Much of a physician's day is spent maintaining the patient health record.1–6 Not only has this negatively impacted job satisfaction for residents and attending physicians,7,8 but it also may be significantly reducing available time for patient care and negatively impacting patient outcomes.9,10 In a 2013 poll, 92% of residents reported that clinical documentation obligations are excessive, and 73% of residents reported compromises in patient care by these requirements.11 Among internal medicine residents surveyed in 2006, two-thirds reported spending more than 4 hours daily on documentation, while only one-third recounted spending this amount of time with patients themselves.1 For every 3 minutes spent face-to-face with a patient, 1 minute is needed for clerical tasks, with charting comprising the brunt of this work.3,12–14 These data are corroborated by a meta-analysis from 2010 that reported only 23% of a hospitalist's time is spent directly interacting with patients.15
One would think that advances in technology16 might reduce time committed to clinical documentation due to streamlining of data through an electronic health record (EHR); however, residents and attending physicians may be spending up to 3 times longer with the EHR than when they were using paper charting.17,18 The purpose of this perspective is to review the utility of the current practice of clinical documentation in US hospitals, assess areas of weakness, and discuss potential avenues for improvement.
Benefits and Weaknesses of Clinical Documentation
Specific degrees of documentation are required by “Meaningful Use” regulations and act as incentives for physician compensation.19,20 It may seem obvious that the current health record has been developed to improve the quality of patient care, and it achieves this through various objectives. Only 2 of the major objectives of the documentation process are reviewed here as examples: (1) the improvement of interprovider communication, and (2) the prevention of medical error. These objectives were selected because they are 2 of the most commonly cited goals for medical data capture,21–23 and they also are high-priority targets for quality improvement, since the outcomes achieved can be quantitatively measured.
Improvement of Interprovider Communication
Anecdotally, medical documentation not only centralizes access to critical medical data, but also serves as a useful tool for information handoff during transitions of care. Unfortunately, whether due to constraints of having to rigorously and repeatedly document medical information or because of laxity, US providers are still not documenting clinical data accurately—thereby decreasing the utility of information being transferred.24,25 With increasing volumes of paperwork and redundancy in data capture, resident and staff physicians are also less likely to review clinical documents in their entirety,26,27 thereby increasing the risk of negligent behavior. Data are frequently automated via templates, which carries significant risk of inaccurate reporting due to falsely negative examination findings.28 Or worse, with the advent of the EHR, information can effortlessly be copied from prior charts, which could thereby perpetuate inaccurate data.29,30 According to a report of 167 000 Veterans Health Administration records, as many as 1 in 4 charts contain copied/pasted examination data, with medical students, interns, and residents responsible for the majority of these copied data.31
Prevention of Medical Error
Particularly with the rising number of pharmacological agents and interactions,32 the risks of medication interaction are expected to skyrocket. It is nearly impossible, even for pharmacists with advanced training, to maintain a sufficient degree of competency to prevent adverse events through drug interactions. The availability of electronic user interfaces during dynamic data documentation combats this weakness in health care and allows for automation of alert messages in order to reduce medication error,22,33 as well as errors with order entry in general. However, with the rising number of alert messages during the dynamic electronic documentation process, we run the risk of “alert fatigue” among care providers. According to 1 survey at a not-for-profit academic center, the majority of polled faculty physicians admitted to neglecting alerts when they appeared on screen.34 To date, there are no prospective studies that have assessed alert fatigue among resident physicians. While centralized documentation may be helpful in preventing medical error, a balance has yet to be struck between automated and appropriate notification.
Targets for Intervention
In order to optimize interprovider communication of health record data, efforts should be made to increase both the utility and accuracy of the data being communicated. While data utility is more of a subjective perception (eg, including echocardiographic data in a discharge summary that may not be particularly useful for the patient's dermatologist), accuracy is measurable and can therefore be targeted. The automation of data capture and documentation (eg, linking laboratory results and vital signs to provider notes) is 1 intervention that has improved charting accuracy in the recent past. The next step would be to determine what other data should or should not be automated in the clinical record without risking templating28 or copy/paste31 errors. This has been the subject of an excellent review by Weis and Levy.30
The prevention of medical error has already been a prominent goal for EHR design. Unfortunately, current alert systems for medication interaction and for clinical deterioration are too many to be appreciated. Rather than the vast compendium of computer data, residents and other care providers are being left with their (sometimes limited) clinical judgment to determine best practices. To reduce the risk of alert fatigue, only the most critical messages should be automated. To accomplish this, investigators at 1 center conducted a retrospective review of alert messages across 7 study periods, with most participants being resident physicians. They demonstrated that a nearly 3-fold reduction in medication error alerts was not associated with an increased risk of medication errors.35 These results should be confirmed by prospective trials using similar internal audits with the aims of reducing alert fatigue and potentially improving provider attention to critical messages. By eliminating superfluous notifications, residents might be more apt to attend to these critical alerts, which are thought to impact decision making.
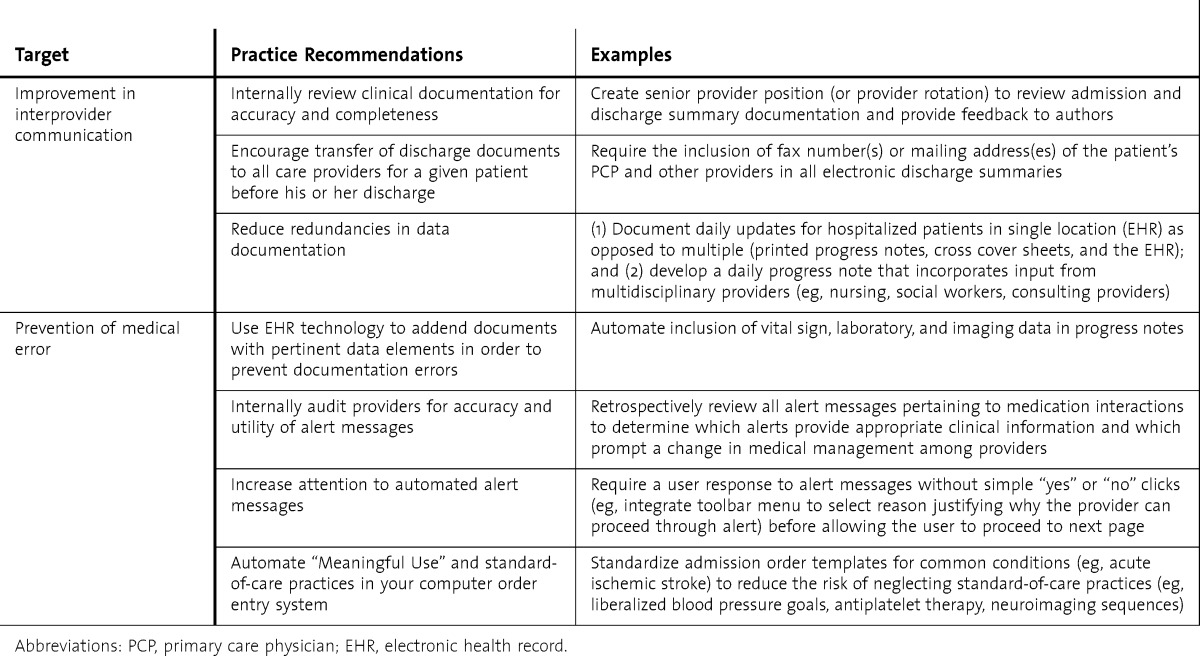
See the table for a summary of suggested practice recommendations for these 2 EHR objectives.
TABLE.
Suggested Practice Recommendations
Conclusions
Clinical documentation is a constantly evolving process that has exploded in recent decades with the advent of the EHR.26 At present, the state-of-the-art health record seems ill-fitted to serve its purpose as a repository of pertinent clinical data. It comes as no surprise that the health record is lacking in both accurate and up-to-date patient information that may be helpful for interprovider communication, and it has become too vast for resident providers to attend to critical messages in order to obviate medical error. In fact, the only truly effective purpose for the health record is to allow providers to bill for services,21 and even this has led to appreciable discontent among residents because of the complexities inherent to billing and the difficulties in obtaining reimbursements for services rendered. The format of the current progress note may even warrant complete redesign to optimize access to medical information, and this has already been explored at some centers.36
All things considered, just as resident physicians are called on to do no harm, they are charged with the task of documenting their decisions. Residents will not be able to enhance health record accuracy, given most current EHRs, unless they spend even less time per patient, or manage fewer patients overall. At present, not only do documentation requirements affect quality of resident life, but they can also limit the available time for educating physician trainees. It is the job of the resident, faculty member, and residency program director to investigate and implement new methods of clinical documentation in order to reduce time spent charting, and ultimately reacquaint the resident with his or her patient. With appropriate interventions to improve documentation strategies, we hope that future residents will make more time for their patients instead of their paperwork.
Footnotes
All authors are at the Hospital of the University of Pennsylvania. James E. Siegler, MD, is a Neurology Resident; Neha N. Patel, MD, is Assistant Professor of Clinical Medicine, Director of Quality, Section of Hospital Medicine, and Codirector of Healthcare Leadership, Quality Residency Track; and C. Jessica Dine, MD, is Assistant Professor of Medicine, Director of the Core Faculty Program, Fellow of the Leonard Davis Institute of Health Economics, and Associate Program Director, Internal Medicine Residency Program.
References
- 1.Oxentenko AS, West CP, Popkave C, Weinberger SE, Kolars JC. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med. 2010;170(4):377–380. doi: 10.1001/archinternmed.2009.534. [DOI] [PubMed] [Google Scholar]
- 2.Baron RJ. What's keeping us so busy in primary care: a snapshot from one practice. N Engl J Med. 2010;362(17):1632–1636. doi: 10.1056/NEJMon0910793. [DOI] [PubMed] [Google Scholar]
- 3.Ammenwerth E, Spötl HP. The time needed for clinical documentation versus direct patient care: a work-sampling analysis of physicians' activities. Methods Inf Med. 2009;48(1):84–91. [PubMed] [Google Scholar]
- 4.Farber J, Siu A, Bloom P. How much time do physicians spend providing care outside of office visits. Ann Intern Med. 2007;147(10):693–698. doi: 10.7326/0003-4819-147-10-200711200-00005. [DOI] [PubMed] [Google Scholar]
- 5.Rolfe IE, Pearson S, Sanson-Fisher R, Fardell SD, Kay FJ, Gordon J. Measuring the hospital experiences of junior doctors. Med Educ. 1998;32(3):312–319. doi: 10.1046/j.1365-2923.1998.00206.x. [DOI] [PubMed] [Google Scholar]
- 6.Dresselhaus TR, Luck J, Wright BC, Spragg RG, Lee ML, Bozzette SA. Analyzing the time and value of housestaff inpatient work. J Gen Intern Med. 1998;13(8):534–540. doi: 10.1046/j.1525-1497.1998.00164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babbott S, Manwell LB, Brown R, Montaque E, Williams E, Schwartz M, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100–e106. doi: 10.1136/amiajnl-2013-001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mechanic D. Physician discontent: challenges and opportunities. JAMA. 2003;290(7):941–946. doi: 10.1001/jama.290.7.941. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(suppl 3):110–127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Kawaguchi T, Karaboyas A, Robinson BM, Li Y, Fukuhara S, Bieber BA, et al. Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. J Am Soc Nephrol. 2013;24(9):1493–1502. doi: 10.1681/ASN.2012080831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christino MA, Matson AP, Fischer SA, Reinert SE, Digiovanni CW, Fadale PD. Paperwork versus patient care: a nationwide survey of residents' perceptions of clinical documentation requirements and patient care. J Grad Med Educ. 2013;5(4):600–604. doi: 10.4300/JGME-D-12-00377.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen MA, Hollenberg JP, Michelen W, Peterson JC, Casalino LP. Patient care outside of office visits: a primary care physician time study. J Gen Intern Med. 2011;26(1):58–63. doi: 10.1007/s11606-010-1494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Leary KJ, Liebovitz DM, Baker DW. How hospitalists spend their time: insights on efficiency and safety. J Hosp Med. 2006;1(2):88–93. doi: 10.1002/jhm.88. [DOI] [PubMed] [Google Scholar]
- 14.Gottschalk A, Flocke SA. Time spent in face-to-face patient care and work outside the examination room. Ann Fam Med. 2005;3(6):488–493. doi: 10.1370/afm.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tipping MD, Forth VE, Magill DB, Englert K, Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med. 2010;5(6):353–359. doi: 10.1002/jhm.647. [DOI] [PubMed] [Google Scholar]
- 16.Cutler DM, McClellan M. Is technological change in medicine worth it. Health Aff (Millwood) 2001;20(5):11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- 17.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5):505–516. doi: 10.1197/jamia.M1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shu K, Boyle D, Spurr C, Horsky J, Heiman H, O'Connor P, et al. Comparison of time spent writing orders on paper with computerized physician order entry. Stud Health Technol Inform. 2001;84(pt 2):1207–1211. [PubMed] [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. EHR incentive programs. 2014. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms/https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms/. Accessed May 27, 2014. [Google Scholar]
- 20.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
- 21.O'Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination: experiences of physician practices. J Gen Intern Med. 2010;25(3):177–185. doi: 10.1007/s11606-009-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radley DC, Wasserman MR, Olsho LE, Shoemaker SJ, Spranca MD, Bradshaw B. Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. J Am Med Inform Assoc. 2013;20(3):470–476. doi: 10.1136/amiajnl-2012-001241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walsh C, Siegler EL, Cheston E, O'Donnell H, Collins S, Stein D, et al. Provider-to-provider electronic communication in the era of meaningful use: a review of the evidence. J Hosp Med. 2013;8(10):589–597. doi: 10.1002/jhm.2082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schnelle JF, Osterweil D, Simmons SF. Improving the quality of nursing home care and medical-record accuracy with direct observational technologies. Gerontologist. 2005;45(5):576–582. doi: 10.1093/geront/45.5.576. [DOI] [PubMed] [Google Scholar]
- 25.Grauer K. Emergency department chart auditing in a family practice residency program. J Fam Pract. 1983;16(1):121–126. [PubMed] [Google Scholar]
- 26.Cusack CM, Hripcsak G, Bloomrosen M, Weaver CA, Wright A, Vawdrey DK, et al. The future state of clinical data capture and documentation: a report from AMIA's 2011 Policy Meeting. J Am Med Inform Assoc. 2013;20(1):134–140. doi: 10.1136/amiajnl-2012-001093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. J Am Med Inform Assoc. 2011;18(2):112–117. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balka E, Tolar M. Everyday ethical dilemmas arising with electronic record use in primary care. Student Health Tech Inform. 2011;169:285–289. [PubMed] [Google Scholar]
- 29.Sheehy AM, Weissburg DJ, Dean SM. The role of copy-and-paste in the hospital electronic health record. JAMA Intern Med. 2014;174(8):1217–1218. doi: 10.1001/jamainternmed.2014.2110. [DOI] [PubMed] [Google Scholar]
- 30.Weis JM, Levy PC. Copy, paste, and cloned notes in electronic health records: prevalence, benefits, risks, and best practice recommendations. Chest. 2014;145(3):632–638. doi: 10.1378/chest.13-0886. [DOI] [PubMed] [Google Scholar]
- 31.Thielke S, Hammond K, Helbig S. Copying and pasting of examinations within the electronic medical record. Int J Med Inform. 2007;76(suppl 1):122–128. doi: 10.1016/j.ijmedinf.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 32.Gu Q, Dillon C, Burt V. Prescription drug use continues to increase: US prescription drug data for 2007–2008. NCHS data brief 2010. http://www.cdc.gov/nchs/data/databriefs/db42.pdf. Accessed May 27, 2014. [PubMed] [Google Scholar]
- 33.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma'Luf N, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc. 1999;6(4):313–321. doi: 10.1136/jamia.1999.00660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schellhase KG, Koepsell TD, Norris TE. Providers' reactions to an automated health maintenance reminder system incorporated into the patient's electronic medical record. J Am Board Fam Pract. 2003;16(4):312–317. doi: 10.3122/jabfm.16.4.312. [DOI] [PubMed] [Google Scholar]
- 35.Beccaro MA, Villanueva R, Knudson KM, Harvey EM, Langle JM, Paul W. Decision Support alerts for medication ordering in a Computerized Provider Order Entry (CPOE) system: a systematic approach to decrease alerts. Appl Clin Inform. 2010;1(3):346–362. doi: 10.4338/ACI-2009-11-RA-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin CT, McKenzie M, Pell J, Caplan L. Health care provider satisfaction with a new electronic progress note format: SOAP vs APSO format. JAMA Intern Med. 2013;173(2):160–162. doi: 10.1001/2013.jamainternmed.474. [DOI] [PubMed] [Google Scholar]


