Abstract
Objective
Despite mounting evidence supporting the use of psychosocial interventions to promote adaptation to cancer, enrolling participants into these interventions is challenging. This is particularly salient for couple-based interventions, and newer, more targeted recruitment strategies to increase enrollment are needed. However, there have been few published empirical studies focused specifically on recruitment–related variables associated with enrollment into these types of interventions. To better understand how to encourage participation in couple-based psychosocial interventions for cancer, we examined facilitating and impeding factors to enrollment into a couple-based intervention for women with early stage breast cancer.
Method
In this sample of 99 women diagnosed with early stage breast cancer, patient demographic variables and method of approaching eligible patients were examined as predictors of enrollment into a randomized controlled trial comparing Couple-Based Relationship Enhancement with treatment-as-usual.
Results
Results indicated that women were more likely to enroll if they were contacted at home or at a follow-up medical appointment rather than when first diagnosed at a busy multidisciplinary clinic; they were also more likely to enroll the closer they lived to the research facility.
Conclusions
In addition to decreasing participant burden, timing and setting of recruitment efforts may have important implications for enhancing participation rates in couple-based intervention studies for cancer.
Keywords: cancer, oncology, couples and breast cancer, psychosocial, recruitment
Introduction
Physical illness can have a psychological impact on the individual with the medical condition as well as on his or her socio-environmental context, including the patient’s spouse or committed partner [1]. This is characteristic of many cancers [2], but is especially so in the case of breast cancer, which may be thought of as a “relational” cancer given the impact of treatment on changes in women’s bodies, body image, and sexual functioning for both partners (see [3] for a review). A recent meta-analysis has demonstrated the efficacy of individually-delivered psychosocial interventions to help address the psychological consequences of breast cancer [4]. In addition, due to the effects on both partners, several couple-based treatments have been developed for breast cancer, indicating positive effects for one or both partners [5–9]. Nonetheless, accrual to clinical trials in this area can be challenging.
When individuals are diagnosed with cancer, the rationale for a psychosocial intervention may not immediately be obvious to them. These challenges are compounded when recruiting for couple-based psychosocial treatment studies because both members of the couple need to agree to participate, yet one or both partners may view the cancer as an individually-based medical condition rather than an impetus for couple-based psychosocial intervention. Several treatment outcome studies of individually-based psychosocial treatments for breast and other cancer indicate that one-third to two-thirds of eligible patients enroll despite their being asked to participate in multiple assessments and treatment sessions [10–14]. Looking to the literature to inform recruitment strategies for couple-based psychosocial interventions is less straightforward, complicated by the paucity of empirical studies that address this issue specifically and the fact that few published couple-based psychosocial treatment outcome studies for breast cancer or other medical conditions provide detailed descriptions of their recruitment procedures, the relative effectiveness of these approaches (e.g., percentage of eligible individuals approached who enrolled in the study), and a comprehensive list of reasons that eligible individuals declined participation. Furthermore, among the studies that do provide information about their recruitment experiences, a wide range of enrollment rates emerge across interventions (e.g., 4% [15] vs. 94% [9]). Reasons for this variability are unclear, perhaps because it is uncommon for researchers to empirically examine specific variables that might increase or decrease the likelihood of a participant’s enrollment into a couple-based intervention for medical problems such as cancer. Indeed, several groups of authors [16–17] have noted that investigators do not commonly provide detailed descriptions of recruitment procedures and their usefulness in clinical trials, suggesting that this phenomenon is not limited to couple-based psychosocial interventions for breast cancer.
One notable exception is a report by Northouse and colleagues [17], who provided extensive details regarding their empirical investigation focused on recruitment and retention efforts in the context of a multi-site couple-based intervention for males with prostate cancer. The investigators reported an enrollment rate of 68% and noted differences in enrollment rates across sites (urban setting vs. non-urban) and stage of disease. Specifically, patients from an urban setting were less likely to enroll, as were patients with advanced cancer. Manne and colleagues [7] also provided useful details regarding recruitment for their couple-based group intervention for women with early stage breast cancer, reporting that the most common reason for refusal to participate was time and that younger patients were more likely to enroll than were older patients.
Detailed descriptions of recruitment procedures, reported utility of different recruitment strategies, and empirical evaluation of variables that might account for variability in enrollment rates for couple-based interventions for breast cancer or cancer more generally are important, as these might ultimately aid investigators in adapting their recruitment procedures to maximize the number of eligible participants enrolled in a particular intervention. High levels of recruitment are important not only to be able to generalize findings from treatment outcome research but also to provide services to the widest range of couples possible. Accordingly, the goal of the present study was to describe and empirically assess facilitating and impeding factors to enrollment into a couple-based psychosocial intervention for women with early stage breast cancer, with a focus on demographic variables and method of approaching eligible participants.
Methods
Participants
Ninety-nine women were recruited for enrollment into a couple-based intervention for early stage breast cancer at an academic, comprehensive cancer center-based practice [18]. Study participation involved random assignment to a six-session couple-based relationship enhancement program (Relationship Enhancement) or treatment as usual (TAU) and completion of four assessments consisting of self-report questionnaires and videotaped communication samples over the course of the study, each of which lasted approximately two hours. A woman was approached for participation in the study if (a) she was diagnosed with stage I or stage II breast cancer within the previous year and had no history of breast cancer or any other cancer within 5 years; (b) she and her male partner were currently married or living together in a committed relationship for at least 12 months; (c) both partners were able to speak English; and (d) both partners were willing to participate.
The mean age of eligible women approached for participation in the study was 52.6 years (SD = 11.5; range = 28–82), and 20% were of a racial/ethnic minority (14% African-American, 1% Latino, and 5% other). The catchment area for the cancer center was large, drawing women from around the state. On average, women lived 52.8 miles (SD = 47.8; range = 3 to 249) from the treatment facility and had received their diagnoses an average of 14.7 days (SD = 16.2, range = 0 to 91 days) prior to being recruited.
Procedures
All assessments and treatment sessions were conducted at a research treatment facility approximately two miles away from the UNC Medical Center. All participants gave written informed consent, and the study was approved by the local Institutional Review Board.
A woman’s eligibility was determined by research staff who reviewed her medical records prior to her first appointment at the weekly multidisciplinary breast cancer clinic at the University of North Carolina (UNC) Hospital, an academic medical center and public hospital that serves the state of North Carolina. During her visit to the clinic, each woman receives care from a variety of health care providers, including medical, surgical, and radiation oncologists, surgical nurses, research staff, radiologists, geneticists, and patient counselors. She can spend one to six hours at the clinic waiting for appointments, being examined, and discussing assessment results and treatment options with health care providers. A woman typically receives her breast cancer diagnosis shortly before or at her first visit to the multidisciplinary clinic.
The initial recruitment strategy involved attempting to approach eligible women at the multidisciplinary breast clinic shortly after diagnosis. At the clinic, a clinical psychology doctoral student or an undergraduate research assistant with extensive cancer center recruitment experience briefly described the program to the woman and asked permission to contact her by phone the following week to describe the program further. If, for some reason, the woman was not able to be seen that day at the multidisciplinary clinic (e.g., she had back-to-back appointments with medical staff and there was no time for her to be seen by research staff, or there was a schedule change and the woman had already left the clinic prior to the recruiters’ arrival), a research staff member attempted to approach the eligible woman at a follow-up medical appointment. If this was not possible, the woman was contacted by telephone at home, and the study was described to her then. Although the study was approved by the clinical directors of the breast clinic, physicians were not asked to introduce the study or explicitly endorse it to participants in order to minimize physician burden.
Recruiters followed a script when introducing the study to prospective participants, whether in person or by telephone. Eligible women were informed that they had the opportunity to participate in a study evaluating a program designed to assist couples during the treatment of the woman’s breast cancer. The rationale was explained as follows: breast cancer can affect both the woman and her male partner and, although a breast cancer diagnosis and treatment can pose difficulties, it also offers couples the opportunity to thrive rather than merely survive. To facilitate this process, eligible couples were being offered the opportunity to learn skills to promote their working as a team to address the breast cancer and to help them focus on the positives despite the challenges posed by the cancer and its treatment. Recruiters were careful to use the term “program” rather than “therapy,” “treatment,” or “psychological intervention” to minimize the risk of pathologizing or alienating prospective participants, particularly those who were not experiencing current relationship distress. If the woman expressed a desire to participate, the recruiter then spoke with her male partner to describe the study in detail. If both partners agreed to enroll, the couple was then scheduled for an initial study assessment session.
In the majority of cases, when a woman declined participation in the study, she spontaneously provided a reason (e.g., “I’m too busy right now” or “It’s not the kind of thing I’m interested in”), and the response was recorded by the research assistant without further inquiry to minimize her feeling that she had to justify her decision or that she was being coerced to participate. When a woman did not spontaneously share the reason for her decision not to enroll, the research assistant asked if she would be comfortable sharing the reason for her decision for our records. In all latter cases, women who declined provided a reason when asked.
Results
Of the 99 eligible women approached, 13.1% agreed to participate in the study, and 86.9% declined. For women who agreed to participate, time from introduction of the study to formal enrollment took an average of 37 days (SD = 26.92; range 5 to 111). As displayed in Table 1, the most common reason for declining was distance lived from the treatment facility, followed by lack of interest and lack of time.
Table 1.
Reported Reasons for Declining Enrollment (N = 86)
| Reason for Declining | Frequency (N) | Percent (%) |
|---|---|---|
| Distance | 35 | 41 |
| Lack of interest | 14 | 16 |
| Time | 9 | 11 |
| Husband too busy | 7 | 8 |
| Unresponsive to follow-up | 6 | 7 |
| “Doing okay” | 5 | 6 |
| “Feeling overwhelmed” | 3 | 4 |
| Stated husband would not participate | 2 | 2 |
| Husband uninterested | 1 | 1 |
| “Too touchy feely” | 1 | 1 |
| Believed study conflicted with religious convictions | 1 | 1 |
| Not want any more research studies | 1 | 1 |
| Privacy concerns | 1 | 1 |
Enrollers and decliners were similar in terms of age (enrollers: M = 52.1 years, SD = 10.3; decliners: M = 52.7, SD = 11.8) and race (20% of each group was a member of a racial or ethnic minority) but differed in terms of how far they lived from the research facility and how they were approached initially. With respect to distance, women who agreed to participate lived an average of 31.7 miles from the research facility (SD = 37.8; range 3 to 146), compared to those who declined, who lived an average of 56 miles from the research facility (SD = 48.5; range 3 to 249). Among women who were initially approached at the multidisciplinary clinic (N = 46), 4% enrolled in the study (N = 2), and 96% declined (N = 44); in contrast, among women who were approached outside of the multidisciplinary clinic (N = 53), 21% enrolled (N = 11: 9 initially contacted by phone, 2 initially approached at a follow-up clinic), and 79% declined (N = 42: 40 initially contacted by phone, 2 initially approached at a follow-up clinic). Despite the small sample size, this difference was significant (p = 0.02, Fisher’s exact test). Additional analyses confirmed that the difference in enrollment rates between the two recruitment settings was not an artifact of time since diagnosis, as there were no differences between enrollers and decliners in the length of time from when they were diagnosed with breast cancer to when they were approached for study participation (t(97) = −0.28, p = .78).
Using logistic regression, we examined the collective impact of women’s age, race (Caucasian vs. non-Caucasian), distance from the research facility, and setting in which they were approached as predictors of enrollment into the study. Prior to evaluating the model, one woman who had enrolled was dropped for inclusion because she was an outlier with respect to distance. (The participant lived 146 miles from the research facility, a distance of more than three standard deviations from the mean of enrollees.) This resulted in a new sample of enrollees whose mean age was 53.5 years (SD = 9.3; range 42 to 76) and mean distance was 22.2 miles from the research facility (SD = 16.5; range 3 to 54). Twenty-five percent were of a racial/ethnic minority heritage, and 83.3% had not been approached at the multidisciplinary clinic.
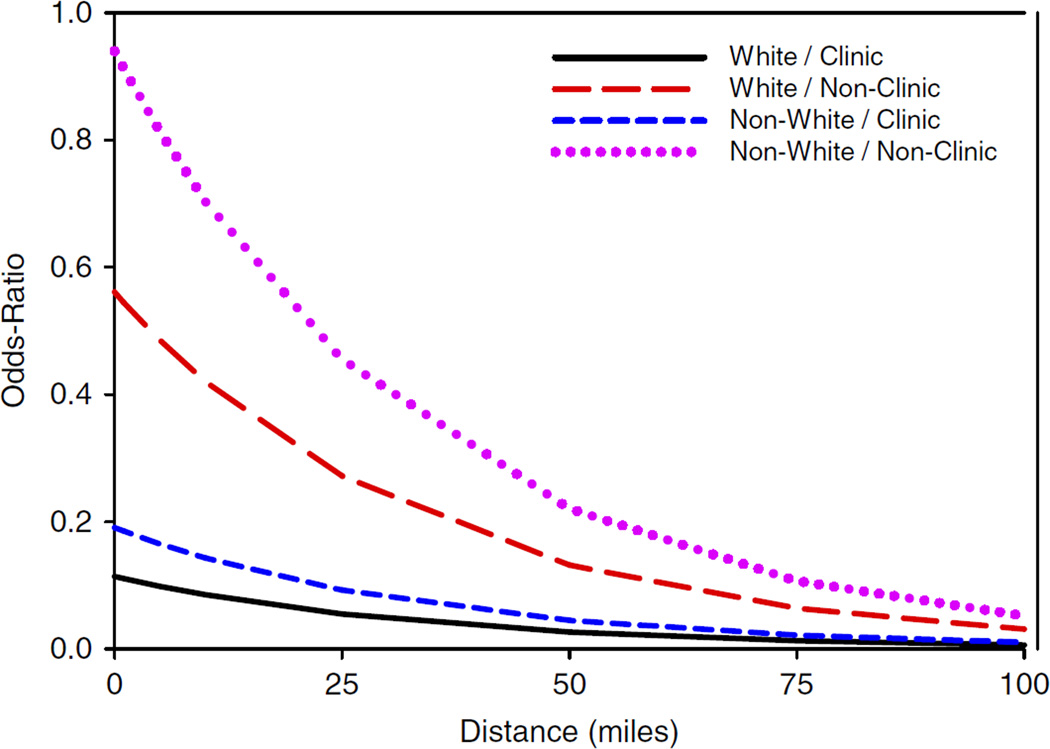
The omnibus four-predictor model was significant (χ2 = 12.62, N = 98, df = 4, p = .01), and there was a significant effect for distance from the research facility (O.R. = 0.49, p = .03), such that for every twenty-five miles patients lived from the treatment facility, the odds of enrolling were approximately 50% lower. The decreasing odds of enrollment as a function of distance from the research facility are represented in Figure 1. There was also a significant effect for setting in which women were approached: the odds of a couple’s enrolling rather than declining to enroll were nearly five times higher (O.R. = 4.93, p = .057) if the woman was initially contacted by phone or approached at a follow-up clinic visit rather than recruited at the multidisciplinary breast clinic. Neither age (O.R. = 0.99, p = .76) nor race (O.R. = 1.68, p = .52) was a significant predictor of enrollment.
Figure 1.
Odds ratios of enrollment as a function of distance from the research facility. This graph displays the decreasing odds ratios of enrolling into the intervention, controlling for participants’ race (White vs non-White) and setting in which they were approached (at multidisciplinary clinic vs outside of multidisciplinary clinic)
Discussion
Despite emerging evidence that couple-based psychosocial interventions can promote adaptation to one partner’s cancer, recruiting participants to these intensive studies can be a challenge. Evaluation of recruitment strategies is important for generalizing research findings and ultimately improving patient care in this area. However, with few published empirical reports focused specifically on recruitment–related variables associated with enrollment into these types of interventions, it is difficult to draw substantive conclusions regarding the usefulness of specific recruitment strategies to guide researchers in this field. The present study represents an effort to help address this gap in the extant literature.
Distance was the most commonly reported reason for declining participation, and the odds of enrolling decreased as the number of miles from the research facility increased, suggesting that distance was a proxy for burden for prospective participants. We also found that women approached at a busy multidisciplinary clinic shortly after initial diagnosis were less likely to enroll in the intervention than were those contacted by telephone at home or approached at a follow-up clinic. It may be that women who were approached at the multidisciplinary clinic were not prepared to integrate information relating to the psychosocial aspects of their breast cancer (e.g., relationship adjustment) because they were attending strongly to the medical aspects of their breast cancer (e.g., what surgery to have, risks and benefits of chemotherapy). In some instances, women had just recently learned of their breast cancer diagnosis and were somewhat overwhelmed, and many were meeting several physicians for the first time at that visit. As a result, they likely had trouble fully absorbing additional information and considering an intervention that might have appeared peripheral to their care at the hospital.
There are other factors that, although not examined empirically in this investigation, also might have contributed to the low rate of enrollment. For example, all women were asked to invest a substantial amount of time to participate. Some women might have felt that four two-hour assessments, with the possibility of six additional 75-minute sessions if assigned to the Relationship Enhancement condition, was more of a commitment than they could make while grappling with the acute stress of their breast cancer diagnosis. Given the high time-related demand (and, in some cases, travel-related burden) that prospective participants would have had to assume, limited direct physician involvement in the recruitment process could have been relevant as well. That is, although the study was approved by the clinical directors of the breast cancer center, the research protocol did not involve their introducing the study or explicitly endorsing it to patients as a potentially valuable component of their overall treatment plan. Physicians’ role in the recruitment process has been associated with patients’ decisions to enroll in cancer clinical trials focusing on medical intervention [19] and psychosocial intervention [13, 20]. Had recruitment been structured such that physicians encouraged participation, patients might have been more inclined to reflect on how breast cancer had impacted, or could impact, their individual psychological well-being and relationship adjustment and been more willing to consider participation despite study-related burden. Future research is needed to empirically assess the impact of physician involvement on enrollment into couple-based psychosocial interventions for cancer and patient perceptions of physician attitudes towards enrollment.
Our interpretations regarding study-related burden and method of approaching eligible participants are consistent with the experiences described by other investigators who have conducted couple-based psychosocial treatment outcome studies for cancer. For instance, by legitimizing the presence of the psychologist as a member of the treatment team and minimizing travel-related burden on the participants, Scott, Halford, and Ward [9] reported an extraordinarily high enrollment rate of 94% in their couple-based intervention for women with early stage breast or gynecological cancers. In that study, the psychologist was in the room with the physician at the time of diagnosis and conducted all four assessments and six intervention sessions in the participants’ homes. Similarly, in the study conducted by Northouse et al. [17], physicians and other medical personnel were involved in recruitment efforts, and all study-based assessment and treatment sessions were conducted at participants’ homes, significantly reducing study-related burden, and likely contributing to their 68% enrollment rate.
Conversely, and looking more broadly at accrual rates for psychosocial interventions for health, couple-based intervention studies that involve high levels of burden on the patient/partner dyad are associated with lower rates of enrollment (e.g., 4% [15, 21]), whereas studies that involve a moderate level of burden have intermediate levels of enrollment, with rates of participation generally increasing as the burden on participants decreased and/or the pertinence of the intervention within a medical setting increased (e.g., 19–50% [22, 7–8], respectively).
The current findings should also be considered in the context of enrollment rates in other types of cancer research. In general, it is frequently reported that only 5% of adult cancer patients participate in clinical trials [23]. However, single institution studies among breast cancer patients demonstrate that the rates of accrual may be greater than 30% for eligible patients presented with the option of trial enrollment [24]. Documented barriers to enrollment include: distance from trial center [23, 25], fear of randomization [26–28], patient perceptions of clinical trials [25, 29], and perceived burdens of trial participation [25, 29]. Many of these issues may have been relevant in the context of the current study as well. Further, Stevens and Ahmedzai [30] provided evidence that feelings of “information overload” among breast cancer patients making treatment decisions can be a barrier to trial accrual, which seems to support our finding that recruitment outside of the busy multidisciplinary clinic was a preferred strategy.
Findings from this and other studies of accrual into cancer research suggest several strategies that researchers conducting couple-based psychosocial interventions for breast and other cancers could employ to increase enrollment. First, participant burden could be decreased by scheduling study-related appointments in conjunction with medical appointments or decreasing the number of sessions and assessments. Alternatively, study staff could travel to participants’ homes to complete assessments and treatment sessions; at the same time, this strategy does raise the question of portability and dissemination, as few providers could offer this level of service. In cases where treatment integrity would not be compromised by non-face-to-face delivery, it might be advantageous to conduct sessions by phone or via the internet.
A second strategy is to approach prospective participants so that the value of psychosocial interventions has increased salience, such as by approaching eligible patients when they are more likely to be grappling with the non-medical, psychological aspects of their medical condition (e.g., at home or at a follow-up clinic) and reinforcing the perception that the psychosocial intervention is an important part of patients’ overall care within a medical setting. Positioning study staff as integral members of patients’ treatment team and maximizing involvement by physicians, whom patients identify as the lead coordinator of their care, during the recruitment process might legitimize the psychosocial intervention as a valuable part of comprehensive medical treatment and mitigate disincentives due to study-related burden. Furthermore, integration of formal psychosocial assessment of all patients in a multidisciplinary context and presentation of participation in a couple-based psychosocial treatment study as one among several strategies to address psychosocial issues arising in breast cancer management might also legitimize trial participation and improve the quality of care of all patients.
At minimum, researchers’ providing detailed descriptions of their recruitment efforts in this field and the relative success of the strategies they employed would be helpful to others conducting similar interventions. Recognition of the barriers to accrual to couple-based psychosocial interventions is the critical first step in efforts to overcome them, improve trial accrual, and facilitate rapid identification of the full benefits, costs, and optimal delivery of this important new tool to improve the lives of patients with breast cancer and their loved ones.
Acknowledgments
We gratefully acknowledge Mort Webster, Ph.D., and Catherine Zimmer, Ph.D., for their assistance with data analysis and presentation. This study was supported in part by National Cancer Institute Grant R01 CA107477-04 and Lineberger Comprehensive Cancer Grant LCCC 0402.
Contributor Information
Steffany J. Fredman, University of North Carolina at Chapel Hill
Donald H. Baucom, University of North Carolina at Chapel Hill
Tina M. Gremore, University of North Carolina at Chapel Hill
Angela M. Castellani, University of North Carolina at Chapel Hill
Theresa A. Kallman, University of North Carolina at Chapel Hill
Laura S. Porter, Duke University Medical Center
Jennifer S. Kirby, University of North Carolina at Chapel Hill
E. Claire Dees, University of North Carolina at Chapel Hill.
Nancy Klauber-Demore, University of North Carolina at Chapel Hill.
Jeffrey Peppercorn, University of North Carolina at Chapel Hill.
Lisa A. Carey, University of North Carolina at Chapel Hill
References
- 1.Schmalling KB, Sher TG. The Psychology of Couples and Illness: Theory, Research, and Practice. Washington, D.C.: American Psychological Association; 2000. [Google Scholar]
- 2.Blanchard CG, Albrecht TL, Ruckdeschel JC. The crisis of cancer: Psychological impact on family caregivers. Oncology. 1997;11:189–194. [PubMed] [Google Scholar]
- 3.Baucom DH, Porter LS, Kirby JS, et al. Psychosocial issues confronting young women with breast cancer. Breast Disease. 2005;22:1–11. doi: 10.3233/bd-2006-23114. [DOI] [PubMed] [Google Scholar]
- 4.Zimmermann T, Heinrichs N, Baucom DH. “Does one size fit all?” moderators of psychosocial interventions for breast cancer: A meta-analysis. Ann Behav Med. 2007;34:225–239. doi: 10.1007/BF02874548. [DOI] [PubMed] [Google Scholar]
- 5.Christensen DN. Postmastectomy couple counseling: An outcome study of a structured treatment protocol. J Sex Mar Ther. 1983;9:266–275. doi: 10.1080/00926238308410913. [DOI] [PubMed] [Google Scholar]
- 6.Kalaitzi C, Vassilios PP, Michas K, et al. Combined brief psychosexual intervention after mastectomy: Effects on sexuality, body image, and psychological well being. J Surg Oncol. 2007;96:235–240. doi: 10.1002/jso.20811. [DOI] [PubMed] [Google Scholar]
- 7.Manne SL, Ostroff JS, Winkel G, et al. Couple-focused group intervention for women with early stage breast cancer. J Consult Clin Psychol. 2005;73:634–646. doi: 10.1037/0022-006X.73.4.634. [DOI] [PubMed] [Google Scholar]
- 8.Shields CG, Rousseau SJ. A pilot study of an intervention for breast cancer survivors and their spouses. Fam Process. 2004;43:95–107. doi: 10.1111/j.1545-5300.2004.04301008.x. [DOI] [PubMed] [Google Scholar]
- 9.Scott JL, Halford WK, Ward BG. United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol. 2004;72:1122–1135. doi: 10.1037/0022-006X.72.6.1122. [DOI] [PubMed] [Google Scholar]
- 10.Antoni MH, Lechner SC, Kazi A, et al. How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psychol. 2006;74:1143–1152. doi: 10.1037/0022-006X.74.6.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boesen E, Boesen S, Christensen S, et al. Comparison of participants and non-participants in a randomized psychosocial intervention study among patients with malignant melanoma. Psychosomatics. 2007;48:510–516. doi: 10.1176/appi.psy.48.6.510. [DOI] [PubMed] [Google Scholar]
- 12.Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized breast cancer: Development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31:261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- 13.Pinto BM, Trunzo JJ, Rabin C, et al. Recruitment strategies for a home-based physical activity intervention for breast cancer patients. J Clin Psychol in Med Settings. 2004;11:171–178. [Google Scholar]
- 14.Segal R, Evans W, Johnson D, et al. Structured exercise improves physical functioning in women with stages I and II breast cancer: Results of a randomized controlled trial. J Clin Oncol. 2001;19:657–665. doi: 10.1200/JCO.2001.19.3.657. [DOI] [PubMed] [Google Scholar]
- 15.Sher TG, Braun LT, Domas A, et al. A couples approach to cardiac risk reduction; Paper presented at the 39th annual meeting of the Association for Behavioral and Cognitive Therapies; Washington, D.C.. 2005. Nov, [Google Scholar]
- 16.Gross CP, Mallory R, Heiat A, et al. Reporting the recruitment process in clinical trials: Who are these patients and how did they get here? Ann Intern Med. 2002;137:689–692. doi: 10.7326/0003-4819-137-1-200207020-00007. [DOI] [PubMed] [Google Scholar]
- 17.Northouse LL, Rosset T, Phillips L, et al. Research with families facing cancer: The challenges of accrual and retention. Res Nurs Health. 2006;29:199–211. doi: 10.1002/nur.20128. [DOI] [PubMed] [Google Scholar]
- 18.Baucom DH, Porter LS, Kirby JS, et al. A couple-based intervention for female breast cancer. Psycho-Oncology. doi: 10.1002/pon.1395. in press. [DOI] [PubMed] [Google Scholar]
- 19.Albrecht TL, Blanchard C, Ruckdeschel JC, et al. Strategic physician communication and oncology clinical trials. J Clin Oncol. 1999;17:3324–3332. doi: 10.1200/JCO.1999.17.10.3324. [DOI] [PubMed] [Google Scholar]
- 20.McNees P, Dow K, Loerzel V. Application of the CuSum Technique to evaluate changes in recruitment strategies. Nurs Res. 2005;54:399–405. doi: 10.1097/00006199-200511000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Sher TG, Bellg AJ, Braun L, et al. Partners for life: A theoretical approach to developing an intervention for cardiac risk reduction. Health Educ Res. 2002;17:597–605. doi: 10.1093/her/17.5.597. [DOI] [PubMed] [Google Scholar]
- 22.Martire LM, Schulz R, Keefe FJ, et al. Feasibility of a dyadic intervention for management of osteoarthritis: A pilot study with older patients and their spousal caregivers. Aging Mental Health. 2003;7:53–60. doi: 10.1080/1360786021000007045. [DOI] [PubMed] [Google Scholar]
- 23.Lara PN, Jr, Higdon R, Lim N, et al. Prospective evaluation of cancer clinical trial accrual patterns: Identifying potential barriers to enrollment. J Clin Oncol. 2001;19:1728–1733. doi: 10.1200/JCO.2001.19.6.1728. [DOI] [PubMed] [Google Scholar]
- 24.Simon MS, Du W, Flaherty L, et al. Factors associated with breast cancer clinical trials participation and enrollment at a large academic medical center. J Clin Oncol. 2004;22:2046–2052. doi: 10.1200/JCO.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Grunfeld E, Zitzelsberger L, Coristine M, et al. Barriers and facilitators to enrollment in cancer clinical trials: Qualitative study of the perspectives of clinical research associates. Cancer. 2002;95:1577–1583. doi: 10.1002/cncr.10862. [DOI] [PubMed] [Google Scholar]
- 26.Fallowfield LJ, Jenkins V, Brennan C, et al. Attitudes of patients to randomised clinical trials of cancer therapy. Eur J Cancer. 1998;34:1554–1559. doi: 10.1016/s0959-8049(98)00193-2. [DOI] [PubMed] [Google Scholar]
- 27.Kornblith AB, Kemeny M, Peterson BL, et al. Survey of oncologists' perceptions of barriers to accrual of older patients with breast carcinoma to clinical trials. Cancer. 2002;95:989–996. doi: 10.1002/cncr.10792. [DOI] [PubMed] [Google Scholar]
- 28.Corbett F, Oldham J, Lilford R. Offering patients entry in clinical trials: Preliminary study of the views of prospective participants. J Med Ethics. 1996;22:227–231. doi: 10.1136/jme.22.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ellis PM, Butow PN, Tattersall MH, et al. Randomized clinical trials in oncology: Understanding and attitudes predict willingness to participate. J Clin Oncol. 2001;19:3554–3361. doi: 10.1200/JCO.2001.19.15.3554. [DOI] [PubMed] [Google Scholar]
- 30.Stevens T, Ahmedzai SH. Why do breast cancer patients decline entry into randomized trials and how do they feel about their decision later: A prospective, longitudinal, in-depth interview study. Patient Educ Couns. 2004;52:341–34. doi: 10.1016/S0738-3991(03)00041-7. [DOI] [PubMed] [Google Scholar]