Abstract
Objectives
Comparative studies examining the difference between empirically supported substance abuse treatments versus their culturally accommodated counterparts with participants from a single ethnic minority group are frequently called for in the literature but infrequently conducted in practice. This RCT was conducted to compare the efficacy of an empirically supported standard version of a group-based cognitive-behavioral treatment (S-CBT) to a culturally accommodated version (A-CBT) with a sample of Latino adolescents primarily recruited from the juvenile justice system. Development of the culturally accommodated treatment and testing was guided by the Cultural Accommodation Model for Substance Abuse Treatment (CAM-SAT).
Methods
Seventy Latino adolescents (mean age = 15.2; 90% male) were randomly assigned to one of two group-based treatment conditions (S-CBT = 36; A-CBT = 34) with assessments conducted at pretreatment, posttreatment, and 3-month follow-up. Longitudinal Poisson mixed models for count data were used to conduct the major analyses. The primary outcome variable in the analytic models was the number of days any substance was used (including alcohol, except tobacco) in the past 90 days. In addition, the variables ethnic identity, familism, and acculturation were included as cultural moderators in the analysis.
Results
Although both conditions produced significant decreases in substance use, the results did not support a time by treatment condition interaction; however, outcomes were moderated by ethnic identity and familism.
Conclusions
The findings are discussed with implications for research and practice within the context of providing culturally relevant treatment for Latino adolescents with substance use disorders.
Keywords: Latino, adolescents, substance abuse treatment, cultural accommodation, group-based CBT
Adolescent substance abuse is a serious public health concern. Data from the 2011 National Survey on Drug Use and Health estimates that 10% of adolescents in the United States between the ages of 12–17 are currently using illicit drugs and almost 7% could be diagnosed with a substance use disorder (SAMHSA, 2012). Alarmingly, the number of adolescents in need of treatment (1.8 million) far outweigh the number (150,000, or roughly 8%) who actually receive it, partly, due to the need for more effective engagement strategies (Ozechowski & Waldron, 2008; SAMHSA, 2010). When adolescents do receive treatment for substance abuse they are most likely to be placed in outpatient programs where individual and group formats are the most popular (SAMHSA, 2009). Among these youth, Latino adolescents are particularly in need of efficacious treatments because they have higher rates of substance use disorders (14%) compared to their White (12.7%) or African American (7%) counterparts (see CASA, 2011). They are also more likely to experience legal involvement, be referred for substance abuse treatment from the criminal justice system, and be mandated to treatment compared to White youth (see Shillington & Clapp, 2003). Latinos are one of the largest and fastest growing ethnic minority groups in the U.S. comprising more than 51 million people with a third of the population being under the age of 18 (Passel & D'Vera, 2008; Pew, 2011). This rapidly growing demographic combined with high national substance use and disorder rates indicate a pressing need to establish efficacious treatments for Latinos in general and adolescents, in particular.
Over the past 20 years there has been a continual push to establish empirical support for psychological treatments that address a range of mental health disorders for adults and adolescents (APA, 2006; Chambless & Hollen, 1998). With some exceptions (see Waldron & Turner, 2008), the efficacy of empirically supported treatments (ESTs) for mental health disorders has largely been established in randomized clinical trials (RCTs) with predominantly White samples (APA, 2006) whereas corresponding studies with ethnically diverse samples are generally lacking (Whaley & Davis, 2007). This lack of representation has been criticized from theoretical, ethical and practice-based viewpoints suggesting that ESTs validated with largely White samples cannot be assumed to meet the needs of ethnic minority individuals (see Hall, 2001; Lau, 2006; Szapocznik, Lopez, Prado, Schwartz, & Pantin, 2006). However, another side of the argument is that ESTs may have universal efficacy for all individuals and that lack of representation is due, in part, to the difficulty of recruiting and retaining ethnic minority participants in RCTs (Dumas, Rollock, Prinz, Hops, & Blechman, 1999; Miranda, Azocar, Organista, Munoz, & Lieberman, 1996). Regardless of the reasons, the lack of representation of ethnic minorities in RCTs greatly reduces our understanding of treatment efficacy for large proportions of the U.S. population and Latinos are a prime example.
Recent findings from meta-analytic studies suggest that ethnic minority individuals can benefit from culturally adapted treatments (Benish, Quintana, & Wampold, 2011; Griner & Smith, 2006). However, the majority of treatments cited in these meta-analyses was not ESTs and included a range of non-RCT study designs that generally compare a culturally adapted treatment to a mixture of other treatment conditions (e.g., no-treatment control, treatment-as-usual, a specifically defined treatment) without cultural modifications. Some meta-analytic studies have been focused more squarely on the efficacy of ESTs for ethnic minority adults and children with psychological disorders (see Huey & Polo, 2008; Huey, Tilley, Jones, & Smith, 2014; Miranda et al., 2005) and conclusions regarding the benefit provided by culturally adapted treatments beyond that of their standard version EST counterparts are not conclusive. While there is some support for the efficacy of ESTs in mitigating psychological disorders for Latino adolescents (see Rossello & Bernal, 1999; Szapocznik et al., 2006; Waldron & Turner, 2008) many argue that direct comparison studies (i.e., testing a standard versus culturally accommodated version of an EST) are needed in order to fully understand if and how ethnic minorities benefit from such treatments (Castro, Barrera, & Holleran Steiker, 2010; Huey & Polo, 2008; Huey et al., 2014; Whaley & Davis, 2007). For example, in a recent comprehensive review of the literature Huey et al., (2014) listed only 10 randomized comparison trials that have been conducted to test standard versus culturally adapted versions of the same treatment. It appears that, at present, the theoretical and conceptual proliferation of cultural adaptation models (see Bernal & Rodriguez, 2012; Castro et al., 2010) require testing in the context of direct comparison RCTs to determine if culturally adapted treatments provide benefit to ethnic minority individuals above that of receiving the standard or non-adapted version of the same treatment (see Huey et al., 2014).
To address the limitations described above, the Cultural Accommodation Model for Substance Abuse Treatment (CAM-SAT; Burrow-Sánchez, Martinez, Hops, & Wrona, 2011) was developed as a framework for guiding the development and testing of culturally accommodated versions of ESTs and is well grounded in the behavioral treatment development literature (i.e., Rounsaville, Carroll, & Onken, 2001). The overall goal of the CAM-SAT is to directly compare a standard version of an EST against its culturally accommodated equivalent with participants from the same ethnic minority group. Direct comparison studies assist in determining if the inclusion of cultural components adds any benefit for ethnic minority participants above and beyond generic versions of a treatment (Huey et al., 2014) . Further, this model is based on a theoretical assumption that treatments with greater cultural relevance for participants will produce more benefit compared to those treatments lacking in relevance (Castro et al., 2010; Frankish, Lovatto, & Poureslami, 2007). It is important to state that other researchers have demonstrated efficacy for culturally accommodated substance abuse interventions with samples of Latino adolescents (e.g., Santisteban, Mena, & McCabe, 2011; Szapocznik, Kurtines, Foote, Perez-Vidal, & Hervis, 1983; Szapocznik et al., 2006) but this statement must be tempered with the understanding that there is a general lack of research comparing standard versions of empirically supported treatments against their culturally accommodated counterparts (see Benish et al., 2011; Griner & Smith, 2006; Huey et al., 2014).
The variables of acculturation, ethnic identity, and familism were integrated in the present study due to their cultural relevancy for Latino adolescents experiencing substance abuse problems (see Burrow-Sánchez et al., 2011; Castro et al., 2010). The process of acculturation occurs when one racial/ethnic group interacts with a second dominant group that results in cultural and psychological changes in the first group and adopting some of the standards, behaviors, and attitudes of the dominant group (Berry, 2006). Acculturation for ethnic minority individuals is a complex bi-dimensional process that involves the orientation one has toward dominant (e.g., Anglo) and non-dominant cultures (e.g., Latino) while living in the context of the dominant culture (Berry, 1980; Berry, Phinney, Sam, & Vedder, 2006). It is well known that the acculturation process is a major developmental influence in the lives of Latinos and has been linked to positive and negative mental health outcomes for adolescents (for a review see Lawton & Gerdes, 2014). In relation to substance use, a number of studies have found that higher levels of acculturation (e.g., Anglo orientation) is associated with higher rates of substance use for Latino adolescents (De La Rosa, Vega, & Radisch, 2000; Ebin et al., 2001; Vega & Gil, 1998, 1999; Vega, Gil, & Wagner, 1998); however, others have noted the opposite conclusion (Zamboanga, Schwartz, Jarvis, & Van Tyne, 2009) or a lack of association (Miller, 2011). Currently, more research is needed to understand how the role of acculturation in the lives of Latino adolescents influences their response to substance abuse treatment.
The level of identification one has with his/her own ethnic group, ethnic identity, is a second cultural variable that has been linked to Latino adolescent substance use. Ethnic identity is defined as a bi-dimensional construct composed of the commitment and exploration a person has for identifying with and seeking knowledge of his/her own ethnic group (Marcia, 1980; Phinney & Ong, 2007). In general, a stronger sense of ethnic identity is associated with higher levels of well-being (e.g., self-esteem, coping) and lower levels of substance use (for reviews see Felix-Ortiz & Newcomb, 1995; Phinney & Ong, 2007; Umana-Taylor, 2011). While generally considered a protective factor there is also some evidence to suggest that a higher level of ethnic identity awareness may indeed act as a risk factor for Latinos by increasing the salience of environmental stressors they experience such as discrimination (Smith & Silva, 2010). What is lacking, however, is research on the possible roles that ethnic identity and its underlying constructs may play for Latino adolescents in the context of substance abuse treatment.
A third variable, familism, encompasses the influential role that the family plays in the lives of Latino adolescents and more specifically, imparting cultural values of strong and loyal attachment to family members (Sabogal, Marin, Otero-Sabogal, & Marin, 1987). These cultural values are thought to be transferred from parents to children and in Latino families with high levels of familism the use of substances is generally not condoned (Vega, 1990). The levels of familism in Latino families are likely influenced by the quality of parenting behaviors which have direct impact on adolescent substance use. For example, more supportive parenting behaviors are related to lower levels of substance use and other mental health problems for Latino adolescents (Castro & Alarcon, 2002; German, Gonzales, & Dumka, 2009; Gonzales, Deardorff, Fromoso, Barr, & Barrera, 2006). On the other hand, there is also evidence to suggest that poor parenting practices in Latino families, especially parent-child conflict, can be risk factors for adolescent substance use and delinquent behavior (McQueen, Gertz, & Bray, 2003; Pasch et al., 2006). Regardless, whether risk or protective factor, familism in Latino families may be an indicator of the influence that parents continue to have on their youth's development; as such, it may play an important role in Latino adolescents' response to substance abuse treatment and requires further investigation. One possible conclusion from the brief review above is that substance abuse treatments for Latino adolescents may be more culturally relevant when they are integrated with variables such as acculturation, ethnic identity and familism (see Burrow-Sánchez et al., 2011; Castro & Alarcon, 2002; Castro et al., 2010).
In the present study, 70 Latino adolescents were randomly assigned to one of two group-based empirically supported substance abuse treatments; that is, a standard version (Kadden et al., 1992) or its culturally accommodated counterpart (Burrow-Sánchez et al., 2011). In the context of conducting a substance abuse treatment study for adolescents it is important to note that the use of a no-treatment, wait-list, or attention-placebo condition is not common due to the ethical concerns of withholding treatment from youth who need it (see Brody & Waldron, 2000; Waldron & Turner, 2008). First, we hypothesized an overall time by group treatment effect that predicted adolescents in the culturally accommodated condition would report less days of substance use at posttreatment and 3-month follow-up compared to those in the standard condition. The rationale for this hypothesis was based on the assumption that a more culturally relevant treatment would produce better outcomes for Latino adolescents compared to a less culturally relevant treatment (see Castro et al., 2010; Hall, 2001; Whaley & Davis, 2007). Second, we hypothesized that the number of days of substance use reported by Latino adolescents in both treatment conditions at posttreatment and 3-month follow-up would be moderated by the variables of acculturation, ethnic identity, and familism; more specifically, adolescents with cultural characteristics congruent with their assigned treatment condition would demonstrate better outcomes (i.e., less days of substance use) compared to those who were incongruent (see Burrow-Sánchez et al., 2011; Castro & Alarcon, 2002; Frankish et al., 2007). This second hypothesis was based on a more refined assumption of cultural relevance in that treatments may be more or less relevant for certain subgroups of Latino adolescents based on the individual cultural characteristics of the participants (Castro et al., 2010; Frankish et al., 2007).
Method
Demographics, Recruitment, and Study Flow
Adolescents were included in the study if they were between 13–18 years of age, provided parental/adolescent consent/assent, met DSM-IV-TR (American Psychiatric Association, 2000) diagnostic criteria for alcohol/drug abuse or dependence measured via the Structured Clinical Interview for DSM-IV (First, Gibbon, Spitzer, & Williams, 2002) and self-identified as Latino/Hispanic. Adolescents were excluded if they were outside the 13–18 age range, spoke only Spanish, did not have parental consent, were not willing to provide assent, required a higher level of care than provided by the study treatment, had completed substance abuse treatment within the 90 days prior to referral or did not identify as Latino/Hispanic. The sample was comprised of 70 Latino adolescents who ranged in age from 13–18 (M = 15.20, SD = 1.24), were mostly male (90%), and primarily born in the U.S. (61.40%). The majority of their parents were born in Mexico (74.3% of mothers; 81.4% of fathers), had a mean age of 41.3 (SD = 6.29) and reported annual household incomes or $25,000 or less (75.7%; see Table 1). The majority of parents that completed measures at the pretreatment assessment were mothers (81.4%) followed by smaller percentages of both parents (11.4%) and fathers (7.1%). Most adolescents were referred by probation officers (63%) or case managers (33%) from the juvenile justice system in a mid-sized Mountain West city in the U.S. and the remainder (4%) came from parents or treatment providers; 74% of adolescents in the sample were mandated to treatment at the time of referral. This study was conducted between the years 2010–2012 and all procedures were approved by the Institutional Review Board at the institution of the first author.
Table 1.
Participant Demographics and Study Variables
| Variable | S-CBT (n = 36) | A-CBT (n = 34) |
|---|---|---|
| Adolescent Demographics | ||
| Age | 15.31 (1.28) | 15.09 (1.19) |
| Grade | 9.72 (1.32) | 9.71 (1.27) |
| Male | 88.9% | 91.2% |
| Language Spoken at Home: | ||
| Spanish | 58%* | 85% |
| English | 28%* | 9% |
| Both | 14% | 6% |
| Birth Country: | ||
| U.S. | 69% | 53% |
| Mexico | 28% | 44% |
| Othera | 3% | 3% |
| Parent Demographics | ||
| Mother Birth Country: | ||
| Mexico | 67% | 82% |
| U.S. | 25% | 9% |
| Othera | 8% | 9% |
| Father Birth Country: | ||
| Mexico | 78% | 85% |
| U.S. | 6% | 3% |
| Othera | 16% | 12% |
| Annual Family Income: | ||
| 25,000 or less | 72% | 71% |
| 25,000 – 45,000 | 20% | 23% |
| 45,000 or more | 8% | 6% |
| Did not answer | 0% | 3% |
| Moderators at Baseline | ||
| Ethnic Identity | ||
| COM | 3.93 (0.97) | 3.89 (1.13) |
| EXP | 3.04 (0.96) | 2.66 (0.90) |
| Familism | ||
| Adolescent | 2.97 (0.42) | 3.06 (0.44) |
| Parent | 3.60 (0.68) | 3.68 (0.77) |
| Acculturation | ||
| MOS | 3.30 (0.61) | 3.49 (0.77) |
| AOS | 3.40 (0.46) | 3.39 (0.53) |
| DSM Diagnosis at Baseline | ||
| Substance Abuseb | 44%* | 71% |
| Alcohol | 3% | -- |
| Marijuana | 31% | 50% |
| 2 or more drugsc | 11% | 21% |
| Substance Dependenced | 56%* | 29% |
| Alcohol | 3% | 3% |
| Marijuana | 36% | 24% |
| 2 or more drugsc | 17% | 3% |
| Drug Use at Baselinee | ||
| Alcohol | 4.17 (7.39) | 4.50 (8.35) |
| Marijuana | 22.03 (23.65) | 18.35 (22.57) |
| Tobacco | 13.61 (27.28) | 7.26 (17.85) |
| Otherf | 1.16 (0.17) | 1.61 (0.19) |
Note. Cell entries are either means (SD) or a percentage of the subsample indicated. S-CBT = Standard Cognitive-Behavioral Treatment condition; A-CBT = Accommodated Cognitive-Behavioral Treatment condition. ARSMA-II = Acculturation Rating Scale for Mexican Americans, Version 2; MEIM = Multi Ethnic Identity Measure. FS = Familism Scale, mean family scores are presented calculated by averaging adolescent and parent scores.
Other = South American country.
Primary abuse diagnosis,
Abuse or dependence diagnosis is for two or more drugs - most commonly alcohol and marijuana in this sample,
Primary dependence diagnosis;
Mean (SD) number of days used in past 90,
Other = hallucinogens, cocaine, opiates, inhalants, prescription meds, etc.,
Indicates significant different (p<.05, Chi-square test) between the two values in the corresponding columns.
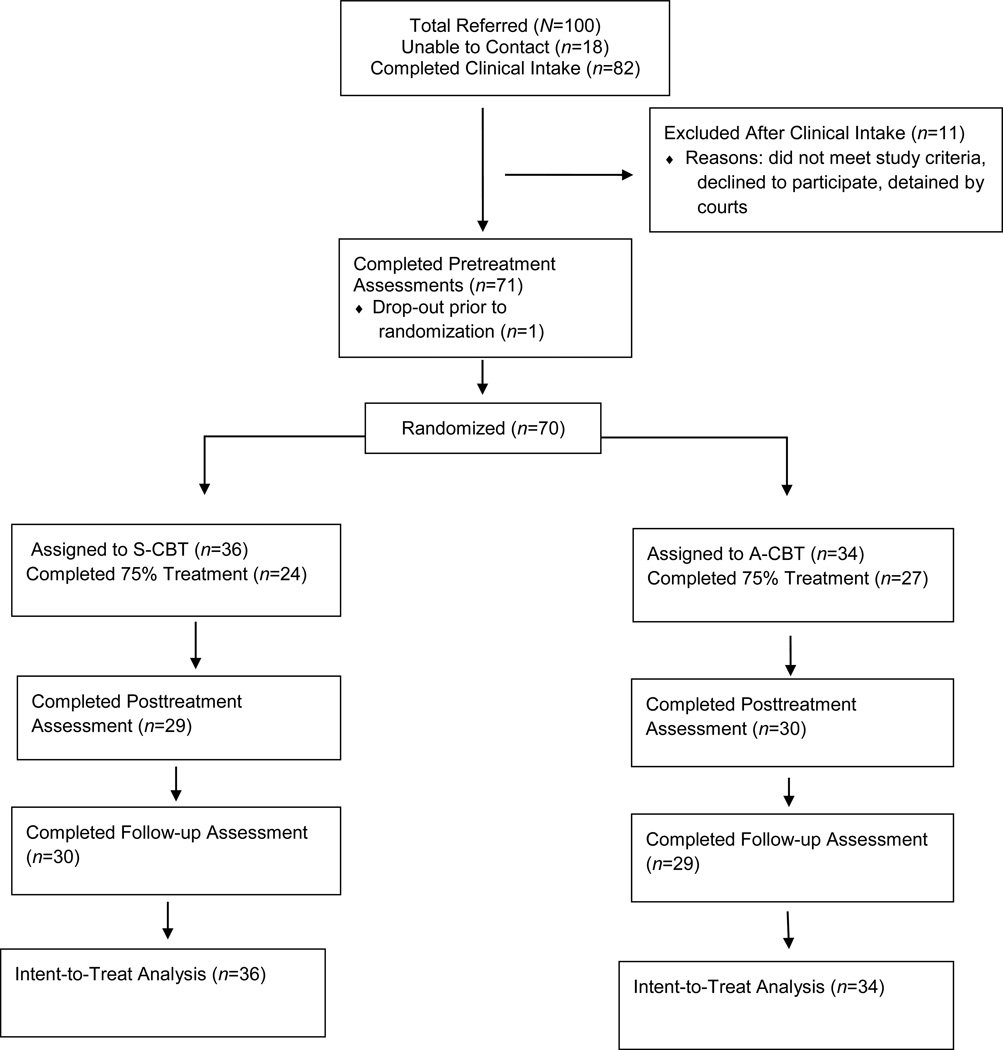
At the start of each treatment round, approximately 16–18 adolescents were randomized into one of two conditions: Standard Cognitive Behavioral Treatment (S-CBT; Kadden et al., 1992) or Accommodated Cognitive Behavioral Treatment (A-CBT; Burrow-Sánchez et al., 2011; see Figure 1 for participant flow). A small-group restricted randomization strategy was used to ensure that treatment conditions had relatively equal numbers in each arm (Shadish, Cook, & Campbell, 2002); that is, 10 participants were randomized at a time until the groups were filled for each treatment round. Random number sequences were generated by the principal investigator using the web-based Research Randomizer (Urbaniak & Plous, 2013) and provided to the program coordinator as needed. The program coordinator used the random number sequence to assign participants to a treatment condition after the pretreatment assessment was completed but participants were not explicitly told which condition (i.e., standard or accommodated) they would receive. Two therapists were primarily assigned to a condition by coin toss and then counterbalanced by condition thereafter. Five treatment rounds were conducted that produced a total of 10 treatment groups. The majority of adolescents completed treatment (73%; S-CBT=67%, A-CBT=79%), defined as attending 9 out of 12 (75%) treatment sessions, and completed posttreatment (83%; S-CBT=81%, A-CBT=88%) and 3-month follow-up assessments (84%; S-CBT=83%, A-CBT=85%). Treatment completion and assessment rates were not significantly different by condition. Across the study, mean attendance rates for the S-CBT and A-CBT conditions were 10.42 (SD = 1.14) and 10.59 (SD = 1.05), respectively.
Figure 1.
Flowchart for Randomized Clinical Trial
Note. S-CBT = Standard Cognitive-Behavioral Treatment, A-CBT = Accommodated Cognitive-Behavioral Treatment
Administration and Measures
Trained bilingual undergraduate and graduate students served as research assistants (RAs) and administered measures (available in English and Spanish) to adolescent and parent participants in their preferred language at each study time-point. The RAs were not informed of participant treatment assignment. Ninety-seven percent of adolescents preferred verbal interactions and completion of the measures in English whereas the majority of parents (83%) preferred Spanish. The Familism Scale is the only measure listed below completed by parents.
Primary Variable of Interest
Timeline Follow Back (TLFB)
The TLFB (Sobell & Sobell, 1992) is a semi-structured interview that has been used extensively with adolescents (Dennis, Funk, Godley, Godley, & Waldron, 2004; Sobell & Sobell, 2003). It utilizes a calendar format and establishes relevant life markers to help individuals remember their history and patterns of substance use over a specific period of time. In the present study, the TLFB was used to assess the dependent variable which was the number of days substances (including alcohol; excluding tobacco) were used in the 90-day period prior to each assessment point.
Secondary Variables of Interest
Acculturation Rating Scale for Mexican Americans-II (ARSMA-II)
The ARSMA-II is designed to measure acculturation levels in participants of Mexican American descent (Cuéllar, Arnold, & Maldonado, 1995). Participants rated their preferences, attitudes, and behaviors regarding acculturation on a “1 – Not at All” to “5 – Extremely Often or Almost Always” scale. The measure has demonstrated good reliability and strong construct and discriminant validity in research with Mexican American samples (Cuéllar et al., 1995). Values from the 13-item Anglo Oriented Subscale and the 17-item Mexican Oriented Subscale were scored separately in accordance with Cuéllar et al., (1995) and a bi-dimensional view of acculturation (Berry, 2006). Internal consistency was α = .66 and α = .85 for AOS and MOS subscales, respectively.
The Multi Ethnic Identity Measure (MEIM)
The MEIM is a widely used measure of ethnic identity for adolescents (Phinney, 1992) and a 12-item modified version was administered that has been validated for Latino adolescents with substance use disorders (Burrow-Sánchez, 2014). Participants rated their attitudes and behaviors regarding ethnic identity on a “1 – Disagree” to “5 – Agree” scale. As suggested by Phinney and Ong (2007) the measure was scored by reducing it to two 3-item subscales: a commitment scale that measures a sense of personal affiliation to an ethnic group and an exploration scale that measures behavior related to seeking information about an ethnic group. Scores from the individual items were averaged to produce two subscale scores for each participant. Internal consistency for the current sample was α = .78 for the commitment subscale and α = .65 for the exploration subscale.
Familism Scale (FS)
The FS is a 14-item instrument used to measure the construct of familism based on the factors of obligations, perceived support , and family as referents (Sabogal et al., 1987) . This measure was administered to adolescents and parents. Items were rated on a scale ranging from “1 – Very Much in Disagreement” to “5 – Very Much in Agreement.” Scores from individual items were averaged to obtain a total score for adolescents and parents separately. For parents, this measure was largely completed by mothers (81.4%) followed by both parents (11.4%) and then fathers (7.1%). When both parents completed the measure their individual scores were averaged to produce one score that was used in the final analysis. Internal consistency for adolescents and parents were α = .73 and α = .85, respectively.
Treatment Conditions and Delivery
Treatment for both conditions was delivered in group format via 12 weekly 1 ½-hour sessions. The Standard Cognitive Behavioral Treatment (S-CBT) manual developed for this study (see Burrow-Sánchez, 2013b) was modeled after the Cognitive-Behavioral Coping Skills Therapy Manual (see Kadden et al., 1992) that was evaluated in Project Match for adults with alcoholism and later adapted for adolescents (see Dennis, Godley, et al., 2004; Kaminer, Burleson, & Goldberger, 2002; Waldron, Slesnick, Brody, Turner, & Peterson, 2001). The S-CBT manual was modified through a cultural accommodation process (see Burrow-Sánchez et al., 2011) resulting in a second manual titled Accommodated Cognitive-Behavioral Treatment (A-CBT; Burrow-Sánchez, 2013a). The A-CBT manual was modified by adjusting aspects of treatment content and delivery to increase cultural relevancy for Latino adolescents. Specific changes to the treatment manual included developing a new module (i.e., Ethnic Identity and Adjustment) based on cognitive-behavioral principles that specifically addressed the ways participants could develop strengths and reduce perceived negativities in relation to their identity as a Latino adolescent. This module also included discussion of related issues such as acculturation and acculturative stress. Further, all of the modules in the A-CBT condition were revised to increase cultural relevance by infusing content such as Spanish names in examples, role-plays relevant for Latino adolescents (e.g., problem-solving in the context of a racist environment) and opportunities to discuss frequently encountered stressors (e.g., translating for a parent, dealing with discrimination). Treatment delivery for parents in the A-CBT condition was modified by holding a Family Introduction Meeting immediately prior to the beginning of the first group and promoting regular (i.e., every third session) phone and mail contact between the therapist and parents. Parents in the S-CBT condition did not receive these modified elements of treatment delivery. Adolescents in both treatment conditions received attendance reminder calls. All modifications were designed to be congruent with the theoretical and structural elements of cognitive-behavioral treatment and specific details of the cultural accommodation process for the A-CBT can be found in Burrow-Sánchez et al., (2011).
The two therapists in this study were doctoral students in counseling and school psychology, respectively, bilingual (English/Spanish), had prior clinical experience working with Latino families, and received 20 hours of training in the clinical delivery of CBT with adolescents by a licensed psychologist with experience in this area. Detailed treatment manuals and corresponding session-by-session adherence checklists were provided to therapists. All group sessions were videotaped. Therapists and the supervising licensed psychologist reviewed the videos independently and rated therapist adherence using a seven-item checklist that ranged from “1-Not Accomplished” to “7-Completely Accomplished.” Ratings were compared and used as a basis for discussion during weekly supervision meetings. Supervisor adherence ratings were calculated (mean, SD, range) for sessions 3, 6, and 9 in each condition (i.e., 25% of total sessions) and results suggested that adherence was acceptable in both treatment arms; S-CBT = 5.61 (SD=0.55; range 5–7) and A-CBT = 5.77 (SD=0.50; range 5–7).
Analytical Plan
A longitudinal generalized linear mixed model approach was used to guide the analysis for the primary and secondary variables of interest in this study (Hedeker & Gibbons, 2006; Stroup, 2013). The dependent variable (DV) was calculated from TLFB measure as the total number of days any drug was used (including alcohol; excluding tobacco) in the past 90 days. The DV was a count variable that indicated the number of times a behavior occurred within a specific time period (Coxe, West, & Aiken, 2009). The recommended analytic strategy for the analysis of count data, in general, and TLFB count data, in particular is a generalized model that can account for the skew in the distribution of the variable (see Atkins, Baldwin, Zheng, Gallop, & Neighbors, 2013; Coxe et al., 2009). Generalized linear models can account for the dependence between participant scores in repeated measures data and estimate parameters when there is missing participant data at certain time-points which is a common issue in longitudinal studies; thus, all available participant data can be included in the model and this approach is most commonly known as an intent-to-treat analysis (see Shadish et al., 2002). In the generalized linear family of models a Poisson approach is commonly employed to analyze count data. An assumption of the Poisson model is that the mean and variance of the distribution are the same value but this condition is rarely met in practice and therefore, we included a standard error correction in all our models to relax this assumption (see Coxe et al., 2009; Stroup, 2013).
Results
An unconditional random intercept Poisson model with the terms Time (coded 0, 1, 2) and Quadratic (coded 0, 1, 4) and the dependent variable TLFB was used as the baseline model. This model produced significant Time (F[1, 127.6] = 9.97, p = .002) and Quadratic (F[1, 127.6] = 5.51, p = .02) terms. Estimates were significant for between-subject (σ2 = 0.30, Wald Z = 3.07, p = .001) and residual (σ2 = 11.71, Wald Z = 7.85, p < .0001) variances. A conditional random intercept Poisson model was conducted that included covariates for Age (grand mean centered) and Diagnosis (0=Substance Abuse, 1=Substance Dependence) in addition to terms for Time, Quad, treatment condition (Group), and time by treatment condition (Time*Group). Baseline drug use did not differ by treatment condition as tested by a Mann-Whitney U test, U(70) = 571.50, p = .634, and was not included as a covariate in the model. This second model produced significant Age (F[1,68.44] = 9.41, p = .003), Diagnosis (F[1,67.39] = 8.56, p = .005), Time (F[1, 132.7] = 9.32, p < .003) and Quad (F[1, 130.5] = 4.97, p < .03) effects but Time*Group was not significant (F[1, 181.9] = 0.19, p = .66). These results suggest that after controlling for age and diagnostic category adolescents in both treatment conditions reported decreases in the number of days of substance use across time (β = −.89) but the trend contained a quadratic element (β = 0.32).
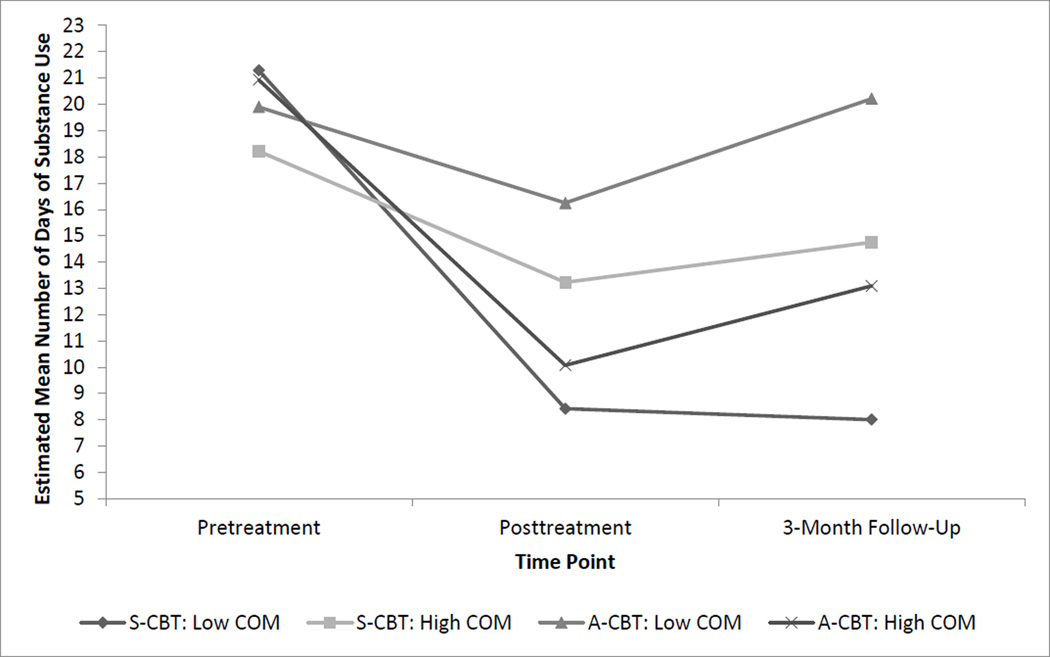
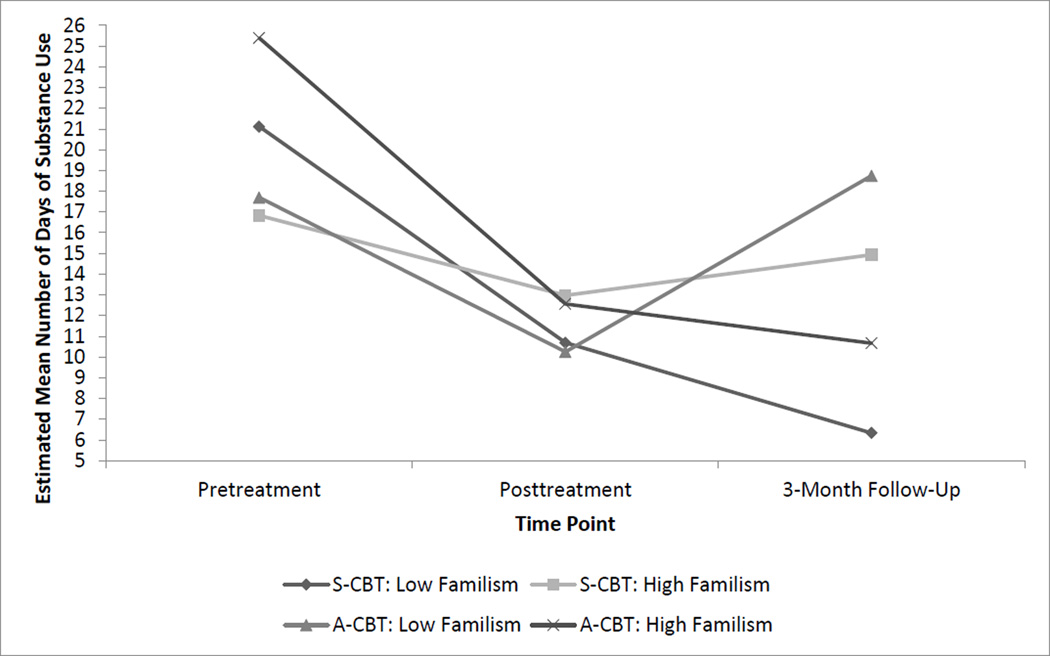
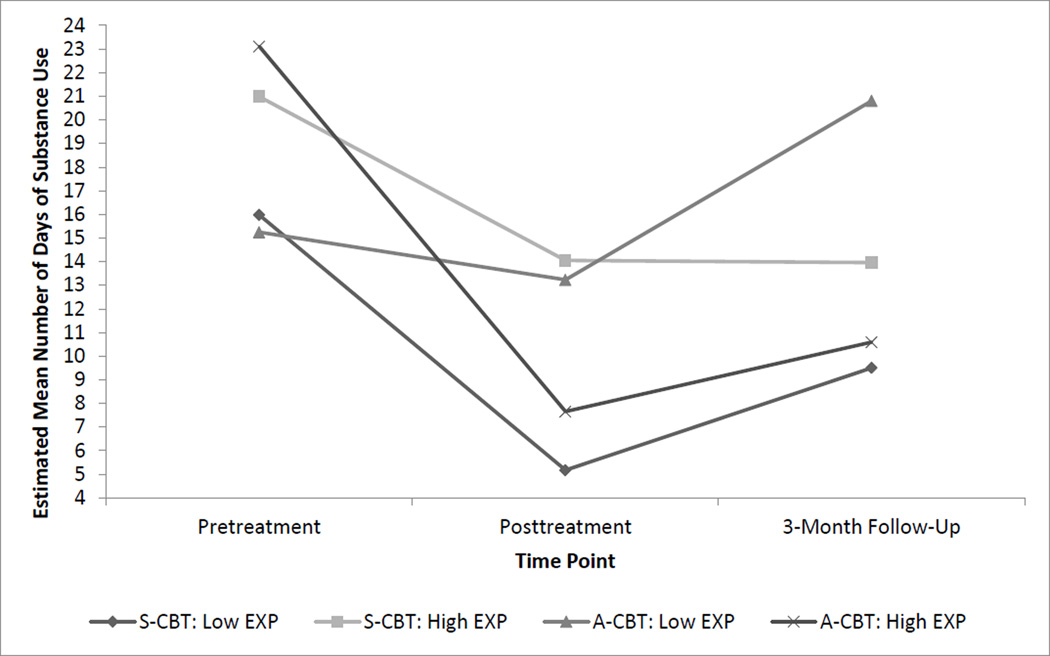
Conditional Poisson models were developed for the cultural moderators with the goal of determining whether the predictors could explain the variability found in TLFB participant scores. The general structure for each model included the following terms: Age, Diagnosis, Time, Quad, Group, Moderator Variable (MV), Time by Group, Time by MV, Group by MV, and Time by Group by MV. The covariate Age and moderator variables were grand mean centered to ease interpretation of the results (Hedeker & Gibbons, 2006) and the Diagnosis variable was coded as described above. Moderator variables were coded using the acronym for the sub-scale of the measure with the exception of the familism measure which was coded based on respondent: commitment = COM, exploration = EXP, familism adolescent score = FS_A, familism parent score = FS_P, Mexican oriented scale = MOS, and Anglo oriented scale = AOS. Random intercept models indicated significant three-way interactions for the COM (β = −0.29, F[1,128.9] = 3.89, p = .05), EXP (β = −0.35, F[1,128.6] = 5.01, p = .03) and FSP (β = −0.68, F[1,136] = 9.49, p = .003) moderator variables (see Tables 2–3). Poisson models produce regression coefficients that represent the predicted logarithm of counts of the DV (see Coxe et al., 2009). In the context of the current study, coefficients are interpreted as the predicted change in the logarithm of counts for the TLFB variable for a 1-unit change in the predictor; however, this metric is not easily interpretable because it is not in the form of the original count variable (i.e., number of days of drug use). In order to place the metric on the scale of the count variable the Poisson coefficients can be exponentiated but doing so causes problems with interpretation. For example, the exponentiated intercept represents the number of days of drug use as measured by the TLFB when all other predictors are zero but the remaining exponentiated coefficients in the model represent the multiplicative change in the TLFB for a 1-unit change in the predictor (Coxe et al., 2009). In order to interpret the interactions in the original count variable with exponentiated values Coxe et al., (2009) recommend plotting the predicted trends for each group at different values of the X variable. Therefore, to interpret the interactions in the current study we dichotomized the moderator variables into < 0 = low and > 0 = high categories and then calculated least square estimated means for the groups at each study time-point. The estimated means were then exponentiated and plotted for groups at each of the three study time-points (see Figures 2–4). Interpretation of the graph for Figure 2 suggests that adolescents with lower commitment in the standard condition displayed the lowest mean number of days of substance use at posttreatment and the 3-month assessment followed by those with higher commitment in the accommodated condition. Figure 3 suggests differences, although not significant in the model, in pretreatment substance use levels across groups but a closer inspection of the plot indicates that adolescents with lower exploration in the standard condition displayed the lowest mean number of days of substance use at the 3-month assessment followed by those with higher exploration in the accommodated condition. Figure 4 also suggests differences, although not significant in the model, in pretreatment substance use levels across groups however the trends are similar to the prior graphs in that adolescents with parents who had lower levels of familism in the standard condition displayed the lowest mean number of days of substance use at the 3-month assessment followed by those with higher parental familism in the accommodated condition. Overall, findings provide support for the commitment and exploration sub-factors of ethnic identity and parental familism as cultural moderators of substance abuse treatment outcome for Latino adolescents in this study.
Table 2.
Random Intercept Models for Substance Use with Ethnic Identity Subfactors as Moderators
| Effect | Estimate | SE | Exp (E)a | 95% Confidence Interval for Estimate |
|
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Commitment Subfactor | |||||
| Fixed effects | |||||
| Intercept | 2.78*** | 0.18 | 16.04 | 2.43 | 3.12 |
| Age | 0.21** | 0.07 | 1.23 | 0.07 | 0.34 |
| Dxb | 0.51** | 0.18 | 1.67 | 0.16 | 0.86 |
| Timec | −0.90** | 0.30 | 0.41 | −1.48 | −0.31 |
| Quadd | 0.32* | 0.15 | 1.38 | 0.03 | 0.61 |
| Groupe | 0.05 | 0.20 | 1.05 | −0.35 | 0.45 |
| COMf | −0.02 | 0.14 | 0.98 | −0.29 | 0.25 |
| Time*Group | 0.05 | 0.15 | 1.05 | −0.24 | 0.35 |
| Time*COM | 0.17 | 0.11 | 1.19 | −0.05 | 0.39 |
| Group*COM | 0.12 | 0.20 | 1.13 | −0.27 | 0.52 |
| Time*Group*COM | −0.29t | 0.15 | 0.75 | −0.59 | 0.0009 |
| Random effects | |||||
| Intercept variance | 0.17* | 0.08 | 0.08 | 0.57 | |
| Residual | 11.87*** | 1.52 | 9.37 | 15.53 | |
| Exploration Subfactor | |||||
| Fixed effects | |||||
| Intercept | 2.68*** | 0.18 | 14.51 | 2.32 | 3.03 |
| Age | 0.20** | 0.07 | 1.22 | 0.06 | 0.34 |
| Dx | 0.58** | 0.17 | 1.79 | 0.24 | 0.93 |
| Time | −0.85** | 0.29 | 0.43 | −1.43 | −0.28 |
| Quad | 0.30* | 0.14 | 1.35 | 0.02 | 0.58 |
| Group | 0.15 | 0.20 | 1.16 | −0.25 | 0.55 |
| EXPg | 0.24 | 0.14 | 1.28 | −0.04 | 0.53 |
| Time*Group | −0.05 | 0.16 | 0.95 | −0.36 | 0.26 |
| Time*EXP | 0.02 | 0.10 | 1.02 | −0.19 | 0.23 |
| Group*EXP | −0.08 | 0.22 | 0.92 | −0.51 | 0.35 |
| Time*Group*EXP | −0.35* | 0.16 | 0.70 | −0.66 | −0.04 |
| Random effects | |||||
| Intercept variance | 0.16* | 0.08 | 0.07 | 0.55 | |
| Residual | 11.25*** | 1.44 | 8.88 | 14.71 | |
p=.05
p<.05
p<.01
p<.0001
Note.
Note. Exponentiation of the estimate;
compared to a diagnosis of substance abuse;
Time = assessment time-point in study;
Quad = quadratic;
Group = treatment group;
COM = commitment subfactor of ethnic identity;
EXP = exploration subfactor of ethnic identity.
Table 3.
Random Intercept Model for Substance Use with Parental Familism as Moderator
| Effect | Estimate | SE | Exp (E)a | 95% Confidence Interval for Estimate |
|
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Fixed effects | |||||
| Intercept | 2.71*** | 0.18 | 15.09 | 2.36 | 3.07 |
| Age | 0.20** | 0.07 | 1.22 | 0.06 | 0.34 |
| Dxb | 0.54** | 0.18 | 1.72 | 0.19 | 0.90 |
| Timec | −0.81** | 0.29 | 0.44 | −1.38 | −0.25 |
| Quadd | 0.30* | 0.14 | 1.35 | 0.02 | 0.58 |
| Groupe | 0.05 | 0.21 | 1.05 | −0.36 | 0.46 |
| FS_Pf | −0.33 | 0.19 | 0.72 | −0.70 | 0.04 |
| Time*Group | 0.02 | 0.14 | 1.02 | −0.27 | 0.31 |
| Time*FS_P | 0.33* | 0.15 | 1.38 | 0.03 | 0.62 |
| Group*FS_P | 0.75** | 0.28 | 2.13 | 0.20 | 1.31 |
| Time*Group*FS_P | −0.63** | 0.21 | 0.53 | −1.04 | −0.22 |
| Random effects | |||||
| Intercept variance | 0.20** | 0.08 | 0.10 | 0.55 | |
| Residual | 11.07*** | 1.42 | 8.73 | 14.48 | |
p<.05
p<.01
p<.0001
Note.
Exponentiation of the estimate;
compared to a diagnosis of substance abuse;
Time = assessment time-point in study;
Quad = quadratic;
Group = treatment group;
FS_P = familism score for parent.
Figure 2.
Plot of Commitment Moderator
Note. S-CBT = Standard Cognitive-Behavioral Treatment; A-CBT= Accommodated Cognitive-Behavioral Treatment; COM = Commitment subfactor of ethnic identity.
Figure 4.
Plot of Familism Moderator for Parent Scores
Note. S-CBT = Standard Cognitive-Behavioral Treatment; A-CBT = Accommodated Cognitive-Behavioral Treatment. Pretreatment mean scores between groups are not significantly different.
Figure 3.
Plot of Exploration Moderator
Note. S-CBT = Standard Cognitive-Behavioral Treatment; A-CBT = Accommodated Cognitive-Behavioral Treatment; EXP = Exploration subfactor of ethnic identity; Pretreatment mean scores between groups are not significantly different.
Discussion
We evaluated the comparative efficacy of standard and culturally accommodated versions of a group-based EST with a sample of juvenile justice involved Latino adolescents. Our first hypothesis was not supported as we did not find a significant time by group interaction. Instead, adolescents in both treatment conditions decreased the number of days of substance use across study time-points. However, consistent with our second hypothesis treatment outcome was moderated by ethnic identity and parental familism. These findings constitute new contributions to understanding how ethnic minority adolescents may respond to a standard EST when compared to its culturally accommodated version. Prior research has indicated that ethnic minorities can benefit from treatment that includes cultural adaptations (Benish et al., 2011; Griner & Smith, 2006); however, our study is one of the few to directly compare two versions of an EST (i.e., standard vs. accommodated) in a randomized trial with a sample from the same ethnic minority group.
Our first hypothesis that A-CBT would lead to lower days of substance use for adolescents than S-CBT was not supported and thus does not provide evidence that the culturally accommodated EST in the current study would provide benefit above and beyond that of its standard version. While the lack of treatment differences in our study is consistent with other direct comparison studies (e.g., Burrow-Sánchez & Wrona, 2012; Huey & Pan, 2006; Lee et al., 2013; McCabe & Yeh, 2009) we also consider potential reasons for this finding. First, any difference between treatments is less likely to be found when comparing two active treatment conditions in the same study (Shadish et al., 2002; Wampold, 2001) and this could help explain our findings from a methodological standpoint. Second, the cultural accommodation threshold may not have been reached for the A-CBT in which to produce differential outcomes compared to the S-CBT. In fact, the point at which cultural accommodations produce differential treatment outcomes or additional benefit beyond non-accommodated treatments is not well understood at present (see Huey et al., 2014). Finally, the current study included outcomes at three months posttreatment but this length of time may not have been sufficient in duration for which to observe differential treatment effects for cognitive-behavioral interventions. For example, there is research to suggest that CBT may have delayed effects that are more likely to be observed at distal posttreatment time-points (see Carroll, 1996; Carroll & Onkin, 2005). Some could argue that the lack of differences between treatments in the current study suggest that culturally accommodated ESTs are not needed for Latino adolescents with substance use disorders but we believe, similar to other researchers (see Castro et al., 2010; Huey et al., 2014), that this perspective may be premature because results from more direct comparison studies are needed prior to drawing firm conclusions on this issue.
We did find support for our second hypothesis—cultural moderators can influence treatment outcome for Latino adolescents. Specifically, adolescents with lower commitment to their ethnic identity in the standard condition reported the lowest mean number of days of substance use at posttreatment and the 3-month assessment followed by those with higher commitment to their ethnic identity in the accommodated condition. This same trend was found for adolescents with lower exploration of their ethnic identity in the standard condition and for those with higher exploration of their ethnic identity in the accommodated condition. These findings suggest that for Latino adolescents with low commitment and exploration of their ethnic identity the standard treatment condition may have been a better fit because it more closely paralleled the larger dominant group; whereas for Latino adolescents with higher commitment and exploration the accommodated condition may have provided a better cultural fit. Taken together, these findings suggest that subgroups of Latino adolescents may experience better outcomes when the EST is culturally congruent with their level of commitment and exploration for ethnic identity.
A similar moderator effect was found for substance use outcomes in relation to parent familism scores. Specifically, adolescents in the standard condition with parents who indicated lower familism reported the lowest mean number of days of substance use at the 3-month assessment followed by adolescents in the accommodated condition with parents who indicated higher familism. These findings are consistent with the idea that culturally congruent ESTs may be important for subgroups of Latino adolescents but also suggest that the family plays an influential role in this relationship. In particular, the level of familism as perceived by a parent may be an important consideration when assessing the cultural fit of a treatment for Latino adolescents. It also underscores the point that Latino families may continue to exert considerable influence on their children even during the adolescent years (Umaña-Taylor & Guimond, 2010).
Findings from the moderator analysis help us to understand the differential benefits of the culturally accommodated EST for the adolescent subgroups. It appears that Latino adolescents in the accommodated condition with higher levels of ethnic identity - commitment and exploration - as well as with parents who indicated higher familism reported less mean number of days of substance use at the 3-month assessments compared to their peers in the same treatment condition but with less affiliation for each of the moderators. More specifically, across these three subgroups adolescents reported a 42% decrease in the mean number of days that substances were used at the last study time-point compared to their less affiliated counterparts in the same treatment condition. Further, the percentage of adolescents in each of the three subgroups that reported less drug use represented, on average, over half (57%) of the total 34 youth who were randomized to the accommodated treatment condition (i.e., commitment = 65%; exploration = 47%; parental familism = 59%). Overall, these findings suggest that Latino adolescents with higher affiliation in the areas of ethnic identity and parental familism may receive more benefit from an accommodated EST. In addition, the percentage of adolescents that may benefit from a culturally accommodated EST (57%) and the amount of benefit they may receive (42% decrease in substance use days) does not appear trivial by any means. A potential implication of these findings is that the benefit provided by culturally accommodated ESTs may need to be considered within the context of the cultural characteristics of the individuals receiving them.
The current study has important implications for research and practice that should be considered within the provision of culturally accommodated treatments for ethnic minority individuals. There are a number of ESTs that have demonstrated efficacy with adolescent participants from different ethnic minority groups (see Huey & Jones, 2013; Huey & Polo, 2008; Waldron & Turner, 2008) but many of these studies have used no-treatment or treatment-as-usual as comparison conditions (see Huey et al., 2014). These types of study designs can provide information on the overall efficacy of a culturally accommodated treatment but they do not provide information regarding the added benefit (or lack thereof) that comes from the inclusion of cultural elements; rather, this type of information is more likely to be provided through direct comparison studies. We also recognize that results from direct comparison studies will not appear overnight in the literature but will take significant time to produce. In the interim, practitioners have many ESTs at their disposal that can be used with Latino adolescents and other ethnic minority clients for treating substance abuse and other mental health disorders. However, the degree of cultural relevance that an intervention may have for an adolescent from a diverse background should be considered by practitioners when assigning such youth to treatments (Castro et al., 2010; Frankish et al., 2007). As the results of this study suggest, there may be identifiable pretreatment characteristics, such as ethnic identity, that can assist therapists in placing youth in more culturally congruent treatments in order to maximize cultural fit and potentially impact the overall benefit they receive. In clinical practice, thorough pretreatment assessments are generally conducted with youth prior to placing them in substance abuse treatment. Perhaps the additional measurement of relevant cultural characteristics should be considered as part of this assessment process. Of course, the treatment-moderator findings found in the current study require further investigation and replication but yet are important for practitioners to consider while waiting for more findings to come to light. It is our hope that as more findings from direct comparison studies are published they will further inform clinical practice and provide more opportunity for ethnic minority adolescents to receive treatments that provide maximum benefit.
Certain limitations need to be considered in the context of the current study. First, the majority of adolescents were male, juvenile justice involved, more highly acculturated, and of Mexican American descent. Generalizing findings from the current study to females and adolescents from other Latino subgroups (e.g., Puerto Rican, Cuban) with varying acculturation levels should be the focus of future research. It should be noted, however, that participants recruited from juvenile justice are predominantly male and thus, the gender composition of our sample is similar to most studies of adolescent substance abuse treatment (see Waldron & Turner, 2008). Second, the lack of data on adolescent co-occurring disorders, collateral information on substance use (e.g., urine analysis, parent report) and analysis of outcomes across drug types are limitations. We suggest that these limitations be addressed in future research due to the high rates of adolescent co-morbidity, the need to validate self-report substance use data and understand outcomes for different drug types. Finally, the sample size for the current study was modest and thus limited the statistical power to test for moderation and within-group nesting effects. It is recommended that future adolescent treatment studies recruit larger numbers of ethnic minority adolescents.
This direct comparison treatment study was embedded within the larger context of a cultural accommodation model for substance abuse treatment (CAM-SAT). The CAM-SAT guided the development of a culturally accommodated treatment (Burrow-Sánchez et al., 2011), its initial evaluation in a small randomized pilot study (Burrow-Sánchez & Wrona, 2012) and now the current study that reports findings from a larger randomized clinical trial. The present study is one of a small group in the literature to employ a research design comparing a standard version of an empirically supported treatment and its culturally accommodated counterpart with participants from the same ethnic minority background. This type of comparative research design needs to be replicated with additional samples of ethnic minority participants and we hope that the present study serves as an example for other researchers conducting similar randomized clinical trials.
Acknowledgements
This research was supported by Award Number K23DA019914 from the National Institute on Drug Abuse awarded to the first author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
The authors wish to thank all members of the VIDA Research Team at the University of Utah and mentors for the K23 award who provided guidance in conducting this research.
Contributor Information
Jason J. Burrow-Sánchez, University of Utah.
Takuya Minami, UMASS – Boston.
Hyman Hops, Oregon Research Institute.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders - Text Revision. 4th ed. Washington, D.C: Author; 2000. [Google Scholar]
- APA. Presidential task force on evidence-based practice. American Psychologist. 2006;61:271–285. doi: 10.1037/0003-066X.61.4.271. [DOI] [PubMed] [Google Scholar]
- Atkins DC, Baldwin SA, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychology of Addictive Behaviors. 2013;27(1):166–177. doi: 10.1037/a0029508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: A direct-comparison meta-analysis. Journal of Counseling Psychology. 2011;58(3):279–289. doi: 10.1037/a0023626. [DOI] [PubMed] [Google Scholar]
- Bernal G, Rodriguez MMD. Cultural adaptations: Tools for evidence-based practice with diverse populations. Washington DC: American Psychological Association; 2012. [Google Scholar]
- Berry JW. Acculturation as varieties of adaptation. In: Padilla A, editor. Acculturation: Theory, models and some new findings. Boulder, CO: Westview; 1980. pp. 9–25. [Google Scholar]
- Berry JW. Acculturation: A conceptual overview. In: Bornstein MH, Cite LR, editors. Acculturation and Parent-Child Relationships: Measurement and Development. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2006. pp. 13–30. [Google Scholar]
- Berry JW, Phinney J, Sam D, Vedder P. Immigrant youth in cultural transitiion: Acculturation, identity and adaptation across national contexts. Mahwah, NJ: Erlbaum; 2006. [Google Scholar]
- Brody JL, Waldron HB. Ethical issues in research on the treatment of adolescent substance abuse disorders. Addictive Behaviors. 2000;25:217–228. doi: 10.1016/s0306-4603(99)00041-6. [DOI] [PubMed] [Google Scholar]
- Burrow-Sánchez JJ. A-CBT: Cognitive-Behavioral Treatment for Adolescent Substance Use Disorders: Culturally Accommodated Version - Unpublished Manual. Salt Lake City: University of Utah; 2013a. [Google Scholar]
- Burrow-Sánchez JJ. S-CBT: Cognitive Behavioral Treatment for Adolescent Substance Use Disorders: Standard Version - Unpublished Manual. Salt Lake City: University of Utah; 2013b. [Google Scholar]
- Burrow-Sánchez JJ. Measuring ethnic identity in Latino adolescents with substance use disorders. Substance Use & Misuse. 2014;49:982–986. doi: 10.3109/10826084.2013.794839. [DOI] [PubMed] [Google Scholar]
- Burrow-Sánchez JJ, Martinez CR, Hops H, Wrona M. Cultural accommodation of substance abuse treatment for Latino adolescents. Journal of Ethnicity and Substance Abuse. 2011;10(3):202–225. doi: 10.1080/15332640.2011.600194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrow-Sánchez JJ, Wrona M. Comparing culturally accommodated versus standard group CBT for Latino adolescents with substance use disorders: A pilot study. Cultural Diversity and Ethnic Minority Psychology. 2012;18(4):373–383. doi: 10.1037/a0029439. [DOI] [PubMed] [Google Scholar]
- Carroll KM. Relapse prevention as a psychosocial treatment: A review of controlled clinical trials. Experimental and Clinical Psychopharmacology. 1996;(4):46–54. [Google Scholar]
- Carroll KM, Onkin LS. Behavioral therapies for drug abuse. American Journal of Psychiatry. 2005;(162):1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASA. Adolescent substance use: America's #1 public health problem. New York, NY: Columbia University; 2011. p. 419. [Google Scholar]
- Castro FG, Alarcon EH. Integrating cultural variables into drug abuse prevention and treatment with racial/ethnic minorities. Journal of Drug Issues. 2002;32:783–810. [Google Scholar]
- Castro FG, Barrera MJ, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annual Review of Clinical Psychology. 2010;6:213–239. doi: 10.1146/annurev-clinpsy-033109-132032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambless DL, Hollen SD. Defining empirically supported therapies. Journal of Clinical and Consulting Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Coxe S, West SG, Aiken L. The analysis of count data: A gentle introduction to Poisson regression and its alternatives. Journal of Personality Assessment. 2009;31(2):121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- Cuéllar I, Arnold B, Maldonado R. Acculturation Rating Scale for Mexican Americans II: A revision fo the original ARSMA scale. Hispanic Journal of Behavioral Sciences. 1995;17(3):275–304. [Google Scholar]
- De La Rosa M, Vega R, Radisch MA. The role of acculturation in the substance abuse behavior of African-American and Latino adolescents: Advances, issues, and recommendations. Journal of Psychoactive Drugs. 2000;32(1):33–42. doi: 10.1080/02791072.2000.10400210. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron HB. Cross-validation of the alchohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. Addiction. 2004;99(2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Funk R. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Dumas JE, Rollock D, Prinz RJ, Hops H, Blechman EA. Cultural sensitivity: Problems and solutions in applied and preventive intervention. Applied & Preventive Psychology. 1999;8:175–196. [Google Scholar]
- Ebin VJ, Sneed CD, Morisky DE, Rotheram-Borus MJ, Magnusson AM, Malotte CK. Acculturaion and the interrelationships between problem and helath-promoting behaviors among Latino adolescents. Journal of Adolescent Health. 2001;28:62–72. doi: 10.1016/s1054-139x(00)00162-2. [DOI] [PubMed] [Google Scholar]
- Felix-Ortiz M, Newcomb MD. Cultural identity and drug use among Latino and Latina adolescents. In: Botvin GJ, Schinke SP, Orlandi MA, editors. Drug abuse prevention with multiethnic youth. Thousand Oaks: Sage Publications; 1995. pp. 147–165. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. User's guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders - Research Version. New York, NY: Biometrics Research Department. New York State Psychiatric Institute; 2002. [Google Scholar]
- Frankish CJ, Lovatto CY, Poureslami I. Models, theories, and principles of health promotion. In: Kline MV, Huff RM, editors. Health promotion in multicultural popluations: A handbook for practitioners and students. 2nd ed. Los Angeles, CA: Sage; 2007. [Google Scholar]
- German M, Gonzales NA, Dumka L. Familism values as a protective factor for Mexican-origin adolescents exposed to deviant peers. Journal of Early Adolescence. 2009;29(1):16–42. doi: 10.1177/0272431608324475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales NA, Deardorff J, Fromoso D, Barr A, Barrera M. Family mediators of the relation between acculturation and adolescent mental health. Family Relations. 2006;55:318–330. [Google Scholar]
- Griner D, Smith T. Culturally adapted mental health interventions: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training. 2006;43(4):531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- Hall GCN. Psychotherapy research with ethnic minorities: Empirical, ethical, and conceptual issues. Journal of Consulting and Clinical Psychology. 2001;69:502–510. doi: 10.1037//0022-006x.69.3.502. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, N.J: John Wiley & Sons; 2006. [Google Scholar]
- Huey SJ, Jones EO. Improving treatment engagement and psychotherapy outcomes for culturally diverse youth and families. In: Paniagua F, Yamada A, editors. Handbook of Multicultural Mental Health. Burlington, MA: Elsevier; 2013. pp. 427–444. [Google Scholar]
- Huey SJ, Pan D. Culture responsive one session treatment for phobic asian americans: A pilot study. Psychotherapy: Theory, Research, Practice, Training. 2006;43(4):549–554. doi: 10.1037/0033-3204.43.4.549. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Polo AJ. Evidence-based psychological treatments for ethnic minority youth. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):262–301. doi: 10.1080/15374410701820174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huey SJ, Tilley JL, Jones EO, Smith C. The contribution of cultural competence to evidence-based care for ethnically diverse popluations. Annual Review of Clinical Psychology. 2014;10:305–338. doi: 10.1146/annurev-clinpsy-032813-153729. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Hester R. Cognitive-behavioral coping skills therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. Vol. 3. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Kaminer Y, Burleson JA, Goldberger R. Cognitive-behavioral coping skills and psychoeducation therapies for adolescent substance abuse. Journal of Nervous and Mental Disease. 2002;190(11):737–745. doi: 10.1097/00005053-200211000-00003. [DOI] [PubMed] [Google Scholar]
- Lau A. Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice. 2006;13(4):295–310. [Google Scholar]
- Lawton KE, Gerdes AC. Acculturation and Latino adolescent mental health: Integration of individual, environmental, and family influences. Clinical Child and Family Psychological Review, online prepublication copy. 2014 doi: 10.1007/s10567-014-0168-0. [DOI] [PubMed] [Google Scholar]
- Lee CS, Lopez SR, Colby SM, Rohsenow D, Hernandez L, Borrelli B, Caetana R. Culturally adapted motivational interviewng for Latino heavy drinkers: Results form a randomized clinical trial. Journal of Ethnicity and Substance Abuse. 2013;12(4):356–373. doi: 10.1080/15332640.2013.836730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcia J. Identity in Adolescence. In: Adelson J, editor. Handbook of adolescent psychology. New York: Wiley; 1980. pp. 159–187. [Google Scholar]
- McCabe K, Yeh M. Parent-child interaction therapy for Mexican Americans: A randomized clinical trial. Journal of Clinical Child and Adolescent Psychology. 2009;38(5):753–759. doi: 10.1080/15374410903103544. [DOI] [PubMed] [Google Scholar]
- McQueen A, Gertz JG, Bray JH. Acculturation, substance use, and deviant behavior: Examining separation and family conflict as mediators. Child Development. 2003;74:1737–1750. doi: 10.1046/j.1467-8624.2003.00635.x. [DOI] [PubMed] [Google Scholar]
- Miller HV. Acculturation, social context, and drug use: Findings from a sample of Hispanic adolescents. Journal of Criminal Justice. 2011;36:93–105. [Google Scholar]
- Miranda J, Azocar F, Organista KC, Munoz RF, Lieberman A. Recruiting and retaining low-income Latinos in psychotherapy research. Journal of Consulting and Clinical Psychology. 1996;64:868–874. doi: 10.1037//0022-006x.64.5.868. [DOI] [PubMed] [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang WC, LaFromboise T. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 2005;1:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozechowski TJ, Waldron HB. Assertive outreach strategies for adolescent substance abuse. Journal of Behavioral Health Services & Research. 2008;37(1):40–63. doi: 10.1007/s11414-008-9136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch LA, Deardorff J, Tschann JM, Flores E, Pennila C, Pantoja P. Acculturation, parent-adolescent conflict, and adolescent adjustment in Mexican American families. Family Processes. 2006;45:75–86. doi: 10.1111/j.1545-5300.2006.00081.x. [DOI] [PubMed] [Google Scholar]
- Passel JS, D'Vera C. U.S. Population Projections: 2005–2050. 2008 Retrieved from www.pewhispanic.org.
- Pew. Pew Research Hispanic Center Tabulations of the 2011 American Community Survey. 2011 Retrieved 3/5/2014, from www.pewhispanic.org.
- Phinney JS. The Multigroup Ethnic Identity Measure: A new scale for use with diverse groups. Journal of Adolescent Research. 1992;7(2):156–176. [Google Scholar]
- Phinney JS, Ong AD. Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology. 2007;54(3):271–281. [Google Scholar]
- Rossello J, Bernal G. The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology. 1999;67:734–745. doi: 10.1037//0022-006x.67.5.734. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage 1. Clinical Psychology: Science and Practice. 2001;18(2):133–142. [Google Scholar]
- Sabogal F, Marin G, Otero-Sabogal R, Marin BV. Hispanic familism and acculturation: What changes and what doesn't. Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]
- SAMHSA. 2009 State Profile - United States, National Survey of Substance Abuse Treatment Services (N-SSATS) 2009 Retrieved from http://www.oas.samhsa.gov/dasis.htm#Reports.
- SAMHSA. NSDUH Series H-38A. Rockville, MD: Substance Abuse and Mental Health Services Administration - Office of Applied Statistics; 2010. Results from the 2009 National Survey on Drug Use and Health: Volume I Summary of Findings. [Google Scholar]
- SAMHSA. NSDUH Series H-144. Rockville, MD: Substance Abuse and Mental Health Services Administration - Office of Applied Statistics; 2012. Results from the 2011 National Survey on Drug Use and Health: Summary of National Findings. [Google Scholar]
- Santisteban DA, Mena MP, McCabe BE. Preliminary results for an Adaptive Family Treatment for Drug Abuse. Journal of Family Psychology. 2011;25(4):610–614. doi: 10.1037/a0024016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin Company; 2002. [Google Scholar]
- Shillington AM, Clapp JD. Adolescents in public substance abuse treatment programs: The impacts of sex and race on referrals and outcomes. Journal of Child and Adolescent Substance Abuse. 2003;12:69–91. [Google Scholar]
- Smith TB, Silva L. Ethnic identity and personal well-being of people of color: A meta-analysis. Journal of Counseling Psychology. 2010;58:42–60. doi: 10.1037/a0021528. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back. In: Litten R, Allen J, editors. Measuring alcohol consumption. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB, editors. Alcohol consumption measures. 2nd ed. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Stroup WW. Generalized Linear Mixed Models: Modern Concepts, Methods and Applications. Boca Raton, FL: Taylor & Francis Group; 2013. [Google Scholar]
- Szapocznik J, Kurtines WM, Foote FH, Perez-Vidal A, Hervis O. Conjoint versus one-person family therapy: Some evidence for the effectiveness of conducting family therapy through one person. Journal of Consulting and Clinical Psychology. 1983;51(6):889–899. doi: 10.1037//0022-006x.51.6.889. [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Lopez B, Prado G, Schwartz SJ, Pantin H. Outpatient drug abuse treatment for Hispanic adolescents. Drug and Alcohol Dependence. 2006;84:54–63. doi: 10.1016/j.drugalcdep.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Umana-Taylor AJ. Ethnic identity. In: Schwartz SJ, Luyckx K, Vignoles VL, editors. Handbook of identity theory and research. New York, NY: Springer; 2011. pp. 791–810. [Google Scholar]
- Umaña-Taylor AJ, Guimond A. A longitudinal examination of parenting behaviors and preceived discrimination predicting Latino adolescents' ethnic identity. Developmental Psychology. 2010;(46):636–650. doi: 10.1037/a0019376. [DOI] [PubMed] [Google Scholar]
- Urbaniak GC, Plous S. Research Randomizer (Version 4.0) 2013 Retrieved from http://www.randomizer.org/
- Vega WA. Hispanic families in the 1980's: A decade of research. Journal of Marriage and the Family. 1990;52:1015–1024. [Google Scholar]
- Vega WA, Gil AG. Drug Use and Ethnicity in Early Adolescence. New York: Plenum Press; 1998. [Google Scholar]
- Vega WA, Gil AG. A model for explaining drug use behavior among Hispanic adolescents. In: Rosa MDL, Segal B, Lopez R, editors. Conducting Drug Abuse Research with Minority Populations: Advances and Issues. The Haworth Press, Inc; 1999. pp. 57–74. [Google Scholar]
- Vega WA, Gil AG, Wagner E. Cultural adjustment and Hispanic adolescent drug use. In: Vega WA, Gil AG, editors. Drug Use and Ethnicity in Early Adolescence. New York: Plenum Press; 1998. pp. 125–148. [Google Scholar]
- Waldron HB, Slesnick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4 month and 7 month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Wampold BE. The Great Psychotherapy Debate: Models, Methods and Findings. Mahwah, NJ: Lawrence Earlbaum Associates Inc; 2001. [Google Scholar]
- Whaley AL, Davis KE. Cultural competence and evidence-based practice in mental health services. American Psychologist. 2007;62(6):563–574. doi: 10.1037/0003-066X.62.6.563. [DOI] [PubMed] [Google Scholar]
- Zamboanga BL, Schwartz SJ, Jarvis LH, Van Tyne K. Acculturation and substance use among Hispanic early adolescents: Investigating the mediating role of acculturative stress and self-esteem. Journal of Primary Prevention. 2009;30:315–333. doi: 10.1007/s10935-009-0182-z. [DOI] [PubMed] [Google Scholar]