Abstract
Background.
A decline in prevalence of late-life disability in activities of daily living (ADLs) has been reported in Western countries. We investigate the time trend of disability in basic ADLs among Chinese older people in 1997–2006, and explore the potential contribution of cardiometabolic diseases to the trend.
Methods.
The study included 7,845 participants (age ≥ 60 years) in the China Health and Nutrition Survey who were examined in 1997, 2000, 2004, and 2006. Data on ADLs were collected through interviews. Disability in basic ADLs was defined as need of assistance or inability to perform at least one of the five self-care activities of bathing, dressing, toileting, feeding, and transferring. Generalized estimating equation models were used to test the time trend in ADL disability and its association with cardiometabolic diseases.
Results.
Prevalence of ADL disability decreased from 13.2% in 1997 to 9.9% in 2006; the trend was statistically evident among people aged 60–69 years, women, and rural residents (p trend < .05). From 1997 to 2006, the prevalence of ADL disability decreased at a relative annual rate of 3.1% in total sample; the decline was statistically more evident in young-olds than older-olds, in men than women, and in rural than urban residents. The disabling effect decreased over time for stroke (p trend = .032) and multiple cardiometabolic diseases (p trend = .014).
Conclusions.
The prevalence of disability in basic ADLs among Chinese older adults decreased from 1997 to 2006. Stroke and multiple cardiometabolic diseases appear to become less disabling over time, which may partly contribute to the favorable trend in ADL disability.
Key Words: Activities of daily living, Disability, Secular trends, Aging, China.
China has experienced an accelerated demographic transition since the late 1970s when the nation implemented one-child policy (1). As a result, the proportion of older people (age ≥ 60 years) increased substantially from 8.0% in 1990 to 13.3% in 2010 (2). Physical functioning deteriorates progressively as people age (3). Indeed, the prevalence of disability in basic activities of daily living (ADLs), such as eating, dressing, toileting, and bathing, increases with advancing age (4). Functional dependence in basic ADLs confers a substantial risk of institutionalization and poor quality of life (5), which significantly increases the need for and costs of long-term care and social services.
The time trend of late-life disability has been frequently reported in Western countries. In the United States, the prevalence of disability or functional limitation in old age substantially declined from the 1980s through the late 1990s (6), although the declining trends might have ended since the 2000s (7). In European countries, reports on the secular trends of functional disability among older people have not been consistent in the last three decades (8–10). In Mainland China, studies on the trends in ADL disability among older people also have reported mixed results in the last two decades: one study showed a decreasing trend from 1998 to 2008 (11), whereas another study found no clear trend from 1992 to 2002 (12). However, some methodological variations (eg, use of various scales for assessing physical functioning) might hamper direct comparisons across studies. Moreover, the time trend was determined based on assessments at only two or three time points in some earlier studies (11,12).
In addition, earlier studies have shown that late-life disability in basic ADLs is associated with unhealthy lifestyles (13), metabolic syndrome (14), chronic diseases (15,16), and comorbidity (17). Thus, changes in unhealthy lifestyles and chronic health conditions may affect the time trends of late-life ADL disability (9,18). However, very few studies have investigated whether, and to what extent, changes in these possible determinants of ADL disability may contribute to the trend of late-life functional disability.
Given the facts that the Chinese population is aging rapidly and that late-life functional disability causes tremendous economic and societal burden, information on the secular trend in basic ADL disability and its potential determinants is critically relevant for policymakers. In the current analysis, using data from the China health and nutrition survey, we seek to investigate the secular trends in prevalence of functional dependence in basic ADLs among Chinese older adults, and further to explore the potential contribution of major cardiometabolic diseases to the trends in ADL disability.
Methods
Study Design and Population
China health and nutrition survey is a nationwide longitudinal survey on health risk factors, nutritional status, and health outcomes in Chinese populations, as fully described elsewhere (19). Briefly, the China health and nutrition survey was conducted in 1989, 1991, 1993, 1997, 2000, 2004, 2006, 2009, and 2011. Data on ADLs were collected only in surveys from 1993 to 2006, mostly on people aged ≥55 years. We excluded data from the survey in 1993 because a considerable proportion of participants had missing information on ADLs. Thus, this analysis included 7,845 subjects who were aged ≥60 years and who participated in the surveys in 1997 (n = 1,668), 2000 (n = 1,671), 2004 (n = 2,154), or 2006 (n = 2,352). Following the survey in 1997, members from newly formed households who resided in the same sample areas, replacement households or replacement communities were added to the sample of subsequent surveys. Owing to this sampling strategy, 34.7%, 30.5%, 19.1%, and 15.7% participated in 1, 2, 3, and all 4 waves of the survey, respectively.
The survey protocols, instruments, and the process for obtaining the informed consent for China health and nutrition survey participants were approved by the Institutional Review Committees of the University of North Carolina at Chapel Hill, North Carolina, United States, and the China National Institute of Nutrition and Food Safety at the Chinese Center for Disease Control and Prevention, Beijing, China. All participants provided written informed consents prior to the surveys.
Data Collection and Definitions
Data on demographics (age, sex, education, and living area), lifestyles (ever smoking and alcohol intake), height, weight, and blood pressure, and use of medications were collected by trained and certified health professionals through interviews and physical examinations (19). Ever smoking was defined as a positive answer to the question “have you ever smoked cigarettes or pipe?” Alcohol intake was defined as regular drinking alcoholic beverage ≥3 times a week (20). Body mass index was calculated as measured weight (kg) divided by height (m) squared. Obesity was defined as body mass index ≥28kg/m2, a cut-off proposed specifically for Chinese adults (21). Hypertension was defined as systolic pressure ≥140 mmHg, or diastolic pressure ≥ 90 mmHg, or currently using antihypertensive medications (22). Diabetes, myocardial infarction, and stroke were defined according to the self-report history of a physician diagnosis. The aggregation of four cardiometabolic diseases (ie, hypertension, diabetes, myocardial infarction, and stroke) was categorized as having none, a single or multiple (≥2) cardiometabolic diseases.
Basic ADLs were measured according to self-reported responses to questions that involved five activities of self-care tasks, that is, bathing, dressing, toileting, feeding, and transferring (standing up from long-term sitting). There were four choices for each activity: “no difficulties,” “has some difficulties but still can do without help,” “need help,” and “unable to do.” Disability in basic ADL was defined as giving the answer of “need help” or “unable to do” in at least one of the five activities.
Statistical Analysis
Trends in the characteristics of participants and in the prevalence of ADL disability over time were assessed by using a multiple generalized estimating equation regression model to address the correlation of repeated measures within individuals. Odds ratio and 95% confidence interval of ADL disability were estimated in each of the surveys in 2000, 2004, and 2006 in comparison with that in 1997. The relative annual changes in the prevalence of ADL disability from 1997 to 2006 were also estimated using generalized estimating equation models, in which ADL disability was considered as a dependent variable and the interval (years) from 1997 to the subsequent survey years as an independent variable. The association of ADL disability with individual and multiple (≥2) cardiometabolic diseases in each survey was examined using logistic regression models controlling for demographics, lifestyle factors, and other cardiometabolic diseases. The time trend in the strength of associations between ADL disability and cardiometabolic diseases across surveys was examined by using multiple generalized estimating equation regression analysis with the interaction term of ADL disability and chronic disease in the models.
IBM SPSS Statistics 22 for Windows (IBM SPSS Inc., Chicago, Illinois, United States) was used for all analyses.
Results
Characteristics of Study Participants
Table 1 shows the characteristics of participants by four waves of the survey. The mean age of participants increased from 69.1 (standard deviation, 6.9) years in 1997 to 69.7 (7.0) years in 2006 (p trend = .005). From 1997 to 2006, the proportion of participants aged 70–79 or ≥80 years significantly increased (p trend = .004), more subjects were living in the rural area (p trend = .002) and highly educated (p trend < .001), and the prevalence significantly increased for smoking (p trend < .001) and decreased for hypertension (p trend = .020). There was no significant difference in the distributions of sex, alcohol intake, obesity, diabetes, myocardial infarction, stroke, and multiple cardiometabolic diseases across surveys (Table 1).
Table 1.
Characteristics of Participants in the Surveys in 1997, 2000, 2004, and 2006
| Characteristics* | 1997 (n = 1,668) | 2000 (n = 1,671) | 2004 (n = 2,154) | 2006 (n = 2,352) | p trend † |
|---|---|---|---|---|---|
| Age (years), mean (SD) | 69.1 (6.9) | 69.2 (6.7) | 69.6 (6.8) | 69.7 (7.0) | .005 |
| Age (years), n (%) | |||||
| 60–69 | 1,033 (61.9) | 1,003 (60.0) | 1,242 (57.7) | 1,341 (57.0) | |
| 70–79 | 488 (29.3) | 536 (32.1) | 730 (33.9) | 799 (34.0) | |
| ≥80 | 147 (8.8) | 132 (7.9) | 182 (8.4) | 212 (9.0) | .004 |
| Women, n (%) | 906 (54.3) | 904 (54.1) | 1,144 (53.1) | 1,249 (53.1) | .287 |
| Rural residents, n (%) | 995 (59.7) | 1,004 (60.1) | 1,335 (62.0) | 1,488 (63.3) | .002 |
| Education, n (%) | |||||
| No formal school | 1,098 (71.0) | 961 (62.4) | 1,102 (51.4) | 1,279 (54.6) | |
| Primary school | 229 (14.8) | 284 (18.4) | 519 (24.2) | 442 (18.9) | |
| Middle school or above | 220 (14.2) | 296 (19.2) | 525 (24.5) | 623 (26.6) | <.001 |
| Ever smoking, n (%) | 478 (28.8) | 478 (28.7) | 711 (33.1) | 766 (32.6) | <.001 |
| Alcohol intake, n (%) | 256 (15.7) | 295 (18.2) | 359 (16.7) | 373 (15.9) | .931 |
| Obesity, n (%) | 127 (8.6) | 148 (9.1) | 208 (10.2) | 214 (9.7) | .356 |
| Hypertension, n (%) | 735 (49.1) | 789 (48.1) | 995 (48.0) | 1,023 (45.3) | .020 |
| Diabetes, n (%) | 53 (3.2) | 68 (4.3) | 79 (3.7) | 90 (3.9) | .979 |
| Myocardial infarction, n (%) | 19 (1.2) | 27 (1.6) | 25 (1.2) | 43 (1.8) | .171 |
| Stroke, n (%) | 45 (2.8) | 51 (3.2) | 93 (4.3) | 76 (3.3) | .246 |
| Number of cardiometabolic diseases, n (%) | |||||
| 0 | 892 (53.5) | 843 (50.4) | 1,104 (51.3) | 1,261 (53.6) | |
| 1 | 707 (42.4) | 732 (43.8) | 923 (42.9) | 960 (40.8) | |
| ≥2 (multiple) | 69 (4.1) | 96 (5.7) | 127 (5.9) | 131 (5.6) | .810 |
Notes: *The number of subjects with missing values was 267 for education, 20 for smoking, 90 for alcohol intake, 516 for body mass index, 377 for hypertension, 155 for diabetes, 73 for myocardial infarction, and 137 for stroke. When these factors were considered as covariates in subsequent analyses, a dummy variable for each of these factors was created to represent the group of subjects with the missing value.
†The linear trend was tested using generalized estimation equations regression models, if applicable, controlling for age, sex, education, and living region.
Secular Trend in Prevalence of ADL Disability
Overall, the prevalence of disability in basic ADLs significantly decreased from 13.2% in 1997 to 9.9% in 2006 in the total sample (unadjusted p trend = .001), and in all subgroups by age, sex, and living regions (unadjusted p trend ≤ .05) (Figure 1).
Figure 1.
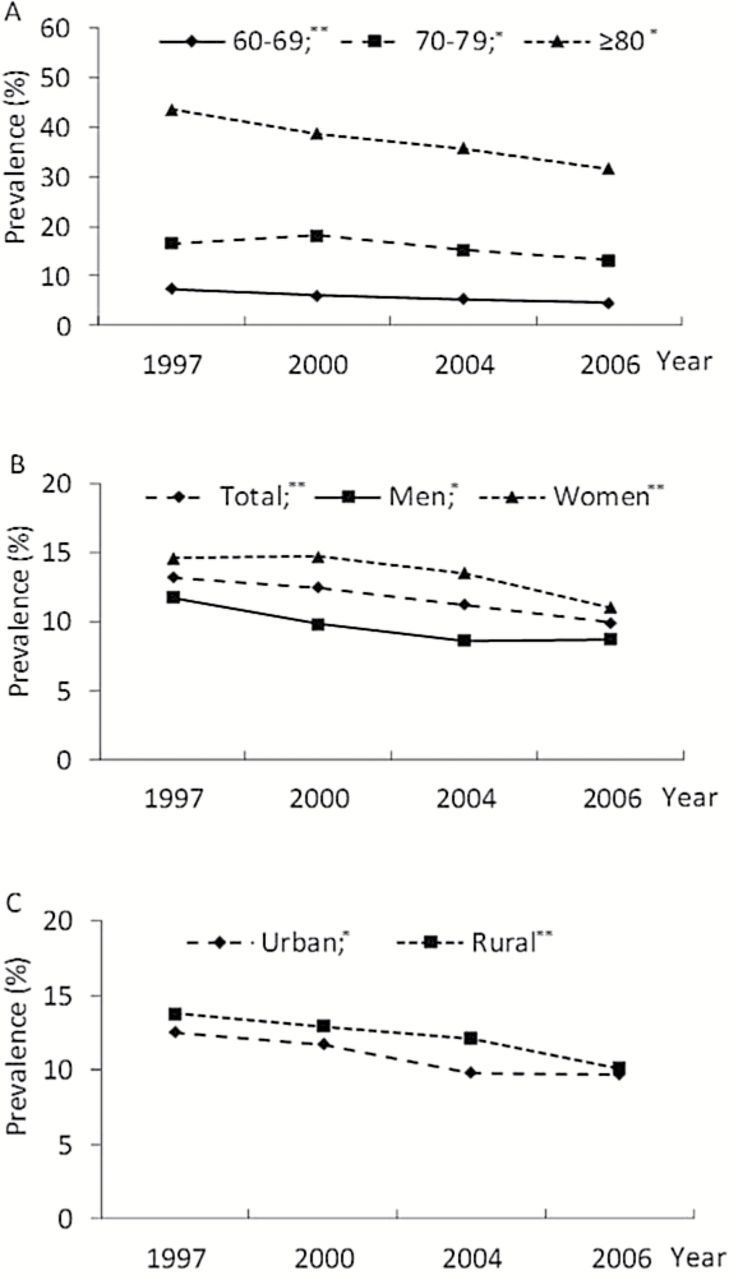
Prevalence of disability in basic activities of daily living over time in 1997, 2000, 2004, and 2006, by age groups (A), sex (B), and living regions (C). *p trend < .05; **p trend < .01. The prevalence of disability in basic activities of daily living significantly decreased from 1997 to 2006: p trend < .01 for the total sample, for people aged 60–69 years, for women, and for rural residents; p trend ≤ .05 for people aged 70–79 years and ≥80 years, for men, and for urban residents.
After controlling for age, sex, living region, education, ever smoking, alcohol intake, obesity, and cardiometabolic diseases, a decrease in the prevalence of ADL disability remained statistically significant in the total sample (p trend = .005), whereas the stratified analysis showed that the prevalence of ADL disability significantly decreased among people aged 60–69 years (p trend = .036), women (p trend = .047), and rural residents (p trend = .019), and marginally decreased in men (p trend = .059) (Table 2).
Table 2.
Trends in the Likelihood of Disability in Basic Activities of Daily Living, 1997–2006: the China Health and Nutrition Survey
| 1997 | 2000 | 2004 | 2006 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | n/N | OR* | n/N | OR (95% CI)† | n/N | OR (95% CI)† | n/N | OR (95% CI)† | p trend † |
| Total | 221/1,668 | 1.00 | 208/1,671 | 1.05 (0.85–1.29) | 242/2,154 | 0.90 (0.73–1.12) | 234/2,352 | 0.76 (0.61–0.94) | .005 |
| Age, years | |||||||||
| 60–69 | 76/1,033 | 1.00 | 60/1,003 | 0.90 (0.64–1.28) | 66/1,242 | 0.79 (0.55–1.14) | 62/1,341 | 0.69 (0.48–0.99) | .036 |
| 70–79 | 81/488 | 1.00 | 97/536 | 1.25 (0.90–1.74) | 111/730 | 1.00 (0.71–1.39) | 105/799 | 0.85 (0.61–1.19) | .143 |
| ≥80 | 64/147 | 1.00 | 51/132 | 1.02 (0.62–1.67) | 65/182 | 0.97 (0.59–1.59) | 67/212 | 0.76 (0.47–1.22) | .230 |
| Sex | |||||||||
| Men | 89/762 | 1.00 | 75/767 | 0.88 (0.62–1.25) | 87/1,010 | 0.74 (0.53–1.04) | 96/1,103 | 0.74 (0.53–1.04) | .059 |
| Women | 132/906 | 1.00 | 133/904 | 1.18 (0.90–1.55) | 155/1,144 | 1.05 (0.79–1.39) | 138/1,249 | 0.79 (0.60–1.05) | .047 |
| Region | |||||||||
| Urban | 84/673 | 1.00 | 78/667 | 1.05 (0.75–1.48) | 80/819 | 0.83 (0.58–1.20) | 84/864 | 0.82 (0.57–1.17) | .174 |
| Rural | 137/995 | 1.00 | 130/1,004 | 1.07 (0.81–1.41) | 162/1,335 | 0.96 (0.73–1.26) | 150/1,488 | 0.75 (0.58–0.98) | .019 |
Notes: CI = confidence interval; OR = odds ratio.
*Referent.
†Controlling for age, sex, education, living region, ever smoking, alcohol intake, obesity, hypertension, diabetes, myocardial infarction, and stroke.
Relative Annual Changes in Prevalence of ADL Disability
In the univariate model (Table 3, model 1), the relative average annual decrease in the prevalence of basic ADL disability was 3.4% in the total sample. After controlling for demographics, lifestyle factors, metabolic factors, and cardiometabolic diseases, the relative average annual decrease in the prevalence of ADL disability was 3.1% (Table 3, model 4). In the multiple logistic model, the annual decrease was statistically significant in people aged 60–69 years (4.0%, 95% confidence interval = 0.2–7.7), in men (3.5%, 95% confidence interval = 0–7.0), and in rural residents (3.0%, 95% confidence interval = 0.3–5.7) (Table 3, model 4).
Table 3.
Average Annual Changes (95% Confidence Interval) in the Prevalence of Disability in Basic Activities of Daily Living, 1997–2006: the China Health and Nutrition Survey
| Average Annual Change (95% Confidence Interval), % | ||||
|---|---|---|---|---|
| Characteristics | Model 1* | Model 2* | Model 3* | Model 4* |
| Total | −3.4 (−5.4, −1.5) | −3.7 (−5.9, −1.6) | −3.2 (−5.4, −1.1) | −3.1 (−5.2, −0.9) |
| Age, years | ||||
| 60–69 | −5.1 (−8.7, −1.6) | −4.9 (−8.5, −1.2) | −4.1 (−7.8, −0.4) | −4.0 (−7.7, −0.2) |
| 70–79 | −3.4 (−6.5, −0.3) | −2.7 (−6.0, 0.6) | −2.5 (−5.8, 0.8) | −2.4 (−5.8, 0.9) |
| ≥80 | −5.3 (−10.0, −0.6) | −3.7 (−8.5, 1.1) | −3.2 (−8.1, 1.7) | −2.8 (−7.8, 2.2) |
| Sex | ||||
| Men | −3.7 (−7.0, −0.4) | −3.8 (−7.2, −0.3) | −3.0 (−6.5, 0.5) | −3.5 (−7.0, 0.0) |
| Women | −3.2 (−5.7, −0.7) | −3.6 (−6.3, −0.9) | −3.3 (−6.0, −0.5) | −2.6 (−5.4, 0.2) |
| Region | ||||
| Urban | −3.4 (−6.8, −0.1) | −3.2 (−6.8, 0.4) | −2.6 (−6.3, 1.0) | −2.7 (−6.5, 1.1) |
| Rural | −3.5 (−6.0, −1.1) | −3.9 (−6.6, −1.3) | −3.5 (−6.1, −0.8) | −3.0 (−5.7, −0.3) |
Note: *Model 1 was univariate; Model 2 was controlled for age, sex, education, and living region; model 3 was additionally controlled for lifestyle factors (ever smoking and alcohol intake); and model 4 was further controlled for metabolic risk factors and cardiometabolic diseases (obesity, hypertension, diabetes, myocardial infarction, and stroke).
Time Trend in the Association Between Cardiometabolic Diseases and ADL Disability
After controlling for multiple potential confounders, stroke and multiple cardiometabolic diseases were significantly associated with an increased likelihood of ADL disability in all four surveys, whereas hypertension was also significantly associated with an increased likelihood of ADL disability in the surveys in 1997 and 2006 (Table 4). There was a significant decrease in the strengths of associations of ADL disability with stroke (p trend = .032) and multiple cardiometabolic diseases (p trend = .014) from 1997 to 2006.
Table 4.
Trends in the Associations between Cardiometabolic Diseases and Disability in Basic Activities of Daily Living, 1997–2006: the China Health and Nutrition Survey
| Cardiometabolic Diseases | 1997 (n = 1,668) | 2000 (n = 1,671) | 2004 (n = 2,154) | 2006 (n = 2,352) | |||||
|---|---|---|---|---|---|---|---|---|---|
| n/N | OR (95% CI)* | n/N | OR (95% CI)* | n/N | OR (95% CI)* | n/N | OR (95% CI)* | p trend* | |
| Hypertension | 115/735 | 1.43 (1.00–2.05) | 109/789 | 1.03 (0.73–1.44) | 123/995 | 1.17 (0.85–1.61) | 122/1,023 | 1.39 (1.01–1.92) | .870 |
| Diabetes | 13/53 | 1.75 (0.83–3.69) | 15/68 | 1.35 (0.63–2.91) | 10/79 | 1.28 (0.61–2.72) | 11/90 | 1.24 (0.60–2.53) | .492 |
| Myocardial infarction | 4/19 | 1.52 (0.44–5.31) | 7/27 | 1.79 (0.62–5.17) | 3/25 | 0.47 (0.12–1.83) | 8/43 | 1.85 (0.79–4.34) | .779 |
| Stroke | 31/45 | 14.0 (6.92–28.4) | 34/51 | 18.5 (9.32–36.9) | 40/93 | 7.68 (4.55–13.0) | 32/76 | 7.05 (4.02–12.4) | .032 |
| Number of diseases | |||||||||
| 0 | 92/892 | 1.00 (reference) | 86/843 | 1.00 (reference) | 105/1,104 | 1.00 (reference) | 92/1,261 | 1.00 (reference) | — |
| 1 | 100/707 | 1.59 (1.12–2.24) | 85/732 | 1.10 (0.78–1.55) | 102/923 | 1.25 (0.91–1.71) | 114/960 | 1.83 (1.33–2.51) | .868 |
| ≥2 (multiple) | 29/69 | 8.57 (4.74–15.5) | 37/96 | 6.24 (3.69–10.6) | 35/127 | 4.11 (2.49–6.79) | 28/131 | 4.38 (2.59–7.39) | .014 |
Notes: CI = confidence interval; OR = odds ratio.
*Controlling for age, sex, education, living region, ever smoking, alcohol intake, obesity, and cardiometabolic diseases listed in the table.
Discussion
The nationwide survey provides evidence that the prevalence of disability in basic ADLs among Chinese older adults decreased from 1997 to 2006. After controlling for possible confounders, the prevalence of ADL disability decreased at a relative rate of 3.1% per annum in the total sample; the decline was more evident in the young-olds than the older-olds, in men than women, and in rural than urban residents. Stroke and multiple cardiometabolic diseases appear to become less disabling over time, which may partly contribute to the favorable trends in ADL disability.
The findings of a decline in prevalence of basic ADL disability from the 1990s to 2000s are consistent with the report from the Shanghai study (11). However, the Shanghai study showed that the trend of improvement in ADL function appeared to be accounted for by the competing health conditions such as comorbidities, depressive symptoms, and cognitive impairment. By contrast, our results indicated that the decreasing trend was present independent of demographic features, lifestyle factors, and cardiometabolic diseases. Unfortunately, we are not able to control for cognitive impairment and depressive symptoms because these data are not available. The favorable trend of disability in basic ADLs implies that the person-years of good function in self-care activities among older people may have increased over time; if this trend continues, the future burden of long-term care and social services for older people owing to functional dependence might be less worrisome than what was previously projected on the basis of relatively stable prevalence of functional disability (23).
The decline in crude prevalence of ADL disability seemed to be more impressive in the oldest-old group (≥80 years) than other two age groups (60–69 and 70–79 years) (Figure 1). This is relevant given that the oldest-old group is the fastest growing segment in population aging. The crude rates reflect the real burden of disability in the society, which has significant implications for policymakers (24). However, the young-old people (60–69 years) seemed to have more improvement in ADL disability over time than the older-olds after demographics, lifestyles, and cardiometabolic diseases were taken into consideration, suggesting that these factors could explain more decline in ADL disability among the oldest-old than the young-old group. The finding of a more decline in ADL disability in rural than urban residents from our study is consistent with the Shanghai study (11). It is possible that the new Rural Co-operative Medical Care System that started from the year of 2000 in rural areas in China may help older rural residents improve medical services and their overall health condition and functional ability as well (25).
Cardiometabolic diseases, especially stroke, are known to substantially contribute to disability (15). Previous studies have suggested either a stable or a decreasing trend in the disabling effects of chronic diseases such as stroke, heart disease, cancer, and multimorbidity (9,26). The time trend in ADL disability might be partly explained by the trend of disabling effect of certain cardiometabolic diseases over time. We found that the strength of association between stroke and ADL disability decreased over time, which is in accordance with a report from the Netherlands (9). This finding may be relevant given that stroke is the leading contributor to disability-adjusted life-years in China (27). From a public health perspective, however, the significance of this finding should not be over-stated because of the relatively small numbers of patients with stroke in this study. Similarly, multiple cardiometabolic diseases also appeared to become less disabling over time. Again, although multiple cardiometabolic diseases become increasingly common as people age, the overall prevalence of the condition in our population was only about 4%–6%. Thus, the decline in population attributable risk of ADL disability owing to changes in disabling effect of stroke or multiple cardiometabolic diseases is likely to be limited.
However, the exact reasons for the favorable trend of late-life ADL disability are not fully understood. The increase in educational achievements over time may contribute to the favorable trends in disability because research has shown that early life higher education is consistently associated with better cognitive and physical function in late life (6). However, the trend of ADL disability was present independent of demographic factors, lifestyles, metabolic risk factors, and cardiometabolic diseases. Moreover, the ability to perform the basic ADLs depends on the gap between personal capacity and actual environment (28). Thus, the continuous development of new assistive devices and improvements of accommodations over time also may contribute to the declining prevalence of late-life disability in basic ADLs (29). This deserves further investigation.
This study is based on a large nationwide sample in China that covers a wide range of demographic features, socioeconomic status, nutritional status, and health conditions (19). Furthermore, the ADL scale was consistently used across different surveys. However, this study also has limitations. First, data on lifestyle factors and cardiometabolic diseases were from self-reports and not verified independently, which might lead to underestimation of the true prevalence of certain cardiometabolic diseases such as diabetes and stroke. Second, the statistical power was limited for some cardiometabolic diseases (eg, diabetes and myocardial infarction) when examining their associations with disability as well as the trend in the strengths of their associations with disability over time. Finally, although a broad range of potential confounding factors were included in the analysis, certain relevant factors such as cognitive impairment and depressive symptoms were still missed.
In conclusion, data from the nationwide surveys suggest that the prevalence of functional disability in basic ADLs decreased from 1997 to 2006 among Chinese older adults. Furthermore, this study provides evidence suggesting that some cardiometabolic diseases may have been less disabling over time. Given the significant implications of the temporal trend in late-life ADL disability for public health and health care service systems of the aging society, further confirmation of these findings is warranted.
Funding
The work was supported by the National Institute of Nutrition and Food Safety at the Chinese Center for Disease Control and Prevention, Carolina Population Center (5 R24 HD050924), the University of North Carolina at Chapel Hill, the National Institutes of Health (NIH) (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the Fogarty International Center, NIH. Dr. Qiu received grants from the Swedish Research Council (no. K2012-99X-2167-01-3), the Swedish Research Council for Health, Working Life and Welfare (no. 2014-1382), and Karolinska Institutet (2011 and 2013 KID Faculty Funds), Stockholm, Sweden. None of the study sponsors or funding sources had a role in the design, conduct, analysis or reporting of the study. Researchers are independent from funders.
Conflict of Interest
Authors report no conflict of interest.
References
- 1. Peng X. China’s demographic history and future challenges. Science. 2011;333:581–587. :10.1126/science.1209396 [DOI] [PubMed] [Google Scholar]
- 2. National Bureau of Statistics of the People’s Republic of China. China’s National Population Census http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/ Accessed February 18, 2014.
- 3. Diehr PH, Thielke SM, Newman AB, Hirsch C, Tracy R. Decline in health for older adults: five-year change in 13 key measures of standardized health. J Gerontol A Biol Sci Med Sci. 2013;68:1059–1067. :10.1093/gerona/glt038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ostchega Y, Harris TB, Hirsch R, Parsons VL, Kington R. The prevalence of functional limitations and disability in older persons in the US: data from the National Health and Nutrition Examination Survey III. J Am Geriatr Soc. 2000;48:1132–1135. [DOI] [PubMed] [Google Scholar]
- 5. Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304:1919–1928. :10.1001/jama.2010.1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–3146. :10.1001/jama.288.24.3137 [DOI] [PubMed] [Google Scholar]
- 7. Lin SF, Beck AN, Finch BK, Hummer RA, Masters RK, Master RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. 2012;102:2157–2163. :10.2105/AJPH.2011.300602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208. :10.1016/S0140-6736(09)61460-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hoeymans N, Wong A, van Gool CH, et al. The disabling effect of diseases: a study on trends in diseases, activity limitations, and their interrelationships. Am J Public Health. 2012;102:163–170. :10.2105/AJPH.2011.300296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sjölund BM, Wimo A, Qiu C, Engström M, von Strauss E. Time trends in prevalence of activities of daily living (ADL) disability and survival: comparing two populations (aged 78+ years) living in a rural area in Sweden. Arch Gerontol Geriatr. 2014;58:370–375. :10.1016/j.archger.2013.12.004 [DOI] [PubMed] [Google Scholar]
- 11. Feng Q, Zhen Z, Gu D, Wu B, Duncan PW, Purser JL. Trends in ADL and IADL disability in community-dwelling older adults in Shanghai, China, 1998-2008. J Gerontol B Psychol Sci Soc Sci. 2013;68:476–485. :10.1093/geronb/gbt012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gu D, Dupre ME, Warner DF, Zeng Y. Changing health status and health expectancies among older adults in China: gender differences from 1992 to 2002. Soc Sci Med. 2009;68:2170–2179. :10.1016/j.socscimed.2009.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Artaud F, Dugravot A, Sabia S, Singh-Manoux A, Tzourio C, Elbaz A. Unhealthy behaviours and disability in older adults: three-City Dijon cohort study. BMJ. 2013;347:f4240. :10.1136/bmj.f4240 [DOI] [PubMed] [Google Scholar]
- 14. Carriere I, Pérès K, Ancelin ML, et al. Metabolic syndrome and disability: findings from the prospective three-city study. J Gerontol A Biol Sci Med Sci. 2014;69:79–86. :10.1093/gerona/glt101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sousa RM, Ferri CP, Acosta D, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374:1821–1830. :10.1016/S0140-6736(09)61829-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Andersen MM, Kritchevsky SB, Morgan TM, et al. Increased cardiovascular stiffness and impaired age-related functional status. J Gerontol A Biol Sci Med Sci. 2014. 10.1093/gerona/glu085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stenholm S, Westerlund H, Head J, et al. Comorbidity and functional trajectories from midlife to old age: The Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2014. 10.1093/gerona/glu113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jagger C, Matthews R, Lindesay J, Robinson T, Croft P, Brayne C. The effect of dementia trends and treatments on longevity and disability: a simulation model based on the MRC Cognitive Function and Ageing Study (MRC CFAS). Age Ageing. 2009;38:319–325. :10.1093/ageing/afp016 [DOI] [PubMed] [Google Scholar]
- 19. Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China Health and Nutrition Survey–monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39:1435–1440. :10.1093/ije/dyp322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Batis C, Gordon-Larsen P, Cole SR, Du S, Zhang B, Popkin B. Sodium intake from various time frames and incident hypertension among Chinese adults. Epidemiology. 2013;24:410–418. :10.1097/EDE.0b013e318289e047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. [PubMed] [Google Scholar]
- 22. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 23. Christensen K, Thinggaard M, Oksuzyan A, et al. Physical and cognitive functioning of people older than 90 years: comparison of two Danish cohorts born 10 years apart. Lancet. 2013;382:1507–1513. :10.1016/S0140-6736(13)60777-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, Minkler M. Unadjusted prevalence rates: why they still matter for older adults’ disability rates. J Gerontol A Biol Sci Med Sci. 2010;65:545–546. :10.1093/gerona/glq031 [DOI] [PubMed] [Google Scholar]
- 25. Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: An impact evaluation of China’s new cooperative medical scheme. J Health Econ. 2009;28:1–19. :10.1016/j.jhealeco.2008.10.007 [DOI] [PubMed] [Google Scholar]
- 26. Hung WW, Ross JS, Boockvar KS, Siu AL. Association of chronic diseases and impairments with disability in older adults: a decade of change? Med Care. 2012;50:501–507. :10.1097/MLR.0b013e318245a0e0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. :10.1016/S0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86:726–734. [PubMed] [Google Scholar]
- 29. Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D’Agostino RB., Sr Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: the Framingham Heart Study. Am J Public Health. 2008;98:1256–1262. :10.2105/AJPH.2007.128132 [DOI] [PMC free article] [PubMed] [Google Scholar]


