Abstract
AIM: To perform a systematic review and meta-analysis on robotic-assisted vs laparoscopic liver resections.
METHODS: A systematic literature search was performed using PubMed, Scopus and the Cochrane Library Central. Participants of any age and sex, who underwent robotic or laparoscopic liver resection were considered following these criteria: (1) studies comparing robotic and laparoscopic liver resection; (2) studies reporting at least one perioperative outcome; and (3) if more than one study was reported by the same institute, only the most recent was included. The primary outcome measures were set for estimated blood loss, operative time, conversion rate, R1 resection rate, morbidity and mortality rates, hospital stay and major hepatectomy rates.
RESULTS: A total of 7 articles, published between 2010 and 2014, fulfilled the selection criteria. The laparoscopic approach was associated with a significant reduction in blood loss and lower operative time (MD = 83.96, 95%CI: 10.51-157.41, P = 0.03; MD = 68.43, 95%CI: 39.22-97.65, P < 0.00001, respectively). No differences were found with respect to conversion rate, R1 resection rate, morbidity and hospital stay.
CONCLUSION: Laparoscopic liver resection resulted in reduced blood loss and shorter surgical times compared to robotic liver resections. There was no difference in conversion rate, R1 resection rate, morbidity and length of postoperative stay.
Keywords: Laparoscopic liver resections, Robotic liver resections, Outcome, Systematic review, Meta-analysis
Core tip: No consensus is available in the literature about which technique between laparoscopic and robotic liver resection is more beneficial to the patient. This is the first systematic review and meta-analysis comparing laparoscopic and robotic liver resection. We investigated these two techniques in terms of estimated blood loss, operative time, conversion rate, R1 resection rate, morbidity and mortality rates, hospital stay and major hepatectomy rates.
INTRODUCTION
Since its introduction by Reich et al[1] in 1991, laparoscopy has been increasingly used for resection of benign and malignant liver lesions, from minor resections to major hepatectomies and living liver donation[2-7]. Several studies have suggested the safety, feasibility, comparable perioperative and long-term outcomes of laparoscopy compared to the standard open approach[8-10]. In many centers, laparoscopic liver resection (LLR) is considered the first choice in well-selected patients. Current limitations include a steep learning curve[11], tumors adjacent to the hilum, the hepatic veins and the inferior vena cava, bulky tumors, difficult access to the posterior segments and the need for biliary and vascular reconstructions[9]. The reports of LLR on the posterior segments are few and have been limited to centers with a wide experience in both open and laparoscopic liver surgery.
Robotics was introduced two decades ago with the aim of overcoming the intrinsic limitations of laparoscopic instruments and visualization. The da Vinci® Robotic Surgical System was introduced in 2000 to improve the surgeon’s dexterity by taking advantage of the camera’s three-dimensional view and endowristed instruments[12-15]. Furthermore, robotics has also been described as an effective tool for non-resective and demanding hepatobiliary surgery, such as bilio-digestive reconstructions and choledocal cysts excisions[16,17].
Radical prostatectomy and various gynecological procedures currently make up the vast majority of robotic surgeries: by 2011, more than 90% of the 360.000 robotic worldwide procedures were urologic and gynecological operations[18]. Perioperative and oncological outcomes are equivalent to those reported in the literature with the standard approach. Two major drawbacks are the lack of haptic feedback and high costs[19].
Many believe that robotic-assisted liver resections (RLR) could be an advantageous technique allowing for accurate tissue dissection and easier intracorporeal sewing; furthermore, it is believed that RLR may allow for the better resection of lesions adjacent to major vessels, close to the liver hilum, or in difficult anatomic positions[20]. However, its evolution to now is not what one would have expected for the LLR. Its use has been relatively unexplored, accounting for few reports with limited patient volume[21-37].
As is the case of laparoscopic surgery, several reports have documented the clinical outcomes of robotic technique compared to open procedures[18]. However, due to the limited number of reports comparing both techniques, it is not yet clear which method is more beneficial to the patient or the most useful for lesions located in difficult liver segments.
Considering the lack of consensus, the objective of this study was to perform a systematic review and meta-analysis on robotic-assisted vs laparoscopic liver resections for all type of liver lesions. The primary outcome measures were estimated blood loss, operative time, conversion rate, R1 resection rate, morbidity and mortality rates, hospital stay and major hepatectomy rates. The analysis was limited to humans and to articles reported in English language but no restriction was set for type of publication, date, or publication status.
MATERIALS AND METHODS
Literature search
PRISMA statement guidelines were followed for conducting and reporting meta-analysis data[38]. PICOS scheme was followed for reporting inclusion criteria. A systematic literature search was performed independently by two of the authors (RM and GB) using PubMed, Scopus and the Cochrane Library Central. The search was limited to humans and to articles reported in English language. No restriction was set for type of publication, date, or publication status. Participants of any age and sex who underwent robotic or laparoscopic liver resection for all type of hepatic lesions were considered; robotic liver resections were considered as the Intervention group while the laparoscopic resections were considered as the comparator group according to the PICOS scheme. The search strategy was based on different combinations of words for each database. For the PubMed database the following combination was used: (Laparoscopic or laparoscopy or laparoscopically or minimally invasive) and (liver resection or liver resections or hepatectomy or hepatectomies or hepatic resection or hepatic resections or liver surgery) and (robotic or robotically or robot or robot assistance or robot-assisted or robotic-assisted).
For the Scopus database the following combination was used: TITLE-ABS-KEY (Laparoscopic or laparoscopy or laparoscopically or “minimally invasive”) and TITLE-ABS-KEY (“liver resection” or “liver resections” or hepatectomy or hepatectomies or “hepatic resection” or “hepatic resections” or “liver surgery”) and TITLE-ABS-KEY (robotic or robotically or robot or “robot assistance” or “robot-assisted” or “robotic-assisted”).
The same key words were inserted in the search manager fields of the Cochrane Library Central. The search was further broadened by extensive cross-checking of reference lists of all retrieved articles fulfilling the inclusion criteria. For all databases, the last search was run on 07 July, 2014.
Study selection
The same two authors independently screened the titles and abstracts of the primary studies that were identified in the electronic search. Duplicate studies were excluded. The following inclusion criteria were set for inclusion in this meta-analysis: (1) Studies comparing robotic and laparoscopic liver resection for all types of hepatic lesions; (2) Studies reporting at least one perioperative outcome including blood loss, operative timing, conversion, mortality, morbidity, R1 resection rates, hospital stay and rate of major hepatectomies; and (3) If more than one study was reported by the same institute, only the most recent or the highest level of study was included.
The following exclusion criteria were set: (1) Original studies assessing the outcome of either laparoscopic or robotic liver resection; (2) Review articles, letters, comments and case reports; and (3) Studies where it was impossible to retrieve or calculate data of interest.
The Cohen kappa statistic was used to quantify agreement between the investigators.
Data extraction
The same two authors extracted the following main data (Table 1 and 2): (1) First author, year of publication and study type; (2) Number and characteristics of patients of both the laparoscopic and robotic resection groups; and (3) Treatment outcomes, including blood loss, operative timing, conversion, mortality, morbidity, R1 resection rates, hospital stay and rate of major hepatectomies. All relevant texts, tables and figures were reviewed for data extraction; whenever further information was required, the corresponding authors of the papers were contacted by e-mail.
Table 1.
Characteristics of included studies
|
Laparoscopic liver resection |
Robotic liver resection |
|||||||||
| Ref. | Country | Type of study | Total n. of patients | No. of patients | Age | M/F | No. of patients | Age | M/F | Score of study quality2 |
| Berber et al[21] | United States | Retro/Comparative | 32 | 23 | 66.7 ± 9.6 | 12/11 | 9 | 66.6 ± 6.4 | 7/2 | 4+2+3 |
| Ji et al[30] | China | Retro/Case-control | 33 | 20 | NR | NR | 13 | 53 (39-79)1 | 9/4 | 3+1+3 |
| Troisi et al[45] | Belgium-Italy | Retro/Comparative | 263 | 223 | 55.3 ± 15.7 | 98/125 | 40 | 64.6 ± 12.1 | 27/13 | 4+1+3 |
| Lai et al[41] | China | Retro/Comparative | 66 | 33 | NR | NR | 33 | NR | NR | 4+1+3 |
| Wu et al[47] | Taiwan | Retro/Comparative | 79 | 41 | 54.1 ± 14 | 28/13 | 38 | 60.9 ± 14.9 | 32/6 | 4+1+3 |
| Tsung et al[46] | United States | Retro/Case-control | 171 | 114 | 58.7 ± 15.8 | 47/67 | 57 | 58.3 ± 14.6 | 24/33 | 3+2+3 |
| Spampinato et al[43] | Italy | Retro/Comparative | 50 | 25 | 62 (33-80)1 | 10/15 | 25 | 63 (32-80) | 13/12 | 4+2+3 |
Data expressed as median (range);
According to the NOS (Newcastle-Ottawa Scale) classification. Retro: Retrospective; NR: Not reported.
Discrepancies between the two reviewers were resolved by consensus discussion.
Risk of Bias
The Newcastle-Ottawa Scale was used for retrospective studies to assess quality. Funnel plots were constructed to assess the risk of publication bias across series for all outcome measures.
Statistical analysis
The meta-analysis was performed using RevMan software version 5.1. Odds ratios (OR) were used as a summary measure of efficacy for dichotomous data and mean differences (MD) between groups were used for continuous variables. A 95%CI was reported for both measures. If the study provided medians and interquartile ranges instead of means ± SD, the means ± SD were imputed, as described by Hozo et al[39]. The fixed-effect model was used when no heterogeneity was detected among studies, while the random-effect model was preferred when variance existed. Statistical heterogeneity was evaluated using the I2 statistic. I2 values of 0-25%, 25%-50% and > 50% were considered as indicative of homogeneity, moderate heterogeneity and high heterogeneity, respectively. All statistical data were considered with a P-value < 0.05. The statistical methods of this study were reviewed by Filippo Oropallo from National Statistical Institute of Italy.
RESULTS
Study selection
The literature search yielded 291 articles; after duplicate removal, 207 titles and abstracts were reviewed (Figure 1). Of these, 196 papers were excluded for the following reasons: 110 were not related to liver resections, 81 did not compare techniques, 3 were review articles and 2 were letters. Finally, eleven articles[21,30,40-48] were selected for full-text review; of these, four more were excluded because of redundant series from the same institute[40,42,44,48]. There was no disagreement regarding eligibility of full-text articles (Cohen kappa = 1). Finally, a total of 7 articles, dated between 2010 and 2014, fulfilled the selection criteria and were therefore included in this meta-analysis; all the articles finally selected were retrospective studies, of which two case-controls[30,46] and five comparative[21,41,43,45,47]. All of the studies included a total of 694 patients: 479 who underwent laparoscopic liver resection and 215 cases of robotic liver resection. The characteristics of the included studies are summarized in Table 1. According to the NOS scale, the study quality was graded 9 for two publications (both 4+2+3 respectively for Selection, Comparability and Exposure measurements)[21,43], 8 for four (three 4+1+3[41,45,47] and one 3+2+3[46]) and 7 for one publication (3+1+3)[30].
Figure 1.

Study selection.
Three corresponding authors were contacted by e-mail for obtaining unpublished or unclear data[21,30,41] and of these, none responded addressing questions. The outcomes of interest of each single study are summarized in Table 2.
Table 2.
Raw data of each included study
| First author | Blood loss (mL) | Operative time (min) | Conversion | Morbidity | R1 rate | Hospital stay (d) |
| Berber et al[21] | ||||||
| Laparoscopic liver resection | 155 ± 54 | 233.6 ± 16.4 | 0% | 17% | NR | NR |
| Robotic liver resection | 136 ± 61 | 258.5 ± 27.9 | 11.10% | 11% | NR | NR |
| Ji et al[30] | ||||||
| Laparoscopic liver resection | NA | 130 ± 42.5 | 10% | 10% | NR | NA |
| Robotic liver resection | NA | 338 ± 166.9 | 0% | 7.80% | NR | NA |
| Troisi et al[45] | ||||||
| Laparoscopic liver resection | 174 ± 133 | 262 ± 111 | 7.60% | 12.60% | 5.40% | 5.9 ± 3.8 |
| Robotic liver resection | 330 ± 303 | 271 ± 100 | 20% | 12.50% | 7.50% | 6.1 ± 2.6 |
| Lai et al[41] | ||||||
| Laparoscopic liver resection | 347.7 ± 498.7 | 133.4 ± 42.7 | NR | 9% | 9.10% | NR |
| Robotic liver resection | 373.4 ± 872 | 202.7 ± 69.8 | NR | 3% | 9.10% | NR |
| Wu et al[47] | ||||||
| Laparoscopic liver resection | 173 ± 165 | 227 ± 80 | 12.20% | 10% | NR | 7.2 ± 4.4 |
| Robotic liver resection | 325 ± 480 | 380 ± 166 | 5% | 8% | NR | 7.9 ± 4.7 |
| Tsung et al[46] | ||||||
| Laparoscopic liver resection | 100 ± 50 | 198.5 ± 20.6 | 8.80% | 26% | 8% | 4 ± 0.3 |
| Robotic liver resection | 200 ± 71.8 | 253 ± 43.7 | 7% | 19.30% | 5% | 4 ± 0.6 |
| Spampinato et al[43] | ||||||
| Laparoscopic liver resection | 512.5 ± 287.5 | 375 ± 105 | 4% | 36% | 9% | 10.2 ± 4.2 |
| Robotic liver resection | 625 ± 450 | 456.2 ± 121 | 4% | 16% | 0% | 10.5 ± 4.5 |
NR: Not reported; NA: Not assessable.
Estimated blood loss
Six of the included studies reported results regarding blood loss in both groups. An overall significant reduction in blood loss was observed in the laparoscopic group compared to the robotic one (MD = 83.96, 95%CI: 10.51-157.41, P = 0.03) (Figure 2).
Figure 2.
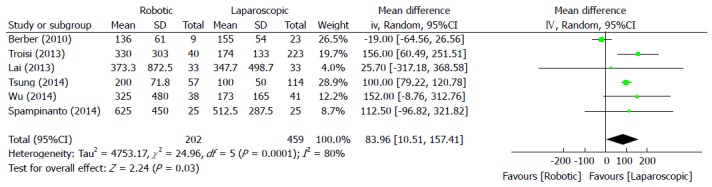
Meta-analysis Forest plot concerning estimated blood loss.
Operative time
All articles were included to determine the overall effect regarding operative time. According to Figure 3, the laparoscopic approach was associated with a significantly lower operative time compared to the robotic technique (MD = 68.43, 95%CI: 39.22-97.65, P < 0.00001).
Figure 3.

Meta analysis Forest plot concerning operative time.
Conversion
Conversion was considered as switching to an open or hand assisted approach during the operation. Six of the seven papers included in the meta-analysis reported data regarding conversion, and no statistically significant overall differences were observed (OR = 1.19, 95%CI: 0.48-2.99, P = 0.71) (Figure 4).
Figure 4.

Meta-analysis Forest plot concerning conversion.
R1 resection rate
No statistically significant difference was found between the two approaches with respect to the R1 resection rate, including four of the seven studies selected (OR = 1.71, 95%CI: 0.95-3.09, P = 0.07) (Figure 5).
Figure 5.

Meta-analysis Forest plot concerning R1 resection rate.
Mortality and morbidity
Due to the different reporting methods in the single papers, overall results regarding mortality were impossible to calculate. In some articles, 30-d mortality was reported[41], while in others, 90-d mortality was the measurement used[43,46]; in some of the papers, no specification was given[45,47]. Finally, two articles did not report any data on mortality[21,30]. Regarding overall morbidity, data were reported in all of the included studies and no overall differences were observed (OR = 0.66, 95%CI: 0.40-1.09, P = 0.10) (Figure 6).
Figure 6.
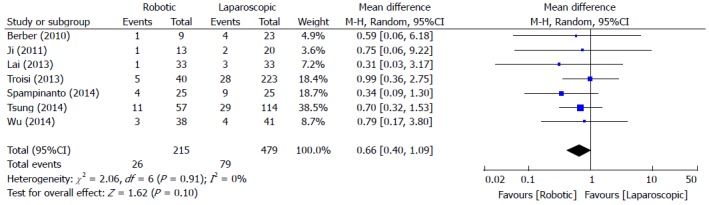
Meta-analysis Forest plot concerning morbidity.
Hospital stay
Four of the seven included studies reported hospital stay outcomes. No overall differences were found between the two approaches (MD = 0.01, 95%CI: -0.15-0.17, P = 0.89, Figure 7).
Figure 7.

Meta-analysis Forest plot concerning hospital stay.
Major hepatectomies rate
Due to the different classifications regarding major and minor hepatectomies and to the lack of reported data among studies, no overall effect was calculated. Specifically, two articles described only minor hepatectomies[21,41], one described only major hepatectomies[43]; one paper considered a major hepatectomy as the resection of 4 or more segments[46] while three articles considered a major hepatectomy as the resection of 3 or more segments[30,45,47].
Publication bias
Funnel plots were constructed for each outcome and showed symmetry, suggesting that publication bias was not large and was unlikely to drive conclusions (Figure 8A). Funnel plots regarding hospital stay showed substantial asymmetry (Figure 8B).
Figure 8.

Funnel plot of morbidity (A) and hospital stay (B) in all included studies.
DISCUSSION
Laparoscopic liver resections are considered safe and effective in well-selected patients and have shown better results in terms of blood transfusion, postoperative hospital stay and morbidity compared to open surgery, as described in the thirteen reported meta-analyses[49-61]. Several variants for the laparoscopic approach have been described, such as the pure laparoscopic, the hand-assisted, the hybrid and single-port techniques. Conversely, it is not yet clear whether robotic assistance demonstrates substantial advantage over the pure laparoscopic technique.
The robotic platform is a tool with which many of the limitations of conventional laparoscopic liver surgery can be overcome: two-dimensional imaging and tremor amplification, fulcrum effect against the port, limited degrees of freedom for manipulation and awkward ergonomics. Furthermore, the augmented dexterity enabled by the endowristed movements, the software filtration of surgeon’s movements and the high-definition three-dimensional vision provided by the stereoscopic camera combine to guarantee a steady and careful dissection of the structures[62]. Nevertheless, RLR has had a slower evolution over the last years; it does not currently provide some useful tools, such as an “endowristed” surgical aspirator or high-energy device that can fully exploit the potential of the movements and vision offered by the robot, especially when operating in a limited resection space (i.e., when approaching P-S segments). Other potential limitations of RLR concern the need of an additional attending surgeon and the high costs of robot purchasing, instrumentation and annual maintenance. There are very few centers in the world that have performed a limited number of robotic liver resections on highly selected patients. The technique has not been standardized and it is questionable whether any of these centers have gone through the learning curve.
Few reports regarding laparoscopic and robotic liver resections have been published that have evaluated different outcomes and results among series; therefore, there has been difficulty not only in interpreting data but also in drawing final conclusions regarding the superiority of one approach over another. A meta-analysis, as a quantitative method for therapeutic evaluation, may be used when controversy persists in order to determine the results.
To our knowledge, this is the first systematic review and meta-analysis comparing robotics to laparoscopy for liver resections. In this analysis, it was possible to include only 7 studies containing 694 patients; all of these articles were retrospective of which 2 case-controls and 5 comparative; to date, this may represent the largest body of information available for the comparison of RLR and LLR. According to the Newcastle-Ottawa scale used for assessing quality of the studies, articles included in this meta-analysis were graded with 9[21,43], 8[41,45-47] or 7[30], reflecting a high quality concerning selection of patients, comparability and exposure measurements.
The first laparoscopic liver resection was described by Gagner et al[63] in 1992, whereas the first robotic liver resection was published in 2003 by Giulianotti et al[64]. While the laparoscopic technique has had a worldwide spread since its introduction, the robotic technique has not had the same evolution, possibly due to the significant upfront costs and the different required learning curve. In 2010, Berber et al[21] described the first study comparing the two methods. Since then, we have observed a progressive increase of publications, suggesting a growing interest in comparing both techniques. Unfortunately, in contrast with laparoscopic surgery, there have been no prospective randomized studies comparing laparoscopic and robotic techniques.
The results of the present meta-analysis shows a significant increase in bleeding in RLR. This may be explained by the different techniques used for liver transection. In fact, the most prevalent technique of hepatic transection used in LLR requires the use of a harmonic scalpel for superficial liver transection; in most of the cases and accordingly to the surgeon’s preference, the Cavitron Ultrasonic Surgical Aspirator (CUSA) is used for deeper transection, which is a tool that allow a meticulous and precise dissection of the parenchymal structures. Conversely, robotic liver transection is mainly based on the crush-clamping technique, which requires, in most cases, the use of an intermittent inflow occlusion (Pringles manoeuver). In this case, an increased ischemia/reperfusion injury should be anticipated when operating on a cirrhotic liver[65].
Another difference we found was that the surgical time was significantly longer in robotic hepatectomy. The difference could be due to the different technique of hepatic resection, but may also be because the robotic technique is more recent and requires greater experience and refinement; in addition, there may be a difference among standardization of the procedures and an obvious docking time of the system.
The rate of conversion was comparable between RLR and LLR, which most likely indicates a similar difficulty in approaching liver surgery.
The basic principle behind the oncological resection of malignant diseases is to keep a sufficient tumor-free margin in order to avoid incomplete tumor resection and possibly iatrogenic spread. Considering the fact that most of the indications for minimally invasive liver surgery are actually met in malignancies[66], margin width is a major indicator in the quality of surgical resection. With the aim of highlighting any differences between the two techniques, the third end-point of our meta-analysis was the margin width. We found that the rate of R1 resection was not statistically different between the two techniques, although there was a trend towards decreased R1 resection margins in the LLR group. These data should be analyzed in more detail in future studies, which may suggest an increased difficulty in the identification of a tumoral lesion by intraoperative ultrasound (IOUS) with the robotic technique. A possible explanation for this is the fact that the surgeon who performs the ultrasound is not the same that performs hepatectomy at the robotic console. Only very recently robotic technology has provided an IOUS guided by the surgeon at the console.
According to our analysis, there was no statistically significant difference in the morbidity rate between the two analyzed techniques, although a trend toward a lower complication rate in the robotic group was observed. One might speculate that RLR offers increased surgical precision leading to meticulous dissection, individuation of small biliary structures, minimizing bile leaks and decreased overall post-operative complications. Unfortunately, we did not evaluate data in terms of the indicators of the degree of difficulty of a minimally invasive procedure performed using both approaches (i.e., resection of P-S segments or living donor hepatectomy). Therefore, we cannot conclude whether laparoscopy was performed for more technically difficult interventions or vice versa. To better characterize this issue, a comparative analysis between RLR and LLR for approaching the P-S segments is warranted.
Finally, the hospital stay showed similar results between the two techniques. These are both minimally invasive procedures; patients seems to have a comparable postoperative course. The two techniques seemed to be different for the surgeon but not for the patient.
The main limitation of this meta-analysis is that it is based on retrospective studies; only two of which are case-control studies. Another limitation of the study is that the included reports are highly heterogeneous in terms of disease indications, types of liver resection (minor or major) and location of liver lesions. One of the included articles was limited to liver resections for hepatocellular carcinoma[47], one of them was limited to major hepatectomies [43], two of them were for minor hepatectomies only[21,41], while four studies[40,42,44,48] were excluded from the meta-analysis because a portion of the patients described had already been considered in other series from the same institutions. In this way, a substantial number of patients were excluded from the analysis.
Estimated blood loss and operative time were associated with significant heterogeneity between studies. Although we used the fixed or random-effects model, as appropriate, this bias was impossible to overcome.
In the present meta-analysis, we did not analyze the technical differences between the two methods in terms of trocars positioning, type/version of the robot, instrumentation for the transection of the liver, intraoperative ultrasound methodology, duration of hilar clamping, or other reported data because our outcomes were decided a priori, based on the highest clinically relevant end-points.
Moreover, in the present systematic review we did not find studies, which focused on cost assessment between RLR and LLR. Ji et al[30] described a general hospital cost of $12.046 per intervention for robotics and $7618 for the laparoscopic technique. Furthermore Packiam et al[42], compared only the direct costs of the operating room supplies, resulting in $5.130 vs $4.408 for RLR and LLR, respectively. Future research should be directed to analyze costs differences between the two procedures.
No prospective randomized trials are reported, therefore, future research should be directed at performing prospective randomized trials comparing RLR to LLR. These prospective trials would have fewer ethical issues than the comparison to the open technique. In fact, RLR and LLR are both minimally invasive approaches without differences in safety and efficacy.
Future research should aim to extrapolate differences in the learning curves between laparoscopic and robotic liver resection and propose a method to objectively assess the degree of difficulty in minimally invasive liver surgery; this will highlight the value of each technique, leading to better outcomes.
In summary, the results of this meta-analysis of retrospective studies, demonstrated that laparoscopic liver resection resulted in less blood loss and shorter surgical times compared to robotic liver resections. There was no difference in the conversion rate, R1 resection rate, morbidity and length of postoperative stay. Future research should be directed in comparing the two techniques, also in terms of cost analysis and learning curve, especially in a prospective randomized controlled fashion.
COMMENTS
Background
The interest in minimally invasive approaches for the surgical resection of liver lesions is growing in recent years. In several centers, laparoscopic and robotic liver surgeries are now considered as the standard of care for selected patients. Despite this, no consensus is available in the literature about which of these two techniques is more beneficial to the patient.
Research frontiers
Nowadays liver resections are performed with a minimally invasive approach in a growing number of centers. The worldwide research is directed towards a type of surgery in which morbidity and stress related to the patient are minimized.
Innovations and breakthroughs
In the present study, the authors investigated the outcomes of two worldwide spread minimally invasive techniques by pooling results from different centers. This is the first report of a meta-analysis comparing robotic and laparoscopic liver resections.
Applications
The present report allows understanding the role of two minimally invasive techniques for liver resections.
Peer-review
This systematic review and meta-analysis of retrospective studies adds useful information for practice and research, and probably for policy.
Footnotes
Conflict-of-interest statement: The authors deny any conflict of interest.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: January 12, 2015
First decision: March 10, 2015
Article in press: May 7, 2015
P- Reviewer: Lee DS, Muscat JE, Plaszewski M S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
References
- 1.Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78:956–958. [PubMed] [Google Scholar]
- 2.Nguyen KT, Laurent A, Dagher I, Geller DA, Steel J, Thomas MT, Marvin M, Ravindra KV, Mejia A, Lainas P, et al. Minimally invasive liver resection for metastatic colorectal cancer: a multi-institutional, international report of safety, feasibility, and early outcomes. Ann Surg. 2009;250:842–848. doi: 10.1097/SLA.0b013e3181bc789c. [DOI] [PubMed] [Google Scholar]
- 3.Descottes B, Glineur D, Lachachi F, Valleix D, Paineau J, Hamy A, Morino M, Bismuth H, Castaing D, Savier E, et al. Laparoscopic liver resection of benign liver tumors. Surg Endosc. 2003;17:23–30. doi: 10.1007/s00464-002-9047-8. [DOI] [PubMed] [Google Scholar]
- 4.Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000;232:753–762. doi: 10.1097/00000658-200012000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, Branchereau S, Chardot C, Gauthier F, Fagniez PL, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 2002;359:392–396. doi: 10.1016/S0140-6736(02)07598-0. [DOI] [PubMed] [Google Scholar]
- 6.Scatton O, Katsanos G, Boillot O, Goumard C, Bernard D, Stenard F, Perdigao F, Soubrane O. Pure laparoscopic left lateral sectionectomy in living donors: from innovation to development in France. Ann Surg. 2015;261:506–512. doi: 10.1097/SLA.0000000000000642. [DOI] [PubMed] [Google Scholar]
- 7.Troisi RI, Wojcicki M, Tomassini F, Houtmeyers P, Vanlander A, Berrevoet F, Smeets P, Van Vlierberghe H, Rogiers X. Pure laparoscopic full-left living donor hepatectomy for calculated small-for-size LDLT in adults: proof of concept. Am J Transplant. 2013;13:2472–2478. doi: 10.1111/ajt.12362. [DOI] [PubMed] [Google Scholar]
- 8.Hu BS, Chen K, Tan HM, Ding XM, Tan JW. Comparison of laparoscopic vs open liver lobectomy (segmentectomy) for hepatocellular carcinoma. World J Gastroenterol. 2011;17:4725–4728. doi: 10.3748/wjg.v17.i42.4725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009;250:825–830. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 10.Montalti R, Berardi G, Laurent S, Sebastiani S, Ferdinande L, Libbrecht LJ, Smeets P, Brescia A, Rogiers X, de Hemptinne B, et al. Laparoscopic liver resection compared to open approach in patients with colorectal liver metastases improves further resectability: Oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol. 2014;40:536–544. doi: 10.1016/j.ejso.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Vigano L, Laurent A, Tayar C, Tomatis M, Ponti A, Cherqui D. The learning curve in laparoscopic liver resection: improved feasibility and reproducibility. Ann Surg. 2009;250:772–782. doi: 10.1097/SLA.0b013e3181bd93b2. [DOI] [PubMed] [Google Scholar]
- 12.Heemskerk J, van Gemert WG, de Vries J, Greve J, Bouvy ND. Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robot-assisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech. 2007;17:171–174. doi: 10.1097/SLE.0b013e31805b8346. [DOI] [PubMed] [Google Scholar]
- 13.Maniar HS, Council ML, Prasad SM, Prasad SM, Chu C, Damiano RJ. Comparison of skill training with robotic systems and traditional endoscopy: implications on training and adoption. J Surg Res. 2005;125:23–29. doi: 10.1016/j.jss.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A. Dexterity enhancement with robotic surgery. Surg Endosc. 2004;18:790–795. doi: 10.1007/s00464-003-8922-2. [DOI] [PubMed] [Google Scholar]
- 15.Mucksavage P, Kerbl DC, Lee JY. The da Vinci(®) Surgical System overcomes innate hand dominance. J Endourol. 2011;25:1385–1388. doi: 10.1089/end.2011.0093. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter SG, Grimsby G, DeMasters T, Katariya N, Hewitt WR, Moss AA, Reddy KS, Castle EP, Mulligan DC. Robotic resection of choledochocele in an adult with intracorporeal hepaticojejunostomy and Roux-en-Y anastomosis: Encouraging progress for robotic surgical treatment of biliary disease. J Rob Surg. 2014;8:77–80. doi: 10.1007/s11701-012-0389-5. [DOI] [PubMed] [Google Scholar]
- 17.Kang CM, Kim DH, Lee WJ. Ten years of experience with resection of left-sided pancreatic ductal adenocarcinoma: evolution and initial experience to a laparoscopic approach. Surg Endosc. 2010;24:1533–1541. doi: 10.1007/s00464-009-0806-7. [DOI] [PubMed] [Google Scholar]
- 18.Brody F, Richards NG. Review of robotic versus conventional laparoscopic surgery. Surg Endosc. 2014;28:1413–1424. doi: 10.1007/s00464-013-3342-4. [DOI] [PubMed] [Google Scholar]
- 19.Hyung WJ. [Robotic surgery in gastrointestinal surgery] Korean J Gastroenterol. 2007;50:256–259. [PubMed] [Google Scholar]
- 20.Abood GJ, Tsung A. Robot-assisted surgery: improved tool for major liver resections? J Hepatobiliary Pancreat Sci. 2013;20:151–156. doi: 10.1007/s00534-012-0560-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J. Robotic versus laparoscopic resection of liver tumours. HPB (Oxford) 2010;12:583–586. doi: 10.1111/j.1477-2574.2010.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Casciola L, Patriti A, Ceccarelli G, Bartoli A, Ceribelli C, Spaziani A. Robot-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc. 2011;25:3815–3824. doi: 10.1007/s00464-011-1796-9. [DOI] [PubMed] [Google Scholar]
- 23.Choi GH, Choi SH, Kim SH, Hwang HK, Kang CM, Choi JS, Lee WJ. Robotic liver resection: technique and results of 30 consecutive procedures. Surg Endosc. 2012;26:2247–2258. doi: 10.1007/s00464-012-2168-9. [DOI] [PubMed] [Google Scholar]
- 24.Choi SB, Park JS, Kim JK, Hyung WJ, Kim KS, Yoon DS, Lee WJ, Kim BR. Early experiences of robotic-assisted laparoscopic liver resection. Yonsei Med J. 2008;49:632–638. doi: 10.3349/ymj.2008.49.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E. Robotic liver surgery: results for 70 resections. Surgery. 2011;149:29–39. doi: 10.1016/j.surg.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Giulianotti PC, Sbrana F, Bianco FM, Addeo P. Robot-assisted laparoscopic extended right hepatectomy with biliary reconstruction. J Laparoendosc Adv Surg Tech A. 2010;20:159–163. doi: 10.1089/lap.2009.0383. [DOI] [PubMed] [Google Scholar]
- 27.Giulianotti PC, Sbrana F, Coratti A, Bianco FM, Addeo P, Buchs NC, Ayloo SM, Benedetti E. Totally robotic right hepatectomy: surgical technique and outcomes. Arch Surg. 2011;146:844–850. doi: 10.1001/archsurg.2011.145. [DOI] [PubMed] [Google Scholar]
- 28.Giulianotti PC, Tzvetanov I, Jeon H, Bianco F, Spaggiari M, Oberholzer J, Benedetti E. Robot-assisted right lobe donor hepatectomy. Transpl Int. 2012;25:e5–e9. doi: 10.1111/j.1432-2277.2011.01373.x. [DOI] [PubMed] [Google Scholar]
- 29.Holloway RW, Brudie LA, Rakowski JA, Ahmad S. Robotic-assisted resection of liver and diaphragm recurrent ovarian carcinoma: description of technique. Gynecol Oncol. 2011;120:419–422. doi: 10.1016/j.ygyno.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Ji WB, Wang HG, Zhao ZM, Duan WD, Lu F, Dong JH. Robotic-assisted laparoscopic anatomic hepatectomy in China: initial experience. Ann Surg. 2011;253:342–348. doi: 10.1097/SLA.0b013e3181ff4601. [DOI] [PubMed] [Google Scholar]
- 31.Lai EC, Tang CN, Li MK. Robot-assisted laparoscopic hemi-hepatectomy: technique and surgical outcomes. Int J Surg. 2012;10:11–15. doi: 10.1016/j.ijsu.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Machado MA, Makdissi FF, Surjan RC, Abdalla RZ. [First robotic-assisted laparoscopic liver resection in Latin America] Arq Gastroenterol. 2009;46:78–80. doi: 10.1590/s0004-28032009000100019. [DOI] [PubMed] [Google Scholar]
- 33.Panaro F, Piardi T, Cag M, Cinqualbre J, Wolf P, Audet M. Robotic liver resection as a bridge to liver transplantation. JSLS. 2011;15:86–89. doi: 10.4293/108680811X13022985131417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Lapalorcia LM, Casciola L. Laparoscopic and robot-assisted one-stage resection of colorectal cancer with synchronous liver metastases: a pilot study. J Hepatobiliary Pancreat Surg. 2009;16:450–457. doi: 10.1007/s00534-009-0073-y. [DOI] [PubMed] [Google Scholar]
- 35.Ryska M, Fronek J, Rudis J, Jurenka B, Langer D, Pudil J. [Manual and robotic laparoscopic liver resection. Two case-reviews] Rozhl Chir. 2006;85:511–516. [PubMed] [Google Scholar]
- 36.Vasile S, Sgarbură O, Tomulescu V, Popescu I. The robotic-assisted left lateral hepatic segmentectomy: the next step. Chirurgia (Bucur) 2008;103:401–405. [PubMed] [Google Scholar]
- 37.Wakabayashi G, Sasaki A, Nishizuka S, Furukawa T, Kitajima M. Our initial experience with robotic hepato-biliary-pancreatic surgery. J Hepatobiliary Pancreat Sci. 2011;18:481–487. doi: 10.1007/s00534-011-0388-3. [DOI] [PubMed] [Google Scholar]
- 38.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lai ECH, Tang CN, Li MKW. Conventional laparoscopic and robot-assisted laparoscopic liver resection for benign and malignant pathologies: A cohort study. J Rob Surg. 2012;6:295–300. doi: 10.1007/s11701-011-0311-6. [DOI] [PubMed] [Google Scholar]
- 41.Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic liver resection for hepatocellular carcinoma: short-term outcome. Am J Surg. 2013;205:697–702. doi: 10.1016/j.amjsurg.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 42.Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, Tsung A. Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg. 2012;16:2233–2238. doi: 10.1007/s11605-012-2040-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U. Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc. 2014;28:2973–2979. doi: 10.1007/s00464-014-3560-4. [DOI] [PubMed] [Google Scholar]
- 44.Tranchart H, Ceribelli C, Ferretti S, Dagher I, Patriti A. Traditional versus robot-assisted full laparoscopic liver resection: a matched-pair comparative study. World J Surg. 2014;38:2904–2909. doi: 10.1007/s00268-014-2679-8. [DOI] [PubMed] [Google Scholar]
- 45.Troisi RI, Patriti A, Montalti R, Casciola L. Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot. 2013;9:160–166. doi: 10.1002/rcs.1495. [DOI] [PubMed] [Google Scholar]
- 46.Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014;259:549–555. doi: 10.1097/SLA.0000000000000250. [DOI] [PubMed] [Google Scholar]
- 47.Wu YM, Hu RH, Lai HS, Lee PH. Robotic-assisted minimally invasive liver resection. Asian J Surg. 2014;37:53–57. doi: 10.1016/j.asjsur.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 48.Lai EC, Tang CN, Yang GP, Li MK. Multimodality laparoscopic liver resection for hepatic malignancy--from conventional total laparoscopic approach to robot-assisted laparoscopic approach. Int J Surg. 2011;9:324–328. doi: 10.1016/j.ijsu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 49.Croome KP, Yamashita MH. Laparoscopic vs open hepatic resection for benign and malignant tumors: An updated meta-analysis. Arch Surg. 2010;145:1109–1118. doi: 10.1001/archsurg.2010.227. [DOI] [PubMed] [Google Scholar]
- 50.Beal SM, Finch CF. An overview of retrospective case-control studies investigating the relationship between prone sleeping position and SIDS. J Paediatr Child Health. 1991;27:334–339. doi: 10.1111/j.1440-1754.1991.tb00414.x. [DOI] [PubMed] [Google Scholar]
- 51.Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 2011;13:295–308. doi: 10.1111/j.1477-2574.2011.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mizuguchi T, Kawamoto M, Meguro M, Shibata T, Nakamura Y, Kimura Y, Furuhata T, Sonoda T, Hirata K. Laparoscopic hepatectomy: a systematic review, meta-analysis, and power analysis. Surg Today. 2011;41:39–47. doi: 10.1007/s00595-010-4337-6. [DOI] [PubMed] [Google Scholar]
- 53.Rao A, Rao G, Ahmed I. Laparoscopic or open liver resection? Let systematic review decide it. Am J Surg. 2012;204:222–231. doi: 10.1016/j.amjsurg.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 54.Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: A meta-analysis. Hepatol Res. 2012;42:51–59. doi: 10.1111/j.1872-034X.2011.00890.x. [DOI] [PubMed] [Google Scholar]
- 55.Zhou YM, Shao WY, Zhao YF, Xu DH, Li B. Meta-analysis of laparoscopic versus open resection for hepatocellular carcinoma. Dig Dis Sci. 2011;56:1937–1943. doi: 10.1007/s10620-011-1572-7. [DOI] [PubMed] [Google Scholar]
- 56.Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol. 2012;18:6657–6668. doi: 10.3748/wjg.v18.i45.6657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yin Z, Fan X, Ye H, Yin D, Wang J. Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol. 2013;20:1203–1215. doi: 10.1245/s10434-012-2705-8. [DOI] [PubMed] [Google Scholar]
- 58.Wei M, He Y, Wang J, Chen N, Zhou Z, Wang Z. Laparoscopic versus open hepatectomy with or without synchronous colectomy for colorectal liver metastasis: a meta-analysis. PLoS One. 2014;9:e87461. doi: 10.1371/journal.pone.0087461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou Y, Xiao Y, Wu L, Li B, Li H. Laparoscopic liver resection as a safe and efficacious alternative to open resection for colorectal liver metastasis: a meta-analysis. BMC Surg. 2013;13:44. doi: 10.1186/1471-2482-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rao A, Rao G, Ahmed I. Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc. 2011;25:1603–1610. doi: 10.1007/s00464-010-1459-2. [DOI] [PubMed] [Google Scholar]
- 61.Rao AM, Ahmed I. Laparoscopic versus open liver resection for benign and malignant hepatic lesions in adults. Cochrane Database Syst Rev. 2013;5:CD010162. doi: 10.1002/14651858.CD010162.pub2. [DOI] [PubMed] [Google Scholar]
- 62.Kitisin K, Packiam V, Bartlett DL, Tsung A. A current update on the evolution of robotic liver surgery. Minerva Chir. 2011;66:281–293. [PubMed] [Google Scholar]
- 63.Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc. 1992;6:99. [Google Scholar]
- 64.Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, Caravaglios G. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777–784. doi: 10.1001/archsurg.138.7.777. [DOI] [PubMed] [Google Scholar]
- 65.Sugiyama Y, Ishizaki Y, Imamura H, Sugo H, Yoshimoto J, Kawasaki S. Effects of intermittent Pringle’s manoeuvre on cirrhotic compared with normal liver. Br J Surg. 2010;97:1062–1069. doi: 10.1002/bjs.7039. [DOI] [PubMed] [Google Scholar]
- 66.Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]


