Abstract
Study Objectives:
We tested whether providing adults with obstructive sleep apnea (OSA) with daily Web-based access to their positive airway pressure (PAP) usage over 3 mo with or without a financial incentive in the first week improves adherence and functional outcomes.
Setting:
Academic- and community-based sleep centers.
Participants:
One hundred thirty-eight adults with newly diagnosed OSA starting PAP treatment.
Interventions:
Participants were randomized to: usual care, usual care with access to PAP usage, or usual care with access to PAP usage and a financial incentive. PAP data were transmitted daily by wireless modem from the participants' PAP unit to a website where hours of usage were displayed. Participants in the financial incentive group could earn up to $30/day in the first week for objective PAP use ≥ 4 h/day.
Measurements and Results:
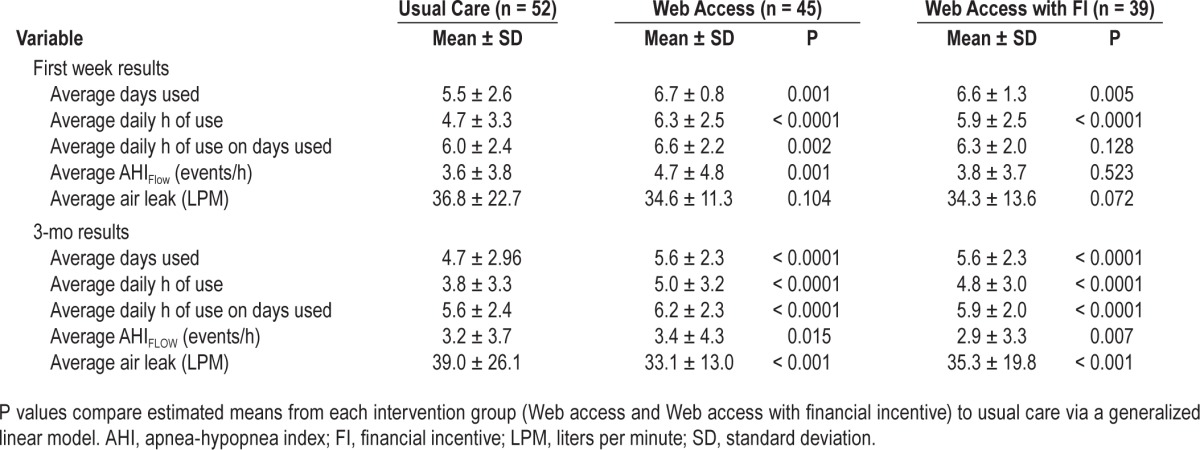
Mean hours of daily PAP use in the two groups with access to PAP usage data did not differ from each other but was significantly greater than that in the usual care group in the first week and over 3 mo (P < 0.0001). Average daily use (mean ± standard deviation) during the first week of PAP intervention was 4.7 ± 3.3 h in the usual care group, and 5.9 ± 2.5 h and 6.3 ± 2.5 h in the Web access groups with and without financial incentive respectively. Adherence over the 3-mo intervention decreased at a relatively constant rate in all three groups. Functional Outcomes of Sleep Questionnaire change scores at 3 mo improved within each group (P < 0.0001) but change scores of the two groups with Web access to PAP data were not different than those in the control group (P > 0.124).
Conclusions:
Positive airway pressure adherence is significantly improved by giving patients Web access to information about their use of the treatment. Inclusion of a financial incentive in the first week had no additive effect in improving adherence.
Citation:
Kuna ST, Shuttleworth D, Chi L, Schutte-Rodin S, Friedman E, Guo H, Dhand S, Yang L, Zhu J, Bellamy SL, Volpp KG, Asch DA. Web-based access to positive airway pressure usage with or without an initial financial incentive improves treatment use in patients with obstructive sleep apnea. SLEEP 2015;38(8):1229–1236.
Keywords: adherence, telehealth, internet
INTRODUCTION
Obstructive sleep apnea (OSA) is characterized by repetitive closure of the pharyngeal airway during sleep. OSA is prevalent and is associated with a significant increase in morbidity and mortality.1,2 Patients with OSA exhibit excessive daytime hypersomnolence that results in decreased job performance and increased incidence of traffic and industrial accidents.3 Patients with OSA are at increased risk of hypertension, ischemic heart disease, and cerebrovascular disease.4–7 The prevalence and consequences of OSA underscore the importance of its adequate treatment.
Positive airway pressure (PAP) is currently the medical treatment of choice for OSA.8 Most PAP units record mask-on time to objectively measure the patient's adherence. This precise measurement of PAP use reveals that only about one-half of subjects use PAP for 4 h or more per day, a level frequently cited in the literature as a threshold for adequate use.9,10 Several studies have demonstrated that objectively measured PAP adherence within the first week is highly correlated with longer-term adherence.11–14 Clinical factors are not highly predictive of PAP adherence and the reasons why patients decide whether or not to use PAP remain poorly understood.15,16 Patient education and support delivered at the beginning of PAP treatment can improve PAP adherence.17–19
Recent studies report that daily wireless transmission of PAP data from the patient's unit to a website that can be accessed by patients and/or practitioners improves PAP adherence.20–22 We therefore tested whether providing patients with OSA daily access to information about their PAP treatment over a 3-mo period improved PAP adherence and functional outcomes. Furthermore, numerous randomized controlled trials, many by coauthors of this report, found that use of a financial incentive is associated with significant improvements in health behavior related to a wide range of clinical outcomes including weight loss, smoking cessation, adherence to medications, and adherence to home monitoring.23–27 To determine the effect of a financial incentive on PAP adherence, we tested whether adding a financial incentive to adhere to treatment in the first week improved PAP adherence and functional outcomes at 3 mo. We anticipated that providing patients with access to PAP results would enhance use of the treatment and daytime function and that adding the financial incentive to use the treatment would further improve these outcomes.
METHODS
The protocol was a pilot study to evaluate a newly developed automated information technology Web portal (Way to Health) based at the University of Pennsylvania that integrates biometric devices, clinical trial randomization and enrollment processes, financial system fulfillment, and secure data capture for research purposes.28 Participants were recruited at sleep centers at the Hospital of the University of Pennsylvania, Lankenau Medical Center, Holy Redeemer Hospital, and Paoli Hospital. The protocol at all participating sites was approved by the Institutional Review Board at the University of Pennsylvania. Patients of at least 18 y of age who were being prescribed PAP treatment for newly diagnosed OSA with an apnea-hypopnea index (AHI) ≥ 10 events/h on in-laboratory polysomnogram were informed of the study by their sleep specialist and flyers posted in the sleep centers. The polysomnograms were scored and interpreted by the sleep center staff at each clinical site using American Academy of Sleep Medicine recommended criteria.29,30
Patients interested in the study contacted the study coordinator via phone or Email and were given more detailed information about the study. After reviewing the study with the patient, the coordinator sent an Email message to individuals expressing interest in participating that provided a link to the website. On initial login, patients created a username and password, entered contact information, and completed the website's eligibility checklist questionnaire. Participants were required to have access to a telephone and the Internet on all days of the week. In the previous 2 mo, they were required to have a stable medical history (no hospitalizations or new medical diagnoses other than OSA), no change in medications, and no regular use (more than three times per week) of sedative or hypnotic medications. Individuals were excluded if they had a diagnosis of another sleep disorder in addition to OSA, had previous medical or surgical treatment for OSA, required supplemental oxygen or bilevel PAP treatment, worked rotating or night shift in the past 3 mo, or had claustrophobia or facial pathology that prevented PAP treatment. We excluded individuals with a recent change in medication(s) to ensure that they had a stable medical history. We excluded individuals who had previous surgery for OSA because most of these patients have had previous exposure to PAP treatment and we wanted the enroll subjects who were naïve to PAP.
Individuals who fulfilled all of the self-administered eligibility criteria were provided the consent form on the website. The consent form informed participants that they would be assigned to one of three groups and that it was possible that they might be able to view their PAP results and/or earn additional money depending on the group to which they were assigned. They were informed about the exact nature of their particular group once they were randomized. Those individuals who submitted their electronic consent were considered to be enrolled.
All participants completed the following questionnaires on the website prior to initiation of PAP treatment and 1 and 3 mo following initiation of PAP treatment: Functional Outcomes of Sleep Questionnaire – short form (a disease-specific quality of life questionnaire, FOSQ-10),31 Epworth Sleepiness Scale (a measure of subjective daytime sleepiness, ESS),32,33 and Health Survey Short-Form 12 (a general quality of life questionnaire, SF-12).34,35 At each time point, all participants received $30 for completing the questionnaires.
Following completion of the baseline questionnaires, participants were randomized by the website's software program to one of three groups: usual care, usual care with access to their PAP data updated daily on the Way to Health website, or usual care with daily Web-based access to PAP data with a financial incentive in the first week of treatment. The Way to Health website used a basic randomization method by which each eligible participant had a one in three chance of being assigned to one of the three different arms. Participants were unblinded to assignment; investigators other than the study coordinator were blinded to assignment until collection of primary outcome data. All of the interactions between the study coordinator and participant were by phone. The study coordinator helped participants if they had any technical difficulties logging into the website but provided no assistance with their actual treatment. Participants in the usual care group did not have access to their PAP data on the website. Participants in the two groups with access to their PAP data could log onto the website at any time throughout the 3-mo period to view a numerical and bar graph display of their daily hours of PAP use (i.e., mask-on time) from the beginning of treatment and over the previous 2 w of treatment. When participants logged into the website to view their PAP adherence, they were asked to indicate (yes/no) if they had used the treatment for at least 4 h in the past 24 h. This response was used to verify that they had logged into the website on a particular day. Participants assigned to the financial incentive group were informed that they could earn $30 for each day in the first week that they logged into the website and had used PAP treatment for at least 4 h in the previous day. Their total possible compensation for adequate PAP use in the first week was $210. The financial incentive payment was made at the end of the first week of treatment.
All participants received either a continuous or automatically adjusting PAP unit (System One, Philips Respironics, Inc, Murrysville, PA) equipped with a wireless modem. Local home healthcare companies used by the participating sleep centers and blinded to randomization delivered the equipment to the participants and explained how to use and maintain the equipment. On a daily basis, the modem transmitted data from the PAP unit to the manufacturer's server, which in turn exported the results to the Way to Health website. The data obtained from the PAP device for analysis included the following measures: hours of mask-on time, apnea-hypopnea index (AHIFLOW), and amount of unintentional air leak. Participants who had Web access to their PAP data were only provided their hours of mask-on time results.
Over the 3-mo intervention, all participants received usual follow-up care at their respective sleep centers. Usual care at the sites uniformly consisted of one clinic visit with the sleep specialist within 1 to 3 mo following initiation of treatment. No instructions were given to the sleep specialist regarding follow-up care. At the time of the clinic follow-up, the sleep specialist had access to the manufacturer's PAP website for clinical management. The sleep specialist could share the PAP information with the participant. The home health care company supplying the PAP equipment conducted routine follow-up care during the 3-mo intervention. This practice was not standardized or monitored but generally consisted of a phone call to the patient at 1 w, 1 mo, and 3 mo. If the patient had a mask or equipment problem, the home healthcare company provided routine clinical care.
Statistical Analysis
Primary analyses were generally focused on examining potential group differences in: (1) mean hours of daily PAP use (all days); (2) mean hours of daily PAP use on days used; and (3) changes in FOSQ-10 scores (baseline to 3 mo). Analyses were completed considering data from the first week only as well as over the entire 3-mo study period (e.g., including week 1) in order to explore any potential temporal effects. Secondary outcomes included subjective functional outcomes measures (e.g., ESS, and SF-12) as well as mean AHIFLOW, and mean air leak from the circuit.
Demographic characteristics and outcomes of interest were summarized for the sample as a whole, as well as by randomized group. Analysis of variance conducted using generalized linear models and adjusted for arm was used to test for mean differences in PAP adherence between each of the intervention arms versus control. The regression models were used to compare estimated mean outcomes: (1) during the first week of the intervention period only; and (2) during the entire 3 mo, including the first week. Specifically, mean outcomes for participants randomized to the Web access only and Web access with financial incentives were compared to mean outcomes for participants randomized to usual care. Results comparing mean changes in each functional outcome (FOSQ-10, ESS, SF-12 (physical) and SF-12 (mental)) from baseline to 3 mo were compared via paired t tests. All analyses were completed using SAS Version 9 (SAS Institute Inc. Cary, NC).
RESULTS
Of the 194 patients who contacted the study coordinator expressing interest in the study, a total of 138 individuals (83 males) successfully enrolled on the website and were randomized (Figure 1). The primary reason that individuals were not enrolled was because they had already started PAP treatment (n = 15). Other individuals were unable or unwilling to participate because they had an irregular work schedule (n = 11), regular use of a sedative-hypnotic (n = 11), or were unwilling to complete the W-9 form on the website (n = 7). One participant in each arm was withdrawn from the study. One subject could not tolerate PAP treatment and was kept in analysis based on intention to treat. The modem was mistakenly not connected to the PAP unit in the other two who were removed from the analysis. The remaining participants had a mean age of 50.9 ± 12.1 y, mean body mass index of 36.7 ± 8.7 kg/m2, and a mean AHI on their diagnostic sleep study of 37.8 ± 26.7 events/h with a range of 9 to 134 events/h (Table 1). There were 17.1% of participants who had mild sleep apnea (5 ≤ AHI < 15), 32.1% had moderate sleep apnea (15 ≤ AHI < 30), and 50.8% had severe sleep apnea (AHI ≥ 30). There were 52.6% who were college graduates, 74.8% had a household income of at least $50,000, and 76.6% were employed. There were no differences in participant characteristics across the three groups.
Figure 1.
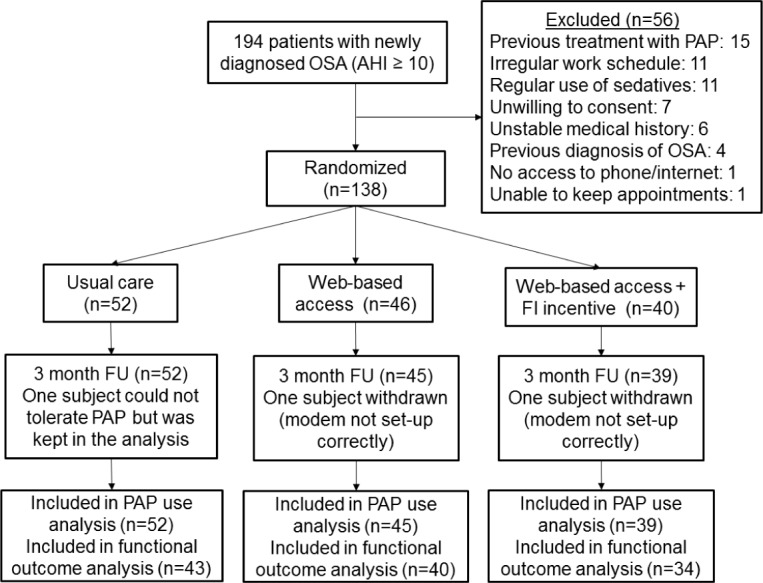
Consort diagram of subject participation. AHI, apnea-hypopnea index; FI, financial incentive; FU, follow-up; OSA, obstructive sleep apnea; PAP, positive airway pressure.
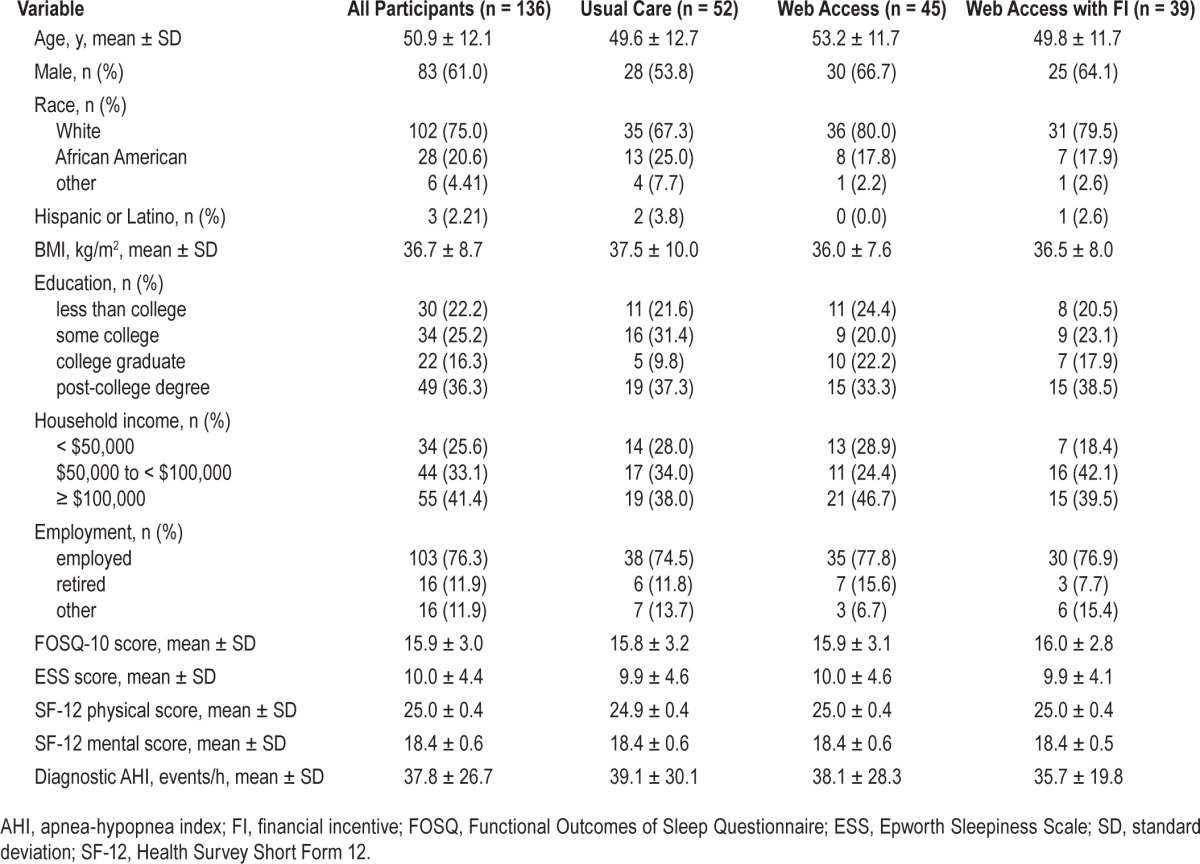
Table 1.
Baseline characteristics of participants.
During the first week of PAP treatment, participants in both groups with Web access to their PAP data were significantly more adherent than those in the usual care group (Figure 2). Average daily use in the first week was 4.7 ± 3.3 h in the usual care group compared to 5.9 ± 2.5 h and 6.3 ± 2.5 h in the Web access groups with and without the financial incentive, respectively (P < 0.0001). No differences in PAP use were observed between the two groups with access to their PAP data with or without the financial incentive (P = 0.063).
Figure 2.
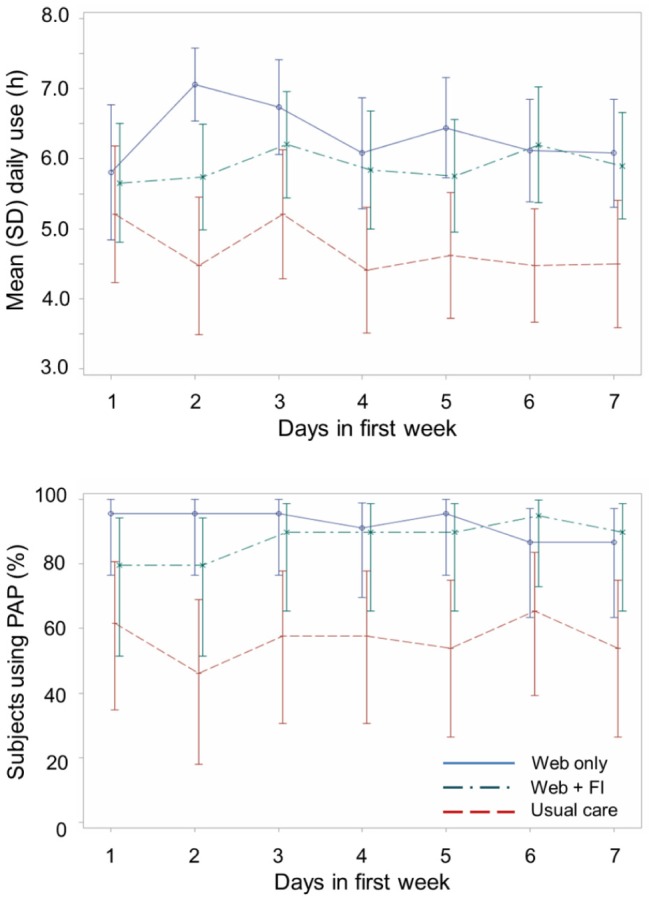
Mean (standard deviation, SD) daily hours of positive airway pressure use (upper graph) and daily percentage of subjects in each group who used the treatment (lower graph) in the first week of treatment. Dashed line, usual care; solid line, usual care with Web access to positive airway pressure (PAP) data; dash-dot line, usual care with Web access to PAP data and a first-week financial incentive (FI).
Adherence over the 3-mo intervention decreased at a relatively constant rate in all three groups. Throughout this period, however, the weekly difference in adherence across groups remained relatively similar to that observed in the first week (Figure 3). Compared to the average daily use during the 3-mo PAP intervention of 3.8 ± 3.3 h in the usual care group, adherence was 4.8 ± 3.0 h and 5.0 ± 3.2 h in the PAP access groups with and without financial incentive, respectively (P < 0.0001).
Figure 3.
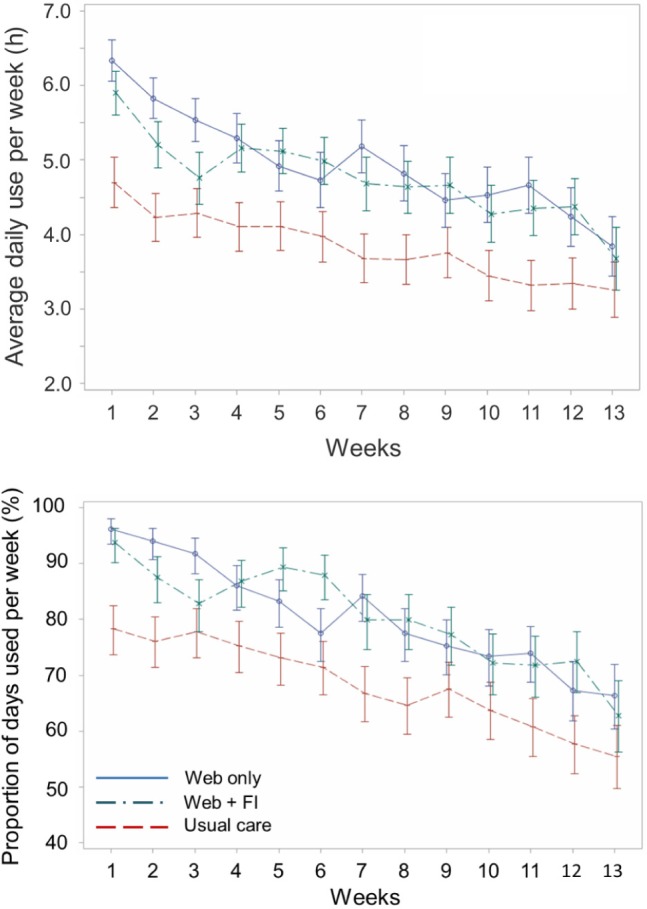
Mean (standard deviation) daily hours of positive airway pressure use per week (upper graph) and percentage of days the treatment was used per week (lower graph) over the 3 mo of treatment in the three groups. Dashed line, usual care; solid line, usual care with Web access to PAP data; dash-dot line, usual care with Web access to PAP data and a first-week financial incentive (FI).
Although there were some statistically significant differences in PAP treatment across groups, it is unlikely that they influenced the results. Significant differences were observed across groups in PAP device measurements of air leak and AHIFLOW at 1 w and 3 mo, but the magnitude of these differences was small and unlikely to have been of clinical significance (Table 2). About 80% of subjects in the two groups without financial incentive were treated with automatic positive airway pressure instead of continuous positive airway pressure, whereas automatic positive airway pressure was used in 62% of subjects in financial incentive group (P = 0.04). No differences were observed across groups in the percentage of subjects using a full face versus nasal mask interface (P = 0.47).
Table 2.
Positive airway pressure device data in first week and 3-mo treatment period.
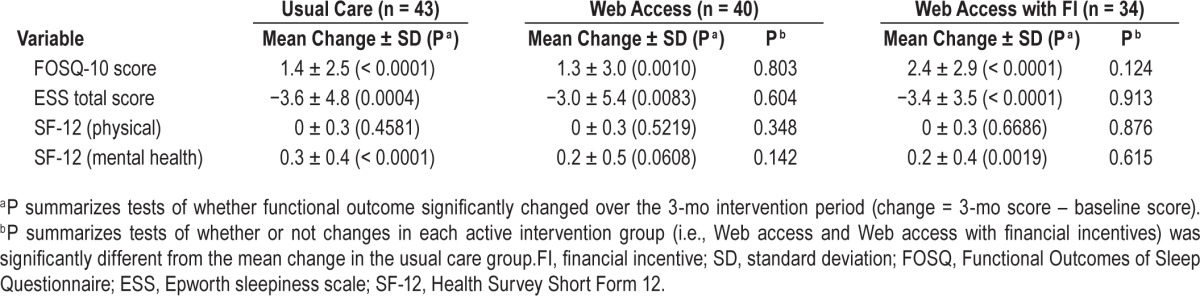
Most functional outcomes scores improved significantly from baseline to 3 mo. Specifically, FOSQ-10 scores improved by an average 1.4 ± 2.5 (P < 0.0001), 1.3 ± 3.0 (P = 0.0010) and 2.4 ± 2.9 (P < 0.0001) points for the usual care, Web access and Web access with financial incentives groups, respectively. Similarly, ESS scores decreased on average 3.6 ± 4.8 (P = 0.0004), 3.0 ± 5.4 (P = 0.0083), and 3.4 ± 3.5 (P < 0.0001), respectively. The mental health component of the SF-12 score significantly improved in the usual care (0.3 ± 0.4; P < 0.0001) and Web-based access with financial incentive groups (0.2 ± 0.4; P = 0.0019). There were no significant changes in the physical component of the SF-12. Despite the greater PAP use in the two groups with Web access to their PAP data, the change scores of their functional outcomes were similar to those in the control group (P > 0.124) (Table 3).
Table 3.
Mean changes in functional outcome measures within and across the three groups following 3 mo of positive airway pressure treatment.
Seventy-nine percent of participants in the financial incentive group received a payment based on their PAP use in the first week. The average payment per participant was $119 ± 27. Twenty-seven of the 39 participants (69%) in that group earned $150 or more based on their PAP usage in the first week; 2 (4%) earned $120, 4 (10%) earned $30, and 8 (21%) did not earn any incentive.
Figure 4 shows the daily percentage of participants in the two groups with Web access to their PAP data who completed the PAP usage questionnaire when they logged into the web-site to view their PAP data. In the first week, the PAP usage questionnaire was completed by 72.9 ± 6.6% of participants in the financial incentive arm and 53.0 ± 9.9% of participants without the financial incentive (P < 0.0001). Following cessation of the financial incentive after the first week, there was no difference between the two groups in the percentage of subjects who completed the questionnaire (P = 0.954). Based on completion of the PAP survey on the website, participants who viewed their PAP data at least four times during the first week of treatment, compared to participants with fewer logins, had greater average daily PAP usage in the first week (6.7 versus 5.5 h, P < 0.0001) and greater percentage of days of PAP use (99% versus 90%, P < 0.0001) during that week. During the 12 w of PAP treatment, participants who viewed their PAP data at least 12 times, compared to those with fewer logins, had greater average daily PAP usage (5.2 versus 4.6 h, P < 0.0001) and greater percentage of days of PAP use (83% versus 78%, P < 0.0001) over that period.
Figure 4.
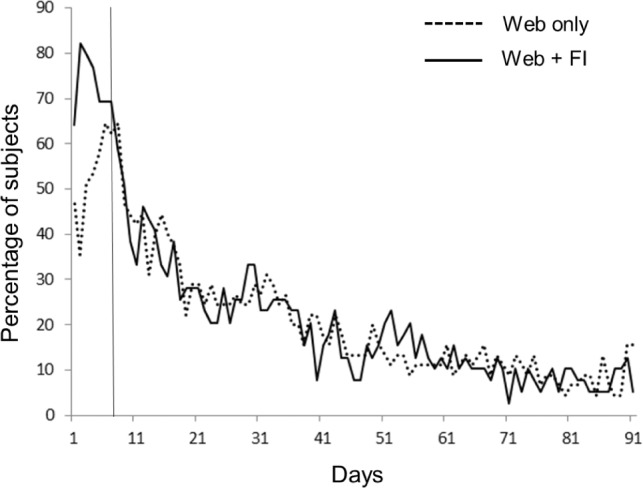
Percentage of participants with Web access to their positive airway pressure (PAP) data who logged into the website and completed the PAP usage form during the 3-mo treatment period. Black line: participants who could receive a financial incentive in the first week; red line: participants who did not receive a financial incentive (FI). Vertical dashed line indicates end of first week of treatment.
DISCUSSION
The results indicate that individuals with OSA improve their adherence to PAP treatment when given access to a website where they can view their daily PAP use. Patients with Web access to their PAP data used the treatment about 1 h per day more than those without access. The greater daily hours of PAP usage in the two groups with daily Web access to their PAP results was evident in the first week of treatment and persisted over the first 3 mo of treatment. We had anticipated that the financial incentive in the first week would further improve PAP use by prompting participants to try harder to overcome initial barriers that might otherwise discourage them from using the treatment. Contrary to our hypothesis, our analysis showed that, although the financial incentive encouraged more frequent logins to the website during the first week than Web access alone (Figure 3), the increased number of logins did not result in greater PAP use compared to the Web access-only arm.
Adherence over the 3-mo intervention decreased at a relatively constant rate in all three groups and had not reached a plateau at the 3-mo endpoint (Figure 3). Throughout this period, however, the difference in adherence across groups remained relatively similar to that observed in the first week. In agreement with previous studies, these results indicate that interventions at initiation of PAP treatment can enhance adherence and that patterns of adherence established at the beginning of the intervention have long lasting effects.11,13,17,21,36 The steady decline in adherence during the intervention period, even in the two groups with Web-based access to their PAP results, emphasizes that patients with OSA need long-term management and that additional strategies are needed to help patients sustain their initial adherence behavior.
Given the magnitude of the enhanced adherence in patients with Web access to their PAP use, one would have expected that their improvement in functional outcomes would have been greater than that in the usual care group. Although significant improvements in functional outcomes over the 3-mo period occurred within each group, the improvements in the two groups with Web access to PAP data were similar to those of the usual care group. Our pilot study was not powered to detect an improvement in functional outcomes and the relatively small sample size may explain these findings. Another possible explanation for the similar improvements in functional outcomes across groups is that the PAP use in the usual care group may have been sufficient to attain the maximum improvement in functional outcomes that would occur with PAP treatment. However, although previous studies did find that PAP use greater than 4–5 h/day does not result in further improvement in the ESS score, the FOSQ score continued to improve as daily hours of PAP use increased.37,38
Contrary to our expectation, the group with Web access to PAP data and the first-week financial incentive did not have greater PAP adherence than the group with Web access to PAP data without the financial incentive. However, a greater percentage of participants with the financial incentive completed the PAP usage questionnaire in the first week compared to participants without the financial incentive. This suggests that the participants in the financial incentive group were aware of the requirements to qualify for reward. It is possible that the relatively high adherence to PAP by participants with Web access but without financial incentive may have resulted in a ‘ceiling effect’ that prevented the financial incentive from having any additional benefit. In the first week, participants in the Web access without financial incentive group averaged 6.3 ± 2.5 h/day of use and used the treatment an average of 6.7 ± 0.8 days. This excellent usage may in part be explained by the relatively high socioeconomic status of our participants (Table 1). The level of socioeconomic status is directly related to PAP adherence.39 An effect of the financial incentive might have been observed if it had been administered without the Web-based feedback.
The primary purpose of the Way to Health study was to develop and test a website that interfaced with home medical devices. Therefore, we designed our pilot study to maximize the number of individuals who would be using the website to view their PAP data. Given the scope of the study, we were unable to include a fourth group that received the financial incentive only. It is also possible that application of the financial incentive in a different patient population may have different results. Based on previous studies, we believe that the amount of financial incentive should have been sufficient to alter health behavior. However, it is possible that extending the financial incentive to a longer period of time or using a different payment strategy, such as a lottery, might have yielded different results. We chose to limit the financial incentive to the first week of treatment because previous studies indicate that this is when most patients decide whether or not to use the treatment.11–14
Our results complement the study of Stepnowsky et al.21 Their study randomized patients with OSA prescribed PAP treatment to either usual care (n = 114) or access to an interactive web-site (n = 126) where the participant could view his/her PAP use, treatment efficacy (PAP- generated AHI), and amount of air leak from the PAP circuit. Participants in the Web access group had greater PAP use at the 2-mo time point relative to participants receiving usual care only (4.1 ± 2.3 versus 3.4 ± 2.4 h/day, respectively; P = 0.02). Similar to the current study, the enhanced PAP adherence in the group with Web access was present in the first week of PAP treatment. Also similar to our results, adherence in both groups decreased over the 4-mo intervention but the difference between groups was sustained. Despite the difference in adherence between the two groups, no differences were found on self-reported measures of OSA symptoms. Participants with Web access to their PAP data responded that they were more likely to use the Internet to obtain information on sleep apnea at the end of the protocol compared to baseline, but the number of times they actually viewed their PAP data was not monitored. There was no incentive to use the site.
The gradual decline in PAP use observed over the 3 mo of treatment raises an important issue regarding the reporting of PAP adherence. Randomized controlled trials evaluating the effect of PAP treatment on a variety of functional and metabolic outcomes, as well as cardiovascular risk factors, typically report the average daily hours of PAP adherence over the entire intervention period. But this measurement may overestimate the PAP adherence at the end of the intervention when outcome measures are collected. For example, our usual care group had an average PAP use over the 3-mo intervention of 3.8 ± 3.3 h/day, but the average usage in the last week of treatment was 3.3 ± 3.3 h/day. Changes in PAP adherence during the intervention should be taken into account in the analyses and interpretation of the outcomes. Results of outcome measures obtained at the end of the PAP intervention are likely to be more closely related to PAP adherence at the time the outcome measures are collected. Furthermore, when endpoint PAP data are missing, carrying forward results collected during the course of the intervention may overestimate the results. Our findings suggest that research studies should report mean PAP adherence not only during the entire intervention, but also at the time the outcome measures are collected.
The website did not automatically track the number of times each participant logged into the website. However, we monitored use of the Web-based platform by participants with access to their PAP results by asking them to complete the PAP usage questionnaire every time they logged into the website. Although it is possible that participants may not have completed the questionnaire every time they logged into the website, the results highlight the importance of developing methods that monitor participant activity on the website. As already mentioned, the greater percentage of participants with a financial incentive completing the questionnaire compared to those without the financial incentive helped verify that the former subjects were aware of the financial reward for their PAP use and that lack of knowledge did not explain why PAP adherence was not greater in the financial incentive group. In addition, the precipitous decline in questionnaire completion and absence of any difference between the two groups after the first week suggests that people quickly lost interest in the website. Other recent Internet studies suggest that this finding is not unique to our study and may be a common feature of Internet-based interventions.40–42 Strategies beyond just providing medical information are needed to sustain patient engagement in Web platforms to promote self-management.
The results of this study demonstrate the advantage of using wireless data transmission to monitor PAP adherence and treatment efficacy in research studies. Prior to the availability of this technology, monitoring of PAP adherence was performed by uploading the datachip in the PAP unit. This required that the patient bring or mail the datachip to the sleep center and resulted in lost data in subjects who did not follow protocol. The wireless modem automatically transmits the data daily to the manufacturer's website and requires no action by the participant. In the current study, of the 138 participants who were randomized, PAP data were obtained in 98% of the participants (Figure 1). Technical problems resulted in the missing PAP data in two of the participants. In contrast, only 117 participants (84%) completed the functional outcome questionnaires at the 3-mo endpoint, even though they could do this on the Way to Health website and were paid $30 for completion.
The advantages of using wireless transmission of PAP data extend to clinical management. Proprietary and software-asa-service systems are currently available that provide patients, home health care companies, and practitioners direct access to the patient's PAP treatment data. Home health care companies and practitioners benefit from the greater timeliness of data retrieval that enables more rapid clinical interventions to support the patient.20,22 Patients may benefit by engaging them in self-management and better adherence. The compatibility of these software systems with computer tablets and smart phones increases their potential use by a large patient population. However, Web e-health literacy and interest are required to benefit from these newer technologies. Consideration of e-health literacy–challenged patients and other high-risk patients will be required as patients and providers use more Web technology and communications.
In summary, the major finding of our study is that PAP adherence is significantly improved by giving patients Web access to information about their use of the treatment. Although the addition of a financial incentive in the first week of treatment did not result in even greater PAP use than just Web access to the PAP results, it is likely that this finding is explained by the impressively high level of adherence in the latter group. Other important results are the sustained difference between the Web access groups versus the usual care group throughout the 3-mo observation despite the gradual decline in PAP adherence in all groups. Finally, we found that daily use of the website in both groups with Web access to PAP data dropped markedly following the first week of treatment. Web-based approaches that provide patients with information about their health are increasingly being used to improve healthcare delivery and promote patient self-management. It is important to objectively monitor how patients use these applications and their effect on patient-centered outcomes in order to design portals that engage patients to successfully alter their health behavior.
DISCLOSURE STATEMENT
This was not an industry supported study. The results of this paper were presented at AcademyHealth's 2014 Annual Research Meeting in San Diego, CA in June, 2014. Funding: NIH RC2-AG036592-01; NIH 1P01-1HL094307. P'unk Ave, Inc., a Web-based software company in Philadelphia, PA, created the Way to Health website for the University of Pennsylvania and continued to support the website during the project. Dr. Kuna and Dr. Schutte-Rodin receive grant support from Philips Respironics. Dr. Asch is a Principal at VAL Health (Philadelphia, PA). Dr. Volpp has received research support from Humana, Weight Watchers, and CVS, and has consulted for Val Health. The other authors have indicated no financial conflicts of interest.
Footnotes
A commentary on this article appears in this issue on page 1157.
REFERENCES
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 3.George C. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax. 2001;56:508–12. doi: 10.1136/thorax.56.7.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan AS, Phillips CL, Cistulli PA. Obstructive sleep apnoea–an update. Intern Med J. 2010;40:102–6. doi: 10.1111/j.1445-5994.2009.02069.x. [DOI] [PubMed] [Google Scholar]
- 5.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Basner RC. Continuous positive airway pressure for obstructive sleep apnea. N Engl J Med. 2007;356:1751–8. doi: 10.1056/NEJMct066953. [DOI] [PubMed] [Google Scholar]
- 9.Kribbs NB, Pack AI, Kline LR, et al. Objective measurements of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am J Respir Crit Care Med. 1993;147:887–95. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 10.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–56. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weaver TE, Kribbs NB, Pack AI, et al. Night-to-night variability in CPAP use over first three months of treatment. Sleep. 1997;20:278–83. doi: 10.1093/sleep/20.4.278. [DOI] [PubMed] [Google Scholar]
- 12.Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30:320–4. [PubMed] [Google Scholar]
- 13.Aloia MS, Arnedt JT, Stanchina M, Millman RP. How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behav Sleep Med. 2007;5:229–40. doi: 10.1080/15402000701264005. [DOI] [PubMed] [Google Scholar]
- 14.Rosenthal L, Gerhardstein R, Lumley A, et al. CPAP therapy in patients with mild OSA: implementation and treatment outcome. Sleep Med. 2000;1:215–20. doi: 10.1016/s1389-9457(00)00012-5. [DOI] [PubMed] [Google Scholar]
- 15.Weaver TE. Adherence to positive airway pressure therapy. Curr Opin Pulm Med. 2006;12:409–13. doi: 10.1097/01.mcp.0000245715.97256.32. [DOI] [PubMed] [Google Scholar]
- 16.Weaver TE, Chasens ER. Continuous positive airway pressure treatment for sleep apnea in older adults. Sleep Med Rev. 2007;11:99–111. doi: 10.1016/j.smrv.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159:1096–100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 18.Hui DS, Chan JK, Choy DK, et al. Effects of augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest. 2000;117:1410–6. doi: 10.1378/chest.117.5.1410. [DOI] [PubMed] [Google Scholar]
- 19.Likar LL, Panciera TM, Erickson AD, Rounds S. Group education sessions and compliance with nasal CPAP therapy. Chest. 1997;111:1273–7. doi: 10.1378/chest.111.5.1273. [DOI] [PubMed] [Google Scholar]
- 20.Fox N, Hirsch-Allen AJ, Goodfellow E, et al. The impact of a telemedicine monitoring system on positive airway pressure adherence in patients with obstructive sleep apnea: a randomized controlled trial. Sleep. 2012;35:477–81. doi: 10.5665/sleep.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stepnowsky C, Edwards C, Zamora T, Barker R, Agha Z. Patient perspective on use of an interactive website for sleep apnea. Int J Telemed Appl. 2013;2013:239382. doi: 10.1155/2013/239382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stepnowsky CJ, Palau JJ, Marler MR, Gifford AL. Pilot randomized trial of the effect of wireless telemonitoring on compliance and treatment efficacy in obstructive sleep apnea. J Med Internet Res. 2007;9:e14. doi: 10.2196/jmir.9.2.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimmel SE, Troxel AB, Loewenstein G, et al. Randomized trial of lottery-based incentives to improve warfarin adherence. Am Heart J. 2012;164:268–74. doi: 10.1016/j.ahj.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300:2631–7. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volpp KG, Pauly MV, Loewenstein G, Bangsberg D. P4P4P: an agenda for research on pay-for-performance for patients. Health Aff (Millwood) 2009;28:206–14. doi: 10.1377/hlthaff.28.1.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360:699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 27.Sen AP, Sewell TB, Riley EB, et al. Financial incentives for home-based health monitoring: a randomized controlled trial. J Gen Intern Med. 2014;29:770–7. doi: 10.1007/s11606-014-2778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Asch DA, Volpp KG. On the way to health. LDI Issue Brief. 2012;17:1–4. [PubMed] [Google Scholar]
- 29.Iber C, Ancoli-Israel S, Chesson AL, Quan SF for the American Academy of Sleep Medicine. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM Manual for the Scoring of Sleep and Associated Events. [Google Scholar]
- 30.Kuna ST, Benca R, Kushida CA, et al. Agreement in computer-assisted manual scoring of polysomnograms across sleep centers. Sleep. 2013;36:583–9. doi: 10.5665/sleep.2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chasens ER, Ratcliffe SJ, Weaver TE. Development of the FOSQ-10: a short version of the Functional Outcomes of Sleep Questionnaire. Sleep. 2009;32:915–9. doi: 10.1093/sleep/32.7.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 33.Johns MW. Daytime sleepiness, snoring and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 34.Jenkinson C, Layte R, Jenkinson D, et al. A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med. 1997;19:179–86. doi: 10.1093/oxfordjournals.pubmed.a024606. [DOI] [PubMed] [Google Scholar]
- 35.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Lettieri CJ, Shah AA, Holley AB, Kelly WF, Chang AS, Roop SA. Effects of a short course of eszopiclone on continuous positive airway pressure adherence: a randomized trial. Ann Intern Med. 2009;151:696–702. doi: 10.7326/0003-4819-151-10-200911170-00006. [DOI] [PubMed] [Google Scholar]
- 37.Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–9. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weaver TE, Maislin G, Dinges DF, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Platt AB, Field SH, Asch DA, et al. Neighborhood of residence is associated with daily adherence to CPAP therapy. Sleep. 2009;32:799–806. doi: 10.1093/sleep/32.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M., Jr The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med. 2003;36:410–9. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 41.Smith L, Weinert C. Telecommunication support for rural women with diabetes. Diabetes Educ. 2000;26:645–55. doi: 10.1177/014572170002600412. [DOI] [PubMed] [Google Scholar]
- 42.Strom L, Pettersson R, Andersson G. A controlled trial of self-help treatment of recurrent headache conducted via the Internet. J Consult Clin Psychol. 2000;68:722–7. [PubMed] [Google Scholar]


