Abstract
Objective
To assess fertility desires by availability and use of ART/PMTCT services in Rakai, Uganda.
Design
Retrospective analyses of longitudinal data from the Rakai Community Cohort Study.
Methods
Study participants were retrospectively identified and categorized by HIV status. Availability of antiretroviral therapy and prevention of mother-to-child transmission (ART/PMTCT) services in Rakai was defined in three periods: 1) Pre-ART/PMTCT (<2005), 2) ART/PMTCT rollout (2005-06), and 3) universal ART/PMTCT (>2006); and use of ART/PMTCT was coded as yes if the woman received services. Trends in fertility desires were assessed by chi-square. “Modified” Poisson regression was performed using generalized linear models with a log link and Poisson family to estimate prevalence rate ratios (PRR) and 95% confidence intervals of desire for another child among previously and currently pregnant women; PRR were adjusted for demographic and behavioral factors.
Results
4,227 sexually active women in Rakai, including 436 HIV+ women, contributed 13,970 observations over 5 survey rounds. Fertility desires increased in the population in the ART/PMTCT rollout (adjusted PRR: 1.08, CI: 1.04-1.13) and the universal availability periods (adj. PRR: 1.11, CI: 1.08-1.14) compared to pre-ART/PMTCT period. A total of 862 woman observations used ART/PMTCT services. Fertility desires were similar among ART/PMTCT service users and non-users in cross-sectional analysis (adj. PRR: 0.84, CI: 0.62-1.14) and one year after ART/PMTCT use (adj. PRR: 1.27, CI: 0.83-1.94).
Conclusion
Availability of ART/PMTCT may increase fertility desires of previously pregnant women in Rakai, Uganda. Use of ART/PMTCT services was not correlated with fertility desires of previously or current pregnant women.
Keywords: HIV, pregnancy intentions, fertility, prevention of mother-to-child transmission, Uganda
Introduction
Sub-Saharan Africa is the region most severely impacted in the human immunodeficiency virus (HIV) epidemic, with 68% of the global HIV burden and 92% of pregnant women living with HIV residing in this region [1-2]. The World Health Organization (WHO) advocates a comprehensive four-pronged strategy for the prevention of mother-to-child transmission (PMTCT) of HIV, which emphasizes improved integration of HIV and reproductive health services so as to reduce both levels of unwanted pregnancies and mother-to-child transmission (MTCT) among HIV positive women [3-4]. Preventing unintended pregnancies is a cost-effective strategy for reducing MTCT and can improve maternal health outcomes [5-6].
With a total fertility rate (TFR) of 6.2, Uganda has one of the highest fertility rates worldwide and more than half of pregnancies among Ugandan women are unintended [7-8]. Unmet need for family planning is high in Uganda, with 34.5% of women who wish to delay or avoid pregnancy not using any contraceptive method [7], and studies have shown higher unmet need for contraceptives among HIV-positive women compared to HIV-negative women in rural Uganda [9,10]. Concurrently, an estimated 7% of Ugandan adults are living with HIV, and MTCT remains a leading cause of new HIV infections in Uganda, where an estimated 20% of new HIV cases result from vertical transmission of HIV [7, 11]. Furthermore, availability of PMTCT services is improving in Uganda and currently 45% of HIV positive women are using antiretroviral therapy (ART) as a component of PMTCT [2].
Increasing availability of ART and PMTCT services throughout sub-Saharan Africa may influence fertility intentions and sexual behavior among women in this region, but the association between ART/PMTCT and fertility desires has not been determined. Previous studies examining fertility desires of women using ART for HIV treatment found that ART users had higher fertility desires than non-users [12-13]. However, a recent meta-analysis showed that ART use was not associated with fertility desires of people living with HIV [14]. ART initiation may also change pregnancy rates among HIV positive women, as both a previous Rakai study and an assessment of the multi- country MTCT Plus Initiative showed higher incidence rates of pregnancy among women using ART [15-16].
This study aims to fill critical knowledge gaps in understanding how ART/PMTCT availability and use may influence fertility desires among a rural population. Most previous studies of fertility desires among women who accessed PMTCT were cross-sectional or qualitative. Our open cohort study design enabled us to measure fertility desires of women over time as ART/PMTCT services became more widely available in Rakai, Uganda, and also to determine the effect of use or non-use of these services on subsequent fertility desires of HIV positive women. This approach was utilized to assess population and individual level trends in fertility desires.
Methods
Study Design
Retrospective analyses of longitudinal data were performed among a cohort of women who were part of the Rakai Community Cohort Study (RCCS) survey Rounds 9-13 between July 2002 and December 2009. The RCCS is a community-based open cohort study that annually enrolls and follows up with consenting participants (15-49 years) through in-person interviews in the Rakai District of Uganda. RCCS methods have been described previously in more detail [17-18].
We excluded women from the analyses if they had never been pregnant, were not sexually active during the past 12 months, had a tubal ligation, or had a partner or partners who reported vasectomy or infertility. Only women with complete demographic and behavioral baseline data were included in the analyses.
We examined the outcome of fertility desires among previously and currently pregnant women. Fertility desires were defined by whether or not a woman desired an additional child. To assess fertility desires, the previously pregnant women in the analyses were asked, ‘would you like to have another child?’ and currently pregnant women were asked, ‘after the birth of the child you are expecting would you want to have any more children?’. Women who responded ‘yes’ to either question were categorized as desiring another child, while we classified women who responded ‘no’ or ‘undecided’ as not desiring another child.
The main covariates were ART/PMTCT availability in the Rakai community and use of ART/PMTCT. Availability of ART/PMTCT services was defined by three time periods: pre-ART/PMTCT, before March 2005 when the first woman in the cohort registered for PMTCT services; ART/PMTCT rollout, between March 2005 and March 2006; and universal ART/PMTCT availability, after March 2006. Use of ART/PMTCT was defined as either a.) Enrollment in the Rakai ART program before or during pregnancy, or b.) Registration for PMTCT services during pregnancy. Prior to September 2007, only single dose nevirapine (sdNVP) was available for PMTCT. During the later portion of the study period, pregnant women who accessed PMTCT in Rakai received combined ART prophylaxis with zidovudine (AZT) initiated at 28 gestational weeks, sdNVP with lamivudine (3TC) at the onset of labor, and postpartum 3TC and AZT [19]. Along with HIV care and treatment services, the following are also offered at no cost to all HIV positive women: free family planning counseling, condoms, and long-acting reversible contraceptive methods, including hormonal contraceptives, diagnosis and treatment of STIs, education about HIV and STI prevention, violence counseling and referral to services that were not available at the clinic [20].
The analyses were adjusted for age, categorized as 15-19, 20-24, 25-29, 30-39 and 40-49 years; education defined as never attended school, primary school (1-7 years of education), and secondary school or higher (8 or more years of education); current marital status was categorized as not married, monogamous marriage if husband had one wife, or polygamous marriage if husband had two or more wives. Current pregnancy status, elapsed time since last pregnancy (<1 year, 1-2 years, >2 years), and study follow-up visit number were also included in the adjusted models.
We adjusted for HIV status, classified as HIV-positive, HIV-negative, and unknown serostatus. Two different enzyme immunoassays (EIA) were used to determine HIV status (Vironostika HIV-1, OrganonTeknika, Charlotte, North Carolina, USA, and Cambridge Biotech, Worcester, Massachusetts, USA), and all sero-conversions and discordant test results were confirmed using Western blot (HIV-1 WB Bio-Merieux–Vitek, St Louis, Missouri, USA). Behavioral covariates in the model were sex with a non-marital partner within the past 12 months; current hormonal contraceptive use, including use of oral contraceptive pills, implants, or injectable contraceptives; and current condom use. These covariates were all self-reported.
Statistical Methods
At baseline, t-tests and Pearson's chi-squared tests were used to compare the demographic and behavioral characteristics of women by desire for another child. We calculated unadjusted and adjusted prevalence rate ratios (PRR) for fertility desires and corresponding 95% confidence intervals (CI) through “modified” Poisson regression using generalized linear models with a log link, Poisson family and robust estimation of variance. We controlled for clustering so as to obtain robust standard errors because individual participants had repeated observations. We used PRR as a measure of association between fertility desires among all previously pregnant women and availability of ART/PMTCT services. In the adjusted analysis, we controlled for marital status, education level, age, availability of ART/PMTCT services, reported sex with a non-marital partner, HIV status, time since last pregnancy, use of hormonal contraceptive, condom use and study follow-up visit. Analyses were performed for the entire study population, and also stratified by HIV status. All the models assessed interaction between ART/PMTCT availability and follow- up visit specific HIV status. In the sub-analysis, we determined the rate of fertility desires among HIV+ women who had been exposed to ART/PMTCT in the previous study visit. STATA 12.0 software package was used to conduct the analyses.
Results
A total of 4,227 eligible women were enrolled in this study, contributing 13,970 woman observations throughout the study period. At baseline, 55.2% of previously pregnant women desired another child, while 37.2% of the 436 HIV-positive women in the study population desired another child.
Table 1 summarizes baseline characteristics associated with desire for more children among previously pregnant women. HIV-positive women were significantly less likely to desire another child compared with HIV-negative women (6.7% versus 14.5%, p<0.001). Approximately 32.2% of women reported current use of condoms, and this did not differ by reported fertility desires (p=0.5). However, current hormonal contraceptive users were less likely to desire another child (25.5% yes, 31.4% no, p<0.001). On average, women who desired another child were younger than women who did not desire another child (mean: 25.5 years vs. mean: 34.0 years, p<0.001), had a higher education level (28.1% attended secondary school or higher vs. 19.9%, p<0.001), and were more likely to be married (93.3% vs. 80.2%, p<0.001) and in a monogamous marriage (75.6% vs. 55.1%, p<0.001). Desire for a child in the future decreased with duration of time since last pregnancy; 46.3% of women who were pregnant during the past year desired another child, 30.8% of women who were pregnant within the past 1-2 years, 14.1% if pregnant within the past 2-3 years, and 8.9% if more than 3 years ago (chi-squared for trend, p<0.001). At baseline, women who reported sex with a non-marital partner within the past 12 months were less likely to desire another child (7.0% vs. 18.0%, p<0.001). At baseline, HIV-infected women who desired another child were significantly younger (p<0.001), more likely to be married (p<0.001), less likely to report a non-marital sexual partner (p<0.001), less likely to report hormonal contraceptive use (p=0.02), and more likely to have been pregnant within the previous 2 years (p<0.001) as compared to HIV-infected women who did not desire another child. Education level (p=0.2) and condom use (p=0.09) did not significantly differ between HIV-infected women who desired another child and those who did not.
Table 1. Baseline Characteristics of Previously or Currently Pregnant Women in Rakai from 2002-2009 (N=4,227 women) and Previously Pregnant HIV+ women (N=436 women), By Desire for Another Child.
| Overall Study Population (N=4,227 women) | HIV+ women (N=436 women) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Demographics | Desire Another Child (N=2,331) |
Do
Not Desire Another Child (N=1,896) |
p-value | Total (N=4,227) |
Desire Another Child (N=162) |
Do
Not Desire Another Child (N=274) |
p-value | Total (N=436) |
| Age Group (years) - % | ||||||||
| 15-19 | 10.1 | 0.6 | <0.001 | 5.8 | 7.4 | 0.4 | <0.001 | 3.0 |
| 20-24 | 42.1 | 9.1 | 27.3 | 35.2 | 8.0 | 18.1 | ||
| 25-29 | 29.1 | 23.7 | 26.7 | 33.3 | 31.8 | 32.3 | ||
| 30-39 | 16.6 | 42.3 | 28.1 | 22.8 | 48.9 | 39.2 | ||
| >40 | 2.0 | 24.3 | 12.0 | 1.2 | 11.0 | 7.3 | ||
| Education Level - % | ||||||||
| No Schooling | 6.7 | 10.6 | <0.001 | 8.5 | 7.4 | 6.2 | 0.2 | 6.7 |
| Primary School Only | 65.2 | 69.5 | 67.2 | 66.1 | 74.1 | 71.1 | ||
| Secondary School or Higher | 28.1 | 19.9 | 24.4 | 26.5 | 19.7 | 22.3 | ||
| Marital Category - % | ||||||||
| Not Married | 6.7 | 19.8 | <0.001 | 12.6 | 17.9 | 40.9 | <0.001 | 32.3 |
| Monogamous Marriage | 75.6 | 55.1 | 66.4 | 61.7 | 39.1 | 47.5 | ||
| Polygamous Marriage | 17.6 | 25.1 | 21.0 | 20.4 | 20.1 | 20.2 | ||
| HIV Sero-Status - % | ||||||||
| HIV-positive | 6.7 | 14.5 | <0.001 | 10.3 | 100% | 100% | N/A | 100% |
| HIV-negative | 90.9 | 81.8 | 86.8 | 0% | 0% | 0% | ||
| Unknown | 2.2 | 3.7 | 2.9 | 0% | 0% | 0% | ||
| Current Non-Marital Sex Partner - % | ||||||||
| Yes | 7.0 | 18.0 | <0.001 | 11.9 | 16.7 | 34.7 | <0.001 | 28.0 |
| Current Use of Hormonal Contraceptives - % | ||||||||
| Yes | 25.5 | 31.4 | <0.001 | 28.2 | 21.0 | 31.0 | 0.02 | 27.3 |
| Current Use of Condom - % | ||||||||
| Yes | 31.8 | 32.7 | 0.5 | 32.2 | 48.2 | 56.6 | 0.09 | 53.4 |
| Time Since Last Pregnancy - % | ||||||||
| <1 year | 46.3 | 29.4 | <0.001 | 38.7 | 34.6 | 23.0 | <0.001 | 27.3 |
| 1-2 years | 30.8 | 20.8 | 26.3 | 32.7 | 24.8 | 27.8 | ||
| 2-3 years | 14.1 | 18.2 | 15.9 | 14.2 | 15.7 | 15.1 | ||
| >3 years | 8.9 | 31.6 | 19.1 | 18.5 | 36.5 | 29.8 | ||
Table 2 summarizes the unadjusted and adjusted prevalence rate ratios (adj. PRR) of desiring another child among previously pregnant women in a cross-sectional analysis during the three periods of ART/PMTCT availability. Desire for another child was significantly higher during the ART/PMTCT rollout period (adj. PRR: 1.08, CI: 1.04-1.13) and universal ART/PMTCT availability (adj. PRR: 1.11, CI: 1.08-1.14) relative to the before ART/PMTCT services were available in Rakai. Among HIV-positive women, desire for another child significantly increased during the ART/PMTCT rollout period (adj. PRR: 1.34, CI: 1.10-1.63); there was no significant change during the universal ART/PMTCT period (adj. PRR: 1.16, CI: 0.97-1.39), as compared to the period with no ART/PMTCT services. Within the overall study population, HIV-positive women were significantly less likely to desire another child than HIV-negative women (adj. PRR: 0.79, CI: 0.74-0.84).
Table 2. Unadjusted and Adjusted Prevalence Rate Ratios (PRR) of Desire for Another Child Among Previously Pregnant Women (N=4,227 women with 13,970 observations) and HIV+ Previously Pregnancy Women (N=436 women with 862 observations) in Rakai.
| Overall Study Population (N=4,227 women) | HIV+ women (N=436 women) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |||||
|
| ||||||||
| Demographics | PRR | 95% CI | PRR | 95% CI | PRR | 95% CI | PRR | 95% CI |
| Availability of ART/PMTCT | ||||||||
| No ART/PMTCT (<2005) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| ART/PMTCT Rollout (2005-2006) | 0.97 | 0.93-1.01 | 1.08 | 1.04-1.13 | 1.19 | 0.96-1.48 | 1.34 | 1.10-1.63 |
| Universal ART/PMTCT (>2006) | 0.89 | 0.86-0.92 | 1.11 | 1.08-1.14 | 0.91 | 0.75-1.11 | 1.16 | 0.97-1.39 |
| Age Group (years) - % | ||||||||
| 15-19 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 20-24 | 0.90 | 0.87-0.93 | 0.87 | 0.84-0.91 | 0.87 | 0.66-1.14 | 0.97 | 0.78-1.20 |
| 25-29 | 0.69 | 0.66-0.72 | 0.67 | 0.64-0.70 | 0.48 | 0.35-0.66 | 0.56 | 0.43-0.74 |
| 30-39 | 0.37 | 0.35-0.39 | 0.37 | 0.34-0.39 | 0.24 | 0.18-0.34 | 0.29 | 0.22-0.40 |
| >40 | 0.09 | 0.07-0.10 | 0.08 | 0.07-0.10 | 0.10 | 0.05-0.21 | 0.12 | 0.06-0.24 |
| Ever Attended School | ||||||||
| Yes | 1.34 | 1.19-1.52 | 1.05 | 0.96-1.16 | 0.96 | 0.60-1.53 | 1.13 | 0.76-1.68 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Currently Married | ||||||||
| Yes | 1.87 | 1.68-2.09 | 1.52 | 1.35-1.71 | 1.80 | 1.37-2.37 | 1.77 | 1.16-2.71 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| HIV-Positive | ||||||||
| Yes | 0.59 | 0.53-0.65 | 0.79 | 0.74-0.84 | N/A | N/A | N/A | N/A |
| No | 1.00 | 1.00 | 86.8 | N/A | N/A | N/A | N/A | |
| Current Non-Marital Sex Partner - % | ||||||||
| Yes | 0.62 | 0.56-0.68 | 1.19 | 1.07-1.32 | 0.62 | 0.47-0.81 | 1.53 | 1.02-2.30 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Current Use of Hormonal Contraceptives - % | ||||||||
| Yes | 0.92 | 0.87-0.96 | 0.82 | 0.78-0.85 | 0.69 | 0.53-0.89 | 0.70 | 0.55-0.89 |
| No | 1.00 | 0.92 | 0.88-0.95 | |||||
| Current Use of Condom - % | ||||||||
| Yes | 0.94 | 0.90-0.99 | 0.92 | 0.88-0.95 | 0.73 | 0.60-0.88 | 0.72 | 0.61-0.85 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Time Since Last Pregnancy - % | ||||||||
| <1 year | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 1-2 years | 0.99 | 0.95-1.03 | 1.10 | 1.06-1.14 | 0.86 | 0.69-1.07 | 0.99 | 0.81-1.22 |
| 2-3 years | 0.82 | 0.78-0.86 | 1.15 | 1.10-1.20 | 0.77 | 0.62-0.96 | 1.03 | 0.83-1.27 |
| >3 years | 0.43 | 0.40-0.46 | 1.05 | 0.98-1.13 | 0.46 | 0.34-0.61 | 0.99 | 0.74-1.32 |
Adjusted for: availability of ART/PMTCT services, marital status, education level, age, HIV status, sex with non-marital partner, use of HC, condom use, and time since last pregnancy
In the entire population, women who reported current use of condoms (adj. PRR: 0.82, CI: 0.78-0.85) or hormonal contraceptives (adj. PRR: 0.92, CI: 0.88-0.95) had significantly lower fertility desires. While HIV-positive condom users (adj. PRR: 0.70, CI: 0.55-0.89) and hormonal contraceptive users (adj. PRR: 0.72, CI: 0.61-0.85) were also less likely to desire another child. Married women were significantly more likely to report desiring another child (overall adj. PRR: 1.52, CI: 1.35-1.71; HIV+ adj. PRR: 1.77, CI: 1.16-2.71). Compared to 15 to 19 year old women, fertility desires decreased in older age groups (20-24 years, adj. PRR: 0.89; 25-29 years, adj. PRR: 0.68; 30-39 years, adj. PRR: 0.37; 40-49 years, adj. PRR: 0.10). Among the entire study population and the subset of HIV-positive women, those who reported a current non-marital sexual partnership, had significantly lower fertility desires in the unadjusted model (overall unadj. PRR: 0.62, CI: 0.56-0.68; HIV+ unadj. PRR: 0.62, CI: 0.47-0.81). The adjusted model showed that women in a non-marital sexual partnership were more likely to desire an additional child (overall, adj. PRR: 1.19, CI: 1.07-1.32; HIV+, adj. PRR: 1.53, CI: 1.02-2.30). Fertility desires did not differ by education level (overall, adj. PRR: 1.05, CI: 0.96-1.16; HIV+, adj. PRR: 1.13, CI: 0.76-1.68). Among HIV-positive women, the number of years since a previous pregnant did not influence fertility desires (1-2 years, adj. PRR: 0.99, CI: 0.81-1.22; 2-3 years, adj. PRR: 1.03, CI: 0.83-1.27; >3 years, adj. PRR: 0.99, CI: 0.74-1.32). Overall, women who had been pregnant within the past 1-2 years (adj. PRR: 1.10, CI: 1.06-1.14) or 2-3 years (adj. PRR: 1.15, CI: 1.10-1.20) were more likely to desire an additional child than women who had been pregnant within the past year.
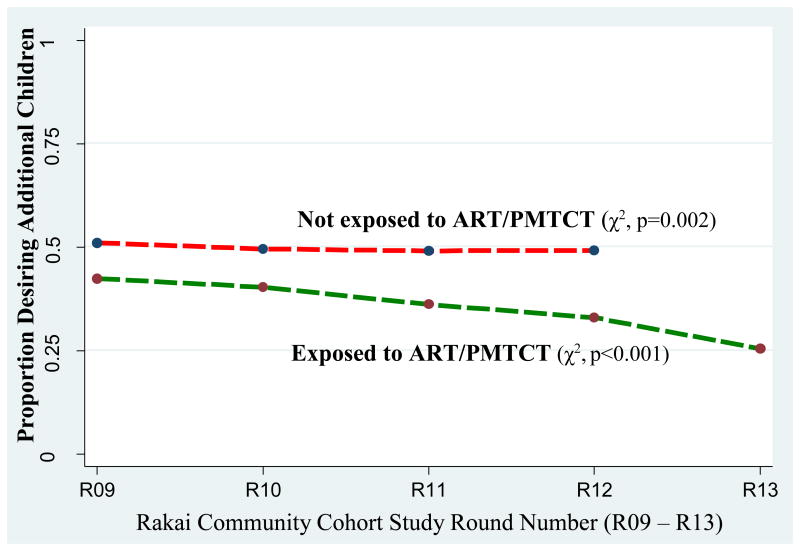
Figure 1 illustrates the trends in desiring a future child by exposure to ART/PMTCT services. Women who did not use ART/PMTCT had approximately a 50% chance of desiring another child, which decreased over time (p=0.002). A larger proportion of women exposed to ART/PMTCT services at the first survey visit desired another child compared to women who access ART/PMTCT during their fourth visit (p<0.001).
Figure 1. Trends in Fertility Desires by Exposure to ART/PMTCT.
Table 3 displays unadjusted and adjusted prevalence rate ratios of desiring another child among previously or currently pregnant HIV-positive women who reported use of ART/PMTCT during a current or previous interview in the RCCS. In the cross-sectional analysis when use of ART/PMTCT and desire for another child were both ascertained at the same visit, we observed no difference in fertility desires of women by use of ART/PMTCT services, (adj. PRR: 0.84, CI: 0.62-1.14). The factor associated with lower probability of desire for another child was being over 25 years relative to 15-19 years old (25-29 years, adj. PRR=0.40, CI: 0.24-0.65; 30-39 years, adj. PRR=0.25, CI: 0.14-0.43; >40 years, adj. PRR=0.06, CI: 0.02-0.19).
Table 3. Unadjusted and Adjusted Prevalence Rate Ratios (PRR) of Desire for Another Child Among HIV+ Previously and Currently Pregnant Women in Rakai who ever used ART/PMTCT services from 2002-2009.
| Demographics | At Time of Current Interview (N=862) | At Subsequent Interview (N=533) | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |||||
|
| ||||||||
| PRR | 95% CI | PRR | 95% CI | PRR | 95% CI | PRR | 95% CI | |
| Used ART/PMTCT Services | ||||||||
| Yes | 0.66 | 0.50-0.86 | 0.84 | 0.62-1.14 | 0.86 | 0.58-1.28 | 1.27 | 0.83-1.94 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Age (years) | ||||||||
| 15-19 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 20-24 | 0.91 | 0.60-1.39 | 0.96 | 0.62-1.48 | 0.63 | 0.33-1.20 | 0.57 | 0.30-1.08 |
| 25-29 | 0.38 | 0.24-0.60 | 0.40 | 0.24-0.65 | 0.32 | 0.16-0.65 | 0.27 | 0.13-0.55 |
| 30-39 | 0.24 | 0.15-0.37 | 0.25 | 0.14-0.43 | 0.20 | 0.10-0.40 | 0.16 | 0.07-0.34 |
| >40 | 0.06 | 0.02-0.17 | 0.06 | 0.02-0.19 | - | - | - | - |
| Married | ||||||||
| Yes | 1.76 | 1.19-2.60 | 1.65 | 0.89-3.05 | 1.26 | 0.76-2.11 | 0.58 | 0.31-1.07 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Ever Attended School | ||||||||
| Yes | 0.85 | 0.46-1.57 | 0.93 | 0.59-1.46 | 0.84 | 0.35-2.00 | 0.76 | 0.37-1.57 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Current Non-Marital Sex Partner | ||||||||
| Yes | 0.65 | 0.44-0.95 | 1.38 | 0.77-2.47 | 0.67 | 0.40-1.13 | 0.56 | 0.31-1.02 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Time Since Last Pregnancy | ||||||||
| <1 year | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 1-2 years | 0.92 | 0.65-1.32 | 0.98 | 0.70-1.38 | 0.95 | 0.58-1.54 | 1.11 | 0.70-1.75 |
| 2-3 years | 0.75 | 0.54-1.02 | 1.17 | 0.83-1.66 | 0.88 | 0.55-1.39 | 1.33 | 0.82-2.17 |
| Currently Pregnant | ||||||||
| Yes | 1.07 | 0.77-1.49 | 0.75 | 0.54-1.04 | 0.95 | 0.62-1.45 | 0.78 | 0.49-1.22 |
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Study Follow-Up Visit Number | ||||||||
| 1 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 2 | 0.82 | 0.60-1.12 | 0.80 | 0.66-1.20 | 1.00 | 0.67-1.51 | 1.05 | 0.70-1.57 |
| 3 | 0.93 | 0.69-1.26 | 1.24 | 0.92-1.67 | 1.09 | 0.73-1.63 | 1.25 | 0.84-1.85 |
| 4 | 0.78 | 0.57-1.08 | 1.12 | 0.78-1.60 | 0.63 | 0.37-1.05 | 0.73 | 0.42-1.28 |
| 5 | 0.49 | 0.32-0.75 | 0.89 | 0.52-1.50 | - | - | - | - |
Adjusted for: use of ART/PMTCT services, study follow-up visit number, marital status, education level, age, sex with non-marital partner, pregnancy status, and time since last pregnancy
In the prospective analysis, we determined the effect of ART/PMTCT use on desire for another child during the follow-up visit among the HIV-positive women. Use of ART/PMTCT services was not significantly associated with desire for another child at the subsequent visit (adj. PRR=1.27, CI: 0.83-1.94). Older women had a lower prevalence of desiring another child at the subsequent visit relative to 15-19 year olds (25-29 years, adj. PRR=0.27, CI: 0.13-0.55; 30-39 years, adj. PRR=0.16, CI: 0.07-0.34).
Discussion
Reproductive health decision making among HIV positive women is influenced by numerous environmental and individual level factors [21]. Our study provided evidence that use of ART/PMTCT services did not influence the fertility desires of HIV-positive women in Rakai, Uganda, despite family planning counseling and reproductive health services being an integral part of PMTCT in Rakai. Our results corroborated a recent meta-analysis, which showed that ART use was not associated with fertility desires of people living with HIV [14].
Our longitudinal analysis showed that after adjusting for ART/PMTCT use, pregnancy status was not correlated with fertility desires as currently and previously pregnant women had the same likelihood of desiring an additional child. When comparing the cohort of women who used ART/PMTCT service to non-users, we found that the probability that a woman desired an additional child decreased over time (Figure 1). ART/PMTCT users interviewed during survey Round 13 were less likely to desire a child than women who used these services in Round 9.
Our results also showed population-level trends that fertility desires of previously pregnant women became higher throughout the seven year study period in Rakai, as women were more likely to report desire for another child during the ART/PMTCT rollout and Universal ART/PMTCT periods. This may be correlated with increasing availability of ART/PMTCT services; however, the subset of HIV-positive women reported higher fertility desires during the ART/PMTCT rollout period but not the Universal ART/PMTCT period. Overall, HIV positive women in our study were significantly less likely to report a desire for having an additional child.
Reproductive health decision making and fertility desires of HIV positive women may differ due to a woman's individual health beliefs as well as contextual factors. Fear of adverse maternal health outcomes associated with pregnancy, as well as concerns about MTCT could reduce fertility desires among HIV positive women [22-25]. However, women who are well-informed about PMTCT and believe that it is effective in reducing MTCT may be more likely to desire and plan for a future pregnancy [26-28]. Perceived health status may also impact fertility intentions, as a previous study found that women who believed they would be able to care for a child were more likely to want one [12, 29]. Patient-provider interactions, attitudes of sexual partners, and cultural norms may further influence fertility desires. Qualitative research shows that HIV positive women rarely talk to service providers about their fertility desires and providers often have negative views of pregnancy among HIV-infected individuals; therefore, women are less likely to desire a child if their service provider disapproves or stigmatizes them [12, 23-24, 30-31]. It may be important that service providers interacting with women during ART initiation or PMTCT services are trained in providing empathetic care and offering family planning counseling to all women.
Fertility desires may be a significant predictor of future pregnancies among HIV-positive women [15]. In our study, women who reported current use of hormonal contraceptives or condoms were less likely to desire another child; however, an estimated two-thirds of women in our Rakai cohort who did not wish to have another child were not using condoms or hormonal contraceptives for limiting or spacing a birth. Similarly, women in Uganda have a high unmet need for modern contraceptives [7]. While ART/PMTCT availability in the community may increase fertility desires, it is essential that the reproductive needs of all women are met. ART/PMTCT services may also provide an opportunity to strengthen family planning services and improve access to hormonal contraceptives and reproductive health services for women who wish to limit their fertility [32]. The associations between availability and use of PMTCT with integrated family planning services and hormonal contraceptive use are unclear, but availability of these services has increased contraceptive use among women in some sub-Saharan African settings [33-35]. Strengthening of family planning services during ART/PMTCT may have implications for reducing unintended pregnancies and decreasing MTCT, and may lessen the trend of increasing fertility desires of women with improved availability of PMTCT services with ART.
Our findings are subject to some limitations. We relied on self-reported data for current hormonal contraceptive use, condom use for HIV/STI prevention or family planning, and non-marital sexual partnerships which is subject to social desirability bias. Due to missing data, we could not control for the total number of births, total number of pregnancies, and pregnancy spacing intentions in the analyses; these factors did not significantly impact fertility desires in a similar prospective cohort study [26]. Our results may not be generalizable to other rural sub-Saharan African settings where levels of ART/PMTCT availability and use may differ. However, these results were consistent with previous findings [14]. Most previous studies of fertility desires among women who accessed PMTCT were cross-sectional or qualitative. Our open cohort study design enabled us to measure fertility desires throughout the process of PMTCT rollout in Rakai, Uganda. Despite these limitations, out study was one of the first to longitudinally measure fertility desires among currently and previously pregnant women by use of ART/PMTCT services.
While fertility desires increased over time within our study population, use of ART or PMTCT services did not significantly change fertility desires of previously pregnant women in Rakai, Uganda. As integrated HIV, family planning and maternal health programs are implemented across sub-Saharan Africa, we believe it is valuable to continue to examine the implications that service availability may have on fertility desires of women. A better understanding of fertility desires and pregnancy intentions may inform strategies for meeting the reproductive health care needs of women in rural settings in sub-Saharan Africa.
Acknowledgments
National Institutes of Health (NINR: 5R01NR011474-03), Bill and Melinda Gates Foundation, grant # 22006.03, grants #U1AI51171 and 1UO1AI075115-O1A1 from the National Institutes of Health, Division of Allergy and Infectious Diseases.
Footnotes
Presented At: IAS Conference on HIV Pathogenesis, Treatment and Prevention, Kuala Lumpur, Malaysia, 1 July 2013
Financial Disclosures: The authors have no financial relationships relevant to this article to disclose.
References
- 1.Joint United Nations Programme on HIV/AIDS. World AIDS Day Report. UNAIDS. 2011 Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/jc2216_worldaidsday_report_2011_en.pdf.
- 2.Joint United Nations Programme on HIV/AIDS. World AIDS Day Report 2012. UNAIDS. 2012 Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/JC2434_WorldAIDSday_results_en.pdf.
- 3.World Health Organization. Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infections in Infants: Recommendations for a Public Health Approach. World Health Organization. 2010 Available at: http://whqlibdoc.who.int/publications/2010/9789241599818_eng.pdf. [PubMed]
- 4.Reynolds HW, Janowitz B, Wilcher R, et al. Contraception to prevent HIV-positive births: current contribution and potential cost savings in PEPFAR countries. Sex Transm Infect. 2008;(Suppl 2):ii49–53. doi: 10.1136/sti.2008.030049. [DOI] [PubMed] [Google Scholar]
- 5.Guttmacher Institute. Unintended Pregnancies and Abortion in Uganda. In Brief Series. 2013;2013(2):1–8. [PubMed] [Google Scholar]
- 6.Sweat MD, O'Reilly KR, Schmid GP, et al. Cost-effectiveness of nevirapine to prevent mother- to-child HIV transmission in eight African countries. AIDS. 2004;18(12):1661–1671. doi: 10.1097/01.aids.0000131353.06784.8f. [DOI] [PubMed] [Google Scholar]
- 7.Uganda Bureau of Statistics (UBOS) and ICF International Inc. Uganda Demographic and Health Survey 2011. Kampala, Uganda: UBOS and Calverton; Maryland: ICF International Inc; 2012. Available at: http://www.ubos.org/onlinefiles/uploads/ubos/UDHS/UDHS2011.pdf. [Google Scholar]
- 8.Uganda AIDS Commission. Global AIDS Response Progress Report: Uganda. Uganda AIDS Commission. 2012 Available at: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_UG_Narrative_Report[1].pdf.
- 9.Heys J, Kipp W, Jhangri GS, et al. Fertility desires and infection with the HIV: results from a survey in rural Uganda. AIDS. 2009;23(Suppl 1):S37–S45. doi: 10.1097/01.aids.0000363776.76129.fd. [DOI] [PubMed] [Google Scholar]
- 10.Jhangri GS, Heys J, Alibhai A, et al. Unmet need for effective family planning in HIV-infected individuals: results from a survey in rural Uganda. J Fam Plann Reprod Health Care. 2012;38(1):23–29. doi: 10.1136/jfprhc-2011-0108. [DOI] [PubMed] [Google Scholar]
- 11.Joint United Nations Programme on HIV/AIDS. HIV and AIDS Estimates: Uganda. UNAIDS. 2011 Available at: http://www.unaids.org/en/regionscountries/countries/uganda/
- 12.Cooper D, Moodley J, Zqeigenthal V, et al. Fertility Intentions and Reproductive Health Care Needs of People Living with HIV in Cape Town, South Africa: Implications for Integrating Reproductive Health and HIV Care Services. AIDS Behav. 2009;13(Suppl 1):S38–S46. doi: 10.1007/s10461-009-9550-1. [DOI] [PubMed] [Google Scholar]
- 13.Maier M, Andia I, Emenyonu N, et al. Antiretroviral Therapy is Associated with Increased Fertility Desire, but not Pregnancy or Live Birth, among HIV+ Women in Early HIV Treatment Program in Rural Uganda. AIDS Behav. 2009;13(Suppl 1):S28–S37. doi: 10.1007/s10461-008-9371-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berhan Y, Berhan A. Meta-analysis of fertility desires of people living with HIV. BMC Public Health. 2013;13:409. doi: 10.1186/1471-2458-13-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makumbi FE, Nakigozi G, Reynolds SJ, et al. Associations between HIV Antiretroviral Therapy and the Prevalence and Incidence of Pregnancy in Rakai, Uganda. AIDS Research and Treatment. 2011;2011:519492. doi: 10.1155/2011/519492. Epub 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myer L, Carter RJ, Katyal M, et al. Impact of Antiretroviral Therapy on Incidence of Pregnancy among HIV-Infected Women in Sub-Saharan Africa: A Cohort Study. PLOS Med. 2009;7(2):e1000229. doi: 10.1371/journal.pmed.1000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wawer MJ, Gray RH, Sewankambo NK, et al. A randomized, community trail of intensive sexually transmitted disease control for AIDS prevention, Rakai, Uganda. AIDS. 1998;12:1211–1225. doi: 10.1097/00002030-199810000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Wawer MJ, Sewankambo NK, Serwadda D, et al. Control of sexually transmitted diseases for AIDS prevention in Uganda: a randomized community trial. The Lancet. 1999;13:525–535. doi: 10.1016/s0140-6736(98)06439-3. [DOI] [PubMed] [Google Scholar]
- 19.Kagaayi J, Gray RH, Brahmbhatt H, et al. Survival of Infants Born to HIV-Positive Mo thers, by Feeding Modality, in Rakai, Uganda. PLOS ONE. 2008;3(12):e3877. doi: 10.1371/journal.pone.0003877. doi:p10.1371/journal.pone.0003877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polis CB, Gray RH, Lutalo T, et al. Trends and correlates of hormonal contraceptive use among HIV-infected women in Rakai, Uganda, 1994-2006. Contraception. 2011;83:549–555. doi: 10.1016/j.contraception.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Kaida A, Andia I, Maier M, et al. The Potential Impact of Antiretroviral Therapy on Fertility in sub-Saharan Africa. Current HIV/AIDS Reports. 2006;3:177–184. doi: 10.1007/s11904-006-0015-0. [DOI] [PubMed] [Google Scholar]
- 22.Castro A, Khawja Y, Gonzalez-Nunez I. Sexuality, reproductive, and HIV in women: the impact of antiretroviral therapy in elective pregnancies in Cuba. AIDS. 2007;21(Suppl 5):S49–S54. doi: 10.1097/01.aids.0000298103.02356.7d. [DOI] [PubMed] [Google Scholar]
- 23.Cooper D, Harries J, Myer L, et al. “Life is still going on”: Reproductive intentions among HIV- positive women and men in South Africa. Soc Sci Med. 2007;65(2):274–283. doi: 10.1016/j.socscimed.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 24.Keogh SC, Urassa M, Roura M, et al. The impact of antenatal HIV diagnosis on postpartum childbearing desires in northern Tanzania: a mixed methods study. Reprod Health Matters. 2012;20(39 Suppl):39–49. doi: 10.1016/S0968-8080(12)39634-1. [DOI] [PubMed] [Google Scholar]
- 25.Heys J, Jhangri G, Rubaale T, et al. Infection with the human immunodeficiency virus and fertility desires: results from a qualitative study in rural Uganda. JWHP. 2012;13(3):5–17. doi: 10.12927/whp.2012.22783. [DOI] [PubMed] [Google Scholar]
- 26.Peltzer K, Chao LW, Dana P. Family planning among HIV positive and negative prevention of mother to child transmission clients in a resource poor setting in South Africa. AIDS Behav. 2009;13(5):97–979. doi: 10.1007/s10461-008-9365-5. [DOI] [PubMed] [Google Scholar]
- 27.Ezeanolue EE, Stumpf PG, Soliman E, et al. Contraception choices of HIV+ women in the era of highly active antiretroviral therapy. Contraception. 2011;84(2011):94–97. doi: 10.1016/j.contraception.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 28.Kaida A, Lima VD, Andia I, et al. The WHOMEN's Scale (Women's HAART Optimism Monitoring and EvaluatioN Scale v.1) and the Associations with Fertility Intentions and Sexual Behaviors Among HIV-Positive Women in Uganda. AIDS Behav. 2009;13(Suppl 1):S72–S81. doi: 10.1007/s10461-009-9553-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McClellan MK, Patel R, Kadzirange G, et al. Fertility Desires and Condom Use among HIV- Positive Women at an Antiretroviral Roll-Out Program in Zimbabwe. Afr J of Public Health. 2010;14(2):27–35. [PMC free article] [PubMed] [Google Scholar]
- 30.Schaan MM, Taylor M, Puvimanasinghe J, Busang L, et al. Sexual and reproductive health needs of HIV-positive women in Botswana: a study of health care worker's views. AIDS Care. 2012;24(9):1120–1125. doi: 10.1080/09540121.2012.672814. [DOI] [PubMed] [Google Scholar]
- 31.Nduna M, Farlane L. Women living with HIV in South African and their concerns about fertility. AIDS Behav. 2009;13(Suppl 1):62–65. doi: 10.1007/s10461-009-9545-y. [DOI] [PubMed] [Google Scholar]
- 32.Sarnquist CC, Rahangdale L, Maldonado Y. Reproductive Health and Family Planning Needs Among HIV-Infected Women in Sub-Saharan Africa. Curr HIV Research. 2013;11(2):160–168. doi: 10.2174/1570162x11311020008. [DOI] [PubMed] [Google Scholar]
- 33.Elul B, Delvaux T, Munyana E, Lahuerta M, Horowitze D, Ndagije F, et al. Pregnancy desires, and contraceptive knowledge and use among prevention of mother-to-child transmission clients in Rwanda. AIDS. 2009;23(Suppl 1):S19–S26. doi: 10.1097/01.aids.0000363774.91376.dc. [DOI] [PubMed] [Google Scholar]
- 34.van den Akker T, Bemelmans M, Ford N, Jemu M, Diggle E, Scheffer S, et al. HIV care need not hamper maternity care: a descriptive analysis of integration of services in rural Malawi. BJOG. 2012;119:431–438. doi: 10.1111/j.1471-0528.2011.03229.x. [DOI] [PubMed] [Google Scholar]
- 35.Chabikuli NO, Awi DD, Chukwujekwu O, et al. The use of routine monitoring and evaluation systems to assess a referral model of family planning and HIV service integration in Nigeria. AIDS. 2009;23(Suppl 1):S97–S103. doi: 10.1097/01.aids.0000363782.50580.d8. [DOI] [PubMed] [Google Scholar]