Abstract
The authors developed and tested a 35-min psychoeducational program with the goal of increasing Spanish-speaking persons’ literacy of psychosis. The program uses popular cultural icons derived from music, art, and videos, as well as a mnemonic device—La CLAve (The Clue)—to increase (a) knowledge of psychosis, (b) efficacy beliefs that one can identify psychosis in others, (c) attributions to mental illness, and (d) professional help-seeking. Assessments were conducted before and after administering the program to both community residents (n = 57) and family caregivers of persons with schizophrenia (n = 38). For community residents, the authors observed increases across the 4 domains of symptom knowledge, efficacy beliefs, illness attributions, and recommended help-seeking. For caregivers, increases were observed in symptom knowledge and efficacy beliefs. La CLAve is a conceptually informed psychoeducational tool with a developing empirical base aimed at helping Spanish-speaking Latinos with serious mental illness obtain care in a timely manner.
Keywords: psychosis, mental health literacy, Latinos, caregivers, community education
Latinos underutilize mental health services relative to their need and relative to other ethnic groups. This has been observed in many community-based epidemiologic research (e.g., Vega, Kolody, Aguilar-Gaxiola, & Catalano, 1999) and patient service (e.g., Barrio et al., 2003) studies. Among the many individual correlates of low service use are nativity, language background, and number of years living in the United States. For example, in a representative sample of Mexican American adults in Fresno County (California), Vega et al. (1999) found that Mexican-born residents with a diagnosable mental disorder were less likely to use mental health services in the last year (5%) than U.S.-born residents of Mexican origin (12%).
Although it is important to identify the factors that underlie low service use (e.g., Aguilera & López, 2008), it is equally important to use such research to ensure that Latinos with serious mental health problems obtain appropriate care in a timely fashion (López, 2002). Aguilar-Gaxiola et al. (2002), for example, presented local policy holders in Fresno County with available epidemiologic data that demonstrated the low number of Mexican Americans receiving mental health care. In addition, they worked with public mental health service systems to increase their responsiveness to this segment of the community. Another action-oriented approach is to educate community residents about matters of mental health (e.g., Johannessen et al., 2001). Subgroups known to make little use of services, such as Spanish-speaking Latinos (Alegría et al., 2007), can be specifically targeted for such educational campaigns. Such efforts could address Latinos’ knowledge or literacy of mental health, which may account, in part, for their low use of services and delayed help-seeking (Urdaneta, Saldaña, & Winkler, 1995).
Psychosis Literacy
The Institute of Medicine (IOM, 2004) defines literacy as the extent to which individuals are able to obtain, process, and understand health information and services to make health decisions. We are specifically interested in one component of health literacy, health knowledge, and its relationship to help-seeking. Health knowledge is not only central to the framework articulated by the IOM’s report, but it is central to our aim of increasing help-seeking. Without knowledge of illness, it is difficult for people to initiate action to address the illness condition.
Our particular focus is on knowledge of psychosis, which is defined by Willerman and Cohen (1990) as delusions, thought disorder as exhibited by disordered speech, and impaired reality testing (e.g., hallucinations). We chose psychosis, as it touches a number of disorders (schizophrenia, bipolar disorder, major depression, dementia, and substance abuse) and is associated with considerable burden to family caregivers (Magaña, Ramirez Garcia, Hernandez, & Cortez, 2007) and society overall (Wu et al., 2005). Moreover, psychotic symptoms may be more easily understood by lay persons than clinical conditions that require attention to fine-grained diagnostic distinctions. For instance, schizophrenia requires two of five characteristic symptoms unless the delusion or hallucination is severe, in which case only one symptom is necessary (American Psychiatric Association, 2000). We reasoned that teaching people to identify psychosis has the advantage of a simple and clear focus with the potential to help a broad range of persons.
Given that family members are among those who facilitate mental health care for their relatives with serious mental illness (Urdaneta et al., 1995), we study literacy or health knowledge as it relates to identifying psychosis in others, not in oneself. This contrasts with much of the current research on individuals’ health literacy and its association with their own health related behavior and outcomes (Baker, 2006).
The IOM’s (2004) report provides a broad framework of health literacy with attention to many components, including print and oral literacy (e.g., reading prescriptions and communicating with health professionals). There is less attention, however, to specific mechanisms that underlie the link between health knowledge and health outcomes, particularly help-seeking. As a result, we draw from related literatures to identify relevant conceptual processes. Specifically, we considered how health knowledge is related to illness attributions or social world attributions (Garro, 1998; Yeh et al., 2005), which in turn can influence caregivers’ decisions obtaining care for their ill relatives. Psychotic episodes are embedded in a rich social world of love interests, family relations, religion, work, school, and many other domains. Individuals with low literacy or knowledge of mental illness may be more inclined to attribute a significant change in the psychological functioning of their relatives to their social world (e.g., a recent divorce, difficulties at school, or some other significant stressor; Weisman, Gomes, & Lopez, 2003) than to a mental disorder (Urdaneta et al., 1995). In many cases, implicating the social world may be accurate, as life stressors contribute to the development of mental disorders (e.g., Caspi et al., 2003). Moreover, the social construal of illness may prompt caregivers to offer support and comfort to their ill relatives; however, there is a downside. Such social attributions may reduce family caregivers’ efforts to consider alternative explanations (e.g., mental illness) and alternative sources of support (e.g., seeking professional help).
Drawing from social cognitive theory (Bandura, 2001), we considered an additional conceptual factor associated with health literacy—a person’s belief that he or she is able to identify psychosis in others. Research in health promotion indicates that self-efficacy beliefs (beliefs that one can carry out certain behaviors) are positively related to specific health behavior outcomes (Bandura, 2004). Although the typical application of social cognitive theory concerns personal efficacy (e.g., self management to improve one’s health), the model can extend to people working to improve the conditions of others (Bandura, 2001). We are particularly interested in potential family caregivers’ efficacy beliefs that they can identify illness in others and, in turn, contribute to improving the mental health status of their ill relatives or friends.
Thus, the conceptual model that guided our research is depicted in Figure 1. Increased health knowledge is thought to lead to higher efficacy beliefs that one can identify illness in others. Together, both health knowledge and efficacy beliefs contribute to greater illness attributions, which in turn lead to increased professional help-seeking. Each of these components is integrated into the brief educational program developed for Spanish-speaking Latinos residing in the United States and Mexico.1
Figure 1.

Conceptual model of health literacy and help-seeking.
La CLAve2 (The Clue)
The focus of our literacy program is health knowledge, specifically knowledge of the key indicators of psychosis. We describe each symptom in clear, every day language, and then we illustrate each one with music, video clips, or art. The idea is not only to tell the participants what the key symptoms are but also to show them. Using the arts helps provide a safe distance in illustrating psychotic phenomenology that can at times be distressing to observe. For example, to illustrate delusions, we use a 2-min segment of the song “El Muelle de San Blas.” The song is about a young woman who holds on to the false belief that her lover will return and who lives waiting at a pier for him to return. Eventually, psychiatric personnel come to retrieve la loca del muelle (the crazy woman from the pier). As the song is playing, we also present the lyrics so that participants can more closely follow the content of the given recording. To add a visual component to the music-based illustrations, we insert paintings. In the case of delusions, we show Rufino Tamayo’s painting of “El Diablo” (The Devil), and we note that oftentimes those who suffer from delusions believe someone or some being is trying to harm the person, including, on occasion, the devil. Our intention in bringing together song, lyrics, and art is two-fold: to enhance the participants’ engagement in the presentation and to increase the participants’ understanding and knowledge of psychosis.
To address the second conceptual factor—the participants’ efficacy belief that they can identify psychosis in others—we include two specific strategies in our educational program. First, we developed a mnemonic device that reflects the key symptoms of psychosis. We organized the presentation of the symptoms around the word clave, which means clue or key. “C” represents creencias falsas (false beliefs or delusions), “L” stands for lenguaje desorganizado (disordered speech or thought disorder), “A” signifies alucinaciones (hallucinations), and “v” and “e” represent the type of hallucination: ver cosas que no existen (see things that do not exist) and escuchar cosas que no existen (hear things that do not exist). One of our main messages is to use La CLAve to detect serious mental illness in others. Our expectation in using the mnemonic device is that it will facilitate the participants’ recall of the symptoms of psychosis (increasing health knowledge) and, in turn, will enhance their belief that they can identify psychosis in others (increasing efficacy).
We use participant learning as another strategy to boost the participants’ efficacy and to introduce them to the concept of illness attribution. After presenting the key symptoms of psychosis and their illustrations, we ask them to listen to a segment of another song, “Sebastian,” and to use La CLAve to detect whether the main character suffers from a serious mental illness. After playing the song, we guide the participants through the following tasks: to recall the sequence of letters in CLAve, to identify the meaning of each letter, and to evaluate whether Sebastian experienced any of the noted symptoms. For example, the presenter asks the group whether Sebastian has a given symptom and corrects any errors in their judgment. We reasoned that by giving the participants an opportunity to apply their newfound knowledge and correcting their responses, they would not only increase their familiarity with the information but also enhance their belief that they are capable of identifying psychosis in others.
Illness attribution was directly addressed in two other ways. First, after presenting all the symptoms, we discussed barriers to treatment that are illustrated in a key segment of the song “La Tristeza de mi Mujer” (My Wife’s Sadness). In this song, a husband struggles to figure out why his wife is sad. He wonders whether it is something that he did or did not do, or something that occurred in her more distant past. We point out that this view represents one barrier to mental health care—caregivers look to their ill relatives’ social world to explain changes in functioning (for a similar point in the context of parental caregivers of youths with special needs, see Yeh et al., 2005). We also point out a related barrier, that caregivers oftentimes fail to consider mental illness as a possible factor. Returning to the song, we indicate that major depression is a mental disorder that could help explain her behavior, yet the husband does not entertain this plausible explanation. Given the importance of the illness attribution process to our framework of literacy, we developed a second strategy to address illness attributions in the specific context of identifying psychosis in a relative. We produced a brief video reenactment based on an actual experience of a family caregiver who was involved in our family research. In the video, the mother relates to the interviewer that when her teenage son first experienced psychotic symptoms, she attributed the symptoms to his having abused drugs, which turned out not to be the case. She did not consider the possibility that he suffered from mental illness.
After the presentation of the brief videotape, the presenter underscored the importance of considering mental illness as an explanation for the identified symptoms. This led to the final conceptual factor: help-seeking. We point out that considering the possibility of mental health problems facilitates obtaining care from mental health professionals. Specifically, we indicate that there are effective treatments for mental illness that not only help the ill relative but also help reduce the burden for the caregiver. The final point of the presentation is to encourage the participants to seek professional help as quickly as possible should they observe these symptoms in their loved ones. At the end of the presentation and evaluation, we distribute a brochure that summarizes the key symptoms and lists the mental health services available in the area identified by the community agency or by our research group. (See Table 1 for a summary of the four conceptual factors and the media used to illustrate each factor and symptom.)
Table 1.
La CLAve (The Clue): Conceptual Factors and Their Illustrations
| Factor | Medium | Artist | Title |
|---|---|---|---|
| Health knowledge | |||
| Creencias falsas (false beliefs) | Song | Mana | El muelle de San Blas |
| Art | R. Tamayo | El diablo | |
| Lenguage desorganizado (disorganized speech) | Movie | Cantinflas | El bolero de Raquel |
| Alucinaciones (hallucinations) | Song | Son by 4 | Sofia |
| Art | E. Mvnch | El grito | |
| Ver cosas que no existen (see things that do not exist) | Song | Son by 4 | Sofia |
| Escuchar voces que no existen (hear voices that do not exist) | Song | Son by 4 | Sofia |
| Efficacy | |||
| Use La CLAve to identify symptoms in song’s character | Song | R. Blades | Sebastián |
| Art | R. Tamayo | El hombre y su mundo | |
| Illness attribution | |||
| Family member attributes relative’s disorder to social world | Song | A. Monges | Tristeza de mi mujere |
| Mother attributes son’s psychosis to drug use | Video | Authors | Pensaba que era por drogas |
| Help-seeking | |||
| Reported treatment helped 70% of patients | Slide | None | Importancia de reconocer sintomas |
Overall Aim and Hypotheses
To examine whether La CLAve can modify Spanish-speaking adults’ literacy regarding psychosis, we carried out a pretraining assessment and a posttraining assessment of the presentation. A key part of this evaluation consisted of participants’ recognition of psychosis in a case in which the social world (a recent divorce), depressive symptoms (e.g., loss of interest in activities), and psychotic symptoms (e.g., delusions) were prominent. For this evaluation, we targeted two groups that we expected to vary with regard to exposure to mental illness: community residents (low exposure) and family caregivers of persons with schizophrenia (high exposure). We expected that including groups with differential exposure to mental illness would help in interpreting the findings by suggesting a lower and a higher range of literacy. We also wanted to assess whether the training could be helpful to family caregivers as well as to the general community. Additionally, we were interested in examining the stability of the training effects over a 3-week time period for a subgroup of participants.
We tested the following hypotheses. First, we expected that prior to any training, community residents would be lower in psychosis literacy and related constructs than family caregivers. Specifically, we hypothesized that relative to caregivers, community residents would identify fewer symptoms of psychosis in their definition of serious mental illness, would report lower efficacy in identifying psychosis in others, would attribute the problems less to mental disorders and more to the social world, would recommend referrals more to personal resources and less to professional resources, and would be less knowledgeable as to where to seek mental health services. Second, we hypothesized that the training would lead both groups to an increase in the domains of knowledge, efficacy belief, illness attribution, and professional referrals. Finally, we expected that over a 3-week time period, there would be little deterioration in the expected gains derived from the training.
Method
Participants
A total of 105 respondents (63 community residents and 42 caregivers) participated in the study, of which 95 (57 community residents and 38 caregivers) took part in both assessments. The 10 respondents who participated in only one assessment (6 community residents and 4 caregivers) were excluded from the analyses. Community residents were drawn from two Spanish-speaking parenting classes at local schools, and one health fair at a local church. All three sites were located in densely populated Latino neighborhoods in east Los Angeles. Either our research team contacted the community agency and invited them to participate in the public education program or the particular agency contacted our research team requesting that we present the educational program. Caregivers were recruited from two ongoing studies of multifamily group interventions for schizophrenia that were taking place in three local outpatient clinics located in Santa Fe Springs, Granada Hills, and northeast Los Angeles—all in the greater Los Angeles metropolitan area. Families were selected for the multifamily group study because they were Spanish-speaking Latinos and they cared for an ill relative with schizophrenia. In two of the clinics, the ill relative had multiple hospitalizations with a history of poor treatment adherence. In addition to the 105 respondents, 8 ill relatives participated in the family group meetings, but their data were not included in the analyses because some of them had attention and memory difficulties. All the community groups and most of the caregivers were recruited beginning May 2006 and ending October 2007. To augment the smaller caregiver group, we administered La CLAve to an additional multiple family group in November 2008.
Procedures
The education program is organized as a set of 42 Power-Point slides with 5 audio clips, 3 video clips, and 4 paintings/drawings. For the training, we used a laptop computer, an LCD projector, and computer speakers. The audiences ranged in size from 9 to 30 persons per training session. The size was based strictly on the availability of participants at each site.
The leader of the multifamily group meeting or the community agency introduced our research team, which included the presenter and two to four assistants. The title of our training was “Learning About Health.” No mention was made of mental health at the beginning of the presentation so as not to prime the participants that we were interested in mental health literacy at the pretraining assessment. We then introduced ourselves and informed the audience that we would teach them about health but that we also wanted to evaluate the training. To do so, we told them that both before and after the main session, we would read them a story and then ask questions about the story and related topics. We then distributed the first handout that included the story and the questionnaire. Those who agreed to participate in the evaluation were then asked to listen closely to the story.
In reading the case, we asked the participants to pretend that they were listening to their comadre (a very close friend) who is telling them a story (platicando) about their neighbor’s daughter Olga. One member of the research team, usually a woman, then read the case. It begins as follows: “¿Qué crees? ¿Te acuerdas de Olga, La hija de mi vecina? Pues se acaba de divorciar de su esposo Ricardo después de 9 años de matrimonio. ¡Ay! Que lástima porque son tan jóvenes, apenas tienen 30 años.” (You’d never believe this. Do you remember Olga, the daughter of my neighbor? Well she just divorced her husband Ricardo after 9 years of marriage. Ay! What a shame because they are both so young. They are barely 30 years old.) The story then unfolded: Olga returned to live with her parents, and she has had several experiences that suggest various clinical symptoms described in every day language. First, the comadre tells of Olga being depressed, becoming sad very easily, and crying over things that did not use to affect her. Olga, who prided herself in her appearance, is also no longer caring for herself; her mother has to remind her regularly to change her clothes and comb her hair. These experiences represent three possible indicators of depression (sadness, crying easily, and a loss of interest). The comadre also describes the possibility of psychotic symptoms as well. She says that the family overhears Olga talking to her ex-husband even though he is not with her (possible auditory hallucinations). Also, more recently Olga has begun to blame her parents for the divorce saying that they never liked Ricardo and that they had a spell placed on him (le hicieron un trabajo de brujería) so that the young couple would separate (a possible delusion). Olga is sure that this is true because she says that she can read people’s minds (another possible delusion). Like depression, we included three possible indicators of psychosis in the case.
Following the presentation of the story, participants were asked to answer a series of questions. We anticipated that some of the participants would have little education and limited reading and writing skills. Therefore, we took the following steps to facilitate their understanding of the questions and to help them with their responses. First, one of the research team members stood before the group and read each question in a measured pace, allowing sufficient time for the participants to respond. Second, we placed the questions and response formats on the Power-Point presentation and advanced them as they were read so that participants could keep track of which question was being read at a given time. Third, other research team members were available to help those who needed assistance in reading or writing their responses. Each of these research team members, all of whom were bilingual, sat with a given participant and assisted them as needed. The pretraining assessment required about 15–20 min to complete.
After the pretraining assessment, Steven R. López presented the training, which was entitled “Reconociendo la enfermedad mental” (Recognizing Mental Illness). The main training session took approximately 35 min. Afterwards, the posttraining assessment was carried out, adhering very closely to the pretraining assessment procedures. The only differences were that the participants’ sociodemographic background and knowledge of where to seek mental health care were assessed only at the pretraining, and their recollection of the meaning of CLAve and the acceptability of the training were assessed only at the posttraining.
Measures
Following the reading of the vignette, three brief sets of measures were administered to assess the participants’ literacy and related constructs, acceptability of the training, and their sociodemographic background. We conceive of literacy as reflecting health knowledge (symptom identification) and its associated constructs of efficacy beliefs that one can identify psychosis in others, illness attributions, and help-seeking (personal vs. professional). Health knowledge or symptom identification was assessed by the participants’ written responses to the following open-ended question: “What are the symptoms or principal signs of a serious mental illness?” Raters coded whether the respondents identified any of the three psychotic symptoms. To measure efficacy beliefs in identifying mental illness, we asked one question: “How sure are you that you can identify someone with a serious mental illness?” A 5-point rating scale followed this question (1 = not at all, 2 = a little, 3 = somewhat, 4 = quite a bit, 5 = very much).
Illness attributions were assessed by their responses to the open-ended questions immediately following the reading of the case: “What’s happening to Olga? What do you think is the matter with her?” Four codes were developed from the responses: psychosis, mental health, depression/sadness, and social world. The responses of each participant could be coded in one or multiple categories. Reference to one of the three possible psychotic symptoms or a description of the symptoms (e.g., she is talking to her husband who is not there) was coded as psychosis. Mental health referred to more general references, such as “Olga has a mental problem” or she is “confused.” Depression was coded when the respondent referred to either sadness or depression. Finally, social world referred to external circumstances, such as the divorce, stress, or family problems. Only 5% of the 93 participants who answered this question at pretraining and 8% of the 93 respondents who answered this question at posttraining had responses that were not coded. These responses were either vague (e.g., “she has a problem”; “she is not well”; “she is ill”) or they were not consistent with the question (“she needs to talk to her parents and friends”). In addition to the open-ended questions, which we refer to as active illness recognition, we assessed passive illness attributions by asking participants to indicate whether they thought Olga had a serious mental illness for which participants answered “yes” or “no.”
Immediately after the open-ended illness attribution questions, we assessed their recommended help-seeking by asking “What should her parents do to help her?” The responses were coded as either recommendations for personal support (e.g., “talk to her and show her affection”) or professional help (e.g., a counselor and a physician). A participant’s response could be coded as both types of help. Only 1 of 93 participants who answered this question at pretraining and 2 of the 93 who answered the question at posttraining had responses that were not coded because they did not refer to a professional or personal helper for Olga. For example, 1 respondent wrote “tell them [the parents] that they are not responsible” and another wrote “false beliefs.” Given the group administration format, no follow-up queries were made to clarify these responses. Also, within the domain of help-seeking, we inquired at only pretraining whether respondents knew where to obtain mental health services: “If you had a relative with a serious mental illness, do you know of a clinic or professional where you could take your ill relative?” The respondent circled either “yes” or “no.”
To assess their recall, we asked the participants at the end of the sessions to write down what each letter of CLAve represented. In addition, we returned to a subsample of participants 3 weeks after the training and asked them to identify the symptoms of serious mental illness, to rate their efficacy in identifying mental illness in others, and to write each symptom associated with CLAve. This group was selected because a relatively large number of residents participated (Time 1: n = 30; follow-up: n = 21), the group met on a weekly basis, and the leader was amenable to the research team returning to carry out the follow-up.
Acceptability of the training was measured with three questions: “How much did you like the presentation?”; “How engaging was the presentation?”; and “What part did you like most?” A 10-point Likert scale ranging from 1 (not at all) to 10 (very much) followed the first two questions.
To assess the participants’ sociodemographic background, we asked them to indicate their gender, their age, the number of years of schooling they completed, whether they were employed, whether they were a homeowner, where they were born, and how many years they have lived in the United States. Also, they were asked to rate how well they speak English and Spanish on separate rating scales drawn from Marin and Gamba’s (1996) Bidimensional Acculturation Scale (4 = very well, 3 = well, 2 = not well, and 1 = very poorly).
Interrater Agreement in Coding of Open-Ended Questions to Assess Literacy
Responses to open-ended questions were transcribed into a Microsoft Excel file and ordered randomly. For the knowledge measure (“What are the symptoms or principal signs of a serious mental illness?”), the first 60 responses were coded by two raters. The raters achieved high interrater agreement (κ= .93) in identifying those responses that reflected one of the three indicators of psychosis.
To assess the reliability in coding the answers to the illness attribution question (“What’s happening to Olga? What do you think is the matter with her?”), we selected the pretraining and posttraining responses for the first 101 cases (including 15 cases from the pilot data that were not used in the final analyses) without reference to whether the response was obtained at pre- or posttraining assessments. Two raters achieved kappas of .89 for psychosis, .90 for mental health problems, 1.00 for depression/sadness, and .84 for the social world.
Two raters also coded responses specific to the question used to elicit the participants’ recommendations for help-seeking, in particular whether they recommended personal or professional resources. The two codes were personal resources (e.g., the family should talk to Olga) and professional resources referring to mental health professionals broadly defined, including physicians. The first 55 responses of a random order of responses were coded, resulting in kappas of .89 for personal resources and .96 for professional help. Interrater reliability was also assessed for the number of correct symptoms associated with the word CLAve. Two raters coded the responses of 56 participants, and they were found to have excellent reliability (κ= .95).
For all the reliability assessments of the open-ended responses, when the two raters disagreed on a given coding, they discussed the rationale for each others’ ratings and derived a consensus rating. Given the overall excellent interrater agreement with sub-samples of responses, after the reliability checks, one of the coders completed the remaining ratings alone.
Missing data
For the dependent measures, the question regarding whether Olga was mentally ill had the most missing cases (7 at pretraining and 5 different cases at posttraining). All the other measures had from 0 to 2 missing cases at either pre- or posttraining assessment. Four questions were added after the first community presentation to more fully assess the respondents’ literacy and possible correlates. They included the health knowledge/symptom identification question, whether they knew where to obtain mental health services, and their self-reported ability to speak English and Spanish. Thus, the n for these measures is 15 less than the other measures. For the demographic data, 15 of the caregivers were not administered the questions regarding employment and home ownership. For those community residents and caregivers who received all the demographic queries, missing data ranged from 0 to 7 cases for selected demographic variables, including years in the United States, employment, and home ownership. No adjustments were made for missing data.
Results
Sociodemographic Background
The participants were largely foreign born (86%). They were better able to speak Spanish (M = 3.56, SD = 0.64) than English (M = 1.99, SD = 1.02), paired t(77) = 11.71, p < .001. They also reported an average of 42 years of age, 8 years of education, and 21 years of residence in the United States. The majority (57%) indicated that they were not employed. Table 2 summarizes the findings comparing the social background of the community participants and the family caregivers. Relative to the caregivers, the community residents were more likely to be women, less likely to own a home, and were younger in age. Community residents also reported living in the United States for fewer years than caregivers. When applying a Bonferroni correction for these multiple tests (.05/9 = .006), each of the group differences remains significant.
Table 2.
Participants’ Background by Group
| Community residents |
Family caregivers |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Background | n | % | M | SD | n | % | M | SD | χ 2 | t |
| Women | 57 | 0.95 | 38 | 0.61 | 17.38* | |||||
| Foreign-born | 57 | 0.84 | 38 | 0.90 | 0.54 | |||||
| Unemployed | 56 | 0.59 | 20 | 0.50 | 0.48 | |||||
| Home owner | 56 | 0.07 | 20 | 0.55 | 21.31* | |||||
| Age (years) | 57 | 36.54 | 10.65 | 38 | 49.92 | 12.21 | 5.66* | |||
| Years of schooling | 55 | 8.80 | 3.36 | 36 | 7.61 | 4.21 | 1.49 | |||
| Years in United States | 53 | 16.96 | 8.90 | 35 | 28.03 | 8.46 | 5.82* | |||
| English-speaking ability | 42 | 2.02 | 1.09 | 37 | 1.95 | 0.94 | 0.34 | |||
| Spanish-speaking ability | 41 | 3.56 | 0.59 | 37 | 3.57 | 0.69 | 0.05 | |||
Note. Missing data were primarily due to individual participants not answering selected questions, except in the case of language, employment, and home ownership. Those questions were not administered across all sites, particularly early in the data collection.
p < .001.
Pretraining Assessment: Do Community Residents Report Less Psychosis Literacy Than Caregivers?
Knowledge
Of the three possible psychotic symptoms that a respondent could refer to when asked to identify the symptoms of serious mental illness, on average, both groups identified less than one of those symptoms. Community residents (M = 0.45, SD = 0.63) though had a significantly lower mean number of symptoms than caregivers (M = 0.76, SD = 0.68), t(77) = 2.06, p = .04, Cohen’s d = 0.47.3
Efficacy belief
Community residents (M = 3.02, SD = 1.09) reported that they were significantly less able to identify serious mental illness in others than the caregivers (M = 3.54, SD = 1.33), t(92) = 2.08, p = .04, Cohen’s d = 0.44.
Illness attributions
In assessing active illness recognition, overall both groups gave little attention to psychosis and mental health problems, but again community residents tended to give less attention—psychosis: residents = 2%, caregivers = 11%, χ2(1, N = 93) = 3.35, p = .07, Φ= .19; mental health problems: residents = 7%, caregivers = 37%, χ2(1, N = 93) = 12.59, p < .001, Φ= .37. For the measure of passive illness recognition, the same general pattern was observed of community residents (54%) recognizing less mental illness than caregivers (75%), χ2(1, N = 88) = 4.06, p = .04, Φ= .22. An opposite pattern of findings pertained to attributions of depression/sadness and ascriptions to the social world. Community residents implicated themes of depression more than caregivers (residents = 86%, caregivers = 47%), χ2(1, N = 93) = 15.49, p < .001, Φ= .41. Residents also tended to ascribe the problem more to the social world than caregivers (residents = 0.56, caregivers = 0.37), χ2(1, N = 93) = 3.43, p = .06, Φ= .19. Applying a Bonferroni correction for the multiple tests (.05/5 = .01), two of the three observed differences remain significant: the ascriptions to general mental health problems and to depression.
Recommended help-seeking
A greater proportion of community residents (71%) than caregivers (49%) indicated that family members should address the problem using personal resources (family and friends), χ2(1, N = 93) = 4.93, p = .03, Φ = .23. However, the two groups did not differ in their consideration of seeking professional help for Olga (residents = 59%, caregivers = 60%), χ2(1, N = 93) = 0.00, p = .96. Fewer community residents than caregivers, however, knew where to obtain mental health services (residents = 45%, caregivers = 84%), χ2(1, N = 79) = 12.58, p < .001, Φ = .40. When applying the Bonferroni correction (.05/3 = .017), only the group difference in knowledge of where to obtain mental health services remains significant.
Posttraining Assessment: Does Training Increase Literacy?
We carried out two types of analyses to assess for training effects. For continuous variables, we conducted 2 (group: residents and caregivers) × 2 (time: pretraining and posttraining) mixed design analyses of variance (ANOVAs). The advantage of these analyses is that they directly test for group differences. For categorical data, we carried out a series of separate McNemar tests to determine whether the training enhanced literacy of first the community residents and then the caregivers.
Knowledge
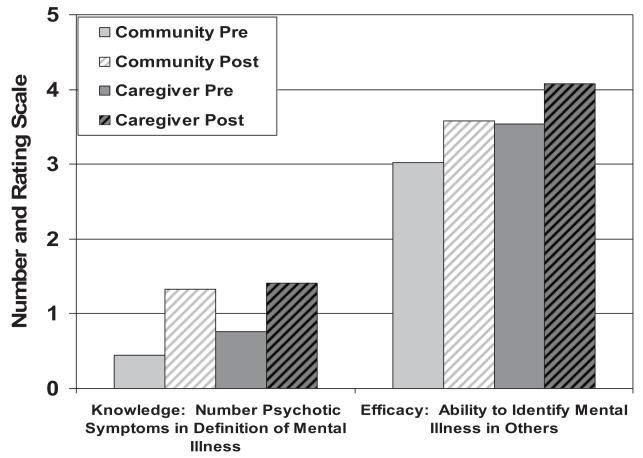
We found a significant main effect for time, F(1, 77) = 47.35, p < .001, η2 = .38, indicating that the training increased the two groups’ reported knowledge of the three symptoms of psychosis (residents: pretraining, M = 0.45, SD = 0.63; posttraining, M = 1.33, SD = 0.95; caregivers: pretraining, M = 0.76, SD = 0.68; posttraining, M = 1.41, SD = 0.97). There was no significant main effect for group (p = .19) and no significant Group × Time interaction, F(1, 77) = 1.09, p = .30. See the first bar graph within Figure 2 for a depiction of these findings.
Figure 2.
Training effects on knowledge (identification of symptoms) and efficacy belief by group. Community Pre = community residents pretraining; Community Post = community residents posttraining; Caregiver Pre = caregivers pretraining; Caregiver Post = caregivers posttraining.
Efficacy belief
For the reported ability to identify mental illness in others, we found a significant main effect for time, F(1, 92) = 17.50, p < .001, η2 = .16, indicating that the training increased efficacy for both community residents and caregivers. In addition, there was a significant main effect for group, F(1, 92) = 6.34, p = .014, η2 = .06. As shown in the second bar graph within Figure 2, the means reveal that community residents reported less of an ability to identify mental illness than caregivers (residents: pretraining, M = 3.02, SD = 1.09; posttraining, M = 3.58, SD = 1.10; caregivers: pretraining, M = 3.54, SD = 1.33; posttraining, M = 4.08, SD = 1.12). No significant interaction was observed for this measure (p = .98).
Illness attributions and referrals
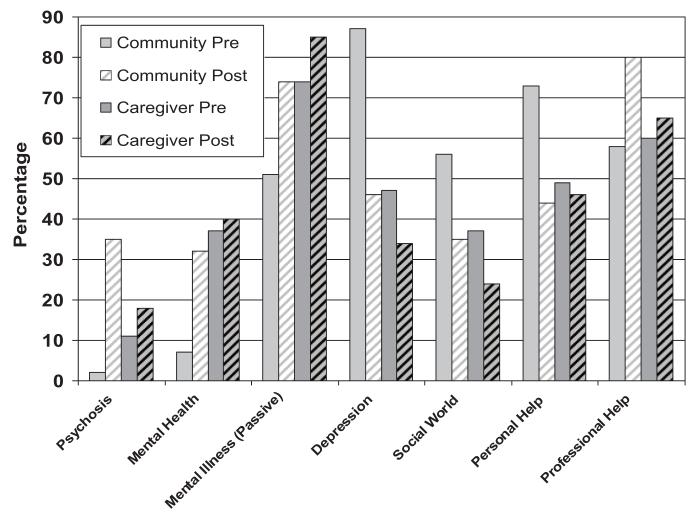
Compared with pretraining illness attributions, posttraining illness attributions of community residents increased with regards to psychosis (pretraining = 2%, posttraining = 35%, n = 54, p < .001), mental health related problems (pretraining = 7%, posttraining = 32%, n = 54, p = .004), and mental illness (passive recognition) (pretraining = 51%, posttraining = 74%, n = 49, p = .007). Illness attributions decreased with regards to depression/sadness (pretraining = 87%, posttraining = 46%, n = 54, p < .001) and the social world (pretraining = 56%, posttraining = 35%, n = 54, p = .027). Also, after the training, community residents were less likely to suggest that family members seek personal solutions (pretraining = 73%, posttraining = 44%, n = 55, p < .001) and were more likely to suggest professional solutions (pretraining = 58%, posttraining = 80%, n = 55, p = .008). Figure 3 illustrates these significant training effects for community residents. Five of the seven pre- and postassessment differences remain significant when applying a Bonferroni correction (p = .007).
Figure 3.
Training effects on illness attributions and recommended help-seeking by group. Community Pre = community residents pretraining; Community Post = community residents posttraining; Caregiver Pre = caregivers pretraining; Caregiver Post = caregivers posttraining.
In contrast to the consistent training effects for the community residents, there were no significant changes observed for caregivers’ illness attributions (ps ranged from .22 [mental illness passive recognition] to 1.00 [mental health problems]) or for professional (p = .79) or personal (p = 1.00) referrals. Figure 3 also depicts the absence of significant training effects for caregivers (e.g., attribution to mental health problems: pretraining = 37%, posttraining = 40%).
Recall and Stability of Literacy Gains
At the very end of the posttraining assessment, we tested the participants’ recall of the meaning of each letter of CLAve. Overall, participants recalled an average of 3.58 indicators (SD = 1.73) of the possible 5 indicators, with 60% of the sample remembering 4–5 indicators. Community residents (M = 3.87, SD = 1.56) tended to remember more symptom indicators than caregivers (M = 3.17, SD = 1.91), t(87) = 1.90, p = .06, Cohen’s d = 0.40.
At 3 weeks, we returned to one of the community resident groups to assess briefly the stability of their increased knowledge and efficacy. Using paired t-tests, we first assessed whether there were still significant differences between the pretraining assessment and the 3-week follow-up on the number of symptoms identified in the participants’ definition of serious mental illness and self-reported efficacy. We found significant increases in the number of identified symptoms (pretraining: M = 0.67, SD = 0.66; 3-week follow-up: M = 1.14, SD = 0.91), t(20) = 1.94, p = .03 (one-tailed), Cohen’s d = 0.59. We also found significant increases in the efficacy ratings (pretraining: M = 3.10, SD = 1.14; 3-week follow-up: M = 3.48, SD = 0.98), t(20) = 1.71, p = .05 (one-tailed), Cohen’s d = 0.53. Although a Bonferroni correction nullifies the significant differences, the effect sizes suggest that the changes observed in the participants’ knowledge and efficacy have some stability over time.
We also assessed whether there was a significant deterioration in community residents’ recall of the meaning of the CLAve indicators from the end of the training to the follow-up. A paired t-test revealed that there was a decline but that it was not significant (posttraining: M = 4.62, SD = 0.97; 3-week follow-up: M = 4.19, SD = 1.33), t(20) = 1.53, p = .14.
Acceptability of Training
A multivariate analysis of variance (MANOVA) was conducted with the two acceptability ratings. At posttraining, both community residents (M = 9.39, SD = 1.33) and caregivers (M = 9.27, SD = 1.54) indicated that they very much liked the presentation, and they found it to be very engaging (residents: M = 9.26, SD = 1.68; caregivers: M = 9.14, SD = 1.40). The MANOVA revealed no significant difference between participant groups in both acceptability measures (p = .91).
Discussion
We successfully accomplished our main goal to develop a clear, theoretically informed, nontechnical presentation to increase Spanish-speaking persons’ psychosis literacy. Our evaluation indicates that La CLAve was well received by participants, and it increased their knowledge of psychotic symptomatology for both community residents and caregivers. Moreover, the follow-up test conducted 3 weeks after the training revealed that there was some stability in the participants’ knowledge of psychosis. La CLAve represents a nontraditional approach with initial empirical support to reach an underserved community (Muñoz & Mendelson, 2005).
Differential Impact
Community residents benefited most from the training. Increases were observed across the four literacy related domains of symptom knowledge, efficacy beliefs, illness attributions, and recommended help-seeking. The message of La CLAve successfully reached this group. Caregivers benefited as well but not in the same fashion. The training does not increase family caregivers’ illness attributions or their recommended help-seeking. However, it does increase the caregivers’ inclusion of psychotic symptoms in their definition of serious mental illness and it increases their perception that they can identify serious mental illness. These improvements in literacy (knowledge) and self-efficacy may be useful in monitoring the course of illness or recovery of their ill relatives.
One reason why community residents may have benefited most from La CLAve is that prior to training, their psychosis literacy broadly defined was, as expected, significantly lower than that of the caregivers. For example, the community residents were less likely to attribute Olga’s problems to a mental health problem (not including depression) than caregivers. However, after training, the community residents’ level of literacy and associated constructs began to approximate that of caregivers. For instance, community residents increased their illness attributions of mental health problems and psychosis, and they decreased their attributions to social problems, which in most cases was in line with family caregivers’ views.
An additional indicator of differential literacy is that less than half (44%) of the community residents reported knowing of a place where they could obtain mental health services, whereas over three fourths of the caregivers reported knowing of such a place. These figures, though much less than ideal, are significantly higher than those obtained from a community survey carried out in Los Angeles 40 years ago. Karno and Edgerton (1969) found that only 20% of a sample of 444 Mexican American residents said they knew where to obtain such services.
Psychosis, Depression/Sadness, and the Social World
Psychosis is a less salient schema than depression for both community residents and caregivers. We presented a vignette that included an equal number of psychotic and depressive symptoms. At pretraining, the ratio of the number of community residents identifying psychotic symptoms relative to those identifying depressive symptoms was 1:47.4 The ratio was much less skewed for caregivers (4:18) but still reflected greater recognition of depression. After the training, the ratios were less extreme for both community residents (19:25) and caregivers (7:13), but they still reflected less recognition of psychosis. One possible interpretation is that the case the participants rated pulled for more depressive phenomenology than psychosis. Divorce is likely perceived to be associated with depression and sadness much more than psychosis. Another interpretation is that Spanish-speaking Latinos have less exposure to psychosis than depression. A third possible explanation is that depression is not perceived to be an illness per se, but it is judged to be more of a normal response to a difficult situation or set of situations. The latter interpretation is consistent with Pincay and Guarnaccia’s (2007) observation that many Latinos initially do not conceive of depression as an illness but rather consider it to be a consequence of social disruptions. Whatever the reason, it is clear that further educational efforts are needed to help this community identify psychosis in others, particularly in the context of depression.
The other salient attribution to the case concerned the character’s social world. In these instances, the problem was defined as stress due to the divorce, family tension, and related circumstances. For example, 1 participant wrote in her phonetic Spanish “Puez a Olga no paza nada porque son cosaz de lavida.” (Well, nothing [bad] happens to Olga; it’s just life.) It is potentially useful to consider the social context of a given mental health problem. Doing so may help individuals construct an unfamiliar experience (mental illness) into a familiar experience (divorce). The emphasis on the familiar may provide some direction on how to help one’s ill relative, for instance, by expressing compassion and understanding.
There is a risk, however, in attributing the observed symptoms to familiar social stressors. The observer may overlook significant mental health problems—as was the case with Olga, in which psychosis was largely overlooked. The educational training was able to address this tendency by increasing attributions to mental health problems, including psychosis. Nevertheless, the increased attention to mental health problems came at cost—a reduction in the implication of the social world. Ideally it is important that observers, in particular caregivers, consider both the social context and mental illness. Doing so provides multiple avenues (personal and professional resources) for facilitating help.
Recommended Help-Seeking
An important reason to consider mental health problems is that doing so will likely facilitate the referral to professional help. For community residents, the relative increase in the identification of psychosis and mental health problems and the relative decrease in reference to the social world corresponded to the pattern of recommended referrals. After the training, community residents recommended less personal resources to address the presenting problem (e.g., the parents should be more understanding) and more professional resources (e.g., the family should take her to a counselor). This appears to be a useful trend, as it reflects a greater recognition of the need for professional help. However, it is not clear that less consideration of personal resources are needed, as anyone with a psychotic illness will require great understanding and affection from their family members, as well as professional help. Indeed, the training encourages individuals to seek professional care for their loved ones when psychotic symptoms are present. Although there is no content to discourage personal support, perhaps not mentioning in the presentation the importance of personal care led to giving priority to professional help. Future training would do well to encourage family support and caring, as research indicates that it may serve as a protective factor in reducing the likelihood of further relapse (López et al., 2004).
Active or Passive Recognition of Mental Illness
The degree of illness recognition varied by the method of inquiry. Prior to the training, when asked in an open-ended manner “What is happening to Olga?,” very few community residents (7%) and under a half of the caregivers (42%) referred to a mental health related problem5 other than depression/sadness. However, when asked directly “Does Olga have a serious mental illness?,” considerably more respondents implicated mental illness (51% of community residents and 74% of caregivers).
These two methods assess different aspects of illness recognition or attribution. The open-ended question requires the participant to actively recognize mental illness in another, whereas the direct query reflects passive recognition. Active recognition more likely reflects what actually takes place in every day life. One has to independently discern that a loved one might be suffering from mental illness. Passive recognition is less likely to occur in every day life but may more likely be elicited when seeking services outside the home (e.g., in primary care or with social service agencies). Moreover, passive recognition may reflect the highest possible level of recognition. Even so, there is still room for improvement, as 49% of the community residents did not identify the character in the vignette as suffering from a mental disorder. We would like our training to increase both types of illness recognition; however, we believe that improving active recognition of mental illness will have the greatest impact on individuals applying their learning to their every day lives. Accordingly, although we will continue measuring both types of illness recognition, our primary aim is to promote active mental illness recognition.
Implications of La CLAve
There is a growing body of research that measures duration of untreated psychosis and examines its association with both clinical and functional outcomes (Perkins, Gu, Boteva, & Lieberman, 2005). There is reason to believe that if the duration of untreated psychosis can be reduced, particularly for first episodes, then the course of illness may be less problematic (McGlashan & Johannessen, 1996). A number of interventions have been developed to not only educate communities about psychosis but also to provide prompt screening evaluations embedded with existing clinical services (e.g., Melle et al., 2004). The current project could serve as part of an educational campaign for Spanish-speaking Latinos and could be embedded in a larger program to increase their prompt receipt of care.
Although there are potential benefits to psychosis literacy campaigns, it is important to recognize their potential risks as well. First, community residents may identify family members as suffering from psychosis when in fact they do not have a psychotic illness. Second, such campaigns may be privileging the mental health field’s construction of experience (psychosis) instead of a wide range of cultural constructions observed in the community (nerves, stress, and bewitchment). Last, educating community residents about psychosis when mental health services are very limited may be communicating a false sense of hope that their ill relatives’ conditions can be treated, when in fact inadequate resources make the provision of care unlikely. All of these risks should be considered carefully before launching such a campaign. However, given the very limited use of mental health services for Latinos, especially Spanish-speaking Latinos, and given the serious disability that people with psychotic disorders incur, it behooves us to reach out to this underserved community and to help them obtain proper care in a timely fashion. Assessing for possible risks prior to and during an educational campaign is one step that can help address these potential risks.
Limitations
One limitation is that we included a relatively small number of caregivers, thus reducing the likelihood of detecting effects in analyses with caregivers. Second, there were significant differences between caregivers and community residents (e.g., gender, age, and economic status as suggested by home ownership) that may have contributed to the observed differences thought to be due to exposure to mental illness. For example, caregivers were much older and lived in the United States much longer than community residents. The caregivers’ increased literacy may be a function of these factors and not their experience of caring for an ill relative. Third, as the assessment of literacy related constructs was tied to the participants’ judgments of a hypothetical case, reactions to the case may not be generalizable to reactions of actual persons with serious mental illness. Fourth, the stability assessment was carried out with the community site that turned out to have the highest recall of psychotic symptoms or CLAve indicators (M = 4.67, SD = 0.88; the other two communities: M = 3.58, SD = 1.62; and M = 2.57, SD = 1.65).6 Because the learning was greatest at this one site, the ability of the participants at this site to recall the key information 3 weeks later may also have been greater than the other community sites or caregiver groups.7 Last, although the educational program increased psychosis literacy, in some cases the magnitude of the increases was modest (e.g., knowledge of psychotic symptoms). This may be due, in part, to the low educational level of some of the participants and the emphasis given to reading and writing skills for both the program and its evaluation. In addition, the application of the Bonferroni correction may have served to reduce some of the training effects. In the development of a novel educational intervention, one could argue that a less conservative analytic strategy would be best to identify the intervention’s potential effects.
Conclusion and Future Directions
La CLAve is a nontraditional, conceptually informed psychoeducational tool with a developing empirical base to help Latinos with serious mental illness seek necessary mental health care. La CLAve can improve psychosis literacy for Spanish-speaking community residents. It also has the potential to be used as part of the psychoeducational training of family caregivers to increase their knowledge of psychosis and to help them feel more confident in their ability to recognize the key symptoms of psychosis in their family members.
Although we will continue to refine the content given future findings, our main attention at this time is to consider dissemination. The present format of the educational program—a Power-Point presentation administered by a mental health professional—has the flexibility of being adapted (changing songs and artwork) to reflect the regional preferences of the diverse Latino communities. The limitation, however, is that its current administration requires a mental health professional: someone knowledgeable of serious mental illness and its treatment. We recently developed a video presentation of La CLAve and are examining whether the administration of the video version by community workers can also help increase mental health literacy. If successful, we will be in position to launch a widespread campaign beginning in southern California. We would target Spanish-speaking residents as well as family caregivers to help both groups bring their loved ones with serious mental illness to the attention of mental health services in a timely manner.
Acknowledgments
This research was supported by the University of California–Mexico Health Initiative (UC-MEXUS); the University of California, Los Angeles (UCLA) Community Partnership Program; the UCLA Life Sciences; and the Latino Behavioral Health Institute (Thousand Oaks, California). We thank Monica Aguilar, Concepcion Barrio, Franklin Carvajal, Mariana Cervantes, Leticia Cuecuecha, Linda Garro, Jorge Ramírez García, Marvin Karno, María Elena Medina-Mora, Isaac Robertos, Ambrose Rodriguez, and Jodie Ullman for their assistance.
Footnotes
In a subsequent report, we will present the data we obtained in Mexico.
Copyright 2005 by Leticia Cuecuecha, Ma. del Carmen Lara, and Steven R. López.
The measure of knowledge was not administered to the first group of community residents, reducing the n on this measure by 15.
The participant could endorse one symptom (psychosis or depression) or both symptoms. Note that the n for the residents changes from 55 for the preassessment to 54 for the postassessment.
In this case, a mental health related problem includes references to psychosis or more general mental health problems.
A one-way ANOVA revealed a significant difference across groups, F(2, 50) = 12.37, p < .001.
Post hoc analyses comparing the demographic background of those who participated in the 3-week follow-up assessment and those who did not participate in the follow-up assessment revealed only one of nine Bonferroni-corrected significant group differences (p < .006). Those who participated in the follow-up assessment reported speaking better Spanish (M = 3.86, SD = 0.40) than those who did not participate in the follow-up assessment (M = 3.32, SD = 0.67), t(38) = 3.23, p = .003. The other eight demographic variables revealed no group differences (ps = .06–.86). See Table 2 for a list of the demographic variables for which analyses were conducted.
Contributor Information
Steven R. López, Department of Psychology, University of Southern California
Alex Kopelowicz, Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, University of California, Los Angeles.
Susana Solano, Department of Psychology, University of California, Los Angeles.
Ma. del Carmen Lara, Department of Psychiatry, School of Medicine, Benemérita Universidad Autónoma de Puebla, Puebla, Mexico
Hector Foncerrada, Department of Psychiatry, School of Medicine, Benemérita Universidad Autónoma de Puebla, Puebla, Mexico.
Adrian Aguilera, Department of Psychology, University of California, Los Angeles.
References
- Aguilar-Gaxiola S, Zelezny L, Garcia B, Edmondson C, Alejo-Garcia C, Vega WA. Translating research into action: Reducing disparities in mental health care for Mexican Americans. Psychiatric Services. 2002;53:1563–1568. doi: 10.1176/appi.ps.53.12.1563. [DOI] [PubMed] [Google Scholar]
- Aguilera A, López SR. Community determinants of Latinos’ use of mental health services. Psychiatric Services. 2008;59:408–413. doi: 10.1176/appi.ps.59.4.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American study. American Journal of Public Health. 2007;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text rev. [Google Scholar]
- Baker DW. The meaning and measure of health literacy. Journal of General Internal Medicine. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: An agentic perspective. Annual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health, Education, and Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Barrio C, Yamada AM, Hough RL, Hawthorne W, Garcia P, Jeste DV. Ethnic disparities in use of public mental health case management services among patients with schizophrenia. Psychiatric Services. 2003;54:1264–1270. doi: 10.1176/appi.ps.54.9.1264. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003 Jul 18;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Garro LC. On the rationality of decision making studies: Part 1. Decision models of treatment choice. Medical Anthropology Quarterly. 1998;12:319–340. doi: 10.1525/maq.1998.12.3.319. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Health literacy: A prescription to end confusion. National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- Johannessen JO, McGlashan TH, Larsen TK, Horneland M, Joa I, Mardal S, et al. Early detection strategies for untreated first-episode psychosis. Schizophrenia Research. 2001;51:39–46. doi: 10.1016/s0920-9964(01)00237-7. [DOI] [PubMed] [Google Scholar]
- Karno M, Edgerton R. Perception of mental illness in a Mexican-American community. Archives of General Psychiatry. 1969;20:233–238. doi: 10.1001/archpsyc.1969.01740140105013. [DOI] [PubMed] [Google Scholar]
- López SR. A research agenda to improve accessibility and quality of mental health care for Latinos. Psychiatric Services. 2002;53:1569–1573. doi: 10.1176/appi.ps.53.12.1569. [DOI] [PubMed] [Google Scholar]
- López SR, Nelson Hipke K, Polo AJ, Jenkins JH, Karno M, Vaughn C, et al. Ethnicity, expressed emotion, attributions, and course of schizophrenia: Family warmth matters. Journal of Abnormal Psychology. 2004;113:428–439. doi: 10.1037/0021-843X.113.3.428. [DOI] [PubMed] [Google Scholar]
- Magaña SM, Ramirez Garcia JI, Hernandez MG, Cortez R. Psychological distress among Latino family caregivers of adults with schizophrenia: The roles of burden and stigma. Psychiatric Services. 2007;58:378–384. doi: 10.1176/appi.ps.58.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS) Hispanic Journal of Behavioral Science. 1996;18:297–316. [Google Scholar]
- McGlashan TH, Johannessen JO. Early detection and intervention with schizophrenia: Rationale. Schizophrenia Bulletin. 1996;22:201–222. doi: 10.1093/schbul/22.2.201. [DOI] [PubMed] [Google Scholar]
- Melle I, Larsen TK, Haahr U, Friis S, Johannessen JO, Opjordsmoen S, et al. Reducing the duration of untreated first-episode psychosis: Effects on clinical presentation. Archives of General Psychiatry. 2004;61:143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- Muñoz RF, Mendelson T. Toward evidence-based interventions for diverse populations: The San Francisco General Hospital prevention and treatment manuals. Journal of Consulting and Clinical Psychology. 2005;73:790–799. doi: 10.1037/0022-006X.73.5.790. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: A critical review and meta-analysis. American Journal of Psychiatry. 2005;162:1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- Pincay IEM, Guarnaccia PJ. “It’s like going through an earthquake”: Anthropological perspectives on depression among Latino immigrants. Journal of Immigrant Minority Health. 2007;9:17–28. doi: 10.1007/s10903-006-9011-0. [DOI] [PubMed] [Google Scholar]
- Urdaneta ML, Saldaña DH, Winkler A. Mexican-American perceptions of severe mental illness. Human Organization. 1995;54:70–77. [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Catalano R. Gaps in services utilization by Mexican Americans with mental health problems. American Journal of Psychiatry. 1999;156:928–934. doi: 10.1176/ajp.156.6.928. [DOI] [PubMed] [Google Scholar]
- Weisman A, Gomes L, Lopez SR. Shifting blame away from ill relatives: Latino families’ reactions to schizophrenia. Journal of Nervous and Mental Disease. 2003;175:143–151. doi: 10.1097/01.nmd.0000087183.90174.a8. [DOI] [PubMed] [Google Scholar]
- Willerman L, Cohen DB. Psychopathology. McGraw Hill; New York: 1990. [Google Scholar]
- Wu EQ, Birnbaum HG, Shi L, Ball DE, Kessler RC, Moulis M, Aggarwal J. The economic burden of schizophrenia in the United States in 2002. Journal of Clinical Psychiatry. 2005;66:1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hough RL, Lau A, Fakhry F, Garland A. Why bother with beliefs? Examining relationship between race/ethnicity, parental beliefs about causes of child problems, and mental health service use. Journal of Consulting and Clinical Psychology. 2005;73:800–807. doi: 10.1037/0022-006X.73.5.800. [DOI] [PubMed] [Google Scholar]