Abstract
Background: We examined associations of material hardship with prepregnancy body mass index (BMI), gestational weight gain (GWG), and substantial postpartum weight retention (SPPWR; ≥5 kg at 1 year).
Methods: We studied 2128 women in Project Viva, a Boston-area cohort with recruitment during1999–2002. At recruitment, women reported whether they experienced material hardship, defined as having ever received public assistance, welfare, or lacked basic necessities (food, rent, or medical care) during childhood, in adulthood before pregnancy, and/or in pregnancy. We used multivariable logistic models adjusted for age, race/ethnicity, and parity (and prepregnancy BMI for GWG and SPPWR) to examine associations of material hardship with the three weight-related outcomes (BMI, GWG, and SPPWR).
Results: Mean age was 31.8 (standard deviation, 5.2) years; 66% of women were white, 16% were obese (prepregnancy BMI ≥30.0 kg/m2), 50% experienced excessive GWG, and 17% experienced SPPWR. Material hardship was most common during childhood (n=192, 9%), followed by adulthood (102, 5%), and pregnancy (41, 2%). Hardship in adulthood was associated with prepregnancy obesity (BMI ≥30 kg/m2 vs. 18.5 to <25.0 kg/m2), odds ratio ([OR] 2.35, 95% confidence interval [CI] 1.29, 4.31), but hardship in childhood was not (OR 1.26, 95% CI 0.80, 1.98). Hardship in childhood was associated with excess GWG (OR 1.45, 95% CI 0.99, 2.14), but hardship in adulthood or during pregnancy was not. We saw trends among hardship in each of the periods and associations with SPPWR, but all confidence intervals included the null.
Conclusion: The timing of hardship exposure may differently influence weight before, during, and after pregnancy.
Introduction
Substantial evidence suggests that living in poverty is associated with higher risk for overweight and obesity,1–4 a relationship that has been termed the “hunger–obesity paradox.5” Women appear to be especially at risk for obesity associated with the experience of poverty.6–10 For example, among homeless adults, the prevalence of obesity has been found to be approximately 50% higher among women compared with men.11,12 While socioeconomic factors such as neighborhood home values, college education, and household income explain the great majority (∼70%) of the variance in obesity among all adults, these factors are especially strong predictors of obesity among women compared with men.13
The childbearing years are a time of particular risk for weight gain, which predicts future obesity and cardiometabolic disease risk in women.14 Furthermore, excess weight entering pregnancy, excess weight gain during pregnancy, and substantial postpartum weight retention are each strong predictors of adverse short- and long-term outcomes for mother and infant, including future obesity.15,16 However, prior research examining relationships of poverty and food insecurity with weight during the peripartum period is limited.
In one study among 810 pregnant women in North Carolina,17 poor women living in a food insecure household (10% of the cohort) were at higher risk for severe pregravid obesity (body mass index [BMI] ≥35 kg/m2, adjusted odds ratio [OR] 2.97, 95% confidence interval [CI] 1.44–6.14), though the association with moderate obesity (BMI >29–35 kg/m2) was weaker (OR 1.53, 95% CI 0.68–3.43). After adjustment for prepregnancy BMI and other factors, women from food insecure households gained an average of 1.87 kilograms (95% CI 0.13–3.62) more during pregnancy than women from food secure household. However, in that study, food insecurity was assessed at a single time point; the sample size of women with food insecurity (n=79) was small, limiting power; and no data were available on weight after delivery. Another study among women enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children in Southern California showed that women living at less than 100% of the federal poverty level were more likely to experience excessive GWG during pregnancy (OR 1.13, 95% CI 1.05–1.20).18 The study was limited, however, by lack of information on important factors such as parity, physical activity, and smoking status. Limited data exist evaluating hardship during different life periods.
In the current study, we examined associations of material hardship, which we define as having ever received public assistance, received welfare, or lacked basic necessities (such as food, rent, or medical care) in childhood, in adulthood before pregnancy, or in the index pregnancy, with three outcomes: prepregnancy BMI category, gestational weight gain, and substantial postpartum weight retention. We hypothesized that material hardship exposure, in which women were exposed to aspects of poverty and food insecurity, would predict higher prepregnancy weight, gestational weight gain, and postpartumweight retention, and also that more proximate exposure in adulthood or pregnancy would be especially predictive. We additionally examined select behavioral mediators (such as sleep duration, new onset depression, and consumption of high calorie foods) of the relationships of material hardship with outcomes.
Methods and Procedures
Study population and design
Participants were enrolled in Project Viva, an ongoing, large, well-characterized, prebirth cohort study. We recruited women during their first prenatal visit at Harvard Vanguard Medical Associates, a multispecialty group practice in eastern Massachusetts. Details on study design and recruitment are reported in detail elsewhere.19 Eligibility criteria included gestational age <22 weeks at enrollment, singleton pregnancy, fluency in English, and intention to remain in the study area through delivery. All participants provided written informed consent, and the Harvard Pilgrim Health Care institutional review board approved the study.
In the current analysis we include all 2128 women with a live birth for our models predicting prepregnancy body mass index (BMI) and gestational weight gain (GWG). In our analyses of substantial postpartum weight retention (SPPWR), we limited our analysis to the 1303 women who provided information on weight at 1 year postpartum via questionnaire. Compared with the 825 excluded women, the 1303 women included in the SPPWR analysis were more likely to be white (74% vs. 54%) and college graduates (72% vs. 53%). Included women experienced slightly less hardship in adulthood (4% vs. 7%), but distributions of hardship were the same during childhood (9% vs. 9%) and pregnancy (2% vs. 2%).
Main exposure: Material hardship
At enrollment (median 9.9 weeks gestation) participants completed a self-administered questionnaire on which we asked whether they had “ever received public assistance, received welfare, or lacked basic necessities (such as food, rent, or medical care)?” during any of three time periods: (i) before age 18 years, or childhood; (ii) from age 18 until the current pregnancy, or adulthood; or (iii) during the current pregnancy. We used the yes/no material hardship responses to these three time periods as primary exposures.
Outcomes: Prepregnancy BMI, GWG, and SPPWR
Participants self reported their prepregnancy weight and height on questionnaires administered at study enrollment. Among 343 women who had weight recorded in the medical record in the 3 months before their last menstrual period, the association between self-reported and clinically measured weight was linear.20 Correlation coefficients (r=0.997 overall) and mean underreporting of weight (approximately 1 kg) did not differ by race/ethnicity, gestational age at study enrollment, prepregnancy BMI category, or history of hardship exposure.
We calculated prepregnancy BMI (kg/m2) and categorized it as underweight (<18.5 kg/m2), normal weight (18.5 to <25.0 kg/m2), overweight (25.0 to <30.0 kg/m2) or obese (≥30 kg/m2). We obtained prenatal weights from the clinical record, and calculated total GWG as the difference between the last weight recorded in the 4 weeks prior to delivery (mean 4 days, standard deviation [SD]=3) and prepregnancy weight. We categorized GWG as inadequate, adequate, or excessive, for each BMI category, according to the 1990 Institute of Medicine guidelines, which were the guidelines currently active when these Project Viva participants were pregnant.21 The outcomes for our GWG analysis were inadequate GWG and excessive GWG.
Participants self-reported their weight at 1 year postpartum on a mailed questionnaire. We defined substantial postpartum weight retention (SPPWR) as at least 5 kg higher weight at 1-year postpartum than prepregnancy, as we have done previously.22,23 As discussed previously, we found tight correlations between self-reported weights and clinically measured weights among women in this cohort.
Covariates
At the initial study visit each participant reported her race/ethnicity, parity, household income, partner status, smoking status, and whether she followed a vegetarian diet, via questionnaire and interview. We assessed maternal diet during the first and second trimesters of pregnancy and at 6 months postpartum using validated food frequency questionnaires,24,25 and estimated intake of total energy, dairy foods and beverages, fried foods, and trans fats. We queried television viewing and physical activity before, during, and after pregnancy and depressive symptoms and sleep duration after pregnancy, via questionnaires.22,23,26–28
Data analysis
As is common in large epidemiologic analyses, many participants were missing data on one or more covariates. We used a chained equations approach to impute missing values (the MI procedure in SAS) for the full cohort of 2128 live births for prepregnancy BMI and GWG, and for the 1303 women with information on PPWR.29 We generated 50 imputed datasets, and all model results were generated by combining these results.30 Among the 2128 observations, we used 24 imputed values for race/ethnicity, 24 for education, 25 for marital status, and 254 for household income. Distributions of variables were similar in imputed and nonimputed datasets.
In separate models, we examined hardship exposure during each of the three hardship exposure periods (childhood, adulthood, pregnancy) with each of the weight-related outcome periods (prepregnancy, gestation, and the postpartum period). For prepregnancy BMI analyses, we did not include material hardship during pregnancy as an exposure, since it would have occurred after the outcome. For each of the models, we compared women with hardship exposure versus without hardship exposure during that particular period. We also examined hardship as a four-category exposure: childhood only, adulthood only (including both before and during pregnancy for the GWG and SPPWR outcomes), both childhood and adulthood, or never.
We used multivariate logistic regression models to examine the extent to which each of these periods of hardship exposure were independently associated with prepregnancy BMI category, GWG category, and SPPWR. We used multinomial logistic regression analyses for the four-category BMI outcome (BMI <18.5 kg/m2, 25.0 to <30.0 kg/m2, or ≥30.0 kg/m2 as compared with the reference category 18.5 to <25.0 kg/m2) and for the three-category GWG outcome (inadequate or excessive as compared with the reference category of adequate weight gain). We first studied unadjusted associations (Model 0), and then we adjusted for maternal age, race/ethnicity, and parity (Model 1). For GWG and SPPWR outcomes, we additionally adjusted Model 1 for prepregnancy BMI, as both excessive GWG and SPPWR are more likely among obese women, and we were interested in the extent to which associations were mediated by BMI entering pregnancy. Models adjusting for the women's education level, marital status, and household income were also included in an additional step (Model 2), as these characteristics are likely to be strongly associated with material hardship.
We next considered whether measured behaviors might mediate associations of material hardship with each of the three outcomes. We focused on those behaviors that we have found to predict GWG and SPPWR in our previous work within this cohort. Thus, we included prepregnancy smoking status, physical activity, and television viewing as covariates in models predicting prepregnancy obesity; pregnancy physical activity, television viewing, and diet (vegetarian, sugar-sweetened beverages, dairy, fried foods, total energy) in models predicting GWG; and postpartum walking, trans fat intake, television viewing, sleep, and depression in models predicting SPPWR.22,23,26–28 In Project Viva, breastfeeding was not associated with SPPWR,22 and other studies have not substantiated this relationship,31 so we did not include it as a covariate. Accounting for these mediators did not result in significant changes in association of material hardship with our outcomes of interest, however, so we did not include this data in our tables.
We performed all analyses using SAS version 9.3 (Cary, NC).
Results
Among the 2128 Project Viva participants with a live birth, mean (SD) age was 31.8 years (5.2); 66% were white, 17% black, 7% Hispanic, 6% Asian, and 4% other race/ethnicity. Nineteen percent were former smokers and 13% smoked during the current pregnancy. Slightly more than half (52%) were parous.
Material hardship exposure was most common in childhood (n=192; 9%), followed by adulthood (102; 5%), and pregnancy (41; 2%). Women who were black or Hispanic were more likely to experience hardship during any period, but especially during adulthood or pregnancy (Table 1). Material hardship was also more common in women who were younger entering the index pregnancy, were parous, experienced depressive symptoms, or who smoked during pregnancy (Table 1). Women who reported material hardship in any of the periods watched more television, but also reported more physical activity. There were no substantial differences in diet or postpartum sleep duration by exposure group.
Table 1.
Characteristics of 2128 Women Enrolled In Project Viva, Overall and by Exposure to Material Hardship
| Experienced material hardship in | |||||
|---|---|---|---|---|---|
| Characteristics | Total | Childhood | Adulthood | Index pregnancy | Never experienced material hardship |
| n (%) or mean (SD) | |||||
| All | 2128 (100%) | 192 (9%) | 102 (5%) | 41 (2%) | 1852 (87%) |
| Maternal age (years) | 31.8 (5.2) | 29.8 (6.8) | 29.9 (7.6) | 26.4 (7.3) | 32.1 (5.2) |
| Race/ethnicity | |||||
| White | 1413 (66%) | 92 (48%) | 36 (35%) | 8 (19%) | 1295 (70%) |
| Black | 352 (17%) | 55 (29%) | 39 (38%) | 20 (48%) | 260 (14%) |
| Hispanic | 156 (7%) | 26 (13%) | 17 (16%) | 9 (21%) | 119 (6%) |
| Asian | 123 (6%) | 4 (2%) | 4 (4%) | 3 (8%) | 114 (6%) |
| Other | 84 (4%) | 15 (8%) | 7 (7%) | 1 (4%) | 64 (3%) |
| Nulliparous | |||||
| No | 1111 (52%) | 103 (54%) | 74 (72%) | 25 (61%) | 946 (51%) |
| Yes | 1017 (48%) | 89 (46%) | 28 (28%) | 16 (39%) | 905 (49%) |
| Smoking status | |||||
| Never | 1458 (69%) | 120 (62%) | 60 (59%) | 24 (59%) | 1287 (70%) |
| Former | 402 (19%) | 37 (19%) | 15 (15%) | 6 (16%) | 353 (19%) |
| During pregnancy | 268 (13%) | 36 (18%) | 26 (26%) | 11 (25%) | 212 (11%) |
| Before pregnancy | |||||
| Total physical activity (hours/week) | 9.9 (8.8) | 11.5 (12.1) | 12.3 (12.5) | 13.1 (11.0) | 9.6 (8.3) |
| TV watching (hours/week) | 11.5 (9.2) | 12.9 (11.5) | 14.5 (13.0) | 13.2 (13.7) | 11.3 (8.9) |
| During pregnancy | |||||
| Total energy (kcal/day) | 2115 (666) | 2199 (763) | 2200 (915) | 2080 (898) | 2104 (657) |
| Trans fat (g/day) | 2.2 (0.7) | 2.3 (0.8) | 2.5 (0.9) | 2.3 (0.9) | 2.2 (0.7) |
| Fried food away from home (servings/week) | 1.0 (0.8) | 1.1 (1.1) | 1.5 (1.5) | 1.2 (1.2) | 0.9 (0.8) |
| Total dairy (servings/day) | 2.9 (1.6) | 3.0 (1.9) | 2.8 (1.9) | 2.7 (2.0) | 2.9 (1.6) |
| Vegetarian diet, n (%) | 142 (7%) | 16 (8%) | 13 (13%) | 6 (15%) | 116 (6%) |
| Total physical activity (hours/week) | 7.5 (8.7) | 10.1 (14.7) | 10 (16.6) | 14.2 (17.1) | 7.1 (7.7) |
| TV watching (hours/week) | 12 (10.5) | 16.4 (16.4) | 15 (14.9) | 17.6 (19.0) | 11.4 (9.6) |
| Six months postpartum* | |||||
| Walking (hours/week) | 5.5 (7.6) | 6.5 (10.7) | 5.6 (12.4) | 7.8 (14.3) | 5.4 (7.2) |
| TV watching (hours/week) | 11.8 (12.6) | 15.2 (17.8) | 14.9 (20.9) | 16.2 (22.6) | 11.4 (11.9) |
| Sleep (hours/day) | 6.8 (1.6) | 6.8 (2.0) | 6.7 (2.8) | 7.2 (3.2) | 6.8 (1.5) |
| Incident postpartum depression | 73 (6%) | 16 (14%) | 4 (9%) | 2 (8%) | 55 (5%) |
| College graduate | |||||
| No | 753 (35%) | 109 (57%) | 77 (75%) | 33 (79%) | 581 (31%) |
| Yes | 1375 (65%) | 83 (43%) | 25 (25%) | 9 (21%) | 1271 (69%) |
| Household income >$70,000/year | |||||
| No | 896 (42%) | 114 (59%) | 88 (86%) | 40 (96%) | 709 (38%) |
| Yes | 1232 (58%) | 78 (41%) | 14 (14%) | 2 (4%) | 1143 (62%) |
| Married or cohabitating | |||||
| No | 183 (9%) | 39 (20%) | 22 (22%) | 20 (49%) | 125 (7%) |
| Yes | 1945 (91%) | 154 (80%) | 80 (78%) | 21 (51%) | 1727 (93%) |
| Breastfeeding duration (months)* | 5.8 (5.2) | 5.2 (5.6) | 5 (6) | 3.8 (5.4) | 5.9 (5.2) |
Among n=1303.
SD, standard deviation.
Mean (SD) prepregnancy BMI was 24.9 (5.6) kg/m2. Few women (4%) were underweight (BMI <18.5 kg/m2) entering pregnancy, while 22% were overweight (BMI 25.0 to <30.0 kg/m2) and 16% were obese (BMI ≥30 kg/m2) (Table 2). In unadjusted models, women who experienced hardship during childhood were more likely to be obese entering pregnancy (OR 1.57, 95% CI 1.02–2.41), but with adjustment for age, race/ethnicity, and parity, the association was attenuated (OR 1.26, 95% CI 0.80–1.98) (Table 2, Model 0). With adjustment for education, marital status, and household income, the association was attenuated slightly further (OR 1.12, 95% CI 0.71–1.78) (Table 2, Model 1).
Table 2.
Associations of Maternal Material Hardship with Prepregnancy BMI Category Among 2128 Women in Project Viva
| Prepregnancy body mass index (BMI) category | ||||||
|---|---|---|---|---|---|---|
| Underweight(BMI <18.5 kg/m2) | Overweight(BMI 25 to <30 kg/m2) | Obese(BMI ≥30 kg/m2) | ||||
| Odds ratio (95% confidence interval) vs. normal (BMI 18.5 to <25)b | ||||||
| Childhood hardship | Childhood hardship | Childhood hardship | ||||
| Modela | Yes (n=6) | No (n=75) | Yes (n=49) | No (n=413) | Yes (n=39) | No (n=297) |
| 0 | 0.99 (0.38–2.63) | 1.0 (reference) | 1.40 (0.95–2.06) | 1.0 (reference) | 1.57 (1.02–2.41) | 1.0 (reference) |
| 1 | 0.79 (0.29–2.16) | 1.0 (reference) | 1.25 (0.84–1.86) | 1.0 (reference) | 1.26 (0.80–1.98) | 1.0 (reference) |
| 2 | 0.75(0.27–2.08) | 1.0 (reference) | 1.20 (0.80–1.79) | 1.0 (reference) | 1.12 (0.71–1.78) | 1.0 (reference) |
| Adulthood hardship | Adulthood hardship | Adulthood hardship | ||||
|---|---|---|---|---|---|---|
| Yes (n=4) | No (n=77) | Yes (n=25) | No (n=437) | Yes (n=34) | No (n=302) | |
| 0 | 1.69 (0.53–5.41) | 1.0 (reference) | 1.79 (0.99–3.24) | 1.0 (reference) | 3.49 (1.98–6.16) | 1.0 (reference) |
| 1 | 1.32 (0.39–4.42) | 1.0 (reference) | 1.39 (0.76–2.57) | 1.0 (reference) | 2.35 (1.29–4.31) | 1.0 (reference) |
| 2 | 1.14 (0.34–3.87) | 1.0 (reference) | 1.28 (0.69–2.38) | 1.0 (reference) | 1.68 (0.91–3.11) | 1.0 (reference) |
Model 0, unadjusted; Model 1, adjusted for maternal age, race/ethnicity, and parity; Model 2, model 1 additionally adjusted for education, marital status, and household income
Sample sizes for normal BMI (18.5 to <25): childhood hardship, yes=97 and no=1151; adult hardship, yes=39 and no=1209.
BMI, body mass index.
Material hardship in adulthood before the index pregnancy, however, was associated with obesity after adjustment for maternal age, race/ethnicity and parity, (OR 2.35, 95% CI 1.29–4.31) (Table 2, Model 1). A model including adjustment for education, marital status, and household income, however, was attenuated and included the null (OR 1.68, 95% CI 0.91–3.11) (Model 2). Associations with prepregnancy overweight were in the same direction as for obesity, but weaker (e.g., adjusted OR 1.39, 95% CI 0.76–2.57 for hardship in adulthood) (Model 1). Hardship was not associated with prepregnancy underweight (Table 2), although confidence intervals were wide given the small number of underweight women.
Half (50%) of women had excessive GWG and 15% had inadequate GWG.21 Women with childhood material hardship were more likely to have excessive (vs. adequate) GWG in both unadjusted (OR 1.50, 95% CI 1.03–2.19) and adjusted (OR 1.45, 95% CI 0.99–2.14) models (Table 3, Models 0 and 1). A model additionally adjusting for education, marital status, and household income showed a similar association (OR 1.47, 95% CI 0.99–2.17) (Model 2). On the other hand, women with hardship exposure in adulthood were somewhat more likely to have inadequate GWG (OR 2.15, 95% CI 1.17–3.97), although that relationship was attenuated in models adjusted for maternal age, race/ethnicity, parity, and prepregnancy BMI (OR 1.55, 95% CI 0.81–2.96) as well as after additional adjustment for education, marital status, and household income (OR 1.44, 95% CI 0.75–2.78). Hardship in adulthood before or during pregnancy was not associated with excessive GWG (Table 3).
Table 3.
Associations of Material Hardship with Gestational Weight Gain Category (Institute of Medicine 1990) Among 2128 Women in Project Viva
| Gestational weight gain categoryOR (95% CI) vs. adequate GWGb | ||||
|---|---|---|---|---|
| Inadequate childhood hardship | Excessive childhood hardship | |||
| Modela | Yes (n=32) | No (n=287) | Yes (n=108) | No (n=954) |
| 0 | 1.48 (0.88–2.48) | 1.0 (reference) | 1.50 (1.03–2.19) | 1.0 (reference) |
| 1 | 1.26 (0.74–2.15) | 1.0 (reference) | 1.45 (0.99–2.14) | 1.0 (reference) |
| 2 | 1.23 (0.72–2.11) | 1.0 (reference) | 1.47 (0.99–2.17) | 1.0 (reference) |
| Adulthood hardship | Adulthood hardship | |||
|---|---|---|---|---|
| Yes (n=29) | No (n=290) | Yes (n=39) | No (n=1023) | |
| 0 | 2.15 (1.17–3.97) | 1.0 (reference) | 0.82 (0.48–1.39) | 1.0 (reference) |
| 1 | 1.55 (0.81–2.96) | 1.0 (reference) | 0.72 (0.41–1.26) | 1.0 (reference) |
| 2 | 1.44 (0.75–2.78) | 1.0 (reference) | 0.71 (0.40–1.25) | 1.0 (reference) |
| Pregnancy hardship | Pregnancy hardship | |||
|---|---|---|---|---|
| Yes (n=12) | No (n=307) | Yes (n=18) | No (n=1044) | |
| 0 | 2.47 (0.92–6.60) | 1.0 (reference) | 1.10 (0.45–2.69) | 1.0 (reference) |
| 1 | 1.91 (0.68–5.34) | 1.0 (reference) | 1.09 (0.43–2.76) | 1.0 (reference) |
| 2 | 1.82 (0.64–5.19) | 1.0 (reference) | 1.12 (0.44–2.88) | 1.0 (reference) |
Model 0: unadjusted; Model 1: adjusted for maternal age, race/ethnicity, parity and prepregnancy BMI; Model 2: model 1 additionally adjusted for education, marital status, and household income.
Sample sizes for adequate GWG: childhood hardship yes=52 and no=695, adult hardship yes=34 and no=714, pregnancy hardship yes=12 and no=735.
CI, confidence interval; GWG, gestational weight gain; OR, odds ratio.
We had information on weight at 1 year postpartum among 1303 women, of whom 219 (17%) retained at least 5 kg compared with their prepregnancy weight. In unadjusted models, women exposed to hardship during any of the three periods were more likely to have SPPWR than women not exposed to material hardship (childhood hardship OR 1.98, 95% CI 1.24–3.16; adulthood hardship OR 1.92, 95% CI 0.92–4.01; pregnancy hardship OR 3.06, 95% CI 1.16–8.11) (Table 4, Model 0). However, all estimates were attenuated toward the null with adjustment for age, race/ethnicity, parity, and prepregnancy BMI (Table 4, Model 1). Additional adjustment for educational, marital status, and household income resulted in only minimal additional attenuation (Table 4, Model 2). Of note, we ran a sensitivity analysis additionally adjusted for the number of people supported by the household income and results did not change for any of the outcomes examined.
Table 4.
Associations of Material Hardship with Weight Retention at 1 Year Postpartum Among 1303 Women in Project Viva
| Substantial postpartum weight retention at 1 year (≥5 kg vs. <5 kg)bOR (95% CI) | ||
|---|---|---|
| Childhood hardship | ||
| Modela | Yes (n=31) | No (n=188) |
| 0 | 1.98 (1.24, 3.16) | 1.0 (reference) |
| 1 | 1.43 (0.87, 2.37) | 1.0 (reference) |
| 2 | 1.34 (0.80, 2.25) | 1.0 (reference) |
| Adulthood hardship | ||
|---|---|---|
| Yes (n=13) | No (n=207) | |
| 0 | 1.92 (0.92, 4.01) | 1.0 (reference) |
| 1 | 1.44 (0.66, 3.15) | 1.0 (reference) |
| 2 | 1.22 (0.56, 2.69) | 1.0 (reference) |
| Pregnancy hardship | ||
|---|---|---|
| Yes (n=9) | No (n=211) | |
| 0 | 3.06 (1.16, 8.11) | 1.0 (reference) |
| 1 | 1.64 (0.56, 4.78) | 1.0 (reference) |
| 2 | 1.24 (0.41, 3.72) | 1.0 (reference) |
Model 0: unadjusted; Model 1: adjusted for maternal age, race/ethnicity, parity and pre-pregnancy BMI; Model 2: model 1 additionally adjusted for education, marital status, and household income
Sample sizes for no substantial postpartum weight retention (<5 kg): childhood hardship, yes=83 and no=1001; adult hardship yes=34 and no=1050; pregnancy hardship, yes=14 and no=1070.
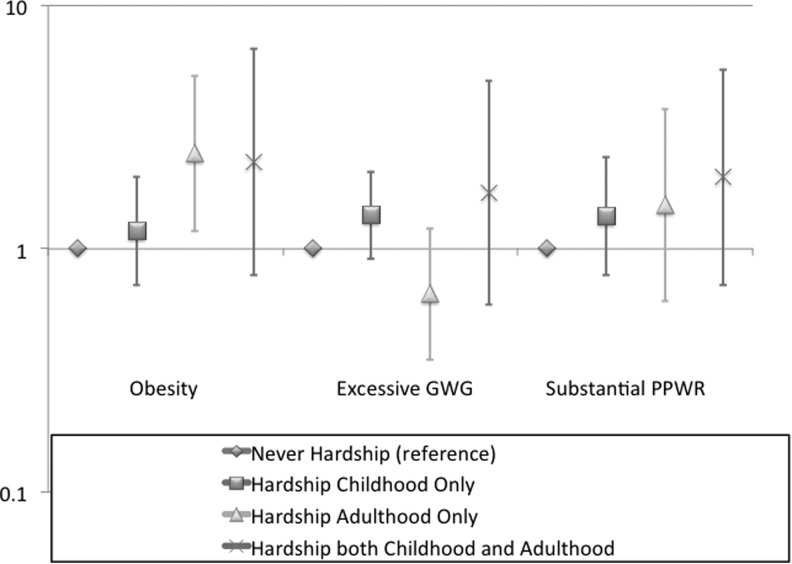
Figure 1 shows odds of obesity, excessive GWG, and SPPWR according to whether participants experienced hardship in childhood only, adulthood only, both childhood and adulthood, or never. The figure shows that odds of all outcomes tended to be more likely with hardship exposure, although the lone statistically significant finding was the association of hardship in adulthood only with prepregnancy obesity. We did not see strong evidence for an additive or multiplicative effect of hardship exposure during both childhood and adulthood (data not shown).
FIG. 1.
Odds of prepregnancy obesity, excessive gestational weight gain, and substantial postpartum weight retention according to the timing of material hardship exposure among women in the Project Viva cohort. The reference group for each analysis is women who never experienced material hardship. Error bars are 95% confidence intervals around the odds ratio. GWG, gestational weight gain; PPWR, postpartum weight retention.
Discussion
In this longitudinal cohort study, we found evidence that experience of material hardship throughout a woman's lifetime was associated with higher risks for excess weight entering pregnancy and weight gain during pregnancy. All effects were attenuated in adjusted models. Women with exposure to material hardship in adulthood were more likely to be obese entering pregnancy than women without exposure to material hardship. Women with childhood hardship exposure were more likely to experience excessive gestational weight gain, though hardship exposure in adulthood before pregnancy did not confer the same risk. Analyses of postpartum weight retention were limited by smaller sample size and thus lower power, but were suggestive of an association of hardship exposure during childhood or adulthood with SPPWR. Similarly, all analyses of women with hardship during pregnancy were limited by a small sample size of only 41 women with this exposure. While our sample of exposed women was relatively small, and thus confidence intervals were broad and many included the null, the consistent directions of the effect estimates suggest that the experience of hardship may influence weight independent of other measured behaviors and characteristics.
This study contributes to the literature in several important ways. We studied women enrolled in a prospective cohort representing a range of socioeconomic status and considered multiple potential confounding and mediating factors. To our knowledge, only one other cohort study has looked at associations of material hardship (specifically food insecurity) with peripartum weight, which focused on hardship experience during pregnancy.17 Other evidence also suggests that current household income has an inverse relationship with gestational weight gain.32 Our results suggest that hardship experiences before pregnancy, including in childhood, are also important in predicting excess weight, weight gain, and weight retention.
Several mechanisms are likely to be contributing to the observed associations. Women under financial stress may choose to consume less expensive but more calorie-dense processed foods.33 In a qualitative study among 21 overweight and obese low-income African American women, women chose foods high in fats and sugars because of taste, cost, and convenience, as well as misconceptions about the healthfulness of certain behaviors or foods.34 Also, fluctuations in food availability may cause people to eat more than they normally would when food is available, ultimately resulting in weight gain.35 Further, when diets are not consistently adequate, the body may compensate for periodic food shortages by becoming more efficient at storing more calories as fat.35 Additionally, financial insecurity may be associated with higher stress,36 more depressive symptoms, and sleep debt,36 although in our study we also did not find these factors mediated associations of hardship with postpartum weight retention.
Setting could be a factor: people faced with poverty are more likely to live in disadvantaged neighborhoods, and both opportunities for physical activity and the food environment track with neighborhood.37,38 However, lower socioeconomic status has been associated with obesity in such disparate settings as Seattle and Paris,39 as well as in developing countries, and supermarket proximity does not always predict where people shop,40 suggesting that factors such as differences in setting such as food environment and health care do not fully explain the relationship. In our study we found variable associations of physical activity and diet with material hardship, and adjustment for these behaviors did not substantially change observed associations.
In the present study we observed that women with hardship exposure in childhood were at somewhat higher risk for both excessive gestational weight gain and substantial postpartum weight retention compared with women without hardship exposure. These relationships were evident even when we examined women with hardship exposure only during childhood. Thus, the period of childhood hardship exposure (before the age of 18) may have been separated from the time of pregnancy (mean age at enrollment among women in the sample was 31.8 years) by many years. These findings could suggest an enduring effect of childhood hardship exposure on weight regulation. We are not aware of other studies that have examined this relationship in particular, although a robust literature connects early life exposures including nutrition and stress with later obesity risk.
Our study should be interpreted in light of several limitations. All women were recruited from a group practice in Eastern Massachusetts from 1999 to 2002 and all had either private or public health insurance during pregnancy, and represented mostly non-Hispanic white, married, educated, and fairly high income women. Results may not be generalizable to other populations. The sample of women with exposure to material hardship during each of the time periods was small, in particular during pregnancy when only 41 women reported hardship. The questionnaire inquiring about hardship has not been validated and could underestimate hardship exposure because of social stigma. We relied on self-reported prepregnancy weight, which may not be accurately reported; however, as we found and others have shown,41–43 self-report tends to be highly correlated with measured weight, and thus ranking is likely to have been preserved across women. Furthermore, the prevalence of obesity, excessive GWG, and SPPWR were each similar to estimates from many other studies conducted around the same period. We assessed hardship via questionnaire and it may be misreported; the direction of bias with the outcomes we studied is uncertain. One difficulty is our inability to detect the timing of the onset of hardship relative to the onset of prepregnancy overweight or obesity, precluding certainty about the direction of the association. Both prepregnancy and postpartum weights were self-reported, although we have found these measures to be highly correlated with measured weights. We are unable to isolate the independent effects of the different components of our material hardship variable (e.g., food insecurity vs. poverty vs. insufficient housing vs. overall stress). Further, we are unable to capture whether the women received public assistance such as supplemental nutrition assistance or access to public housing during their periods of hardship; variable access to assistance may explain some of the attenuation of effect of material hardship, and we are unable to parse this out in our sample.
This study adds to the extant literature on associations of poverty with obesity in several ways. We studied several weight-related measures in the peripartum period, each of which is an important predictor of both pregnancy outcomes and longer-term maternal and child health. We examined the relationships of discrete periods of material hardship exposure, in the past as well as during the index pregnancy. We accounted for depressive symptoms and obesogenic behaviors that we have previously found to predict these outcomes in our analyses, but these measured factors did not appear to explain the observed associations of hardship exposure with outcomes.
In conclusion, in unadjusted models, we found that women with material hardship in adulthood were more likely to be obese entering pregnancy, and women with hardship in childhood were more likely to have excessive gestational weight gain. Suggestive but nonstatistically significant associations were also seen for hardship exposure in both childhood and adulthood with risk for substantial postpartum weight retention. More research is needed to determine the pathways by which material hardship influences weight change across the life course; in particular, replicating this analysis in a cohort with a larger number of women exposed to material hardship may elucidate the relationships between maternal hardship and peripartum weight status. Nevertheless, these findings suggest that material hardship can have not only short-term but also longstanding influence on weight regulation. Since maternal peripartum weight is associated with offspring long-term weight regulation,16 programs and policies to promote financial well-being among girls and women throughout their lives may prevent obesity and its sequelae across multiple generations. Furthermore, caregivers may consider inquiring about financial security during visits with childbearing age women and offering referrals to appropriate social service agencies.
Acknowledgments
This study was funded by the U.S. National Institutes of Health (K24 HD069408, R37 HD 034568, P30 DK092924). The funders were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. We are indebted to the mothers and children of Project Viva for their generous participation, and appreciate the invaluable assistance of past and present Project Viva staff.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Brunner EJ, Marmot MG, Nanchahal K, et al. Social inequality in coronary risk: Central obesity and the metabolic syndrome. Evidence from the Whitehall II study. Diabetologia 1997;40:1341–1349 [DOI] [PubMed] [Google Scholar]
- 2.Molarius A, Seidell JC, Sans S, Tuomilehto J, Kuulasmaa K. Educational level, relative body weight, and changes in their association over 10 years: An international perspective from the WHO MONICA Project. Am J Public Health 2000;90:1260–1268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drewnowski A, Darmon N. The economics of obesity: Dietary energy density and energy cost. Am J Clin Nutr 2005;82:265S–273S [DOI] [PubMed] [Google Scholar]
- 4.Drewnowski A, Specter SE. Poverty and obesity: The role of energy density and energy costs. Am J Clin Nutr 2004;79:6–16 [DOI] [PubMed] [Google Scholar]
- 5.Scheier LM. What is the hunger-obesity paradox? J Am Diet Assoc 2005;105:883–884, 886. [DOI] [PubMed] [Google Scholar]
- 6.Beydoun MA, Wang Y. How do socio-economic status, perceived economic barriers and nutritional benefits affect quality of dietary intake among US adults? Eur J Clin Nutr 2008;62:303–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibson D. Long-term Food Stamp Program participation is positively related to simultaneous overweight in young daughters and obesity in mothers. J Nutr 2006;136:1081–1085 [DOI] [PubMed] [Google Scholar]
- 8.Gibson D. Food stamp program participation is positively related to obesity in low income women. J Nutr 2003;133:2225–2231 [DOI] [PubMed] [Google Scholar]
- 9.Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP. Food insecurity is positively related to overweight in women. J Nutr 2001;131:1738–1745 [DOI] [PubMed] [Google Scholar]
- 10.Martin KS, Ferris AM. Food insecurity and gender are risk factors for obesity. J Nutr Educ Behav 2007;39:31–36 [DOI] [PubMed] [Google Scholar]
- 11.Luder E, Ceysens-Okada E, Koren-Roth A, Martinez-Weber C. Health and nutrition survey in a group of urban homeless adults. J Am Diet Assoc 1990;90:1387–1392 [PubMed] [Google Scholar]
- 12.Koh KA, Hoy JS, O'Connell JJ, Montgomery P. The hunger-obesity paradox: Obesity in the homeless. J Urban Health 2012;89:952–964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drewnowski A, Rehm CD, Arterburn D. The geographic distribution of obesity by census tract among 59 767 insured adults in King County, WA. Int J Obes (Lond) 2014;38:833–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev 2000;22:261–274 [DOI] [PubMed] [Google Scholar]
- 15.Oken E, Kleinman KP, Belfort MB, Hammitt JK, Gillman MW. Associations of gestational weight gain with short- and longer-term maternal and child health outcomes. Am J Epidemiol 2009;170:173–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oken E. Maternal and child obesity: The causal link. Obstet Gynecol Clin North Am 2009;36:361–377, ix–x. [DOI] [PubMed] [Google Scholar]
- 17.Laraia BA, Siega-Riz AM, Gundersen C. Household food insecurity is associated with self-reported pregravid weight status, gestational weight gain, and pregnancy complications. J Am Diet Assoc 2010;110:692–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koleilat M, Whaley SE. Trends and predictors of excessive gestational weight gain among hispanic WIC participants in Southern California. Matern Child Health J 2013;17:1399–1404 [DOI] [PubMed] [Google Scholar]
- 19.Oken E, Baccarelli AA, Gold DR, et al. Cohort profile: Project Viva. Int J Epidemiol 2015:44:37–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oken E, Taveras EM, Kleinman KP, Rich-Edwards JW, Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol 2007;196:322..e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute of Medicine. Nutrition during pregnancy, vol I Washington, DC: National Academy Press, 1990 [Google Scholar]
- 22.Oken E, Taveras EM, Popoola FA, Rich-Edwards JW, Gillman MW. Television, walking, and diet: Associations with postpartum weight retention. Am J Prev Med 2007;32:305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gunderson EP, Rifas-Shiman SL, Oken E, et al. Association of fewer hours of sleep at 6 months postpartum with substantial weight retention at 1 year postpartum. Am J Epidemiol 2008;167:178–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fawzi WW, Rifas-Shiman SL, Rich-Edwards JW, Willett WC, Gillman MW. Calibration of a semi-quantitative food frequency questionnaire in early pregnancy. Ann Epidemiol 2004;14:754–762 [DOI] [PubMed] [Google Scholar]
- 25.Rifas-Shiman SL, Fawzi W, Rich-Edwards JW, Willett WC, Gillman MW. Validity of a semi-quantitative food frequency questionnaire (SFFQ) during early pregnancy. Paediatr Perinat Epidemiol 2000;14:A25–A26 [DOI] [PubMed] [Google Scholar]
- 26.Herring SJ, Rich-Edwards JW, Oken E, Rifas-Shiman SL, Kleinman KP, Gillman MW. Association of postpartum depression with weight retention 1 year after childbirth. Obesity (Silver Spring) 2008;16:1296–1301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oken E, Ning Y, Rifas-Shiman SL, Radesky JS, Rich-Edwards JW, Gillman MW. Associations of physical activity and inactivity before and during pregnancy with glucose tolerance. Obstet Gynecol 2006;108:1200–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stuebe AM, Oken E, Gillman MW. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. Am J Obstet Gynecol 2009;201:58..e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med 2011;30:377–399 [DOI] [PubMed] [Google Scholar]
- 30.Rubin DB. Multiple imputation for non response in surveys. New York: J. Wiley & Sons, 1987 [Google Scholar]
- 31.Oken E, Patel R, Guthrie LB, et al. Effects of an intervention to promote breastfeeding on maternal adiposity and blood pressure at 11.5 y postpartum: Results from the Promotion of Breastfeeding Intervention Trial, a cluster-randomized controlled trial. Am J Clin Nutr 2013;98:1048–1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sutherland G, Brown S, Yelland J. Applying a social disparities lens to obesity in pregnancy to inform efforts to intervene. Midwifery 2013;29:338–343 [DOI] [PubMed] [Google Scholar]
- 33.Dinour LM, Bergen D, Yeh MC. The food insecurity-obesity paradox: A review of the literature and the role food stamps may play. J Am Diet Assoc 2007;107:1952–1961 [DOI] [PubMed] [Google Scholar]
- 34.Reyes NR, Klotz AA, Herring SJ. A qualitative study of motivators and barriers to healthy eating in pregnancy for low-income, overweight, African-American mothers. J Acad Nutr Diet 2013;113:1175–1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Center on Hunger and Poverty. The paradox of hunger and obesity in America. Available at www.nufs.sjsu.edu/clariebh/Hunger%20and%20Obesity.pdf Accessed February25, 2014
- 36.Laraia BA, Siega-Riz AM, Gundersen C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr 2006;136:177–182 [DOI] [PubMed] [Google Scholar]
- 37.Hurvitz PM, Moudon AV, Rehm CD, Streichert LC, Drewnowski A. Arterial roads and area socioeconomic status are predictors of fast food restaurant density in King County, WA. Int J Behav Nutr Phys Act 2009;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children's neighborhoods. Soc Sci Med 2010;71:584–591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Drewnowski A, Moudon AV, Jiao J, Aggarwal A, Charreire H, Chaix B. Food environment and socioeconomic status influence obesity rates in Seattle and in Paris. Int J Obes (Lond) 2014;38:306–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drewnowski A, Aggarwal A, Hurvitz PM, Monsivais P, Moudon AV. Obesity and supermarket access: Proximity or price? Am J Public Health 2012;102:e74–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Paez KA, Griffey SJ, Thompson J, Gillman MW. Validation of self-reported weights and heights in the avoiding diabetes after pregnancy trial (ADAPT). BMC Med Res Methodol 2014;14:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brunner Huber LR. Validity of self-reported height and weight in women of reproductive age. Matern Child Health J 2007;11:137–144 [DOI] [PubMed] [Google Scholar]
- 43.Lin CJ, DeRoo LA, Jacobs SR, Sandler DP. Accuracy and reliability of self-reported weight and height in the Sister Study. Public Health Nutr 2012;15:989–999 [DOI] [PMC free article] [PubMed] [Google Scholar]