Abstract
Aim
High-quality cardiopulmonary resuscitation (CPR) may improve survival. The quality of CPR performed during pediatric out-of-hospital cardiac arrest (p-OHCA) is largely unknown. The main objective of this study was to describe the quality of CPR performed during p-OHCA resuscitation attempts.
Methods
Prospective observational multi-center cohort study of p-OHCA patients ≥1 and < 19 years of age registered in the Resuscitation Outcomes Consortium (ROC) Epistry database. The primary outcome was an a priori composite variable of compliance with American Heart Association (AHA) guidelines for both chest compression (CC) rate and CC fraction (CCF). Event compliance was defined as a case with 60% or more of its minute epochs compliant with AHA targets (rate 100–120 min−1; depth ≥38 mm; and CCF ≥0.80). In a secondary analysis, multivariable logistic regression was used to evaluate the association between guideline compliance and return of spontaneous circulation (ROSC).
Results
Between December 2005 and December 2012, 2,564 pediatric events were treated by EMS providers, 390 of which were included in the final cohort. Of these events, 22% achieved AHA compliance for both rate and CCF, 36% for rate alone, 53% for CCF alone, and 58% for depth alone. Over time, there was a significant increase in CCF (p< 0.001) and depth (p=0.03). After controlling for potential confounders, there was no significant association between AHA guideline compliance and ROSC.
Conclusions
In this multi-center study, we have established that there are opportunities for professional rescuers to improve prehospital CPR quality. Encouragingly, CCF and depth both increased significantly over time.
Introduction
Pediatric out-of-hospital cardiac arrest (p-OHCA) affects thousands of children around the world each year.1–4 Over the past decade, there have been significant improvements in survival after pediatric in-hospital cardiac arrest;5 yet, p-OHCA continues to be associated with poor outcome. Best estimates reveal that less than 10 percent of children will survive to hospital discharge with favorable neurological outcome after p-OHCA.1–3 The potential years of lost productive life are substantial.
Several studies have demonstrated that professional rescuer CPR has room for improvement.6–10 Inadequate chest compression rate9,11,12 and depth,10,13 and long interruptions in CPR,6–8 have been particularly problematic. As of yet, these studies have excluded p-OHCA resuscitation, focusing on either adult or in-hospital pediatric CPR quality. As high CPR quality is associated with improved cardiac arrest outcome,6,9,10,14,15 investigations designed to describe current practice and suggest areas for improvements in prehospital resuscitation quality are an attractive approach to improve outcomes.
When compared to adults, relatively little quantitative CPR data have been collected in children during cardiac arrest. As a result, pediatric CPR guidelines have been developed with data often extrapolated from adult and animal investigations.16,17 Most of what we know about pediatric resuscitation quality comes from single center in-hospital investigations.12,14,18–20 As such, there is a need for larger pediatric studies that can describe resuscitation practice, and rigorously evaluate the association between CPR quality measures and survival in children.
The main objective of this study was to describe the quality of CPR performed during p-OHCA resuscitation attempts. The secondary objective was to evaluate the association between American Heart Association (AHA) guidelines and survival outcomes. We hypothesized that the quality of out-of-hospital pediatric CPR would frequently not meet recommended care targets, and further, that CPR performed in compliance with AHA guidelines17 is associated with improved short term survival.
Methods
Design and Setting
This was a prospective observational cohort study of data collected from the Resuscitation Outcomes Consortium (ROC). The ROC consists of 36,000 EMS professionals within 260 EMS agencies transporting patients to 287 different hospitals.21 This study includes ROC Epistry–Cardiac Arrest22 patients treated by EMS and for whom pediatric CPR quality data was available (101 agencies from 11 sites). Appropriate local institutional review boards (U.S.) or research ethics boards (Canada) granted a waiver of documentation of written consent under minimal risk criteria. Strict confidentiality was maintained at all times and no personal identifiers were retained in the database.
Population
We included all children < 19 years of age from the ROC Epistry who received chest compressions (CCs) by EMS providers for non-traumatic cardiac arrest. We excluded patients < 1 year of age in an attempt to omit cases of sudden infant death syndrome (SIDS), where the likelihood of a good outcome irrespective of resuscitation quality is exceedingly rare.1 We excluded cases with < 1 minute of quantitative data for rate or chest compression fraction (fraction of time during cardiac arrest that CCs are provided; CCF). Compression depth data were available for only a fraction of cases because commercially available CPR recording devices are primarily approved for older children (≥8 years of age)12 and many monitors do not measure or report this variable.
Data Collection
Quantitative CPR quality data was obtained by commercially available CPR recording defibrillators (Physio-Control, Redmond, WA: n=227; Philips Healthcare, Andover MA: n=40; Zoll Medical Corporation, Chelmsford, MA: n=113; Other/unknown: n=10). CPR feedback was available on all monitors; however, this study did not capture which responding agencies employed the technology (i.e., was feedback enabled?). Therefore, we cannot report with certainty which cases received CPR feedback. The following CPR process measures were collected when available: 1) CC rate (min−1); 2) depth (mm); and 3) CCF. Averages during each minute of recorded CPR were collected for each subject. Only the first ten minutes of CPR with quantitative data were included in the analysis.
Patient and clinical data were abstracted from EMS and hospital records by trained research staff at the individual study sites using standardized definitions for patient characteristics, EMS processes, and outcomes. After local abstraction, data were de-identified and then transmitted electronically to the data coordinating center (DCC). Data quality assurance by the DCC included internal checks for consistency of the data, comparisons to reference ranges, data audits, and site visits.22
Study Variables
Event compliance with AHA guidelines was defined a priori as a case with 60% or more of its minute epochs10,14,15 compliant with AHA targets (rate 100–120 min−1; depth ≥38mm (2005 AHA recommendation); and CCF ≥0.80.23,24 The definition for AHA compliance includes recommendations from the 2013 AHA CPR Quality Consensus Statement24 and the 2005 Guidelines.23 The authors chose to include the depth target of 2005 because most of the events happened before deeper compressions (≥51mm) were recommended in the 2010 Guidelines.17 In a secondary analysis, we defined event compliance as a case with 90% or more of its minute epochs compliant with AHA targets. All available minutes of resuscitation were included up to and including minute ten. We first described an a priori composite variable of AHA compliance for both rate and CCF. Additional CPR quality outcomes included AHA compliance for each of the individual CPR quality parameters, the CPR quality targets expressed as continuous variables, and 2010 AHA depth compliance defined as ≥51mm for all subjects ≥1 year of age.17 Because of varying recording devices, this study has two distinct cohorts: 1) events with at least rate and CCF; and 2) a smaller subgroup that also had quantitative depth collected. A priori we chose to report CPR quality in two separate age categories (pediatric: ages 1–11 years; adolescent: ≥12 years), a distinction currently recognized by the AHA guidelines.17
For our second objective, the primary outcome was return of spontaneous circulation (ROSC), chosen based upon the following considerations: 1) it is the most proximate outcome to the resuscitation, and 2) previous studies of p-OHCA1–4 demonstrated low rates of survival to hospital discharge which would limit our ability to adjust for potential confounders in multivariable models. Secondary outcomes included survival to 24 hours and survival to hospital discharge. Covariates included in the multivariable logistic regression models evaluating the association between fraction and rate compliance and outcomes were selected a priori based on scientific understanding, and included age (categorical), gender, witnessed status, bystander CPR, EMS response time, initial rhythm, defibrillation data, location of arrest, and the natural cubic spline of adult survival to hospital admission at each site. The latter variable was included in an attempt to adjust for site variation in resuscitation care. Univariate association with depth was used to select a reduced subset of potential confounding variables to include in the models of depth and outcomes, and resulted in the inclusion of age, gender, witnessed status, initial rhythm, location of arrest, and site adjustment.
Statistical Analysis
Standard descriptive statistics, appropriate for the distribution of each variable, were used to summarize the quality of CPR performed during p-OHCA resuscitation. In the primary analysis, proportions of resuscitations meeting AHA event compliance definitions were reported. Differences in baseline characteristics between analyzed and excluded patients, and between pediatric and adolescent arrest victims, were evaluated using Student’s t-test or chi-squared testing as appropriate. The association between event AHA compliance and survival outcomes was quantified using multivariable logistic regression with Huber-White sandwich standard errors.25,26 Effect of calendar year on CPR quality was assessed using a Wald test for linear trend. All statistical analyses were performed with commercially available statistical packages (SAS, version 9.3, Cary, NC; R, version 2.14.1, Vienna, Austria; STATA, version 12.0, College Station, TX).
Results
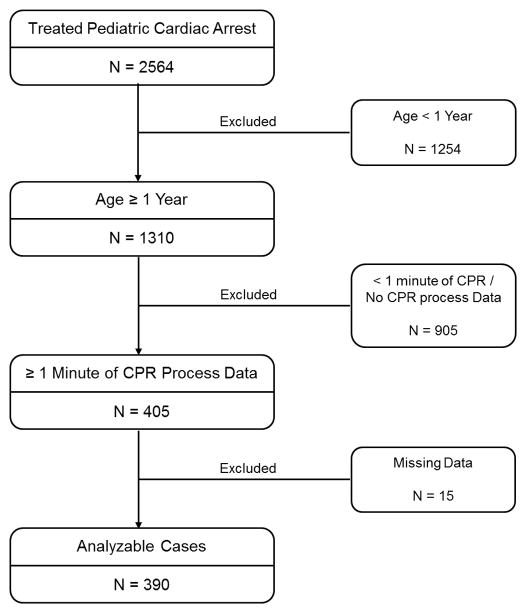
Between December 2005 to December 2012, 2,564 cases of pediatric cardiac arrest were treated by the EMS agencies of the ROC. All but 390 were excluded from the current study for the reasons indicated in Figure 1. Quantitative CC depth was available for 153 cases (pediatric n = 34; adolescent n = 119). There were notable differences between the subjects in the final cohort and the excluded population. Excluded patients were younger with characteristics typical of infant cardiac arrest (e.g., more unwitnessed, less bystander CPR, less VF/VT) and with lower survival rates (Table 1). The included cohort was older with 53% bystander CPR and 16% shockable rhythms. Of subjects in the final cohort, 31.8% had ROSC, 27.4% survived to 24 hours, and 13.8% survived to hospital discharge. Subject characteristics of the pediatric and adolescent subgroups are detailed in Table 1.
Figure 1.
Patient flow diagram.
Table 1.
Descriptive Statistics of Analyzed and Excluded Populations1
| Overall Analyzed Cohort | Excluded | p3 | Analyzed 1 to 11 years | Analyzed 12 to 18 years | p4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | N | N | N | |||||||
|
|
||||||||||
| N | 390 | 2174 | 146 | 244 | ||||||
| Age (years) | 390 | 11.9 (± 5.6) | 2174 | 4.0 (± 5.9) | <0.01 | 146 | 5.4 (± 3.5) | 244 | 15.8 (± 1.9) | <0.01 |
| Male | 390 | 247 (63.3 %) | 2165 | 1288 (59.5 %) | 0.15 | 146 | 85 (58.2 %) | 244 | 162 (66.4 %) | 0.10 |
| Witnessed status | <0.01 | 0.26 | ||||||||
| EMS witnessed | 390 | 15 (3.8 %) | 2174 | 87 (4 %) | 146 | 4 (2.7 %) | 244 | 11 (4.5 %) | ||
| Bystander witnessed | 390 | 128 (32.8 %) | 2174 | 432 (19.9 %) | 146 | 48 (32.9 %) | 244 | 80 (32.8 %) | ||
| Not witnessed | 390 | 236 (60.5 %) | 2174 | 1459 (67.1 %) | 146 | 87 (59.6 %) | 244 | 149 (61.1 %) | ||
| Unknown/missing | 390 | 11 (2.8 %) | 2174 | 196 (9 %) | 146 | 7 (4.8 %) | 244 | 4 (1.6 %) | ||
| Bystander CPR | 390 | 206 (52.8 %) | 2174 | 1010 (46.5 %) | 0.02 | 146 | 88 (60.3 %) | 244 | 118 (48.4 %) | 0.02 |
| EMS response time (minutes)2 | 375 | 6 (± 2.6) | 1972 | 5.7 (± 3.5) | 0.11 | 142 | 5.4 (± 1.9) | 233 | 6.3 (± 2.9) | <0.01 |
| Initial rhythm | <0.01 | <0.01 | ||||||||
| VT/VF/AED-Shock | 390 | 61 (15.6 %) | 2174 | 102 (4.7 %) | 146 | 10 (6.8 %) | 244 | 51 (20.9 %) | ||
| Pulseless Electrical Activity | 390 | 58 (14.9 %) | 2174 | 245 (11.3 %) | 146 | 24 (16.4 %) | 244 | 34 (13.9 %) | ||
| Asystole | 390 | 250 (64.1 %) | 2174 | 1286 (59.2 %) | 146 | 105 (71.9 %) | 244 | 145 (59.4 %) | ||
| Cannot determine/other | 390 | 21 (5.4 %) | 2174 | 541 (24.9 %) | 146 | 7 (4.8 %) | 244 | 14 (5.7 %) | ||
| Shock Delivered | 390 | 104 (26.7 %) | 2161 | 222 (10.3 %) | <0.01 | 146 | 19 (13.0 %) | 244 | 85 (34.8 %) | <0.01 |
| Number of shocks (if shocked) | 102 | 2.8 (± 2.4) | 219 | 2.6 (± 2.4) | 0.35 | 17 | 2.4 (± 1.7) | 85 | 2.9 (± 2.5) | 0.23 |
| Public location | 390 | 74 (19.0 %) | 2158 | 203 (9.4 %) | <0.01 | 146 | 18 (12.3 %) | 244 | 56 (23.0 %) | <0.01 |
| ROSC | 390 | 124 (31.8 %) | 2173 | 312 (14.4 %) | <0.01 | 146 | 28 (19.2 %) | 244 | 96 (39.3 %) | <0.01 |
| Survival to 24 hours | 383 | 105 (27.4 %) | 2094 | 366 (17.5 %) | <0.01 | 143 | 26 (18.2 %) | 240 | 79 (32.9 %) | <0.01 |
| Survival to hospital discharge | 383 | 53 (13.8 %) | 2097 | 153 (7.3 %) | <0.01 | 143 | 15 (10.5 %) | 240 | 38 (15.8 %) | 0.14 |
Categorical variables are reported as No. (%). Continuous variables are reported as mean (± standard deviation).
Excludes EMS witnessed cases.
p value for comparison across included and excluded populations
p value for comparison across pre-determined age categories
Quantitative CPR Quality Data (Table 2)
Table 2.
Summary of CPR Quality Parameters in Analyzed Population1
| Overall Cohort | 1 to 11 years | 12 to 18 years | p-value2 | |
|---|---|---|---|---|
| Summary Statistics | ||||
| Fraction | ||||
| No. (%) | 390 (100.0 %) | 146 (100 %) | 244 (100 %) | |
| Mean (± SD) | 0.76 (± 0.17) | 0.78 (± 0.19) | 0.75 (± 0.15) | 0.16 |
| Rate | ||||
| No. (%) | 390 (100.0 %) | 146 (100 %) | 244 (100 %) | |
| Mean (± SD) | 118.7 (± 22.2) | 124.7 (± 28.3) | 115.1 (± 16.8) | <0.01 |
| Depth | ||||
| No. (%) | 153 (39.2 %) | 34 (23.3 %) | 119 (48.8 %) | |
| Mean (± SD) | 39.5 (± 10.7) | 32.5 (± 9.8) | 41.5 (± 10.1) | <0.01 |
| Compliance with AHA Guidelines | ||||
| Fraction and Rate Compliant | 85 (21.8 %) | 22 (15.1 %) | 63 (25.8 %) | 0.01 |
| Fraction Compliant (≥ 0.80) | 205 (52.6 %) | 92 (63 %) | 113 (46.3 %) | <0.01 |
| Rate Compliant (≥ 100 and ≤ 120 per minute) | 141 (36.2 %) | 34 (23.3 %) | 107 (43.9 %) | <0.01 |
| Depth Compliant (≥ 38 mm) | 89 (58.2 %) | 12 (35.3 %) | 77 (64.7 %) | <0.01 |
| Depth Compliant (≥ 51 mm)3 | 12 (16.0 %) | 0 (0 %) | 12 (21.8 %) | 0.02 |
Categorical variables are reported as No. (%). Continuous variables are reported as mean (± standard deviation).
p value for comparison across pre-determined age categories
Arrests occurring in 2011 or later.
For the overall cohort, the median number of CPR process minutes included in the analysis is 7 (IQR: 5, 10), which represent a median of 43% (IQR: 27%, 75%) of the overall CPR duration. Summary statistics for the quantitative CPR quality variables are as follows: CPR fraction 0.76 ± 0.17; rate: 118.7 ± 22.2 min−1; depth 39.5 ± 10.7 mm. For the primary analysis (60% of event epochs achieving targets), the proportion of events meeting AHA compliance targets was low. Specifically, 22% of events met criteria for both rate and CCF, 36% for rate alone, 53% for CCF alone, and 58% for depth alone. In arrests from 2011 and later, compliance with 2010 AHA Guidelines for depth was not common (16% overall), with none of the events in 1–11 year olds meeting criteria and only 12 (21.8%) of the events in 12–18 year olds having depth ≥51mm. Compared to events in 12–18 year old subjects, events in 1–11 year olds were characterized by: lower proportions of rate compliance (23.3 vs. 43.9 %) and depth compliance (35.3 vs. 64.7%) and a higher proportion of CCF compliance (63 vs. 46.3 %); p<0.01 for all comparisons. In our secondary analysis (90% of event epochs achieving targets), event compliance was much lower: 18% for rate alone; 15% for CCF alone; and 35% for depth alone. There was an inverted U-shaped relationship between CC depth and rate (test of splines, p<0.01, Figure 2).
Figure 2.
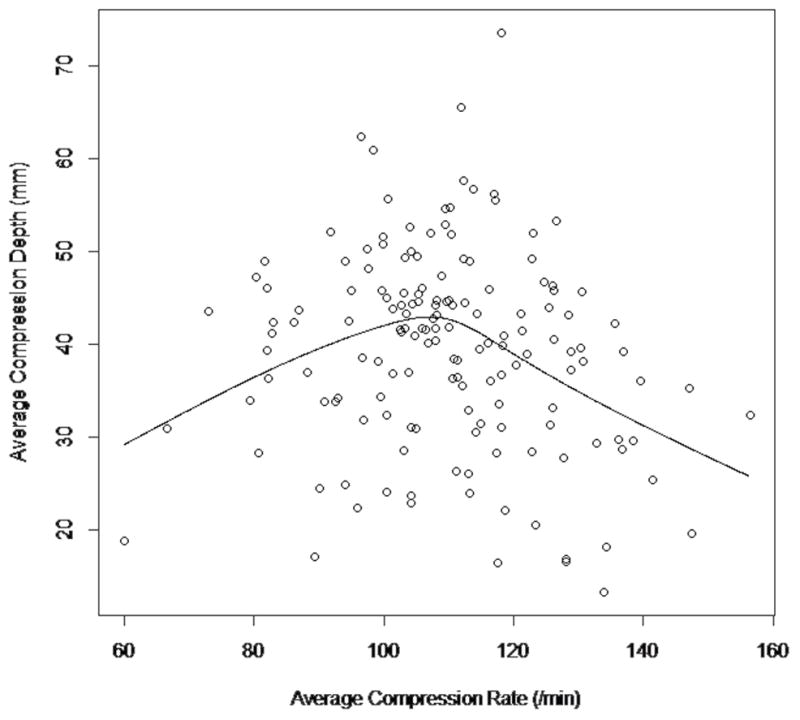
Spline from a linear regression using a normal spline basis with four degrees of freedom. The F-test of whether the spline is significantly different from a straight line has a p-value <0.001.
Secondary Variables
For the entire cohort, ROSC occurred more frequently when CPR was compliant for rate (39.7% vs. 27.2%), but ROSC occurred less often when cases were compliant with CCF recommendations (26.3% vs. 37.8%; eTable 1; p=0.01 for both comparisons). After adjusting for potential confounders, there was no significant association between rate or CCF compliance and any of the survival outcomes (Table 3a). Age, bystander witnessed arrest, and shockable initial rhythm were associated with a higher odds of ROSC (Table 3a).
Table 3a.
Adjusted logistic regression of outcome on compliance
| ROSC (n=390) | Survival to 24 Hours (n=383) | Survival to Discharge (n=383) | ||||
|---|---|---|---|---|---|---|
| aOR1 (95% CI) | p | aOR1 (95% CI) | p | aOR1 (95% CI) | p | |
| Fraction compliant (≥ 0.8) | 0.69 (0.42, 1.15) | 0.16 | 0.96 (0.56, 1.66) | 0.89 | 0.98 (0.41, 2.35) | 0.97 |
| Rate compliant (100–120) | 1.50 (0.88, 2.54) | 0.13 | 1.07 (0.61, 1.89) | 0.80 | 1.14 (0.51, 2.53) | 0.76 |
| Age 1–11 years | 0.49 (0.28, 0.85) | 0.01 | 0.53 (0.30, 0.94) | 0.03 | 1.11 (0.47, 2.59) | 0.82 |
| Male | 0.85 (0.52, 1.40) | 0.52 | 0.64 (0.38, 1.08) | 0.09 | 0.75 (0.35, 1.60) | 0.46 |
| Bystander witnessed arrest | 1.66 (0.96, 2.87) | 0.07 | 1.04 (0.59, 1.86) | 0.88 | 3.65 (1.62, 8.25) | 0.00 |
| EMS witnessed arrest | 1.89 (0.52, 6.92) | 0.33 | 0.59 (0.16, 2.21) | 0.44 | 0.95 (0.08, 11.02) | 0.97 |
| Shockable initial rhythm | 4.58 (2.25, 9.30) | <0.01 | 6.81 (3.26, 14.20) | <0.01 | 13.06 (5.56, 30.69) | <0.01 |
| EMS response time (minutes) | 0.95 (0.83, 1.08) | 0.40 | 0.88 (0.79, 0.98) | 0.02 | 0.86 (0.75, 1.00) | 0.05 |
| Bystander CPR | 1.18 (0.70, 1.99) | 0.54 | 1.01 (0.59, 1.73) | 0.97 | 1.05 (0.49, 2.24) | 0.90 |
| Public location | 1.60 (0.84, 3.03) | 0.15 | 1.58 (0.82, 3.05) | 0.17 | 0.88 (0.31, 2.52) | 0.81 |
Odds ratio also adjusted for adult survival to hospital admission at each site as a measure of site variation in care. A sensitivity analysis that substituted an indicator of study site did not substantially alter the results.
In the subset of subjects for whom CC depth data were available (n=153), ROSC occurred more frequently when CPR was compliant with recommended depth (49.4% vs. 29.7%; p=0.01) (eTable 1). After adjusting for potential confounders, there was no significant association between depth compliance and ROSC. In this subset of subjects, shockable initial rhythm was associated with ROSC (Table 3b).
Table 4.
Table 3b. Adjusted logistic regression of ROSC on compliance in subset of events with depth
| ROSC (n=153) | ||
|---|---|---|
| aOR1 (95% CI) | p | |
| Depth compliant (≥38 mm) | 1.99 (0.90, 4.42) | 0.09 |
| Fraction compliant (≥0.8) | 0.66 (0.31, 1.40) | 0.28 |
| Rate compliant (100–120) | 1.13 (0.52, 2.45) | 0.75 |
| Age 1–11 years | 0.50 (0.19, 1.30) | 0.15 |
| Male | 0.90 (0.43, 1.89) | 0.78 |
| Bystander witnessed arrest | 1.13 (0.46, 2.82) | 0.79 |
| EMS witnessed arrest | 2.70 (0.48, 15.18) | 0.26 |
| Shockable initial rhythm | 5.62 (1.62, 19.51) | <0.01 |
| Public location | 1.19 (0.45, 3.13) | 0.73 |
Odds ratio also adjusted for adult survival to hospital admission at each site as a measure of site variation in care.
Discussion
In this large multi-center study of out-of-hospital pediatric CPR quality, we observed that prehospital rescuer CPR frequently did not meet AHA guidelines during p-OHCA resuscitation attempts. In spite of a definition of event compliance requiring only 60% of the minutes to have achieved quality goals, less than 25% of the resuscitations met both rate and CPR fraction targets. Achieving 2010 AHA depth targets (≥51mm) was even less common, as only 16% of resuscitations from 2011 and later achieved this goal. Encouragingly, the survival to hospital discharge rate in this large multi-center cohort was 13.8%–one of the highest reported for p-OHCA to date. Importantly CCF and depth have both increased significantly over time. A higher percentage of events meeting rate or depth compliance achieved ROSC; however, after controlling for potential confounders, we found no significant association between any of the CPR quality targets and survival.
Most pediatric CPR quality data has come from single center studies of in-hospital resuscitation.12,14,18–20 This study fills an important gap in the pediatric resuscitation knowledge base by providing multi-center pediatric CPR quality data and describing the landscape of p-OHCA resuscitation quality. Similar to previous in-hospital reports, healthcare providers had difficulty delivering CPR compliant with AHA guidelines. This occurred despite network-wide attention devoted to the study and to the delivery of high quality CPR.22 We do not know if these data are completely representative of CPR quality outside of this network.
The survival to hospital discharge rate in this study was 13.8%, one of the highest reported for p-OHCA to date.1–4 Yet, nearly three times as many children will survive to discharge if their cardiac arrest occurs in a hospital compared to this out-of-hospital cohort.5 Low survival rates after p-OHCA are attributable to numerous factors such as witnessed status, initial rhythms, and period of untreated arrest.1,4 However, these data suggest that CPR quality is also a modifiable risk factor for survival outcomes. In a recent study by Wolfe et al., post-cardiac arrest debriefing was used to improve pediatric in-hospital CPR quality.27 In that before-after interventional study, the authors reported doubling AHA compliance rates and concomitantly, the rate of survival to discharge with good neurological outcome rates also nearly doubled. In short, achieving high levels of compliance with AHA guidelines is possible, and more importantly, there is an association between improved CPR quality and survival outcome. As the rate of AHA compliance in that study was much higher than what we report here, interventions to improve prehospital pediatric CPR quality are warranted, and if successful, could result in more children surviving their event.
Previous studies of pediatric in-hospital CPR have demonstrated a strong association between CPR quality and survival outcomes, particularly as it pertains to CC depth10,14,15 and CCF.6,8 The apparent lack of association in this study deserves comment. The primary aim of this observational study was to quantitatively describe the quality of CPR performed during prehospital resuscitation attempts. This study was not powered to detect differences in ROSC or survival. However, it is encouraging that compared to a previous ROC investigation encompassing events up to 2007,1 we report a nearly 40% relative increase in the rate of survival to discharge. These improved survival rates occurred as CCF and depth were increasing significantly over time. While speculative, this may suggest that efforts to improve resuscitation quality may lead to improved p-OHCA survival. Further, we hypothesize that life-saving clinical interventions such as defibrillation, which lower CCF, may have “falsely” indicated that CCF compliance is not associated with outcome. This speculation is supported by our data where shockable initial rhythm was most associated with survival (Table 3a and 3b).
In previous adult studies, when rescuers compressed the chest at a high rate, the compressions were less deep,9 suggesting that rescuers might compromise adequate chest compression depth when trying to increase compression rate. In a previous single center study of pediatric in-hospital CPR quality,14 the same relationship was not observed. The authors of this pediatric study hypothesized that either lack of variation in chest compression rate (there were no extremes of compression rate which could have compromised depth in this study) or the higher compliance of pediatric chest walls (i.e., providers could push hard and fast) explained this apparent lack of association between chest compression depth and rate. Our data here may provide further insight suggesting the former may be true. In this study, there was a large variation in CC rate and indeed, we found a non-linear relationship between CC rate and depth–which were inversely associated at high CC rates. Therefore, future Guideline iterations may consider emphasizing the importance of avoiding excessive CC rate even in children so as to avoid compromising CC depth. However, the upper limit of rate at which CC depth would be compromised in children still remains an unanswered question.
This study has limitations. First, the data reported here represent a convenience sample of ROC cases during which pediatric CPR quality data was collected. Important differences were noted between the included and excluded populations (Table 1). Our study population was primarily an adolescent population.17 Future studies of prehospital CPR quality in pre-pubertal children are warranted. Second, ventilation rate, incomplete release between compressions, and peri-shock pauses in CPR, important quality variables,8,28–30 were not recorded. Third, while we reported the first ten minutes of recorded CPR in an attempt to limit our evaluation to the first critical minutes of the resuscitation, the authors do not know with certainty how long CPR was provided before sensor placement in many cases. While speculative, it is possible that during pediatric resuscitation attempts, which more commonly have a preceding respiratory deterioration,31,32 that EMS providers focused on early airway management prior to defibrillator deployment. Later assessment of CPR quality could partly explain the lack of association between quality and survival, as children with longer cardiac arrest events (and more eligible minutes of quality recording) would be selected for this analysis. Finally, it is important to note that the compliance targets used in the primary analysis, while based upon the best available science23,24 and consistent with previous publications,10,14,15 do entail some level of arbitrary assignment. The optimal cut-points associated with survival represent a significant gap in the pediatric resuscitation science knowledge base that will require further study.
Conclusions
These data fill an important gap in our knowledge related to p-OHCA resuscitation. In this multi-center observational study of pediatric CPR quality, professional rescuers often failed to achieve compliance with AHA guidelines. Encouragingly, CCF and depth have both increased significantly over time in this large multi-center cohort. Future interventions to improve p-OHCA resuscitation quality may improve survival outcomes.
Supplementary Material
Figure 3.
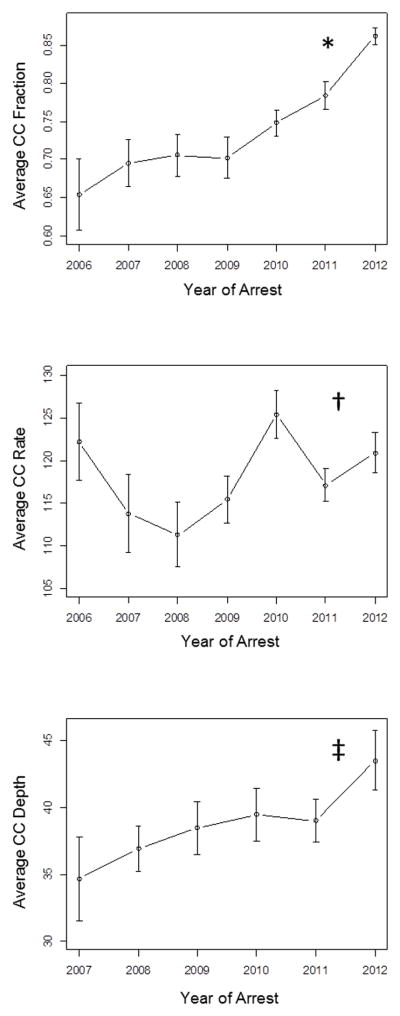
Averages for chest compression fraction (CCF), CC rate, and CC depth over calendar year. Error bars represent standard error of the mean. Wald test of trend: *p=<0.001; †p=0.09; ‡p=0.03.
Footnotes
Conflicts of Interest
Dr. Robert M. Sutton receives funding from the National Institute of Child Health and Human Development (NICHD; K23HD062629) and has received a speaker honoraria from Zoll Medical. Dr. Christian Vaillancourt is supported by a University of Ottawa Research Chair. He has received funding from the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, and the National Institutes of Health (NIH) for work related to cardiac arrest and prehospital care. Dr. Mohamud Daya receives funding from the NIH and is an unpaid consultant for Philips HealthCare. Dr. Sheldon Cheskes receives grant funding from the NIH as co-primary investigator (PI) of the ROC Toronto site. He has received speaker honoraria and funding from Zoll Medical. Dr. Ahamed H. Idris receives research funding from the National Heart, Lung, and Blood Institute (NHLBI), the US Army, and the AHA. Dr. James J. Menegazzi receives funding from the NHLBI (R01HL117979). Dr. Graham Nichol has received support from the NIH as co-PI of the ROC Coordinating Center. He is the PI of the Dynamic AED Registry which is funded by the Food and Drug Administration, Cardiac Science Corporation, Heartsine Technologies Inc., Philips Healthcare Inc., Physio-Control Inc., and the Zoll Medical Corporation. He is PI of the Simple EMS Registry funded by the AHA, and PI of the Washington Study of Ultrasound in Resuscitation funded by Philips Healthcare Inc. Erin Case, Jack Nuttall, Heather Herren, and Drs. Ian R. Drennan, Michael A. Austin, Siobhan P. Brown, Clifton W. Callaway, Douglas L. Andrusiek, Jim Christenson, Diane L. Atkins, Vinay M. Nadkarni, Jonathan Kaltman, Jamie Hutchison, Thomas D. Rea, and Robert A. Berg have nothing to disclose.
Financial Disclosure: The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077865-University of Iowa, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael’s Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Hospital Research Institute, HL077887-University of Texas SW Medical Ctr/Dallas, HL077908-University of California San Diego) from the NHLBI in partnership with the National Institute of Neurological Disorders and Stroke (NINDS), U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defense Research and Development Canada, the Heart, Stroke Foundation of Canada and the AHA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NHLBI or the NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Robert M. Sutton, Email: suttonr@email.chop.edu, The Children's Hospital of Philadelphia, 34th St. and Civic Center Blvd., Philadelphia, PA 19104.
Erin Case, Email: ecase@uw.edu, Resuscitations Outcome Consortium, 1107 NE 45th St., Suite 505, Seattle, WA 98105-4680.
Siobhan P. Brown, Email: spes@uw.edu, Resuscitations Outcome Consortium, 1107 NE 45th St., Suite 505, Seattle, WA 98105-4680.
Dianne L. Atkins, Email: dianne-atkins@uiowa.edu, University of Iowa Carver College of Medicine, Stead family Department of Pediatrics, Iowa City, IA 52242.
Vinay M. Nadkarni, Email: nadkarni@email.chop.edu, The Children's Hospital of Philadelphia, 34th St. and Civic Center Blvd., Philadelphia, PA 19104.
Jonathan Kaltman, Email: kaltmanj@nhlbi.nih.gov, National Heart, Lung, and Blood Institute, 6701 Rockledge Dr., Bethesda, MD 20817.
Clifton W. Callaway, Email: callawaycw@upmc.edu, University of Pittsburgh, 400A Iroquois, 3600 Forbes Ave., Pittsburgh, PA 15260.
Ahamed H. Idris, Email: ahamed.idris@utsouthwestern.edu, aidris@sbcglobal.net, University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd., Dallas, TX 75390-8579.
Graham Nichol, Email: grahamnichol@icloud.com, Medical Director, Resuscitation Outcome Consortium Clinical Trial Center, University of Washington, Seattle, WA 98104.
Jamie Hutchison, Email: jamie.hutchison@sickkids.ca, The Hospital for Sick Children, 555 University Ave., Toronto, Ontario Canada, M5G 1X8.
Ian R. Drennan, Email: DrennanI@smh.ca, Rescu, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto 30 Bond St., Toronto, Ontario, Canada M5B 1W8.
Michael A Austin, Email: tassiemlm@yahoo.com.au, University of Ottawa The Ottawa, Hospital, Civic campus, 1053 Carling Ave., Ottawa, ON, Canada K1Y 4E9.
Mohamud Daya, Email: dayam@ohsu.edu, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd., Portland, OR, 97239-3098, Mailcode: CDW-EM.
Sheldon Cheskes, Email: Sheldon.Cheskes@sunnybrook.ca, Sunnybrook Center for Prehospital Medicine, 77 Browns Line, Toronto, Ontario M8W 3S2.
Jack Nuttall, Email: nuttallj@ohsu.edu, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd., Portland, OR 97239.
Heather Herren, Email: hherren@uw.edu, Resuscitations Outcome Consortium, 1107 NE 45th St., Suite 505, Seattle, WA 98105-4680.
James Christenson, Email: jim.christenson@ubc.ca, Professor and Head, Department of Emergency Medicine, University of British Columbia Faculty of Medicine, Room 3300 3rd Floor, 910 West 10th Ave., Vancouver, BC V5Z 1M9.
Douglas L Andrusiek, Email: dug.andrusiek@alumni.ubc.ca, Senior Lecturer, Discipline Lead School of Medical Sciences, Faculty of Health, Engineering and Science, Edith Cowan University, Building 19, Room 129d, 270 Joondalup Dr. Joondalup, Western Australia, Australia, 6023.
Christian Vaillancourt, Email: cvaillancourt@ohri.ca, University of Ottawa, The Ottawa Hospital Research Institute, The Ottawa Hospital, Civic campus, Room F649, 1053 Carling Ave., Ottawa, ON, Canada K1Y 4E9.
James J. Menegazzi, Email: menegazzijj@upmc.edu, University of Pittsburgh, 3600 Forbes Ave., Pittsburgh, PA 15261.
Thomas D. Rea, Email: rea123@u.washington.edu, University of Washington 206, 3rd Ave. South, Seattle, WA 98104.
Robert A. Berg, Email: bergra@email.chop.edu, The Children's Hospital of Philadelphia, 34th St. and Civic Center Blvd., Philadelphia, PA 19104.
References
- 1.Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The resuscitation outcomes consortium epistry-cardiac arrest. Circulation. 2009;119(11):1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kitamura T, Iwami T, Kawamura T, et al. Nationwide improvements in survival from out-of-hospital cardiac arrest in japan. Circulation. 2012;126(24):2834–2843. doi: 10.1161/CIRCULATIONAHA.112.109496. [DOI] [PubMed] [Google Scholar]
- 3.Donoghue AJ, Nadkarni V, Berg RA, et al. Out-of-hospital pediatric cardiac arrest: An epidemiologic review and assessment of current knowledge.[see comment] Ann Emerg Med. 2005;46(6):512–522. doi: 10.1016/j.annemergmed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 4.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Girotra S, Spertus JA, Li Y, et al. Survival trends in pediatric in-hospital cardiac arrests: An analysis from Get with the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6(1):42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaillancourt C, Everson-Stewart S, Christenson J, et al. The impact of increased chest compression fraction on return of spontaneous circulation for out-of-hospital cardiac arrest patients not in ventricular fibrillation. Resuscitation. 2011;82(12):1501–1507. doi: 10.1016/j.resuscitation.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheskes S, Schmicker RH, Christenson J, et al. Perishock pause: An independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation. 2011;124(1):58–66. doi: 10.1161/CIRCULATIONAHA.110.010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Idris AH, Guffey D, Aufderheide TP, et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125(24):3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stiell IG, Brown SP, Christenson J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: A prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 12.Sutton RM, Niles D, French B, et al. First quantitative analysis of cardiopulmonary resuscitation quality during in-hospital cardiac arrests of young children. Resuscitation. 2014;85(1):70–4. doi: 10.1016/j.resuscitation.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 14.Sutton RM, French B, Niles DE, et al. 2010 American Heart Association recommended compression depths during pediatric in-hospital resuscitations are associated with survival. Resuscitation. 2014;85(9):1179–84. doi: 10.1016/j.resuscitation.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stiell IG, Brown SP, Nichol G, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130(22):1962–70. doi: 10.1161/CIRCULATIONAHA.114.008671. [DOI] [PubMed] [Google Scholar]
- 16.Gazmuri RJ, Nadkarni VM, Nolan JP, et al. Scientific knowledge gaps and clinical research priorities for cardiopulmonary resuscitation and emergency cardiovascular care identified during the 2005 international consensus conference on ECC [corrected] and CPR science with treatment recommendations: A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian Resuscitation Council, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, and the New Zealand Resuscitation Council); the American Heart Association Emergency Cardiovascular Care Committee; the Stroke Council; and the Cardiovascular Nursing Council.".[erratum appears in circulation. 2007 nov 20;116(21):Following 2512] Circulation. 2007;116(21):2501–2512. doi: 10.1161/CIRCULATIONAHA.107.186228. [DOI] [PubMed] [Google Scholar]
- 17.Kleinman ME, de Caen AR, Chameides L, et al. Part 10: Pediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122(16 Suppl 2):S466–515. doi: 10.1161/CIRCULATIONAHA.110.971093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutton RM, Maltese MR, Niles D, et al. Quantitative analysis of chest compression interruptions during in-hospital resuscitation of older children and adolescents. Resuscitation. 2009;80(11):1259–1263. doi: 10.1016/j.resuscitation.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Sutton RM, Wolfe H, Nishisaki A, et al. Pushing harder, pushing faster, minimizing interruptions... but falling short of 2010 cardiopulmonary resuscitation targets during inhospital pediatric and adolescent resuscitation. Resuscitation. 2013;84(12):1680–1684. doi: 10.1016/j.resuscitation.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sutton RM, Niles D, Nysaether J, et al. Quantitative analysis of CPR quality during inhospital resuscitation of older children and adolescents. Pediatrics. 2009;124(2):494–499. doi: 10.1542/peds.2008-1930. [DOI] [PubMed] [Google Scholar]
- 21.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of emergency medical service systems participating in the resuscitation outcomes consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 22.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the resuscitation outcomes consortium epistry-cardiac arrest. Resuscitation. 2008;78(2):161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: Pediatric basic life support. Pediatrics. 2006;117(5):e989–1004. doi: 10.1542/peds.2006-0219. [DOI] [PubMed] [Google Scholar]
- 24.Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: Improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation. 2013;128(4):417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 25.Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. 1967;1:221–233. [Google Scholar]
- 26.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–830. [Google Scholar]
- 25.Wolfe HA, Zebuhr C, Topjian AA, et al. Interdisciplinary intensive care unit cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42(7):1688–95. doi: 10.1097/CCM.0000000000000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aufderheide TP, Lurie KG. Death by hyperventilation: A common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9 Suppl):S345–51. doi: 10.1097/01.ccm.0000134335.46859.09. [DOI] [PubMed] [Google Scholar]
- 29.Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109(16):1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 30.Zuercher M, Hilwig RW, Ranger-Moore J, et al. Leaning during chest compressions impairs cardiac output and left ventricular myocardial blood flow in piglet cardiac arrest. Crit Care Med. 2010;38(4):1141–1146. doi: 10.1097/CCM.0b013e3181ce1fe2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moler FW, Meert K, Donaldson AE, et al. In-hospital versus out-of-hospital pediatric cardiac arrest: A multicenter cohort study. Crit Care Med. 2009;37(7):2259–2267. doi: 10.1097/CCM.0b013e3181a00a6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295(1):50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.