Abstract
Acquired resistance to EGF receptor (EGFR) tyrosine kinase inhibitor (TKI) is a critical problem in the treatment of lung cancer. Although several mechanisms have been shown to be responsible for acquired resistance, all mechanisms have not been uncovered. In this study, we investigated the molecular and cellular profiles of the acquired resistant cells to EGFR-TKI in EGFR-mutant lung cancers. Four EGFR-mutant cell lines were exposed to gefitinib by stepwise escalation and high-concentration exposure methods, and resistant sublines to gefitinib were established. The molecular profiles and cellular phenotypes of these resistant sublines were characterized. Although previously reported, alterations including secondary EGFR T790M mutation, MET amplification, and appearance of epithelial-to-mesenchymal transition (EMT) features were observed, these 2 drug-exposure methods revealed different resistance mechanisms. The resistant cells with EMT features exhibited downregulation of miRNA-200c by DNA methylation. Furthermore, the HCC827-derived subline characterized by the high-concentration exposure method exhibited not only EMT features but also stem cell–like properties, including aldehyde dehydrogenase isoform 1 (ALDH1A1) overexpression, increase of side-population, and self-renewal capability. Resistant sublines with stem cell–like properties were resistant to conventional chemotherapeutic agents but equally sensitive to histone deacetylase and proteasome inhibitors, compared with their parental cells. ALDH1A1 was upregulated in clinical samples with acquired resistance to gefitinib. In conclusion, our study indicates that the manner of EGFR-TKI exposure influences the mechanism of acquired resistance and the appearance of stem cell–like property with EGFR-TKI treatment.
Introduction
EGF receptor (EGFR) mutations are oncogenic alterations in non–small cell lung carcinoma (NSCLC; refs. 1, 2). First-generation EGFR-tyrosine kinase inhibitors (TKI), such as gefitinib and erlotinib, have exhibited significant antiproliferative effects against NSCLC with EGFR mutations in preclinical studies (1, 2) and have also resulted in prolonged disease-free survival in randomized phase III studies (3–5). However, patients with EGFR-activating mutations who initially respond to EGFR-TKIs eventually acquire resistance, which is a critical problem in the treatment of patients with advanced NSCLC. Several mechanisms are believed to be responsible for acquired resistance to EGFR-TKI, including secondary EGFR T790M and minor mutations, MET amplification, and activation of MET/HGF axis, acquiring an epithelial-to-mesenchymal transition (EMT) signature, and transformation from NSCLC into small cell lung cancer (SCLC; refs. 6–11). More recently, AXL kinase activation and loss of the EGFR-mutant allele have been reported as possible mechanisms of resistance, but it is likely that additional mechanisms remain to be identified (12, 13).
Establishment of resistant sublines is a common experimental method to investigate the mechanism of drug resistance. The properties of resistant cells can vary according to the experimental methods used in the developing process. For example, in endometrial cancer, cisplatin-resistant cells established by stepwise escalation exposure and high-concentration exposure methods showed different cellular properties that may be either a cause or result of drug resistance (14). This fact suggests that the mechanism of EGFR-TKI resistance may vary according to in vitro culture conditions, resulting in finding of novel features of resistant cells. Although the majority of previously reported cells that were resistant to EGFR-TKI were established with stepwise escalation of EGFR-TKI concentration, we successfully established resistant cells with the high-concentration exposure method as well as the stepwise escalation method, and identified novel features of cells resistant to EGFR-TKI. The purposes of this study were to investigate the acquired mechanism of resistance to EGFR-TKI and to explore strategies to overcome resistance to EGFR-TKI.
Materials and Methods
Cell lines and reagents
EGFR-mutant HCC827 (exon19del E746–A750), PC-9 (exon19del E746–A750), HCC4006 (exon19del L747–E749), and HCC4011 (L858R) cells were used. These cell lines except for PC-9 were established by one of the authors (AF. Gazdar). PC-9 was obtained from Immuno-Biological Laboratories. All the cell lines were cultured in RPMI-1640 media supplemented with 10% FBS, and grown in a humidified incubator with 5% CO2 at 37° C. EGFR-TKI–resistant sublines were established by 2 different methods: parental cells were cultured with stepwise escalation of concentrations of gefitinib from 5 nmol/L to 2 µmol/L over 6 months (stepwise escalation method), or initially high concentration of gefitinib (2 µmol/L) over 6 months (high-concentration method). Finally, gefitinib-resistant sublines named as HCC827-GR-step, PC-9-GR-step, HCC4006-GR-step, and HCC4011-GR-step were established by stepwise escalation method, and HCC827-GR-high1, HCC827-GR-high2, PC-9-GR-high, HCC4006-GR-high, and HCC4011-GR-high were established by high-concentration method. About HCC827-GR-high1 and high2, these 2 sublines were independently established from different cultures with high-concentration method. The identities of all the parental and resistant cells were confirmed by analyzing the short tandem repeat profile using the Cell ID System (Promega) and ABI Prism 310 Genetic Analyzer (Applied Biosystems), according to the manufacturer’s instructions. Clonal-resistant cells were isolated by limiting dilution.
Details about the reagents used in the cell proliferation assay and the antibodies for Western blot analysis, fluorescence immunocytochemistry, and immunohistochemistry are included in the Supplementary Methods.
Determination of cell proliferation
Cell proliferation was determined by a modified MTS assay with CellTiter 96 AQueous One Solution Reagent (Promega) as previously reported (15). The antiproliferative effects are shown as IC50, which is the concentration of the drug required to inhibit cell proliferation by 50%.
Western blot analysis
The detailed protocol for the Western blotting has been described previously (15). Monoclonal antiactin antibody, used as an equal loading control, was purchased from Merch KGaA. The following secondary antibodies were used: goat anti-rabbit or anti-mouse immunoglobulin G (IgG)-conjugated horseradish peroxidase (Santa Cruz Biotechnology). To detect specific signals, the membranes were examined using ECL Prime Western Blotting Detection System (GE Healthcare).
Phospho-receptor tyrosine kinase array and phospho-kinase arrays
A Human Phospho-Receptor Tyrosine Kinase (RTK) Array Kit and a Human Phospho-Kinase Array Kit (R&D Systems) were used to measure the relative level of tyrosine phosphorylation of 42 distinct RTKs and the relative level of phosphorylation of 46 distinct intracellular kinases. Both arrays were conducted according to the manufacturer’s instructions.
Fluorescence immunocytochemistry
The cells were cultured and fixed by 4% formaldehyde on chamber slides. Primary antibodies against EGFR, E-cadherin, vimentin, aldehyde dehydrogenase isoform 1 (ALDH1A1), and ABCB1 were used. Further details are provided in the Supplementary Methods.
DNA and RNA extraction
Genomic DNAs were isolated from cell lines, frozen tumors, or paraffin-embedded tumor by using DNeasy Blood and Tissue Kit (Qiagen), standard phenol–chloroform (1:1) extraction followed by ethanol precipitation, or QIAmp DNA FFPE Tissue Kit (Qiagen), respectively. Total RNAs were extracted from cell lines using RNeasy Plus Mini Kit (Qiagen). The cDNA was synthesized from total RNA using High-Capacity cDNA Reverse Transcription Kits (Applied Biosystems) according to the manufacturer’s instructions.
Direct sequencing, PCR-based length polymorphism assay, and subcloning
We determined the mutational status of EGFR, KRAS, NRAS, and BRAF genes by direct sequencing, and PCR conditions are provided in Supplementary Table S1A. EGFR exon 19 deletion was also detected with PCR-based length polymorphism assay, which have previously reported (16). For subcloning, PCR products were cloned into pCR2.1-TOPO vector using TOPO TA Cloning Kit (Invitrogen). One hundred clones were randomly selected for PCR-based length polymorphism assay.
Analyses of copy number by qPCR and FISH assays
Copy number gains (CNG) of EGFR and MET genes were determined by quantitative real-time PCR (qPCR) assay using Power SYBR Green PCR Master Mix (Applied Biosystems), as previously reported (17, 18). Primer sequences are provided in Supplementary Table S1B. In brief, gene dosage of each target and LINE-1 gene, a reference gene, was calculated using the standard curve method. Relative copy number of each sample was determined by comparing the ratio of target gene to LINE-1 in each sample with the ratio of these genes in human genomic DNA (EMD Biosciences). On the basis of our previous study, we defined high-level amplification as values greater than 4 in cell lines and those greater than 5 in clinical samples (17, 18).
A dual-color FISH assay was conducted using the LSI EGFR SpectrumOrange/CEP7 SpectrumGreen probe (Vysis) according to the manufacturer’s instructions. Twenty metaphase spreads and 200 interphase nuclei were analyzed in each slide.
Hybridoma production and TKI sensitivity analysis
The parental HCC827 cells were fused with HCC827-GR-high2 using Sendai virus (hemagglutinating virus of Japan) envelope (HVJ-E) GenomONE-CF (Ishihara Sangyo Kaisha Ltd.) according to the manufacturer’s instructions. In brief, HCC827 cells stained with PKH26 Red fluorescent Cell Linker Kit (Sigma-Aldrich) were mixed at a ratio of 1:1 HCC827-GR-high2 cells stained with PKH67 Green fluorescent Cell Linker Kit (Sigma-Aldrich). The fused cells were confirmed as double-fluorescent positive cells in fluorescent microscopy. Cells were treated with 2 µmol/L of gefitinib and the presence of double-fluorescent positive and single-fluorescent positive cells (HCC827 and HCC827-GR-high2) was examined 14 days after.
Expression profiling analysis
RNA from cells was profiled on Illumina HumanHT-12 V4 Expression BeadChip arrays according to the Illumina protocol. The array measures expression levels for more than 47,000 transcripts derived from the NCBI RefSeq Release 38. BRB array tools (version 4.2) were used to conduct robust spline normalization on background corrected data to generate log2-transformed normalized data. Fold change in expression for individual probes was calculated and probes with fold changes exceeding 2-fold or below 2-fold were considered over- and underexpressed, respectively (Supplementary Table S2).
mRNA and miRNA expression analysis by qRT-PCR
mRNA expression analysis by quantitative reverse transcription PCR (qRT-PCR) was conducted on cDNA using TaqMan probes and the TaqMan Universal PCR Master Mix (Applied Biosystems). In miRNA expression analysis, the miRNA was isolated with TaqMan MicroRNA Cells-to-CT Kit (Ambion), and reverse transcription was conducted with TaqMan Micro-RNA Reverse Transcriptional Kit systems (Applied Biosystems) using TaqMan primers for each miRNA. Primer and probe sets (Supplementary Table S1C and S1D) were purchased from Applied Biosystems and used according to manufacturer’s instructions. PCR amplification was conducted on an ABI StepOne Real-Time PCR Instrument (Applied Biosystems) and gene expression was calculated using the comparative CT method. Three replicates per sample were assayed for each gene. To quantify the relative changes in gene expression, the 2 (–ΔΔCT) method was used and reactions were normalized to endogenous control gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) expression levels in mRNA expression analysis, and miR-374 expression level in miRNA expression analysis, respectively.
DNA methylation analysis
DNA was subjected to bisulfate treatment using Epitect Bisulfite Kit (Qiagen) according to the manufacturer’s protocol. DNA methylation status was examined by bisulfite genomic sequencing and methylation-specific PCR (MSP) as previously reported (19). Primers are listed in Supplementary Table S1E and S1F.
Sphere formation assays in serum-free cultures
A total of 5 × 103 of cells were plated in 24-well plates with Ultra-Low Attachment surface (Corning Inc.), and cultured in serum-free Dulbecco’s Modified Eagle Medium F12 (Invitrogen) supplemented with 20 ng/mL EGF and 10 ng/mL basic fibroblast growth factor (bFGF; all from Sigma-Aldrich). The numbers of spheres exceeding 150 µm in size for each well were counted by microscope after 14 days of culturing.
Side-population analysis
The basic protocol for side-population analysis was based on Goodell and colleagues (20). Cells were resuspended at 1 × 106/mL in prewarmed RPMI-1640, and Hoechst 33342 dye (Sigma-Aldrich) was added to a final concentration of 5 µg/mL in the presence or absence of verapamil (30 µg/mL; Sigma-Aldrich). The cells were then incubated at 37°C for 75 minutes with intermittent shaking. Propidium iodide (Sigma-Aldrich) was added to the cells, to a final concentration of 1 µg/mL, to gate the viable cells. The cell preparations were filtered through a 40-mm cell strainer to obtain single cell suspension. The cell samples were then analyzed on a BD FACSVantage SE (BD Biosciences) cell sorter. The side population was identified as a group of cells that did not take up the Hoechst dye, a characteristic abolished with verapamil treatment (20). These analyses were conducted at ReproCELL.
Tumor cell implantation experiments
HCC827, HCC827-GR-high1, and HCC827-GR-high2 cells were subcutaneously injected into the nonobese diabetic/ severe combined immunodeficient (NOD/SCID) mice purchased from Charles River. Groups of mice were inoculated with each cell line at 5 × 106 . Tumor growth was monitored and individual tumor volumes were measured using a digital caliper and approximated according to the formula V = 1/2ab2 (a, the long diameter and b, the short diameter of the tumor). At the end of experiments, mice were sacrificed after 4 weeks and tumors were harvested, measured, photographed, and pathologically examined.
Immunothistochemical anaylses of clinical samples
Tumor samples were obtained at Okayama University Hospital (Okayama, Japan) with patients’ consent under Institutional Review Board–approved protocols. Biopsied samples after acquisition of EGFR-TKI resistance were fixed in 10% formaldehyde and embedded in paraffin. Immunohistochemical (IHC) staining with ALDH1A1 (diluted 1:400 in PBS), ABCB1 (1:200), E-cadherin (1:1,000), and vimentin (1:200) was conducted. The detailed protocol for the IHC staining has been described previously (21).
Statistical analyses
All data were analyzed using JMP v 9.0.0 software (SAS Institute Inc.). P < 0.05 was considered significant. All tests were two-sided.
Results
Genotypic mechanisms of acquired resistance to EGFR-TKIs
Four cell lines (HCC827, PC-9, HCC4006, and HCC4011) with TKI-sensitive EGFR mutations were exposed to gefitinib by 2 different methods: stepwise escalation (GR-step series) and high-concentration exposure (GR-high series). From these efforts, 9 sublines resistant to gefitinib were established: HCC827-GR-step, PC-9-GR-step, HCC4006-GR-step, HCC4011-GR-step, HCC827-GR-high1, HCC827-GR-high2, PC-9-GR-high, HCC4006-GR-high, and HCC4011-GR-high. The IC50 values against gefitinib and erlotinib of these 9 resistant sublines exceeded 5 µmol/L (Table 1). The expressions of EGFR and its effector proteins in these cell lines were profiled (Supplementary Fig. S1A). To explore the genotypic changes following acquired resistance to EGFR-TKIs, we examined the genomic DNA of both parental and resistant cells. In sublines established with the stepwise escalation method, qPCR revealed that HCC827-GR-step and HCC4011-GR-step exhibited MET amplification (Supplementary Fig. S1B), whereas PC-9-GR-step showed the presence of EGFR T790M mutation detected by direct sequencing (Supplementary Fig. S1C). Among sublines established with the high-concentration method, only HCC4011-GR-high showed MET amplification (Supplementary Fig S1B). These resistance mechanisms were consistent with the results of previous studies (22–24). Neither T790M nor MET amplification was observed in any of the other 5 sublines (HCC4006-GR-step, HCC827-GR-high1, HCC827-GR-high2, PC-9-GR-high, and HCC4006-GR-high). No resistant sublines harbored secondary mutations in the KRAS, NRAS, or BRAF gene.
Table 1.
EGFR-TKI–resistant cell lines and resistant mechanisms
| Cell Line | Gefitinib exposure |
Gefitinib IC50, µmol/L |
Erlotinib IC50, µmol/L |
EGFR T790M |
MET amp |
Other |
|---|---|---|---|---|---|---|
| HCC827 | — | 0.0076 | 0.0042 | No | No | N/A |
| HCC827-GR-step | Stepwise | 9.23 | >10 | No | Yes | — |
| HCC827-GR-high1 | High | 8.84 | >10 | No | No | EMT, stem cell–like properties |
| HCC827-GR-high2 | High | >10 | >10 | No | No | EMT, stem cell–like properties EGFR-WT |
| PC-9 | — | 0.071 | 0.15 | No | No | N/A |
| PC-9-GR-step | Stepwise | >10 | >10 | Yes | No | — |
| PC-9-GR-high | High | >10 | >10 | No | No | Unknown |
| HCC4006 | — | 0.024 | 0.034 | No | No | N/A |
| HCC4006-GR-step | Stepwise | 9.33 | >10 | No | No | EMT |
| HCC4006-GR-high | High | >10 | >10 | No | No | EMT |
| HCC4011 | — | 0.033 | 0.11 | No | No | N/A |
| HCC4011-GR-step | Stepwise | 5.07 | >10 | No | Yes | — |
| HCC4011-GR-high | High | 6.48 | >10 | No | Yes | — |
Abbreviations: amp, amplification; N/A, not applicable; WT, wild-type.
After acquiring resistance to EGFR-TKIs, all sublines except HCC827-GR-high2 retained EGFR mutations, CNG, and protein expression, as determined by direct sequencing, qPCR, and Western blotting, respectively (Supplementary Fig. S1). Originally, parental HCC827 cells showed focal amplification of EGFR with 32.3 copies estimated by FISH and qPCR assays. In HCC827-GR-high2, qPCR, PCR-based length polymorphism and FISH assays revealed progressive decrease in the EGFR-mutant allele through the course of passages leading to the disappearance of focally amplified EGFR alleles (Fig. 1). Sub-cloning of the PCR product from HCC827-GR-high2 produced 100 of 100 clones exhibiting wild-type EGFR instead of the exon 19 deletion, as determined by PCR-based length polymorphism assay. In addition, 3 sublines from independent single cells were established from HCC827-GR-high2. No mutant alleles were detected in 2 of these sublines, whereas a small population of mutant alleles was identified in the third subline as determined by direct sequencing. These data indicate that the focal amplification of the EGFR gene, which was considered a mutant allele, disappeared in HCC827-GR-high2.
Figure 1.
Loss of EGFR-mutant allele and progressive decrease of EGFR copy number in HCC827-derived resistant subline. HCC827-GR-high2 showed progressive decrease in the EGFR-mutant allele through the course of passages, leading to the disappearance of focally amplified EGFR alleles. A and B, fluorescence immunocytochemistry of EGFR E746-A750 deletion mutation-specific protein (A; green, mutation-specific protein; blue, nucleus) and FISH (B; red, EGFR; green, CEP7; blue, nucleus). C, progressive decrease in the EGFR-mutant allele by qPCR and PCR-based length polymorphism assay. P-, passage. Scale bars, 100 µm (A); 10 µm (B).
Phenotypic change in acquiring resistance
Microscopically, each of the 4 sublines, HCC827-GR-high1, HCC827-GR-high2, HCC4006-GR-high, and HCC4006-GR-step, exhibited a spindle cell–like morphology that was different from their parental cell lines. As expected, these 4 sublines displayed EMT features in Western blotting and fluorescence immunocytochemistry for E-cadherin and vimentin (Supplementary Fig. S2A and S2B). In contrast, PC-9 and HCC4011 cells and the derived resistant sublines did not show EMT features.
Expression profile of mRNA and kinases in HCC827 cells
Because we had a great interest in HCC827-GR-high2 whose amplified EGFR-mutant alleles disappeared, we examined the mRNA expression profile in HCC827-GR-high2 by using cDNA microarray. Details of this expression profile are presented in Supplementary Table S2. We identified upregulation of many genes, and particularly noticed upregulation in the expression of genes encoding ALDH1A1 and ABC transporters, which were observed in the cells with stem cell–like properties. The upregulation of stem cell-related markers such as ALDH1A1, ABC transporters, and CD44 was confirmed by qRT-PCR (Fig. 2). In addition, the upregulation of ALDH1A1 in HCC827-GR-highs was confirmed by Western blotting and fluorescent immunocytochemistry (Supplementary Fig. S2C and S2D). ALDH1A1 was not detected in the other sublines.
Figure 2.
Relative gene expression levels of stem cell–related markers by qRT-PCR. The mRNA expressions of ALDH1A1, ABCB1, ABCG2, and CD44 were confirmed by qRT-PCR. The expression of stem cell–related markers ALDH1A1, ABCG2, and CD44 were higher than that of the parental line in HCC827-GR-highs. In addition, the expression of ABCB1 was significantly higher than that of the parental line in HCC827-GR-step, HCC827-GR-highs, PC-9-GR-high, and HCC4006-GR-high.
We conducted phospho-RTK array and phospho-kinase array to find no significant differences including AXL between parental HCC827 and HCC827-GR-highs, except for the down-regulation of phosphorylated EGFR protein in HCC827-GR-highs (Supplementary Fig. S3).
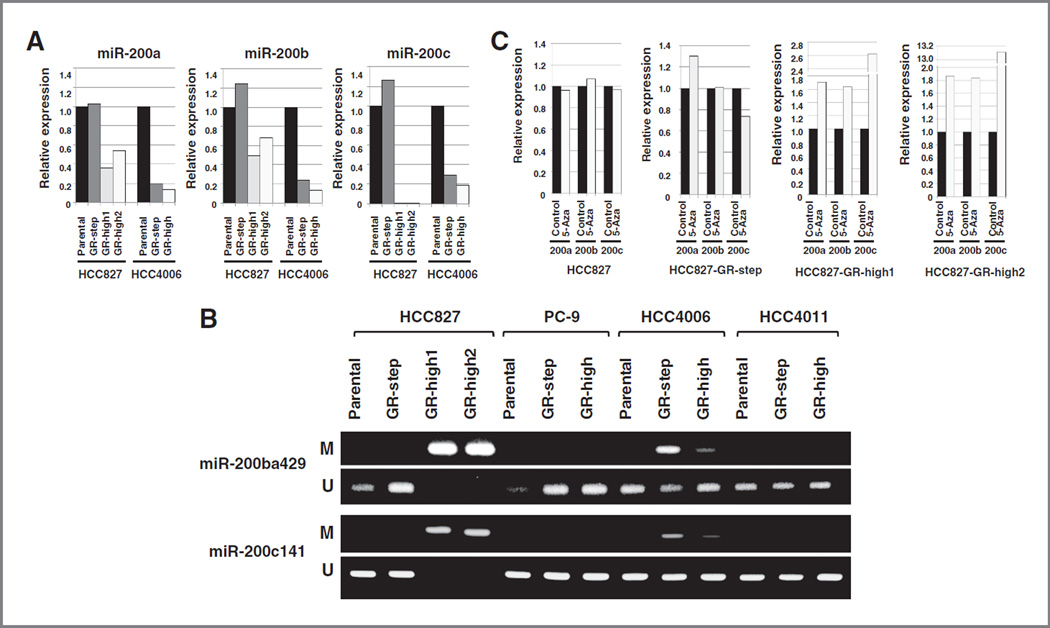
Expression status of miR-200 family in resistant cell lines with EMT features
The result of cDNA microarray in HCC827-GR-high2 indicated the upregulation of Zinc-finger enhancer binding (ZEB) transcription factors (ZEB1 and ZEB2), which are crucial EMT activators (25–27). Because EMT was reported to be regulated by miR-200 family targeting ZEB1 and ZEB2, we analyzed the expression status of the miR-200 family by qRT-PCR. As shown in Fig. 3A, miR-200a, miR-200b, and miR-200c were down-regulated in both HCC827- and HCC4006-derived resistant sublines with EMT features. In particular, miR-200c was extensively downregulated in HCC827-GR-highs compared with parental HCC827. To investigate the mechanism of down-regulation of miR-200 family, we examined the methylation status of miR-200 family by MSP (Fig. 3B) and bisulfite genomic sequencing (data not shown). Our results indicate that miR-200 families were methylated and their expressions were recovered following treatment with 5-aza-2′-deoxycytidine (Fig. 3C).
Figure 3.
CpG island hypermethylation-associated silencing of the miR-200 family in acquired resistance to EGFR-TKI sublines with EMT features. A, the expression of miR-200 family was extensively downregulated in resistant sublines with EMT features compared with parental lines by qRT-PCR. B, the MSP revealed the hypermethylation of miR-200 family in resistant cells with EMT features. C, the miR-200 family expressions were recovered following treatment with DNA-demethylating agent 5-aza-2’ -deoxycytidine (5-Aza) in miR-200 family methylated cells. M, methylated; U, unmethylated.
Stem cell–like property in acquiring resistance
Upregulation of ALDH1A1 and ABC transporters suggests that HCC827-GR-highs may acquire stem cell–like properties. Thus, we quantified the side population by dual wavelength flow cytometry. We found an extreme increase in the number of side-population cells in HCC827-GR-highs as illustrated in Fig. 4A. The majority of the side-population fraction in HCC827-GR-highs was eliminated in the presence of verapamil, indicating the specificity of the side population. In addition, we conducted a sphere formation assay to examine the cellular functional features of stem cell–like properties. We found that HCC827-GR-highs acquired higher ability to form spheres in suspension culture compared with parental HCC827 and HCC827-GR-step (Fig. 4B). To examine the stem cell–like properties in vivo, we conducted tumor transplantation experiments (28, 29). We subcutaneously implanted HCC827, HCC827-GR-high1, and HCC827-GR-high2 cells to examine the tumor-forming capability in NOD/SCID mice. We found that HCC827-GR-highs exhibited higher tumorigenicity than parental HCC827 cells did. The HCC827-GR-highs established larger tumors with shorter latencies than the parental HCC827 cells did (Fig. 4C). HCC827-GR-highs showed a significant increase in the expression of ALDH1A1, as indicated by IHC staining (Supplementary Fig. S4). These results further indicate that HCC827-GR-highs acquired stem cell–like properties. Of interest, the histologic finding of HCC827-GR-highs was different from that of parental HCC827 (Supplementary Fig. S4). Even after culturing of HCC827-GR-highs with gefitinib-free medium for 6 months, HCC827-GR-high2 still exhibited both the EMT and stem cell–like features, and did not exhibit production of EGFR-mutant–specific protein or further increase of either mutant allele or EGFR copy number (Supplementary Fig. S5). The appearance of stem cell–like properties in HCC827-resistant sublines established by high-concentration method was independently confirmed in 3 additional different culture dishes.
Figure 4.
Emergence of the stem cell–like properties in acquiring resistance to EGFR-TKI cells. A, side population analysis shows the extreme increase of side-population cells in HCC827-GR-highs compared with parental cells. The majority of the side-population fraction in HCC827-GR-highs was eliminated in the presence of verapamil. B, by sphere formation assay, HCC827-GR-highs acquired high ability to form spheres in suspension culture. C, the HCC827-GR-highs established larger tumors with shorter latencies than the parental HCC827 cells did in NOD/SCID mice, indicating HCC827-GR-highs exhibited higher tumorigenicity than parental HCC827 cells. D, representative images of IHC staining of pretreatment and recurrent tumor after EGFR-TKI treatment (case no. 5). The postresistant biopsy (right) shows an EMT feature with positive IHC staining for vimentin with expression of stem cell–related marker ALDH1A1. Scale bars, 100 µm.
Gefitinib sensitivity of HCC827 and HCC827-GR-high2 hybridoma
A hybridoma model was generated with parental and resistant cells to distinguish whether the causative factor for EGFR-TKI resistance in HCC827-GR-high2 that exhibited loss of mutant EGFR alleles, EMT, and stem cell–like properties involved either loss- or gain-of-function. A hybridoma cell line was generated by fusing HCC827 with HCC827-GR-high2, which was then treated with gefitinib. The hybridoma exhibited resistance to gefitinib at a concentration of 2 µmol/L, indicating that the resistant cells had acquired drug-resistant properties to parental cells, rather than having lost drug sensitivity.
Sensitivity to various drugs in each cell line
Drug sensitivities against various agents are shown in Table 2. The sublines of HCC827, PC-9, and HCC4006 generated under high concentrations of gefitinib exhibited higher IC50 values for docetaxel and paclitaxel than those of parental cells. Moreover, we examined the antitumor effects of histone deacetylase (HDAC) inhibitors [trichostatin A and vorinostat (SAHA)] and a proteasome inhibitor (bortezo-mib). These inhibitors produced moderate to strong anti-tumor effects in both parental and resistant cells, which did not acquire resistance to these drugs (Table 2; refs. 30, 31).
Table 2.
IC50 values (µmol/L) against various agents
| Cell line | Chemotherapeutic agent |
HDAC inhibitor |
Proteasome inhibitor Bortezomib |
|||
|---|---|---|---|---|---|---|
| CDDP | DOC | PTX | TSA | SAHA | ||
| HCC827 | 4.51 | 0.0021 | 0.0032 | 0.082 | 1.85 | 0.0044 |
| HCC827-GR-step | 4.29 | 0.0020 | 0.0020 | 0.092 | 0.63 | 0.0072 |
| HCC827-GR-high1 | 4.45 | 0.022a | 0.15a | 0.097 | 2.05 | 0.0061 |
| HCC827-GR-high2 | 8.04 | 0.51a | 1.46a | 0.092 | 2.20 | 0.0074 |
| PC-9 | 2.92 | 0.00066 | 0.0014 | 0.020 | 1.06 | 0.0097 |
| PC-9-GR-step | 2.49 | 0.0060 | 0.0014 | 0.018 | 1.14 | 0.0073 |
| PC-9-GR-high | 5.64 | 0.0020a | 0.0022 | 0.026 | 1.03 | 0.017 |
| HCC4006 | >10 | 0.038 | 0.038 | 0.55 | 9.15 | 0.13 |
| HCC4006-GR-step | >10 | 0.025 | 0.015 | 0.13 | 5.94 | 0.14 |
| HCC4006-GR-high | >10 | 0.824a | 1.10a | 2.22 | 8.20 | 0.15 |
| HCC4011 | >10 | 0.0011 | 0.0014 | 0.021 | 0.97 | 0.0033 |
| HCC4011-GR-step | >10 | 0.00069 | 0.0017 | 0.017 | 0.86 | 0.0061 |
| HCC4011-GR-high | >10 | 0.00034 | 0.0014 | 0.018 | 0.93 | 0.0055 |
Abbreviations: CDDP, cisplatin; DOC, docetaxel; PTX, paclitaxel; TSA, trichostatin A.
The ratio of the IC50 value in each resistant line to the parental line is higher than 10 times.
Molecular profile of EGFR-TKI–resistant clinical samples
Clinical tumor samples, which showed acquired resistance to TKIs, were collected both before and after TKI treatment and examined genetically and immunohistologically (Table 3). Among 16 cases with acquired resistance to TKIs, corresponding pretreatment samples were available in 3 cases (no. 1, 5, and 16). After acquiring resistance, 3 cases exhibited EGFR T790M mutation and 2 exhibited MET amplification. In addition, some samples harboring EMT features (based on E-cadherin and vimentin expression status) also exhibited expression of stem cell–related markers ALDH1A1 and ABCB1, determined by IHC staining (Fig. 4D). In total, 5 of 16 cases exhibited ALDH1A1 expression in samples that showed acquired resistance to TKI. In 3 cases whose pretreatment samples were available, ALDH1A1 was not expressed prior to TKI treatment. Among them, 2 cases (no. 5 and 16) exhibited ALDH1A1 expression after acquiring resistance to TKI. Of note, case no. 5 was a patient with recurrent lung cancer after surgery and no other anticancer drugs except gefitinib and erlotinib were administrated.
Table 3.
Acquired resistance to EGFR-TKIs; clinical samples
| No. | Age | Sex | EGFR mutation | Genetic alteration | Immunohistochemistry |
||
|---|---|---|---|---|---|---|---|
| Vimentin | ALDH1A1 | ABCB1 | |||||
| 1 | 88 | F | L858R | T790M | −/− | −/− | +/+ |
| 2 | 72 | F | 19 del | T790M | N/A | N/A | N/A |
| 3 | 53 | F | 19 del | N/A | N/A | N/A | |
| 4 | 34 | F | 19 del | Loss of EGFR-mut | + | N/A | N/A |
| 5 | 75 | F | L858R | −/+ | −/+ | +/+ | |
| 6 | 43 | M | 19 del | ||||
| 7 | 73 | F | 19 del | MET amp | |||
| 8 | 62 | F | 19 del | + | − | − | |
| 9 | 70 | M | 19 del | MET amp | − | − | + |
| 10 | 52 | F | 19 del | T790M | − | − | + |
| 11 | 49 | M | L858R | + | + | + | |
| 12 | 65 | M | L858R | − | − | + | |
| 13 | 43 | M | 19 del | − | − | + | |
| 14 | 59 | F | G719C | − | + | + | |
| 15 | 53 | M | L858R | + | + | + | |
| 16 | 71 | F | L858R | −/+ | −/+ | +/+ | |
NOTE: Among 16 cases with acquired resistance to TKIs, corresponding pretreatment samples were available in 3 cases (no. 1,5, and 16).
Abbreviations: amp, amplification; del, deletion; mut, mutation; N/A, not applicable.
Discussion
In this study, we showed that the method of drug exposure in cell culture influences the mechanisms of acquired resistance to EGFR-TKI. Studies using EGFR-mutant cell lines have indicated that the different types of resistance mechanisms are determined within the individual cell lines in response to certain conditions. For instance, both PC-9 and H3255 are known to develop resistance to EGFR-TKIs through EGFR T790M mutation as a result of stepwise escalation exposure (22, 23). On the other hand, HCC827 is known to overcome EGFR-TKI through MET amplification (8, 32). Interestingly, Suda and colleagues reported that HCC827 cells developed the T790M mutation under the inhibition of MET signaling, suggesting that the microenvironment of the tumor cells influenced the mechanisms of resistance (32). Indeed, in an analysis using multiple gefitinib refractory tumors obtained from autopsies, the lesions from patients exhibited T790M and/or MET amplification depending on the lesion sites (32). In addition to these resistance mechanisms accompanying somatic gene alterations, recent studies have indicated that some biologic signatures such as acquisition of EMT pheno-type and transformation to SCLC were associated with EGFR-TKI resistance, the causative genetic alterations of which are not known (11, 33, 34). EMT was observed in HCC4006 sublines and HCC827-GR-highs, but not in HCC827-GR-step sublines. Summarily, these observations suggest that cancer cells might be able to enact different mechanisms based on the microenvironment to survive and escape cell death from apoptotic pressure of EGFR-TKI.
Among identified EMT-related genes, ZEB1 expression was reported to be most significantly correlated with mesenchymal phenotype in human malignancies including NSCLC (25, 26). The cDNA array revealed upregulation of ZEB1 and ZEB2 expression in HCC827-GR-high2 and we consequently focused on the miR-200 family, which is reported to repress ZEB1 as a key regulator of EMT (35). Indeed, our results indicate down-regulated expression of the miR-200 family, especially miR-200c, in resistant sublines with EMT features. Moreover, a recent study has indicated that loss of miR-200c expression with DNA methylation is associated with chemoresistant phenotype in NSCLC (36). Of note, it is now known that EMT activators not only activate cellular motility but are also associated with the maintenance of stem cell properties and cell survival (37, 38). Our findings present the novel insight that the repression of miR-200 family by DNA methylation is responsible for EMT during the acquisition of resistance to EGFR-TKI.
As an important finding, some resistant cells with EMT signatures exhibited stem cell–like properties. Cancer stem cells (CSC), which are characterized by the capacity for pluripotency and self-renewal, have been attracting interest as a source of cancer cells (39). The significance of stem cell–like properties in lung cancer has been investigated in both basic and clinical research (40, 41). However, the CSC of lung cancers remains a subject of ongoing research, and its specific makers have not yet been identified. In our study, several cell surface proteins, including CD133, that may be candidate markers of general CSC, were not upregulated in resistant sublines. These results collectively suggest that understanding and overcoming drug resistance from the viewpoint of stem cell identity may present new and challenging opportunities.
We examined the sensitivity of various types of drugs, including conventional chemotherapeutic agents, HDAC inhibitors, and proteasome inhibitor, to resistant sublines. HCC827-GR-highs, HCC4006-GR-high, and PC-9-GR-high exhibited significant resistance to docetaxel and paclitaxel, but not to cisplatin. This result is reasonable because docetaxel and paclitaxel, unlike cisplatin, are considered to be effluxed by the ABC transporter system, which was upregulated in these sublines. These results would lead to selection of appropriate chemotherapeutic drugs following acquired resistance to EGFR-TKI.
In our study, clinically usable HDAC inhibitor and protea-some inhibitor SAHA and bortezomib exhibited similar anti-tumor efficacy for both parental and resistant cells. Clinical studies have shown that SAHA is effective for NSCLC when combined with other cancer therapies (42, 43). Notably, HDAC inhibitors are reported to be effective in treating chronic myelogenous leukemia, in which stem cells appeared after the acquisition of resistance to imatinib mesylate (44). The protea-some inhibitor, bortezomib failed to produce antitumor effects either alone or in conjunction with other drugs in a clinical trial, although preliminary data suggested that bortezomib as a single agent may show antitumor activity in patients with NSCLC (45, 46). However, current research is rapidly working toward the development of next-generation proteasome inhibitors (47), and our data indicating that bortezomib activity was not influenced by the EGFR-TKI resistance state may be useful for the future development of proteasome inhibitors.
Our results support the usefulness of in vitro experiment to investigate the mechanisms of resistance to EGFR-TKI. In the pharmacokinetic analysis of gefitinib, the plasma concentration of gefitinib was found to reach a steady-state level within 7 days, in most of the cases (48). Nakamura and colleagues reported that the plasma concentration of gefitinib in patients receiving 250 mg gefitinib daily ranged from 115 to 2,012 ng/mL (0.257–4.502 µmol/L) on day 3 (D3) and 126 to 2,926 ng/mL (0.282–6.547 µmol/L) on day 8 (D8), whereas the median D8-to-D3 ratio was 1.578 and ranged from 0.758 to 6.094 (49). These results indicate considerable variation in plasma concentration and the pharmacokinetics of gefitinib according to individual patients. Of note, D8-to-D3 ratio under 1.0 indicates that drug concentration may reach a plateau shortly after initiation of gefitinib treatment. This condition may be similar to that of drug contact to cells in our high-concentration method. In addition, Haura and colleagues reported that tumor levels during treatment with gefitinib were higher than, but not related to, plasma levels (50). Further resistance-related research will require additional elaboration about culture conditions and microenvironment.
It is still not known what caused the emergence of stem cell–like properties in HCC827-GR-highs; however, 2 possibilities should be considered: (i) high-concentration exposure induces cells with stem cell–like properties; and (ii) the cells with stem cell–like properties existed as minor clones in HCC827 prior to gefitinib exposure, and these were finally selected as the major clones. For the latter possibility, it is also not clear as to why cells with stem–like properties appeared as the major population only from the high-concentration exposure method.
In conclusion, culture conditions with EGFR-TKI seem to influence the mechanism of acquired resistance, suggesting that the microenvironment is a determinating factor for the mechanisms underlying acquisition of resistance to EGFR-TKI. Our study indicated that EGFR-TKI treatment induced stem cell–like properties and is associated with EGFR-TKI resistance.
Supplementary Material
Acknowledgments
The authors thank Ms. Fumiko Isobe (Department of Cancer and Thoracic Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan) for her excellent technical support.
Footnotes
Note: Supplementary data for this article are available at Cancer Research Online (http://cancerres.aacrjournals.org/).
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Authors’ Contributions
Conception and design: K. Shien, S. Toyooka, Y. Maki, A.F. Gazdar
Development of methodology: K. Shien, S. Toyooka, H. Asano
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): K. Shien, S. Toyooka, S. Hashida, N. Takigawa, K. Kiura, S. Miyoshi
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): K. Shien, J. Soh, K.L. Thu, W.L. Lam
Writing, review, and/or revision of the manuscript: K. Shien, S. Toyooka, H. Yamamoto, J. Soh, E. Ichihara, A.F. Gazdar, W.L. Lam, S. Miyoshi
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): K. Shien, S. Toyooka, M. Jida, Y. Maki
Study supervision: H. Asano, K. Tsukuda, S. Miyoshi
References
- 1.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 2.Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 3.Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–957. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 4.Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, et al. Gefitinib or chemotherapy for non–small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 5.Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, et al. Gefitinib versus cisplatin plus docetaxel in patients with non- small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–128. doi: 10.1016/S1470-2045(09)70364-X. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi S, Boggon TJ, Dayaram T, Jäanne PA, Kocher O, Meyerson M, et al. EGFR mutation and resistance of non–small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- 7.Pao W, Miller VA, Politi KA, Riely GJ, Somwar R, Zakowski MF, et al. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS Med. 2005;2:e73. doi: 10.1371/journal.pmed.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–1043. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 9.Bean J, Brennan C, Shih JY, Riely G, Viale A, Wang L, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci U S A. 2007;104:20932–20937. doi: 10.1073/pnas.0710370104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yano S, Wang W, Li Q, Matsumoto K, Sakurama H, Nakamura T, et al. Hepatocyte growth factor induces gefitinib resistance of lung adeno-carcinoma with epidermal growth factor receptor-activating mutations. Cancer Res. 2008;68:9479–9487. doi: 10.1158/0008-5472.CAN-08-1643. [DOI] [PubMed] [Google Scholar]
- 11.Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3:75ra26. doi: 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Z, Lee JC, Lin L, Olivas V, Au V, Laframboise T, et al. Activation of the AXL kinase causes resistance to EGFR-targeted therapy in lung cancer. Nat Genet. 2012;44:852–860. doi: 10.1038/ng.2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tabara K, Kanda R, Sonoda K, Kubo T, Murakami Y, Kawahara A, et al. Loss of activating EGFR mutant gene contributes to acquired resistance to EGFR tyrosine kinase inhibitors in lung cancer cells. PLoS ONE. 2012;7:e41017. doi: 10.1371/journal.pone.0041017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sagawa Y, Fujitoh A, Nishi H, Ito H, Yudate T, Isaka K. Establishment of three cisplatin-resistant endometrial cancer cell lines using two methods of cisplatin exposure. Tumour Biol. 2011;32:399–408. doi: 10.1007/s13277-010-0133-6. [DOI] [PubMed] [Google Scholar]
- 15.Shien K, Ueno T, Tsukuda K, Soh J, Suda K, Kubo T, et al. Knockdown of the epidermal growth factor receptor gene to investigate its therapeutic potential for the treatment of non–small-cell lung cancers. Clin Lung Cancer. 2012;13:488–493. doi: 10.1016/j.cllc.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Asano H, Toyooka S, Tokumo M, Ichimura K, Aoe K, Ito S, et al. Detection of EGFR gene mutation in lung cancer by mutant-enriched polymerase chain reaction assay. Clin Cancer Res. 2006;12:43–48. doi: 10.1158/1078-0432.CCR-05-0934. [DOI] [PubMed] [Google Scholar]
- 17.Soh J, Okumura N, Lockwood WW, Yamamoto H, Shigematsu H, Zhang W, et al. Oncogene mutations, copy number gains and mutant allele specific imbalance (MASI) frequently occur together in tumor cells. PLoS ONE. 2009;4:e7464. doi: 10.1371/journal.pone.0007464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kubo T, Yamamoto H, Lockwood WW, Valencia I, Soh J, Peyton M, et al. MET gene amplification or EGFR mutation activate MET in lung cancers untreated with EGFR tyrosine kinase inhibitors. Int J Cancer. 2009;124:1778–1784. doi: 10.1002/ijc.24150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davalos V, Moutinho C, Villanueva A, Boque R, Silva P, Carneiro F, et al. Dynamic epigenetic regulation of the microRNA-200 family mediates epithelial and mesenchymal transitions in human tumorigenesis. Oncogene. 2012;31:2062–2074. doi: 10.1038/onc.2011.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodell MA, Brose K, Paradis G, Conner AS, Mulligan RC. Isolation and functional properties of murine hematopoietic stem cells that are replicating in vivo . J Exp Med. 1996;183:1797–1806. doi: 10.1084/jem.183.4.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shien K, Toyooka S, Ichimura K, Soh J, Furukawa M, Maki Y, et al. Prognostic impact of cancer stem cell-related markers in non-small cell lung cancer patients treated with induction chemoradiotherapy. Lung Cancer. 2012;77:162–167. doi: 10.1016/j.lungcan.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Ogino A, Kitao H, Hirano S, Uchida A, Ishiai M, Kozuki T, et al. Emergence of epidermal growth factor receptor T790M mutation during chronic exposure to gefitinib in a non small cell lung cancer cell line. Cancer Res. 2007;67:7807–7814. doi: 10.1158/0008-5472.CAN-07-0681. [DOI] [PubMed] [Google Scholar]
- 23.Engelman JA, Mukohara T, Zejnullahu K, Lifshits E, Borrás AM, Gale CM, et al. Allelic dilution obscures detection of a biologically significant resistance mutation in EGFR-amplified lung cancer. J Clin Invest. 2006;116:2695–2706. doi: 10.1172/JCI28656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ohashi K, Sequist LV, Arcila ME, Moran T, Chmielecki J, Lin YL, et al. Lung cancers with acquired resistance to EGFR inhibitors occasionally harbor BRAF gene mutations but lack mutations in KRAS, NRAS, or MEK1. Proc Natl Acad Sci USA. 2012;109:E2127–E2133. doi: 10.1073/pnas.1203530109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10:593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 26.Park SM, Gaur AB, Lengyel E, Peter ME. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brabletz S, Brabletz T. The ZEB/miR-200 feedback loop -a motor of cellular plasticity in development and cancer? EMBO Rep. 2010;11:670–677. doi: 10.1038/embor.2010.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–768. doi: 10.1038/nrc2499. [DOI] [PubMed] [Google Scholar]
- 29.Rosen JM, Jordan CT. The increasing complexity of the cancer stem cell paradigm. Science. 2009;324:1670–1673. doi: 10.1126/science.1171837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miyanaga A, Gemma A, Noro R, Kataoka K, Matsuda K, Nara M, et al. Antitumor activity of histone deacetylase inhibitors in non–small cell lung cancer cells: development of a molecular predictive model. Mol Cancer Ther. 2008;7:1923–1930. doi: 10.1158/1535-7163.MCT-07-2140. [DOI] [PubMed] [Google Scholar]
- 31.Scagliotti G. Proteasome inhibitors in lung cancer. Crit Rev Oncol Hematol. 2006;58:177–189. doi: 10.1016/j.critrevonc.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Suda K, Murakami I, Katayama T, Tomizawa K, Osada H, Sekido Y, et al. Reciprocal and complementary role of MET amplification and EGFR T790M mutation in acquired resistance to kinase inhibitors in lung cancer. Clin Cancer Res. 2010;16:5489–5498. doi: 10.1158/1078-0432.CCR-10-1371. [DOI] [PubMed] [Google Scholar]
- 33.Rho JK, Choi YJ, Lee JK, Ryoo BY, Na II, Yang SH, et al. Epithelial to mesenchymal transition derived from repeated exposure to gefitinib determines the sensitivity to EGFR inhibitors in A549, a non–small cell lung cancer cell line. Lung Cancer. 2009;63:219–226. doi: 10.1016/j.lungcan.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 34.Suda K, Tomizawa K, Fujii M, Murakami H, Osada H, Maehara Y, et al. Epithelial to mesenchymal transition in an epidermal growth factor receptor-mutant lung cancer cell line with acquired resistance to erlotinib. J Thorac Oncol. 2011;6:1152–1161. doi: 10.1097/JTO.0b013e318216ee52. [DOI] [PubMed] [Google Scholar]
- 35.Mongroo PS, Rustgi AK. The role of the miR-200 family in epithelial–mesenchymal transition. Cancer Biol Ther. 2010;10:219–2122. doi: 10.4161/cbt.10.6312548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ceppi P, Mudduluru G, Kumarswamy R, Rapa I, Scagliotti GV, Papotti M, et al. Loss of miR-200c expression induces an aggressive, invasive, and chemoresistant phenotype in non–small cell lung cancer. Mol Cancer Res. 2010;8:1207–1216. doi: 10.1158/1541-7786.MCR-10-0052. [DOI] [PubMed] [Google Scholar]
- 37.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morel AP, Lièvre M, Thomas C, Hinkal G, Ansieau S, Puisieux A. Generation of breast cancer stem cells through epithelial–mesenchymal transition. PLoS ONE. 2008;3:e2888. doi: 10.1371/journal.pone.0002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 40.Eramo A, Lotti F, Sette G, Pilozzi E, Biffoni M, Di Virgilio A, et al. Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ. 2008;15:504–514. doi: 10.1038/sj.cdd.4402283. [DOI] [PubMed] [Google Scholar]
- 41.Berns A. Stem cells for lung cancer? Cell. 2005;121:811–813. doi: 10.1016/j.cell.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 42.Ramalingam SS, Maitland ML, Frankel P, Argiris AE, Koczywas M, Gitlitz B, et al. Carboplatin and Paclitaxel in combination with either vorinostat or placebo for first-line therapy of advanced non–small-cell lung cancer. J Clin Oncol. 2010;28:56–62. doi: 10.1200/JCO.2009.24.9094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Traynor AM, Dubey S, Eickhoff JC, Kolesar JM, Schell K, Huie MS, et al. Vorinostat (NSC# 701852) in patients with relapsed non-small cell lung cancer: a Wisconsin Oncology Network phase II study. J Thorac Oncol. 2009;4:522–526. doi: 10.1097/jto.0b013e3181952478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang B, Strauss AC, Chu S, Li M, Ho Y, Shiang KD, et al. Effective targeting of quiescent chronic myelogenous leukemia stem cells by histone deacetylase inhibitors in combination with imatinib mesylate. Cancer Cell. 2010;17:427–442. doi: 10.1016/j.ccr.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fanucchi MP, Fossella FV, Belt R, Natale R, Fidias P, Carbone DP, et al. Randomized phase II study of bortezomib alone and bortezomib in combination with docetaxel in previously treated advanced non–small -cell lung cancer. J Clin Oncol. 2006;24:5025–5033. doi: 10.1200/JCO.2006.06.1853. [DOI] [PubMed] [Google Scholar]
- 46.Ramalingam SS, Davies AM, Longmate J, Edelman MJ, Lara PN, Jr, Vokes EE, et al. Bortezomib for patients with advanced-stage bronch-ioloalveolar carcinoma: a California Cancer Consortium Phase II study (NCI 7003) J Thorac Oncol. 2011;6:1741–1745. doi: 10.1097/JTO.0b013e318225924c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dick LR, Fleming PE. Building on bortezomib: second-generation proteasome inhibitors as anti-cancer therapy. Drug Discov Today. 2010;15:243–249. doi: 10.1016/j.drudis.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 48.Baselga J, Rischin D, Ranson M, Calvert H, Raymond E, Kieback DG, et al. Phase I safety, pharmacokinetic, and pharmacodynamic trial of ZD1839, a selective oral epidermal growth factor receptor tyrosine kinase inhibitor, in patients with five selected solid tumor types. J Clin Oncol. 2002;20:4292–4302. doi: 10.1200/JCO.2002.03.100. [DOI] [PubMed] [Google Scholar]
- 49.Nakamura Y, Sano K, Soda H, Takatani H, Fukuda M, Nagashima S, et al. Pharmacokinetics of gefitinib predicts antitumor activity for advanced non -small cell lung cancer. J Thorac Oncol. 2010;5:1404–1409. doi: 10.1097/JTO.0b013e3181e59a7b. [DOI] [PubMed] [Google Scholar]
- 50.Haura EB, Sommers E, Song L, Chiappori A, Becker A. A pilot study of preoperative gefitinib for early-stage lung cancer to assess intratumor drug concentration and pathways mediating primary resistance. J Thorac Oncol. 2010;5:1806–1814. doi: 10.1097/JTO.0b013e3181f38f70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.