Abstract
Radial tunnel syndrome is a disease which we should consider it in elbow and forearm pains. It is diagnosed with lateral elbow and dorsal forearm pain may radiate to the wrist and dorsum of the fingers. The disease is more prevalent in women with the age of 30 to 50 years old. It occurs by intermittent compression on the radial nerve from the radial head to the inferior border of the supinator muscle, without obvious extensor muscle weakness. Compression could happen in five different sites but the arcade of Frose is the most common area that radial nerve is compressed. To diagnosis radial tunnel syndrome, clinical examination is more important than paraclinic tests such as electrodiagnsic test and imaging studies. The exact site of the pain which can more specified by rule of nine test and weakness of the third finger and wrist extension are valuable physical exams to diagnosis. MRI studies my show muscle edema or atrophy along the distribution of the posterior interosseous nerve. Although non-surgical treatments such as rest, NSAIDs, injections and physiotherapy do not believe to have permanent relief, but it is justify undergoing them before surgery. Surgery could diminish pain and symptoms in 67 to 93 percents of patients completely.
Keywords: Diagnosis, Radial Tunnel Syndrome, Treatment
Introduction
Intermittent compression of the radial nerve through the radial tunnel is thought to be the pathological basis for radial tunnel syndrome (RTS). The condition is not associated with extensor muscle weakness and due to the fact that the diagnosis is mostly clinical so, the existence of RTS remains controversial (1). However, those authors who support the diagnosis have identified a number of potential etiologies including compression of the nerve due to the bands of fascia, radial recurrent vessels, edge of supinator and rarely a haemangioma, lipoma, dislocated head of radius, inflamed synovium or accessory muscles (1-3).
Radial Tunnel Syndrome controversy
Those clinicians who do not support the diagnosis note that the only constant symptom is pain. Yet if thought to be a compressive neuropathy of the posterior interosseouus nerve, why would the EMG universally be negative. To refute this, the fact that motor nerves can provide pain stimuli and unmyelinated and small myelinated fibers are not generally assessed with the EMG. Moreover, the existence of define anatomic space, definitive tenderness in anterior and distal of elbow and the fact motor nerve can provide pain stimuli support the PIN as the responsible factor in RTS.
History
The presentations and proposed pathologies of RTS have had multiple nomenclatures over time. Michelle and Krueger first described the RTS in 1954 as “radial pronator syndrome” (4). In 1972, Roles and Maudsley reported an association between pain and compression of the posterior interosseous nerve (PIN) which they referred to as “resistant tennis elbow with a nerve entrapment” (3, 5). The terminology, “Radial Tunnel Syndrome” was used by Eversmann in 1993 to describe the effect of the nerve compression by the supinator brevis muscle (6). Subsequent articles adapted the nomenclature of RTS to describe the physiological symptoms due to the compression of the radial nerve in the radial tunnel (in the elbow) by varying sources such as the bands of fascia, radial recurrent vessels, and the inferior edge of the supinator muscle (2, 7). Table 1 summarizes the historical development in the understanding of RTS as defined today.
Table 1.
Historical developments in the definition of Radial Tunnel Syndrome (RTS)
| Year | Researcher | Event |
|---|---|---|
| 1955 | Michelle & Krueger | Referred to Radial Tunnel Syndrome (RTS) as ‘radial pronator syndrome’ |
| 1972 | Roles & Maudsley | Identified the association between pain and compression of the PIN, and termed the condition Radial Tunnel Syndrome or resistant tennis elbow. The patients were treated via surgical decompression of the nerve |
| 1979 | Lister et al | Identified the pain with resisted middle finger extension as a pathognomonic sign of Radial Tunnel Syndrome |
Anatomy
The radial nerve originates from the posterior cord of the brachial plexus to innervate the triceps muscle, extensors of the wrist, and the extensors of the fingers and thumb (8). The nerve divides in to the superficial and deep branches immediately proximal to the superior border of superficial layer of supinator muscle (the arcade of Frohse). PIN also carries unmyelinated (group IV) afferent fibers from wrist capsule and small myelinated (group IIA) afferent fibers from muscle along its distribution. Group IV unmyelinated fibers from muscles have been associated with nociception and pain which may explain the patient sensory complaints in pure PIN engagement.
The anatomic radial tunnel extends from the radial head to the inferior border of the supinator muscle (2). the boundaries is formed by the supinator, extensor carpi radialis longus, extensor carpi radialis brevis, and brachioradialis muscles (9). Table 2 and Figure 1 demonstrate the potential compression sites of the radial nerve.
Table 2.
Potential radial nerve compression sites that may lead to RTS
| Order | Location | Basis for compression | Sensory involvement |
|---|---|---|---|
| 1 | Lateral elbow joint in radial head | Osteoarthritis or fibrous bands anterior to the radiocapitellar joint or synovitis of the radiocapitellar joint. | May engage sensory area |
| 2 | Leash of Henry | An arcade of anastomosing branches of the recurrent radial artery at the radial neck | May engage sensory area |
| 3 | Fibrous edge of the ECRB | The leading (medial proximal) edge of the extensor carpi radialis brevis | May engage sensory area |
| 4 | The arcade of Frohse | The proximal edge of the superficial layer of supinator muscle | Does not engage sensory area |
| 5 | Distal edge of radial tunnel | The distal edge of supinator muscle | Does not engage sensory area |
Figure 1.
Leash of Henry and arcade of Frohse are two possible sites of radial nerve compression.
Prevalence
The annual incidence rate of the posterior interosseous nerve (PIN) compression is estimated 0.03% while the rate for superficial radial nerve (SRN) compression is 0.003% (10, 11). In comparison, the most common neuropathy, carpal tunnel syndrome, has an annual incidence between 0.1% and 0.35% in the general population (11, 12).
The entrapment of the radial nerve and its deep branch can occur at five different sites within the radial tunnel [Table 2] and most have identified it to be due to the arcade of Frohse [Figure 1] (13). The reported female to male occurrence ratios vary from 1:1 to 6:1 (1, 2). The patients are typically between 30 to 50 years old at the time of diagnoses of RTS (1-3, 14, 15). RTS usually involving the dominant side. In the study by Roles et al, 35 patients out of the 36 with the diagnosis of RTS were right hand dominant (3). Bilateral involvement in a RTS patient is rare. Sarhadi et al only report one bilateral RTS out of 26 patients (7). History of previous surgical procedure is a common finding in RTS. Bolster et al. reported 5 out of 12 patients with the diagnosis of RTS had previous surgical intervention on the ipsilateral upper extremity for various pathologies such as shoulder instability, trigger finger, osteoarthritic finger joint, and carpal tunnel syndrome (1). In the study performed by Dean et al, 7 out of 35 patients with the diagnosis of RTS had previous surgical treatments for carpal tunnel syndrome, carpal tunnel syndrome with cuncurrent cubital tunnel syndrome, or DeQuervain’s tenosynovitis on the same side (15). Other contributing factors of RTS occurrence may include trauma and heavy manual labor (13, 16). 13 out of 35 patients in Dean`s study had history of elbow or forearm trauma (15). Roquelaure et al., proposed an increased risk for RTS in factory workers in their study with patients who perform effort intensive forearm extensions in pronation or supination (16).
Sign and symptoms
Determining the exact location of the pain in the forearm, is the primary step in evaluating for RTS. The main clinical feature of RTS is a localized tenderness over the radial nerve 5 cm distal to the lateral epicondyle. Patients typically report aggravated pain at nights that may interfere with sleeping. The pain can also become more severe when increased traction is applied to the nerve by extending the elbow, pronating the forearm, or flexing the wrist. Two accepted clinical tests to confirm the diagnosis include exacerbation of the pain with resisted supination with the other being increased pain in the proximal radial forearm and over the radial tunnel when the wrist is hyperextended against resistance (1, 17). Studies have concluded the pain elicited with resisted middle finger extension as a pathognomonic sign in diagnosing of RTS (1). However, other studies noted the pain is rarely induced during resisted extension of the middle finger (17). Electromyography (EMG) and nerve conduction velocity (NCV) studies in patients with RTS are typically negative (18, 19).
The Rule of Nine [Figure 2] is another valuable test in diagnosis of RTS. Developed by Loh et al, the Rule of Nine is utilized when evaluating patients with non-specific elbow and proximal forearm pain (20). The test is administered by subdividing the anterior, proximal forearm just distal to the elbow crease in to nine circular regions arranged in a 3×3 grid. The grid is about the size of a half dollar [Figure 3]. Patients are asked to determine each place as painful, uncomfortable, or nothing when pressure is applied to the individual areas. Three medial pressure circles are the control areas and expected to be free of pain and discomfort. Tenderness on the two proximal circles at the lateral column indicates radial nerve irritation. The posterior interosseous branch of radial nerve lies more distally and between the two heads of supinator muscle. Thus, pressure on the third distal circle would not irritate the radial nerve and it could be used as a control site for RTS in addition to the medial column (8, 20). In the middle column, the two distal circles overlie the route of median nerve, and pain and tenderness in this area indicates a high level of median nerve irritation (8).
Figure 2.

The rule of nine test: Volar side of left proximal forearm, distal to elbow crease is divided to nine pressure points in three columns. Tenderness over two proximal lateral circles (red circles) indicates radial nerve irritation while tenderness over pressure points of 5 and 6 (yellow circles) indicates proximal median nerve irritation. Three medial points are control area.
Figure 3.
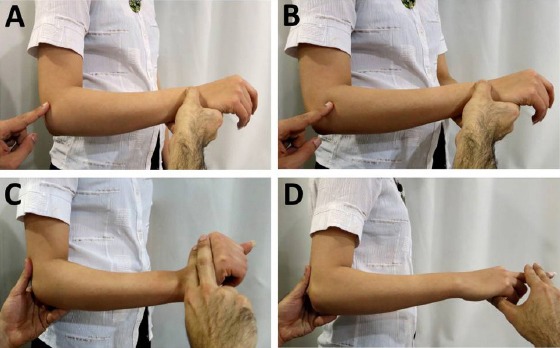
Physical tests for Radial Tunnel Syndrome. A and B: Different sites of pain in RTS and lateral epicondylitis. Tenderness in lateral epicondylitis is directly on the lateral epicondyle while in RTS the tenderness is 5 cm distal to the epicondyle. C: Increased pain in the proximal radial forearm and over the radial tunnel, on hyperextension of the wrist against resistance. D: Pain during resisted extension of the middle finger is a valuable test in diagnosis of RTS.
Imaging studies
MRI studies of patients with RTS usually show no pathology but in some cases they may show muscle edema or atrophy along the distribution of the radial and posterior interosseous nerves (finger extensors, supinator and less, pronator muscles) but the validity of the MRI findings is controversial (21). Ferdinand et al. reported abnormal MRI findings in 21 out of 25 patients with RTS. The most common finding was muscle denervation along the posterior interosseous nerve distribution within the supinator muscle (22). However some studies stated that MRI imaging does not have a key role in the RTS diagnosis and workup (21).
EMG and NCV tests
Electromyography (EMG) and nerve conduction velocity (NCV) results are typically normal in patients diagnosed with RTS. Previously, studies have been performed to demonstrate nerve conduction abnormality after different active maneuvers. Rosén et al compared the motor latency at rest and with active resisted supination but they could not find difference in these two different conditions (23). Kupfer et al. measured differences in motor latency in forearm neutral, supination, and pronation positions. In the study, patients who previously had a confirmed diagnose of RTS had a greater average differential latency compared with controls which formed the basis for the recommended differential latency of 0.30 ms or greater as diagnostic criteria for RTS (11, 24).
Differential Diagnosis
Pain on the dorsal forearm that worsens at night and arm fatigue are typical presentation of RTS. However these symptoms are not specific to RTS and diagnosing of RTS based on the presentation is difficult (1, 6). Another confounding factor in diagnosis of RTS is the lack of confirmatory clinical tests. Therefore, RTS is a diagnosis of exclusion and is dependent on clinical signs and symptoms.
The preliminary step in evaluation of RTS requires the exclusion of proximal nerve pathology such as inflammation or trauma of the brachial plexus. Brachial plexus injuries can present as pain in the shoulder and upper limb. In addition, biceps muscle and its tendon may induce elbow pain that can be mistaken for RTS. Tendinopathy is a commonly associated with a rotator cuff tear or shoulder disorders (25).
Ultrasound, magnetic resonance imaging (MRI), and electromyography can be utilized to rule out other pathologies that can underlie lateral elbow pain. Lateral epicondylitis, PIN syndrome, osteoarthritis of the radioapitellar joint, impingement of the articular branch of the radial nerve, synovitis of the radiocapitellar joint, a muscle tear of the extensor carpi radialis brevis, and posterior plica impingement are diseases that can present with lateral elbow pain (8).
Lateral epicondylitis, which is differentiated from RTS by the tenderness directly on the lateral epicondyle, has been identified concurrently in several studies to 21 - 41 % (15, 26, 27). Conversely, RTS has been estimated to be present in 5% of patients diagnosed with lateral epicondylitis (28). We believe that in some patients the pain associated with lateral epicondylitis is because the ECRB lies next to the PIN and the fact that the PIN carries afferent impulses may explain the pain from the degenerated ECRB tendon.
Motor signs such as digital and thumb extensor motor weakness distinguish PIN syndrome from RTS. Even in complete PIN palsy, the function of the extensor carpi radialis longus muscle and the ability to extend and radially deviate the wrist are preserved (10). PIN syndrome also does not present with pain, which is the predominant complaint in patients with RTS (5).
The pain due to the irritation of the superficial branch of the radial nerve can be mimicked by De Quervain’s tenosynovitis syndrome (8).
Treatment
The goals of treatment in RTS management are pain resolution and encouraging the patient to return to work and previous activities (29). Both surgical and non-surgical treatments are available for management of RTS (25).
Non-surgical treatment
Common non-surgical methods include immobilization of the wrist with splinting or casting, anti-inflammatory medication, ultrasound massage, and physical therapy (1). Radial nerve block using a local anesthetic injection through the radial tunnel in may provide a partial or complete resolution of the symptoms. Activity modifications such as avoiding prolonged elbow extension, forearm pronation, and wrist flexion are recommended as a part of the non-operative management. However, the success rate of conservative treatments is in doubt. Steven et al report only 4 out of 15 patients with the diagnosis of RTS had improvement with non-surgical treatments (30). Jui-Tien Lee reports similarly poor results as well (29). One study reported a single injection of 2 mL 1% lidocaine and 40 mg of triamcinolone in 1 mL of carrier achieved 72% pain relief after 6 weeks and 64% for a period of more than two years (7). Surgical intervention is recommended if the symptoms do not improve with three months of conservative treatments (10).
Surgical treatment
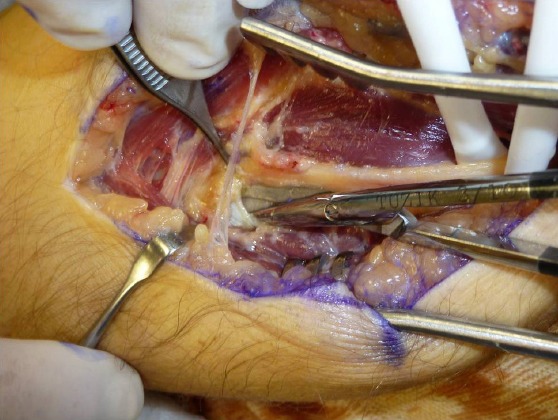
In 1983, Steven H reported the first series of patients with RTS treated surgically with the success rate of 14 out of 15 patients (93.4%) (30). A patient whose symptoms do not respond to the non-surgical treatment is a good candidate for the surgical decompression (1). The decompression is performed for the radial nerve and both of its branches: the posterior interosseous nerve (PIN) and the superficial branch of the radial nerve (SBRN). The success rate for decompressing of patients suffering from RTS was estimated between 10 to 95% (1). Regardless of the surgical approaches, release of the nerve from the arcade of Frohse and ligating the radial recurrent blood vessels is essential (13).
Transbrachioradialis and anterior approaches are the more frequently used approaches used today among the several known approaches to surgical release of the radial nerve. Bolster et al. demonstrated in a study involving 12 patients that 11 patients (91.6%) were satisfied with the transbrachioradial approach.
Dorsal approach between mobile wad and finger extensors (Thompson):
The forearm is positioned in pronation and the incision is made one inch distal to the lateral epicondyle and extended along the midpoint of the wrist. The posterior cutaneous nerve of the forearm, usually located anterior to the incision, should be identified and protected. Then, the mobile wad, formed by the muscle bellies of the brachioradialis, extensor carpi radialis longus and brevis, is identified and dissected from the rest of the extensor muscles. A well-defined yellowish fascial which is more prominent at distal is the landmark which separates extensor carpi radialis berevis and extensor digitorom commonis mucles from each other. After separating the two muscles bluntly, the underlying supinator muscle, with its characteristic shiny oblique fibers, is identified. The arcade of Frohse is identified as a tendinous band at proximal side of supinator muscle. Initially the radial recurrent blood vessels (leash of Henry) should be ligated just proximal to the arcade of Frohse. The arcade of Frohse is released, and the superficial head of the supinator muscle is divided totally to ensure that the inferior margin of the supinator is completely released. If surgical treatment of associated lateral epicondylitis is desired, the incision can be extended proximally.
Dorsal approach between brachioradialis and wrist extensors:
The skin incision is similar to dorsal (Thompson) approach. Unlike the previous approach, the interval between the brachioradialis and extensor carpi radialis longus is selected. The posterior cutaneous nerve of the forearm should be identified and protected. After identification of fascial interval between the two muscles, there belies divided from each other and the supinator mascle is exposed. The rest of the dissection can be continued bluntly to expose the arcade of Frohse. Some investigators advocate the release of the extensor carpi radialis brevis tendon at the lateral epicondyle from its origin to treat any associated lateral epicondylitis as well.
Anterior approach:
While the forearm is in supination, a curvilinear incision is chosen; beginning before the lateral epicondyle and extending distally along the groove between the brachioradialis muscle and the biceps. The incision is extended between the mobile wad and Brachioradialis where the radial nerve exists. After identification of the radial nerve, the nerve is followed distally as it bifurcates into the superficial radial nerve and the posterior interosseous nerve (PIN). The arcade of Frohse is released and the radial recurrent blood vessels are ligated. The entire length of the supinator muscle is visualized and completely released.
Since an anterior approach has the capability of exposure of the radial nerve both proximal and distal to the elbow, it is more useful in cases with probable compression of the radial nerve proximal to the elbow.
Transmuscular brachioradialis-splitting approach:
In this approach, the incision is slightly anterior to the previous incision described with Thompson. After skin incision, the Brachioradialis fascia is released longitudinally and the muscle fibers are split along the muscle fibers bluntly until the radial nerve is exposed. The arcade of Frohse and the superficial head of the supinator muscle are divided completely.
Outcomes
Although non-surgical treatment shows a reliable outcome, surgical treatment is more promising. PIN release alone showed a 39% to 95% success rate while this amount in release of both PIN and SBRN was equal to 67% to 92% (2, 3, 7, 9, 14, 15, 17, 19, 26, 27, 30-33). In the Stanley et al. study, they concluded that if the patient could not recover completely over the period of 9 months, the surgery should be considered unsuccessful (8). Some studies emphasized at decompression of both PIN and SBRN together for better outcome.
Radial tunnel syndrome is a disease which we should consider as presenting in elbow and forearm pains (34). It is diagnosed with lateral elbow and dorsal forearm pain which may radiate to the wrist and dorsum of fingers. The disease is more common amongst women aged 30 to 50 years old. A painful point exists one inch distal to the lateral epicondyle and over the radial tunnel which exacerbates with resisted active extension of the wrist and third finger could confirm the diagnosis.
Although non-surgical treatments such as rest, NSAIDs, injections, and physiotherapy do not believe to have permanent relief, it is justified employing them before the decision for surgery. Surgery has been reported to have completely diminished the symptoms in 67% to 93% of patients.
References
- 1.Bolster MA, Bakker XR. Radial tunnel syndrome: emphasis on the superficial branch of the radial nerve. J Hand Surg Eur. 2009;34(3):343–7. doi: 10.1177/1753193408099832. [DOI] [PubMed] [Google Scholar]
- 2.Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg Am. 1979;4(1):52–9. doi: 10.1016/s0363-5023(79)80105-7. [DOI] [PubMed] [Google Scholar]
- 3.Roles NC, Maudsley RH. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J Bone Joint Surg Br. 1972;54(3):499–508. [PubMed] [Google Scholar]
- 4.Michele AA, Krueger FJ. Lateral epicondylitis of the elbow treated by fasciotomy. Surgery. 1956;39(2):277–84. [PubMed] [Google Scholar]
- 5.Naam NH, Nemani S. Radial tunnel syndrome. Orthop Clin North Am. 2012;43(4):529–36. doi: 10.1016/j.ocl.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Eversmann WW. Entrapment and compression neuropathies. In: Green DP, Hotchkiss RN, editors. Operative Hand Surgery. 3rd ed. New York: Churchill Livingstone; 1993. pp. 1341–85. [Google Scholar]
- 7.Sarhadi NS, Korday SN, Bainbridge LC. Radial tunnel syndrome: diagnosis and management. J Hand Surg Br. 1998;23(5):617–9. doi: 10.1016/s0266-7681(98)80015-6. [DOI] [PubMed] [Google Scholar]
- 8.Stanley J. Radial Tunnel Syndrome: A Surgeon's Perspective. J Hand Ther. 2006;19(2):180–4. doi: 10.1197/j.jht.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop. 1998;22(2):102–6. doi: 10.1007/s002640050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dang AC, Rodner CM. Unusual Compression Neuropathies of the Forearm, Part I: Radial Nerve. J Hand Surg Am. 2009;34(10):1906–14. doi: 10.1016/j.jhsa.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 11.van den Ende KI, Steinmann SP. Radial Tunnel Syndrome. J Hand Surg Am. 2010;35(6):1004–6. doi: 10.1016/j.jhsa.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Barnum M, Mastey RD, Weiss AP, Akelman E. Radial tunnel syndrome. Hand Clin. 1996;12(4):679–89. [PubMed] [Google Scholar]
- 13.Clavert P, Lutz JC, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn JL. Frohse's arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95(2):114–8. doi: 10.1016/j.otsr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Atroshi I, Johnsson R, Ornstein E. Radial tunnel release. Unpredictable outcome in 37 consecutive cases with a 1-5 year follow-up. Acta Orthop Scand. 1995;66(3):255–7. doi: 10.3109/17453679508995536. [DOI] [PubMed] [Google Scholar]
- 15.Sotereanos DG, Varitimidis SE, Giannakopoulos PN, Westkaemper JG. Results of surgical treatment for radial tunnel syndrome. J Hand Surg Am. 1999;24(3):566–70. doi: 10.1053/jhsu.1999.0566. [DOI] [PubMed] [Google Scholar]
- 16.Roquelaure Y, Raimbeau G, Saint-Cast Y, Martin YH, Pelier-Cady MC. Occupational risk factors for radial tunnel syndrome in factory workers. Chir Main. 2003;22(6):293–8. doi: 10.1016/j.main.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Hagert CG, Lundborg G, Hansen T. Entrapment of the posterior interosseous nerve. Scand J Plast Reconstr Surg. 1977;11(3):205–12. doi: 10.3109/02844317709025519. [DOI] [PubMed] [Google Scholar]
- 18.van Rossum J, Buruma OJ, Kamphuisen HA, Onvlee GJ. Tennis elbow-A radial tunnel syndrome? J Bone Joint Surg Br. 1978;60(2):197–8. doi: 10.1302/0301-620X.60B2.659463. [DOI] [PubMed] [Google Scholar]
- 19.Verhaar J, Spaans F. Radial tunnel syndrome. An investigation of compression neuropathy as a possible cause. J Bone Joint Surg Am. 1991;73(4):539–44. [PubMed] [Google Scholar]
- 20.Loh YC, Lam WL, Stanley JK, Soames RW. A new clinical test for radial tunnel syndrome-the Rule-of-Nine test: a cadaveric study. J Orthop Surg (Hong Kong) 2004;12:83–6. doi: 10.1177/230949900401200115. [DOI] [PubMed] [Google Scholar]
- 21.Ferdinand BD, Rosenberg ZS, Schweitzer ME, Stuchin SA, Jazrawi LM, Lenzo SR, et al. MR Imaging Features of Radial Tunnel Syndrome: Initial Experience. Radiology. 2006;240(1):161–8. doi: 10.1148/radiol.2401050028. [DOI] [PubMed] [Google Scholar]
- 22.Thomas SJ, Yakin DE, Parry BR, Lubahn JD. The anatomical relationship between the posterior interosseous nerve and the supinator muscle. J Hand Surg Am. 2000;25(5):936–41. doi: 10.1053/jhsu.2000.16360. [DOI] [PubMed] [Google Scholar]
- 23.Rosén I, Werner CO. Neurophysiological investigation of posterior interosseous nerve entrapment causing lateral elbow pain. Electroencephalogr Clin Neurophysiol. 1980;50(1-2):125–33. doi: 10.1016/0013-4694(80)90329-6. [DOI] [PubMed] [Google Scholar]
- 24.Kupfer DM, Bronson J, Lee GW, Beck J, Gillet J. Differential latency testing: a more sensitive test for radial tunnel syndrome. J Hand Surg Am. 1998;23(5):859–64. doi: 10.1016/S0363-5023(98)80163-9. [DOI] [PubMed] [Google Scholar]
- 25.Smith RS. The upper limb in primary care Part 1: Upper and lower arm, elbow. Reports Rheumatic Dis. 2012;6(11):1–10. [Google Scholar]
- 26.Ritts GD, Wood MB, Linscheid RL. Radial tunnel syndrome: a ten-year surgical experience. Clin Orthop Relat Res. 1987;219:201–5. [PubMed] [Google Scholar]
- 27.Jebson PJ, Engber WD. Radial tunnel syndrome: long-term results of surgical decompression. J Hand Surg Am. 1997;22(5):889–96. doi: 10.1016/S0363-5023(97)80086-X. [DOI] [PubMed] [Google Scholar]
- 28.Lee JT, Azari K, Jones NF. Long term results of radial tunnel releasee the effect of co-existing tenn is elbow, multipl e compressio n syndromes and workers ' compensation. J Plast Reconstr Aesthet Surg. 2008;61(9):1095–9. doi: 10.1016/j.bjps.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Cleary CK. Management of radial tunnel syndrome: a therapist's clinical perspective. J Hand Ther. 2006;19(2):186–91. doi: 10.1197/j.jht.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 30.Moss SH, Switzer HE. Radial tunnel syndrome: A spectrum of clinical presentations. J Hand Surg Am. 1983;8(4):414–20. doi: 10.1016/s0363-5023(83)80201-9. [DOI] [PubMed] [Google Scholar]
- 31.Younge DH, Moise P. The radial tunnel syndrome. Int Orthop. 1994;18(5):268–70. doi: 10.1007/BF00180222. [DOI] [PubMed] [Google Scholar]
- 32.De Smet L, Van Raebroeckx T, Van Ransbeeck H. Radial tunnel release and tennis elbow: disappointing results? Acta Orthop Belg. 1999;65(4):510–3. [PubMed] [Google Scholar]
- 33.Lawrence T, Mobbs P, Fortems Y, Stanley JK. Radial tunnel syndrome: A retrospective review of 30 decompressions of the radial nerve. J Hand Surg Br. 1995;20(4):454–9. doi: 10.1016/s0266-7681(05)80152-4. [DOI] [PubMed] [Google Scholar]
- 34.Moradi A, Ebrahimzadeh MH, Ring D. Nonspecific Arm Pain. Arch Bone Jt Surg. 2013;1(2):53–8. [PMC free article] [PubMed] [Google Scholar]


