Abstract
BACKGROUND
Community-based self-screening may provide opportunities to increase detection of hypertension, and identify raised blood pressure (BP) in populations who do not access healthcare. This systematic review aimed to evaluate the effectiveness of non-physician screening and self-screening of BP in community settings.
METHODS
We searched the Cochrane Central Trials Register, Medline, Embase, CINAHL, and Science Citation Index & Conference Proceedings Citation Index—Science to November 2013 to identify studies reporting community-based self-screening or non-physician screening for hypertension in adults. Results were stratified by study site, screener, and the cut-off used to define high screening BP.
RESULTS
We included 73 studies, which described screening in 9 settings, with pharmacies (22%) and public areas/retail (15%) most commonly described. We found high levels of heterogeneity in all analyses, despite stratification. The highest proportions of eligible participants screened were achieved by mobile units (range 21%–88%) and pharmacies (range 40%–90%). Self-screeners had similar median rates of high BP detection (25%–35%) to participants in studies using other screeners. Few (16%) studies reported referral to primary care after screening. However, where participants were referred, a median of 44% (range 17%–100%) received a new hypertension diagnosis or antihypertensive medication.
CONCLUSIONS
Community-based non-physician or self-screening for raised BP can detect raised BP, which may lead to the identification of new cases of hypertension. However, current evidence is insufficient to recommend specific approaches or settings. Studies with good follow-up of patients to definitive diagnosis are needed.
Keywords: blood pressure, community health services, hypertension, primary care, screening, self-evaluation, self-screening.
Hypertension is one of the leading preventable risk factors in the global burden of disease,1,2 and its treatment reduces the risk of both stroke and coronary heart disease: a 10mm Hg reduction in blood pressure (BP) is associated with a 41% and a 22% reduction in stroke and coronary heart disease, respectively.3 However, regular health surveys in a number of countries suggest that underdiagnosis and undertreatment of hypertension are common.4–6
At present, hypertension is mainly detected through either opportunistic or routine systematic screening in primary care. However, both methods require attendance at primary care settings, which excludes individuals who do not routinely attend primary care, or those in whom routine screening is not practiced.
Community-based screening by non-physicians may provide an opportunity to increase routine detection of hypertension in the community, outside of established healthcare organizations, and to target high-risk populations as well as those who do not attend primary care. Self-screening, where individuals measure their own BP, is now routinely available in a number of pharmacies, with some studies reporting large numbers of individuals using these facilities.7,8
The aim of this study was therefore to systematically review the evidence for self-screening and other community-based non-physician screening strategies, and the associated rates of target populations screened, detection of raised BP, and rates of follow-up and intervention, including new diagnoses, in primary care. A further aim was to establish the factors, such as appropriate settings, screeners, and targeted populations that underpin a successful screening program for hypertension. We considered that a successful screening program would obtain good coverage of the targeted population, and refer all new cases of screen-detected high BP for definitive diagnosis without excessive numbers of false-positive referrals.
METHODS
Search strategy
We searched the Cochrane Central Register of Controlled Trials (Issue 4 2011), Medline (from 1948), Embase (from 1974), CINAHL (from 1980), and Science Citation Index & Conference Proceedings Citation Index—Science (from 1945) from the start of each database until 25th November 2013 using a search strategy developed with the assistance of an information specialist. The search strategy included terms relating to BP measurement, community sites and screeners, and self-screening (Supplementary Appendix A). We subsequently added an exclusion criterion for studies conducted prior to 1980, as initial screening confirmed that suitable devices for self-screening were not generally available before this date. Additional studies were identified by searching reference lists of included studies.
Inclusion and exclusion criteria
We included studies reporting self-screening or community-based screening by non-physicians of BP in adults ≥18 years of age (Table 1). “Self-screening” included home measurement of BP for screening purposes, but not for diagnostic or monitoring purposes. Screening carried out by clinically trained screeners (e.g., nurses) in clinical settings were excluded, although we included studies in community dentistry, as routine BP measurement is not usually practiced in community dentistry, and so this represents a novel setting for BP screening. No limit by comparator or study design was applied. Studies where BP measurements were obtained during screening with the primary aim of detecting a condition other than hypertension, as well as those where multiple screening tests were performed in a single visit were included.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria: |
| • Self-screening or screening in community settings, including mass screenings, community dentistry, and pharmacy-based screening |
| • Majority of participants aged over 18 years |
| • Blood pressure screening performed by non-physicians, including nurses, medical students, dentists, pharmacists, and lay people |
| • Reporting, as a minimum, either numbers screened for hypertension, or numbers found to be hypertensive following screening |
| Exclusion criteria: |
| • Home blood pressure measurement for diagnostic or monitoring purposes |
| • Blood pressure screening performed by qualified physicians (studies were not excluded if physicians gave postscreening advice but did not participate in blood pressure measurement) |
| • Screening by clinically trained personnel (including nurses) in clinical settings—community dentistry was not included in this definition of a clinical setting |
| • Screening of employees in workplace or military settings |
| • Studies where all participants had an existing hypertension diagnosis |
| • Studies of established research cohorts (including those using hypertension screening as a recruitment tool) |
| • Studies of groups identified by stratified or other sampling methods intended for use in epidemiological studies |
| • Studies carried out in low-income or lower-middle income countries, as defined by the World Bank |
| • Studies published before 1980 |
| • Studies published in a language other than English |
Study selection
Two authors (S.F. and H.A.) screened all titles and abstracts, and retrieved full text articles for potentially eligible studies. Where necessary, authors of studies were contacted up to 2 times by electronic mail for clarification of inclusion status. If study eligibility could not be confirmed after 2 attempts to contact the authors, the study was excluded.
Data extraction
Data from each paper were extracted by one author (S.F., H.A., D.M., R.J.M., C.H., or A.W.), and the data extraction form checked by a second author in the group, with disagreements resolved by consensus or a third author (S.F. or H.A.). Extracted data included study characteristics, the number screened, and where reported, the proportion eligible for screening, the proportion with screen-detected hypertension, the hypertension threshold used, the proportion with existing hypertension, and any follow-up carried out.
Assessment of quality
Quality assessment was conducted using criteria based on the Quality Assessment tool for Diagnostic Accuracy Studies-2 (QUADAS-2) at the same time as extraction, and by the same authors, with disagreements resolved by consensus or a third author (S.F. or H.A.).9 The criteria assessed applicability and bias due to patient selection, appropriateness of patients and setting, method of BP measurement, the prespecification and appropriateness hypertension threshold, and blinding to preexisting hypertension status (Supplementary Appendix B).
Data synthesis
Characteristics of included studies were summarized, including the populations screened, setting, and aspects of study design (Supplementary Appendix C).
Data on the proportion of participants screened, and the proportion with high screening BP were reported grouped by the hypertension threshold defined in the study, size of study (number screened), qualification of person conducting the screening, and type of setting.
High levels of data heterogeneity meant that statistical synthesis was not possible. However, where at least 3 similar studies were included, their results were summarized using a box and whiskers plot, and possible factors relating to outliers discussed. We defined outliers as values further than 1.5 interquartile ranges from the nearest quartile.10 Statistical analyses were carried out using R (version 3.0.1, R Foundation for Statistical Computing).
RESULTS
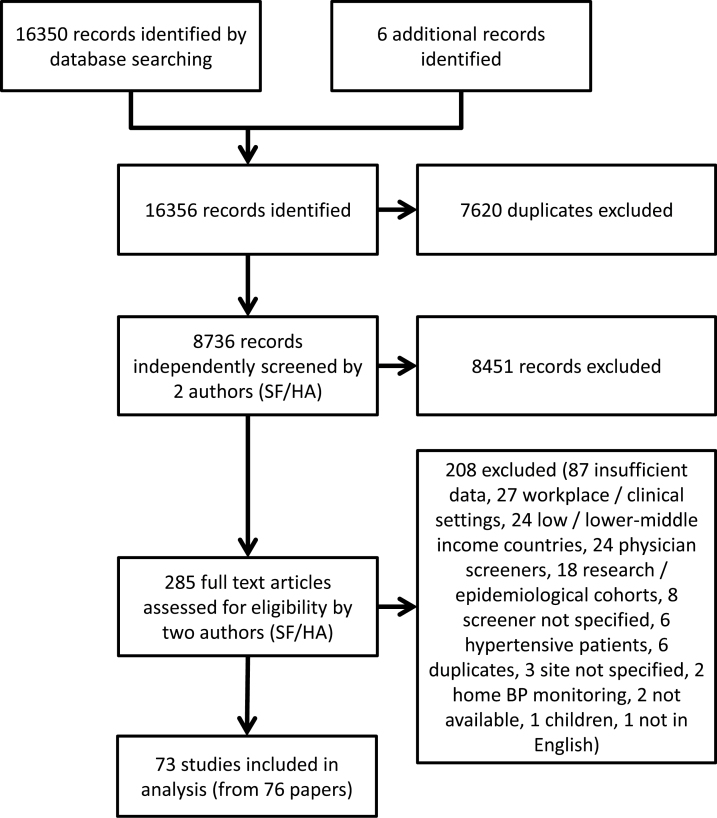
We identified 16,356 studies (Figure 1). After initial screening of titles and abstracts, we examined 285 full text papers, of which 73 met our inclusion criteria.
Figure 1.
Flow chart.
Characteristics of included studies
An overview of the variation in study design and location is given in Table 2. Where reported (18 out of 73 studies, 25%), age of participants varied from a mean age of 41–75 years. Several studies targeted specific populations; for example, 14 studies screened ethnic minority populations, and 2 screened men.
Table 2.
Overview of study designs
| Characteristics | Subgroups | Number (%) |
|---|---|---|
| Location of study | North America | 49 (67.1) |
| Europe | 19 (26.0) | |
| Australasia | 4 (5.5) | |
| Asia | 1 (1.4) | |
| Setting | Pharmacies | 16 (21.9) |
| Public area/retail | 11 (15.1) | |
| Community building (e.g., fire stations, places of worship) | 10 (13.7) | |
| Mobile unit | 10 (13.7) | |
| Home | 8 (11) | |
| Dental | 7 (9.6) | |
| Mixed (multiple settings used within one study) | 7 (9.6) | |
| Health fair | 3 (4.1) | |
| Health center (screening by lay person or self-screening) | 1 (1.4) | |
| Screeners | Nurses | 17 (23.3) |
| Lay screeners | 15 (20.5) | |
| Pharmacy | 11 (15.1) | |
| Other healthcare professional (e.g., paramedics, phlebotomists) | 10 (13.7) | |
| Dental | 8 (11.0) | |
| Mixed (e.g., nurses and lay screeners) | 5 (6.8) | |
| Students | 4 (5.5) | |
| Self-screening | 3 (4.1) | |
| Method of recruitment | Opportunistic in healthcare (e.g., at dental appointments) | 12 (16.4) |
| Media and advertising | 12 (16.4) | |
| Letter or personal invitation | 10 (13.7) | |
| Opportunistic outside healthcare | 9 (12.3) | |
| Passing trade | 7 (9.6) | |
| Poster and flyers | 5 (6.8) | |
| Door-to-door | 4 (5.5) | |
| Not specified | 14 (19.2) | |
| Communication of results | Verbally to participant | 16 (21.9) |
| Written to participant | 14 (19.2) | |
| Referral | 10 (13.7) | |
| Written to participant and primary care provider | 7 (9.6) | |
| Not specified | 26 (35.6) |
Screening was conducted in 9 different types of setting (Table 2). The majority of studies reporting data on the number of screening sites used (n = 29 out of 49 studies reporting these data, 59%) described between 1 and 5 screening sites.
The most frequently reported types of people performing the screening were nurses (n = 17, 23%), followed by lay screeners (n = 16, 22%), and only 3 studies used self-screening (Table 2). Only 39 (53%) studies reported the type of BP measurement device used, which included automated devices in 25 (34%) studies, and a manual sphygmanometer in 14 studies (19%). The number of measurements taken on each occasion was reported by 27 studies and ranged from 1 to 12. If more than one BP was taken there was significant variation in the timing of subsequent measurements.
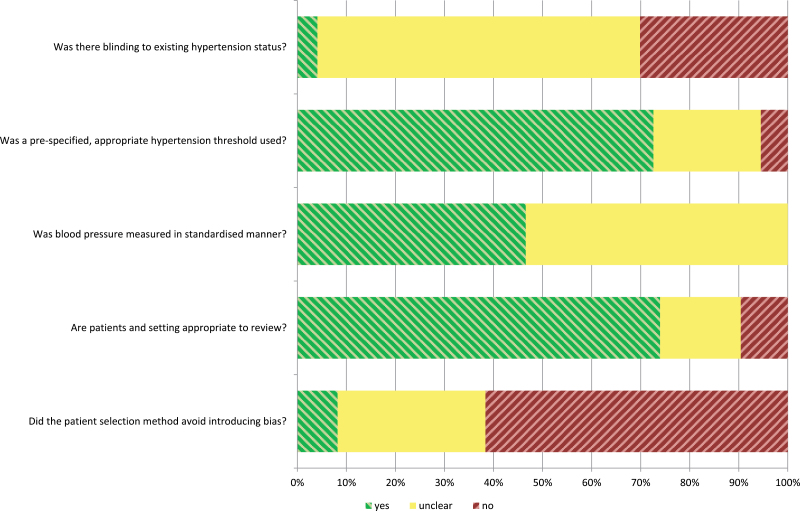
Quality assessment
The results of the quality assessment (Figure 2) showed that few studies reported blinding to existing hypertension status (Supplementary Appendix D). Many studies (62%) were assessed as vulnerable to bias due to their recruitment methods, such as convenience sampling. The method for measuring BP was also poorly reported in the majority of studies, although most studies prespecified an appropriate threshold for hypertension.
Figure 2.
Visualization of quality assessment.
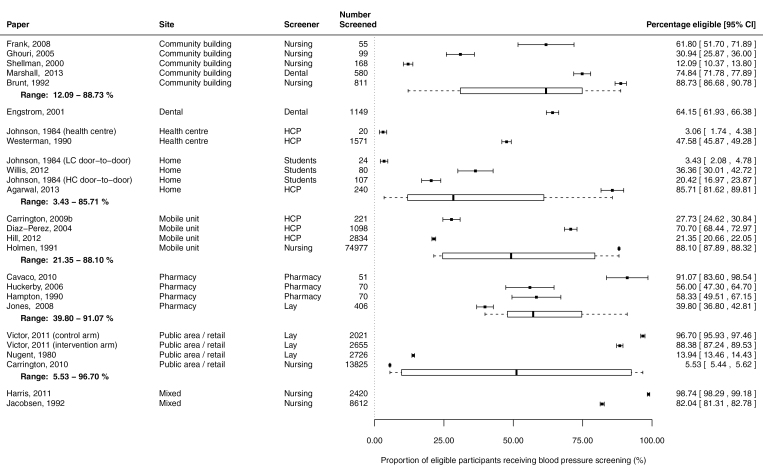
Proportion of eligible participants screened
Twenty-three studies reported data for both the eligible population and the number screened, allowing the coverage of the screening strategies to be calculated. There was considerable heterogeneity both between and within sites (Figure 3): for example, 5 studies conducted in community buildings found that 12%–89% of eligible people were screened. A similar range was noted for screeners: for example, where nurses performed the screening, the proportion screened ranged from 5.5% to 99%. Mobile units (range 21%–88%) and pharmacies (range 40%–91%) achieved relatively high coverage across a range of studies. Some of the observed heterogeneity in coverage can be explained by differences in how eligible participants were defined in different studies. For example, 3 studies conducted in public areas and retail sites found that 5.5%–97% of eligible people were screened, the main differences being whether the population at large or the population attending a particular setting was defined as the denominator.11–13 Results also varied widely both within and between each type of screener. Student screeners achieved a low range of coverage (3.4%–36%), whereas pharmacy staff obtained higher coverage of the eligible population (56%–91%).
Figure 3.
Proportion of eligible participants receiving screening, ordered by site.
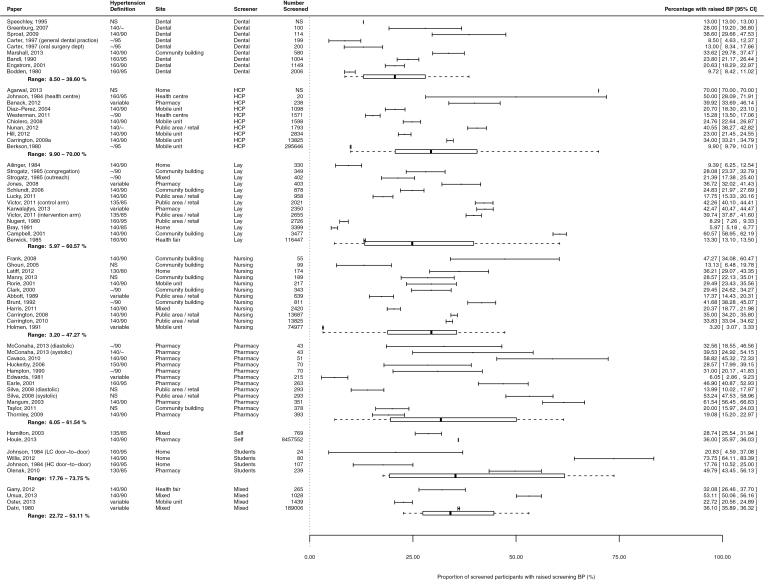
Detection of hypertension in screened participants
Fifty-nine studies contained sufficient data to calculate the proportion of screened participants who had hypertension. Although the definition of hypertension varied considerably between studies, there did not appear to be any relationship between hypertension threshold and detection rate (Supplementary Appendix F).
Most studies, whether grouped by site or screener, showed considerable heterogeneity in detection rate. Two types of site appeared to have lower detection rates: dental sites (range 8.5%–39%) and mobile sites (range 3.2%–34%) (Supplementary Appendix G). A number of the mobile sites served communities with reduced access to healthcare (e.g., immigrant communities in the United States).
It was notable that the 2 self-screening studies (i.e., those where participants measured their own BP)14,15 both resulted in detection rates (29% and 36%) comparable to the median detection rates seen in studies using a variety of other screeners (Figure 4).
Figure 4.
Proportion of screened participants with raised screening blood pressure, ordered by screener.
One outlier study16 was found during the analysis, with considerably lower detection rates than the other studies carried out in pharmacies. This paper was relatively old and used considerably higher hypertension cut-offs than more contemporary work (variable with minimum cut-off of 160/100mm Hg), which would be expected to result in lower detection rates given a similar population.
Detection of hypertension in participants with and without preexisting diagnoses
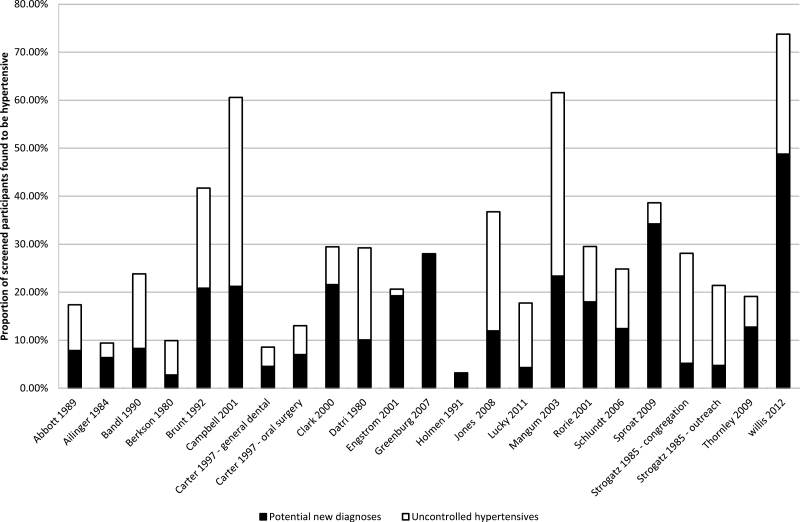
Twenty-four studies provided data on detection of raised BP in participants with and without preexisting hypertension diagnoses. Figure 5 shows that in many of these studies, the proportion of participants with uncontrolled hypertension (i.e., those with an existing hypertension diagnosis and a raised BP on screening) equaled or exceeded the proportion of potential new diagnoses (i.e., participants with raised BP on screening, but without any known diagnosis of hypertension). Most of these studies recruited from populations which were likely to be representative of the general population in the study area, rather than selected subgroups.
Figure 5.
Proportion of screened participants with and without preexisting hypertension diagnoses found to have high screening blood pressure.
Follow-up of participants after screening
Twelve studies provided data on participants following screening (Supplementary Appendix E). Only 3/7 (43%) referred all participants with elevated screening BP to primary care, and in one case, as few as 26% of those screening positive were referred. Eight studies reported the outcome of the referral, with a median of 44% (range 17%–100%) of those referred receiving a new hypertension diagnosis or new antihypertensive treatment. In 6 out of the 8 studies, this proportion exceeding 40%.
DISCUSSION
The results of this review show that community screening of BP by non-physicians (including self-screening) appears effective for detecting raised BP at screening, and that where data exists for this outcome, high screening BP leads to a new diagnosis or treatment for hypertension in a median of 44% of those referred. However, given the large amount of heterogeneity between study designs, it was not possible to carry out meta-analyses. Combined with the large amounts of variability in results between studies, this makes it difficult to recommend an optimal approach or setting. However, given the likely lower cost of self-screening compared to screening using nurses and other healthcare professionals, it is notable that self-screening appears to detect a similar proportion of participants with high BP as other screening strategies.
While many patients with existing hypertension may use community screening facilities, this is not necessarily a concern, particularly given the proportion of treated patients with uncontrolled BP.6 Raised pressure in treated hypertensives may prompt them to seek further appropriate medical care. Clear pathways for the referral and follow-up of patients identified with increased BP at screening are essential if the diagnosis of hypertension is to be established and any management benefits realized, but few studies reported any aspect of such follow-up. In many cases, raised screening BP was not subsequently acted upon, with only 3 out of 7 studies evaluating a system with universal referral of all such participants. Reassuringly, where participants were referred and subsequently attended primary care, around 40% received an intervention (new hypertension diagnosis or antihypertensive therapy), indicating the value of follow-up.
Considerable heterogeneity was observed across all analyses, despite stratification, precluding formal meta-analysis. The remaining heterogeneity likely reflects differences in the underlying study populations, and how well these populations are able to access hypertension diagnosis and treatment options. Additional potential sources of heterogeneity include methods of BP measurement, participant age range (which was typically poorly defined), and the influence of recruitment methods, some of which may have been more effective at targeting high-risk populations.
Blinding to existing hypertension status was poorly reported, but other than self-screening, there are no methodological barriers to blinding observers to this outcome. Although a lack of blinding would not be a significant concern for studies using automated devices, many studies in the review used manual BP measurement, which is known to be subject to terminal digit preference, and so observer bias may have been an issue for some of these studies where blinding was not present.17,18
The majority of studies (39, 53%) were undertaken in the United States. We may have missed studies from other countries; however, we did screen over 16,000 studies, and examined 285 full text papers. This suggests a lack of generalizability of our findings to other countries, as the effects of screening may be dependent on the organization and coverage of the healthcare system.
No previous systematic reviews of community screening or self-screening for hypertension were identified in the search results, suggesting that this paper provides the first comprehensive review of the literature on this subject. International community-based surveys of BP and hypertension prevalence continue to suggest both significant proportions of undetected hypertension and of poor control among those detected.19
The quality of the studies we found limits our ability to come to a definite conclusion as to the best method for implementing hypertension screening. We therefore perceive the need for high-quality studies that include BP target definitions, measurement methods, and subsequent data on the proportion of new hypertensive patients diagnosed. Indeed, those implementing self-screening should routinely embed a robust evaluation to underpin the ongoing use of resources in this area. To ultimately determine the cost effectiveness of these methods, there will be a need for robust randomized trials.
New developments in technology, including the use of social media to promote screening, use of smartphones, and enhanced network connectivity enabling screening results to be incorporated directly into electronic medical records, may improve the uptake and efficacy of community BP screening, and particularly self-screening.20
As few studies followed up all participants to diagnosis, we are unable to assess what proportion of participants with raised BP at screening had true hypertension. The lack of studies with adequate follow-up make it currently impossible to determine whether these initiatives are effective or worthwhile. Properly powered studies including both cost and efficacy data are therefore required. As with standard clinical practice, such studies should follow-up all cases of raised BP with robust diagnostic methods.
In conclusion, despite a large number of studies reporting community-based BP screening by non-physicians, the evidence base for its effectiveness is very poor. Detection of high screening BP by self-screening is similar to that of more resource-intensive methodologies to identify participants with high BP, but cannot currently be recommended due to a paucity of data on this methodology.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at American Journal of Hypertension (http://ajh.oxfordjournals.org).
DISCLOSURE
H.A. is in receipt of a fellowship from the National Institute for Health Research School for Primary Care Research (NIHR SPCR), and receives grant funding from the NIHR. S.G. has received support from the NIHR for travel to meetings. F.D.R.H. is part funded, through supervision sessions, by the NIHR SPCR, NIHR Oxford Biomedical Research Centre, and NIHR Collaboration for Leadership in Applied Health Research and Care Oxford, but underwritten by Oxford University (and therefore partly by the Higher Education Funding Council for England). Research part funded by the above, plus the Medical Research Council, Wellcome, NHS Support for Science, and industrial NIHR Health Technology Assessment sponsors of equipment or research conduct or dissemination (Roche Diagnostics, Omron, Microlife, Bayer, Pfizer/BMS, BI, and Amgen in the past 3 years). R.J.M. holds an NIHR professorship and receives grant funding from the NIHR. In addition, he has received research funding from Lloyds Pharmacy and Omron for blood pressure monitoring equipment and payment and expenses from the Japanese Society of Hypertension for speaking at a conference. A.W. holds grant funding from the NIHR, the NIHR SPCR, and the WHO. C.H. has received expenses and payments for his media work from Channel 4, BBC, FreshOne TV productions and the Guardian, and also expenses from the WHO and the US FDA, and holds grant funding from the NIHR, the NIHR SPCR, The Wellcome Trust, and the WHO. In addition, C.H. is an expert witness in an ongoing medical device legal case, has received payment from BUPA for analyzing and appraising guidelines and income from the publication of a series of toolkit books published by Blackwells. On occasion C.H. receives expenses for teaching EBM and is paid for NHS GP work in the out of hours service in Oxford. C.H. is also a director of CEBMi, which produces an iphone application with the BMJ, but receives no payment for this activity. The authors report no other relevant conflicts of interest.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank D. Yeomans and D. Shaw for their valuable suggestions and support while carrying out this review. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. This article presents independent research funded by a National Institute for Health Research Programme Grant RP-PG-1209–10051.
REFERENCES
- 1. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng AT, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FG, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD, 3rd, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Mohd Hanafiah K, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CD, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA, 3rd, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJ, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, Van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJ, Ezzati M, AlMazroa MA, Memish ZA. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organisation. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. 2009. [Google Scholar]
- 3. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009; 338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013: 1–8. [PubMed] [Google Scholar]
- 5. Wilkins K, Campbell NR, Joffres MR, McAlister FA, Nichol M, Quach S, Johansen HL, Tremblay MS. Blood pressure in Canadian adults. Health Rep 2010; 21:37–46. [PubMed] [Google Scholar]
- 6. Craig R, Mindell J. Health Survey for England 2011: Health, social care and lifestyles. Health & Social Care Information Centre, Leeds, 2012. [Google Scholar]
- 7. Houle SK, Chuck AW, Tsuyuki RT. Blood pressure kiosks for medication therapy management programs: business opportunity for pharmacists. J Am Pharm Assoc (2003) 2012; 52:188–194. [DOI] [PubMed] [Google Scholar]
- 8. Kaczorowski J, Chambers LW, Dolovich L, Paterson JM, Karwalajtys T, Gierman T, Farrell B, McDonough B, Thabane L, Tu K, Zagorski B, Goeree R, Levitt CA, Hogg W, Laryea S, Carter MA, Cross D, Sabaldt RJ. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP). BMJ 2011; 342:d442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011; 155:529–536. [DOI] [PubMed] [Google Scholar]
- 10. Chambers J, Cleveland W, Kleiner B, Tukey P. Graphical Methods for Data Analysis. Wadsworth: Belmont, CA, 1983. [Google Scholar]
- 11. Carrington MJ, Jennings GL, Stewart S. Pattern of blood pressure in Australian adults: results from a national blood pressure screening day of 13,825 adults. Int J Cardiol 2010; 145:461–467. [DOI] [PubMed] [Google Scholar]
- 12. Nugent CA, Gerlach BA. Hypertension control: the role of screening and referral to community physicians. Prev Med 1980; 9:569–577. [DOI] [PubMed] [Google Scholar]
- 13. Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, Knowles P, Storm JS, Adhikari E, Bibbins-Domingo K, Coxson PG, Pletcher MJ, Hannan P, Haley RW. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med 2011; 171:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hamilton W, Round A, Goodchild R, Baker C. Do community based self-reading sphygmomanometers improve detection of hypertension? A feasibility study. J Public Health Med 2003; 25:125–130. [DOI] [PubMed] [Google Scholar]
- 15. Houle SK, Tsuyuki RT. Public-use blood pressure machines in pharmacies for identification of undetected hypertension in the community. J Clin Hypertens (Greenwich) 2013; 15:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Edwards C. Blood pressure measurement by pharmacists. J R Coll Gen Pract 1981; 31:674–676. [PMC free article] [PubMed] [Google Scholar]
- 17. Hla KM, Vokaty KA, Feussner JR. Observer error in systolic blood pressure measurement in the elderly. A case for automatic recorders? Arch Intern Med 1986; 146:2373–2376. [PubMed] [Google Scholar]
- 18. Rose GA, Holland WW, Crowley EA. A Sphygmomanometer For Epidemiologists. Lancet 1964; 1:296–300. [DOI] [PubMed] [Google Scholar]
- 19. Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, McAlister FA, Johansen H, Baclic O, Campbell N. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open 2013; 3:e003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Logan AG. Community hypertension programs in the age of mobile technology and social media. Am J Hypertens 2014; 27:1033–1035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.