Abstract
Those impacted by the loss of a loved one to violent death (i.e., homicide, suicide, or accident) may be at risk for posttraumatic stress, depression, and prolonged grief. Restorative Retelling (RR) is a structured group intervention developed to improve coping skills, integrate commemoration of the deceased, and approach traumatic memories. This paper provides initial evidence for the utility of RR in reducing trauma, depression, and prolonged grief symptoms in a records review open trial of 51 violent loss survivors at a community counseling clinic. Results suggested that RR was well tolerated with a significant decrease in symptoms.
Keywords: violent loss, grief therapy, group therapy, complicated bereavement
As many as 30% of Americans have lost a loved one to a violent death - an accident, suicide, or homicide (Norris, 1992). Survivors of violence loss are at increased risk for a variety of psychological symptoms and disorders including post-traumatic stress disorder (PTSD), depression, and substance abuse (Amick-McMullan, Kilpatrick, & Resnick, 1991; Zinzow et al, 2009) as well as prolonged grief (Lobb et al., 2010), a psychiatric disorder characterized by separation distress (e.g., yearning for the deceased), and associated symptoms (Shear et al., 2011). These psychological symptoms and disorders may persist at elevated rates for years after the death (Murphy et al., 1999).
Complicated grief, depression, and PTSD are not only common after surviving a violent loss, but they are also commonly co-occurring. For example, among outpatients who had experienced the loss of a loved one, 25% of those with depression versus 2.8% of nondepressed individuals had a diagnosis of comorbid prolonged grief (Sung et al., 2011). Similarly, among individuals seeking treatment for prolonged grief, major depressive disorder, and PTSD are commonly comorbid conditions; of individuals with prolonged grief, just over 50% had depression and 30% had PTSD (Melhem et al., 2001). This common co-occurrence suggests that for many people, it would be useful to provide treatments that target the various symptoms after violent loss.
Rynearson (2001) found that survivors of violent loss commonly report repetitive, intrusive thoughts and images of the loved one’s (which most survivors of violent loss did not witness first hand). These thoughts and images are highly distressing, as the violent dying defies loved ones’ assumptions of a continuing, caring relationship. These intrusive thoughts, in Rynearson’s (2001; 2012) view, lead survivors to mentally undo or compensate for the loss through thoughts of revenge, reunion, or remorse. All of these thought processes complicate efforts at integrative the loss into a coherent, meaningful narrative that is logically consistent with the relationship that previously existed between deceased and survivor (see also Currier, Holland, & Neimeyer, 2006). For Rynearson (2001; 2012), critical to rebuilding a meaningful life after violent loss is both the development of a meaningful, coherent narrative that simultaneously highlights the meaningfulness of the deceased person’s life and relationship with the survivor, and contextualizes and de-centers the imagined scene of the violent dying.
Current Treatment Approaches for Violent Loss Survivors
Current literature on the impact of violent loss suggests the need for bereavement intervention. Treatments for survivors of violent loss have roots in both professional psychological treatment and nonprofessional (peer) support services. Peer support groups for the bereaved provide emotional support and interaction with others who have knowledge and experience in situations similar to one's own. In one study of a representative sample of parents who had lost a child to a violent death, a sizable minority of mothers (30%) and fathers (21%) attended support groups 4 months after the loss (Murphy, Johnson, Lohan, & Tapper, 2002). Individuals who attended the support groups tended to be more distressed than individuals who did not attend them. At follow-up 5 years after the loss, there was no difference in distress level between individuals who attended the groups and individuals who did not. This was interpreted as evidence against the effectiveness of support groups, but given that support group attenders were more distressed at baseline, the comparability of their distress to that of the non-attenders 5 years later may indicate support group effectiveness. When asked directly 5 years after the loss, parents listed support groups as one of the 3 most helpful resources that they had in getting through their grief. However empirical evidence on the effectiveness of support groups is mixed (Videka-Sherman & Lieberman 1985).
Professionally led groups are situated to provide the combination of the emotional support of peers who undergone similar experiences while also providing the benefits of professional leadership, for example the establishment of structure, goals, and expert guided interventions to reach those goals. Murphy and her colleagues (1998) developed and tested a structured group treatment for parents who had lost a child to violent death. In a randomized controlled trial testing the treatment, they contacted bereaved parents from a list of death certificates (i.e., recruited regardless of whether they were experiencing distress or psychopathology) and asked them to participate. The group treatment consisted of 10 two-hour sessions each session combined a psychoeducation and skill building component with an opportunity for members to share with and provide support to each other. This treatment, compared to the no treatment control condition, reduced the symptoms of grief and emotional distress among the more highly distressed mothers but not among the less distressed mothers. This is consistent with other evidence that intervention is only useful for those bereaved people who have significant psychological symptoms following the loss (Neimeyer & Currier, 2009).
Newer treatments have aimed more specifically at survivors presenting with elevated PTSD symptoms after violent death bereavement. Two research groups have now examined the effectiveness of group treatment approaches for adolescents exposed to traumatic events and bereavement. One intervention is a 20-week structured approach that involves distress-management (psychoeducation, coping skills); trauma processing (reviewing the traumatic experience and exploring its meaning); promotion of healthy grief (e.g., processing anger, and reconstruction of a “nontraumatic” image of the deceased) (Layne et al., 2001; Saltzman, Pynoos, Layne, Steinberg, Aisenberg, 2001). Treatment participants experienced reductions in PTSD symptoms, complicated grief, and (in the case of Layne et al 2001) depressive symptoms as well as improvements in grades. These results suggest that a group treatment that includes elements aimed at reducing general distress and PTSD symptoms, and promoting healthy grief, can effectively reduce symptoms of PTSD and complicated grief in survivors of traumatic events. A follow up efficacy trial also supports this group therapy having greater benefits than a psychoeducation and skills training intervention, though both produced reductions in PTSD and depression symptoms (Layne et al., 2008).
Salloum and Vincent (1999) described a similar group for adolescents who have survived the homicide death of a loved one. The group, based in schools, consisted of 10 sessions including psychoeducation, coping, sharing feelings, coping with PTSD symptoms and anger management. In a pilot study, adolescent participants experienced a reduction of PTSD symptoms from pre- to post-test (Salloum, Avery, & McClain, 2001). Limited research has been conducted on examining structured bereavement focused group interventions for adults who have experienced violent loss.
Restorative Retelling
Restorative retelling (RR; Rynearson, 1998, 2001; Rynearson & Correa, 2008) is a structured, 10-session intervention for adult survivors of violent deaths. The treatment mode underlying the intervention conceptualizes non-recovery from violent death of a loved one as involving a combination of separation distress and trauma distress. The intervention includes elements aimed at stabilization, including relaxation training and commemoration of the life of the deceased through sharing of positive memories. This commemoration may also help relieve separation distress by promoting the establishment of a positive continuing bond. The trauma distress is conceptualized as centering around imagined “reenactments” (i.e. flashbacks, intrusive images, dreams) of the loved one’s dying (Rynearson & McCreary, 1993). RR addresses these traumatic stress symptoms via an exercise in which participants draw the scene of the dying and share the drawing and the story of the dying with other group members. Groups range in size from 6 to 10 members. Therapists protect the safety of the group environment by screening for high levels of traumatic stress and personality disorder, and referring these individuals for individual treatment prior to or instead of group treatment.
Given the paucity of research on bereavement interventions specifically targeting various symptoms experienced by violent loss survivors, evaluating developed interventions that are currently being implemented would advance knowledge within the grief field. When conducting treatment outcome research, the goals of Phase 1 trials are to determine the safety, feasibility, acceptability, and potential effectiveness of a treatment. Initial studies typically are in the form pilot open trials. The current paper presents results from the first empirical investigation of restorative retelling, conducted in a records review open trial of a community setting sample.
This effectiveness trial aims to test one acceptability and two effectiveness hypotheses. First, we hypothesized that group members would find the intervention acceptable as evidenced by a high completion rate. Second, we hypothesized that post-RR participants would report fewer depressive, avoidance, intrusion, and complicated grief symptoms. Third, we hypothesized that baseline symptom severity would moderate change in symptoms over the course of treatment such that treatment would be effective for survivors who have a high level of symptoms, but not for those who have fewer symptoms.
Method
Participants
Initially, we reviewed records of 118 violent death survivors. These records included all survivors who had lost a loved one to violent death, were seeking counseling services for bereavement issues, and were provided with the RR group treatment at a community grief counseling center between 1998-2011. Of these 118, four did not complete the treatment. Of note, the completion rate for Murphy’s (1998) adult violent loss treatment package was 90%, suggesting that the RR treatment is acceptable to violent loss survivors compared to only other existing adult group program (Hypothesis 1).
Of the 114 treatment completers, 63 were excluded: 20 because of significant missing data (i.e., at least three measures, or half the necessary data, missing); 7 because they were couples or mother/daughter pairs in the same treatment group; and 36 records because they were receiving concurrent individual therapy or were recently prescribed psychiatric medications at the time of group. The final sample was 51 participants. Table 1 describes their characteristics.
Table 1.
Participants’ demographic characteristics.
| Characteristic | Mean or Frequency (SD or %) |
n answering question |
|---|---|---|
| Women | 37 (72.5%) | 51 |
| Age | 44.84 (13.35) | 51 |
| Race/Ethnicity | 51 | |
| European-American | 37 (72.5%) | |
| African-American | 4 (7.8%) | |
| Hispanic | 8 (15.7%) | |
| Other | 2 (3.9%) | |
| Highest level of education | 51 | |
| Graduate school | 7 (13.7%) | |
| College | 24 (47.1%) | |
| High school | 18 (35.3%) | |
| Junior high | 2 (3.9%) | |
| Means of death | 51 | |
| Homicide | 41 (80.4%) | |
| Suicide | 6 (11.8%) | |
| Accident | 4 (7.8%) | |
| Relationship to the deceased | 51 | |
| Parent | 15 (29.4%) | |
| Romantic partner | 6 (11.8%) | |
| Child | 11 (21.6%) | |
| Sibling | 8 (15.7%) | |
| Other relative | 8 (15.7%) | |
| Relationship quality | 2.85 (2.05) | 49 |
| Months since loss - mean | 51.59 (126.92) | 51 |
| Months since loss - median | 6 (range .5-664) | 51 |
| Saw scene of death | 19 (37.3%) | 49 |
Note. Unless otherwise specified, data are means for continuous variables and counts for categorical variables; numbers in brackets represent standard deviation for continuous variables and percent of total sample for categorical variables.
Treatment Package
Restorative Retelling was developed to treat distress and grief responses of violent death survivors within a group therapy context. Its aims are to provide members with skills to manage grief related distress as well as techniques to approach distressing thoughts and images about the violent loss that survivors may avoid or endure with significant distress. Thus, RR teaches stress reduction and relaxation strategies. Members were encouraged to share the life stories of their loved ones as well as retell the violent death story. Treatment was delivered in 10 weekly sessions.
Community therapists
Therapists who conducted groups were either one of the RR developers or directly trained and supervised by one of the RR developers. There were 14 therapists leading the RR groups. Six were psychiatrists and eight were master’s level clinicians. Eleven were women. Therapist training consisted of reading the RR manual and viewing video-taped group sessions, as well as co-leading at least one group with an experienced RR therapist. All therapists participated in a weekly 2-hour group supervision meeting during the time they were leading groups.
Treatment exclusion criteria
RR therapists offered individual rather than group treatment for individuals who had a current, severe psychiatric disorder that would make it difficult to focus exclusively on issues related to violent loss in a short-term group. Also excluded from the group and offered individual treatment were individuals who had severe personality disorders given the risk that these individuals would behave in ways that would interfere with group cohesion. Finally, some individuals who would otherwise have been eligible for participation in RR did not want to be in a group, and were therefore not included.
Measures
Beck Depression Inventory –A (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) is a 21-item self-report scale, is among the most widely used instruments to measure depression. Each item contains four statements reflecting current manifestations of depression in increasing intensity, from neutral (e.g., "I am not particularly discouraged about the future.") to severe (e.g., "I feel that the future is hopeless and that things cannot improve."). Each item is scored 0 to 3 and total scores range from 0 to 63, with higher scores indicating greater depressive severity. Of the 21 items on the scale, 13 are primarily psychological in nature, 8 are primarily somatic. Beck and Steer (1984) and Gallagher, Nies, and Thompson (1982) demonstrated that the BDI has high internal consistency (α=.86 and α=.91, respectively).
Impact of Events Scale (IES & IES-R Horowitz, Wilner, & Alvarez, 1979; Weiss & Marmar, 1996) is a 15-item self-report measure of distress due to avoidance and intrusion. The IES-R is a 22-item scale that contains hyperarousal as well. For both scales, items are rated on a 5-point scale from 0 (“not at all”) to 4 (“extremely”). In the current sample, both measures showed high reliability (αs > .90).
Inventory of Traumatic Grief (ITG: Prigerson et al.,1995) is a 33-item measure that includes questions related to rating of symptoms based upon the contruct of complicated grief on a Likert scale ratings. This measure provides both diagnosis of complicated grief as well as a total intensity score (ranging from 9: no symptoms, to 45: extreme symptoms). Assessed are Criterion A (separation distress); Criterion B (other symptoms such as difficulty with the following: accepting the death, trusting others, experiencing feelings other than numbness, moving on; as well as feeling: bitter, as though life were meaningless, as though the future holds no purpose, and on edge); and Criterion C (Impairment in functioning). Given data collection within the community clinic occurred over several years, several versions of the ITG were utilized as revisions became available (original 33 items, revised 34 items, re-revised 37 items. The ITG had high reliability (α = .90) in this sample.
Demographics & loss characteristics
At pre-treatment, demographics and characteristics related to the death were collected, which included survivor gender, age, race/ethnicity, marital status, education, and relationship to the deceased. Information about the deceased were collected including gender, age at time of death, time since loss, type of loss, whether survivor witnessed death or found deceased. Relationship quality was also assessed which included items assessing 5 aspects (closeness, peacefulness, ease, supportiveness, and compatibility) rated on a likert scale of 1-10 (1 = most positive and 10 = least positive). Reliability for this scale is high; α=.89 in this sample. As Table 1 shows, the average of 2.85 (SD = 2.02) indicated that participants generally reported having good relationships with the deceased.
Procedure
Survivors were contacted by outreach or were referred by community service providers or mental health workers. They sought assistance for intense distress following the violent death of a close friend or family member. It should be emphasized that only a tiny minority of community members spontaneously seeks psychological assistance, so these participants represent a biased sub sample of the community who were highly distressed by the violent death (Rynearson, 1995).
All participants were assessed in a semi-structured, individual interview to provide requisite crisis support, while clinically judging the presence of co-morbidity and consideration of psychiatric consultation before enrollment in the RR group intervention. After agreeing to an intervention, each completed a questionnaire that included a detailed account of the dying, an assessment of their relationship with the deceased, and demographic and historical data on each participant before the violent death. All participants then completed the pretreatment assessment battery (BDI, ITG, and IES/IES-R). Survivors participated in a weekly 1 ½ hour RR group treatment for 10 sessions. Groups averaged 6-8 members per group. The same measures were repeated at end of the intervention.
All records for RR group members during 1998-2011 were reviewed, and de-identified data were entered in an SPSS database. Given this was records review of a community-based sample, we anticipated a higher rate of missing data than a research based sample. To remain conservative in managing missing data of certain items but allow for inclusion of participants who completed pre and post assessments, we handled missing data in the following manner: For the ITG, BDI-A, and IES: if there were 1-3 items left unanswered (which was the case in a minority of participants), values for these items were imputed using the NORM program for multiple imputation (Schafer, 1997). For the BDI-A, we noticed that some participants (nine at pre-assessment and nine at post-assessment) did not complete page two (included 6 items) resulting in these participants having a BDI that was only 16 items long. Thus, we include these people and pro-rated their BDI scores.
Results
The 51 participants who were in included in the analyses had a mean baseline BDI score of 19.25 (SD=12.08, median = 17.00), indicative of mild to moderate depressive symptoms. This level of depression symptom severity is comparable to the level of depression symptoms present in other survivors of violent loss presenting for RR treatment (M=19.4, SD=11.3, Rynearson et al., 2008) and in a community sample of survivors of homicide (M=15.43, SD=11.27; Burke, Neimeyer, & McDevitt-Murphy, 2010).
In terms of intrusion and avoidance, participants’ mean level of IES avoidance symptoms was 11.92 (SD=1.04, median= 11.04), a symptom level comparable to symptoms in other survivors of violent loss presenting for RR treatment (M=15.8 SD=8.2, Rynearson et al., 2008). However, our sample’s avoidance symptom level was significantly lower than a small group of highly distressed survivors of violent loss who agreed to treatment when contacted by homicide support services (M=24.2, SD=7.6), and more comparable to treatment refusers from the same study (M=9.8, SD=8.0, Rynearson, 1995). The avoidance symptoms were significantly less than those reported by individuals seeking psychological treatment subsequent to a stressful life event such as the death of a loved one (for women, M=42.1 SD=16.7, for men, M=35.3, SD=22.6, Horowitz et al., 1979). The mean level of intrusion symptoms on the IES was 14.84 (SD=4.69, median = 14.98), again more comparable to treatment-refusing survivors of violent loss (M=15.3, SD=8.4) than treatment-seeking survivors of violent loss (M=29.4, SD=6.3), or individuals seeking psychological treatment subsequent to a stressful life event such as the death of a loved one (for women, M=21.4, SD=8.6; for men, M=21.2, SD=12.5).
Participants’ average score on ITG items was 2.75 (SD=.84, median = 2.56), higher than the average in one previous sample of treatment-seeking individuals who had a violent loss (M=1.96, SD=.77; Rynearson et al., 2008), and within a standard deviation of the average score in a second sample of individuals seeking treatment for emotional difficulties following the death of a loved one (M=3.05, SD=.64; Boelen, van den Bout, & Keijser, 2003).
To test for symptom reduction in depressive, avoidance, intrusion, and traumatic grief symptoms), repeated measures ANOVAs were conducted for each symptom score with time (pre- versus post-testing) as the within-subjects variable. As Table 2 shows, symptoms decreased over the course of treatment depressive, intrusion, and traumatic grief symptoms, but not for avoidance.
Table 2.
Means and Standard Deviations for outcome measures.
| Measure | Pre- treatment M (SE) |
Post- treatment M (SE) |
Significance test |
Partial η2
effect size |
|---|---|---|---|---|
| Beck Depression Inventory | 19.32 (1.77) | 13.21 (1.36) | F(1,47)=13.64* | .23 |
| Impact of Events Scale | ||||
| Avoidance | 11.92 (1.04) | 10.48 (1.04) | F(1,39)=1.59 | .04 |
| Intrusion | 14.84 (4.69) | 11.83 (6.16) | F(1,36)=10.35* | .22 |
| Inventory of Traumatic Grief | 2.72 (.14) | 2.38 (.13) | F(1,36)=19.30* | .35 |
Note. Numbers are estimated marginal means where time since loss is 51.21 months. Scores on the Inventory of Traumatic Grief are item averages; scores for all other measures are total scores.
p<.005
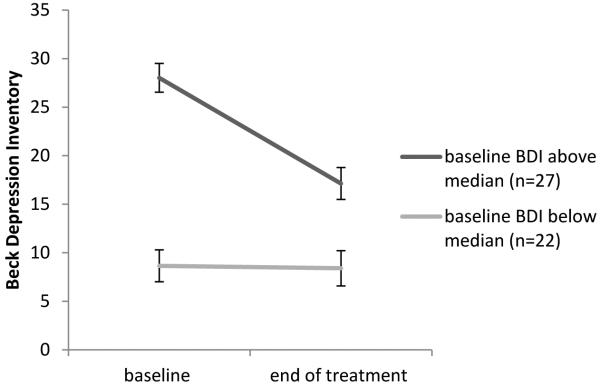
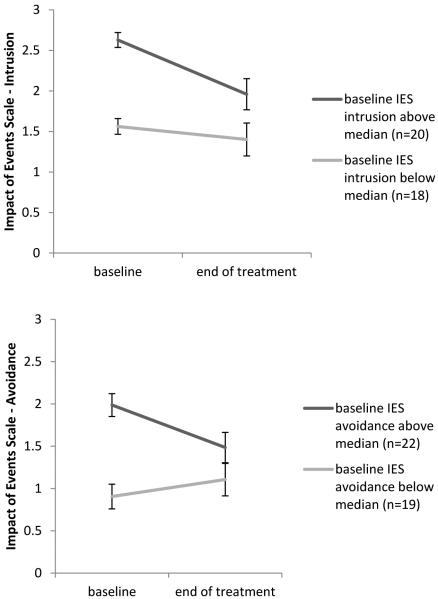
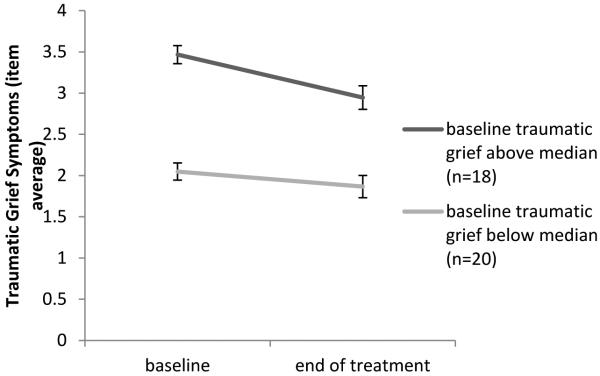
Too see if individuals with more severe symptoms at baseline would experience greater decreases in symptoms over the course of treatment than individuals with less severe symptoms at baseline, repeated measures ANOVAS were conducted with time as the within-subjects variable, pre-treatment symptoms (above or below the median) as the between-subjects variable, and time since loss as a covariate. There were significant symptom severity X time interaction effect for depressive symptoms, F(1, 46)=15.45, p < .001, partial η2 = .25. (Figure 1); avoidance symptoms, F(1, 38)=7.85, p = .008 (see Figure 2a), partial η2 = .17; and traumatic grief symptoms, F(1, 35)=4.96, p = .032, partial η2 = .12 (See Figure 3). There was a marginally significant symptom severity X time interaction effect for intrusion, F(1, 35)=3.99, p = .054 (see Figure 2b), partial η2 = .10. For each of these variables, those above the median improved over time, but those below the median did not change significantly.
Figure 1.
Change in depressive symptoms from baseline to end of treatment as a function of baseline depressive symptoms.
Figures 2a &2b.
Change in intrusive symptoms (above) and avoidance symptoms (below) from baseline to end of treatment as a function of baseline symptoms.
Figure 3.
Change in traumatic grief symptoms from baseline to end of treatment as a function of baseline traumatic grief symptoms.
Discussion
Results from this open trial suggest that RR is potentially an effective intervention for adults seeking treatment for bereavement following a loved one’s violent death. These preliminary results are promising for directing future treatment outcome trials given limited research has been conducted in this area. Findings from this study suggest that RR is associated with decreased depression symptoms, diminished avoidance, and less prolonged grief reactions. These results are consistent with similar findings for other structured coping skills and exposure-based treatments for traumatic loss (e.g., Layne et al., 2001; Salloum, et al., 2001). However, previous studies focused on adolescent populations. Present results indicate that adults, too, can benefit from RR. Interestingly, the only trauma cluster that was not impacted by RR was avoidance symptoms. Of note, the baseline mean for this subscale was fairly low, indicating a possible floor effect for this subset of symptoms. Further, RR appears to ameliorate symptoms for those survivors who reported higher levels of distress at baseline. These results suggest that RR may be an effective treatment approach for those survivors more severely impacted by their loss.
In addition to overall decreased symptoms, the majority of participants who attended the first session completed the group intervention, indicating that the intervention is well tolerated. Findings from this open trial are consistent with results from a trial by Murphy and colleagues (1998) of a similar group treatment that targets increasing coping skills and activities to approach emotional avoidance of trauma distress after violent loss (Murphy et al., 1998). In addition, several recent interventions utilize an individual format and have focused on prolonged grief response for general loss (e.g., Acierno et al., 2012; Shear, 2006; Shear & Mulhare, 2008). RR is unique in that it is provided in a group format, providing additional benefit of emotional support, and is focused solely on loss by violent death.
Strengths to this open trial include the large sample size for an open trial pilot study. Positive results were found even though this was a community-based sample, suggesting a high potential effectiveness of the treatment. Limitations for this study should be noted. This was a records review of a community sample; therefore, there were significant missing data and change in measure administration. As is typical in community clinics, the therapists’ adherence to the treatment protocol was not assessed. There are limitations to the generalizability of the findings to populations different from the current sample. Although participants were comparable to other treatment-seeking samples in their level of depression and complicated grief, they had relatively low levels of traumatic stress symptoms; this may especially dilute treatment results for traumatic stress symptoms. Survivors who had more significant symptoms were more likely referred for additional individual counseling or medication intervention and therefore not included in these analyses. It is unclear if RR would be helpful for the more distressed individual. The majority of participants were White, non-Hispanic women; thus, these results may not be generalizable to men and members of non-White racial groups or individuals of Hispanic ethnicity. Similarly, the majority of survivors in this sample were survivors of homicide; therefore, it is unclear whether the results generalize to survivors of accidental or suicidal violent losses.
Finally, given that this was an open trial there was no comparison group. Positive treatment results may have been a function of improvements made because of time or regression to the mean. Although participants were excluded from analysis if they were concurrently enrolled in additional formal psychiatric or psychological treatment, we did not assess or exclude for individuals’ involvement with or participation in non-professional sources of help such as support groups. For these reasons, the true causality of outcomes cannot be made beyond initial inference.
This is a first step in understanding the potential efficacy of RR for trauma and grief symptoms related to violent loss. RR is a brief structured group intervention that is well tolerated and potentially effective in decreasing distress related to violent loss. A gold standard randomized control trial would prove useful to determine RR’s efficacy in improving trauma distress, depression symptoms, and prolonged grief reactions. Future randomized control trials should incorporate long term follow-up assessment and clearer inclusion and exclusion criteria. Future research with larger sample sizes could further examine the impact of RR on symptoms reduction as moderated by characteristics of the loss and survivor, for example, types of loss, quality and type relationship with the deceased.
Acknowledgments
This research was supported by South Carolina Clinical & Translational Research Institute voucher award (NIH/NCRR#UL1RR029882, voucher #3013-5057 PI: Rheingold).
References
- Acierno R, Rheingold A, Amstadter A, Kurent J, Amella E, Resnick H, Muzzy W, Lejuez C. Behavioral activation and therapeutic exposure (BA-TE) for bereavement in older adults. American Journal of Hospice and Palliative Medicine. 2012;29:13–25. doi: 10.1177/1049909111411471. [DOI] [PubMed] [Google Scholar]
- Amick-McMullan A, Kilpatrick DG, Resnick HS. Homicide as a risk factor for PTSD among surviving family members. Behavior Modification. 1991;15:545–559. doi: 10.1177/01454455910154005. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. Journal of Clinical Psychology. 1984;40:1365–1367. doi: 10.1002/1097-4679(198411)40:6<1365::aid-jclp2270400615>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Burke LA, Neimeyer RA, McDevitt-Murphy ME. African-American homicide bereavement: Aspects of social support that predict complicated grief, PTSD, and depression. Omega. 2010;61:1–24. doi: 10.2190/OM.61.1.a. [DOI] [PubMed] [Google Scholar]
- Currier JM, Holland JM, Neimeyer RA. Sense-making, grief, and the experience of violent loss: Toward a meditational model. Death Studies. 2006;30:403–428. doi: 10.1080/07481180600614351. [DOI] [PubMed] [Google Scholar]
- Gallagher D, Nies G, Thompson L. Reliability of the Beck Depression Inventory with Older Adults. Journal of Consulting and Clinical Psychology. 1982;50:152–153. doi: 10.1037//0022-006x.50.1.152. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosomatic Medicine. 1979;41:209–18. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Jordan JR, McMenamy J. Interventions for Suicide Survivors: A Review of the Literature. Suicide and Life-Threatening Behavior. 2004;34:337–349. doi: 10.1521/suli.34.4.337.53742. [DOI] [PubMed] [Google Scholar]
- Kaltman S, Bonanno GA. Trauma and bereavement: Examining the impact of sudden and violent deaths. Journal of Anxiety Disorders. 2003;17:131–147. doi: 10.1016/s0887-6185(02)00184-6. [DOI] [PubMed] [Google Scholar]
- Layne CM, Saltzman WR, Poppleton L, Burningame GM, Pasalic A, Durakovic-Belko E, Pynoos RS. Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1048–1062. doi: 10.1097/CHI.0b013e31817eecae. [DOI] [PubMed] [Google Scholar]
- Layne CM, Pynoos RS, Saltzman WR, Arslanagic B, Black M, Saviak N, Popovic T, Durakovic E, Music M, Campara N, Djapo N, Houston R. Trauma and grief-focused group psychotherapy: School-based postward intervention with traumatized Bosnian adolescents. Group Dynamic-Theory Research and Practice. 2001;5:277–290. [Google Scholar]
- Lobb EA, Kristjanson LJ, Aoun SM, Monterosso L, Halkett GKB, Davies A. Predictors of complicated grief: a systematic review of empirical studies. Death Studies. 2010;34:673–698. doi: 10.1080/07481187.2010.496686. [DOI] [PubMed] [Google Scholar]
- Meert KL, Shear K, Newth CJ, Harrison R, Berger J, Zimmerman J, Nicholson C. Follow-up study of complicated grief among parents eighteen months after a child’s death in the pediatric intensive care unit. Journal of Palliative Medicine. 2011;14:207–214. doi: 10.1089/jpm.2010.0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Rosales C, Karageorge J, Reynolds CF, Frank E, Shear KM. Comorbidity of axis I disorders in patients with traumatic grief. Journal of Clinical Psychiatry. 2001;62:884–887. doi: 10.4088/jcp.v62n1108. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Johnson C, Cain KC, Das Gupta A, Dimond M, Lohan J, Baugher R. Broad-spectrum group treatment for parents bereaved by the violent deaths of their 12- to 28-year-old children: A randomized controlled trial. Death Studies. 1998;22:209–235. doi: 10.1080/074811898201560. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Das Gupta A, Cain KC, Johnson LC, Lohan J, Wu L, Mekwa J. Changes in parents mental distress after the violent death of an adolescent or young adult child: a longitudinal prospective analysis. Death Studies. 1999;23:129–159. doi: 10.1080/074811899201118. [DOI] [PubMed] [Google Scholar]
- Murphy SA, Johnson LC, Lohan J, Tapper VJ. Bereaved parents’ use of individual, family, and community resources 4 to 60 months after a child’s violent death. Family and Community Health. 2002;25:71–82. doi: 10.1097/00003727-200204000-00010. [DOI] [PubMed] [Google Scholar]
- Neimeyer RA, Currier JM. Grief therapy: Evidence of efficacy and emerging directions. Current Directions in Psychological Science. 2009;18:352–356. [Google Scholar]
- Norris FH. Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Maciejewski’ PK, Reynolds CF, Bierhals AJ, Newsom JT, Fasiczka’ A, Miller M. Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research. 1995;59:65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- Rynearson EK, McCreery JM. Bereavement after homicide: A synergism of trauma and loss. American Journal of Psychiatry. 1993;150:258–261. doi: 10.1176/ajp.150.2.258. [DOI] [PubMed] [Google Scholar]
- Rynearson EK. Bereavement after homicide: A comparison of treatment seekers and refusers. British Journal of Psychiatry. 1995;166:507–510. doi: 10.1192/bjp.166.4.507. [DOI] [PubMed] [Google Scholar]
- Rynearson EK. Retelling Violent Death. Brunner/Routledge; Philadelphia: 2001. [Google Scholar]
- Rynearson EK. Accommodation to violent dying: A guide to restorative retelling and support. 1998 Unpublished manuscript. [Google Scholar]
- Rynearson EK. The Narrative dynamic of grief after homicide. Omega. 2012;65:239–249. doi: 10.2190/OM.65.3.f. [DOI] [PubMed] [Google Scholar]
- Rynearson EK, Correa F. Accommodation to violent dying: A guide to restorative retelling and support. 2008. Unpublished manuscript.
- Salloum A, Vincent NJ. Community-based groups for inner city adolescent survivors of homicide victims. Journal of Child and Adolescent Group Therapy. 1999;9:27–45. [Google Scholar]
- Salloum A, Avery L, McClain RP. Group psychotherapy for adolescent survivors of homicide victims: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1261–1267. doi: 10.1097/00004583-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Saltzman WR, Pynoos RS, Lane CM, Steinberg AM, Eisenberg E. Trauma and grief focused intervention for adolescents exposed to community violence: Results of a school-based screening and treatment protocol. Group dynamics: Theory, research, and practice. 2001;5:291–301. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. Chapman & Hall; London: 1997. [Google Scholar]
- Shear MK. The treatment of complicated grief. Grief Matters. 2006;9:39–42. [Google Scholar]
- Shear MK, Mulhare EM. Complicated grief. Psychiatric Annals. 2008;38:662–670. [Google Scholar]
- Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, Keshaviah A. Complicated grief and related bereavement issues for DSM-5. Depression and Anxiety. 2011;28:103–117. doi: 10.1002/da.20780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung SC, Dryman MT, Marks E, Shear MK, Ghesquiere A, Fava M, Simon NM. Complicated grief among individuals with major depression: prevalence, comorbidity, and associated features. Journal of Affective Disorders. 2011;134:453–458. doi: 10.1016/j.jad.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Videka-Sherman L, Lieberman M. The effects of self-help and psychotherapy intervention on child loss: The limits of recovery. American Journal of Orthopsychiatry. 1985;55:70–82. doi: 10.1111/j.1939-0025.1985.tb03422.x. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma and PTSD: A Practitioner’s Handbook. Guilford Press; New York: 1997. pp. 399–411. [Google Scholar]
- Zinzow HM, Rheingold AA, Hawkins AO, Saunders BE, Kilpatrick DG. Losing a loved one to homicide: prevalence and mental health correlates in a national sample of young adults. Journal of Traumatic Stress. 2009;22:20–27. doi: 10.1002/jts.20377. [DOI] [PMC free article] [PubMed] [Google Scholar]