Abstract
Study Objective:
To determine whether preoperatively untreated obstructive sleep apnea (OSA) affects postoperative outcomes.
Design:
Cohort study of patients undergoing surgery between July 2012 and September 2013, utilizing prospectively collected data from the Michigan Surgical Quality Collaborative. Multivariable regression models were used to compare complication rates between treated and untreated OSA, while adjusting for important patient covariates and clustering within hospitals.
Setting:
Fifty-two community and academic hospitals in Michigan.
Patients:
Adult patients undergoing various general or vascular operations were categorized as: (1) no diagnosis or low risk of OSA; (2) documented OSA without therapy or suspicion of OSA; and (3) diagnosis of OSA with treatment (e.g., positive airway pressure).
Exposures:
OSA, preoperatively treated or untreated, was the exposure variable. Postoperative 30-day cardiopulmonary complications including arrhythmias, cardiac arrest, myocardial infarction, unplanned reintubation, pulmonary embolism, and pneumonia were the outcomes of interest.
Measurements and Results:
Of 26,842 patients, 2,646 (9.9%) had a diagnosis or suspicion of OSA. Of those, 1,465 (55.4%) were untreated. Patient and procedural risk factors were evenly balanced between treated and untreated groups. Compared with treated OSA, untreated OSA was independently associated with more cardiopulmonary complications (risk-adjusted rates 6.7% versus 4.0%; adjusted odds ratio [aOR] = 1.8, P = 0.001), particularly unplanned reintubations (aOR = 2.5, P = 0.003) and myocardial infarction (aOR = 2.6, P = 0.031).
Conclusions:
Patients with obstructive sleep apnea (OSA) who are not treated with positive airway pressure preoperatively are at increased risks for cardiopulmonary complications after general and vascular surgery. Improving the recognition of OSA and ensuring adequate treatment may be a strategy to reduce risk for surgical patients with OSA.
Citation:
Abdelsattar ZM, Henren S, Wong SL, Campbell DA, Ramachandran SK. The impact of untreated obstructive sleep apnea on cardiopulmonary complications in general and vascular surgery: a cohort study. SLEEP 2015;38(8):1205–1210.
Keywords: obstructive sleep apnea, surgery, outcomes
INTRODUCTION
Obstructive sleep apnea (OSA) is a highly prevalent co-morbid condition in adult surgical populations. Approximately one in 4 middle-aged men and one in 10 women in the United States are estimated to have OSA.1 OSA is increasingly being recognized as a risk factor for adverse postoperative complications.2–6 Despite the growing awareness of OSA's effect on postoperative outcomes, up to 80% of patients presenting for surgery may actually have undiagnosed OSA and are therefore untreated for this condition.1,7 In other words, adults may present for surgery without adequate preoperative risk assessment for OSA, possibly putting them at heightened risk for postoperative complications. Therefore, the American Society of Anesthesiologists (ASA) has issued practice guidelines specific to the perioperative management of patients with OSA.8 In these guidelines, the ASA recommends screening patients for OSA prior to surgery and implementing special care pathways if OSA is present. However, these recommendations are based on expert opinion in the absence of scientific evidence on whether screening and preoperative therapy are associated with improved outcomes.1,8
Although previous research has demonstrated that patients who are known to have OSA have worse postoperative cardio-pulmonary outcomes than patients without this diagnosis,3–6 these studies do not specifically identify patients who are not treated preoperatively or those who have the disease but are otherwise undiagnosed. For example, in a large national study, Memtsoudis and colleagues6 reported significantly worse postoperative pulmonary outcomes, including aspiration pneumonia, acute respiratory distress syndrome, and emergent endotracheal intubation, in patients with OSA compared with those without OSA. In another study, Mokhlesi and colleagues3 show that OSA is associated with emergent intubation and subsequent prolonged hospital stays, higher costs, and inpatient mortality. Although these studies have several important findings, their major limitation is the reliance on existing diagnosis codes to identify patients with OSA using administrative data. Given that OSA is likely under-diagnosed in the general adult population, using diagnosis codes alone essentially ignores this patient population. Second, even in patients who do carry a diagnosis code for OSA, it is not known if these patients are receiving preoperative positive airway pressure (PAP) therapy to optimize their condition. Thus, it is impossible from these studies to draw any conclusions about a large proportion of patients, who are undiagnosed or untreated preoperatively.
In this context, we sought to investigate the prevalence of OSA in patients presenting for general and vascular surgery at diverse practice settings, community and academic, in the state of Michigan. Using a screening instrument, we prospectively identify patients who are potentially undiagnosed and those who are untreated preoperatively. More specifically, we hypothesize that patients, who are at high risk of having OSA or are preoperatively untreated, have higher rates of cardio-pulmonary complications than patients with known OSA who are treated preoperatively. The results of this study would provide a basis for an increase in the utilization of resources for screening surgical patients preoperatively, and guide health-care providers toward developing strategies aimed at reducing postoperative risks for surgical patients with OSA.
METHODS
Data Sources
The Michigan Surgical Quality Collaborative (MSQC) is a 52-hospital consortium representing diverse practice settings, community and academic, throughout the state. MSQC data abstraction and data quality assurance details have been described elsewhere.9–12 In brief, specially trained data abstractors prospectively collect patient characteristics, intraoperative processes of care, and 30-day postoperative outcomes for patients undergoing specified general and vascular surgical operations utilizing a sampling algorithm that minimizes selection bias. This algorithm divides each calendar year into 46 8-day cycles, from which the first 25 consecutive surgical operations that meet MSQC inclusion criteria are selected. The cycle rotates every 8 days to ensure that every cycle begins with a different day of the week. The MSQC does not collect data for patients younger than 18 y, those categorized as ASA class 6, those undergoing bariatric, trauma, or transplant surgeries, nor for surgeries performed within 30 days of another surgery captured by MSQC. Certain very high-volume operations, such as laparoscopic cholecystectomy, are limited to the first three cases in each cycle so that these surgical procedures do not overwhelm the database. Regular data audits ensure registry data validity in accordance with established policies and procedures.11 Data collection for MSQC is Institutional Review Board (IRB) exempt at participating hospitals, and the current study was reviewed and deemed “non-regulated” by the University of Michigan's IRB.
Patient Population
Patients aged 18 y and older undergoing general abdominal or vascular surgery from July 2012 to September 2013 at any of 52 MSQC community and academic hospitals were included in this study.
Independent Variables
Registry-based clinical and demographic data analyzed included age, race, sex, ASA class, surgical priority, and body mass index (BMI). Comorbidities included preoperative cardiac, pulmonary, renal, neurological, hematological, infectious, and endocrine diagnoses. A composite variable for comorbidity index was created based on the presence or absence of these comorbid conditions, and patients were categorized as having 0 comorbid conditions; 1 comorbid condition; or 2+ comorbidities.
Exposure Variable
OSA was the main exposure variable in this study and was abstracted from the emergency department records, hospital admission notes, and the anesthesia preoperative assessment records. This variable had the following three mutually exclusive categories:
No OSA: No documented diagnosis nor suspicion of OSA.
Untreated or undiagnosed OSA: Documented diagnosis or suspicion of OSA but no regular use of a PAP device at home by patient self-report, or if there was documentation of a minimum 3 out of 8 score on the STOP-BANG questionnaire. The proportions of patients with a diagnosis, suspected or assigned in this category based on STOP-BANG questionnaire were not captured at the time of data collection by the nurse abstractors. In addition, each patient's individual score was not collected.
Treated OSA: Documented diagnosis of OSA and regular use of PAP at home by patient self-report.
The STOP-BANG questionnaire has been previously published and validated.13,14 A score of ≥ 3 has been shown to have a high sensitivity for detecting moderate and severe OSA, whereas individuals with scores < 3 are considered to be at low risk of having OSA. The questionnaire includes the following items snoring; tiredness, fatigue, or excessive daytime sleepiness; observed episode of apnea; high blood pressure; BMI > 35; Age > 50 y; neck circumference > 40 cm; and male gender. Data on the STOP-BANG variables is routinely collected as part of the preoperative screening of patients presenting for surgery.
Main Outcome Measures
The development of any cardiopulmonary complication within 30 days of the index surgery was the main outcome of interest in this study. Cardiopulmonary complications included any arrhythmias, cardiac arrest, myocardial infarction, unplanned reintubation, pulmonary embolism, and pneumonia occurring up to 30 days from the index surgery. Each complication was further studied separately as a secondary outcome to identify the specific associations with OSA.
Statistical Analyses
Clinical and demographic variables for patients who underwent general or vascular surgery at one of 52 MSQC hospitals across the three categories of OSA exposure were analyzed using Chi-square tests for categorical variables and one-way analysis of variance tests with the Scheffé method for multiple comparisons for continuous variables as indicated, with significance set at P < 0.05.
Multivariable logistic regression was used to examine the associations between the main exposure variable and the outcomes of interest. The patient covariates included in the models were age, sex, BMI, ASA class, procedure type, emergency status, comorbidity index, and smoking status. The independent variables were selected empirically based on prior literature.15 In total, there were seven models—one for each outcome—using the same list of independent variables. The models were evaluated for discrimination using the c-statistic. The c-statistic evaluates model discrimination and represents the area under the receiver operator characteristic curve.
Next, we calculated the risk-adjusted rates for the specific outcomes, with which there were a statistically significant association with the OSA exposure variable. The β coefficients of the covariates generated by the multivariable model allow for the calculation of an adjusted rate for each category in the exposure variable. This is achieved by fixing the value of the exposure variable for each patient while keeping all other covariate values as they were observed. This method, in essence, creates two hypothetical populations—one where all patients have untreated OSA, and one where all patients have treated OSA—that have the exact same values on the other covariates in the model. The logic is similar to that of matching studies, where subjects have identical values on every independent variable except one (the exposure). In Stata statistical software, this is performed using the –margins– command.16 This analysis was limited to the two OSA groups as the primary focus of this study is to compare treated versus untreated OSA, and the OSA groups are comparably similar in terms of the other patient covariates.
An additional model, which included the individual co-morbid condition instead of the comorbidity index, was used to test the robustness of the association with the outcomes in a post hoc analysis. The results were qualitatively similar and thus not presented. All statistical analyses were conducted using Stata special edition (version 13.1, StataCorp, College Station, TX, USA).
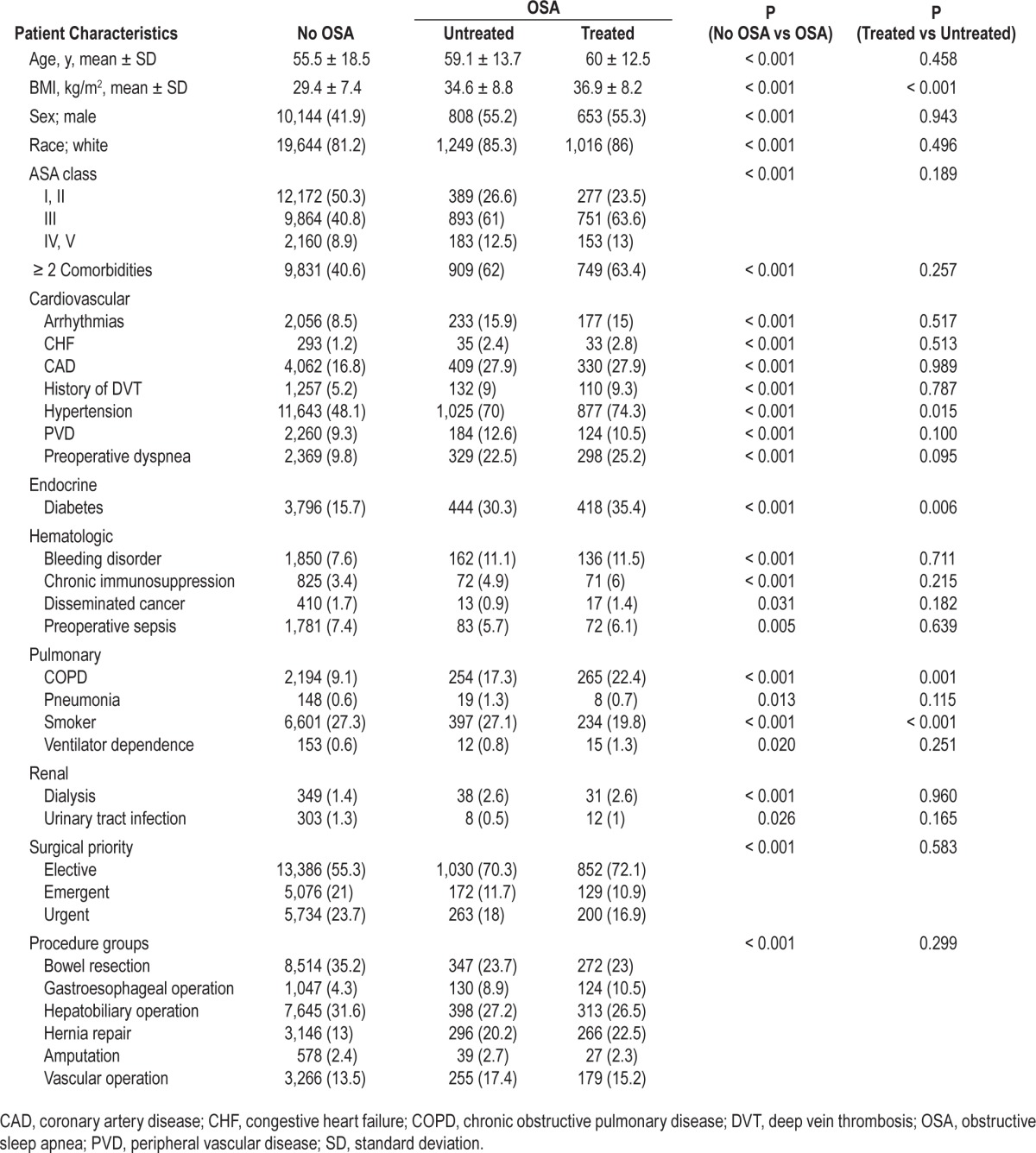
RESULTS
Of 26,842 patients undergoing general or vascular surgery at one of 52 MSQC hospitals, 2,646 (9.9%) had a diagnosis or suspicion of OSA, and 1,465 of those (55.4%) were untreated. The clinical and demographic characteristics are shown in Table 1. When compared to patients in the no OSA category, patients in the OSA (treated and untreated) categories were older, more likely to be male, had higher BMIs and ASA scores, and had higher comorbidity burdens. Upon comparing the treated and the untreated OSA groups, the patient characteristics were statistically similar and well balanced within these two groups. Of note, patients in the untreated subgroup had slightly lower mean BMIs and were less likely to have chronic obstructive pulmonary disease, hypertension, or diabetes, but they were more likely to be smokers.
Table 1.
Clinical and demographic characteristics.
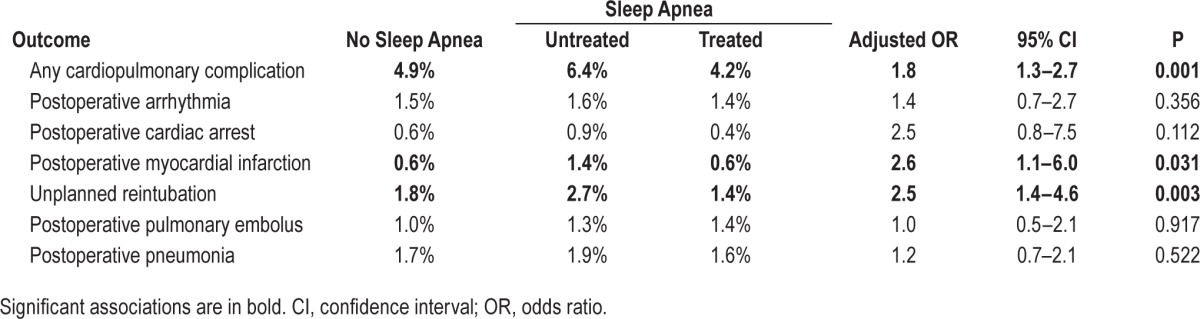
As our hypothesis is that patients, who are at high risk of having OSA or are preoperatively untreated, have higher rates of cardiopulmonary complications than patients with known OSA who are treated preoperatively, the next analyses are limited to the two OSA groups (untreated versus treated). On multivariable analyses, untreated OSA was independently associated with the occurrence of any cardiopulmonary complication (adjusted odds ratio [aOR] = 1.8, P = 0.001), as shown in Table 2, along with older age, higher ASA classes, vascular surgery, and comorbidity index. When examining the individual cardiopulmonary complications, untreated OSA was also found to be significantly associated with unplanned reintubations (aOR = 2.5, P = 0.003) and postoperative myocardial infarction (aOR = 2.6, P = 0.031) compared to treated OSA. There was an increasing trend for the occurrence of the other complications in untreated patients, but this did not reach statistical significance. All models had a c-statistic > 0.7, which is similar to previously published postoperative outcome models.17
Table 2.
Unadjusted incidence rates, and adjusted odds ratios of cardiopulmonary complications in untreated and treated obstructive sleep apnea patients.
The risk-adjusted rates of the associated cardiopulmonary complications for patients with untreated OSA and those with treated OSA are displayed in Figure 1. The risk-adjusted rate of any cardiopulmonary complication was 1.7 times higher in the untreated vs. the treated patient groups. Similarly, there was a more than twofold increased risk for unplanned reintubation and postoperative myocardial infarctions.
Figure 1.
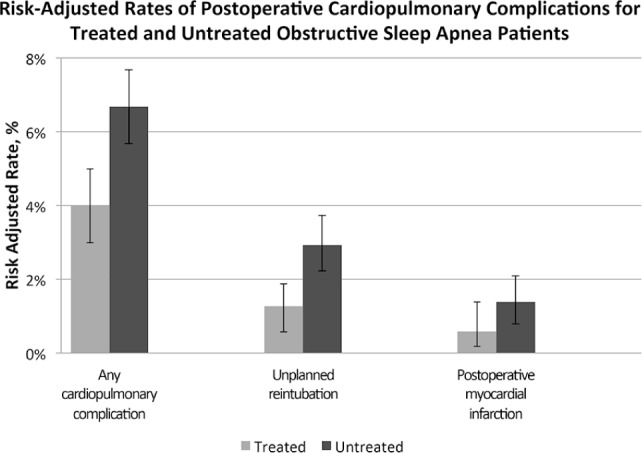
Risk-adjusted rates of any cardiopulmonary complication, unplanned reintubation, and postoperative myocardial infarction among patients with treated versus untreated obstructive sleep apnea. The error bars represent the 95% confidence intervals. Covariates in the models include age, sex, body mass index, American Society of Anesthesiologists class, procedure type, emergency status, comorbidity index, and smoking status.
DISCUSSION
In this multi-institutional cohort study of 27,000 patients undergoing general and vascular surgery, approximately 10% had a diagnosis and/or suspicion of OSA and over half of those were untreated. Untreated OSA was associated with approximately twofold to threefold increased risk of any cardiopulmonary complication; specifically, unplanned reintubation and postoperative myocardial infarction. This underscores the importance of improving the recognition of OSA. The findings further suggest a need for clinical trials to demonstrate that routine screening and treatment of OSA can reduce postoperative complications and ensuring adequate preoperative treatment would reduce the occurrence of adverse events.
The overall prevalence of OSA in 10% of the study's population is similar to other population-based reports highlighting the growing epidemic of OSA.3,6 It is noteworthy to mention that over the past 10 y, the prevalence of OSA (∼2% in 2004)3 has more than quadrupled in adult surgical populations. Unique to this study, we identified that over 55% of patients who were known or deemed at high risk to have OSA were not receiving PAP therapy prior to their surgery.
Although previous research has demonstrated that OSA is associated with adverse postoperative outcomes,3,4,6 the reliance on administrative data and diagnosis codes is a major limitation that left a lot to be desired in the general understanding of OSA's effect on postoperative outcomes. In the current study, we demonstrate that untreated OSA is associated with about a twofold increased risk of any cardiopulmonary complication, unplanned reintubation, and postoperative myocardial infarction, compared to OSA treated with preoperative PAP therapy from a population-based clinical registry.
The marked differences in the postoperative risks in these two patient cohorts may suggest that the adverse outcomes of OSA are potentially avoidable. The observed benefit of PAP therapy in this study may be due to several factors. Preoperative PAP therapy may offer a “carryover” protective effect due to a decrease in upper airway inflammation or edema, and increased upper airway stability. Alternatively, it may be due to increased utilization of postoperative PAP therapy in these patients. Although we did not have data on postoperative PAP use, we presume that patients who use PAP devices at home may be more likely to be compliant with its use in the early postoperative period, or be more vigilant in raising their concerns to the surgical team. These patients are also more likely to receive postoperative therapy, as the ASA guidelines recommend instructing these patients to bring their own device to the hospital.8 In a randomized trial, Squadrone and colleagues18 showed significant reduction in respiratory failure with early PAP treatment for patients with postoperative hypoxia. Although the trial was not specifically designed for patients with OSA, it raises the possibility that the apparent benefit observed in the current study may not reflect preoperative OSA therapy per se, but rather a nonspecific effect of perioperative PAP that might benefit all patients. Finally, patients with OSA may be receiving higher levels of respiratory-directed care and monitoring, such as overnight pulse oximetry or telemetry, which may allow their healthcare providers to promptly recognize warning signs thereby preventing adverse events.
The widespread adoption of simple perioperative screening tools, such as the STOP-BANG questionnaire for assessing the risk for OSA, means that many patients are labeled with a suggested diagnosis/suspicion of OSA for the first time when they present for surgery. This increased awareness is beneficial for the general health of the patient, but poses a challenge in the perioperative setting to the surgical provider. The findings presented in this observational study suggest that there may be a benefit to preoperative PAP therapy in patients with OSA; however, randomized controlled trials are needed to establish causality, and guide practice on how to best optimize these patients and how to manage them if a new diagnosis is made at the time of surgery. Indeed, optimizing a patient's risk profile before surgery has become an accepted approach for other co-morbid conditions such as ischemic heart disease and diabetes, and this may be the case for OSA in the near future.
The current study has several limitations. First, we are limited by the inherent limitations noted in observational studies. Even though the patients in the two OSA categories were similar in regard to the measured characteristics, several unmeasured characteristics may confound or moderate the results. For example, research suggests that patients who are adherent to their prescription medications are also more adherent to PAP therapy for OSA,19 and thus may have better control on their comorbidities. We were also unable to account for the severity of OSA in patients who carried the diagnosis, nor were we able to quantify the adherence to the use of postoperative PAP therapy in either patient category. In addition, we could not assess the interaction of different anesthesia techniques and/or medications (such as muscle relaxants) with OSA on the studied outcomes; however, given the similarity in the measurable covariates between the two OSA groups, these differences are assumed to occur at random and should not influence the conclusions of this study. Finally, patient self-report of PAP therapy may be overestimated; however, this would theoretically bias the results toward the null. Thus, the results presented herein may be conservative estimates of the true effect of untreated OSA on postoperative outcomes. Notwithstanding these limitations, the results presented herein, which have not been previously demonstrated in the literature, are relevant, have several implications, and align with the primary focus of this study in examining the association between untreated OSA and postoperative outcomes compared to a similar group of patients who are treated for this condition.
In conclusion, this study shows that patients with a diagnosis or suspicion of OSA and are not treated with PAP therapy preoperatively are at a significantly increased risk for cardio-pulmonary complications following general and vascular surgery. This suggests that improving the recognition of OSA, ensuring adequate therapy, and close observation of these patients may be a strategy to reduce the incidence of adverse postoperative outcomes. The findings further suggest a need for clinical trials to examine the effect of routine preoperative screening and preoperative treatment of OSA on postoperative complications and adverse events.
DISCLOSURE STATEMENT
Dr. Abdelsattar is supported by AHRQ T32 HS000053-22. Dr. Ramachandran has received consulting honoraria from Galleon Pharmaceuticals, Horsham, PA and Merck Sharp and Dohme, Whitehouse Station, NJ. He has active research funding from Merck Sharp and Dohme, Whitehouse Station, NJ. Role of the sponsor: the funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Author contributions: Dr. Ramachandran had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Abdelsattar, Ramachandran. Data acquisition: Hendren, Wong, Campbell. Analysis and interpretation: Abdelsattar, Wong, Hendren, Ramachandran. Drafting the manuscript: Abdelsattar, Ramachandran. Critical revision and final approval: all authors.
Footnotes
A commentary on this article appears in this issue on page 1155.
REFERENCES
- 1.Memtsoudis SG, Besculides MC, Mazumdar M. A rude awakening–the perioperative sleep apnea epidemic. N Engl J Med. 2013;368:2352–3. doi: 10.1056/NEJMp1302941. [DOI] [PubMed] [Google Scholar]
- 2.Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc. 2001;76:897–905. doi: 10.4065/76.9.897. [DOI] [PubMed] [Google Scholar]
- 3.Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO. Sleep-disordered breathing and postoperative outcomes after elective surgery: analysis of the nationwide inpatient sample. Chest. 2013;144:903–14. doi: 10.1378/chest.12-2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mokhlesi B, Hovda MD, Vekhter B, Arora VM, Chung F, Meltzer DO. Sleep-disordered breathing and postoperative outcomes after bariatric surgery: analysis of the nationwide inpatient sample. Obes Surg. 2013;23:1842–51. doi: 10.1007/s11695-013-0991-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaw R, Pasupuleti V, Walker E, Ramaswamy A, Foldvary-Schafer N. Postoperative complications in patients with obstructive sleep apnea. Chest. 2012;141:436–41. doi: 10.1378/chest.11-0283. [DOI] [PubMed] [Google Scholar]
- 6.Memtsoudis S, Liu SS, Ma Y, et al. Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg. 2011;112:113–21. doi: 10.1213/ANE.0b013e3182009abf. [DOI] [PubMed] [Google Scholar]
- 7.Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnea. Chest. 2010;138:1489–98. doi: 10.1378/chest.10-1108. [DOI] [PubMed] [Google Scholar]
- 8.Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology. 2014;120:268–86. doi: 10.1097/ALN.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 9.Campbell DA, Englesbe MJ, Kubus JJ, et al. Accelerating the pace of surgical quality improvement: the power of hospital collaboration. Arch Surg. 2010;145:985–91. doi: 10.1001/archsurg.2010.220. [DOI] [PubMed] [Google Scholar]
- 10.Hendren S, Fritze D, Banerjee M, et al. Antibiotic choice is independently associated with risk of surgical site infection after colectomy: a population-based cohort study. Ann Surg. 2013;257:469–75. doi: 10.1097/SLA.0b013e31826c4009. [DOI] [PubMed] [Google Scholar]
- 11.Campbell DA, Jr, Kubus JJ, Henke PK, Hutton M, Englesbe MJ. The Michigan Surgical Quality Collaborative: a legacy of Shukri Khuri. Am J Surg. 2009;198:S49–55. doi: 10.1016/j.amjsurg.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Rowell KS, Turrentine FE, Hutter MM, Khuri SF, Henderson WG. Use of national surgical quality improvement program data as a catalyst for quality improvement. J Am Coll Surg. 2007;204:1293–300. doi: 10.1016/j.jamcollsurg.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812–21. doi: 10.1097/ALN.0b013e31816d83e4. [DOI] [PubMed] [Google Scholar]
- 14.Chung F, Subramanyam R, Liao P, Sasaki E, Shapiro C, Sun Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth. 2012;108:768–75. doi: 10.1093/bja/aes022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144:581–95. doi: 10.7326/0003-4819-144-8-200604180-00009. [DOI] [PubMed] [Google Scholar]
- 16.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12:308–31. [Google Scholar]
- 17.Merkow RP, Hall BL, Cohen ME, et al. Relevance of the c-statistic when evaluating risk-adjustment models in surgery. J Am Coll Surg. 2012;214:822–30. doi: 10.1016/j.jamcollsurg.2011.12.041. [DOI] [PubMed] [Google Scholar]
- 18.Squadrone V, Coha M, Cerutti E, et al. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA. 2005;293:589–95. doi: 10.1001/jama.293.5.589. [DOI] [PubMed] [Google Scholar]
- 19.Platt AB, Kuna ST, Field SH, et al. Adherence to sleep apnea therapy and use of lipid-lowering drugs: a study of the healthy-user effect. Chest. 2010;137:102–8. doi: 10.1378/chest.09-0842. [DOI] [PMC free article] [PubMed] [Google Scholar]


