Abstract
BACKGROUND
Information on travel distance and time to care for children with birth defects is lacking. We examined factors associated with travel distance and time to cleft care among children with orofacial clefts.
METHODS
In 2006, a mail/phone survey was administered in English and Spanish to all resident mothers of children with orofacial clefts born 2001 to 2004 and identified by the North Carolina birth defects registry. We analyzed one-way travel distance and time and the extent to which taking a child to care was a problem. We used multivariable logistic regression to examine the association between selected sociodemographic factors and travel distance (≤60 miles and >60 miles) and time (≤60 min and >60 min) to cleft care.
RESULTS
Of 475 eligible participants, 51.6% (n = 245) responded. Of the respondents, 97.1% (n = 238) were the child’s biological mother. Approximately 83% (n = 204) of respondents were non-Hispanic White; 33.3% (n = 81) were college educated; and 50.0% (n = 115) had private health insurance. One-way mean and median travel distances were 80 and 50 miles, respectively (range, 0–1058 miles). One-way mean and median travel times were 92 and 60 min, respectively (range, 5 min to 8 hr). After adjusting for selected sociodemographics, travel distance varied significantly by maternal education, child’s age, and cleft type. Travel time varied significantly by child’s age. Approximately 67% (n = 162) reported taking their child to receive care was not a problem.
CONCLUSION
Approximately 48% of respondents traveled > 1 hr to receive cleft care. Increasing access to care may be important for improving health outcomes among this population.
Keywords: barriers to care, health care accessibility, travel time, travel distance, cleft lip, cleft palate, orofacial clefts
INTRODUCTION
Orofacial clefts (OFC) are one of the most common birth defects found in infants born in the United States (Parker et al., 2010). This type of birth defect affects an infant’s face and mouth and occurs when the lip or roof of the mouth does not form properly during fetal development (Dixon et al., 2011). Children with OFC can be born with a cleft palate, cleft lip, or cleft lip with cleft palate. Annually, in the United States, 2651 infants are born with a cleft palate, and 4437 infants are born with a cleft lip with or without a cleft palate (Parker et al., 2010).
Children with OFC may have trouble with speech development and feeding and may require specialized management and treatment, such as speech therapy, and dental and orthodontic care. Access to these services for affected families is an important area of study. In a meeting of experts convened by the Centers for Disease Control and Prevention (CDC), identifying barriers to care among children with OFC was noted as an important public health research priority (Yazdy et al., 2007). Although results from the National Survey of Children with Special Health Care Needs have shown that children with special health care needs encounter more obstacles accessing care than children without special needs (McPherson et al., 2004; Newacheck and Kim, 2005; Skinner and Slifkin, 2007; Strickland et al., 2009), information on barriers to care for children with birth defects, a subset of children with special health care needs, are lacking.
Population-based studies on barriers to care, specifically for families who have children with birth defects, like OFC, are needed (Yazdy et al., 2007; Strauss and Cassell, 2009; Wehby and Cassell, 2010; Cassell et al., 2012). According to a recent review of the literature, adequate access to care, costs, and coordination of services are concerns for mothers of children with OFC (Nelson et al., 2012). In a qualitative assessment on perceived barriers to care among children with OFC in North Carolina, which used a state-wide, population birth defects registry, the authors found that structural barriers, such as accessing health services, was a concern for mothers of children with OFC (Cassell et al., 2012).
Only a few studies have specifically examined geographic barriers for children with birth defects using birth defects registry data, which examined the location of services and its effect on survival and health service use (Case et al., 2008; Cassell et al., 2009; Fixler et al., 2012). For children with OFC, only a few studies have examined geographic barriers to primary cleft and craniofacial care among children with OFC. The first study was conducted in Maryland in the early 1980s and included questions on mean distance traveled to care (White, 1981). Another study used Florida Birth Defects Registry data to track the use of state-wide treatment centers among children with OFC. Birth defects registry data were linked to the use of cleft and craniofacial centers and were mapped to describe the percentage of families in each county that came into contact with craniofacial centers (Williams et al., 2003).
Two studies examined access to dental care in children with special health care needs, including children with OFC. One study found that geographic barriers to dental care were a problem for children with special health care needs (Al Agili et al., 2004). The other study examined barriers to dental care for children with special health care needs and compared results across several primary diagnoses categories. The authors found that children with a primary diagnosis of a craniofacial anomaly like OFC were impacted by a greater number of environmental barriers (e.g., cost of care and accessibility of care) and nonenvironmental barriers (e.g., child’s behavior and competing demands) than children with other primary diagnoses, except for cerebral palsy (Nelson et al., 2011). Although the study by Nelson et al. (2011) examined difficulties traveling to access dental care, neither of these studies focused on children with birth defects and did not specifically examine travel distance and time to care.
To our knowledge, no recent study has measured geographic barriers, such as distance and time traveled to and from specialized health care providers, using both state birth defects registry and survey data, specifically for families of children with OFC. Our study sought to address these gaps in knowledge by determining oneway travel distance and time to receive primary cleft or craniofacial care for families of children with OFC and the extent to which taking a child to cleft and craniofacial care was perceived as a problem. We also examined selected sociodemographic factors associated with travel time and distance to primary cleft care.
MATERIALS AND METHODS
Study Population
For this study, live-born children with OFC were identified using the North Carolina Birth Defects Monitoring Program (NCBDMP). The NCBDMP is a state-wide, active population-based birth defects registry that includes all resident live births, fetal deaths, and therapeutic abortions at any gestational age. The NCBDMP covers all North Carolina hospitals and includes approximately 120,000 resident births per year (NBDPN, 2011). Using the NCBDMP, we identified all infants born in North Carolina from January 1, 2001, through December 31, 2004, and who were diagnosed with an OFC during their first year of life. Infants with OFC were identified by the NCBDMP using the British Pediatric Association codes 749.000 to 749.290. Because we were interested in distance to care and travel times in North Carolina for the past 12 months, we excluded mothers whose child with OFC had died at any point or lived out-of-state. We excluded those that died at any point by matching with death certificates.
Survey Instrument
A combination mail/phone survey instrument in both English and Spanish was developed, pilot-tested, and distributed between May and October of 2006. The survey, a recruitment letter, and a fact sheet about the study were mailed to all mothers of identified children with OFC. After 1 month, nonresponders were sent a second mailing, and in some cases, a third mailing was sent 1 month later. Nonrespondents after two or three mailings were followed-up by phone. A $10 gift card to a major retail store was sent to all participants who completed the survey.
The survey instrument was composed of 76 open- and closed-ended questions. Of these questions, 39 were slightly modified from a validated “barriers to care” questionnaire, which was developed through a literature review, focus groups, and cognitive interviews of both English- and Spanish-speaking parents of children with chronic health conditions (Seid et al., 2004). Questions on the overall survey covered various financial, structural, and personal barriers. The survey included questions about demographics, health services use, knowledge and use of craniofacial centers and/or teams, receipt of medical care (including primary craniofacial care), reasons why care was not received, advantages/disadvantages of their primary craniofacial care venue, and satisfaction with care (Seid et al., 2004; Cassell et al., 2012).
In addition to asking questions about problems accessing medical care, we asked participants open-ended questions about their average one-way travel distance and distance to take their child to receive primary cleft and craniofacial care. For travel distance, we asked respondents: “On average, how far do you have to travel for your child with facial difference to receive primary craniofacial care (ONE-WAY TRIP)?” For travel time, we asked: “On average, how much time does it take you to travel with your child with facial difference to receive primary cleft care (ONEWAY TRIP)?” Travel distance and time were measured in miles and minutes, respectively. Survey respondents also were asked to what extent it was a problem, if any, to take their child with facial differences to receive primary cleft or craniofacial care.
Definition of Variables and Outcomes Examined
Sociodemographic measures
Several sociodemographic variables were measured. Maternal demographics included age, education, race/ethnicity, marital status, job status, annual household income, and number of children with special health care needs living in the household, excluding the child with OFC. Child characteristics examined included age, race/ethnicity, preterm birth, birth weight, primary health insurance, sex, cleft type, and presence of other anomalies in addition to the OFC. All sociodemographic data were taken directly from the self-reported survey except for the child’s sex, cleft type, presence of other anomalies, preterm birth, and low birth weight, which were obtained from the NCBDMP data.
To assess any sociodemographic differences in those that responded and those that did not respond to the survey, we analyzed the following variables that were available and collected in the same manner from the NCBDMP: maternal age, maternal education, maternal race/ethnicity, child’s sex, child’s age, cleft type, presence of other birth defects, preterm birth, and low birth weight.
Child’s primary health insurance categories were collapsed to private, public, and military. Private health insurance was defined as enrollment in the State Employee Health Plan or a private health insurance plan purchased from an employer or directly from an insurance company. Public health insurance was defined as enrollment in one of the following insurance plans: North Carolina Health Choice (the State Children’s Health Insurance Program), Medicaid, Carolina ACCESS or Health Check. Military insurance was defined as having insurance through Civilian Health and Medical Program of the Uniformed Services, TRICARE (formerly Civilian Health and Medical Program of the Uniformed Services), or the Veteran’s Administration.
Race/ethnicity categories included on the survey were: White, Hispanic, Black/African-American, American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, and an open-ended “Other” category. Survey respondents were able to select all that apply. For analysis, we created a mutually exclusive race/ethnicity variable with categories of “non-Hispanic White” and “Other” due to small numbers. Thirteen respondents selected more than one race category. These 13 respondents selected White as one of those categories and did not check Hispanic. These 13 respondents were recoded into the non-Hispanic White category.
Outcomes: satisfaction with and accessing care
Potential responses to the question of to what extent it was a problem, if any, to take their child with facial differences to receive primary cleft or craniofacial care included: “not a problem,” “small problem,” “somewhat of a problem,” and “big problem.” This question was based on a validated “barriers to care” questionnaire (Seid et al., 2004). Due to small numbers, these responses were collapsed into two categories: “not a problem” and “any problem.”
We also examined satisfaction with care and whether or not primary cleft and craniofacial care worked well for the child in the last 12 months. For satisfaction, we used a Likert-scale of “very satisfied,” “satisfied,” “neither satisfied or dissatisfied,” “dissatisfied,” and “very dissatisfied.” Due to small numbers, we collapsed these into two categories: (1) “very satisfied” and “satisfied”; and (2) “neither satisfied or dissatisfied,” “dissatisfied,” and “very dissatisfied.” For whether or not primary cleft and craniofacial care worked well during the last 12 months, we used a Likert-scale of “never,” “almost never,” “sometimes,” “often,” and “almost always,” based on the same validated “barriers to care” questionnaire (Seid et al., 2004). Due to small numbers, we collapsed these into three categories: (1) “often” and “almost always” worked well; (2) “sometimes” worked well; and (3) “never” and “almost never” worked well.
Outcomes: travel distance and time
We examined maternal report of one-way travel distance in miles and one-way travel time in min. Mean, median, ranges, and total travel distance and time were reported. One-way travel distance and time were categorized based on frequency distributions, meaningful cut-points for analyses, and the literature on distance and time to medical care for birth defects and other medical conditions, such as cancer (Kuehn et al., 2007; Case et al., 2008; Huang et al., 2009; Henry et al., 2011; Fixler et al., 2012; Pinto et al., 2012). Travel distance was analyzed in four categories, 0 to 30 miles, 31 to 60 miles, 61 to 90 miles, and greater than 90 miles. Travel time also was measured in four categories: 0 to 30 min, 31 to 60 min, 61 to 90 min, and greater than 90 min. Due to small numbers, for the multivariable analyses, travel distance was collapsed into 0 to 60 miles (reference) and greater than or equal to 61 miles, and travel time was collapsed into 0 to 60 min (reference) and greater than or equal to 61 min.
Statistical Analyses
Descriptive analyses were conducted using respondents’ sociodemographic data from the survey and from the NCBDMP, where relevant. Bivariate analyses were also conducted to determine one-way travel distance and time, stratified by cleft type and the presence of other birth defects. We also used bivariate analyses to examine the extent to which taking a child to cleft and craniofacial care was a problem. Chi-square analyses were conducted to determine significance level using a p-value of 0.05. Where appropriate, we used Fisher’s exact test to account for small cell counts.
Logistic regression was used to calculate crude and adjusted odds ratios (aOR) and 95% confidence intervals (CI) to determine if the selected sociodemographic factors were associated with one-way travel distance and time. All the selected sociodemographic variables were included in the final logistic regression models. We used logistic regression due to the binary nature of our outcomes, travel distance and time.
Data were analyzed using SAS 9.3 (SAS Institute, Inc., Cary, NC). This study was approved by the North Carolina Division of Public Health Institutional Review Board and the University of North Carolina at Chapel Hill Public Health and Nursing Institutional Review Board.
RESULTS
Of the 478 initially eligible participants, three (0.6%) were excluded due to incomplete survey data after the survey was distributed. Of 475 eligible participants, 230 (48.4%) did not respond to the survey (nonrespondents): 205 (89.1%) were lost to follow-up, and 25 (10.9%) were contacted but refused to participate for a variety of reasons (e.g., child’s death and parent denial of child having an OFC). Thus, the final study sample consisted of 245 eligible respondents (51.6% of the 475 subjects), of which 65.3% (n = 160) responded by mail, and 34.7% (n = 85) responded by phone.
Of the nine maternal and child characteristics compared between respondents and nonrespondents, respondents and nonrespondents differed significantly with respect to maternal race/ethnicity (p < 0.0001) and maternal education (p< 0.0001). There were significantly more non-Hispanic White respondents than nonrespondents and significantly more respondents were of greater than high school education than nonrespondents.
Demographic Characteristics
Of the 245 survey respondents, 97.1% (n = 238) were the child’s biological mother. As indicated in Table 1, most respondents were non-Hispanic White (n = 204, 83.3%) and married (n = 170, 70.0%). Almost two-thirds of mothers (n = 158, 65.0%) had some college education or had graduated college and almost 60% were employed (n = 141). At the time of the survey, the majority of respondents were less than 35 years old (n = 177, 72.2%), and the average age was 32.0 years old (range, 20–64 years old). For 50.0% (n = 115) of the children with OFC, the primary health insurance was private health insurance, and 45.2% (n = 104) of the children with OFC had public insurance. No respondents lacked health insurance at the time the survey was completed (data not shown). Approximately 60% (n = 145) of children had an isolated OFC (OFC was the only birth defect diagnosis). Eighty-nine (36.3%) of the children had cleft palate only, 47 (19.2%) had cleft lip only, and 109 (44.5%) had cleft lip with cleft palate. The age range of children with OFC was between 2 and 6 years old, and 55.9% (n = 137) of children were between the ages of 3 and 4 years old (Table 1). For 93.9% (n = 230) of the mothers, English was the primary language spoken in the household (data not shown).
Table 1.
Selected Demographic Characteristics of Survey Respondents and Their Children with Orofacial Cleft (OFC) in North Carolina, 2001 to 2004
| Characteristics | N=245 | |
|---|---|---|
| Maternal | n | % |
| Age (years) | ||
| < 30 | 92 | 37.6 |
| 30–35 | 85 | 34.7 |
| ≥ 36 | 68 | 27.8 |
| Education | ||
| Elementary and some high school | 28 | 11.5 |
| High school graduate | 57 | 23.5 |
| Some college | 77 | 31.7 |
| College graduate | 81 | 33.3 |
| Race/ethnicity | ||
| Non-Hispanic White | 204 | 83.3 |
| Othera | 41 | 16.7 |
| Marital status | ||
| Currently married | 170 | 70.0 |
| Previously married | 39 | 16.1 |
| Never married | 34 | 14.0 |
| Job status | ||
| Employed | 141 | 58.0 |
| Unemployed | 102 | 42.0 |
| Annual household income (before taxes) | ||
| ≤ $19,999 | 70 | 29.9 |
| $20,000 to $49,999 | 72 | 30.8 |
| ≥ $50,000 | 92 | 39.3 |
| No. of children with special health care needs in household (other than child with OFC) | ||
| None | 171 | 71.0 |
| ≥1 child | 70 | 29.0 |
| Child | ||
| Age (years) | ||
| 2 | 60 | 24.5 |
| 3 | 75 | 30.6 |
| 4 | 62 | 25.3 |
| 5 | 30 | 12.2 |
| 6 | 18 | 7.4 |
| Race/ethnicity | ||
| Non-Hispanic White | 199 | 81.2 |
| Othera | 46 | 18.8 |
| Preterm birth | ||
| < 37 weeks | 46 | 18.8 |
| ≥ 37 weeks | 199 | 81.2 |
| Low birth weight (≤2500 g) | ||
| Yes | 42 | 17.1 |
| No | 203 | 82.9 |
| Primary insurance13 | ||
| Private health insurance | 115 | 50.0 |
| Public health insurance | 104 | 45.2 |
| Military | 11 | 4.8 |
| Cleft type | ||
| Cleft palate only | 89 | 36.3 |
| Cleft lip only | 47 | 19.2 |
| Cleft lip with cleft palate | 109 | 44.5 |
| Presence of other anomalies | ||
| Isolated anomaly (orofacial cleft diagnosis only) | 145 | 59.2 |
| Multiple anomalies (orofacial cleft + another birth defect) | 100 | 40.8 |
| Sex | ||
| Male | 141 | 57.6 |
| Female | 104 | 42.5 |
The total N may not equal 245 due to missing data.
Other includes respondents who indicated a race of Hispanic, Black/African-American, American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, or an open-ended other option.
Private health insurance was defined as enrollment in the State Employee Health Plan or a private health insurance plan purchased from an employer or directly from an insurance company. Public health insurance was defined as having enrollment in one of the following insurance plans: North Carolina Health Choice (State Children’s Health Insurance Program), Medicaid, Carolina ACCESS or Health Check. Military insurance was defined as having insurance through Civilian Health and Medical Program of the Uniformed Services, TRICARE (formerly Civilian Health and Medical Program of the Uniformed Services), or the Veteran’s Administration.
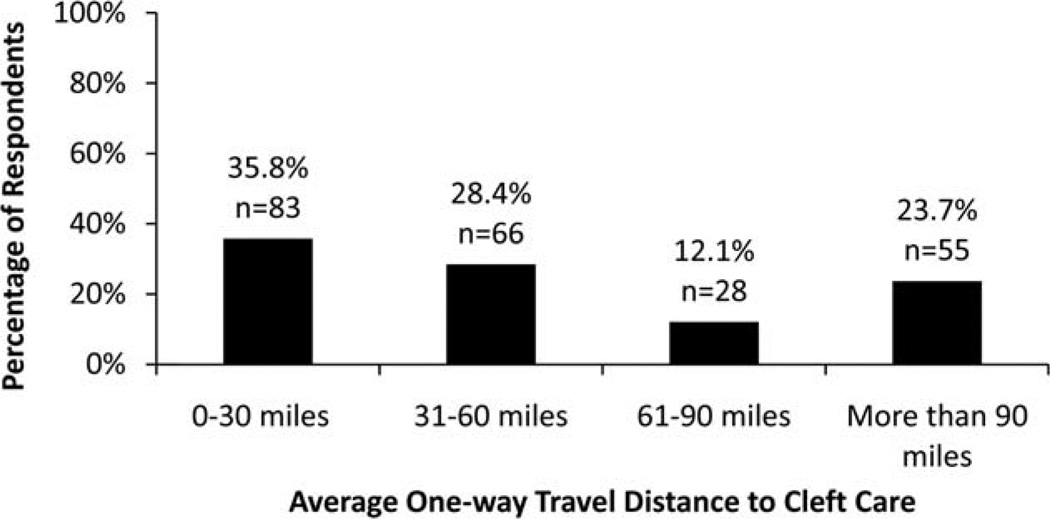
Travel Distance
Mothers reported an average one-way distance traveled to care ranging from zero miles to 1058 miles, with a mean distance of 80.2 miles and a median distance of 50 miles. The mother who reported traveling 1058 miles took her child out-of-state for cleft care. When travel distance responses were dichotomized, 64.2% (n = 149) of mothers traveled an average of less than or equal to 60 miles to receive care (Fig. 1).
Figure 1.
Survey respondents’ reported average one-way travel distance to primary cleft and craniofacial care for their child with orofacial clefts in North Carolina, 2001 to 2004 (N = 232).
After adjusting for selected sociodemographic variables, travel distance varied significantly by maternal education, cleft type, and child’s age (Table 2). Mothers who had some college education were 75% less likely to travel greater than 60 miles to cleft care compared with mothers who were college graduates (aOR, 0.25; 95% CI, 0.10–0.63). Child’s age was also significantly associated with travelling greater distances to receive primary cleft and craniofacial care. Compared with mothers of children who were three years old, mothers of children with OFC who were 2 years old were 67% less likely and mothers of children who were 4 years old were 73% less likely to travel greater than 60 miles to receive cleft and craniofacial care (aOR, 0.33; 95% CI, 0.13–0.82 and aOR, 0.27; 95% CI, 0.11–0.68, respectively). A child’s cleft type was also found to have a significant impact on travel distance. Compared with children with a cleft lip only, children with a cleft lip with cleft palate were almost three times more likely to travel greater than 60 miles to receive care (95% CI, 1.06–7.55). Mothers with a family income of $20,000 to $49,999 were more than twice as likely to drive more than 60 miles for care compared with women with family incomes of $50,000 or more, although this difference was not statistically significant (95% CI, 0.88–6.53) (Table 2).
Table 2.
Crude and Adjusted Odds Ratio Estimates and 95% Confidence Intervals for Association between Selected Sociodemographics and One-Way Travel Distance (> 60 Miles vs. ≤60 Miles [Reference]) (N=232)
| Characteristics | Crude odds ratios (95% confidence intervals) |
Adjusted odds ratios (95% confidence intervals) |
|---|---|---|
| Maternal | ||
| Age (years) | ||
| < 30 | Reference | Reference |
| 30–35 | 0.54 (0.28–1.03) | 0.56 (0.25–1.24) |
| ≥ 36 | 0.72 (0.37–1.39) | 0.65 (0.27–1.56) |
| Education | ||
| Elementary and some high school | 1.09 (0.48–2.74) | 0.51 (0.12–2.19) |
| High school graduate | 1.56 (0.77–3.18) | 0.83 (0.28–2.51) |
| Some college | 0.61 (0.30–1.22) | 0.25 (0.10–0.63) |
| College graduate | Reference | Reference |
| Annual household income (before taxes) | ||
| ≤$19,999 | 1.00 (0.50–1.99) | 0.93 (0.24–3.60) |
| $20,000 to $49,999 | 1.99 (1.03–3.85) | 2.40 (0.88–6.53) |
| ≥$50,000 | Reference | Reference |
| Marital status | ||
| Currently married | Reference | Reference |
| Previously married | 1.24 (0.60–2.59) | 1.89 (0.68–5.31) |
| Never married | 0.83 (0.37–1.87) | 0.63 (0.18–2.20) |
| No. of children with special health care needs in household (other than child with OFC) | ||
| None | Reference | Reference |
| ≥ 1 child | 1.44 (0.80–2.56) | 1.56 (0.74–3.29) |
| Child | ||
| Age (years) | ||
| 2 | 0.54 (0.26–1.12) | 0.33 (0.13–0.82) |
| 3 | Reference | Reference |
| 4 | 0.51 (0.25–1.06) | 0.27 (0.11–0.68) |
| 5 | 0.73 (0.30–1.77) | 0.48 (0.16–1.45) |
| 6 | 0.50 (0.16–1.57) | 0.35 (0.07–1.64) |
| Race/ethnicity | ||
| Non-Hispanic White | Reference | Reference |
| Othera | 1.16 (0.59–2.29) | 1.41 (0.57–3.47) |
| Preterm birth | ||
| < 37 weeks | 0.91 (0.46–1.82) | 0.77 (0.33–1.82) |
| ≥ 37 weeks | Reference | Reference |
| Cleft type | ||
| Cleft palate only | 1.48 (0.67–3.30) | 1.75 (0.64–4.81) |
| Cleft lip only | Reference | Reference |
| Cleft lip with cleft palate | 1.74 (0.80–3.75) | 2.83 (1.06–7.55) |
| Presence of other anomalies | ||
| Isolated anomaly (orofacial cleft diagnosis only) | Reference | Reference |
| Multiple anomalies (orofacial cleft + another birth defect) | 1.24 (0.72–2.13) | 1.35 (0.65–2.83) |
| Sex | ||
| Male | Reference | Reference |
| Female | 1.16 (0.68–2.00) | 0.80 (0.40–1.58) |
| Primary insuranceb | ||
| Private health insurance | Reference | Reference |
| Public health insurance | 1.27 (0.71–2.25) | 0.89 (0.32–2.52) |
| Military | 2.11 (0.57–7.76) | 1.32 (0.28–6.15) |
Adjusted for all covariates listed in table and statistically significant results in bold.
Other includes respondents who indicated a race of Hispanic, Black/African-American, American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, or Other.
Private health insurance was defined as enrollment in the State Employee Health Plan or a private health insurance plan purchased from an employer or directly from an insurance company. Public health insurance was defined as having enrollment in one of the following insurance plans: North Carolina Health Choice (State Children’s Health Insurance Program), Medicaid, Carolina ACCESS or Health Check. Military insurance was defined as having insurance through Civilian Health and Medical Program of the Uniformed Services, TRICARE (formerly Civilian Health and Medical Program of the Uniformed Services), or the Veteran’s Administration.
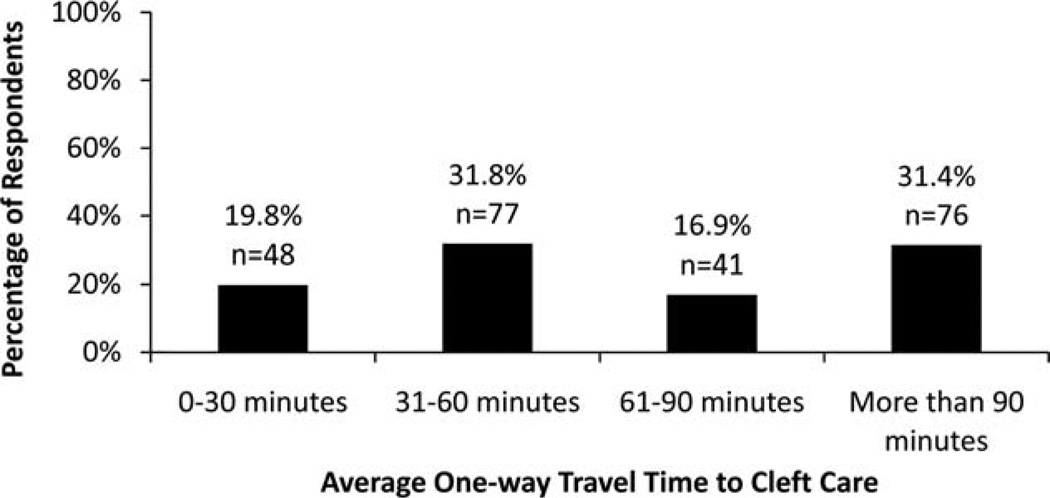
Travel Time
Responses for average one-way time spent traveling to primary cleft and craniofacial care ranged from 5 min to 480 min. The average one-way travel time was 91.7 min, while the median travel time was 60 min. Approximately 52% (n = 125) of mothers had travel times of less than or equal to 60 min (Fig. 2).
Figure 2.
Survey respondents’ reported average one-way travel time to primary cleft and craniofacial care for their child with orofacial clefts in North Carolina, 2001 to 2004 (N = 242).
After adjusting for selected sociodemographic variables, travel time varied significantly by child’s age (Table 3). Mothers of 2-year-old children were 61% less likely to travel greater than 60 min compared with mothers of 3-year-old children (aOR, 0.39; 95% CI, 0.17–0.87). This was the only statistically significant factor associated with increased one-way travel time, although family income of $20,000 to $49,999, presence of other anomalies, and having military insurance remained positively associated with increased travel time (Table 3).
Table 3.
Crude and Adjusted Odds Ratio Estimates and 95% Confidence Intervals for Association between Selected Sociodemographics and One-Way Travel Time (> 60 Minutes vs. ≤60 Minutes [Reference]) (N=242)
| Characteristics | Crude odds ratios (95% confidence intervals) |
Adjusted odds ratios (95% confidence intervals) |
|---|---|---|
| Maternal | ||
| Age (years) | ||
| < 30 | Reference | Reference |
| 30–35 | 0.76 (0.42–1.37) | 0.81 (0.40–1.65) |
| ≥ 36 | 0.75 (0.40–1.41) | 0.79 (0.35–1.78) |
| Education | ||
| Elementary and some high school | 1.59 (0.67–3.77) | 0.92 (0.25–3.37) |
| High school graduate | 1.78 (0.89–3.57) | 0.86 (0.32–2.34) |
| Some college | 0.78 (0.41–1.46) | 0.45 (0.20–1.01) |
| College graduate | Reference | Reference |
| Annual household income (before taxes) | ||
| ≤$19,999 | 1.53 (0.81–2.89) | 1.62 (0.49–5.40) |
| $20,000 to $49,999 | 1.86 (1.00–3.47) | 2.19 (0.90–5.33) |
| ≥$50,000 | Reference | Reference |
| Marital status | ||
| Currently married | Reference | Reference |
| Previously married | 1.14 (0.56–2.30) | 1.10 (0.43–2.83) |
| Never married | 1.37 (0.65–2.89) | 1.19 (0.39–3.60) |
| No. of children with special health care needs in household (other than child with OFC) | ||
| None | Reference | Reference |
| ≥ 1 child | 1.33 (0.76–2.32) | 1.20 (0.61–2.37) |
| Child | ||
| Age (years) | ||
| 2 | 0.52 (0.26–1.03) | 0.39 (0.17–0.87) |
| 3 | Reference | Reference |
| 4 | 0.52 (0.26–1.03) | 0.51 (0.23–1.11) |
| 5 | 0.89 (0.37–2.12) | 0.87 (0.31–2.43) |
| 6 | 0.51 (0.17–1.47) | 0.37 (0.09–1.45) |
| Race/ethnicity | ||
| Non-Hispanic White | Reference | Reference |
| vOthera | 0.98 (0.51–1.85) | 0.65 (0.28–1.48) |
| Preterm birth | ||
| < 37 weeks | 1.35 (0.71–2.56) | 1.35 (0.63–2.87) |
| ≥ 37 weeks | Reference | Reference |
| Cleft type | ||
| Cleft palate only | 1.11 (0.54–2.27) | 1.02 (0.43–2.40) |
| Cleft lip only | Reference | Reference |
| Cleft lip with cleft palate | 1.43 (0.71–2.85) | 1.38 (0.60–3.15) |
| Presence of other anomalies | ||
| Isolated anomaly (orofacial cleft diagnosis only) | Reference | Reference |
| Multiple anomalies (orofacial cleft + another birth defect) | 1.58 (0.94–2.65) | 1.46 (0.75–2.81) |
| Sex | ||
| Male | Reference | Reference |
| Female | 1.09 (0.65–1.81) | 1.04 (0.57–1.92) |
| Primary insuranceb | ||
| Private health insurance | Reference | Reference |
| Public health insurance | 1.46 (0.85–2.49) | 1.04 (0.41–2.61) |
| Military | 2.36 (0.65–8.50) | 1.79 (0.42–7.57) |
Adjusted for all covariates listed in table and statistically significant results in bold.
Other includes respondents who indicated a race of Hispanic, Black/African-American, American Indian, Alaskan Native, Asian, Native Hawaiian, Pacific Islander, or Other.
Private health insurance was defined as enrollment in the State Employee Health Plan or a private health insurance plan purchased from an employer or directly from an insurance company. Public health insurance was defined as having enrollment in one of the following insurance plans: North Carolina Health Choice (State Children’s Health Insurance Program), Medicaid, Carolina ACCESS or Health Check. Military insurance was defined as having insurance through Civilian Health and Medical Program of the Uniformed Services, TRICARE (formerly Civilian Health and Medical Program of the Uniformed Services), or the Veteran’s Administration.
Satisfaction with and Accessing Care
Approximately 98% (n = 236/242) of respondents were “very satisfied” or “satisfied” with the primary cleft and craniofacial care their child had received. Approximately 87% (n = 161/186) of all respondents said primary cleft and craniofacial care “often” or “almost always” worked well in the last 12 months for their child. Over two-thirds of respondents (67.2%; n = 162/241) said that taking their child to receive primary cleft or craniofacial care was “not a problem” despite having potentially long travel times or distances to care.
There was no evidence of an association between travel distances and whether or not taking a child to cleft care was a problem. However, for travel time, mothers who traveled more than 60 min to cleft care were significantly more likely to indicate that taking their child to care was a problem compared with mothers who traveled 60 min or less (p = 0.0062).
DISCUSSION
In our study, almost half of all survey respondents traveled more than an hour and over a third of respondents traveled over 60 miles to obtain primary cleft and craniofacial care for their child. Although respondents often had to travel long distances and travelled a long time to take their children to receive care, most survey respondents indicated that such travel was not a problem.
We found associations between increased travel distance and maternal education, child’s age, and cleft type. Children with both a cleft lip and palate were more likely to travel a longer distance to care than children with a cleft lip alone or a cleft palate alone. Typically, children with a cleft lip with cleft palate have more complex health needs than a child with cleft lip or palate alone. This association may be explained because children with a more severe OFC may need to travel farther to receive more specialized, extensive care.
One surprising finding of our study was that insurance type and the presence of other congenital anomalies were not statistically significantly associated with shorter travel times and distance to primary cleft care. We expected that families of children with multiple birth defects or certain types of health insurance would choose to live closer to medical centers or cleft or craniofacial centers to obtain the care their child needed. We also thought the child’s age would be more of an important predictor due to different services recommended at various age groups for children with OFC (ACPA, 2009).
Long one-way travel times and distances reported in our study may be due to mothers taking their child with OFC out-of-state for care. Several respondents living in North Carolina indicated in other survey questions taking their child to Texas, Hawaii, New York, Pennsylvania, California, Virginia, and Tennessee to receive cleft care for their child, which resulted in high travel distances and times. We did not restrict our analysis to those that only received care in-state because we know families can take their child to receive cleft and craniofacial care out-of-state. Depending on where families resided in the state and where families took their children for cleft and craniofacial care, families may have long travel distances and high travel times. Because our study relied on maternal self-report, we cannot rule out that mothers’ perception of travel distance and time may have included reporting round trip results instead of one-way or by a combination of transportation methods, such as by plane, automobiles and/or public transportation, which may have also impacted our results.
Few studies exist to which we can compare our results. These previous studies examined geographical barriers to dental care for children with OFC (Al Agili et al., 2004; Nelson et al., 2011). Our results were not consistent with those of Al Agili et al. (2004) who reported that long travel distance was a perceived barrier to receiving dental care among children with OFC in Alabama. Our results were not congruent with those of Nelson et al. (2011) who reported that children with craniofacial anomalies were affected more by barriers, such as cost and distance to the dentist, than children with other types of special health care needs.
Other studies have found disparities in access to care for children with special health care needs depending on geographic location, although they did not measure distance to care. In one study, researchers examined access to a medical home in different states among children with special health care needs. They found that medical home access for children with special health care needs differed significantly by state (Singh et al., 2009). Authors in another study examined factors associated with receiving care from a medical home and compared these factors across levels of socioeconomic status. Geographic location was significantly associated with receiving care in a medical home for both the lowest and highest income categories (Fulda et al., 2009).
There have been a few previous studies that have used geographic information systems (GIS) to examine geographic barriers and access to care for children with birth defects. One recent study in Texas used a state-wide birth defect registry and GIS to examine first-year mortality risk for children born between 1996 and 2003 with certain kinds of congenital heart disease and its association with their residence’s geographic distance from a cardiac care center (Fixler et al., 2012). In a different study, researchers evaluated the distance of residential addresses of children born 1999 to 2004 with major and chromosomal birth defects in Texas from pediatric clinical genetic service providers. The authors found disparities in geographic access to services among these children (Case et al, 2008). These studies illustrate that GIS is a convenient and readily available alternative to surveys in identifying geographic barriers to care for children with birth defects, such congenital heart defects and chromosomal defects that require coordinated, specialized care.
In Cromley and McLafferty’s book on GIS and Public Health (2011), Penchansky and Thomas (1981), Aday and Andersen (1974), and Aday and Andersen (1981), the authors discuss the importance of access to care, including travel distance and time to care. Cromley and McLafferty (2011) and Penchansky and Thomas (1981) discuss five components of access to medical care, one of which is accessibility and includes geographical barriers to care, such as travel distance and time, cost, and transportation. Travel distance and time provide only one aspect of measuring access to care (or barriers to care) and are important variables to examine to help better understand access to care for children with special health care needs, including children with birth defects.
Strengths and Limitations
There were several limitations to our study. Our survey collected self-reported satisfaction, whether care worked well, whether traveling to care was a problem, and travel distance and time. Such self-report can be subject to misinterpretation and bias, although some research suggests that maternal recall of a young child’s health care events is generally accurate (Pless and Pless, 1995; D’Souza-Vazirani et al., 2005). Unfortunately, we do not know the actual location or respondents’ address or the location where children actually received cleft and craniofacial services to calculate exact distances to services. In addition, parents may take their children to multiple locations to receive care.
The survey specifically asked about taking children to primary cleft and craniofacial care; however, we cannot rule out respondents interpreting this question as receiving any care. Additionally, a child’s primary cleft and craniofacial care center may not be the closest facility to the child’s home residence, which could increase both travel distance and time.
Our study was focused on only one state in 2006, which may limit the generalizability of our results to other states. Furthermore, our results may reflect a relatively small proportion of families experiencing problems accessing care. The perceived barriers to accessing services identified in our survey may also vary depending on a child’s age and/or diagnosis, the lack of organization of services, and the health care system structure. Reported barriers to care may not capture the entire experience of receiving craniofacial care, nor provide complete context for these experiences.
Treatment of children with cleft and craniofacial anomalies like OFC has traditionally relied upon cleft and craniofacial teams or centers to provide a coordinated, interdisciplinary team approach to care. The interdisciplinary teams are generally composed of physicians and health care professionals from different specialties. These teams and centers have become the standard in assessment and treatment of children with craniofacial anomalies (Shah and Wong, 1980; Sharp, 1995; Strauss, 1999). In our study, we did not control for such factors (e.g., whether or not children received treatment at a cleft and craniofacial center or received team care for their primary cleft care), because we had insufficient information to analyze these factors.
Another limitation was that the response rate to our survey was approximately 52%. This low response might have meant that our findings were subject to selection bias, especially if those who did not participate differed from the respondents (e.g., under-representation of racial/ ethnic minorities and those with lower education attainment). When we compared characteristics of the respondents and nonrespondents for which there was available data, the characteristics were similar except for maternal race/ethnicity and maternal education. Most of the demographic characteristics of our study population were similar to that of all mothers of children with OFC in the state during the study period, suggesting that our sample was generally representative of the population of interest.
Another limitation was that our survey did not ask about the mode of transportation. In addition, we cannot rule out the possibility that respondents may have under- or over-estimated one-way travel distance and time, and we cannot determine the extent to which this affected our results.
The two primary strengths of our study were using data from an active, state-wide, population-based birth defects registry and use of validated ‘barriers to care’ questions. Because we used surveillance data, we could verify a child’s cleft diagnosis through medical records. Most previous studies on barriers to care of this population did not verify the birth defect diagnosis. We also adjusted for the severity of the cleft and the presence of other birth defects, which are factors that could potentially affect the travel distance and time results. As a result, we controlled for confounding by factors that may increase travel distance or time to care. Previous studies did not adjust for such factors.
Another primary strength was that our survey was based on a reliable “barriers to care” survey that was developed and validated for the study of English- and Spanish-speaking parents of children with chronic diseases (Seid et al., 2004). All the demographic questions came from validated survey instruments, and the five main outcomes (i.e., travel distance, travel time, satisfaction, problem accessing care, and whether care worked well) assessed in this study came from validated ‘barriers to care’ questions (Seid et al., 2004). This study demonstrates the usefulness of birth defects registry and survey data to determine geographical barriers to care for children with birth defects, such as OFC.
Public Health Implications and Access to Health Services
This study also has implications for public health and access to health services. First, it helps us to better understand barriers to health care, which may provide areas to focus public health and health care resources and interventions. The results from this study have several implications for cleft and craniofacial care. Although geographic location of health care services may be a barrier to some parents seeking care for their children with OFC, we found that most parents in our survey were able to overcome this when seeking care for their child, and they did not consider it a problem taking their child to care. Coordinated health care teams and centers provide important services for families of children with birth defects, including OFC, and other medical conditions. Our study suggests that decreasing travel distance and time to care for families with OFC may vary in its impact based on various maternal and child characteristics. Furthermore, characteristics associated with increased travel distance and time to care are similar to those characteristics associated with access to care, quality of life and health outcomes among children with OFC. Findings from this study increase our knowledge and provide evidence about the types of geographic barriers parents encounter accessing care for their child with OFC as recently identified by convened experts at the CDC (Yazdy et al., 2007) and the updated U.S. Surgeon General’s Report on Oral Health (US DHHS, 2000; Strauss and Cassell, 2009). To our knowledge, this study is the first to examine parental report of travel distance and time for children of OFC and examine potential associations with selected sociodemographic factors, using a state-wide, population-based birth defect registry.
Future studies could use GIS to calculate Euclidean measures of distance and time in conjunction with self-reported measures to determine if additional medical centers and/or cleft and craniofacial centers are needed in certain location(s). Such studies also could further assess traffic patterns (e.g., time of day, day of week, and month) and reason for seeking care (e.g., referral to services, closer to family or employment, types of services offered, and increased quality of care). These studies could also obtain additional information on residential addresses and whether parents moved from the time of the infant’s birth and anytime throughout infancy and childhood and the reasons for those moves (e.g., to seek care, employment, and better school system, and perhaps for additional family support). Future studies could use birth defects surveillance systems, parent surveys, and GIS to better understand geographic barriers to care for children with special health care needs, such as birth defects.
ACKNOWLEDGMENTS
We acknowledge the survey participants for their time and thoughtful comments, providing much needed insight on this topic. We also thank the entire staff of the NCBDMP for without them birth defects data collection would not be able to be obtained. We also acknowledge Eleanor Howell, Cinda Meyer, and Vanessa White who assisted in data collection and preliminary analysis and the phone interviewers with the North Carolina State Center for Health Statistics for their time and effort in conducting the phone interviews. Lastly, we thank Michael Seid for allowing us to use the validated “barriers to care” survey instrument created for children with special health care needs.
Supported in part by grant number U50/CCU422096 by the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention (CDC).
Footnotes
Parts of this manuscript were presented at the National Birth Defects Prevention Network annual meeting, February 24–27, 2012, in Arlington, Virginia, and at the 17th Annual Maternal and Child Health Epidemiology Conference December 14–16, 2011, in New Orleans, Louisiana, and American Cleft Palate Craniofacial Association annual meeting April 14–18, 2008, in Philadelphia, Pennsylvania.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors have no conflict of interest to declare.
REFERENCES
- Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- Aday L, Andersen R. Equity of access to medical care: a conceptual and empirical overview. Med Care. 1981;19:4–27. [PubMed] [Google Scholar]
- Al Agili DE, Roseman J, Pass MA, et al. Access to dental care in Alabama for children with special needs: parents’ perspectives. J Am Dent Assoc. 2004;135:490–495. doi: 10.14219/jada.archive.2004.0216. [DOI] [PubMed] [Google Scholar]
- American Cleft Palate-Craniofacial Association (ACPA) Parameters for evaluation and treatment of patients with cleft lip/palate and other craniofacial anomalies. Revised edition. Chapel Hill, NC: 2009. [Accessed March 24, 2013]. pp. 1–34. available at: http://www.acpa-cpf.org/uploads/site/Parameters_Rev_2009.pdf. [Google Scholar]
- Case AP, Canfield MA, Barnett A, et al. Proximity of pediatric genetic services to children with birth defects in Texas. Birth Defects Res A Clin Mol Teratol. 2008;82:795–798. doi: 10.1002/bdra.20515. [DOI] [PubMed] [Google Scholar]
- Cassell CH, Daniels J, Meyer RE. Timeliness of primary cleft lip/ palate surgery. Cleft Palate Craniofac J. 2009;46:588–597. doi: 10.1597/08-154.1. [DOI] [PubMed] [Google Scholar]
- Cassell CH, Mendez DD, Strauss RP. Maternal perspectives: qualitative responses about perceived barriers to care among children with orofacial clefts in North Carolina. Cleft Palate Craniofac J. 2012;49:262–269. doi: 10.1597/09-235. [DOI] [PubMed] [Google Scholar]
- Cromley E, McLafferty S. GIS and public health. 2nd ed. New York: Guilford Press; 2011. [Google Scholar]
- Dixon MJ, Marazita ML, Beaty TH, Murray JC. Cleft lip and palate: understanding genetic and environmental influences. Nat Rev Genet. 2011;12:167–178. doi: 10.1038/nrg2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Souza-Vazirani D, Minkovitz CS, Strobino DM. Validity of maternal report of acute health care use for children younger than three years. Arch Pediatr Adolesc Med. 2005;159:167–172. doi: 10.1001/archpedi.159.2.167. [DOI] [PubMed] [Google Scholar]
- Fixler DE, Nembhard WN, Xu P, et al. Effect of acculturation and distance from cardiac center on congenital heart disease mortality. Pediatrics. 2012;129:1118–1124. doi: 10.1542/peds.2011-3114. [DOI] [PubMed] [Google Scholar]
- Fulda KG, Lykens K, Bae S, Singh K. Factors for accessing a medical home vary among children with special health care needs from different levels of socioeconomic status. Matern Child Health J. 2009;13:445–456. doi: 10.1007/s10995-008-0371-z. [DOI] [PubMed] [Google Scholar]
- Henry KA, Boscoe FP, Johnson CJ, et al. Breast cancer stage at diagnosis: is travel time important? J Community Health. 2011;36:933–942. doi: 10.1007/s10900-011-9392-4. [DOI] [PubMed] [Google Scholar]
- Huang B, Dignan M, Han D, Johnson O. Does distance matter? Distance to mammography facilities and stage at diagnosis of breast cancer in Kentucky. J Rural Health. 2009;25:366–371. doi: 10.1111/j.1748-0361.2009.00245.x. [DOI] [PubMed] [Google Scholar]
- Kuehn CM, Mueller BA, Checkoway H, Williams M. Risk of malformations associated with residential proximity to hazardous waste sites in Washington State. Environ Res. 2007;103:405–412. doi: 10.1016/j.envres.2006.08.008. [DOI] [PubMed] [Google Scholar]
- McPherson M, Weissman G, Strickland BB, et al. Implementing community-based systems of services for children and youths with special health care needs: how well are we doing? Pediatrics. 2004;113:1538–1544. [PubMed] [Google Scholar]
- National Birth Defects Prevention Network (NBDPN) State birth defects surveillance program directory. Birth Defects Res. 2011;A91:1028–1049. [Google Scholar]
- Nelson LP, Getzin A, Graham D, et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011;33:29–36. [PubMed] [Google Scholar]
- Nelson P, Glenny AM, Kirk S, Caress AL. Parents’ experiences of caring for a child with a cleft lip and/or palate: a review of the literature. Child Care Health Dev. 2012;38:6–20. doi: 10.1111/j.1365-2214.2011.01244.x. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med. 2005;159:10–17. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Parker SE, Mai CT, Canfield MA, et al. National Birth Defects Prevention Network. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008–1016. doi: 10.1002/bdra.20735. [DOI] [PubMed] [Google Scholar]
- Penchansky R, Thomas JW. The concept of access: definition and relationships to consumer satisfaction. Med Care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- Pinto NM, Lasa J, Dominguez TE, et al. Regionalization in neonatal congenital heart surgery: the impact of distance on outcome after discharge. Pediatr Cardiol. 2012;33:229–238. doi: 10.1007/s00246-011-0116-4. [DOI] [PubMed] [Google Scholar]
- Pless CE, Pless IB. How well they remember: the accuracy of parent reports. Arch Pediatr Adolesc Med. 1995;149:553–558. doi: 10.1001/archpedi.1995.02170180083016. [DOI] [PubMed] [Google Scholar]
- Seid M, Sobo EJ, Gelhard LR, Varni JW. Parents’ reports of barriers to care for children with special health care needs: development and validation of the barriers to care questionnaire. Ambul Pediatr. 2004;4:323–331. doi: 10.1367/A03-198R.1. [DOI] [PubMed] [Google Scholar]
- Shah CP, Wong D. Management of children with cleft lip and palate. Can Med Assoc J. 1980;122:19–24. [PMC free article] [PubMed] [Google Scholar]
- Sharp HM. Ethical decision-making in interdisciplinary team care. Cleft Palate Craniofac J. 1995;32:495–499. doi: 10.1597/1545-1569_1995_032_0495_edmiit_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Singh GK, Strickland BB, Ghandour RM, van Dyck PC. Geographic disparities in access to the medical home among US children with special health care needs. Pediatrics. 2009;124:S352–S360. doi: 10.1542/peds.2009-1255E. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Health. 2007;23:150–157. doi: 10.1111/j.1748-0361.2007.00082.x. [DOI] [PubMed] [Google Scholar]
- Strauss RP. The organization and delivery of craniofacial health services: the state of the art. Cleft Palate Craniofac J. 1999;36:189–195. doi: 10.1597/1545-1569_1999_036_0189_toadoc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- Strauss RP, Cassell CH. Critical issues in craniofacial care: quality of life, costs of care, and implications of prenatal diagnosis. Acad Pediatr. 2009;9:427–432. doi: 10.1016/j.acap.2009.09.019. [DOI] [PubMed] [Google Scholar]
- Strickland BB, Singh GK, Kogan MD, et al. Access to the medical home: new findings from the 2005–2006 National Survey of Children with Special Health Care Needs. Pediatrics. 2009;123:e996–e1004. doi: 10.1542/peds.2008-2504. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services (US DHHS) Oral health in America: a report of the Surgeon General. Rockville, MD: Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- Wehby GL, Cassell CH. The impact of orofacial clefts on quality of life and healthcare use and costs. Oral Dis. 2010;16:3–10. doi: 10.1111/j.1601-0825.2009.01588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White RB. Services for children with congenital facial clefts through a state Crippled Children’s Service Program. Cleft Palate J. 1981;18:116–121. [PubMed] [Google Scholar]
- Williams CA, Mardon RE, Grove D, et al. Treatment of oralfacial clefts by state-affiliated craniofacial centers and cleft palate clinics. Birth Defects Res A Clin Mol Teratol. 2003;67:643–646. doi: 10.1002/bdra.10115. [DOI] [PubMed] [Google Scholar]
- Yazdy MM, Honein MA, Rasmussen SA, Frias JL. Priorities for future public health research in orofacial clefts. Cleft Palate Craniofac J. 2007;44:351–357. doi: 10.1597/06-233.1. [DOI] [PubMed] [Google Scholar]