Abstract
Perampanel [2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2-dihydropyridin-3-yl)benzonitrile; E2007] is a potent, selective, orally-active non-competitive AMPA receptor antagonist developed for the treatment of epilepsy. Perampanel has a 2,3’-bipyridin-6’-one core structure, distinguishing it chemically from other AMPA receptor antagonist classes. Studies in various physiological systems indicate that perampanel selectively inhibits AMPA receptor-mediated synaptic excitation without affecting NMDA receptor responses. Blocking of AMPA receptors occurs at an allosteric site that is distinct from the glutamate recognition site. Radioligand binding studies suggest that the blocking site coincides with that of the non-competitive antagonist GYKI 52466, believed to be on linker peptide segments of AMPA receptor subunits that transduce agonist binding into channel opening. As is typical for AMPA receptor antagonists, perampanel exhibits broad-spectrum anti-seizure activity in diverse animal seizure models. Perampanel has high oral bioavailability, dose-proportional kinetics, and undergoes oxidative metabolism, primarily via CYP3A4, followed by glucuronidation. The terminal half-life (t½) in humans is 105 h; however, in the presence of a strong CYP3A4 inducer (such as carbamazepine) the t½ can be reduced. In sum, perampanel is a selective, centrally-acting, negative allosteric modulator of AMPA receptors with good oral bioavailability and favorable pharmacokinetic properties.
Keywords: AMPA receptor antagonist, antiepileptic drug, epilepsy, perampanel
Introduction
AMPA receptors, the major mediators of glutamate-mediated excitatory neurotransmission, are critical for epileptic synchronization and for the spread of epileptic seizures (1). Perampanel is a structurally distinct non-competitive AMPA receptor antagonist. Recent clinical trials have demonstrated that once-daily perampanel is efficacious as adjunctive therapy in the treatment of partial seizures (2, 3, 4, 5). This article describes how perampanel was discovered and summarizes its pharmacological properties.
Discovery of perampanel
Perampanel was built on a chemical template discovered via high-throughput screening (HTS). At the time of initiation of the perampanel discovery program, AMPA receptor antagonists of a variety of structural classes were known (1). The search for new AMPA receptor antagonists was stimulated by the recognition that many competitive AMPA receptor antagonists failed to penetrate the blood–brain barrier, and for compounds such as NBQX that did enter the brain, there were safety concerns due to poor solubility. At the same time, while 2,3-benzodiazepine AMPA receptor antagonists did show good blood–brain barrier penetration, they had modest potency. The objective was to discover structures with improved safety and higher potency. HTS was performed using a [3H]AMPA binding assay to search for compounds that competitively displaced binding at the glutamate recognition site (competitive antagonists). AMPA-induced neuronal cell death in rat primary cortical neuron cultures served as a functional assay of AMPA receptor blockade. To exclude neuroprotective compounds that did not act on the AMPA receptor target, compounds were tested for their ability to inhibit AMPA-induced Ca2+ influx, a more direct assay of AMPA receptor antagonist activity. No promising new compounds were identified with the [3H]AMPA binding assay. However, among hits in the functional assay, 2,4-diphenyl-4H-[1,3,4]oxadiazin-5-one – which showed AMPA receptor blocking activity with an IC50 value of about 5 µM – was selected as the starting point for a medicinal chemistry effort (Figure 1). Initial efforts focused on increasing potency and water solubility, with the aim of creating a drug to be administered intravenously in the treatment of acute stroke. Subsequently, the focus changed to developing a compound with oral efficacy that could be used in the treatment of chronic neurological diseases. This reduced the requirement for water solubility and expanded the options for chemical modification. The core structure 1,3,5-triaryl-1H-pyridin-2-one was identified following this change in strategy. Perampanel [2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2-dihydropyridin-3-yl)benzonitrile hydrate 4:3] (Figure 1) was discovered by optimization of the core structure, mainly focusing on increasing oral efficacy. Although perampanel has very poor solubility in aqueous solution at neutral and alkaline pH, it has a pKa of 3.24 and the charged species dissolves readily at low pH (such as in gastric acid) so that it is completely absorbed from the gastrointestinal tract.
Figure 1.
Structures of 2,4-diphenyl-4H-[1,3,4]oxadiazin-5-one, a low affinity AMPA receptor antagonist, representing the core structure that was optimized to develop perampanel. The colors of the atoms in the conventional structure correspond with those in the 3-dimensional view below.
Perampanel in vitro pharmacology
Perampanel inhibited AMPA-induced increases in intracellular Ca2+ in cultured rat cortical neurons with an IC50 of 93 nM (6). The magnitude of inhibition of AMPA-induced Ca2+ responses was similar with low (2 µM) and high (100 µM) AMPA concentrations, suggesting that perampanel block occurs in a non-competitive fashion. This conclusion was bolstered by patch clamp recordings from cultured rat hippocampal neurons, where perampanel caused a concentration-dependent inhibition of non-desensitizing AMPA receptor currents evoked by kainate that was similar throughout a range of agonist concentrations (7) (Figure 2A). In contrast, for desensitizing AMPA-evoked currents, a modest interaction between AMPA concentration and level of block was observed. Moreover, patch clamp recordings indicated that perampanel had similar affinities for the open and closed states of AMPA receptors and did not affect AMPA receptor desensitization. In contrast to its effect on AMPA receptors, perampanel caused little or no inhibition of NMDA-induced Ca2+ responses (6) or patch clamp currents (7), indicating a high selectivity for AMPA receptors versus NMDA receptors.
Figure 2.
Perampanel block of AMPA receptor currents and synaptic responses (field EPSPs) in hippocampampal neurons. A, AMPA but not NMDA receptor currents are inhibited by perampanel in whole-cell voltage clamp recordings from cultured hippocampal neurons. Currents induced by perfusion with 100 µM AMPA were nearly completely blocked by application of 10 µM perampanel (A1) whereas currents induced by 10 µM NMDA were only minimally affected by 30 µM perampanel (A2). Note that AMPA receptor currents exhibit rapid desensitization whereas NMDA receptor currents do not. From Rogawski et al. (7). B, Field EPSPs were recorded in the stratum radiatum of the CA1 area in hippocampal slices following Schaffer collateral stimulation. Perfusion with 0.3 and 3 µM perampanel causes a concentration dependent inhibition of the synaptic response (B1).Concentration-response relationship for inhibition of the field EPSP giving the concentration for half-maximal inhibition (IC50) (B2). Adapted from Ceolin et al. (8) with permission from Elsevier.
Studies in the hippocampal slice preparation have also demonstrated that perampanel selectively blocks AMPA receptor-mediated synaptic transmission (8) (Figure 2B). Extracellularly recorded field excitatory postsynaptic potentials (EPSPs) evoked in the stratum radiatum of the CA1 area by electrical stimulation of the Schaffer collaterals were inhibited with an IC50 of 0.23 µM and there was complete block at 3 µM. The action of perampanel was not use-dependent. Perampanel was much more potent than the prototypical non-competitive AMPA antagonist GYKI 52466, which inhibited AMPA receptor-mediated field EPSPs with an IC50 of 7.8 µM. As in other preparations where perampanel exhibited selectivity for AMPA receptors, perampanel at a concentration of 10 µM did not affect the component of field EPSPs mediated by NMDA receptors. It also did not affect the kainate receptor-mediated component of EPSPs.
Radioligand binding studies with radiolabelled perampanel support the conclusions drawn from the functional studies. Thus, [3H]perampanel was found to bind to a single high affinity site in rat forebrain membranes with a Kd and Bmax of 59.8 ± 5.2 nM and 3.2 ± 0.1 pmoles/mg, respectively. [3H]Perampanel was not displaced by AMPA, glutamate, kainate, or NBQX, supporting the conclusion that perampanel does not interact with the glutamate recognition site of AMPA receptors. In contrast, the non-competitive AMPA receptor antagonists GYKI 52466 and CP-465,022 did displace [3H]perampanel binding, suggesting that perampanel binds to a similar site on AMPA receptors as these antagonists. Overall, among ionotropic glutamate receptors, perampanel has a high selectivity for AMPA receptors. Radioligand binding studies examining a wide range of receptors, transporters, enzymes and other cellular targets failed to show significant effects on binding at concentrations up to 28.6 µM (Eisai data on file).
Perampanel in vivo pharmacology
As is typical for AMPA receptor antagonists, perampanel exhibited broad-spectrum efficacy in various animal models used to evaluate drugs for anti-seizure activity. It had high potency against audiogenic seizures in DBA/2 and was also effective in the maximal electroshock seizure test, the subcutaneous pentylenetetrazol (PTZ) test, and the 6 Hz seizure test (6) (Table 1). The broad-spectrum activity distinguishes perampanel from sodium channel blocking antiepileptic drugs (AEDs) such as carbamazepine, which are weak or inactive in the PTZ and 6 Hz seizure tests. Many AEDs exhibit reduced potency in the 6 Hz test as the stimulus intensity is increased from 32 mA to 44 mA (9). However, perampanel demonstrated nearly equal potency at the two intensity levels, further reinforcing its distinctive profile. The activity of perampanel in the 6 Hz model was maintained and possibly augmented in the presence of carbamazepine, phenytoin and valproate (6). These observations are consistent with the results of clinical trials that have found adjunctive perampanel to be efficacious in combination with these and other AEDs (2, 3, 4).
Table 1.
Comparison of the efficacy of perampanel in various acute seizure models with other antiepileptic drugs in mice.
| Drug | Audiogenic | MES | PTZ | 6 Hza | Rotarod | ||
|---|---|---|---|---|---|---|---|
| ED50 (mg/kg), p.o. | TD50 (mg/kg) |
||||||
| Carbamazepine | 6.1 | 21 | >100 | 50 (32 mA) | ND | ||
| Sodium valproate |
160 | 460 | 350 | 394 (32 mA) |
ND | ||
| Perampanel | 0.47 | 1.6 | 0.94 | 2.1 (32 mA) 2.8 (44 mA) |
1.8 | ||
ED50, estimated dose at which 50% of animals are protected; MES, maximal electroshock test; p.o., orally; PTZ, pentylenetetrazol seizure test; 6 Hz, 6 Hz seizure test (32 mA or 44 mA stimulation intensity); TD50, estimated dose at which 50% of animals exhibit motor impairment in rotarod test. Drugs were dosed 30 to 60 min prior to testing. In rats, the TD50 value of perampanel is 9.14 mg/kg. Adapted from Hanada et al. (2011) with permission.
Eisai data on file.
Perampanel was also studied in chronic epilepsy models. In rats with limbic-like epilepsy induced by amygdala kindling, perampanel at a dose of 10 mg/kg orally (p.o.) reduced the duration of the electrographic seizure discharge (afterdischarge) evoked by electrical stimulation, and at doses of 5 and 10 mg/kg caused a reduction in the behavioral seizure duration and seizure severity. However, as is the case generally for AMPA receptor antagonists (10), perampanel was inactive in an absence seizure model (genetic absence epilepsy rats from Strasbourg [GAERS]) at doses of 1, 3 and 10 mg/kg, p.o. (6).
As has been observed for other AMPA receptor antagonists (11), there was little or no separation between the doses of perampanel that are effective in the seizure tests and the doses causing motor impairment (Table 1). Given the role of AMPA receptors in mediating excitatory neurotransmission throughout the brain, acute motor toxicity of AMPA receptor antagonists is not unexpected. However, the low therapeutic window for AMPA receptor antagonists in animal models does not necessarily imply reduced tolerability in clinical use compared with other AED classes and perampanel has demonstrated acceptable tolerability in clinical studies (2, 3, 4). As is the case for most other AEDs, increasing doses of perampanel are associated with a dose-dependent increase in reversible adverse effects attributable to impairment of central nervous system functioning.
Perampanel pharmacokinetics
Perampanel exhibited favorable pharmacokinetic properties in experimental animals following oral dosing, although the terminal half-life (t½) was relatively short. Very low metabolic turnover rate in human liver microsomes suggested that perampanel might have a longer t½ in humans and that it might be suitable for once daily dosing (6). Perampanel was therefore selected as a candidate for clinical studies. Perampanel is not a substrate of P-glycoprotein (P-gp) or the breast cancer resistance protein (BCRP), according to studies with human P-gp and BCRP overexpressing cell lines (12). Hence, these blood–brain barrier transporters are unlikely to limit access of perampanel to the brain.
Oral perampanel is rapidly and almost completely absorbed, with low systemic clearance and high relative bioavailability in humans. In line with expectations from the human liver microsome studies, the t½ values in clinical studies ranged from 53 to 136 h (average of 105 h in 19 Phase I studies). In healthy human subjects and in patients with epilepsy treated in clinical trials, perampanel exposure increased linearly with the administered dose over the range of 0.25–12 mg (13). The therapeutic dose range for perampanel is 4–12 mg per day (2, 3, 4). With 14 days of repeat daily dosing in healthy male volunteers, blood levels ranged from 212 to 358 ng/mL (0.61–1.01 µM) with a 4 mg daily dose and from 275 to 456 ng/mL (0.79–1.31 µM) with a 6 mg daily dose. Assuming 95% protein binding (experimental values ranged from 95.3% to 95.8% in humans), free plasma concentrations were 0.03–0.07 µM. Thus, at efficacious doses perampanel concentrations at the receptor would be much lower that the IC50 value for inhibition of neuronal transmission in hippocampal slices, but still within the range of inhibitory effects on AMPA receptor-mediated responses (8). This suggests that a low level of inhibition of AMPA receptors is sufficient for seizure protection, highlighting the importance of AMPA receptors in the generation of epileptic activity (1). Higher levels of inhibition would be expected to result in neurological impairment, given the importance of AMPA receptors in brain function. In the Phase III clinical program, a relationship between dose and clinical response was demonstrated for perampanel doses up to 8 mg; the frequency of treatment-emergent adverse events, most notably dizziness, also increased with dose (4). Pharmacokinetic-pharmacodynamic modeling has indicated that the perampanel plasma concentration is statistically related to the reduction in seizure frequency across the effective dose range (14). There is a decrease in seizure frequency of 0.06% for an increase of 1 ng/mL in perampanel plasma concentration (Eisai data on file). However, the variability in plasma perampanel concentrations was high (132% CV between-subject variability).
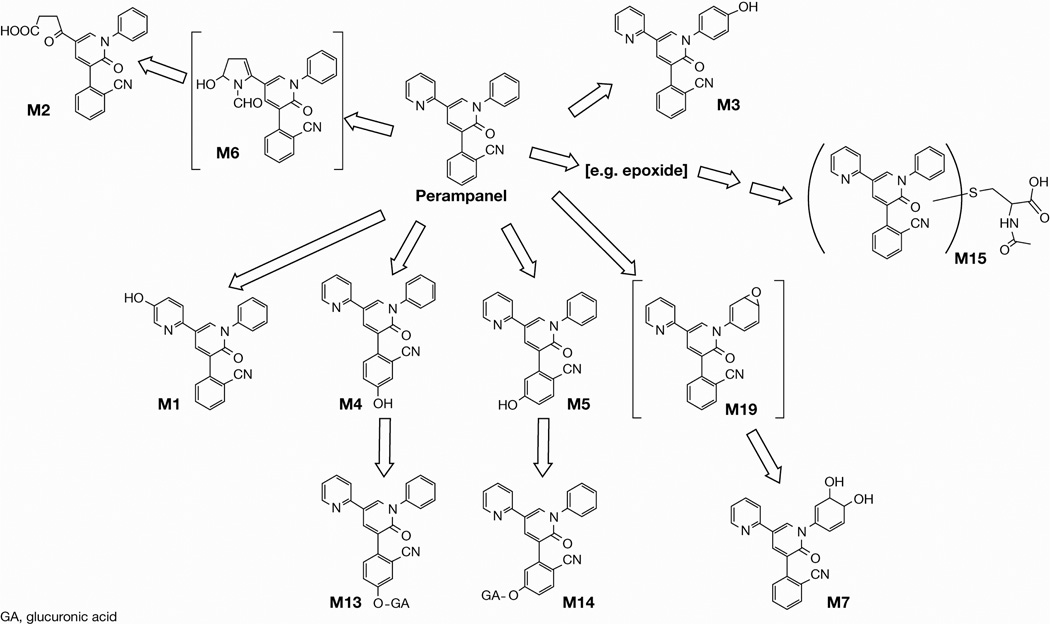
Perampanel is mainly metabolized by CYP3A4 and CYP3A5. The principal metabolic pathways in rats, monkeys, and humans, as illustrated in Figure 3, are (a) ring hydroxylation leading to compounds M1, M3, M4, and M5) and their sequential glucuronides; (b) rearrangement of the pyridine ring to form the carboxylic acid metabolite M2; and (c) the formation of a dihydrodiol metabolite M7 (13). In rats and monkeys, unchanged perampanel was the major component in plasma although small amounts of the metabolites were observed in the circulation. In humans, the quantity of metabolites in the circulation was even lower. Although certain metabolites did inhibit AMPA receptors, their potencies were less than the parent. Thus, M1, M3, M4, M5, and M7, were 44-, 3.0-, 3.8-, 7.7-, and 27-fold weaker respectively than perampanel in the AMPA-induced Ca2+ influx assay. M2 did not inhibit the increase in intracellular calcium up to 10 µM. Considering the observed plasma concentrations of the metabolites and their inhibitory potencies on AMPA receptors, it can be assumed that the contribution of the metabolites to the therapeutic activity of perampanel is negligible.
Figure 3.
Proposed metabolites of perampanel. From Committee for Medicinal Products for Human Use (13).
Conclusions
Perampanel is a potent allosteric inhibitor of AMPA receptors. The evidence to date indicates that the drug is highly selective; no other molecular target has been identified that would likely be substantially affected at therapeutic doses. However, a complete investigation of the activity of perampanel at other ion channel or other non-ion channel targets has not been conducted and further studies to determine effects on non-AMPA receptor targets are required. Additional studies are also required to determine (a) if there is any subunit selectivity among AMPA receptor isoforms; (b) whether auxiliary proteins associated with AMPA receptors such as transmembrane AMPA receptors regulatory proteins (TARPs) influence the activity of perampanel; or (c) if the activity of perampanel is affected by covalent modifications of the receptor, such as phosphorylation. Further investigations are also required to define the binding site for perampanel on AMPA receptors and to understand the allosteric blocking mechanism. Perampanel is the first selective AMPA receptor antagonist to be introduced into clinical practice. Greater understanding of its pharmacology and blocking mechanism will inform future efforts to develop clinical therapeutic agents that target AMPA receptors.
Acknowledgments
We are grateful to D. Squillacote (Eisai Inc.) for comments on the manuscript. D. McGregor (Complete Medical Communications) provided assistance with editing the manuscript for non-intellectual content. M. A. Rogawski has received research support from the National Institute of Neurological Disorders and Stroke (Grants NS072094, NS079202, NS077582) and Eisai Inc.
Footnotes
Conflict of interest
M. A. Rogawski has served as a consultant to Eisai Inc. and T. Hanada is an employee of Eisai Co., Ltd.
References
- 1.Rogawski MA. AMPA receptors as a molecular target in epilepsy therapy. Acta Neurol Scand. 2013;127(Suppl 197):9–18. doi: 10.1111/ane.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.French JA, Krauss GL, Biton V, Squillacote D, Yang H, Laurenza A, Kumar D, Rogawski MA. Adjunctive perampanel for refractory partial-onset seizures: Randomized phase III study 304. Neurology. 2012;79:589–596. doi: 10.1212/WNL.0b013e3182635735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.French JA, Krauss GL, Steinhoff BJ, Squillacote D, Yang H, Kumar D, Laurenza A. Evaluation of adjunctive perampanel in patients with refractory partial-onset seizures: Results of randomized global phase III study 305. Epilepsia. 2013;54:117–125. doi: 10.1111/j.1528-1167.2012.03638.x. [DOI] [PubMed] [Google Scholar]
- 4.Krauss GL, Serratosa JM, Villanueva V, Endziniene M, Hong Z, French J, Yang H, Squillacote D, Edwards HB, Zhu J, Laurenza A. Randomized phase III study 306: adjunctive perampanel for refractory partial-onset seizures. Neurology. 2012;78:1408–1415. doi: 10.1212/WNL.0b013e318254473a. [DOI] [PubMed] [Google Scholar]
- 5.Kerling F, Kasper B. Efficacy of perampanel: a review of clinical trial data. Acta Neurol Scand. 2013;127(Suppl 197):25–29. doi: 10.1111/ane.12101. [DOI] [PubMed] [Google Scholar]
- 6.Hanada T, Hashizume Y, Tokuhara N, Takenaka O, Kohmura N, Ogasawara A, Hatakeyama S, Ohgoh M, Ueno M, Nishizawa Y. Perampanel: a novel, orally active, noncompetitive AMPA-receptor antagonist that reduces seizure activity in rodent models of epilepsy. Epilepsia. 2011;52:1331–1340. doi: 10.1111/j.1528-1167.2011.03109.x. [DOI] [PubMed] [Google Scholar]
- 7.Rogawski MA, Chen C-Y, Matt L, Hell JW. Blocking mechanism of the APMA receptor antagonist perampanel. Epilepsy Curr. 2013;13(Suppl 1) Abs 1.013. [Google Scholar]
- 8.Ceolin L, Bortolotto ZA, Bannister N, Collingridge GL, Lodge D, Volianskis A. A novel anti-epileptic agent, perampanel, selectively inhibits AMPA receptor-mediated synaptic transmission in the hippocampus. Neurochem Int. 2012;61:517–522. doi: 10.1016/j.neuint.2012.02.035. [DOI] [PubMed] [Google Scholar]
- 9.Barton ME, Klein BD, Wolf HH, White HS. Pharmacological characterization of the 6 Hz psychomotor seizure model of partial epilepsy. Epilepsy Res. 2001;47:217–227. doi: 10.1016/s0920-1211(01)00302-3. [DOI] [PubMed] [Google Scholar]
- 10.KamińSki RM, Van Rijn CM, Turski WA, Czuczwar SJ, Van Luijtelaar G. AMPA and GABAB receptor antagonists and their interaction in rats with a genetic form of absence epilepsy. Eur J Pharmacol. 2001;430:251–259. doi: 10.1016/s0014-2999(01)01393-0. [DOI] [PubMed] [Google Scholar]
- 11.Yamaguchi S, Donevan SD, Rogawski MA. Anticonvulsant activity of AMPA/kainate antagonists: comparison of GYKI 52466 and NBQX in maximal electroshock and chemoconvulsant seizure models. Epilepsy Res. 1993;15:179–184. doi: 10.1016/0920-1211(93)90054-b. [DOI] [PubMed] [Google Scholar]
- 12.Hibi S, Ueno K, Nagato S, Kawano K, Ito K, Norimine Y, Takenaka O, Hanada T, Yonaga M. Discovery of 2-(2-oxo-1-phenyl-5-pyridin-2-yl-1,2-dihydropyridin-3-yl)benzonitrile (perampanel): a novel, noncompetitive α-amino-3-hydroxy-5-methyl-4-isoxazolepropanoic acid (AMPA) receptor antagonist. J Med Chem. 2012;55:10584–10600. doi: 10.1021/jm301268u. [DOI] [PubMed] [Google Scholar]
- 13.Committee For Medicinal Products For Human Use. Fycompa (perampanel) assessment report. European Medicines Agency 424476. 2012 [Google Scholar]
- 14.Laurenza A, Ferry J, Hussein Z. Population pharmacokinetics and pharmacodynamics of perampanel: a pooled analysis from three phase III trials. Epilepsy Curr. 2012;12(Suppl 1) Abs 2.231. [Google Scholar]