Abstract
Objectives:
We examined the changes in waking electroencephalography (EEG) biomarkers with modafinil during continuous positive airway pressure (CPAP) withdrawal in patients with obstructive sleep apnea (OSA) to investigate neurophysiological evidence for potential neurocognitive improvements.
Design:
Randomized double-blind placebo-controlled crossover study. CPAP was used for the first night and then withdrawn for 2 subsequent nights. Each morning after the 2 CPAP withdrawal nights, patients received either 200 mg modafinil or placebo. After a 5-w washout, the procedure repeated with the crossover drug.
Setting:
University teaching hospital.
Participants:
Stable CPAP users (n = 23 men with OSA)
Measurement and Results:
Karolinska Drowsiness Test (KDT) (awake EEG measurement with eyes open and closed), Psychomotor Vigilance Task (PVT), and driving simulator Performance were assessed bihourly during the 3 testing days following CPAP treatment and CPAP withdrawal nights. Compared to placebo, modafinil significantly increased awake EEG activation (faster EEG frequency) with increased alpha/delta (A/D) ratio (P < 0.0001) and fast ratio = (alpha+beta)/(delta+theta) (P < 0.0001) across the 2 days of CPAP withdrawal. The A/D ratio significantly correlated with the driving simulator response time (P = 0.015), steering variation (P = 0.002), and PVT reaction time (P = 0.006). In contrast, individual EEG band power of alpha, beta, theta, and delta did not correlate with any neurocognitive performance.
Conclusions:
Modafinil administration during continuous positive airway pressure (CPAP) withdrawal increased awake EEG activation, which correlated to improved performance. This study provides supporting neurophysiological evidence that modafinil is a potential short-term treatment option during acute CPAP withdrawal.
Citation:
Wang D, Bai XX, Williams SC, Hua SC, Kim JW, Marshall NS, D'Rozario A, Grunstein RR. Modafinil increases awake EEG activation and improves performance in obstructive sleep apnea during continuous positive airway pressure withdrawal. SLEEP 2015;38(8):1297–1303.
Keywords: sleep apnea, EEG spectra, EEG frequency, motor vehicle accident, neurocognitive function, brainwave activity, neurobehavioral performance
INTRODUCTION
Obstructive sleep apnea (OSA) is a common disorder that may lead to excessive daytime sleepiness, reduced neuro-cognitive function, and decreased quality of life.1,2 Untreated OSA is also a significant contributor to motor vehicle crashes.3 As the gold standard treatment for OSA, continuous positive airway pressure (CPAP) has been reported to reverse daytime sleepiness and impairment in cognitive function, including simulated driving performance in patients with OSA.4,5 However, adherence to CPAP is low and temporary withdrawal from CPAP therapy is common because of travel, shift work, mask-related problems, nasal irritation, or respiratory infections.6,7 Acute CPAP withdrawal results in the relapse of sleep disordered breathing and the associated symptoms.6,7
Previously, using a randomized double-blind placebo-controlled crossover design, we demonstrated that acute administration of modafinil, a wakefulness promoter, can improve performance on a driving simulator and sustained attention task, and subjective alertness in patients with OSA during acute CPAP withdrawal.8 Data were collected and analyzed from the AusEd driving simulator (Woolcock Institute, Sydney, Australia), Psychomotor Vigilance Task (PVT, Ambulatory Monitoring, Inc., Ardsley, NY), and Karolinska Sleepiness Scale (KSS).8 Although the waking electroencephalography (EEG) was also performed during this study, the results were not analyzed in our original report because they were not classified as a clinical outcome.8 However, changes in waking EEG may relate to neurobehavioral improvements. Although there are limited studies available, quantitative analysis of EEG (qEEG) / power spectral analysis (PSA) has shown interesting links between awake EEG spectral activity, daytime sleepiness, and neurobehavioral performance.9–13 For example, a new EEG biomarker of detrended fluctuation analysis (DFA) scaling exponent significantly correlated with driving simulator performance and self-rated sleepiness in sleep deprived patients with OSA and control subjects.9 Patients with OSA had a higher DFA scaling exponent and delta power during wakefulness than controls.9 Also, there is a significant cross-correlation between reduced hypercapnia, faster EEG activity (reduced EEG delta/alpha ratio), and reduced daytime sleepiness in patients with severe sleep disordered breathing using positive airway pressure treatment.14
The current study is an investigation of the mechanism for the clinical effect seen in our trial.8 We investigated whether modafinil alters waking EEG activity during CPAP withdrawal in order to elucidate relevant brain neuroelectrical mechanisms of the neurocognitive improvement. We also examined whether EEG biomarkers such as DFA, alpha/delta (A/D) ratio, fast ratio [the power ratio of (alpha+beta)/(delta+theta)], and individual EEG frequency bands correlated with the clinical neurocognitive performance improvements.
METHODS
This randomized double-blind, placebo-controlled, crossover study was conducted at the Department of Respiratory and Sleep Medicine, Royal Prince Alfred Hospital, a major teaching hospital of the University of Sydney. The protocol was ethically approved by the Sydney South West Area Health Service Ethics Review Committee (Protocol No: X04 0091). The Australian New Zealand Clinical Trials Registry number is ACTRN12606000027516. All patients gave written informed consent prior to the study. The primary trial findings of the effects of modafinil on neurocognitive measures have been described previously.8
Participants
We recruited 23 male patients with OSA who received a diagnosis using overnight polysomnography (PSG) with apnea-hypopnea index (AHI) > 10 and had successfully used CPAP for at least 1 y. They were modafinil naïve and did not have any other uncontrolled concurrent medical or psychiatric conditions. They did not take medications that may have affected alertness.8
Study Protocol
The procedure is summarized in Figure 1. Eligible patients, after a period of screening, were admitted to the laboratory for 3 consecutive nights. CPAP was administered on the first night, then withdrawn on the 2 subsequent nights. We defined the “on-CPAP” night as the baseline night, followed by the baseline day. The 2 following days were defined as Day 1 and Day 2, respectively. Throughout the baseline day and Day 1, Karolinska Drowsiness Test (KDT), driving simulator, PVT, and KSS were repeatedly administered at 2-h intervals from approximately 08:00 to 20:00 (seven repeated sessions each day). On Day 2, those tests were performed every 2 h from 08:00 to 14:00 (four sessions). Patients were randomly assigned to be administered an oral dose of either 200 mg modafinil or placebo with both of their breakfasts on Days 1 and 2 (around 07:00).
Figure 1.
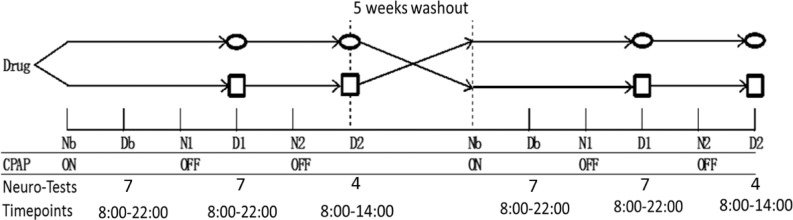
Diagram of the study procedure. Neuro-Tests indicate numbers of the bihourly testing sessions of Karolinska Drowsiness Test, Psychomotor Vigilance Task, AusEd driving simulator, and Karolinska Sleepiness Scale in each testing day. D, day; Db, baseline day; N, night; Nb, baseline night; ovals, administration of 200 mg modafinil; rectangles, administration of placebo; CPAP, continuous positive airway pressure.
Following a 5-w washout period, participants repeated the protocol but received the alternate medication (Figure 1). Study personnel involved with those procedures/tests or with recruitment of patients never had access or knowledge of the allocation sequence and were blinded to which drug the patients were receiving. Patients were told that they would be receiving either modafinil or placebo in random order in each of their testing weekends. Modafinil and placebo tablets had identical appearances and were dispensed by a research pharmacist who had no contact with patients.8
Measurements
Resting awake EEG was recorded during a KDT, which comprised repeated sessions of 7.5-min EEG recordings.4 Each 7.5-min session started with a 2.5-min eyes-open time, then 2.5-min eyes closed, then another 2.5-min of eyes open. Thirty seconds at the beginning of each 2.5-min segment were discarded from analysis to avoid the artefact caused by patients settling to the new task after being instructed to change behavior. The Alice 4 PSG system (Philip Respironics, Murrysville, PA, USA) was used with a sampling rate of 200 Hz. EEG recording channels included C3-A2, C4-A1, Fz-A2, Cz-A1, Pz-A2, Oz-A1 and left and right electrooculogram (EOG).
Other neurobehavioral tests included 2-h repeated sessions of 30-min AusEd driving simulator,15 10-min Psychomotor Vigilance Task (PVT) (Ambulatory Monitoring, Inc., Ardsley, NY),16 and Karolinska Sleepiness Scale (KSS).17
EEG Spectral Analyses
The EEG recordings were blindly analyzed by one of the authors (JWK) using internally developed software and validated methods that have been described previously.9,18 Delta, theta, alpha, and beta bands were defined as the frequency ranges 0.5–4.5 (delta), 4.5–8 (theta), 8–12 (alpha), and 12–32 (beta) Hz, respectively. The EEGs were then further examined by an automatic algorithm that excluded EOG artefact via the independent components method and EEG segments showing excessive delta and/or beta power using a standard statistical rule (i.e., median + standard deviation).9,18 For our statistical analyses, we focused primarily on the EEG recorded at C3-A2. However, when the C3-A2 channel was contaminated by artefact, we used C4-A1 as an alternative channel. Individual spectral band power and total summed power between 0.5–32 Hz were calculated. A/D ratio was calculated as absolute delta power/alpha power. Fast ratio was defined as the power ratio of (alpha+beta)/(delta+theta). Detailed methods of analyzing DFA scaling exponent have been described previously.9,19
Statistical Analysis
Descriptive data were expressed as mean ± standard deviation unless otherwise stated. Mixed-model analyses of variance were used to compare the drug effects on EEG biomarkers overall and at each time point (SAS Institute, version 9.1, Cary, NC). Within-subject correlations between the EEG biomarkers and neurocognitive outcomes were tested with Bland-Altman correlation coefficients for repeated observations using SPSS (SPSS 21, Chicago, IL, US).20 A P value less than 0.05 was considered significant.
RESULTS
Two participants withdrew from the study due to CPAP technical difficulties and personal schedule conflicts. Twenty-one men in whom OSA was diagnosed (apnea-hypopnea index [AHI] 48.7 ± 23.9/h; age 55 ± 8 y; BMI 32.7 ± 4.1 kg/m2) completed the study. While on CPAP, the participants' baseline Epworth Sleepiness Scale (ESS) was 8.7 ± 4.0 and residual AHI was 2.6 ± 1.2/h. Average CPAP usage was 7.1 ± 0.8 h. All measured parameters of driving simulator performance and overall reaction time were improved by modafinil during CPAP withdrawal. Modafinil also improved PVT response time and frequency of lapses and improved subjective alertness (KSS). Further patient characteristic details and results can be found in the main publication.8
The Effect of Modafinil on Awake EEG during CPAP Withdrawal
Compared to placebo, modafinil use resulted in significantly faster/more active awake EEG during CPAP withdrawal, with significantly higher A/D ratio and fast ratio and lower DFA scaling exponent (all P ≤ 0.001) on all three states (eyes open, closed, and overall, see Table 1). Overall state was calculated as the average of eyes open and eyes closed states. In contrast, except for delta power, individual EEG spectral band powers did not show major difference between modafinil and placebo in any state (all P > 0.05, Table 1). Delta power was lower with modafinil use during eyes open and overall state (P = 0.001), but that difference was not observed during eyes closed (P = 0.49). There was a trend toward a reduced theta power with modafinil during eyes open and overall (P < 0.1).
Table 1.
The effects of modafinil on electroencephalographic biomarkers.
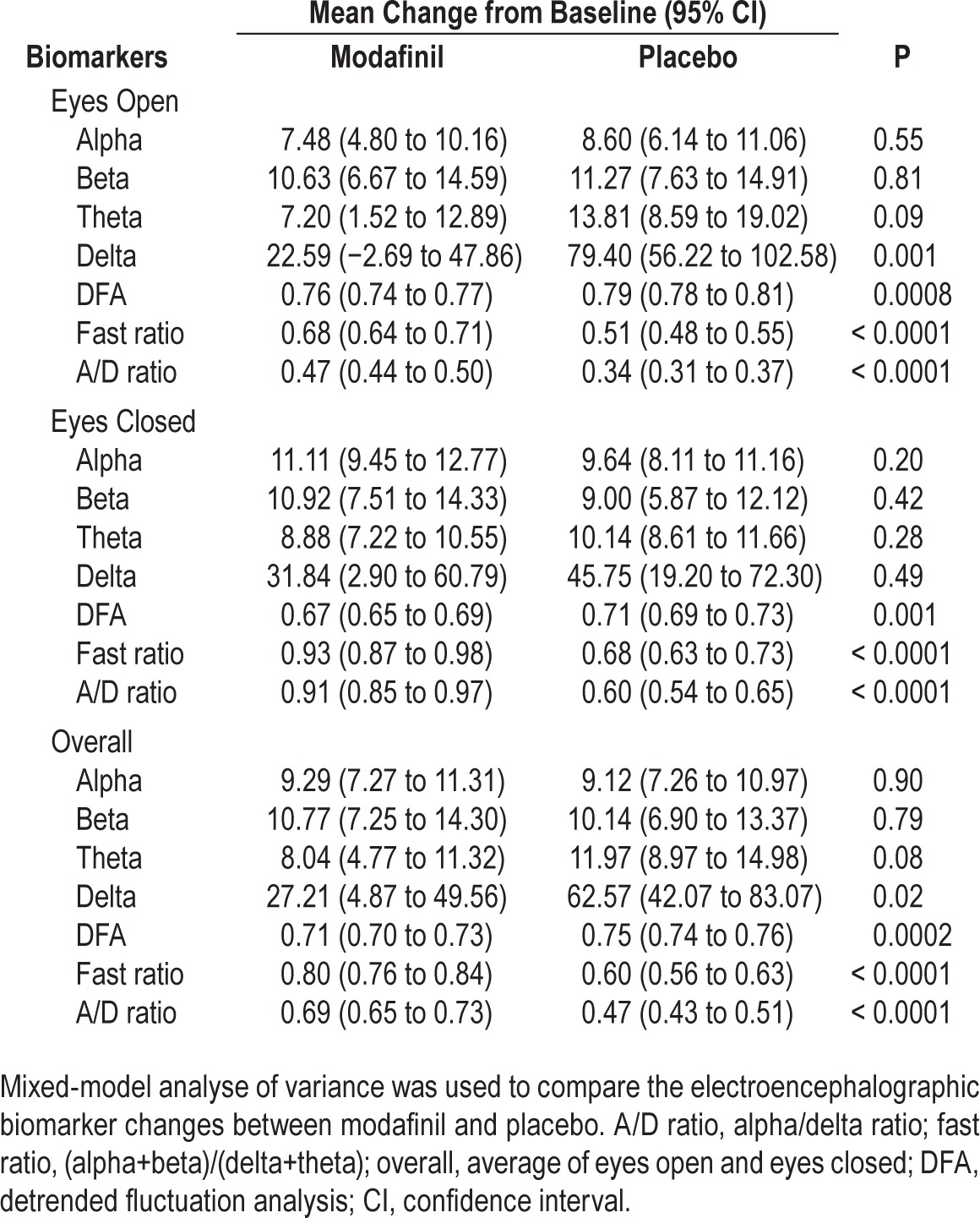
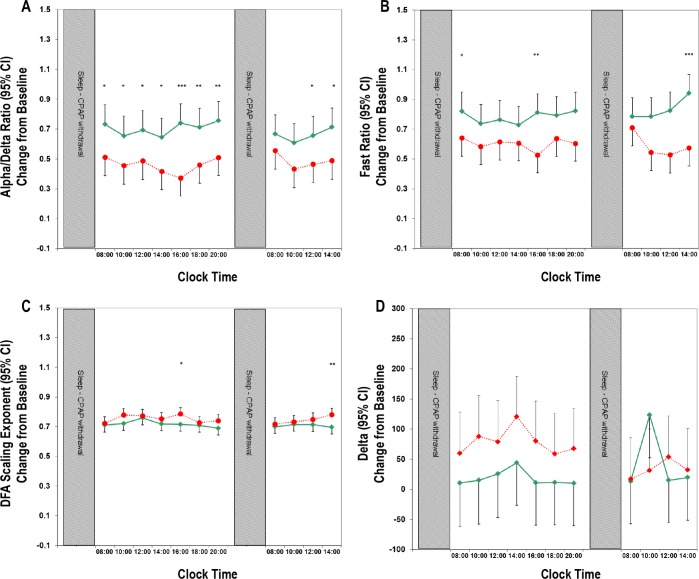
Figure 2 shows bihourly changes in four key EEG bio-markers during the 2 days of CPAP withdrawal with the use of modafinil/placebo (Table 1 shows significant overall differences and Figure 2 shows when specifically they occurred). A/D ratio showed differences in 9 of 11 time points between the real and placebo drugs. In contrast, fast ratio, DFA scaling exponent, and delta power only showed significant differences at 3 of 11, 2 of 11, and 0 of 11 time points, respectively.
Figure 2.
Comparison of the effects of modafinil and placebo on four key electroencephalography (EEG) biomarkers during 2-h assessments over the 2 days of CPAP withdrawal. The four biomarkers were alpha/delta ratio (A), fast ratio (B), detrended fluctuation analysis (DFA) scaling exponent (C), and delta band power (D). The EEG biomarkers were average values of the eyes-open and eyes-closed states. Mixed model analyses of variance were used to test the differences at each time point. Error bars denote the 95% confidence intervals (CIs). Solid green lines, modafinil; dashed red lines, placebo. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001. CPAP, continuous positive airway pressure; CI, confidence interval.
Correlation Between EEG Biomarkers and Neurobehavioral Performance
EEG activation significantly correlated with neurocognitive performance. As shown in Table 2, during the eyes-closed state, A/D ratio significantly correlated (P < 0.05) with three of five key parameters in the driving simulator and PVT performance, and tended to correlate (P < 0.1) with the remaining two key parameters. Fast ratio significantly correlated with two of the key parameters and tended to correlate with two others. The DFA scaling exponent also significantly correlated with two of the five key parameters (Table 2). Those correlations were more apparent during the eyes-closed state. None of the traditional individual EEG frequency band powers significantly correlated with any of the neurocognitive outcomes (Table 2).
Table 2.
Association between electroencephalographic biomarkers and neurocognitive outcomes.
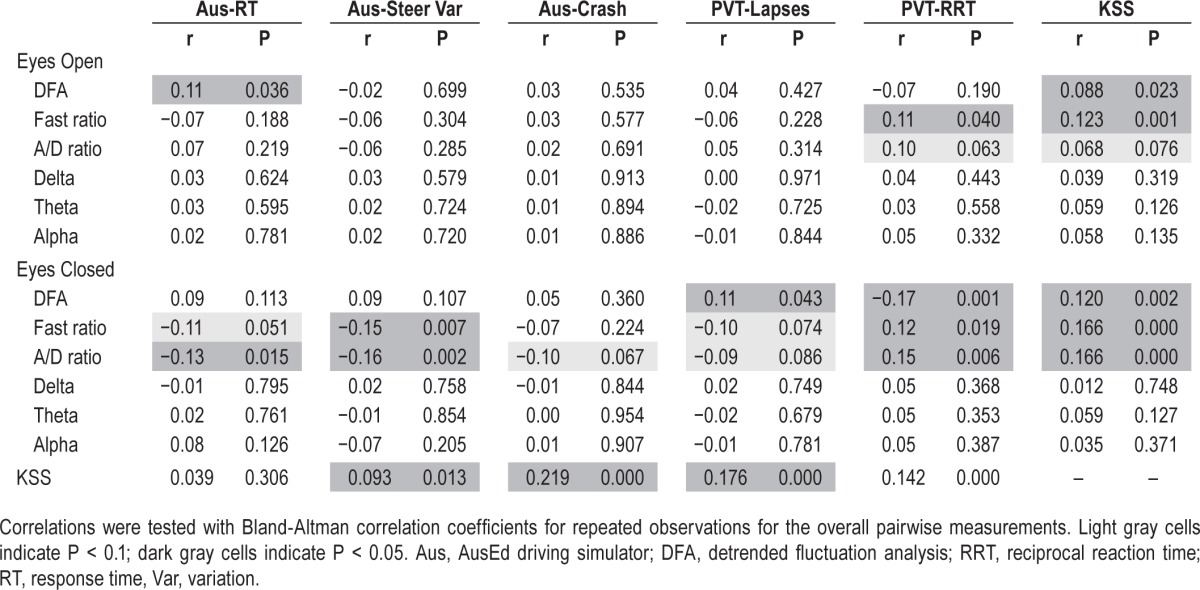
Similar to the driving simulator and PVT parameters, during the eyes-closed state, subjective alertness KSS significantly correlated with A/D ratio, fast ratio, and DFA but not with any of the individual frequency bands. In addition, KSS significantly correlated with four of five key parameters in driving simulator and PVT performance (Table 2).
DISCUSSION
This randomized placebo-controlled crossover study demonstrated that modafinil increases EEG activation (faster EEG frequency) in patients with OSA undergoing acute CPAP withdrawal and that these EEG changes correlated with the modafinil-induced improvements in neurocognitive performance. This finding provides neurophysiological evidence that modafinil treatment during acute CPAP withdrawal ameliorates EEG slowing in OSA in parallel with cognitive and neurobehavioral improvements in tests such as simulated driving. In addition, we found that compared to other EEG biomarkers, the A/D ratio was a robust biomarker in tracking drug-induced changes.
As a wake-promoting agent, the EEG-modifying properties of modafinil have been mainly studied in the context of narcolepsy and sleep deprivation.21 Using low resolution brain electromagnetic tomography (LORETA), 3 w of treatment with 400 mg modafinil reversed the decrement of alpha-2 and beta-1–3 power in 16 patients with narcolepsy compared to the normal controls.22 There was also a decrease of theta and delta power in resting EEG with the modafinil use.22 Additional study from this group found that 3 w of 400 mg modafinil improved a cognitive performance test (Pauli test) in 15 patients with narcolepsy. The improvement in Pauli test results was correlated with the decrease in delta, theta, and alpha-1 power.13 A less significant correlation was observed between midmorning EEG LORETA and multiple sleep latency test (MSLT). No correlation was found between EEG LORETA and subjective daytime sleepiness measurement ESS.13 Modafinil has also been reported to promote wakefulness by reducing delta and theta activity and increasing alpha and beta activity in 25 sleep deprived healthy men.23 These findings are generally consistent with our observations in that modafinil may promote wakefulness and vigilance through inducing a faster EEG.
The current study differs from previous reports in that it involves a CPAP-withdrawal paradigm in a standard clinical sleep laboratory setting in patients with OSA. In addition, we correlated the EEG markers with simulated driving ability and PVT, which are particularly relevant to real-life scenarios. In addition, although most of the previous studies have investigated the effect of modafinil on individual EEG frequency bands, there is a clinical rationale to determine whether a single EEG biomarker relates to simulated driving and neurocognitive impairment. Previously we observed that the DFA scaling exponent generally correlates better than individual EEG bands in driving simulator performance and PVT using a sleep deprivation paradigm.9 Moreover, delta/alpha ratio is a key marker of EEG activation significantly cross-correlating with the improvement of subjective daytime sleepiness and hypercapnia in patients with hypercapnia and sleep disordered breathing.14 In the current study, as shown in Table 1 and Figure 2, A/D ratio, fast ratio, and DFA are much more sensitive than individual EEG frequency bands in picking up modafinil induced EEG changes. Similarly, A/D ratio, fast ratio, and DFA significantly correlated with driving simulator performance, PVT, and KSS, whereas individual band power did not correlate with any cognitive parameter (Table 2). There are a few potential reasons. First, drowsiness could be more related to an overall EEG slowing effect with simultaneous decrease in fast wave activity and increased in slow wave activity.14 Second, total EEG power is variable between each measurement where a ratio measure would be less affected for an EEG slowing effect. Third, certain health conditions can easily affect a single frequency band power. For example, “alpha-delta sleep” can often be seen in fibromyalgia syndrome, and a variety of pain and psychiatric conditions are related to alpha-sleep anomaly.24,25 A single alpha band is unlikely to be an ideal marker for alertness.
Our study shows that A/D ratio is particularly sensitive in picking up the modafinil induced bihour EEG change compared to other EEG markers (Figure 2). In addition, A/D ratio showed more significant correlations with the key cognitive parameters than fast ratio and DFA. Given that A/D ratio is simpler to calculate compared to the fast ratio and DFA scaling exponent, A/D ratio appears to be the most sensitive EEG bio-marker in the current study in reflecting modafinil-induced performance improvements. A/D ratio has been reported as a marker of EEG slowing in Alzheimer disease correlating with cerebrospinal fluid tau level in those patients with severe cognitive decline.26 It is also useful in differencing Alzheimer disease from subcortical vascular dementia in patients with the same degree of dementia.27 In addition, A/D ratio has been reported as a marker of pain during sleep28 and a sensitive marker to detect delayed cerebral ischemia.29 In animal studies, A/D ratio was used as a biomarker to determine unconsciousness, which correlated closely with loss of posture in broilers.30
Our findings were derived from standard clinical PSG laboratory settings. EEG spectral analyses were calculated from channel C3-A2 or C4-A1. In this context, we found that individual alpha, beta, or theta power did not correlate with any cognitive change. In addition, the calculation of fast ratio [(alpha+beta)/(delta+theta)] did not provide a better correlation compared to a simple A/D ratio. Our findings may not apply outside of the relatively tightly controlled clinical PSG laboratory context. The neuroanatomic sites of action of modafinil are poorly understood. It is possible that modafinil may activate brainstem centers and diffuse widely on cortical distribution.21,31 Using frontotemporal topography, a recent study found that modafinil may enhance oscillatory power associated with high-control rule selection in theta, alpha, and beta ranges.32 Both EEG alpha and theta oscillations are important in cognitive and memory performance but may reflect different subtypes with different underlying mechanisms in brain feedback loops.33 Further studies with comprehensive EEG placement/whole brain functional magnetic resonance imaging/neurochemical analyses are needed to better understand the effect of modafinil on brain neuro-electrical activity.
Our study also has other limitations. The sample size was relatively small, which was limited by the efficiency required by the randomized controlled trial study design and extremely labor-intensive testing protocol. We only tested men because both OSA and motor vehicle accidents are more likely in males and there are major differences in EEG pattern between men and women.34–36 Further studies including females and with larger sample sizes are certainly needed to fully generalize our findings to the general population. In addition, the effect of modafinil administration was studied in a short period of CPAP withdrawal. The efficacy in a longer withdrawal period is also worth investigating.
In conclusion, modafinil administration during short-term cessation of CPAP in patients with OSA increased EEG activation, which correlated with the improvement in neurocognitive performance. This study provided neurophysiological evidence that modafinil as a short-term treatment option may prevent motor vehicle accidents. A/D ratio could be considered as a key EEG biomarker for EEG activation, which correlates to cognitive performance in this patient group.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Wang is supported by NHMRC Project Grant (1043633). Professor Grunstein is supported by NHMRC Practitioner Fellowship (1022730). Dr. Kim, Dr. Williams, and Dr. D'Rozario were supported by NHMRC Centre for Research Excellence in Sleep Medicine (571421) and the NHMRC Centre for Research Excellence in NeuroSLEEP (1060992). The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- A/D ratio
Alpha/Delta ratio
- AHI
apnea-hypopnea index
- CPAP
continuous positive airway pressure
- DFA
detrended fluctuation analysis
- EOG
electrooculogram
- ESS
Epworth Sleepiness Score
- KDT
Karolinska Drowsiness Test
- KSS
Karolinska Sleepiness Scale
- LORETA
low resolution brain electromagnetic tomography
- MSLT
multiple sleep latency test
- OSA
obstructive sleep apnea
- PVT
Psychomotor Vigilance Task
- PSG
polysomnography
REFERENCES
- 1.Lindberg E, Carter N, Gislason T, Janson C. Role of snoring and daytime sleepiness in occupational accidents. Am J Respir Crit Care Med. 2001;164:2031–5. doi: 10.1164/ajrccm.164.11.2102028. [DOI] [PubMed] [Google Scholar]
- 2.Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002;360:237–45. doi: 10.1016/S0140-6736(02)09464-3. [DOI] [PubMed] [Google Scholar]
- 3.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 4.Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006:CD001106. doi: 10.1002/14651858.CD001106.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Kylstra WA, Aaronson JA, Hofman WF, Schmand BA. Neuropsychological functioning after CPAP treatment in obstructive sleep apnea: a meta-analysis. Sleep Med Rev. 2013;17:341–7. doi: 10.1016/j.smrv.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Phillips CL, Yang Q, Williams A, et al. The effect of short-term withdrawal from continuous positive airway pressure therapy on sympathetic activity and markers of vascular inflammation in subjects with obstructive sleep apnoea. J Sleep Res. 2007;16:217–25. doi: 10.1111/j.1365-2869.2007.00589.x. [DOI] [PubMed] [Google Scholar]
- 7.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams SC, Marshall NS, Kennerson M, Rogers NL, Liu PY, Grunstein RR. Modafinil effects during acute continuous positive airway pressure withdrawal: a randomized crossover double-blind placebo-controlled trial. Am J Respir Crit Care Med. 2010;181:825–31. doi: 10.1164/rccm.200908-1307OC. [DOI] [PubMed] [Google Scholar]
- 9.D'Rozario AL, Kim JW, Wong KK, et al. A new EEG biomarker of neurobehavioural impairment and sleepiness in sleep apnea patients and controls during extended wakefulness. Clin Neurophysiol. 2013;124:1605–14. doi: 10.1016/j.clinph.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 10.Finnigan S, Robertson IH. Resting EEG theta power correlates with cognitive performance in healthy older adults. Psychophysiology. 2011;48:1083–7. doi: 10.1111/j.1469-8986.2010.01173.x. [DOI] [PubMed] [Google Scholar]
- 11.Lal SK, Craig A. Driver fatigue: electroencephalography and psychological assessment. Psychophysiology. 2002;39:313–21. doi: 10.1017/s0048577201393095. [DOI] [PubMed] [Google Scholar]
- 12.Morisson F, Lavigne G, Petit D, Nielsen T, Malo J, Montplaisir J. Spectral analysis of wakefulness and REM sleep EEG in patients with sleep apnoea syndrome. Eur Respir J. 1998;11:1135–40. doi: 10.1183/09031936.98.11051135. [DOI] [PubMed] [Google Scholar]
- 13.Saletu M, Anderer P, Semlitsch HV, et al. Low-resolution brain electromagnetic tomography (LORETA) identifies brain regions linked to psychometric performance under modafinil in narcolepsy. Psychiatry Res. 2007;154:69–84. doi: 10.1016/j.pscychresns.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Wang D, Piper AJ, Yee BJ, et al. Hypercapnia is a key correlate of EEG activation and daytime sleepiness in hypercapnic sleep-disordered breathing patients. J Clin Sleep Med. 2014;10:517–22. doi: 10.5664/jcsm.3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai AV, Wilsmore B, Bartlett DJ, et al. The utility of the AusEd driving simulator in the clinical assessment of driver fatigue. Behav Res Methods. 2007;39:673–81. doi: 10.3758/bf03193039. [DOI] [PubMed] [Google Scholar]
- 16.Basner M, Dinges DF. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011;34:581–91. doi: 10.1093/sleep/34.5.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gillberg M, Kecklund G, Akerstedt T. Relations between performance and subjective ratings of sleepiness during a night awake. Sleep. 1994;17:236–41. doi: 10.1093/sleep/17.3.236. [DOI] [PubMed] [Google Scholar]
- 18.Kim JW, Shin HB, Robinson PA. Quantitative study of the sleep onset period via detrended fluctuation analysis: normal vs. narcoleptic subjects. Clin Neurophysiol. 2009;120:1245–51. doi: 10.1016/j.clinph.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 19.Kim JW, Shin H, Kim EJ, et al. Characteristic time scales of electroencephalograms of narcoleptic patients and healthy controls. Comput Biol Med. 2010;40:831–8. doi: 10.1016/j.compbiomed.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Bland JM, Altman DG. Calculating correlation coefficients with repeated observations: Part 1–Correlation within subjects. BMJ. 1995;310:446. doi: 10.1136/bmj.310.6977.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minzenberg MJ, Carter CS. Modafinil: a review of neurochemical actions and effects on cognition. Neuropsychopharmacology. 2008;33:1477–502. doi: 10.1038/sj.npp.1301534. [DOI] [PubMed] [Google Scholar]
- 22.Saletu M, Anderer P, Saletu-Zyhlarz GM, et al. EEG-tomographic studies with LORETA on vigilance differences between narcolepsy patients and controls and subsequent double-blind, placebo-controlled studies with modafinil. J Neurol. 2004;251:1354–63. doi: 10.1007/s00415-004-0543-8. [DOI] [PubMed] [Google Scholar]
- 23.James LM, Iannone R, Palcza J, et al. Effect of a novel histamine subtype-3 receptor inverse agonist and modafinil on EEG power spectra during sleep deprivation and recovery sleep in male volunteers. Psychopharmacology (Berl) 2011;215:643–53. doi: 10.1007/s00213-010-2158-3. [DOI] [PubMed] [Google Scholar]
- 24.May KP, West SG, Baker MR, Everett DW. Sleep apnea in male patients with the fibromyalgia syndrome. Am J Med. 1993;94:505–8. doi: 10.1016/0002-9343(93)90085-4. [DOI] [PubMed] [Google Scholar]
- 25.Moldofsky H. Sleep and pain. Sleep Med Rev. 2001;5:385–96. doi: 10.1053/smrv.2001.0179. [DOI] [PubMed] [Google Scholar]
- 26.Jelic V, Blomberg M, Dierks T, et al. EEG slowing and cerebrospinal fluid tau levels in patients with cognitive decline. Neuroreport. 1998;9:157–60. doi: 10.1097/00001756-199801050-00032. [DOI] [PubMed] [Google Scholar]
- 27.Gawel M, Zalewska E, Szmidt-Salkowska E, Kowalski J. The value of quantitative EEG in differential diagnosis of Alzheimer's disease and subcortical vascular dementia. J Neurol Sci. 2009;283:127–33. doi: 10.1016/j.jns.2009.02.332. [DOI] [PubMed] [Google Scholar]
- 28.Della Marca G, Frusciante R, Vollono C, et al. Pain and the alpha-sleep anomaly: a mechanism of sleep disruption in facioscapulohumeral muscular dystrophy. Pain Med. 2013;14:487–97. doi: 10.1111/pme.12054. [DOI] [PubMed] [Google Scholar]
- 29.Claassen J, Hirsch LJ, Kreiter KT, et al. Quantitative continuous EEG for detecting delayed cerebral ischemia in patients with poor-grade subarachnoid hemorrhage. Clin Neurophysiol. 2004;115:2699–710. doi: 10.1016/j.clinph.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 30.Benson ER, Alphin RL, Rankin MK, Caputo MP, Kinney CA, Johnson AL. Evaluation of EEG based determination of unconsciousness vs. loss of posture in broilers. Research in veterinary science. 2012;93:960–4. doi: 10.1016/j.rvsc.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Della Marca G, Restuccia D, Rubino M, Maiese T, Tonali P. Influence of modafinil on somatosensory input processing in the human brain-stem. Clin Neurophysiol. 2004;115:919–26. doi: 10.1016/j.clinph.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Minzenberg MJ, Gomes GC, Yoon JH, et al. Modafinil augments oscillatory power in middle frequencies during rule selection. Psychophysiology. 2014;51:510–9. doi: 10.1111/psyp.12201. [DOI] [PubMed] [Google Scholar]
- 33.Klimesch W. EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain research. Brain research reviews. 1999;29:169–95. doi: 10.1016/s0165-0173(98)00056-3. [DOI] [PubMed] [Google Scholar]
- 34.Dijk DJ, Beersma DG, Bloem GM. Sex differences in the sleep EEG of young adults: visual scoring and spectral analysis. Sleep. 1989;12:500–7. doi: 10.1093/sleep/12.6.500. [DOI] [PubMed] [Google Scholar]
- 35.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 36.Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]