In an era of rising co-pays, patients with cancer want cost-of-treatment discussions, and these conversations do not lead to negative feelings in the majority of patients.
Abstract
Purpose:
As one solution to reducing costs and medical bankruptcies, experts have suggested that patients and physicians should discuss the cost of care up front. Whether these discussions are possible in an oncology setting and what their effects on the doctor-patient relationship are is not known.
Methods:
We used the National Comprehensive Cancer Network (NCCN) Guidelines and the eviti Advisor platform to show patients with metastatic breast, lung, or colorectal cancer the costs associated with their chemotherapy and/or targeted therapy options during an oncology consultation. We measured provider attitudes and assessed patient satisfaction when consultations included discussion of costs.
Results:
We approached 107 patients; 96 (90%) enrolled onto the study, three (3%) asked if they could be interviewed at a later date, and eight (7%) did not want to participate. Only five of 18 oncologists (28%) felt comfortable discussing costs, and only one of 18 (6%) regularly asked patients about financial difficulties. The majority of patients (80%) wanted cost information, and 84% reported that these conversations would be even more important if their co-pays were to increase. In total, 72% of patients responded that no health care professional has ever discussed costs with them. The majority of patients (80%) had no negative feelings about hearing cost information.
Conclusion:
In an era of rising co-pays, patients with cancer want cost-of-treatment discussions, and these conversations do not lead to negative feelings in the majority of patients. Additional training to prepare clinicians for how to discuss costs with their patients is needed.
Introduction
As a result of the significant treatment advances in the last decade, the number of cancer survivors in the United States will increase from 13.8 million in 2010 to 18.1 million in 2020.1 Unfortunately, with great progress also comes increased costs, and cancer care expenditure is soaring, with costs expected to increase from $125 billion in 2010 to at least $173 billion in 2020.1 With drug prices now commonly exceeding $5,000 to 10,000 a month2,3 and expensive end-of-life care becoming more intensive,4 the current system is unsustainable.5 Medical bankruptcies are increasing; patients with cancer are twice as likely to file for bankruptcy as people without cancer, and younger patients appear particularly vulnerable to “financial toxicities.”6 The current marketplace and the Affordable Care Act have led to an increase in high-deductible health plans, which may exacerbate the significant financial hardships experienced by patients with expensive chronic conditions such as cancer.7
We know that most physicians recognize their obligations to help control costs.8 Most doctors, however, feel ill prepared to discuss costs with their patients because they either do not know the costs or do not have the training.9 The primary objective of this study was to learn if it was possible for patients and oncologists to discuss treatment costs in real time and to determine whether these discussions upset patients.
Methods
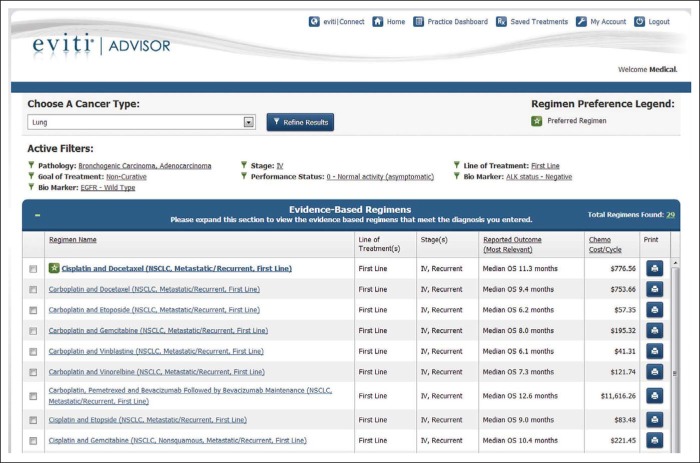
We approached 107 patients with previously treated metastatic breast, lung, or colorectal cancer who were either on active treatment or surveillance about participating in the study between February 2013 and October 2013. Each week, we identified patients by contacting participating providers to provide a list of eligible patients attending their clinic. All the physicians who contributed were faculty members at Johns Hopkins specializing in the treatment of these malignancies. If patients were to receive news of disease progression during their consultation or if their doctor felt they were too unwell, then we did not approach them at that time, but many of these patients were invited to participate at a later date. At the time of registration, every patient received information about the study and signed a consent form in the presence of a member of the study team. Patients completed a baseline questionnaire evaluating their need for cost of treatment information before their consultation. At the end of the clinical encounter, all participating providers were asked to discuss with their patients whether they had any financial difficulties with their treatments to date. Physicians did not receive formal training but were provided with a prescripted text to help them introduce cost discussions and were aware that patients had been approached to participate before their appointment. Chemotherapy and targeted therapy costs for evidence-based National Comprehensive Cancer Network (NCCN) metastatic regimens for breast, lung, or colorectal cancer were provided to the patient by their oncologist during the consultation using the Web-based eviti Advisor oncology decision-support platform (Figure 1). The eviti system shows the outcomes and cost per cycle of the evidence-based regimens appropriate for the cancer type, pathology, biomarkers, treatment intent (curative/noncurative), and line of treatment. The cost shown includes both treatment and supportive care drugs. For purposes of benchmarking and comparison, cost is based on the average sales price +6 (for infused chemotherapy agents, community-based oncologists are paid at the average sale price plus a 6% mark up under Medicare Part B). Both doctors and patients could see and discuss the costs of care. It was explained to patients that the costs shown were not their personal responsibility but rather the cost of drugs to the health care system and that the costs did not take into account other considerations such as facility fees, co-pays for ancillary drugs (eg, ondansetron), their deductible status, or other out-of-pocket costs.
Figure 1.
Sample screenshot of first-line treatment options and the costs per chemotherapy cycle for stage IV non–small-cell lung cancer as generated by the eviti Advisor system. The costs include both treatment and supportive care drugs and represent what the patient and/or insurer would be billed for the treatment.
The primary objective was to assess the satisfaction ratings among prescribers and patient's when the cost of chemotherapy was introduced into the doctor-patient relationship. We measured satisfaction using questions adapted from the Satisfaction with Decision Scale.10 We measured needs for cost information during the consultation using questions adapted from a needs assessment questionnaire for patients with cancer.11 Items most relevant to communication and involvement in decision making and endorsed as important by more than 20% of the patients in the original study were included.12 We asked subjects to rate communication about costs during the consultation using questions adapted from a validated questionnaire on communication in serious illness.13 Subjects ranked their level of need for cost information during the consultation using questions adapted from a goals questionnaire for patients with serious illness.14 A protocol amendment adding an additional question to evaluate whether rising copays or deductibles would affect a patient's need for cost information was included after 32 patients had enrolled.
Statistics
We originally planned to enroll 150 patients with metastatic cancer (50 breast, 50 lung, and 50 colorectal cancers) and to summarize our results via descriptive statistics. The introduction of a new electronic medical record to our institution substantially decreased patient flow and accrual, so we examined the data with the first 96 patients. The results indicated that with the accrual of 50 more patients no substantial differences would have been observed. With 96 patients, precision (half-width of a 95% CI) of proportions is 10% instead of 8% with 150 patients.
Results
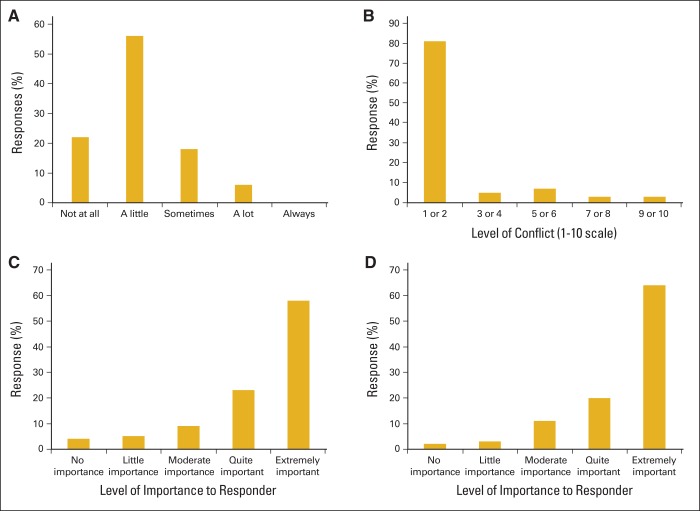
Before interviewing patients, we questioned 18 oncology specialists about how often they discuss cost of treatments with their patients (Figure 2). No physician said they always discussed costs with patients, and only one (6%) admitted to frequently asking patients. Ten physicians (55%), said they discuss costs a little, and three (17%) reported they sometimes discuss costs. Significantly, four oncologists (22%) reported that they never ask patients about costs of treatment. Only five physicians (28%) felt comfortable discussing costs with patients.
Figure 2.
The frequency, importance, and impact of cost of care discussions between physicians and patients, as indicated by responses to (A) How frequently do you discuss costs of treatment with patients? (B) Level of conflict when discussing costs with providers. (C) Importance of understanding what patient will be responsible for paying. (D) Importance of advance notices for increases in copayment.
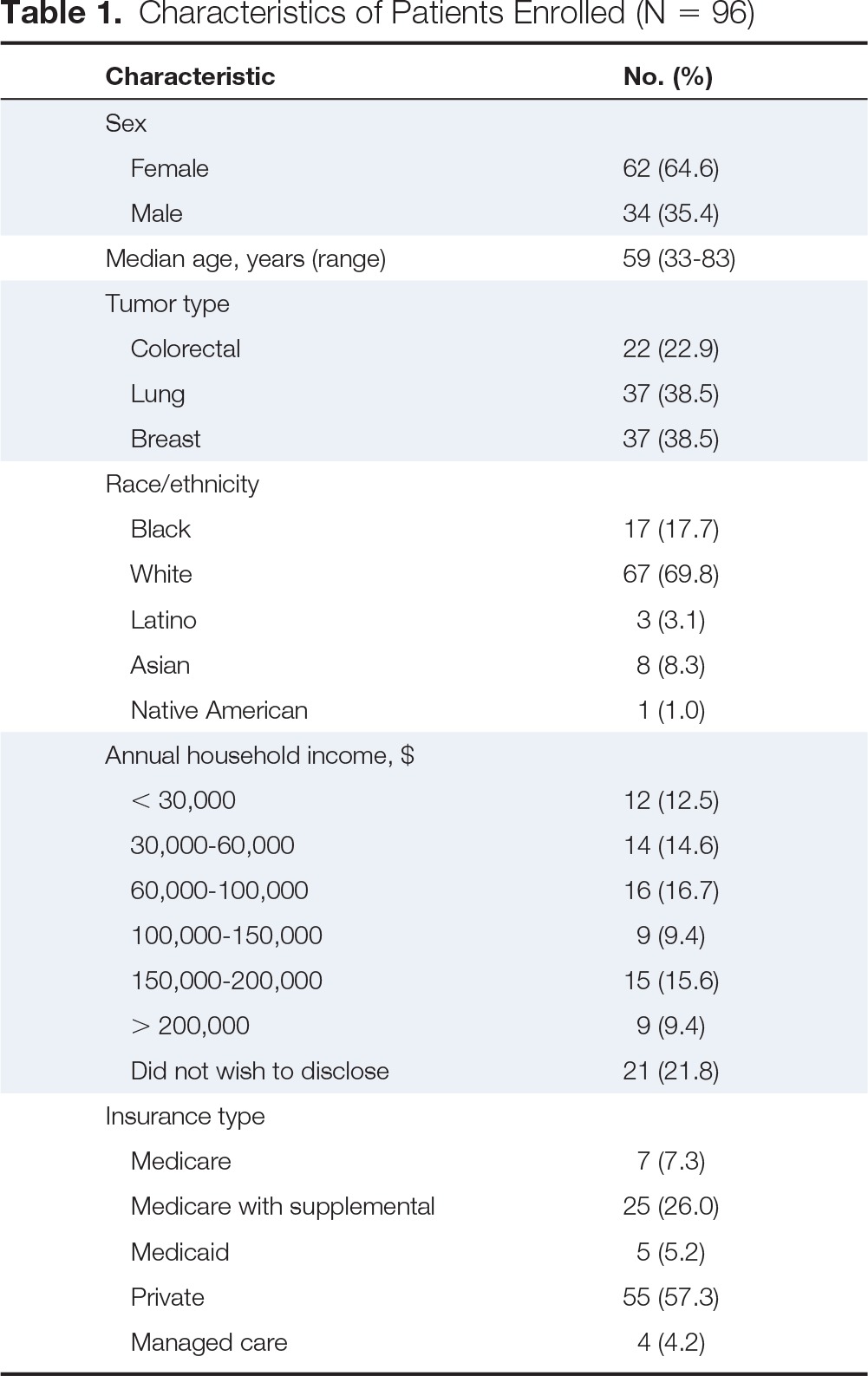
We approached 107 patients about participating in the study, and 96 (90%) gave written consent. Only eight (7%) did not want to participate, and three (3%) asked if they could complete the questionnaire during their next clinic appointment because of personal time constraints. Patient characteristics are described in Table 1. Over 80% (78 of 96) of respondents reported that it is “quite important” or “extremely important” for them to know what they will be personally responsible for paying (Figure 2). A similar percentage of patients (81.2%) reported that they felt no negative feelings or conflicts (graded 1-2 on 10-point Likert scale) when they discussed cost of treatments with their oncologist, saying financial discussions were a “normal part of life” (Figure 2). Surprisingly 72% of patients reported that no health care professional had ever discussed costs with them for any medical problem. When asked “If in the future you have to pay more of a co-pay or a deductible than you do now, how important would it be for you to know upfront how much you would be responsible for paying?” the majority (54 of 64; 84%) of patients felt that they would like upfront cost discussions about the implications such increases would have on their out-of-pocket expenses (Figure 2). Of note, 15 of 18 oncologists (83%) stated that the NCCN clinical practice guidelines should include costs.
Table 1.
Characteristics of Patients Enrolled (N = 96)
| Characteristic | No. (%) |
|---|---|
| Sex | |
| Female | 62 (64.6) |
| Male | 34 (35.4) |
| Median age, years (range) | 59 (33-83) |
| Tumor type | |
| Colorectal | 22 (22.9) |
| Lung | 37 (38.5) |
| Breast | 37 (38.5) |
| Race/ethnicity | |
| Black | 17 (17.7) |
| White | 67 (69.8) |
| Latino | 3 (3.1) |
| Asian | 8 (8.3) |
| Native American | 1 (1.0) |
| Annual household income, $ | |
| < 30,000 | 12 (12.5) |
| 30,000-60,000 | 14 (14.6) |
| 60,000-100,000 | 16 (16.7) |
| 100,000-150,000 | 9 (9.4) |
| 150,000-200,000 | 15 (15.6) |
| > 200,000 | 9 (9.4) |
| Did not wish to disclose | 21 (21.8) |
| Insurance type | |
| Medicare | 7 (7.3) |
| Medicare with supplemental | 25 (26.0) |
| Medicaid | 5 (5.2) |
| Private | 55 (57.3) |
| Managed care | 4 (4.2) |
Discussion
In this study, we provided actual cost of drug per cycle information using the eviti Advisor system to oncology patients and their doctors. We have demonstrated that patients do want to know the costs of their treatment, and that these costs are not being routinely discussed in academic medicine. In addition, we show that there are minimal conflicts and no harm to the doctor-patient relationship when costs are introduced. Our results show that patients want to discuss costs now and even more so if they are asked to bear more of the cost responsibility in the form of higher co-pays or deductibles.
Access to high-quality cancer care for all Americans is the goal of recent legislation. Unfortunately patients with cancer who cannot pay for their treatment have worse outcomes for the same diseases.15,16 Additional research addressing insurance- and cost-related barriers to cancer care is a critical component of efforts to ensure that all patients benefit from the progress achieved in recent years. We do know that medical bankruptcy rates are increasing and younger patients seem particularly at risk from cancer-related financial toxicity.6 A greater emphasis on the shared decision-making process involving upfront cost discussions with an emphasis on personal cost responsibility combined with evidence-based outcomes should empower patients to make better educated choices and may ultimately help bend the cost curve downward.
Our study has several weaknesses, including the small sample size and the fact that it is a single-institution study. Because it was not possible for this study to generate the final out-of-pocket expenses for patients, we concentrated on the larger simple question: can we even discuss costs of drugs with patients in the clinic? We did not have resources to audio-tape clinical encounters, and although each provider was educated via a standardized script as to how to introduce costs, we cannot comment on what physicians told their patients about chemotherapy expenses. Professional interviewers were not used. We did not assess patient comprehension. Our questionnaires may have had some ceiling effects.
There are, however, some strengths to the study as well. We concentrated on simple yet important questions: can we discuss treatment costs in the clinic, and will the discussion disrupt the patient-physician relationship? Our broad inclusion criteria, together with a variety of educational, racial, and economic backgrounds as well as differing insurance coverage, suggest that these data represent a real-world oncology clinic and the interactions that take place on a daily basis in a large academic cancer center. Five health care professionals conducted all the patient-doctor surveys using a standard questionnaire and met on a weekly basis in an effort to ensure consistency across the study team. Our results are straightforward and understandable.
Oncologists are increasingly aware of escalating treatment costs,5 most notably for targeted and immunotherapeutic agents, and are now tasked with discussing them with patients.17 Significant difficulties that will need to be addressed are that cost information is not routinely available, patient out-of-pocket expenses vary considerably, doctors feel poorly trained to discuss costs with patients, and these discussions take time. To ensure the delivery of high-quality cancer care, patients and their families must be knowledgeable about their illnesses and prognoses, so they can make informed decisions about their care.18,19 Increasingly, this will include costs. Patients often believe they can be cured when cure is not possible,20 but the evidence shows that patients with advanced cancer and their families prefer to receive accurate and truthful information about their illnesses.21
The Affordable Care Act and the individual mandate have made the cost of health care front and center news in the United States. A national conversation, guided by the best information and decision aids22 including costs embedded in the ASCO, NCCN, and other guidelines, aimed at explicit understanding of choices, tradeoffs, and expectations is needed. The ASCO Value in Cancer Care Task Force is currently in the process of developing an algorithm to determine the relative value of cancer drugs. The first therapies being evaluated include those for advanced non–small-cell lung cancer, prostate cancer, and multiple myeloma. This much-needed approach will define the clinical benefit as defined by overall or progression-free survival in addition to quality of life improvement, toxicity profile, and costs associated with drug administration. Now more than ever before, patients should be empowered to ask their physicians about their therapeutic options and to understand the personal financial implications of the recommended treatments.
Acknowledgment
Supported by a National Comprehensive Cancer Network Young Investigator Award (R.J.K.) and by National Cancer Institute Grant No. P 30 006973 to Sidney Kimmel Comprehensive Cancer Center.
Authors' Disclosures of Potential Conflicts of Interest
Disclosures provided by the authors are available with this article at jop.ascopubs.org.
Author Contributions
Conception and design: Ronan J. Kelly, Patrick M. Forde, Arlene A. Forastiere, Gary L. Rosner, Thomas J. Smith
Financial support: Ronan J. Kelly, Thomas J. Smith
Administrative support: Ronan J. Kelly, Thomas J. Smith
Provision of study materials or patients: Ronan J. Kelly, Patrick M. Forde, Shereef M. Elnahal, Arlene A. Forastiere, Thomas J. Smith
Collection and assembly of data: Ronan J. Kelly, Patrick M. Forde, Shereef M. Elnahal, Thomas J. Smith
Data analysis and interpretation: Ronan J. Kelly, Patrick M. Forde, Shereef M. Elnahal, Gary L. Rosner, Thomas J. Smith
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Patients and Physicians Can Discuss Costs of Cancer Treatment in the Clinic
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Ronan J. Kelly
Consulting or Advisory Role: Novartis, Eli lilly, Clovis Oncology
Patrick M. Forde
Research Funding: Novartis, BMS
Travel, Accommodations, Expenses: Celgene, Astra-Zeneca, Seattle Genetics
Shereef M. Elnahal
No relationship to disclose
Arlene A. Forastiere
Employment: eviti
Stock or Other Ownership: eviti
Gary L. Rosner
Stock or Other Ownership: Pfizer, Johnson & Johnson, Walgreens
Honoraria: Novartis
Travel, Accommodations, Expenses: Novartis
Thomas J. Smith
Stock or Other Ownership: United Healthcare
References
- 1.Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103:117–28. doi: 10.1093/jnci/djq495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bach PB. Limits on Medicare's ability to control rising spending on cancer drugs. N Engl J Med. 2009;360:626–633. doi: 10.1056/NEJMhpr0807774. [DOI] [PubMed] [Google Scholar]
- 3.Hillner BE, Smith TJ. Efficacy does not necessarily translate to cost effectiveness: A case study in the challenges associated with 21st-century cancer drug pricing. J Clin Oncol. 2009;27:2111–2113. doi: 10.1200/JCO.2008.21.0534. [DOI] [PubMed] [Google Scholar]
- 4.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–477. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shih YC, Ganz PA, Aberle D, et al. Delivering high-quality and affordable care throughout the cancer care continuum. J Clin Oncol. 2013;31:4151–4157. doi: 10.1200/JCO.2013.51.0651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 2013;32:1143–1152. doi: 10.1377/hlthaff.2012.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wharam JF, Ross-Degnan D, Rosenthal MB. The ACA and high-deductible insurance–Strategies for sharpening a blunt instrument. N Engl J Med. 2013;369:1481–1484. doi: 10.1056/NEJMp1309490. [DOI] [PubMed] [Google Scholar]
- 8.Tilburt JC, Wynia MK, Sheeler RD, et al. Views of US physicians about controlling health care costs. JAMA. 2013;310:380–388. doi: 10.1001/jama.2013.8278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schrag D, Hanger M. Medical oncologists' views on communicating with patients about chemotherapy costs: A pilot survey. J Clin Oncol. 2007;25:233–237. doi: 10.1200/JCO.2006.09.2437. [DOI] [PubMed] [Google Scholar]
- 10.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: The satisfaction with decision scale. Med Dec. 1996;16:58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 11.Tamburini M, Gangeri L, Brunelli C, et al. Assessment of hospitalised cancer patients' needs by the Needs Evaluation Questionnaire. Ann Oncol. 2000;11:31–37. doi: 10.1023/a:1008396930832. [DOI] [PubMed] [Google Scholar]
- 12.Tamburini M, Gangeri L, Brunelli C, et al. Cancer patients' needs during hospitalisation: A quantitative and qualitative study. BMC Cancer. 2003;3:12. doi: 10.1186/1471-2407-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: Increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32:1484–1488. doi: 10.1097/01.ccm.0000127262.16690.65. [DOI] [PubMed] [Google Scholar]
- 14.Hawkins NA, Ditto PH, Danks JH, et al. Micromanaging death: Process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45:107–117. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- 15.Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. The Lancet Oncology. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 16.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 17.Meropol NJ, Schrag D, Smith TJ, et al. American Society of Clinical Oncology guidance statement: The cost of cancer care. J Clin Oncol. 2009;27:3868–3874. doi: 10.1200/JCO.2009.23.1183. [DOI] [PubMed] [Google Scholar]
- 18.Ganz PA, Levit LA. Charting a new course for the delivery of high-quality cancer care. J Clin Oncol. 2013 doi: 10.1200/JCO.2013.53.7993. [DOI] [PubMed] [Google Scholar]
- 19.Peppercorn JM, Smith TJ, Helft PR, et al. American Society of Clinical Oncology statement: Toward individualized care for patients with advanced cancer. J Clin Oncol. 2011;29:755–760. doi: 10.1200/JCO.2010.33.1744. [DOI] [PubMed] [Google Scholar]
- 20.Weeks JC, Mack JW, Schrag D. Talking with patients about dying. N Engl J Med. 2013;368:480–481. doi: 10.1056/NEJMc1214249. [DOI] [PubMed] [Google Scholar]
- 21.Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: Patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34:81–93. doi: 10.1016/j.jpainsymman.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 22.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Data Syst Rev. 2011;10:CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]