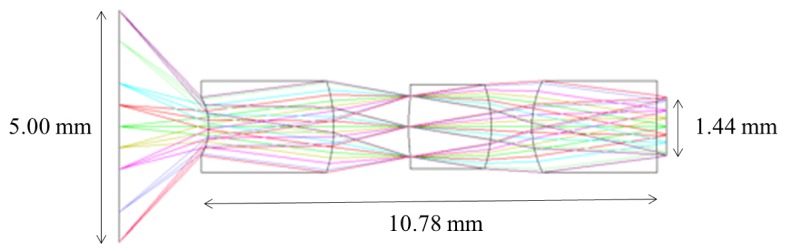
Optical layout of foveated design.
The design consists of three elements: zinc sulfide (ZnS) and two poly (methyl-methacrylate) (PMMA) aspheric lenses. The first lens, which provides most of the optical power, is fabricated from zinc sulfide (ZnS), a rugged polycrystalline material with a high refractive index (n = 2.419 at 500 nm). The second and third lenses of PMMA, with a refractive index of n = 1.49, provide ease of fabrication for aspheric surfaces, low auto florescence for the design wavelength, and high transmission. The optical prescription of the objective can be found in Table 1.
Table 1. Optical prescription of the foveated objective.
| Glass | Radius | Thickness | Semi-Diameter | 2nd Order Term | 4th Order Term |
|---|---|---|---|---|---|
| — | Infinity | 2.150000 | 2.500000 | — | — |
| ZnS | −1.455565 | 3.011256 | 0.671249 | −0.072069 | 0.021755 |
| — | −3.318246 | 1.801397 | 1.064858 | — | — |
| PMMA | 4.894459 | 1.993937 | 0.709224 | −0.013088 | — |
| — | −2.986461 | 0.980410 | 0.982669 | — | — |
| PMMA | 2.369662 | 3.004441 | 1.066610 | — | — |
| — | −4.055369 | 0.231411 | 0.722063 | 0.647925 | −0.716443 |
The expected foveated image is produced by the distortion that is introduced via the first surface of the objective, resulting in the fisheye-like appearance. The current objective was optimized for the 510 nm wavelength with a ± 50 nm range; in order to be near the emission peak of proflavine. Proflavine is a fluorescent dye that stains cell nuclei, enhancing visualization. Table 2 provides the expected change in magnification and NA as the field changes. According to the equation for Rayleigh Resolution (d = 0.61*λ/NA), with an NA of 0.1, at the wavelength of 510 nm would provide a resolution of 3.11 μm, where d is the minimum distance between two points where it is possible to distinguish each.
Table 2. Design parameters across the field.
| Working Distance 2.1 mm | |||
|---|---|---|---|
| Field (mm) | NA | M | Rayleigh Resolution (μm) |
| 0 | 0.100 | 0.39 | 3.11 |
| 0.5 | 0.098/0.095 | 0.37 | 3.17/3.27 |
| 1 | 0.092/0.082 | 0.30 | 3.38/3.79 |
| 2 | 0.074/0.045 | 0.14 | 4.20/6.91 |
| 2.5 | 0.061/0.024 | 0.06 | 5.10/13.0 |
Field refers to the semi diameter from the optical axis. Due to the elliptical pupil at larger fields, the tangential/sagittal values are each defined by the two numbers with a slash. M refers to magnification. The Rayleigh resolutions were calculate for λ = 510 nm.
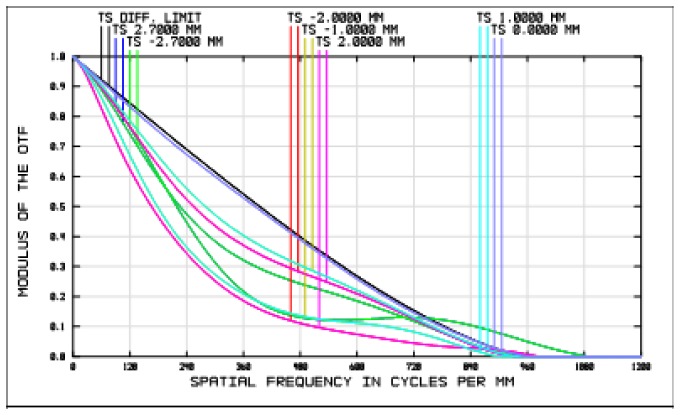
As displayed by the modulation transfer function (Fig. 2), the design is diffraction limited along the axis, with an expected drop off across the field due to the matching decreasing NA and associated magnification.
Fig. 2.
The modulation transfer function of the foveated design.
The design is telecentric in the image space, with a NA of 0.22 that does not change across the field, allowing the objective to be integrated with an optical fiber guide with high coupling efficiency.
3. Tolerancing and fabrication
When optimizing an optical design, it is crucial to take into account the effects that manufacturing and the assembly process impart on optical performance. Of particular importance for single-point diamond-turning (SPDT), is accounting for surface and element tilt, surface quality in terms of roughness, decentration, surface radii, and distances between surfaces and elements. The expected values of these tolerances are unique to the manufacturing process. For example, the surface roughness and the surface radius are due to SPDT tool alignment and cutting speeds. Analysis with a white-light interferometer allows for quantification of the quality of the optical surface in terms of surface roughness, while a Fizeau interferometer provides deviations of the cut radii from the design. From the white-light interferometer, typical achievable root-mean-squared (RMS) roughnesses were measured to be approximately 10 nm for PMMA and 5 nm for ZnS.
Radius values typically have approximately 1% error. Expected surface and element tilt are due to the frequent realignment of the mounts holding the elements after each cut. Tilt refers to the change in angle of the optomechanical axis from predicted to actual, while decentration is the distance between the predicted and actual center axis. Experimentally, it was found that tilt values vary significantly depending on the length of the lens, with a value of 3° not uncommon for lenses below 1 mm in length. For longer lenses (as used in this design) however, this number is significantly reduced. ZEMAX calculates the change in RMS wavefront error via a Monte-Carlo analysis due to perturbations of the tolerances in order to ensure a diffraction-limited system. The wavefront error is the average deviation from the expected wavefront, due to aberrations and tolerances that have caused the wavefront to change. Generally, if the RMS wavefront error is kept below 0.07*λ, then the expected fabricated system is considered diffraction limited. A list of the expected tolerances can be found in Table 3.
Table 3. Expected fabrication tolerances for lenses.
| Tolerance Parameter | Expected Limit |
|---|---|
| Radius (%) | ± 1 |
| Thickness (mm) | ± 0.040 |
| Surface Decenter (mm) | ± 0.020 |
| Surface Tilt (deg) | ± 0.15 |
| Element Tilt (deg) | ± 0.30 |
| Index (%) | ± 1 |
The fabricated objective consists of three single-point diamond-turned (SPDT) elements. Each element is fabricated to include spacing features that act as optical stops for the clear apertures, provide precise alignment, and allow the lenses to be press-fitted inside a hypodermic tube. The design was optimized to include a cover slip on the object side to further protect the objective. SPDT allows for the fabrication of both high quality miniature spherical and aspheric lenses. Aspheric lenses, while traditionally more difficult to manufacture using other methods, provide corrections for spherical and monochromatic aberrations. Because of this, it is possible to design diffraction-limited objectives with fewer elements.
To begin the lens fabrication process, precursors are cut from large disks or rods of the appropriate raw material. The coordinates of the cut are determined using the program NanoCAM 2D (Moore Nanotechnology Systems, LLC, Swanzey, New Hampshire) Manual coordinates were added to cut each lens surface to include precision spacer features, which accurately maintain the distance between each element. Figure 3 displays the cut path of the machine with the added spacing features - the optical lens surface (red) transitions into a slant (pink) to the flat surface that defines the position of the lens within the system (blue).
Fig. 3.
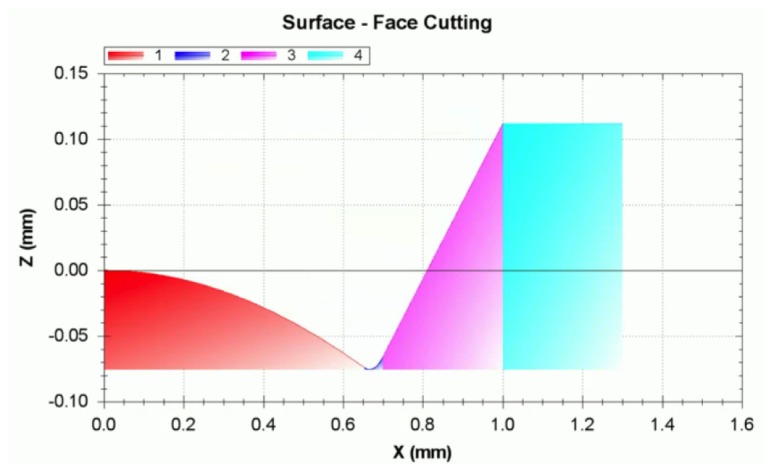
NanoCAM 2D drawing of the face cutting to be performed by the diamond turning machines of one surface of one of the lenses in the objective. The central axis of the lens is on the far left at point 0.00, 0.00. The red spherical surface is the optical surface. The pink surface and blue surfaces are covered with an acrylic marker in order to clearly define the clear aperture and reduce unwanted scattering of the light.
A hypodermic tube acts as the barrel that encloses the objective. Without the use of any other optomechanics, the compression provided by the tube is the only factor controlling the alignment of optical components. The hypodermic tubing is able to maintain an alignment tolerance of influencing decentration +/− 0.020 mm due to the quality of the surface of the tube as measured by an interferometer.
4. Objective performance and distortion removal
The initial validation of the foveated objective was performed using a 1951 USAF resolution target to assess the achievable resolution by observing the smallest resolvable features, find the Modulation Transfer Function (MTF), and estimate the Strehl Ratio (SR). The SR, a standard relationship used to evaluate measured optical performance relative to an ideal, compares the measured peak irradiance in the Airy disk to the expected theoretical Airy disk of a diffraction limited system [17]. The slanted edge technique approximates the SR by comparing the area under the measured MTF to the theoretical. The area under the measured MTF is found with the resolution target by measuring contrast between the white and black regions as imaged by the detector. A system with a SR of 0.8 is traditionally considered to be diffraction limited.
For testing purposes, the foveated endomicroscope was relayed through a 10x, 0.25NA commercial Zeiss objective onto an inverted brightfield Zeiss microscope at 490 nm. At the designed working distance of 2.1 mm, and a wavelength of 490 nm, the objective should be able to resolve 2.98 μm, corresponding to between elements 3 and 4 of group 8. An image of the USAF objective at the center of the FOV shows the ability of the objective to resolve at least element 3 in group 8 as indicated by the red box (Fig. 4(c)). The slanted edge technique resulted in a SR of 0.82.
Fig. 4.

(A) Image of 1951 resolution target imaged through the objective showing the full field (5 mm) with red box indicating the higher resolution features. (B) Close up of resolution target with red box indicating the highest resolution features. (C) Close up of the highest resolved features, with the ability to resolve group 8, element 4 in red box.
In addition to observing performance on axis, the resolution target was translated across the foveated objective in order to assess achievable resolution across the field. The high resolution features of the target were translated and imaged 0.5 mm, 1 mm and 2.5 mm from the axial position (Fig. 5). Testing at a wavelength of 490 nm, the values from Table 2 vary slightly to an expected resolution of 1.53/1.57 μm, 1.62/1.82 μm, and 2.45/6.23 μm at 0.5 mm, 1 mm and 2.5 mm, respectively. As previously mentioned, the two numbers refer to the tangential/sagittal values, which differ due to the elliptical pupil at larger fields. The tangential resolution values correspond to group 8, element 3, group 8 element 2 and group 7, element 5, respectively, which can each be resolved in Fig. 5 (blue boxes). The sagittal values correspond to group 8, element 3, group 8, element 1, and group 6, element 2, which can each also be resolved in Fig. 5 (green boxes).
Fig. 5.

(A) Image of resolution target imaged through the objective after translating the target 0.5 mm from the center of the FOV. The red box indicating the higher resolution features, with blue and green boxes highlighting the expected tangential and sagittal resolvable features (group 8, element 3 for both), respectively. (B) Image of target translated 1 mm from the center, resolving group 8, element 2 and group 8, element 1. (C) Image of target translated 2.5 mm from the center, resolving group 7, element 5 and at least group 6, element 2.
The goal of the foveated objective however is to provide not only high-resolution imaging, but also a large FOV. With the foveated objective relayed onto the 10x, 0.25NA objective, a comparison can be made with a commercial 0.1 NA Olympus objective. The foveated objective is able to collect a FOV comparable to the commercial objective while having a clear aperture several times smaller (Fig. 6).
Fig. 6.

(A) Image taken with 0.1 NA commercial objective of Cartesian grid pattern of dots of 0.0625 mm with a spacing of 0.125 mm between dots. (B) Image of Cartesian pattern taken through the foveated objective with comparable field to the commercial objective.
While the FOV of the commercial objective and the foveated objective are similar in size, the diameter of the commercial objective is 24 mm with a height of 30 mm. Additionally, the clear aperture is 8.5 mm, more than four times larger than the clear aperture of the foveated objective (~2 mm). A comparison of the scale of the objectives can be seen in Fig. 7.
Fig. 7.
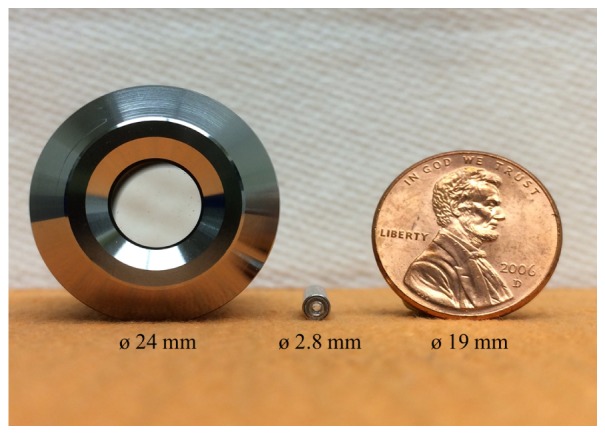
Comparison of the commercial 0.1 NA objective (left) with the foveated objective (center) and penny for scale (right).
In order to effectively utilize the image produced by the foveated objective, it is necessary to remove the distortion. In our previous publication [10], we were able to remove the distortion and unwarp the image using a piecewise polynomial-mapping algorithm written in Python. We have rewritten the algorithm in MATLAB and to provide a more rapid piecewise polynomial-mapping. To remove the distortion, a Cartesian grid pattern printed on a glass slide was used as a calibration target to manually match the points as imaged through the foveated objective. The dots on the grid pattern have diameter of 0.0625 mm with a spacing of 0.125 mm between dots. The algorithm utilizes interpolation of the data points, creating undistorted images with approximately twice as many pixels.
Examples of the original distorted and corrected resolution target as imaged by a custom built confocal microscope can be seen in Fig. 8. The images of the resolution target show the full 5.0 mm field of the endomicroscope.
Fig. 8.
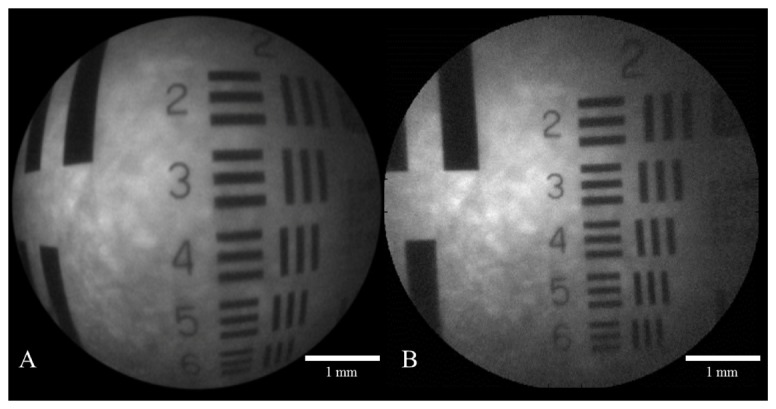
(A) Foveated image of resolution target. (B) Corrected foveated image with distortion removed.
5. Experimental imaging results
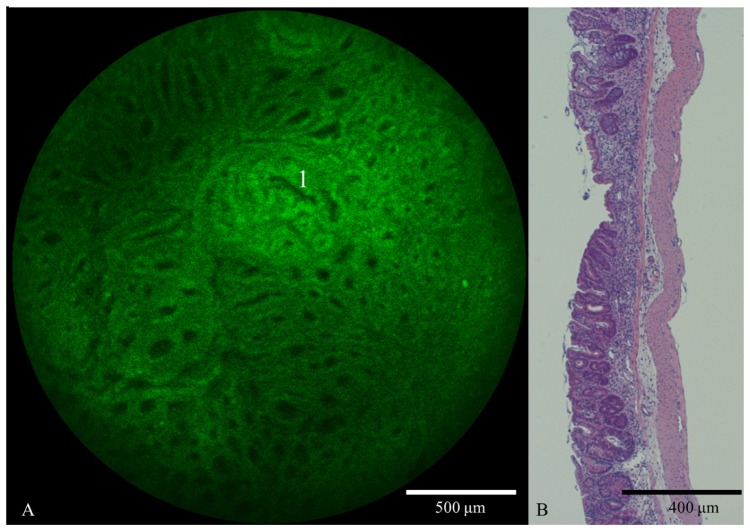
To assess the biological relevance, non-cancerous ex vivo mouse esophageal tissue treated with the proflavine fluorescent dye was imaged with the foveated objective using both a fluorescence microscope and a custom confocal microscope (Fig. 9). In these images, where only the center fields are observed, it is possible to identify individual nuclei due to the proflavine dye, which stains the cell nuclei.
Fig. 9.
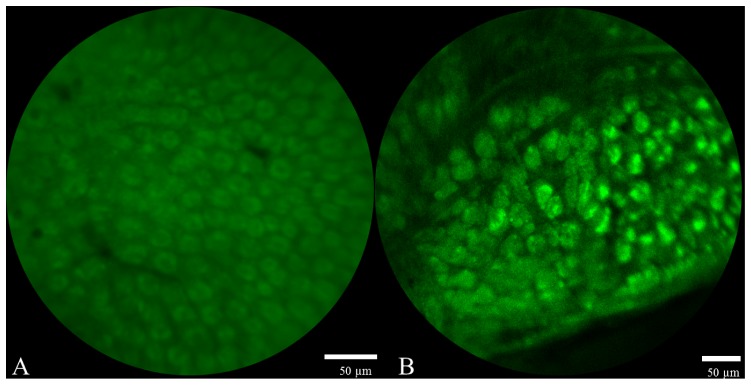
(A) Close up fluorescence image of normal ex vivo mouse esophageal tissue taken through foveated objective. (B) Close up confocal image of ex vivo mouse esophageal tissue dyed with proflavine taken through the foveated objective.
The custom built fluorescence confocal microscope uses a 1W 455nm handheld laser pointer as the light source, miniature scanning galvanometer mirrors, and commercial grade optics to produce a diffraction limited point of excitation light that is scanned across the area of interest and collected by a photomultiplier tube. The light that actually interrogates the sample is only 0.45 mW/cm2 after it is attenuated though the system and foveated objective, well below the acceptable maximum according to the Threshold Limit Value (TLV) set by the American Conference of Governmental Industrial Hygienists (ACGIH) [18]. The entire field could not be imaged with the confocal microscope due to loss of contrast at the edge of the field coinciding with the drop off of numerical aperture. For this reason only the central fields were captured, showing less distortion than the full field of the foveated objective.
Comparisons of the foveated objective with the commercial 0.1 NA objective for imaging esophageal tissue of a larger field were also made (Fig. 10). The FOVs were cropped down slightly to show similar regions of the same tissue.
Fig. 10.

(A) Slightly cropped fluorescence image of normal ex vivo mouse esophageal tissue dyed with proflavine taken through commercial 0.1 NA objective. (B) Same tissue imaged through foveated objective, with high resolution region in the center of the field.
The images show overlapping regions with similar identifiable points of interest. In the foveated image it is possible to identify individual cells on the center of the image with an expected blurring towards the edge of the field as NA and magnification decrease. The ability to observe this cellular structure aids in the localization of abnormal, potentially cancerous regions.
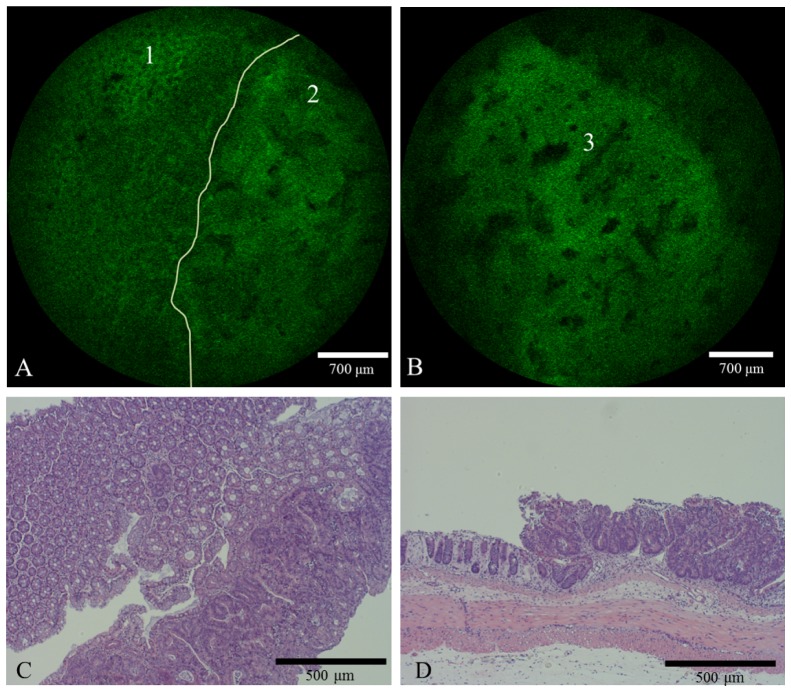
6. Dysplasia identification
The primary benefit of the foveated endomicroscope is providing a large field of view in a small package with sufficient achievable resolution to observe structural changes due to abnormalities. To assess this advantage, a large segment from a mouse colon was imaged with the confocal foveated scope. The colon was chosen because the columnar epithelium of BE segments is similar in appearance and structure to the epithelium of the colon. Additionally the colon of a mouse contains more surface area than the esophagus, allowing for better assessment of the large field of the foveated objective. In order to induce the rapid development of colorectal lesions similar to ones found in humans, mice were exposed to a combination of azoxymethane (AOM) and dextran sodium sulphate (DSS). The AOM/DSS model is well established for observing colon carcinogenesis [19]. In this study, carcinogenesis was induced in male Balb/c mice with an intraperitoneal injection of AOM (10mg/kg) followed by one week cycles of 2% DSS in the drinking water at 1, 4 and 7 weeks. All animal experiments were reviewed and approved by the Institutional Animal Care and Use Committee of Rice University. The development of the cancer begins with appearance of aberrant crypts in the distal end of the colon and eventually the presence of rapidly growing polyps. The latency time for the complete tumors to grow is 2-3 months. Images through the foveated objective were taken at multiple time points. Four weeks after AOM/DSS treatment a mouse was sacrificed and the entire colon was resected, dyed with proflavine and flattened with a cover glass slide. Starting from the anus, the foveated confocal scope was translated across the colon. As previously stated, the entire FOV on the foveated objective was not imaged due to limitations of the confocal scope. A video was recorded of the foveated objective traversing the colon (Media 1 (9.4MB, MOV) ). Figure 11 displays frames taken at several time points showing hair near the anus on the top left down to normal columnar epithelium and eventually an abnormal region with elongated asymmetrical crypt structures found in the bottom right image (white arrow), several millimeters from the anus. At the four week time point, focal high grade tubular adenomas were confirmed with histopathology. The series of images demonstrates the ability of the device to rapidly traverse a large segment to find an abnormal region.
Fig. 11.
Series of confocal images taken through the foveated objective of ex vivo mouse colon 4 weeks after AOM/DSS treatment and dyed with proflavine. The hair in the top left image is the fur near the anus. Normal columnar cells can then be observed in the next images until the bottom right image, where the elongated crypts can be viewed (white arrow). The scale bar is 700 μm. Video of these frames can be found in supplemental information (Media 1 (9.4MB, MOV) ).
Figure 12 is an enlarged version of the bottom right of Fig. 11. Again, in this image it was possible to observe the irregular gland pattern, indicating adenomatous changes, specifically the elongated crypt found at point 1.
Fig. 12.
(A) Slightly zoomed in confocal image taken through the foveated objective of ex vivo mouse colon dyed with proflavine 4 weeks after AOM/DSS treatment. Asymmetrical elongated crypts associated with the beginning of neoplasia can be viewed in this image (Point 1). (B) Hematoxylin and eosin (H&E) stained histology section from a mouse colon exhibiting distorted crypts after undergoing AOM/DSS treatment for 4 weeks.
Ten weeks after treatment, additional mice were sacrificed to observe later stage cancer development. Histopathology confirmed high grade tubular adenomas and focal intramucosal adenocarcinomas present in animals at this timepoint. In the tissue sample, several polypoids are present that can be observed with the device. Images taken with the foveated endomicroscope exhibit an architectural morphology corresponding to this histopathology diagnosis. Of particular interest, the transition from normal, regularly spaced glands to large abnormal cryps associated with adnocarcinoma was captured (Fig. 13).
Fig. 13.
Confocal images taken through the foveated objective of ex vivo mouse colon dyed with proflavine ten weeks after AOM/DSS treatment. (A) The normal region (1) abruptly transitions into the large abnormal crypts associated adenocarcinoma (2) as defined by the added white border. (B) Full field mage of the tumor with crypt observed at point 3. (C) H&E stained histology section from a mouse colon segment transitioning from normal pathology (left) into large abnormal crypts (right) after undergoing AOM/DSS treatment for 10 weeks. (D) Standard H&E stained histology cross section from an area similar to the transition shown in C.
7. Conclusions
Current generation high-definition endoscopes lack the resolving power to identify molecular changes associated with EAC. On the other hand, high-resolution endomicroscopes provide adequate resolution, but a reduced FOV, limiting adoption by clinicians. By mimicking the human eye, the multimodal foveated endomicroscope system combines the lower navigation sampling of a large FOV of 5.0 mm with high resolution in the central portion of the field to observe morphological features. The foveated objective presented in this work is capable of resolving ~3 μm while providing a large FOV on the same scale as a large commercial objective that is four times the size. The large FOV allows for rapid traversing of the large tissue samples in order to quickly locate troubled regions for further analysis, reducing the number of random biopsies. This objective, when combined with a confocal microscope, aids in rapid and reliable EAC detection in both BE and the colon.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute of Biomedical Imaging and Bioengineering under Award Number R21EB015022 and the National Cancer Institute of the National Institutes of Health under Award Number R01CA103830. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References and links
- 1.Mayer R. J., Venook A. P., Schilsky R. L., “Progress against GI cancer during the American Society of Clinical Oncology’s first 50 years,” J. Clin. Oncol. 32(15), 1521–1530 (2014). 10.1200/JCO.2014.55.4121 [DOI] [PubMed] [Google Scholar]
- 2.Pohl H., Sirovich B., Welch H. G., “Esophageal adenocarcinoma incidence: are we reaching the peak?” Cancer Epidemiol. Biomarkers Prev. 19(6), 1468–1470 (2010). 10.1158/1055-9965.EPI-10-0012 [DOI] [PubMed] [Google Scholar]
- 3.Shaheen N. J., “Advances in Barrett’s esophagus and esophageal adenocarcinoma,” Gastroenterology 128(6), 1554–1566 (2005). 10.1053/j.gastro.2005.03.032 [DOI] [PubMed] [Google Scholar]
- 4.Falk G. W., “Risk factors for esophageal cancer development,” Surg. Oncol. Clin. N. Am. 18(3), 469–485 (2009). 10.1016/j.soc.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 5.Hvid-Jensen F., Pedersen L., Drewes A. M., Sørensen H. T., Funch-Jensen P., “Incidence of adenocarcinoma among patients with Barrett’s esophagus,” N. Engl. J. Med. 365(15), 1375–1383 (2011). 10.1056/NEJMoa1103042 [DOI] [PubMed] [Google Scholar]
- 6.Kariv R., Plesec T. P., Goldblum J. R., Bronner M., Oldenburgh M., Rice T. W., Falk G. W., “The Seattle protocol does not more reliably predict the detection of cancer at the time of esophagectomy than a less intensive surveillance protocol,” Clin. Gastroenterol. Hepatol. 7(6), 653–658 (2009). 10.1016/j.cgh.2008.11.024 [DOI] [PubMed] [Google Scholar]
- 7.R. Shukla, “Endoscopic imaging: How far are we from real-time histology?,” WJGE 3(10), 183 Baishideng Publishing Group Co., Ltd. (2011). [DOI] [PMC free article] [PubMed]
- 8.Haidry R., Lovat L., Medical Imaging in Clinical Practice, Erondu O. F., ed. (InTech, 2013), Chap. 7. [Google Scholar]
- 9.Sharma P., Hawes R. H., Bansal A., Gupta N., Curvers W., Rastogi A., Singh M., Hall M., Mathur S. C., Wani S. B., Hoffman B., Gaddam S., Fockens P., Bergman J. J., “Standard endoscopy with random biopsies versus narrow band imaging targeted biopsies in Barrett’s oesophagus: a prospective, international, randomised controlled trial,” Gut 62(1), 15–21 (2013). 10.1136/gutjnl-2011-300962 [DOI] [PubMed] [Google Scholar]
- 10.Hagen N., Tkaczyk T. S., “Foveated endoscopic lens,” J. Biomed. Opt. 17(2), 021104 (2012). 10.1117/1.JBO.17.2.021104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van der Spiegel J., Kreider G., Claeys C., Debusschere I., Sandini G., Dario P., Fantini F., Bellutti P., Soncini G., The Kluwer International Series in Engineering and Computer Science, Allen J., Mead C., Ismail M., Eds. (Springer, (1989), Chapt. 8, pp. 189–211. [Google Scholar]
- 12.McCarley P. L., Massie M. A., Curzan J. P., “Infrared Systems and Photoelectronic Technology II,” in Photonic Devices + Applications 6660, Longshore R. E., Sood A. K., Dereniak E. L., Hartke J. P., eds. (SPIE, 2007) pp. 666002. [Google Scholar]
- 13.Hua H., Liu S., “Dual-sensor foveated imaging system,” Appl. Opt. 47(3), 317–327 (2008). 10.1364/AO.47.000317 [DOI] [PubMed] [Google Scholar]
- 14.Qin Y., Hua H., Nguyen M., “Characterization and in-vivo evaluation of a multi-resolution foveated laparoscope for minimally invasive surgery,” Biomed. Opt. Express 5(8), 2548–2562 (2014). 10.1364/BOE.5.002548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.S. Shimizu, Y. Suematsu, and S. Yahata, “Proceedings of the 1996 IEEE IECON. 22nd International Conference on Industrial Electronics, Control, and Instrumentation,” in IECON-96 3, pp. 1600–1605, IEEE. [Google Scholar]
- 16.Wakamiya K., Senga T., Isagi K., Yamamura N., Ushio Y., Kita N., “Optomechatronic machine vision,” in Optomechatronic Technologies 2005 6051, Sumi K., Ed. (SPIE, 2005), p. 605107. [Google Scholar]
- 17.Tzannes A. P., Mooney J. M., “Measurement of the modulation transfer function of infrared cameras,” Opt. Eng. 34(6), 1808 (1995). 10.1117/12.203133 [DOI] [Google Scholar]
- 18.Acgih, TLVs and BEIs (American Conference of Governmental Industrial Hygenists 2010), p. 254.
- 19.De Robertis M., Massi E., Poeta M. L., Carotti S., Morini S., Cecchetelli L., Signori E., Fazio V. M., “The AOM/DSS murine model for the study of colon carcinogenesis: from pathways to diagnosis and therapy studies,” J. Carcinog. 10(1), 9 (2011). 10.4103/1477-3163.78279 [DOI] [PMC free article] [PubMed] [Google Scholar]