Abstract
For older adults aging in the community, living conditions can promote health, enhance coping, and reduce disablement – but they can also create stress and increase risks of illness, accidents, and decline. While socioeconomic disparities in housing likely contribute to inequalities in interior conditions, I argue that living conditions are also shaped by social resources such as co-residential relationships, social network ties, and social support. In this paper, I examine the distribution of a set of risky or stressful physical and ambient living conditions including structural disrepair, clutter, lack of cleanliness, noise, and odor. Using data from the National Social Life, Health, and Aging Project (NSHAP), I find that low income and African American older adults have more disordered living conditions, as do those with poorer physical and mental health. In addition, older adults who have a co-resident partner, more non-residential network ties, and more sources of instrumental support are exposed to fewer risky or harmful living conditions. This suggests that living conditions are an important, though overlooked, mechanism through which household composition, social networks, and social support affect health and well being in later life.
Keywords: Aging in place, household composition, housing, marriage/partnership, social inequality, social networks, social support
The vast majority of older adults prefer to remain in their homes as long as possible, and much attention has been devoted to role of neighborhood contexts and communities in supporting the needs of an aging population (see, e.g., American Association of Retired Persons, 2005; Cagney & York Cornwell 2010; Yen, Michael, & Perdue, 2009). But less consideration has been afforded to the conditions of their interior housing environments. For some older adults, living conditions may be a resource that promotes well being and enables coping with health problems or functional decline. But for others, physical and ambient features of the interior living space may threaten health and well being, create stress, exacerbate illness, further disablement, and hasten decline. Previous research suggests that disparities in living conditions reflect older adults’ functional health as well as social status, with lower income older adults more likely to be exposed to substandard housing (Frumkin, 2005; Golant & LaGreca, 1994b). But social resources available in and around the household may also shape living conditions. In this paper, I use data from the National Social Life, Health, and Aging Project (NSHAP) to consider how social status, household composition, social networks, and social support are implicated in the emergence of living conditions that threaten the health and well being of community-residing older adults.
AGING IN PLACE AT HOME
For the growing proportion of older adults who are aging in the community, there’s no place like home. As individuals age, daily life tends to converge within the home – so that the oldest old spend upwards of 80 percent of their waking hours there (Krantz-Kent & Stewart, 2007). Gerontological research over the past several decades points to housing deficiencies such as plumbing problems, inadequate heating, and broken fixtures as creating “environmental press,” for older adults who suffer functional impairments, health problems, or other vulnerabilities (Lawton and Nahemow, 1973). For these older adults, dwelling deficiencies present daily challenges, stressors, and difficulties, and may ultimately increase the risk of functional decline and accidents (Iwaarson 2005; Wahl, Fänge, Oswald, Gitlin, & Iwarsson 2009). The home is also increasingly the site of formal and informal caregiving arrangements (Oswald & Wahl 2004), and it is within this context that older adults cope with chronic conditions, illness, and functional or cognitive declines. Housing features and modifications can therefore play a critical role in determining the extent to which a health problem or impairment results in disablement or decline (Fänge and Iwarsson, 2005; Liu and Lapane 2009; Verbrugge & Jette, 1994).
Other features of the interior living environment such as clutter, lack of cleanliness, and odors, are more subtle and transient than dwelling deficiencies like plumbing or electrical problems, but they may be just as consequential for daily life, health, and well-being. Physical and ambient conditions of the living space can directly impact older adults’ health. For example, poor ventilation and a lack of cleanliness expose residents to toxins, bacteria, and allergens that can cause respiratory and infectious diseases (Fisk, 2007; Stanwell-Smith, 2003). Clutter may impair mobility and increase the risk of falls and other accidents (Sattin, 1998). Ambient conditions like noise and odors can cause stress (Staples, 1996; Evans, Hygge, & Bullinger, 1995) and disrupt sleep (Zaharna & Guilleminault, 2010). Collectively, these conditions heighten risks of morbidity and mortality (Oswald & Wahl, 2004). And, for those who are already coping with health problems common in later life, such as respiratory illness, suppressed immune function, limited mobility, or depression, these living conditions may be particularly hazardous (Lawton and Nahemow 1973).
Housing studies and environmental health research primarily attribute differences in housing and living conditions to social stratification. In fact, research emphasizes the importance of addressing hazardous living conditions for reducing health disparities (Shaw 2004; Rauh, Landrigan, & Claudio 2008). Low-income individuals and minorities are more likely to live near pollution and toxic emission sites (Brown, 1995) and to reside in older and more dilapidated housing often characterized by holes in walls or flooring, a lack of central heating, inadequate sewer or septic systems, and a lack of insulation (Frumkin, 2005; Golant and LaGreca, 1994b). These dwelling deficiencies provide fertile ground for the emergence of interior conditions like odor and noise. And when housing-related problems arise, lower status groups are less likely to be able to address them. For example, a lack of financial resources or access to services may limit one’s ability to make home modifications (Newman 2003; Pynoos, 1993) and pay for housekeeping or maintenance services. Renters are also limited in their ability to make home improvements, and typically lack incentives to do so. Thus, seniors who have low incomes and those who are racial/ethnic minorities are less likely to be able to mitigate the effects of housing quality on interior conditions like mold or odor.
Sociological research has also pointed out that living environments reflect residents’ preferences, patterns of behavior, cultural traditions, or social norms (see, e.g., Bourdieu, 1980 [1970]; Chapin, 1935; Laumann and House, 1970). But older adults who have less proactive attitudes and lower sense of control over their environments are less likely to have the wherewithal to construct a living space that satisfies their needs and preferences (Oswald, et al. 2003). Poor physical or mental health, functional impairment, and cognitive decline may also limit elders’ overall “competence” for completing tasks related to home maintenance and upkeep (Lawton, 1983).
Less attention has been devoted to the processes through which physical and ambient features of living space may be shaped by relationships with co-residents and family members and friends. In fact, recent reviews of research in environmental gerontology have called for more attention to the interrelationships among social environments and physical environments (see, e.g., Evans, 2003; Gitlin, 2003; Rauh, Landrigan, & Claudio 2008). It is possible that residential relationships and social resources such as network ties and social support play a key role in preventing and addressing hazardous or disordered living conditions among community-residing older adults. If this is true, the reduction of hazardous home environments may be another mechanism through which social relationships affect health and well being (Berkman, Glass, Brissette, and Seeman, 2000; Thoits 2011). Below I draw from sociological research to consider how co-residential relationships, as well as residents’ social networks and support, may shape physical and ambient living conditions.
Household Composition and the Division of Household Labor
More than two thirds of older adults living in the community reside with at least one other person. Just over half of older adults reside with a spouse, and an increasing share reside in multigenerational households, with extended family, or with non-relatives, often due to health issues or economic needs (Administration on Aging 2011). Household crowding, as a function of the number of residents and the size of the dwelling, is an important aspect of housing inequality among older adults (Golant & LaGreca, 1994a). African-Americans, Latinos, recent immigrants, and lower-income individuals tend to have more crowded living spaces due to disparities in financial resources and residential segregation (Conley, 2001; Myers & Lee 1996). To the extent that co-residence is related to financial limitations, larger households may reside in dwellings with more problems or deficiencies, which may increase the likelihood of disordered living conditions.
Households containing more people may also have more disordered living conditions because they simply present greater demands for housekeeping and repairs. In line with this, a large literature points to negative effects of household crowding on physical health, mental health, and well being (Gomez-Jacinto & Hombrados-Mendieta, 2002; Gove, Hughes, & Galle, 1979; Regoeczi, 2008). But not all large households are crowded households. And, co-residential arrangements may also allow individuals to pool financial resources or facilitate caregiving for an elderly parent or younger grandchildren (Choi 2003), thereby increasing efficiency and perhaps leading to better living conditions.
While most older adults have at least one co-resident, a growing share of community-residing older adults live alone (Administration on Aging 2011). Older adults who live alone tend to be poorer (O’Brien, Wu, and Baer 2010), which means that they may be more likely to reside in substandard housing. They may also have fewer social resources in the sense that they lack co-residents who might contribute to housekeeping. But, at the same time, they have fewer housekeeping burdens than those who live with others (Hughes & Waite, 2002).
Because co-residence can be both resource and burden with respect to home maintenance and upkeep, the question of who resides in the household may be more important for living conditions than simple measures of household size or density. Co-residents’ coordination and cooperation around household tasks may be consequential for living conditions. The study of the division of household labor is perhaps the most active area of social scientific research related to the social context of the household (for reviews of this literature see Coltrane, 2000; Shelton & John, 1996). This arrangement of household labor – an effort that is essentially aimed at addressing conditions such as clutter, lack of cleanliness, odor, and disrepair – is related to co-residential arrangements, social roles, and relationships.
For one thing, the household division of labor reflects both gendered competence and gender norms (Goldscheider & Waite 1991). Both men and women likely contribute to tasks that affect ambient and physical living conditions. Physiologically, older men may be better able than older women to complete home repairs such as fixing holes in walls and floors or addressing a lack of insulation from outside noises and odors. Outdoor work and home maintenance are also male-typed tasks, compared to traditionally female-typed tasks such as cleaning and tidying the living space (Hochschild, 1989). However, across all living arrangements and even among unmarried adults, cohabiters, and widowed adults living alone, women spend more time than men doing housework (South & Spitze, 1994). Gender differences in housework among men and women who live alone may reflect women’s greater commitments to household upkeep based on socialization to traditional gender norms, or the fact that men are less adept at completing housekeeping tasks because they are not accustomed to doing so.
Sociological research on the division of household labor suggests that family roles – such as spouse/partner, wife/mother, husband/father, and child – structure contributions to household labor. Entry into these roles, such as through marriage and motherhood, increases women’s feelings of commitment to housework (Perkins & DeMeis, 1996) and the time that they spend on household tasks (South & Spitze 1994). In addition, spousal and parent-child relationships often imply responsibilities and obligations that discourage risky behavior (Umberson, 1987). Drawing from this, occupation of primary social roles such as spouse or parent may encourage individuals to address problems in the living space or discourage behaviors that lead to excessive noise, odors, clutter, or lack of cleanliness.
At the same time, combined households complicate typical parent-child roles and increase household demands, particularly if an older adult is dependent upon an adult child for care. Research suggests that women who care for a co-residential elderly parent devote more time to housework than women who do not provide care for a parent (Laditka and Laditka, 2000). But such arrangements also increase stress, role strain, and family conflict (Kwak, Ingersoll-Dayton, & Kim, 2012). This may reduce contributions to, and cooperation around, housekeeping and home maintenance.
Finally, the quality of co-residential relationships may also shape living conditions. Several studies suggest that individuals perform more household tasks when they have closer relationships with their co-residents. Women who report greater closeness with their spouses also feel more appreciated for doing housework and are therefore likely to spend more time on household tasks (Lee & Waite, 2010). Relationship closeness increases husbands’ contributions to housework when their wives are ill (Allen & Webster, 2001) and adult children’s care-work for their co-residential elderly parents (Piercy, 2007). It is possible, then, that close co-residential relationships – particularly likely among spouses/partners and nuclear family members – bring greater flexibility and cooperation around household tasks. Households containing residents who have closer relationships may therefore be better able to stave off disordered living conditions like odors, clutter, lack of cleanliness, and disrepair.
Non-Resident Network Ties and Social Support
The home is not only a context for co-residential relationships, but it can also be a busy hub for social interactions with non-resident friends and family members. In fact, it is within their living spaces that older adults most often interact with family and members of their social networks (Bronfenbrenner & Evans, 2000). The relationships and interactions that occur in and around the home environment may constitute valuable sources of social capital and support.
Sociological research has highlighted a multitude of benefits of social connectedness, and a number of pathways through which social ties lead to better health (Berkman, et al. 2000; Thoits 2011). The promotion of more ordered living conditions may be yet another advantage. While social relationships with co-residents may shape the division of household labor and flexibility and cooperation around household tasks, social ties to non-resident friends and family members may bring access to outside resources that help residents avoid or address living conditions such as cleanliness, odors, and minor repairs. For example, social capital accessed through network ties may provide individuals with information about home repairs or referrals to services that assist with home maintenance and upkeep. In addition, larger networks tend to enhance self-esteem, sense of belonging, and perceived control (Cornman Goldman, Weinstein, & Chang, 2003), which may increase older adults’ proactive attitudes and behaviors. Network members, like co-residents, may also encourage health-promoting behaviors through direct or indirect social control (Lewis & Rook, 1999). Finally, older adults who have a larger network of non-resident friends and family members may devote more time and energy to housekeeping tasks in anticipation of visits.
Social network ties may also be beneficial for living conditions by conferring access to social support. Not all network ties are supportive; closer relationships are more likely to bring access to various forms of support or assistance (Smith and Christakis 2008; Seeman and Berkman 1988). Instrumental support, which involves help or assistance with practical tasks or problems (Thoits 2011), may include assistance with housekeeping tasks or home repairs. For example, friends and family members who visit and observe noise, odor, clutter, lack of cleanliness, or structural problems may provide or arrange for assistance out of a concern for an older adult’s safety and well being. Family members are particularly likely to provide this type of practical support (Lee, Ruan, & Lai, 2005), which may be particularly important for older adults who live alone (Spitze, 1999). For those have co-residents, housekeeping is likely to be part of an ongoing exchange structured by the division of household labor. But support from non-resident family and friends may confer particular benefits by bringing additional hands on deck when housing problems arise or housekeeping becomes overwhelming, perhaps due to illness or functional decline.
HYPOTHESES
In this study, I examine the distribution of five living conditions that pose health risks for older adults: noise, odor, clutter, lack of cleanliness, and general structural disrepair. Because of disparities in housing quality, I hypothesize that older adults who have less education and lower incomes, as well as members of disadvantaged racial/ethnic groups, are exposed to more disordered living conditions. More crowded dwellings present greater housekeeping burdens, so I expect that larger households have more disordered living conditions. But living conditions are also likely to be shaped by residents’ roles, relationships, and their ability to coordinate and cooperate around household tasks. I hypothesize that less disorder will be found in the living spaces of older adults who are married/partnered and those who reside with nuclear family only. Finally, I hypothesize that older adults who have more social resources, in the form of social network ties and access to instrumental support, will have less disordered living conditions.
DATA AND METHODS
To examine the distribution and social correlates of living conditions among older adults, I use data from the first wave of the National Social Life, Health, and Aging Project (NSHAP). This is a nationally representative, population-based study of community-residing older adults. The NSHAP study is well-suited for this research because it includes assessments of respondents’ living conditions alongside information about their household composition, social networks, and social support.
The NSHAP sample was based on a multi-stage area probability design screened by the Institute for Social Research for the Health and Retirement Study (HRS). The HRS design oversampled by race-ethnicity; NSHAP retained this design and also stratified by age and gender in order to attain an equal number of cases in each of six age/gender categories (O’Muircheartaigh, Eckman, & Smith, 2009). From summer 2005 to spring 2006, NSHAP conducted in-person interviews with 3,005 individuals, ages 57–85, achieving a final weighted response rate of 75.5 percent.
Dependent Variable: Disordered Living Conditions
Neighborhood isorder is broadly defined as observable features of decay or deterioration that convey a lack of social cohesion, support, and control in the residential environment (Ross & Mirowsky, 1999; Skogan, 1990). I use this term with the intention of extending the concept of disorder to interior living conditions such as clutter, lack of cleanliness, noise, odor, and disrepair (York, 2008). Accordingly, the assessment of disordered living conditions in NSHAP draws from approaches designed for the systematic observation of neighborhood disorder (Sampson & Raudenbush, 1999).
During face-to-face, in-home interviews conducted for NSHAP, field interviewers gained a first-hand view of respondents’ living conditions. Following each interview, NSHAP field interviewers completed a Field Interviewer Questionnaire (FIQ) in which they were asked, “How well-kept is the building in which the respondent lives?” Responses for this item ranged from “very poorly kept (needs major repairs)” to “very well kept.” Interviewers also answered a series of questions regarding the physical and ambient features of the respondent’s living space. Interviewers described the room in which the interview was conducted on continua ranging from 1 to 5 for each of the following characteristics: 1) lack of cleanliness (from “clean” to “dirty”); 2) messiness (from “neat and tidy” to “messy”; and 3) noise (from “quiet” to “noisy”). The presence of odor was assessed on a 5-point scale from “no smell” to “strong smell.” For respondents whose living conditions at least some odor, field interviewers characterized the odor on a scale ranging from “pleasant smell” to “unpleasant smell.” These ratings are combined in a continuum ranging from 1, where the respondent’s living conditions had no odor or a pleasant odor, to 5, where the respondent’s living conditions had an unpleasant odor.
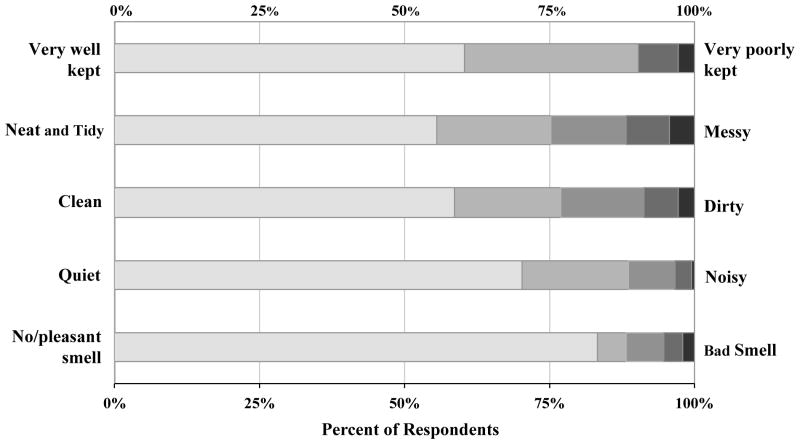
Unweighted distributions of these variables across NSHAP respondents included in the analyses below (n = 2334) are presented in Figure 1. Note that about two-thirds of respondents’ homes were rated in the most ordered categories for upkeep, tidiness, and cleanliness. And, around three-quarters of respondents’ living spaces were very quiet and had no odor or a pleasant odor. However, these conditions vary widely across dwellings. Only about a third of respondents (37.4 percent) had ratings that were in the most ordered category for all of the characteristics of their living conditions. And extremely disordered conditions are rare. Only about 10 percent of respondents’ living conditions were very messy, very dirty, or in serious disrepair. Even fewer homes were rated as very noisy or very malodorous. Weighted means and standard deviations for these ratings are presented in Table 1.
Figure 1.
Distribution of Interviewer Ratings of Respondents’ Living Conditions (n = 2,334)
Table 1.
Descriptive Statistics for Ratings of Disordered Living Conditions
| Measurement | Weighted meana | Standard deviation | N | |||
|---|---|---|---|---|---|---|
| 1 | to | 5 | ||||
|
|
||||||
| Noise | quiet | to | noisy | 1.444 | .802 | 2,332 |
| Odor | pleasant smell | to | bad smell | 1.333 | .898 | 2,328 |
| Dirtiness | clean | to | dirty | 1.728 | 1.078 | 2,325 |
| Messiness | neat and tidy | to | messy | 1.816 | 1.162 | 2,327 |
| Overall disrepair | {1 = “very well kept;” 2 = “fairly well kept;” 3 = “poorly kept;” 4 = “very poorly kept”} | 1.474 | .747 | 2,331 | ||
Means are survey-adjusted and weighted for the probability of selection with post-stratification adjustments for survey non-response, missing data due to out-of-home interviews, and item-level non-response.
I combine these five ratings to create a scale of disordered living conditions. The scale has good internal consistency reliability; Cronbach’s alpha is .83 and all item-rest correlations are moderate to strong. To calculate each respondent’s score on the disorder scale, the ratings are standardized and their sum is divided by the total number of characteristics on which the respondent has valid ratings. The scale may therefore be interpreted as a standardized variable. It ranges from −.71 to 3.37, with a weighted mean of −.07 and standard deviation of .75.
By capturing a broad range of living conditions on five-point ratings scales, the NSHAP ratings expand upon previous research that has typically focused on only one or two features or relied on dichotomous (presence/absence) measures (Simonsen, 1981). Interviewer observations may also be preferable to respondents’ assessments of their own living conditions because the ratings are not as likely to be confounded by respondent characteristics such as psychological distress (Christensen, Carp, Cranz, & Whiley, 1992). Another advantage is that there is very low item-level non-response on the ratings of living conditions (about .05 percent) because field interviewers were required to complete the FIQ in order to close each case.
However, a notable limitation of this approach is the potential for interviewer bias in their assessments of respondents’ living conditions. Field interviewers were not provided with explicit training on how to evaluate respondents’ living conditions. Interviewers’ personal characteristics, their previous interviewing experiences, their subjective appraisal of the respondent, and their social distance or status asymmetry with the respondent may shape how they perceive or rate the respondent’s living conditions. In supplemental analyses, I have examined the degree to which ratings of living conditions vary according to characteristics of the 131 NSHAP field interviewers (also see York 2008). I find that younger interviewers tended to note more disorder, on average, than older interviewers. It is possible that this reflects different personal standards for living conditions or differences in the ability to detect things such as noise and odor. However, disorder ratings do not differ according to race, gender, and prior experience. Nor does racial or gender-based status asymmetry between interviewer and respondent seem to affect ratings of respondents’ living conditions. Yet, recent research has revealed intriguing variations in the perception of neighborhood disorder (Sampson, 2004); attention to subjectivities in the observation and experience of living conditions is an important direction for future work. Given this, I use fixed-effects regression models, as described below, to account for variation in disorder ratings attributable to observed and unobserved differences in interviewers’ perceptions of disorder.
Household Composition and Social Resources
Variables capturing marriage/partnership and household composition, as well as social network size, are drawn from the NSHAP egocentric social network roster. Respondents were asked to list up to five individuals with whom they most often discussed things that were important to them over the last 12 months (see Cornwell et al. 2009). Each respondent was permitted to name up to five network members, and then allowed to name an additional individual with whom they feel particularly close. The respondent was subsequently asked whether each of the individuals live with him or her, and what other individuals (if any) reside in the household. For each individual listed in the network roster and the household roster, respondents indicated their relationship, such as spouse/partner, child, other family member, or friend.
From this information, I derive an indicator of whether the respondent has a co-resident spouse/partner (=1, else = 0) and a count of the respondent’s co-residents. Only about 2 percent of all NSHAP respondents reported more than two co-residents, so I cap the number of co-residents at “3 or more.” I also construct a six-category classification of living arrangements based on the presence of a spouse/partner, child(ren), and other (non-partner, non-child) individuals in the respondent’s household. Keep in mind that most (about 88 percent) of the co-resident children of respondents in this sample are adult children. Table 2 provides descriptive statistics for these and other key variables.
Table 2.
Summary Statistics for Key Variables (n = 2,334)
| Meana or Proportion | Standard Deviation | |
|---|---|---|
| Disordered Living Conditions (Cronbach’s alpha = .826) | −.062 | .744 |
| Household Composition and Social Resources | ||
| Number of co-residentsb | ||
| 0 | .281 | --- |
| 1 | .544 | --- |
| 2 | .103 | --- |
| 3 or more | .073 | --- |
| Co-resident spouse or partner {1 = yes, 0 = no} | .621 | --- |
| Household compositionb | ||
| Living with a spouse/partner only | .484 | --- |
| Spouse/partner and child(ren) | .076 | --- |
| Spouse/partner and other(s) | .062 | --- |
| Living alone | .281 | --- |
| Single, living with child(ren) | .035 | --- |
| Single, living with other(s) | .063 | --- |
| Network members outside of the householdb | ||
| 0–1 | .159 | --- |
| 2–3 | .335 | --- |
| 4–6 | .506 | --- |
| Sources of social support {R can often rely on…}b | ||
| Neither family nor friends | .261 | --- |
| Family only | .310 | --- |
| Friends only | .078 | --- |
| Both family and friends | .350 | --- |
| Respondent Characteristics and Residential Context | ||
| Age (in decades) | 6.799 | .784 |
| Female {1 = yes; 0 = no} | .517 | --- |
| Black {1 = yes; 0 = no} | .100 | --- |
| Hispanic {1 = yes; 0 = no} | .070 | --- |
| Educationb | ||
| Less than high school | .217 | --- |
| High school degree | .272 | --- |
| Some college | .292 | --- |
| College degree or higher | .219 | --- |
| Annual household incomeb | ||
| Less than $25,000 | .346 | --- |
| $25,000 – 49,999 | .301 | --- |
| $50,000 – 99,999 | .241 | --- |
| $100,000 or higher | .113 | --- |
| Physical impairment {number of daily activities that pose at least some difficulty for the respondent; range = 0,7} | .848 | 1.603 |
| Cognitive impairment {number of errors on the SPMSQ; range = 0,10} | .682 | 1.036 |
| Depressive symptoms {score from CES-D; range = 11,44} | 16.378 | 5.220 |
| Poverty rate of census tract (2005–2009 ACS) | .139 | .122 |
| Urbanicity of census tract (2000 Census) | 77.910 | 33.809 |
| Detached single-family home {1 = yes, 0 = no} | .801 | --- |
Survey-adjusted and weighted for probability of selection, with post-stratification adjustments for non-response.
Response proportions and frequencies presented are unweighted.
I use information from network roster, along with the questions about each network members’ residence, to derive a count of network contacts who do not live with the respondent. This variable ranges from 0 to 6. In supplemental analyses, I found that the relationship between non-residential network ties and living conditions is most parsimoniously captured by dividing respondents into three categories: those who have 0–1, 2–3, and 4–6 non-resident network members.
NSHAP assessed respondents’ social support by asking: “How often can you rely on members of your family for help if you have a problem?” and “How often can you rely on friends for help if you have a problem?” Responses ranged from “hardly ever (or never)” to “some of the time” and “often.” Supplemental analyses indicated that respondents’ living conditions are more strongly associated with differences in sources of support rather than frequency of support. Because it provides the most parsimonious representation of the relationship between social support and living conditions, I utilize indicators of whether the respondent can often access instrumental support from neither friends nor family members, family members only, friends only, or both family members and friends.
Respondent Characteristics and Residential Context
I consider the respondent’s age, gender, and racial/ethnic background, as well as educational attainment, based on the highest level of education that he or she had completed. Respondents’ household income was assessed through a series of questions. First, respondents were asked to report the approximate gross income of their households in the previous year. Respondents who refused to answer or indicated that they didn’t know were asked a series of questions allowing them to bracket their income as above or below $25,000, $50,000, or $100,000. I use these two sources of information to categorize respondents’ household income as shown in Table 2.
The poverty rate of the respondent’s census tract is an additional indicator of the respondent’s socioeconomic status, and it may also convey the general quality of his or her housing. The census tracts in which respondents live were determined by research staff at NORC at the University of Chicago, and these census tracts were linked to tract-level poverty rates from the 2005–2009 American Community Survey. Urbanicity was determined based on the percentage of households in the respondent’s census tract that are classified as “urban” according to the 2000 Census. The respondent’s housing type was indicated by the field interviewer; I focus on whether the respondent resides in a detached single-family home (=1, else=0) because it suggests greater control over living conditions compared to dwellings that share walls with neighbors.
Finally, I consider three measures of health that may limit older adults’ capacities to maintain order within their living spaces. Physical impairment was assessed by asking respondents about their ability to complete each of nine tasks, including walking one block, walking across a room, eating, and getting in and out of bed. Second, NSHAP assessed cognitive function using the 10-item Short Portable Mental Status Questionnaire (SPMSQ), which includes items that assess knowledge of general and personal information (Pfeiffer 1975). I utilize a shortened 11-item version of the Center for Epidemiological Studies of Depression Scale (CES-D) (Radloff 1977) assesses depressive symptoms.
Analytic Strategy
The main goal of my analyses is to examine the distribution of disordered living conditions among community-dwelling older Americans. Because the NSHAP data are cross-sectional, causal inferences should be made with caution. Rather than building causal models, I use multiple regression analysis as a tool to examine the net associations between living conditions and social factors.
I use ordinary-least squares regression because the disorder scale is an interval variable. Recall that ratings of living conditions may be shaped by interviewer characteristics. I employ fixed-effects for field interviewers to account for between-interviewer differences that may be associated with the ratings. In the context of OLS regression, this approach effectively enters into the regression equation a dummy variable for each interviewer (Wooldridge, 2002). This should attenuate most of the unobserved heterogeneity in disorder ratings that is attributable to measured and unmeasured interviewer characteristics.
Variance estimates are adjusted for strata and Primary Sampling Units and all models include person-level weights provided with the NSHAP data, which account for differential probabilities of selection into the study (with post-stratification adjustments for non-response). I have modified these NSHAP-provided weights to adjust for potential selection issues related to the exclusion of cases from my analyses. There are three primary reasons why NSHAP respondents may be excluded from my analyses. First, I exclude the 152 respondents who were not interviewed in their homes. Another source of missing cases is related to the modular design of the NSHAP study. Of those who were interviewed in their homes, 939 respondents were randomly selected to respond to questions about social support (and other topics) on a paper-and-pencil questionnaire and return it by mail. However, 147 of these 939 respondents did not return the leave-behind questionnaire. Because these individuals have missing data on social support, they are excluded from all models. Finally, listwise deletion leads 227 respondents to drop out of my models due to missing data on income. An additional 145 respondents are excluded because of item-level non-response or missing data on one of the following variables: type of housing unit, depressive symptoms, social support, racial/ethnic background, census tract poverty rate, and physical impairment, and disordered living conditions. All together, the sample size for each of my models is 2,334. To attenuate potential selection effects caused by the exclusion of respondents, I employ a complete-case weighting form of missing data adjustment (Morgan & Todd, 2008). Adjusting the NSHAP-provided weights by the inverse of the probability that a respondent is included in my analyses effectively affords disproportionate weight to the cases least likely to be included in the analysis.
RESULTS
The distribution of household risks within the older adult population generally reflects broader social inequalities. As shown in Model 1 of Table 3, disordered living conditions are negatively associated with income. This is consistent with my first hypothesis. Older adults who have household incomes of $100,000 or higher have disorder ratings that are more than a third of a standard deviation lower than those whose household incomes were $25,000 or below (b = −.388; p < .001). Those in the highest household income bracket also had significantly lower disorder ratings than those who had incomes of between $25,000 and $49,999 (b = −.388 and b = −.205, respectively; Wald test of difference: F(df = 1, 50) = 11.58; p < .001)). Education is not associated with disorderly living conditions. But, even after adjusting for income, black respondents have disorder ratings that are nearly a quarter of a standard deviation higher than whites, on average. Black older adults also have more stressful or risky living conditions than Hispanic older adults (b = .226 and b = −.017, respectively; Wald test of difference: F(df = 1, 50) = 7.44; p < .01) but living conditions do not differ across Hispanic and white older adults. Finally, older adults who live in poorer neighborhoods have more risky households. A ten percentage point increase in census tract residents whose incomes are below the poverty line is associated with an increase of about .055 on the disorder scale. Living conditions are slightly less disordered among older adults who reside in more urban areas, but housing type is not associated with living conditions.
Table 3.
Results from Fixed-Effects Regressions of Disordered Living Conditions on Social Status and Co-Residencea
| Model 1
|
Model 2
|
Model 3
|
||||
|---|---|---|---|---|---|---|
| b | (SE) | b | (SE) | b | SE) | |
| Age (tens of years) | −.117*** | (.021) | −.111*** | (.020) | −.113*** | (.020) |
| Female | −.093** | (.031) | −.097** | (.031) | −.117** | (.031) |
| Black | .226** | (.065) | .217** | (.064) | .200** | (.064) |
| Hispanic | −.017 | (.070) | −.026 | (.069) | −.034 | (.068) |
| Education | ||||||
| Less than high school (ref.) | --- | --- | --- | --- | --- | --- |
| High school diploma | −.053 | (.063) | −.036 | (.061) | −.043 | (.061) |
| Some college | −.036 | (.057) | −.021 | (.058) | −.035 | (.058) |
| College degree or more | −.063 | (.060) | −.046 | (.058) | −.062 | (.058) |
| Household income | ||||||
| Less than $25,000 (ref.) | --- | --- | --- | --- | --- | --- |
| $25,000 – 49,999 | −.205*** | (.039) | −.183*** | (.039) | −.155*** | (.040) |
| $50,000 – 99,999 | −.307*** | (.054) | −.285*** | (.052) | −.245*** | (.053) |
| $100,000 or higher | −.388*** | (.061) | −.350*** | (.058) | −.306*** | (.060) |
| Neighborhood poverty | .546* | (.209) | .518* | (.212) | .515* | (.203) |
| Urbanicity | −.002* | (.001) | −.002** | (.001) | −.002** | (.001) |
| Detached single-family home | −.020 | (.044) | −.014 | (.045) | −.002 | (.044) |
| Physical impairment | .034* | (.014) | .034* | (.014) | .035* | (.014) |
| Cognitive impairment | .038* | (.019) | .034 | (.018) | .030 | (.019) |
| Depressive symptoms | .011** | (.004) | .010** | (.004) | .010* | (.004) |
| Number of co-residents | ||||||
| 0 (ref.) | --- | --- | --- | --- | ||
| 1 | −.120** | (.035) | .101 | (.067) | ||
| 2 | .062 | (.054) | .271** | (.080) | ||
| 3 or more | .115 | (.060) | .312*** | (.083) | ||
| Co-resident partner | −.272*** | (.067) | ||||
| Constant | .845 | (.201) | .834 | (.197) | .879 | (.197) |
| N | 2,335 | 2,335 | 2,335 | |||
| Number of interviewers | 130 | 130 | 130 | |||
| R-squared | .323 | .334 | .343 | |||
p < .05;
p < .01;
p < .001 (two-tailed tests)
Robust standard errors are presented in parentheses.
As expected, older adults who suffer from functional impairments, depression, and cognitive impairment reside in more disordered living conditions. Net of this, age is negatively associated with disordered living conditions. Female respondents have less disordered living conditions than male respondents. However, because a majority of the NSHAP respondents (61.6 percent) reside with a spouse or partner, the relationship between gender and household risks is difficult to discern here.
Co-Residence and Household Risks
Results in model 2 reveal a non-linear relationship between household size and living conditions. Older adults who reside with one other person have the lowest levels of household risks, on average. Disorder is more prevalent among respondents living alone and among those who reside with two or more other people. There is some evidence that the largest households have more disordered living conditions. Disorder ratings are .115 higher for older adults who live with three or more other people, compared to those who live alone; this difference is marginally significant (b = .115; p = .060).
But who resides in the household may be more important than sheer household size. Model 3 indicates that, as I hypothesized, co-residence with a partner is associated with less disordered living conditions. Older men and women who reside with a partner only have less disordered living conditions. Note that after I account for the presence of a co-resident spouse or partner, household risks increase as a linear function of household size.
The first model in Table 4 introduces a more detailed breakdown of living arrangements. Consistent with my hypothesis, disorder ratings are lowest in households where co-residents are limited to a spouse/partner. Unpartnered older adults who live alone have more disordered living conditions than those who live with a partner only (b = .173; p < .173). However, living conditions of those who live alone differ by gender. An interaction term added to this model in supplemental analyses indicates that women who live alone have disorder scores that are .152 lower, on average, than those of men who live alone (b = .152; p < .05).
Table 4.
Results from Fixed-Effects Regressions of Disordered Living Conditions on Household Composition and Social Resourcesa
| Model 1
|
Model 2
|
Model 3
|
||||
|---|---|---|---|---|---|---|
| b | (SE) | b | (SE) | b | SE) | |
| Age (tens of years) | −.112*** | (.020) | −.111*** | (.020) | −.116*** | (.020) |
| Female | −.115** | (.031) | −.093** | (.032) | −.086* | (.032) |
| Black | .210** | (.065) | .211** | (.064) | .204** | (.064) |
| Hispanic | −.028 | (.068) | −.034 | (.066) | −.038 | (.066) |
| Education | ||||||
| Less than high school (ref.) | --- | --- | --- | --- | --- | --- |
| High school diploma | −.045 | (.059) | −.045 | (.059) | −.043 | (.062) |
| Some college | −.036 | (.057) | −.028 | (.056) | −.029 | (.058) |
| College degree or more | −.062 | (.057) | −.050 | (.057) | −.056 | (.058) |
| Household income | ||||||
| Less than $25,000 (ref.) | --- | --- | --- | --- | --- | --- |
| $25,000 – 49,999 | −.159*** | (.040) | −.155*** | (.039) | −.150*** | (.039) |
| $50,000 – 99,999 | −.243*** | (.053) | −.238*** | (.054) | −.236*** | (.052) |
| $100,000 or higher | −.304*** | (.060) | −.301*** | (.060) | −.303*** | (.060) |
| Neighborhood poverty | .515* | (.206) | .504* | (.207) | .481* | (.200) |
| Urbanicity | −.002** | (.001) | −.002** | (.001) | −.002** | (.001) |
| Detached single-family home | .005 | (.044) | .007 | (.044) | .006 | (.044) |
| Physical impairment | .035* | (.014) | .035** | (.014) | .035* | (.014) |
| Cognitive impairment | .031 | (.019) | .028 | (.019) | .027 | (.020) |
| Depressive symptoms | .010* | (.004) | .010* | (.004) | .008* | (.004) |
| Household composition | ||||||
| Spouse/partner only (ref.) | --- | --- | --- | --- | --- | --- |
| Spouse/partner and child(ren) | .134* | (.065) | .113 | (.065) | .119 | (.068) |
| Spouse/partner and other(s) | .257*** | (.054) | .234*** | (.052) | .240*** | (.054) |
| Lives alone | .173*** | (.035) | .180*** | (.035) | .182*** | (.034) |
| No spouse/partner, lives with child(ren) | .258* | (.122) | .260* | (.121) | .273* | (.125) |
| No spouse/partner, lives with other(s) | .380*** | (.074) | .376*** | (.073) | .379*** | (.073) |
| Non-resident network size | ||||||
| 0–1 member (ref.) | --- | --- | --- | --- | ||
| 2–3 members | −.090* | (.041) | −.073 | (.045) | ||
| 4–6 members | −.135** | (.047) | −.107* | (.046) | ||
| Support sources | ||||||
| Neither family nor friends (ref.) | --- | --- | ||||
| Family only | −.062 | (.039) | ||||
| Friends only | −.007 | (.065) | ||||
| Both family and friends | −.099* | (.040) | ||||
| Constant | .682** | (.193) | .765*** | (.192) | .852*** | (.201) |
| N | 2,335 | 2,335 | 2,335 | |||
| Number of interviewers | 130 | 130 | 130 | |||
| R-squared | .344 | .346 | .349 | |||
p < .05;
p < .01;
p < .001 (two-tailed tests)
Robust standard errors are presented in parentheses.
Partnered and unpartnered older adults who live with a child or children also have more disordered living conditions than those who live with a spouse/partner only (b = .136; p < .05 for partnered older adults living with a child or children; b = .258; p < .05 for unpartnered older adults living with a child or children). These results suggest that households including partnered older adults and their adult child(ren) may have complicated social roles, leading to more disordered living conditions. The most disordered living conditions are found among unpartnered older adults whose households include someone who is not a child. Older adults in these types of households have disorder ratings that are more than a third of a standard deviation higher, on average, than those who live only with a partner (b = .380; p < .001). Older adults who live with a partner as well as another resident who is not a child also have more disordered living conditions than those who reside with a partner only.
However, I do not find significant differences between nuclear and non-nuclear living arrangements. Older adults who reside with a partner and non-child do not have significantly higher disorder ratings than those who reside with a partner and a child or children (Wald test of difference: F(df = 1, 50) = 2.11; p = .153). Nor do unpartnered older adults who live with a non-child have higher disorder ratings than those who reside with a child or children (Wald test of difference: F(df = 1, 50) = .81; p = .373). These findings do not support my hypothesis that nuclear households have less disordered conditions than non-nuclear households. But it is important to note that these relationships between household composition and living conditions persist net of household income. This provides some evidence that the differences in living conditions do not simply reflect socioeconomic disadvantages that may lead to the formation of combined or non-nuclear households.
Social Network Ties, Social Support, and Household Risks
Model 2 in Table 4 shows that, as expected, older adults who have more social network connections outside of the household have less disordered living conditions. Having two or more non-residential network ties is associated with fewer risky or harmful living conditions. Those who have a large number of non-residential network ties (4–6 ties) have disorder ratings that are .135 lower, on average, than those who have 0–1 ties. But the difference in disorder ratings across older adults with 2–3 non-residential network members and those with 4–6 is not significant (b = −.090 and b = −.135, respectively; Wald test of difference in coefficients: F(1,50) = 2.26; p = .139).
Social support is added in the next model. Consistent with my hypothesis, older adults who have more social support are less likely to be reside in risky or harmful living conditions. But it is diversity of support – not simply having support from one type of source – that is associated with less disordered conditions. Older adults who can rely on either friends or family members do not have lower disorder ratings; but those who can rely on both family and friends enjoy less disordered living conditions (b = −.099; p < .05). Note that both household composition and non-residential network ties are also associated with disordered living conditions, net of social support. This suggests that each of these social factors contributes to living conditions through separate pathways.
I find some evidence that social support may be particularly important for older adults who live alone. In supplemental analyses, I tested interaction terms crossing living alone with each of the indicators of social support. The interactions with support from family only and support from friends only are not significant. But having support from both family and friends is more strongly related to living conditions for those who live alone (b = −.256; p < .01). Therefore, disordered living conditions may be another factor increasing the vulnerability of older adults who live alone and are socially isolated. However, it is possible that having more support allows individuals to live alone in the first place – or that some other factor, such as personality or health, is associated with living alone, more ordered living conditions, and greater availability of support. More research and studies using longitudinal data are needed to explore these possibilities.
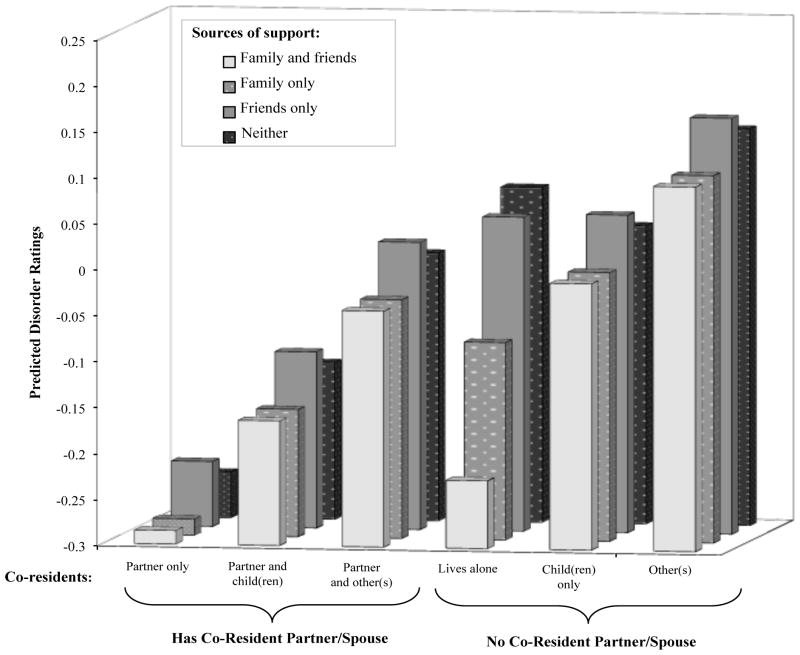
Figure 2 illustrates how both household composition and social support are associated with living conditions. The bars indicate predicted disorder ratings based on Model 3 with the inclusion of the interaction term for those who live alone. Respondents who live only with a spouse/partner have the most orderly living spaces overall, while those who reside in non-nuclear or non-partnered living arrangements have the highest disorder ratings. But the availability of social support serves as a buffer – particularly for those who live alone. In fact, older adults who live alone and do not have instrumental support from family members have predicted disorder ratings that are similar to those who reside in larger, non-nuclear households. On the other hand, those who live alone and can rely on both family and friends have less disordered living conditions – similar to those enjoyed by individuals who live with only a spouse or partner.
Figure 2. Disordered Living Conditions, by Household Composition and Social Support.
Note: This figure plots adjusted mean household risk scores calculated using the coefficients from Model 3 in Table 4, with the inclusion of interaction terms crossing living alone with social support. Values of other predictors included in that model are held constant at their mean (for scale variables) or mode (for categorical variables).
DISCUSSION
The health risks of inadequate and unsafe housing are so well-established that recent reviews have referred to the growing prevalence of substandard housing as a public health crisis (Bashir, 2002). For older adults, in particular, much attention has been devoted to the challenge of building communities and providing housing options that meet the needs of individuals who may be coping with chronic illness, disablement, and social isolation (American Association of Retired Persons, 2005). But less attention has been devoted to the interior conditions of older adults’ homes. Most older adults want to remain in their homes as long as possible, but for some individuals, exposure to disordered physical and ambient conditions may significantly increase their risk of infection, illness, disablement, and decline.
Consistent with existing policy-related research and studies of environmental health, (see, e.g., Evans & Kantrowitz, 2002; Frumkin, 2005), I find that household risks reflect social disadvantage. Black older adults, as well as those with lower incomes and those who reside in poorer neighborhoods, have living conditions that present more risks for their physical and mental health. Differences in living conditions across black and white older adults may be another disadvantage stemming from discriminatory housing practices that sort minorities into lower quality housing. At the same time, higher incomes enable some older adults to afford better quality housing and pay for assistance with home repairs or housekeeping. Rates of homeownership may play an important role in the extent to which some groups are able to modify their dwellings, but I was unable to examine that here. Nevertheless, disparities observed in this study of living conditions may therefore contribute to persistent inequalities in trajectories of health and aging.
My main argument is that social resources available in and around the household may also be associated with interior living conditions. Preventing or addressing the emergence of disorder within one’s living space requires effort on the part of residents and their family members, in addition to financial resources. Consistent with this, I found evidence that co-residential relationships are associated with living conditions. Older adults who live with a spouse have the lowest disorder ratings across all of the living arrangement categories. This is good news, since over half of non-instutionalized adults over the age of 65 reside with a spouse (Administration on Aging, 2011). But it is important to note that some older adults are more likely to benefit from co-resident partnership than others. Older men are more likely to have a co-resident partner than older women. In the NSHAP sample, more than 76 percent of the male respondents have a co-resident partner compared to only 48 percent of the female respondents. African-American older adults in this sample are also less likely than whites to have a coresident partner (42.55 percent and 65.90 percent, respectively). Thus, white men are disproportionately benefitting from residing in a partnered household in later life, when living conditions may be critical for trajectories of health and well being.
I find that partnered older adults who reside with a child have more disordered living conditions than those who live with only their partner. Because most of these older adults are residing with adult children, this household composition may result from financial strain or caregiving needs that typically drive elderly parents to co-reside with their adult children. And these living situations may complicate social roles and strain relationships. As I expected, non-partnered individuals and those who reside with someone who is not a spouse or child are also likely to endure more stressful or risky living conditions. Drawing from sociological research on the household division of labor and family structure, I argued that non-nuclear households involve less clear social roles, lower levels of support and control, and more distant relationships – all of which may weaken cooperation around household tasks. Although I do not find that non-nuclear households bring a distinct disadvantage, more research is needed to explore how qualitative features of co-residential relationships may shape living conditions and therefore put some older adults at risk of declines in physical and mental health.
I also found evidence that interior living conditions reflect non-residential social resources. Previous research has not explored the role of social networks and social support for older adults’ living conditions. Results from this study indicate that older adults who have fewer social network ties and less social support have living environments that present more physical and ambient risks. Non-residential network ties may provide access to information or resources that enable housekeeping and home maintenance. And, even after accounting for non-residential network ties, access to instrumental support from family members and friends is associated with less disordered living conditions.
An important implication of these findings is that interior living conditions may be a key mechanism through which social relationships affect health and well-being. Previous research on the household context and health has indicated, for example, that living arrangements are consequential for older adults’ physical and mental health. Married couples living alone or with children are particularly advantaged, enjoying lower rates of functional impairment and better self-rated health (Hughes & Waite, 2002; Waite & Hughes, 1999). My results suggest that older adults in these living situations may fare better because partners and/or family members are able to organize and cooperate to keep disorder at bay.
Similarly, the effects of network ties and social support on health are well-documented – but the mechanisms through which social resources are beneficial have not been fully elaborated (Berkman, et al. 2000; Thoits, 2011; Umberson, Crosnoe, & Reczek, 2010). The findings here suggest an underexplored possibility – that social connectedness and social support may enhance housekeeping and home maintenance for older adults residing in the community. Social connectedness may be particularly important for the living conditions of older adults who live alone, because they must depend on non-residential family and friends for help with household tasks.
From a broader standpoint, these results highlight the fact that the conditions of the home environment are linked with the social relationships and interactions that occur in and around this space. Research on neighborhoods has long recognized that physical neighborhood features can provide visual cues signifying the presence of social order, social cohesion, and social capital (Ross & Mirowsky 1999; Sampson & Raudenbush, 1999). Following this, disordered living conditions may signal that an older adult faces challenges that outweigh available social resources. Clutter, a lack of cleanliness, odors, and structural disrepair may indicate a lack of access to social capital and inadequate social support. Indeed, social service organizations often use living conditions as indicators of overall well being, with features of decay and disrepair suggesting neglect, mistreatment, and abuse (see, e.g., Fulmer, Guadagno, Dyer, and Connoly 2004; McKeever et al. 2006). In this sense, social service agencies already recognize the link between living conditions and social resources that I have tested in this paper. From a policy-oriented standpoint, greater attention to the types of social relationships that are associated with better living conditions or fewer in-home risks could inform community and social programs aimed at helping seniors to remain safe and comfortable in their own homes.
The goal of this paper has been to describe the living conditions of community-residing older adults and examine how co-residence, social network ties, and social support are associated with stressful, risky, and disordered conditions. This project has been limited to cross-sectional analyses, which have not allowed me to identify causal directions or pathways. Thus, my results indicate associations, but I cannot elucidate the extent to which the social affects the physical, and vice versa. It is important to note that physical and ambient living conditions may also affect social relationships and support. There is some evidence that residence in low-quality housing or cluttered, cramped, and noisy households can weaken co-residential relationships (Gove, Hughes, & Galle, 1979) and lead to social withdrawal (Wells & Harris, 2007). Stressful living conditions may strain relationships among co-residents, or discourage family members from visiting. Longitudinal analyses and qualitative research on social interactions in household context will be particularly useful for unpacking the dynamic processes through which older adults’ living conditions shape – and are shaped by – their social relationships.
Acknowledgments
Support for this research was provided by a National Institute on Aging Predoctoral Fellowship and Pilot Funding from the Center on Demography and Economics of Aging at NORC and the University of Chicago (P30 AG012857). Support was also provided by the National Social Life, Health, and Aging Project, which is funded by the National Institutes of Health (R01 AG021487; R01 AGO33903), including the National Institute on Aging, the Office of Women’s Health Research, the Office of AIDS Research, and the Office of Behavioral and Social Sciences Research. I thank Linda Waite, Kathleen Cagney, Benjamin Cornwell, Edward Laumann, and Phil Schumm for comments and suggestions in the development of this research.
Biography
Erin York Cornwell is assistant professor of sociology at Cornell University. Her research examines the mechanisms through which social context affects older adults’ health and well being. Previous work has been published in Journal of Health and Social Behavior, Journals of Gerontology, and Annual Review of Gerontology and Geriatrics.
References
- Administration on Aging. A Profile of Older Americans: 2011. U.S. Department of Health & Human Services; 2011. [Google Scholar]
- Allen SM, Webster PS. When Wives Get Sick: Gender Role Attitudes, Marital Happiness, and Husbands’ Contributions to Household Labor. Gender and Society. 2001;15(6):898–916. [Google Scholar]
- American Association of Retired Persons. Beyond 50.05: A Report to the Nation on Liveable Communities: Creating Environments for Successful Aging. Washington, D.C: 2005. [Google Scholar]
- Bashir SA. Home is Where the Harm Is: Inadequate Housing as a Public Health Crisis. American Journal of Public Health. 2002;92(5):733–738. doi: 10.2105/ajph.92.5.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From Social Integration to Health: Durkheim in the New Millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. The Logic of Practice. Stanford, CA: Stanford University Press; 1980 [1970]. The Kabyle House or the World Reversed; pp. 271–283. [Google Scholar]
- Bronfenbrenner U, Evans GW. Developmental Science in the 21st Century. Social Development. 2000;9:115–125. [Google Scholar]
- Brown P. Race, Class, and Environmental Health: A Review and Systematization of the Literature. Environmental Research. 1995;69:15–30. doi: 10.1006/enrs.1995.1021. [DOI] [PubMed] [Google Scholar]
- Cagney KE, Cornwell York. Neighborhoods and Health in Later Life: The Intersection of Biology and Community. Annual Review of Gerontology and Geriatrics. 2010;30:323–348. [Google Scholar]
- Chapin FS. Contemporary American Institutions. New York: Harper; 1935. [Google Scholar]
- Choi NG. Coresidence between Unmarried Aging Parents and their Adult Children: Who Moved in with Whom and Why? Research on Aging. 2003;25:384–404. [Google Scholar]
- Christensen DL, Carp FM, Cranz GL, Whiley JA. Objective Housing Indicators as Predictors of the Subjective Evaluations of Elderly Residents. Journal of Environmental Psychology. 1992;12:225–236. [Google Scholar]
- Coltrane S. Research on Household Labor: Modeling and Measuring the Social Embeddedness of Routine Family Work. Journal of Marriage and the Family. 2000;62(4):1208–1233. [Google Scholar]
- Conley D. A Room With a View or a Room of One’s Own?: Housing and Social Stratification. Sociological Forum. 2001;16:263–280. [Google Scholar]
- Cornman JC, Goldman N, Glei DA, Weinstein M, Chang M. Social Ties and Perceived Support: Two Dimensions of Social Relationships and Health among the Elderly in Taiwan. Journal of Aging and Health. 2003;15:616–644. doi: 10.1177/0898264303256215. [DOI] [PubMed] [Google Scholar]
- Cornwell B, Schumm P, Laumann EO, Graber J. Social Networks in the NSHAP Study: Rationale, Measurement, and Preliminary Findings. Journal of Gerontology: Social Sciences. 2009;64B(Suppl 1):i45–i55. doi: 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW. The Built Environment and Mental Health. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2003;80:536–555. doi: 10.1093/jurban/jtg063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Hygge S, Bullinger M. Chronic Noise and Psychological Stress. Psychological Science. 1995;6:333–338. [Google Scholar]
- Evans GW, Kantrowitz E. Socioeconomic Status and Health: The Potential Role of Environmental Risk Exposure. Annual Review of Public Health. 2002;23:303–331. doi: 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- Fänge A, Iwarsson S. Changes in ADL Dependence and Aspects of Usability Following Housing Adaptation – A Longitudinal Perspective. American Journal of Occupational Therapy. 2005;59:296–304. doi: 10.5014/ajot.59.3.296. [DOI] [PubMed] [Google Scholar]
- Fisk WJ, Lei-Gomez Q, Mendell MJ. Meta-Analyses of the Associations of Respiratory Health Effects with Dampness and Mold in Homes. Indoor Air. 2007;17:284–295. doi: 10.1111/j.1600-0668.2007.00475.x. [DOI] [PubMed] [Google Scholar]
- Frumkin H. Health, Equity, and the Built Environment. Environmental Health Perspectives. 2005;113(5):290–291. doi: 10.1289/ehp.113-a290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulmer T, Guadagno L, Dyer CB, Connolly MT. Progress in Elder Abuse Screening and Assessment Instruments. Journal of the American Geriatrics Society. 2004;52:297–304. doi: 10.1111/j.1532-5415.2004.52074.x. [DOI] [PubMed] [Google Scholar]
- Gitlin Laura N. Conducting Research on Home Environments: Lessons Learned and New Directions. The Gerontologist. 2003;43:628–637. doi: 10.1093/geront/43.5.628. [DOI] [PubMed] [Google Scholar]
- Golant SM, LaGreca AJ. Differences in Housing Quality of White, Black, and Hispanic U.S. Elderly Households. Journal of Applied Gerontology. 1994a;13:413–437. [Google Scholar]
- Golant SM, LaGreca AJ. Housing Quality of U.S. Elderly Households: Does Aging in Place Matter? The Gerontologist. 1994b;34:803–814. doi: 10.1093/geront/34.6.803. [DOI] [PubMed] [Google Scholar]
- Goldscheider FK, Waite LJ. New Families, No Families? The Transformation of the American Home. Berkeley, CA: University of California Press; 1991. [Google Scholar]
- Gomez-Jacinto L, Hombrados-Mendieta I. Multiple Effects of Community and Household Crowding. Journal of Environmental Psychology. 2002;22:233–246. [Google Scholar]
- Gove WR, Hughes M, Galle OR. Overcrowding in the Home: An Empirical Investigation of Its Possible Pathological Consequences. American Sociological Review. 1979;44(1):59–80. [PubMed] [Google Scholar]
- Hochschild A. The Second Shift. New York: Avon Books; 1989. [Google Scholar]
- Hughes ME, Waite LJ. Health in Household Context: Living Arrangements and Health in Late Middle Age. Journal of Health and Social Behavior. 2002;43:1–21. [PMC free article] [PubMed] [Google Scholar]
- Iwarsson S. A Long-Term Perspective on Person-Environment Fit and ADL Dependence among Older Swedish Adults. Gerontologist. 2005;45:327–336. doi: 10.1093/geront/45.3.327. [DOI] [PubMed] [Google Scholar]
- Krantz-Kent R, Stewart J. How Do Older Americans Spend Their Time? Monthly Labor Review. 2007;130:8–26. [Google Scholar]
- Kwak M, Ingersoll-Dayton B, Kim J. Family Conflict from the Perspective of Adult Child Caregivers: The Influence of Gender. Journal of Social and Personal Relationships. 2012;29:470–487. [Google Scholar]
- Laditka JN, Laditka SB. Aging Children and Their Older Parents: The Coming Generation of Caregiving. Journal of Women & Aging. 2000;12:189–204. doi: 10.1300/J074v12n01_12. [DOI] [PubMed] [Google Scholar]
- Lawton MP. Environment and Other Determinants of Well-Being in Older People. The Gerontologist. 1983;23:349–357. doi: 10.1093/geront/23.4.349. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Nahemow L. Ecology and the Aging Process. In: Eisdorfer C, Lawton MP, editors. Psychology of Adult Development and Aging. Washington, D.C: American Psychological Association; 1973. pp. 619–674. [Google Scholar]
- Laumann EO, House JS. Living Room Styles and Social Attributes: The Patterning of Material Artifacts in a Modern Urban Community. Sociology and Social Research. 1970;54:321–342. [Google Scholar]
- Lee RPL, Ruan D, Lai G. Social Structure and Support Networks in Beijing and Hong Kong. Social Networks. 2005;27:249–274. [Google Scholar]
- Lee YS, Waite LJ. How Appreciated Do Wives Feel for the Housework They Do? Social Science Quarterly. 2010;91(2):476–492. [Google Scholar]
- Lewis MA, Rook KS. Social Control in Personal Relationships: Impact on Health Behaviors and Psychological Distress. Health Psychology. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- Liu SY, Lapane KL. Residential Modifications and Decline in Physical Function among Community-Dwelling Older Adults. The Gerontologist. 2009;49:344–354. doi: 10.1093/geront/gnp033. [DOI] [PubMed] [Google Scholar]
- McKeever PD, Scott HM, Chipman ML, Osterlund K, Eakin JM. Hitting Home: A Survey of Housing Conditions of Homes Used for Long-Term Care in Ontario. International Journal of Health Services. 2006;36:521–533. doi: 10.2190/764R-NQY9-RXEV-3FGT. [DOI] [PubMed] [Google Scholar]
- Morgan SL, Todd JJ. A Diagnostic Routine for the Detection of Consequential Heterogeneity of Causal Effects. Sociological Methodology. 2008;38:231–281. [Google Scholar]
- Myers D, Lee SW. Immigration Cohorts and Residential Overcrowding in Southern California. Demography. 1996;33:51–65. [PubMed] [Google Scholar]
- Newman S. The Living Conditions of Elderly Americans. The Gerontologist. 2003;43(1):99–109. doi: 10.1093/geront/43.1.99. [DOI] [PubMed] [Google Scholar]
- O’Brien E, Wu KB, Baer D. Older Americans in Poverty: A Snapshot. Washington, D.C: AARP Public Policy Institute; 2010. [Google Scholar]
- O’Muircheartaigh C, Eckman S, Smith S. Statistical Design and Estimation for the National Social Life, Health, and Aging Project. Journals of Gerontology, Series B: Psychological and Social Sciences. 2009;64B(S1):i12–i19. doi: 10.1093/geronb/gbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald F, Wahl HW. Housing and Health in Later Life. Reviews on Environmental Health. 2004;19(3–4):223–252. [PubMed] [Google Scholar]
- Oswald F, Wahl H-W, Martin M, Mollenkopf H. Toward Measuring Proactivity in Person-Environment Transactions in Late Adulthood: The Housing-Related Control Beliefs Questionnaire. Journal of Housing for the Elderly. 2003;17:135–152. [Google Scholar]
- Perkins HW, DeMeis DK. Gender and Family Effects on the ‘Second-Shift” Domestic Activity of College-Educated Young Adults. Gender & Society. 1996;10(1):78–93. [Google Scholar]
- Pfeffer E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients. Journal of the American Geriatric Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Piercy KW. Characteristics of Strong Commitments to Intergenerational Family Care of Older Adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62:S381–S387. doi: 10.1093/geronb/62.6.s381. [DOI] [PubMed] [Google Scholar]
- Pynoos J. Toward a National Policy on Home Modification. Technology and Disability. 1993;2:1–8. [Google Scholar]
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rauh VA, Landrigan PJ, Claudio L. Housing and Health: Intersection of Poverty and Environmental Exposures. Annals of the New York Academy of Sciences. 2008;1136:276–288. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- Regoeczi WC. Crowding in Context: An Examination of the Differential Responses of Men and Women to High-Density Living Environments. Journal of Health and Social Behavior. 2008;49(3):254–268. doi: 10.1177/002214650804900302. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Disorder and Decay: The Concept and Measurement of Perceived Neighborhood Disorder. Urban Affairs Review. 1999;34:412–432. [Google Scholar]
- Sampson RJ, Raudenbush SW. Seeing Disorder: Neighborhood Stigma and the Social Construction of “Broken Windows”. Social Psychology Quarterly. 2004;67(4) [Google Scholar]
- Sampson RJ, Raudenbush SW. Systematic Social Observation of Public Spaces: A New Look at Disorder in Urban Neighborhoods. American Journal of Sociology. 1999;105:603–651. [Google Scholar]
- Sattin RW, Rodriguez JG, DeVito CA, Wingo PA. Home Environmental Hazards and the Risk of Fall Injury Events Among Community-Dwelling Older Persons. Journal of the American Geriatrics Society. 1998;46:669–676. doi: 10.1111/j.1532-5415.1998.tb03799.x. [DOI] [PubMed] [Google Scholar]
- Seeman T, Berkman LF. Structural Characteristics of Social Networks and Their Relationships with Social Support in the Elderly: Who Provides Support. Social Science and Medicine. 1988;I26:737–749. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- Shelton BA, John D. The Division of Household Labor. Annual Review of Sociology. 1996;22:299–322. [Google Scholar]
- Simonsen J. Measuring Inadequate Housing Through the Use of the Annual Housing Survey. U.S. Department of Housing and Urban Development, Office of Policy Development and Research; 1981. [Google Scholar]
- Skogan W. Disorder and Decline: Crime and the Sprial of Decay in American Neighborhoods. Berkeley: University of California Press; 1990. [Google Scholar]
- Smith KP, Christakis NA. Social Networks and Health. Annual Review of Sociology. 2008;34:405–429. [Google Scholar]
- South SJ, Spitze G. Housework in Marital and Nonmarital Households. American Sociological Review. 1994;59:327–347. [Google Scholar]
- Spitze G. Getting Help with Housework: Household Resources and Social Networks. Journal of Family Issues. 1999;20(6):724–745. [Google Scholar]
- Stanwell-Smith R. The Infection Potential in the Home and the Role of Hygiene: Historical and Current Perspectives. International Journal of Environmental Health Research. 2003;13:S9–S17. doi: 10.1080/0960312031000102769. [DOI] [PubMed] [Google Scholar]
- Staples SL. Human Response to Environmental Noise: Psychological Research and Public Policy. American Psychologist. 1996;51(2):143–150. doi: 10.1037//0003-066x.51.2.143. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Mechanisms Linking Social Ties and Support to Physical and Mental Health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Umberson D. Family Status and Health Behaviors: Social Control as a Dimension of Social Integration. Journal of Health and Social Behavior. 1987;28:306–319. [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social Relationships and Health Behavior Across the Life Course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The Disablement Process. Social Science and Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Waite LJ, Hughes ME. At Risk on the Cusp of Old Age: Living Arrangements and Functional Status Among Black, White, and Hispanic Adults. Journal of Gerontology. 1999;54B(3):S136–S144. doi: 10.1093/geronb/54b.3.s136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl HW, Fänge A, Oswald F, Gitlin LN, Iwarsoon Susanne. The Home Environment and Disability-Related Outcomes in Aging Individuals: What Is the Empirical Evidence? The Gerontologist. 2009;49:355–367. doi: 10.1093/geront/gnp056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells NM, Harris JD. Housing Quality, Psychological Distress, and the Mediating Role of Social Withdrawal: A Longitudinal Study of Low-Income Women. Journal of Environmental Psychology. 2007;27:69–78. [Google Scholar]
- Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2002. [Google Scholar]
- Yen IH, Michael YL, Perdue L. Neighborhood Environment in Studies of Health of Older Adults: A Systematic Review. American Journal of Preventative Medicine. 2009;37:455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York E. Household Disorder. (Doctoral dissertation.) 2008. Retrieved from ProQuest Dissertations and Theses. [Google Scholar]
- Zaharna M, Guilleminault C. Sleep, Noise, and Health: Review. Noise and Health. 2010;12:64–69. doi: 10.4103/1463-1741.63205. [DOI] [PubMed] [Google Scholar]