Abstract
Background
HIV-infected individuals with a history of transmission via injection drug use (IDU) have poorer survival than other risk groups. The extent to which higher rates of hepatitis C (HCV) infection in IDU explain survival differences is unclear.
Methods
Adults who started antiretroviral therapy (ART) between 2000-2009 in 16 European and North American cohorts with >70% complete data on HCV status were followed for 3 years. We estimated unadjusted and adjusted [for age, sex, baseline CD4 count and HIV-1 RNA, AIDS diagnosis prior to ART, and stratified by cohort] mortality hazard ratios (HR) for IDU (versus non-IDU) and for HCV-infected (versus HCV-uninfected).
Results
Of 32,703 patients 3,374 (10%) were IDU; 4,630 (14%) HCV+; 1,116 (3.4%) died. Mortality was higher in IDU compared with non-IDU (adjusted HR 2.71; 95% CI 2.32,3.16) and in HCV+ compared with HCV− (2.65; 2.31,3.04). The effect of IDU was substantially attenuated (1.57; 1.27,1.94) after adjustment for HCV, while attenuation of the effect of HCV was less substantial (2.04; 1.68,2.47) after adjustment for IDU. Both IDU and HCV were strongly associated with liver-related mortality (10.89; 6.47,18.3 for IDU and 14.0; 8.05,24.5 for HCV) with greater attenuation of the effect of IDU (2.43; 1.24,4.78) than for HCV (7.97; 3.83,16.6). Rates of CNS, respiratory and violent deaths remained elevated in IDU after adjustment for HCV.
Conclusions
A substantial proportion of the excess mortality in HIV-infected IDU is explained by HCV co-infection. These findings underscore the potential impact on mortality of new treatments for HCV in HIV-infected people.
Keywords: HIV-1, Hepatitis C virus, injection drug use, antiretroviral therapy, cohort study, mortality
Introduction
Treated HIV-infected people with a history of injection drug use (IDU) have substantially poorer survival than those in other transmission risk groups, both before and after adjustment for patient characteristics at the time of starting antiretroviral therapy (ART) (1, 2). The excess mortality associated with a history of IDU varies considerably between settings (3), suggesting that IDU may be a proxy for more direct causes of death such as violence (4), overdose (5), higher rates of smoking (6), poorer ART adherence (7), more frequent bacterial infections (8), or greater overall organ system injury (9, 10). Interventions to end or reduce substance abuse may reduce excess mortality among IDU via effects on these risk factors (11).
IDU is a major risk factor for chronic hepatitis C (HCV) infection, the prevalence of which varies among injection drug using populations (12, 13). Excess mortality attributable to HCV may not be addressed by interventions to reduce harm from substance abuse, because the infection often persists after injection drug use has stopped. An improved understanding of the contribution of HCV and general organ system injury to higher mortality rates among HIV positive patients with a history IDU who are treated with ART is urgently needed, now that highly effective treatments for HCV infection are available because this data would inform clinical and cost-effectiveness analyses of the benefit of HCV treatment in dual infected patients (14, 15).
Based on a collaboration of HIV cohort studies, we aimed to determine whether the association between IDU and mortality that we previously reported (1, 16) is explained by differential rates of HCV infection. We also examined whether IDU is independently predictive of non-violent deaths. Our hypothesis was that, after adjustment for HCV infection, IDU no longer has an independent association with all-cause or cause-specific mortality.
Methods
Cohort and patient selection
The Antiretroviral Therapy Cohort Collaboration (ART-CC), which is described in detail elsewhere (17), is an international collaboration of cohorts from North America and Europe that combines data on HIV-infected individuals who were antiretroviral-naïve when they started ART with a combination of at least three drugs. This study was based on data from sixteen cohorts that recorded history of IDU and for which data on HCV test status was >70% complete. The included cohorts were: the AIDS Therapy Evaluation Project Netherlands (ATHENA); French Hospital Database on HIV (FHDH); Aquitaine Cohort, France; Departments of Internal Medicine at University of Cologne and Bonn, Germany; Italian Cohort of Antiretroviral-Naïve Patients (ICONA); CORIS, Spain; Proyecto para la Informatización del Seguimiento Clínico-epidemiológico de la Infección por HIV y SIDA (PISCIS), Spain; Royal Free Hospital Cohort, London UK; Swiss HIV Cohort Study (SHCS); The multicenter Study Group on EuroSIDA; Southern Alberta Clinic, Canada; HIV Atlanta Veterans affairs Cohort Study (HAVACS), USA; UAB 1917 Clinic Cohort, Birmingham, Alabama, USA; Veterans Ageing Cohort Study (VACS8),USA; Vanderbilt-Meharry Center for AIDS Research Nashville, Tennessee, USA; University of Washington HIV Cohort, Seattle, WA, USA. Cohorts were checked for overlap and duplicate patients removed. Institutional review boards from each cohort approved analysis of routinely collected data. Eligible patients were HIV-positive, age ≥16 years, and initiated ART between 2000 and 2009. All patients had CD4 cell count and HIV-1 RNA measured in the period from three months before to one month after ART initiation. HCV+ status was defined as a positive antibody test or positive plasma HCV-RNA viral load. IDU status refers to HIV transmission risk group recorded by the cohort: records of ongoing active injection drug use were not available in these data. All transmission risk groups except IDU were categorised as non-IDU (men who have sex with men, heterosexual, blood, other/unknown). Patients with missing HCV status were excluded from analyses. Patients were followed up for death within 3 years of starting of ART. Causes of death were classified using methodology adapted from the CoDe system (www.chip.dk/CoDe/tabid/55/Default.aspx) using methods reported previously (4). The NHS Health Research Authority South West - Cornwall and Plymouth Research Ethics Committee, UK, approved the study (REC reference 12/SW/0253).
Statistical analysis
Patient demographics and clinical characteristics at start of ART were tabulated and differences between those who were and were not HCV positive were examined using chi-squared statistics and the Wilcoxon rank-sum test for medians. Kaplan-Meier estimates of cumulative survival were plotted by HCV and IDU status and log-rank tests were used to compare survival curves. Follow up was from initiation of ART (“baseline”), and was censored at 3 years to avoid violation of the proportional hazards assumption. Cox models were used to estimate unadjusted and adjusted [for age (16-29, 30-39, 40-49, 50-59, ≥60 years), sex, baseline CD4 cell count (<50, 50-99, 100-199, 200-349, ≥350 cells/mm3), baseline HIV-1 RNA (<10 000, 10 000-99 999, ≥100 000 copies/mL), AIDS diagnosis prior to ART] mortality hazard ratios (HR) for IDU (versus non-IDU) and for HCV+ (versus HCV uninfected), before and after adjusting the effect of each for the other. All models were stratified by cohort. We tested for interactions between age and both IDU and HCV status. We repeated analyses stratifying by age (<45, ≥45 years). We also tested for interactions between sex and both IDU and HCV status.
In a sensitivity analysis, we assessed the effect of possible misclassification of both IDU and HCV status on hazard ratios. We calculated positive predictive values of IDU and HCV status using plausible values for sensitivity and specificity which were based on consensus expert clinician opinion of conservative estimates for these parameters, and used these to define weights that were used to adjust for misclassification of IDU, HCV and both variables simultaneously.
In a second sensitivity analyses we excluded patients with “other/unknown” risk transmission group and repeated the main analysis re-estimating the crude and adjusted mortality HR for IDU and HCV status.
We estimated adjusted hazard ratios for different causes of death [AIDS, non-AIDS infection, liver-related, non-AIDS malignancy, myocardial infarction/ischaemic heart disease, stroke, renal failure, violence (includes suicide and substance abuse), central nervous system (other than stroke), other heart /vascular disease, and respiratory disease (includes chronic obstructive pulmonary disease), other (includes infrequent causes of death), and unknown (includes unclassifiable)]. All analyses were performed using Stata version 12.1.
Results
Data on HCV status were available on 32,703/39,249 (83%) patients, of whom 1,116 (3.4%) died within 3 years of starting ART during 931,485 person-years of follow up. 3,374 (10.3%) patients had presumed HIV transmission via IDU and 4,630 (14.2%) had tested positive for HCV (HCV+). Compared with those in the study population, the proportion of patients who were IDU was lower in those without HCV status recorded (8% vs. 10%). Table 1 shows patient demographics and clinical characteristics at start of ART according to HCV status. Compared with HCV uninfected individuals, those HCV+ were more likely to be aged between 30-49 years old, have started ART in earlier years and to have a history of IDU. CD4 cell counts at start of ART were similar in HCV infected and uninfected individuals.
Table 1.
Patient demographics and clinical characteristics at start of ART by HCV status.
| HCV uninfected N (%) | HCV infected N (%) | P difference | |
|---|---|---|---|
| Number of patients | 28073 (86%) | 4630 (14%) | |
| Number of deaths | 810 (3%) | 306 (7%) | |
| Male | 18891 (67%) | 3299 (71%) | <0.001 |
| IDU | 506 (2%) | 2868 (62%) | <0.001 |
| Age (median (IQR)) years | 37 (31 - 45) | 39 (34 - 44) | <0.001 |
| 16-29 | 5811 (21%) | 490 (11%) | |
| 30-39 | 10833 (39%) | 1998 (43%) | |
| 40-49 | 7085 (25%) | 1710 (37%) | |
| 50-59 | 3115 (11%) | 323 (7%) | |
| ≥ 60 | 1229 (4%) | 109 (2%) | |
| AIDS before ART | 6607 (24%) | 998 (22%) | 0.003 |
| CD4 (median (IQR)) cell/mm 3 | 208 (93 - 312) | 206 (101 – 314) | 0.16 |
| <50 | 4526 (16%) | 666 (14%) | |
| 50-99 | 2782 (10%) | 467 (10%) | |
| 100-199 | 6082 (22%) | 1081 (23%) | |
| 200-349 | 9299 (33%) | 1498 (32%) | |
| ≥ 350 | 5384 (19%) | 918 (20%) | |
| HIV-RNA (median(IQR)) log copies/mL | 4.85 (4.12 – 5.36) | 4.76 (3.89 – 5.27) | <0.001 |
| Year of starting ART | <0.001 | ||
| 2000-2002 | 10827 (37%) | 2100 (45%) | |
| 2003-2005 | 10344 (37%) | 1585 (34%) | |
| 2006-2009 | 7442 (27%) | 945 (20%) |
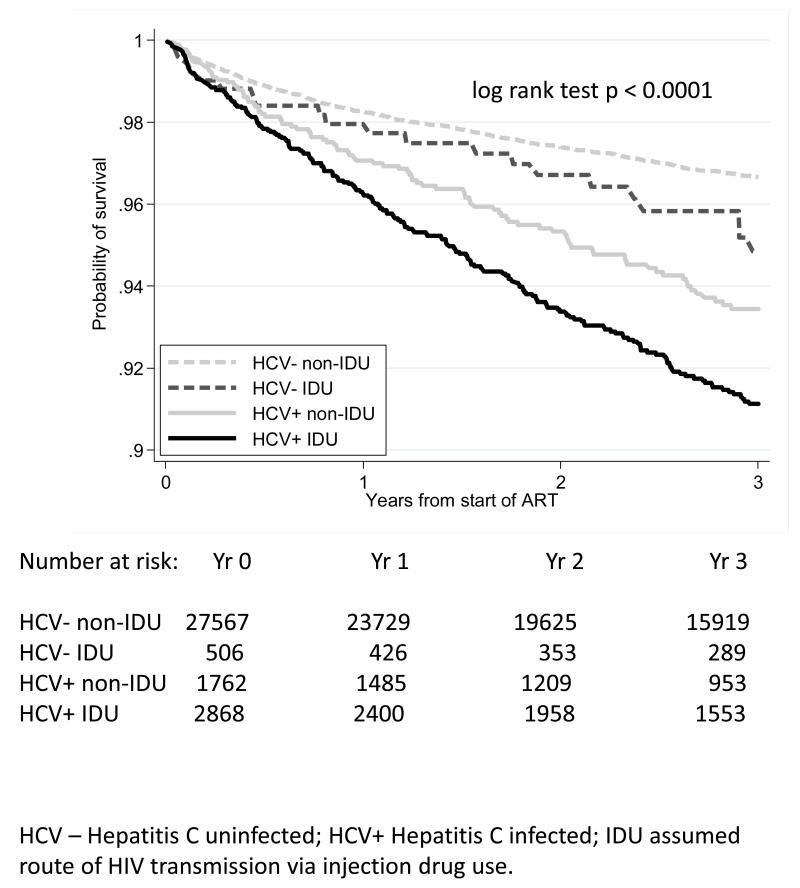
The prevalence of HCV among IDU was 85%: this varied from 36% to 92% between cohorts. 38% of HCV+ were non-IDU. Figure 1 shows Kaplan-Meier survival curves by HCV and IDU status. Survival was worst for HCV+ IDU and somewhat better for HCV+, non IDU. Patients who were HCV uninfected had better survival than HCV+ whether or not their transmission was via IDU, with IDU having worse survival than non-IDU within HCV strata. The survival curves were different overall, (p <0.0001 log-rank test), and between HCV+ and HCV uninfected in both non-IDU (p <0.0001) and IDU (p = 0.009). The survival curves for IDU compared with non-IDU differed more amongst HCV+ (p = 0.01), than amongst HCV uninfected patients (p = 0.08).
Figure 1.
Kaplan-Meier estimate of survival probability by HCV status and IDU transmission group.
Table 2 shows unadjusted and adjusted mortality HR for IDU versus non-IDU and for HCV+ versus HCV uninfected. HRs for both IDU and HCV were similar and substantially elevated. They increased after adjustment for age, sex, and baseline CD4, HIV-1 RNA, and AIDS diagnoses, to 2.71 (95% CI 2.32, 3.16) for IDU and 2.65 (2.31, 3.04) for HCV. When IDU and HCV were included in the same model, attenuation of the HR for IDU (1.57; 95% CI 1.27, 1.94) was more marked than attenuation of the HR for HCV (2.04; 1.68, 2.47). There was little evidence of interaction between sex and either IDU (p = 0.07), or HCV status (p = 0.06). There was strong evidence of interaction (P<0.001) between both IDU and HCV status and age. In analyses stratified by age (<45, ≥45 years), the HRs for both IDU and HCV were greater in younger than older patients. In both older and younger patients, and consistent with the overall findings, attenuation of the HR for IDU was more marked than attenuation of the HR for HCV when IDU and HCV were included in the same model.
Table 2.
Unadjusted and adjusted mortality hazard ratios for IDU (v. Non IDU) and HCV infected (v. HCV uninfected) up to three years after starting ART from Cox models stratified by cohort: (i) all patients, (ii) patients aged <45, (iii) patients aged ≥45.
| Unadjusted | Controlling for age, sex, baseline CD4, RNA and AIDS diagnosis |
Additionally controlling for IDU/HCV |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Deaths/patients | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| All patients | 1116/32703 | |||||||||
| IDU | 232/3374 | 2.45 | (2.11, 2.85) | <0.001 | 2.71 | (2.32, 3.16) | <0.001 | 1.57 | (1.27, 1.94) | <0.001 |
| HCV+ | 306/4630 | 2.46 | (2.15, 2.82) | <0.001 | 2.65 | (2.31, 3.04) | <0.001 | 2.04 | (1.68, 2.47) | <0.001 |
|
| ||||||||||
| Age <45 | 462/8145 | |||||||||
| IDU | 46/549 | 3.29 | (2.76, 3.92) | <0.001 | 3.13 | (2.62, 3.74) | <0.001 | 1.62 | (1.24, 2.10) | <0.001 |
| HCV+ | 83/995 | 3.23 | (2.74, 3.81) | <0.001 | 3.18 | (2.69, 3.76) | <0.001 | 2.15 | (1.68, 2.76) | <0.001 |
|
| ||||||||||
| Age≥45 | 654/24558 | |||||||||
| IDU | 186/2825 | 1.67 | (1.22,2.27) | 0.001 | 1.76 | (1.29,2.39) | <0.001 | 1.33 | (0.91, 1.96) | 0.145 |
| HCV+ | 223/3635 | 1.66 | (1.30, 2.11) | <0.001 | 1.91 | (1.50,2.43) | <0.001 | 1.88 | (1.40, 2.54) | <0.001 |
HCV + Hepatitis C infected; IDU assumed route of HIV transmission via injection drug use.
In the sensitivity analyses allowing for misclassification of IDU and HCV, assuming a sensitivity of 0.8 and a specificity of 0.95 for both IDU and HCV increased the mutually adjusted mortality HR for IDU from 1.57 to 2.01 and for HCV from 2.04 to 2.51. The ratio of HRs (HR HCV/ HR IDU), which shows the relative importance of HCV compared with IDU, was 1.30 in the main analysis, decreased to 1.01 if only IDU was misclassified, increased to 1.62 if only HCV was misclassified, and was 1.25 assuming both were equally misclassified (Supplementary table 1).
In a second sensitivity analysis we excluded 2449/32703 (7.5%) patients with “other/unknown” risk group of whom only 239/2449 (10%) were HCV+. Compared with the main analysis, crude and adjusted mortality HR for both IDU and HCV were marginally stronger albeit with wider confidence intervals, but the mutually adjusted HR were very similar (Supplementary table 2).
Table 3 shows numbers of deaths from specific causes, and cause-specific mortality hazard ratios for IDU and HCV. For most causes of death, mortality was higher in IDU compared with non-IDU and in HCV+ compared with HCV−. For both IDU and HCV, the strongest associations were with liver-related mortality (adjusted HR 10.89; 95% CI 6.47,18.3 for IDU and 14.0; 8.05,24.5 for HCV) and with violent death (7.53; 4.19,13.52 for IDU and 5.95; 3.39,10.44 for HCV). The HR for deaths due to substance abuse was 14.03 (5.41, 36.39) in HCV+ compared with HCV−. For liver-related mortality, the effect of IDU was substantially attenuated (HR 2.43) after adjustment for HCV, while attenuation of the effect of HCV was less substantial (HR 7.97) after adjustment for IDU. By contrast, for CNS and respiratory mortality attenuation in the effect of IDU was less marked than attenuation in the effect of HCV. Rates of violent death also remained elevated in IDU after adjustment for HCV. Supplementary table 3 provides additional information on mortality rates for specific causes of death. Rates of all causes of death, except myocardial infarction and ischaemic heart disease, were higher for HCV + than for HCV uninfected individuals.
Table 3.
Adjusted hazard ratio for specific causes of death for IDU compared with non-IDU and HCV-infected compared with HCV-uninfected
| HR§ (95% CI) IDU v. Non IDU |
HR§ (95% CI) HCV-infected v. HCV-uninfected |
||||
|---|---|---|---|---|---|
| Cause of death | Number (%) of deaths |
additionally adjusted for HCV |
additionally adjusted for IDU |
||
| All | 1116 (100) | 2.71 (2.32,3.16) | 1.57 (1.27,1.94) | 2.65 (2.31,3.04) | 2.04 (1.68,2.47) |
| AIDS | 459 (41.1) | 1.40 (1.05,1.88) | 1.01 (0.69,1.48) | 1.55 (1.21,1.99) | 1.54 (1.11,2.14) |
| Non-AIDS infection | 84 (7.5) | 3.18 (1.89,5.34) | 1.86 (0.88,3.93) | 2.92 (1.82,4.71) | 1.99 (1.00,3.99) |
| Liver-related | 69 (6.2) | 10.89 (6.47,18.3) | 2.43 (1.24,4.78) | 14.0 (8.05,24.5) | 7.97 (3.83,16.6) |
| Non-AIDS malignancy | 103 (9.2) | 1.50 (0.78,2.88) | 0.72 (0.33,1.58) | 2.22 (1.38,3.58) | 2.58 (1.45,4.60) |
| MI/IHD | 22 (2.0) | 0 | 0 | 0.48 (0.06,3.65) | 0.91 (0.12,6.85) |
| Stroke | 10 (0.9) | 1.74 (0.19,15.77) | 0.71 (0.06,8.57) | 2.82 (0.69,11.53) | 3.15 (0.65,15.38) |
| Renal failure | 12 (1.1) | 2.71 (0.56,13.12) | 1.59 (0.19,13.40) | 2.52 (0.66,9.64) | 1.97 (0.32,12.17) |
| Violence* | 52 (4.7) | 7.53 (4.19,13.52) | 3.65 (1.48,9.02) | 5.95 (3.39,10.44) | 2.52 (1.04,6.09) |
| CNS (other than stroke) | 16 (1.4) | 6.02 (2.01,18.08) | 5.35 (1.00,28.60) | 3.45 (1.20,9.90) | 1.16 (0.23,5.93) |
| Other heart/vascular | |||||
| disease | 34 (3.1) | 3.08 (1.33,7.13) | 1.38 (0.45,4.23) | 3.31 (1.60,6.84) | 2.78 (1.05,7.38) |
| Respiratory disease* | 16 (1.4) | 5.55 (1.86,16.55) | 4.64 (0.84,25.69) | 3.56 (1.24,10.18) | 1.26 (0.23,6.73) |
| Other | 48 (4.3) | 2.38 (1.11,5.09) | 1.27 (0.45,3.59) | 2.54 (1.32,4.89) | 2.21 (0.90,5.43) |
| Unknown* | 191 (17.1) | 3.91 (2.76,5.54) | 2.45 (1.50,4.00) | 3.19 (2.30,4.41) | 1.90 (1.20,3.01) |
Adjusted for age, sex, CD4 cell count, HIV-1 RNA and AIDS at baseline, stratified by cohort
Violence includes suicide, substance abuse; Respiratory includes chronic obstructive pulmonary disease (COPD); unknown includes unclassifiable.
MI Myocardial Infarction; IHD Ischaemic Heart Disease; CNS Central Nervous System
HCV+ Hepatitis C infected; IDU assumed route of HIV transmission via injection drug use.
Discussion
Main results
Based on a large dataset combined from 16 HIV cohort studies that recruited patients in Europe and North America, we examined the extent to which presumed HIV transmission via injection drug use, and HCV infection, independently predicted all-cause and cause-specific mortality. The association of transmission via IDU with all-cause mortality was attenuated after adjustment for HCV co-infection, but mortality remained more than 50% higher in IDU than in non-IDU. Effects of both IDU and HCV were greater in patients under 45 years of age (considered more likely to be active IDU (18)) than in older individuals, but patterns of attenuation were similar. Sensitivity analyses confirmed that error in measuring both IDU and HCV status affects the extent of attenuation if there is greater measurement error in one than the other risk factor. Analyses of cause-specific mortality confirmed that HCV is a stronger predictor than IDU for liver-related mortality, but identified particular causes of death for which associations with IDU are not explained by HCV.
Strengths and limitations
We analysed a large dataset with over 30,000 patients and over 1,000 deaths, of which 85% had causes classified using standardised procedures. Our analysis may suffer from ascertainment bias as individuals with HCV serostatus available were more likely to have an injecting drug use history which may have prompted testing for HCV compared with those excluded from the study. We did not know if IDU were chronic or past injection drug users, as IDU status was based on self-reported likely transmission route of infection. It is likely that some patients reporting no history of IDU were either past or current IDU, and this possibility is consistent with our finding of a substantial prevalence of HCV among those recorded as non-IDU: this underscores the importance of testing and treating HCV among all individuals who are HIV-infected, particularly as incidence of HCV infection has been reported to be increasing in men who have sex with men in some regions(19). Further work is needed to investigate modes of HCV acquisition among HIV-positive individuals in order to prevent re-infection after HCV treatment. We did not have information on HBV co-infection, which might differ between IDU and HCV+ and affect prognosis. Our information on HCV infection was limited as we did not have data on active Hepatitis C viremia (20, 21). Previous research has shown that the presence of viremia increases mortality, particularly that due to liver-related deaths. We did not have details of treatments for HCV infection. However, during the calendar period included in our analyses, HCV treatment rates among those with HIV infection were low (22, 23). We did not analyse longitudinal HCV-RNA tests to see if patients had spontaneously cleared the virus or were successfully treated. However, the proportion that spontaneously clears HCV infection is substantially lower among HIV-infected than HIV-uninfected individuals (24-26). Furthermore, HIV-infected individuals with spontaneous control of HCV remain at significant risk for a second episode of viremia (27). The results of the sensitivity analysis that attempted to quantify the possible effects of misclassification bias showed that our conclusions about the relative importance of HCV compared with IDU for predicting mortality were robust if both IDU and HCV were equally misclassified, although hazard ratios for both risk factors may have been under-estimated. However, if only IDU were misclassified then IDU and HCV might have similar mutually adjusted mortality hazard ratios, which would imply that both factors are equally important predictors of mortality. Our results were also robust to the exclusion of the small proportion of patients with “other/unknown” transmission group, some of whom may have been IDU misclassified as non-IDU in the main analysis.
Results in context with other studies
In our study, HIV-infected individuals with HCV co-infection experienced 2.5 fold greater mortality rates than those without HCV co-infection. Most of this excess mortality was not explained by other risks associated with IDU. Other studies have found that HCV causes substantial morbidity from liver (28) and renal injury (29) as well as increases the risk of coronary disease (30) and diabetes (31). Our study confirmed higher rates of mortality in HCV+ for liver-related deaths and also for AIDS and non-AIDS, non-liver related causes of deaths. Although HCV status is likely associated with lifestyle factors, such as tobacco use, which are associated with higher mortality rates, HCV infection may directly contribute to non-liver related deaths via impaired immune responses to treatment for HIV infection (32). HRs for IDU were greater in younger patients, suggesting that active injection drug use, which is more likely at younger ages (18), has additional harms compared with historic use. An alternative explanation is that differences in HR by age may be partly due to diversification of causes of death in IDU at older ages, with increased risk of deaths due to cardiovascular disease and cancer. However among older patients, for whom active injection drug use is less likely, HCV co-infection remained strongly associated with mortality. There may nonetheless be lifestyle factors that differ between those with and without HCV infection, and are not captured by IDU status, for example risky sexual behaviour, commercial sex work, or intranasal drug use, which may contribute to the higher mortality in those with HCV infection.
Implications
While there is a growing consensus on the importance of treating HCV co-infection among those living with HIV, many barriers remain. These include higher rates of contraindications and concerns regarding decreased antiretroviral adherence and drug-drug interactions from polypharmacy (33). Our analyses underscore the importance of overcoming these barriers if we are to achieve better survival among those aging with HIV, many of whom no longer use injection drugs but are continuing to suffer consequences of past use. New oral direct acting antiviral protease inhibitor-based therapies have been shown to result in cure rates exceeding 65% and have shortened the period during which the poorly tolerated drug interferon has to be used (34). Furthermore, interferon-free direct acting antiviral HCV treatment for HIV-infected individuals with markedly reduced toxicity, high efficacy (>90% cure), improved dosing schedules (once or twice-daily) and shortened treatment duration (6-24 weeks) (15), are quickly becoming more widely available. This revolution in treatment of HCV could enable increased treatment uptake, not just amongst IDU, but also in the emerging MSM epidemic, which could have a major preventative impact (35). However, treatment costs may limit scale-up as new drugs are expensive.
Conclusions
HCV infection explained much of the association of IDU with mortality in a cross cohort analysis of HIV-infected individuals initiating ART especially among those 45 years of age and older who were considered less likely to be active IDU. This underscores the potential of HCV treatment to impact mortality in this co-infected population, in addition to interventions to stop substance abuse and address other lifestyle factors. Treatment for HCV infection is now feasible in HIV-infected people with the advent of new therapies, which are shorter, less toxic, and have higher cure rates. Future work will investigate the extent to which treating HCV infection reduces mortality in this population and the causes of death that are impacted.
Supplementary Material
Acknowledgments
We thank all patients, doctors, and study nurses associated with the participating cohort studies. Data from European cohorts were pooled in July 2012 within COHERE in EuroCoord (www.cohere.org and www.EuroCoord.net). COHERE receives funding from the European Union Seventh Framework Programme (FP7/2007-2013) under EuroCoord grant agreement n° 260694. Sources of funding of individual cohorts include the Agence Nationale de Recherche sur le SIDA et les hépatites virales (ANRS), the Institut National de la Santé et de la Recherche Médicale (INSERM), the French, Italian and Spanish Ministries of Health, the Swiss National Science Foundation (grant 33CS30_134277), the Ministry of Science and Innovation and the “Spanish Network for AIDS Research (RIS; ISCIII-RETIC RD06/006), the Stichting HIV Monitoring, the European Commission (EuroCoord grant 260694), the British Columbia and Alberta Governments, the National Institutes of Health (NIH) [UW Center for AIDS Research (CFAR) (NIH grant P30 AI027757), UAB CFAR (NIH grant P30-AI027767), The Vanderbilt-Meharry CFAR (NIH grant P30 AI54999), National Institute on Alcohol Abuse and Alcoholism (U10-AA13566, U24-AA020794), the US Department of Veterans Affairs, the Michael Smith Foundation for Health Research, the Canadian Institutes of Health Research, the VHA Office of Research and Development and unrestricted grants from Abbott, Gilead, Tibotec-Upjohn, ViiV Healthcare, MSD, GlaxoSmithKline, Pfizer, Bristol Myers Squibb, Roche and Boehringer-Ingelheim.
Source of Funding: Colette Smith has received honoraria for preparing educational materials, attending Ad boards or conference sponsorship from: Janssen, ViiV, Gilead and BMS. John Gill has been a member of the National HIV Advisory Boards to Abbvie, Gilead, Janssen Merck and ViiVHealthcare.
This work was supported by the UK Medical Research Council [grant numbers G0700820, MR/J002380/1] and the Department for International Development (DFID). Jonathan Sterne is funded by National Institute for Health Research Senior Investigator award NF-SI-0611-10168.
Footnotes
Conflicts of Interest: For the remaining authors none were declared.
Contributor Information
Margaret T May, School of Social and Community Medicine, University of Bristol, Bristol, UK.
Amy C Justice, Yale University, New Haven, Connecticut, and VA Connecticut Healthcare System, West Haven, Connecticut.
Kate Birnie, School of Social and Community Medicine, University of Bristol, Bristol, UK.
Suzanne M Ingle, School of Social and Community Medicine, University of Bristol, Bristol, UK.
Colette Smit, Stichting HIV Monitoring, Amsterdam, The Netherlands.
Colette Smith, Research Department of Infection and Population Health, University College London, London, UK.
Didier Neau, Fédération des Maladies Infectieuses, Centre Hospitalo-Universitaire Pellegrin, Bordeaux, France.
Marguerite Guiguet, INSERM U943 and UPMC UMR-S-943, Paris, F75013 France.
Carolynne Schwarze-Zander, Department of Internal Medicine, University Hospital Bonn, Germany.
Santiago Moreno, Ramón y Cajal Hospital, IRYCIS, Madrid, Spain.
Jodie L. Guest, HIV Atlanta VA Cohort Study (HAVACS), Atlanta Veterans Affairs Medical Center, Decatur, GA, USA.
Antonella d’Arminio Monforte, Clinic of Infectious Diseases & Tropical Medicine, San Paolo Hospital, University of Milan, Italy.
Cristina Tural, Hospital Universitari Germans Trias i Pujol, Universitat Autònoma de Barcelona, Badalona, Spain.
Michael J Gill, Division of Infectious Diseases, University of Calgary, Calgary, Canada.
Andrea Bregenzer, Department of Infectious Diseases, Cantonal Hospital St. Gallen, 9007 St. Gallen, Switzerland.
Ole Kirk, CHIP, Department of Infectious Diseases, Rigshospitalet, University of Copenhagen, Copenhagen, Denmark.
Michael Saag, Division of Infectious Disease, Department of Medicine, University of Alabama, Birmingham, USA.
Timothy R Sterling, Vanderbilt University School of Medicine, Nashville, TN, USA.
Heidi M Crane, University of Washington School of Medicine, Seattle, WA, USA.
Jonathan A C Sterne, School of Social and Community Medicine, University of Bristol, Bristol, UK.
References
- 1.Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360(9327):119–29. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 2.Larsen MV, Omland LH, Gerstoft J, et al. Impact of injecting drug use on mortality in Danish HIV-infected patients: a nation-wide population-based cohort study. Addiction. 2010;105(3):529–35. doi: 10.1111/j.1360-0443.2009.02827.x. [DOI] [PubMed] [Google Scholar]
- 3.Mathers BM, Degenhardt L, Bucello C, et al. Mortality among people who inject drugs: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2013;91(2):102–23. doi: 10.2471/BLT.12.108282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gill MJ, May MT, Lewden C, et al. Causes of death in HIV-1 infected patients treated with antiretroviral therapy 1996-2006: collaborative analysis of 13 HIV cohorts. Clin Infect.Dis. 2010;50(10):1387–96. doi: 10.1086/652283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Green TC, McGowan SK, Yokell MA, et al. HIV infection and risk of overdose: a systematic review and meta-analysis. AIDS. 2012;26(4):403–17. doi: 10.1097/QAD.0b013e32834f19b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferreros I, Lumbreras B, Hurtado I, et al. The shifting pattern of cause-specific mortality in a cohort of human immunodeficiency virus-infected and non-infected injecting drug users. Addiction. 2008;103(4):651–9. doi: 10.1111/j.1360-0443.2008.02135.x. [DOI] [PubMed] [Google Scholar]
- 7.Spire B, Lucas GM, Carrieri MP. Adherence to HIV treatment among IDUs and the role of opioid substitution treatment (OST) International Journal of Drug Policy. 2007;18(4):262–70. doi: 10.1016/j.drugpo.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Kohli R, Lo Y, Howard AA, et al. Mortality in an urban cohort of HIV-infected and at-risk drug users in the era of highly active antiretroviral therapy. Clin Infect Dis. 2005;41(6):864–72. doi: 10.1086/432883. [DOI] [PubMed] [Google Scholar]
- 9.Schiavini M, Angeli E, Mainini A, et al. Risk factors for fibrosis progression in HIV/HCV coinfected patients from a retrospective analysis of liver biopsies in 1985-2002. HIV Medicine. 2006;7(5):331–7. doi: 10.1111/j.1468-1293.2006.00384.x. [DOI] [PubMed] [Google Scholar]
- 10.Izzedine H, Sene D, Cacoub P, et al. Kidney diseases in HIV/HCV-co-infected patients. AIDS. 2009;23(10):1219–26. doi: 10.1097/QAD.0b013e32832ac36a. [DOI] [PubMed] [Google Scholar]
- 11.Altice FL, Kamarulzaman A, Soriano VV, et al. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–87. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vickerman P, Hickman M, May M, et al. Can hepatitis C virus prevalence be used as a measure of injection-related human immunodeficiency virus risk in populations of injecting drug users? An ecological analysis. Addiction. 2010;105(2):311–8. doi: 10.1111/j.1360-0443.2009.02759.x. [DOI] [PubMed] [Google Scholar]
- 13.Nelson PK, Mathers BM, Cowie B, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378(9791):571–83. doi: 10.1016/S0140-6736(11)61097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soriano V, Labarga P, Fernandez-Montero JV, et al. The changing face of hepatitis C in the new era of direct-acting antivirals. Antiviral Res. 2013;97(1):36–40. doi: 10.1016/j.antiviral.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Poordad F, Lawitz E, Kowdley KV, et al. Exploratory Study of Oral Combination Antiviral Therapy for Hepatitis C. New England Journal of Medicine. 2013;368(1):45–53. doi: 10.1056/NEJMoa1208809. [DOI] [PubMed] [Google Scholar]
- 16.Murray M, Hogg RS, Lima VD, et al. The effect of injecting drug use history on disease progression and death among HIV-positive individuals initiating combination antiretroviral therapy: collaborative cohort analysis. HIV.Med. 2012;13(2):89–97. doi: 10.1111/j.1468-1293.2011.00940.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.May MT, Ingle SM, Costagliola D, Justice AC, de Wolf F, Cavassini M. Cohort profile: Antiretroviral Therapy Cohort Collaboration (ART-CC) IJE. 2014;43(3):691–702. doi: 10.1093/ije/dyt010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green TC, Kershaw T, Lin HQ, et al. Patterns of drug use and abuse among aging adults with and without HIV: A latent class analysis of a US Veteran cohort. Drug Alcohol Depend. 2010;110(3):208–20. doi: 10.1016/j.drugalcdep.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wandeler G, Gsponer T, Bregenzer A, et al. Hepatitis C virus infections in the Swiss HIV Cohort Study: a rapidly evolving epidemic. Clin Infect Dis. 2012;55(10):1408–16. doi: 10.1093/cid/cis694. [DOI] [PubMed] [Google Scholar]
- 20.Lee MH, Yang HI, Lu SN, et al. Chronic hepatitis C virus infection increases mortality from hepatic and extrahepatic diseases: a community-based long-term prospective study. J Infect Dis. 2012;206(4):469–77. doi: 10.1093/infdis/jis385. [DOI] [PubMed] [Google Scholar]
- 21.Uto H, Stuver SO, Hayashi K, et al. Increased rate of death related to presence of viremia among hepatitis C virus antibody-positive subjects in a community-based cohort study. Hepatology. 2009;50(2):393–9. doi: 10.1002/hep.23002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Butt AA, Justice AC, Skanderson M, et al. Rate and predictors of treatment prescription for hepatitis C. Gut. 2007;56(3):385–9. doi: 10.1136/gut.2006.099150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Butt AA, McGinnis KA, Skanderson M, Justice AC. Hepatitis C treatment completion rates in routine clinical care. Liver Int. 2010;30(2):240–50. doi: 10.1111/j.1478-3231.2009.02156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piasecki BA, Lewis JD, Reddy KR, et al. Influence of alcohol use, race, and viral coinfections on spontaneous HCV clearance in a US veteran population. Hepatology. 2004;40(4):892–9. doi: 10.1002/hep.20384. [DOI] [PubMed] [Google Scholar]
- 25.Grebely J, Raffa JD, Lai C, et al. Factors associated with spontaneous clearance of hepatitis C virus among illicit drug users. Canadian Journal of Gastroenterology. 2007;21(7):447–51. doi: 10.1155/2007/796325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schnuriger A, Dominguez S, Guiguet M, et al. Acute hepatitis C in HIV-infected patients: rare spontaneous clearance correlates with weak memory CD4 T-cell responses to hepatitis C virus. AIDS. 2009;23(16):2079–89. doi: 10.1097/QAD.0b013e328330ed24. [DOI] [PubMed] [Google Scholar]
- 27.Kim AY, Schulze zur Wiesch J, Kuntzen T, et al. Impaired hepatitis C virus-specific T cell responses and recurrent hepatitis C virus in HIV coinfection. PLoS Med. 2006;3(12):e492. doi: 10.1371/journal.pmed.0030492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernando V, Perez-Cachafeiro S, Lewden C, et al. All-cause and liver-related mortality in HIV positive subjects compared to the general population: differences by HCV co-infection. J Hepatol. 2012;57(4):743–51. doi: 10.1016/j.jhep.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Fischer MJ, Wyatt CM, Gordon K, et al. Hepatitis C and the risk of kidney disease and mortality in veterans with HIV. J Acquir Immune Defic Syndr. 2010;53(2):222–6. doi: 10.1097/QAI.0b013e3181b980d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Butt AA, Xiaoqiang W, Budoff M, et al. Hepatitis C virus infection and the risk of coronary disease. Clin Infect Dis. 2009;49(2):225–32. doi: 10.1086/599371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Butt AA, Fultz SL, Kwoh CK, et al. Risk of diabetes in HIV infected veterans pre- and post-HAART and the role of HCV coinfection. Hepatology. 2004;40(1):115–9. doi: 10.1002/hep.20289. [DOI] [PubMed] [Google Scholar]
- 32.Greub G, Ledergerber B, Battegay M, et al. Clinical progression, survival, and immune recovery during antiretroviral therapy in patients with HIV-1 and hepatitis C virus coinfection: the Swiss HIV Cohort Study. Lancet. 2000;356(9244):1800–5. doi: 10.1016/s0140-6736(00)03232-3. [DOI] [PubMed] [Google Scholar]
- 33.Edelman E, Gordon K, Glover K, et al. The Next Therapeutic Challenge in HIV: Polypharmacy. Drugs and aging. 2013;30(8):16. doi: 10.1007/s40266-013-0093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dore GJ. The changing therapeutic landscape for hepatitis C. Medical Journal of Australia. 2012;196(10):629–32. doi: 10.5694/mja11.11531. [DOI] [PubMed] [Google Scholar]
- 35.Martin N, Vickerman P, Grebely J, et al. HCV treatment for prevention among people who inject drugs: modeling treatment scale-up in the age of direct-acting antivirals. Hepatology. 2013;58(5):1598–609. doi: 10.1002/hep.26431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.