Pharm2Pharm is a new service model funded by the Centers for Medicare & Medicaid Services (CMS) Innovation Center that aims to improve care and reduce costs by leveraging the unique expertise of pharmacists to optimize medications across care settings. This model is called “Pharm2Pharm” because of the collaboration between hospital and community pharmacists as patients are being discharged and transition home. Approximately 2,500 patients who are at risk of medication-related hospitalization and emergency department (ED) use in Hawai‘i have been enrolled in Pharm2Pharm statewide. Initially, this model was launched in the three rural counties of Hawai‘i, where physician shortages are more severe.1 This service model has since been expanded to Honolulu County in areas with the highest preventable hospitalization rates.2 This article describes the key elements of the Pharm2Pharm model, the health information technology currently supporting the program, and the economics necessary to sustain this new model of medication management.
The Pharm2Pharm Model
Pharm2Pharm aims to address medication problems among complex, high risk patients during care transitions and for up to one year post-discharge to ensure their medications are optimized and that patients are actively self-managing. During care transitions, common medication problems include unresolved medication discrepancies, patient confusion about which home medications to resume and which to discontinue, and adjustments needed due to diet and activity changes from hospital to home. Once in the community, the patient can experience medication problems due to lack of coordination among prescribers, lack of medication expertise (eg, regarding medications to avoid in the elderly), inadequate monitoring, and barriers to medication adherence. The Pharm2Pharm model aims to improve patient health, improve the healthcare system, and reduce total costs of care. Pharm2Pharm is funded by a Health Care Innovation Award through the CMS Innovation Center.
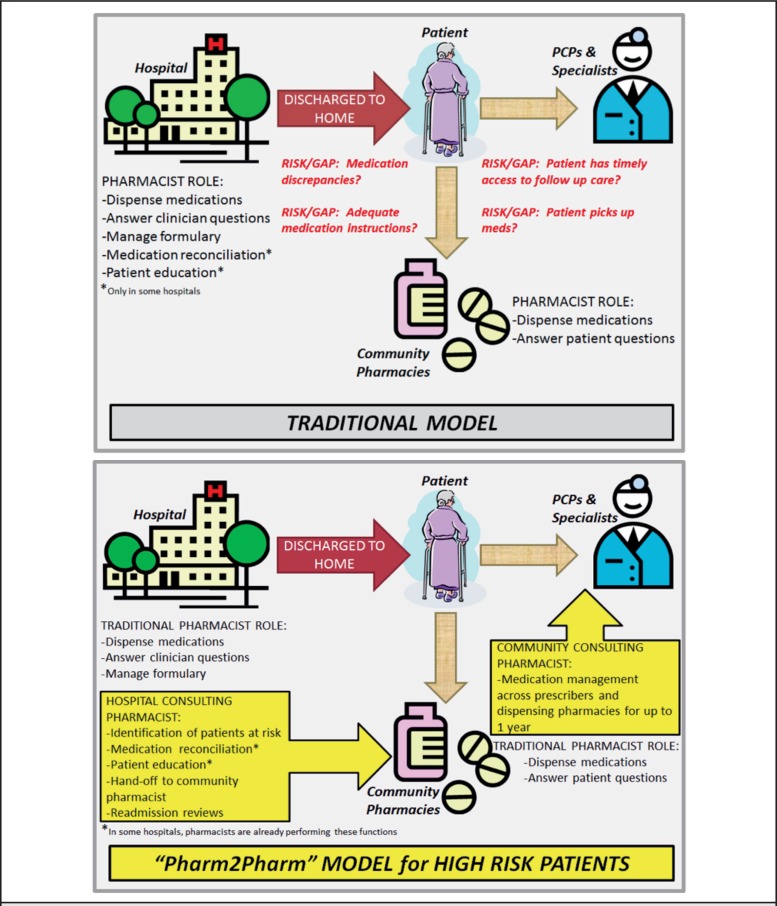
Pharm2Pharm began with the vision of the founding leaders of the Hawai‘i Community Pharmacist Association (HCPA), a network of independent, not publicly traded pharmacies in Hawai‘i, to move underutilized community pharmacists out of traditional, reactive, isolated roles and into proactive, integrated, targeted roles that are completely independent of dispensing. In the dispensing role, pharmacists wait for prescriptions to come in, fill them, and offer counseling on the dispensed medications (Figure 1). Medication counseling is often provided without access to relevant patient-specific clinical information, as pharmacists are peripheral to the healthcare providers treating the patient. In Pharm2Pharm, hospital-based and community-based “consulting pharmacists” find high risk patients, gather relevant clinical information, and systematically identify and resolve drug therapy problems in collaboration with the patient and members of the care team. While this role shift has already occurred in some integrated, closed healthcare systems, Pharm2Pharm project partners have demonstrated that this model can be implemented across care settings regardless of the patient's insurance coverage, primary care provider, or dispensing pharmacies.
Figure 1.
Traditional Pharmacist Roles Compared to Pharm2Pharm Roles
In the Pharm2Pharm model, the hospital consulting pharmacist (HCP) screens new hospital admissions for patients who are at risk for medication-related problems and who will be discharged home (or to short-term rehabilitation, then home). Specific enrollment criteria are described in the Pharm2Pharm Standard Operating Procedure manual3 and focus on the following evidence-based risk factors:
Number of medications (the greater the number, the greater the risk, especially among the elderly)4
Type of medications (warfarin, oral antiplatelet agents, insulins, oral hypoglycemic agents, opioid analgesics, and digoxin are the most commonly involved medications in emergency admissions among older adults)5
Previous acute care use (ie, hospitalization or ED visit) due to medication problems.6
Once eligibility is determined, the HCP begins educating the patient about their medications and encourages patients to work with a community consulting pharmacist (CCP) after discharge. Patients select the CCP they would like to work with and an appointment is scheduled within three days of discharge. The HCP reconciles the patients' medications and works to resolve any drug therapy problems prior to discharge. Within a day of discharge, the HCP calls each patient to ensure the patient has obtained the correct medications and knows which medications to take and which not to take and to remind them of their appointments with the CCP and with their follow-up provider. The HCP sends care transition documents to the CCP and sends written notification of enrollment to the patient's primary care provider. Finally, the HCP reviews any readmissions to determine if the admission was potentially preventable and medication-related. If so, model enhancements, additional training, and other improvements are considered to prevent future recurrence.
While most care transition programs focus on the 30-day post-discharge period, the CCP follows Pharm2Pharm patients on a case-by-case basis during the one-year period after discharge. Extending the CCP support beyond the 30-day post-discharge period is critical for these complex patients because it takes time to optimize medications. It also takes time to fully educate patients about their medications and for them to gain competency and efficacy in self-care management. Stress experienced in the hospital setting (eg, sleep disturbance, poor nutrition, discomfort, inactivity) can affect cognitive functioning and complicate recovery after discharge.7
At each visit, the CCP completes the following procedures sequentially:
Reconciles medications to ensure there is a complete and accurate list of what the patient is taking and is currently prescribed, including over-the-counter medications (OTCs), herbal medicines, and supplements.
- Checks each medication for:
- indication,
- effectiveness in achieving the clinical goals,
- safety and side effects, and
- proper adherence
Checks for any untreated conditions for which drug therapy is indicated.
Notifies prescribers of any updates to the medication list.
Works to resolve any drug therapy problems through patient education, adherence counseling, and/or making recommendations to prescribers.
The CCP is the outpatient medication expert who is responsible for coordinating medications and systematically resolving drug therapy problems across prescribers and across dispensing pharmacies — an important role for optimally managing complex, high risk patients.
Hawai‘i Pacific Health and Hawai‘i Health Systems Corporation have been collaborating partners in Pharm2Pharm implementation, launching patient enrollment from several of their hospitals.
The Health Information Technology Supporting Pharm2Pharm
Initially, the Pharm2Pharm model was implemented without health information technology (IT) so that key technology needs could be clearly identified and defined based on experience with the model. Hawai‘i Health Information Exchange (HHIE) has the infrastructure to support Health Information Exchange (HIE) state-wide and across payers and providers and has been a key project partner in facilitating assessment and implementation of targeted health IT. The following technology is now in use:
All written communications among HCPs and CCPs (including care transition documents) are sent via HHIE secure email rather than fax. An increasing number of physicians have requested that the consulting pharmacists use HHIE instead of fax when sending written communications.
HCS Med 360 is a software solution used to support medication reconciliation. This technology allows the consulting pharmacists to rapidly query over a dozen national databases and see the patient's prescription fill history as well as gaps in the fill history. Experience to date shows that this robust system captures all prescription medications in Hawai‘i except those filled at Kaiser or the VA and those paid 100% self pay. The consulting pharmacist then completes the reconciliation process and produces a current medication list, including OTC medications, herbals, and supplements. The fill history and complete medication list are being built so that this information can be included in the patient's HHIE Community Health Record.
Language Access Network, a virtual translation service currently in use at most hospitals in Hawai‘i, is now available to CCPs so that patients with language barriers can enroll into Pharm2Pharm.
An electronic registry has been implemented via HHIE allowing consulting pharmacists to easily manage their Pharm2Pharm patients. The registry automatically verifies and transfers information among different technology tools, thus reducing data entry time and errors.
The HHIE Community Health Record is now being used by consulting pharmacists to access patient labs and other clinical information to support medication management. The Community Health Record allows real-time patient data from the hospitals and laboratories to be viewed securely through a single portal, reducing the need to refer to paper records received through mail, fax and other less efficient means.
In Hawai‘i, this is the first time that health IT has been implemented on a state-wide basis and integrates community pharmacists into care teams outside of integrated health systems.
Why Now?
Given how frequently medication problems are at the root of hospitalization and ER visits, why hasn't this model been implemented previously? There are two primary reasons: workforce shortages and limited reimbursement for clinical pharmacy services.
Nationwide there has been a severe pharmacist shortage with projections of the shortage worsening.8 However, given that the Doctor of Pharmacy degree has been in high demand by students who seek a health profession, there has been a corresponding growth in the number of colleges of pharmacy and subsequently the pharmacists shortage has eased.9 The other barrier is inadequate compensation for pharmacist services other than dispensing. As noted in a 2011 report to the US Surgeon General, compensation is severely lagging for these roles: “Pharmacists are increasingly requested by many health systems, providers, and primary care teams to improve outcomes and delivery of care. However, in terms of pharmacist services, as the complexity or level of clinical service increases, the revenue generation potential is reduced. This is in stark contrast to the clinical services provided by other health professionals.”10 The Health Care Innovation Award has provided funding for both HCPs and CCPs in Hawai‘i. However, this funding source is time-limited and must be replaced by other sources for these pharmacists to continue providing Pharm2Pharm services.
The Economics of Pharm2Pharm
Pharm2Pharm is not a randomized controlled trial, so scientific conclusions about effectiveness are limited. However, qualitative and quantitative analyses are underway by the project team and independently by the CMS Innovation Center. In addition, previous research has demonstrated that pharmacists, deployed strategically, can add significant value to the healthcare system. For example, Fairview Health Services in Minnesota integrated pharmacists into several primary care clinics and examined the impact on quality and cost. Compared to a control group, patients receiving medication management services from these pharmacists were more likely to meet criteria for hypertension and cholesterol management. In addition, the total cost of care for the patients receiving these services decreased by more than 30% even though the cost of patients' prescription medications increased almost 20%.11 The cost of hospitalizations and ED use decreased nearly 60%. The types of mediation problems found and corrected by the pharmacists in the Minnesota study shed light on the cost impact. The most common problem found was the patient needed additional medication for an untreated indication (more than 5 times as common as needing to discontinue an unnecessary medication). In addition to indication problems, these pharmacists also addressed effectiveness, safety, and adherence problems.11 This demonstrates that pharmacists focused on getting patients on the right medications (not necessarily the cheapest medications) can save costs overall by preventing much more expensive acute care use.
Pharm2Pharm was designed to achieve similar results outside of an integrated healthcare system by targeting high risk inpatients and improving medication management from discharge to home.
The following are key facts pertaining to the sustainability of the Pharm2Pharm model:
HCP enrollment volume: In hospitals with adequate infrastructure and support, each full-time HCP can enroll and hand-off over 20 patients per month. Placing an HCP in the hospital is an efficient and effective way to find high cost, high risk patients and get them on a path toward medication optimization and lower acute care costs. Additionally, HCPs provide specialized patient education and resolve discrepancies missed by other clinicians. In Hawai‘i, seven hospitals have participated in the Pharm2Pharm model.
Community pharmacy payment: The payment to community pharmacies for providing this comprehensive medication management service in the current model is $695 per patient per year. For patients who exit the service early, the payments are prorated to a lower amount. HCPA-member pharmacies have provided the CCP services in the Pharm2Pharm model.
Baseline hospital cost per patient: The average baseline acute care cost of Pharm2Pharm patients prior to their enrollment and handoff to a CCP is over $26,000 per patient per year (these data are based on actual inpatient, observation, and ER charges provided by Hawai‘i Health Information Corporation, with a 0.385 cost-to-charge ratio applied per CMS methodology, a common approach that uses hospital charges to estimate acute care cost).12
Since the launch of the Daniel K. Inouye College of Pharmacy, the supply of pharmacists in Hawai‘i has greatly improved. If deployed strategically, this workforce can extend the short supply of physicians and add unique medication expertise to the healthcare system. Stakeholders here in Hawai‘i and nationally have an opportunity now to leverage pharmacist expertise by integrating them into teams across the continuum of care.
Acknowledgement
The project described is supported by Funding Opportunity Number CMS-1C1-12-0001 from Centers for Medicare and Medicaid Services, Center for Medicare and Medicaid Innovation. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of HHS or any of its agencies.
References
- 1.Hawaii/Pacific Basin Area Health Education Center, author. Workforce. [March 19, 2015]. http://www.ahec.hawaii.edu/?page_id=79.
- 2.Healthcare Association of Hawaii, author. Honolulu County Community Health Needs Assessment July 3, 2013. [March 19, 2015]. http://hah.org/wp-content/uploads/2013/12/hah.hi_chna_final_report_honolulu_county_-_generic.pdf.
- 3.Pharm2Pharm Standard Operating Procedures, version May 6, 2014. Daniel K. Inouye College of Pharmacy; [Google Scholar]
- 4.Petrovic M, van der Cammen T, Onder G. Adverse drug reactions in older people — detection and prevention. Drugs & Aging. 2012;29(6):453–462. doi: 10.2165/11631760-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365:2002–2012. doi: 10.1056/NEJMsa1103053. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet-Zamponi D, d'Arailh L, Konrat C, Delpierre S, Lieberherr D, Lemaire A, Tubach F, Lacaille S, Legrain S. Drug-related readmissions to medical units of older adults discharged from acute geriatric units — results of the optimization of medication in AGEd multicenter randomized controlled trial. Journal of the American Geriatrics Society. 2013;61(1):113–121. doi: 10.1111/jgs.12037. [DOI] [PubMed] [Google Scholar]
- 7.Krumholz HM. Post-hospital syndrome — an acquired, transient condition of generalized risk. New England Journal of Medicine. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Adequacy of Pharmacist Supply: 2004–2030. US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions; 2008. Dec, [Google Scholar]
- 9.Pellegrin KL, Pezzuto JM. Strategic direction for high demand degrees: an analysis of the US pharmacy degree competitive market. International Journal of Management in Education. 2011;5(2/3):285–300. [Google Scholar]
- 10.Giberson S, Yoder S, Lee MP. Improving Patient and Health System Outcomes through Advanced Pharmacy Practice. A Report to the U.S. Surgeon General. Office of the Chief Pharmacist. U.S. Public Health Service; 2011. Dec, [Google Scholar]
- 11.Isetts BJ, Schondelmeyer SW, Artz MB, Lenarz LA, Heaton AH, Wadd WB, Brown LM, Cipolle RJ. Clinical and economic outcomes of medication therapy management services: The Minnesota experience. J Am Pharm Assoc. 2008;48:203–214. doi: 10.1331/JAPhA.2008.07108. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services, author. Cost-to-Charge Ratios. [March 19, 2015]. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/outlier.html.