Abstract
Background
It is important to describe the characteristics of well-being in resident physicians to develop resident wellness initiatives in postgraduate medical education.
Objective
To characterize the predictors of well-being in resident physicians by assessing personal and work-related burnout, work dissatisfaction, nutritional needs while on call, and sleep needs while on call.
Methods
We set up an online survey in 2012 to collect data from current residents at the University of Calgary in Canada. The WHO-Five Well-Being Index, personal and work-related subscales of the Copenhagen Burnout Inventory, questions on work dissatisfaction, as well as sleep and nutrition management needs while on call, were used in the survey. Descriptive statistics, univariate analysis, and linear regression were applied to the data.
Results
The survey response rate was 45% (317 of 706) of eligible residents, with a mean age of 30.9 years (SD = 4.3). Fifty-three percent (168 of 317) of residents had a well-being score of 13 or less, indicating poor mental well-being. There were significant differences between men and women with respect to personal burnout (47.9 versus 54.2, P = .002) and work-related burnout (46.4 versus 50.4, P = .008). The only significant predictors of well-being overall were personal burnout and work dissatisfaction.
Conclusions
Survey results suggest that a high proportion of residents at this institution have low well-being. This study did not find work-related burnout to be a significant predictor of well-being, after adjustment for other variables.
What was known and gap
Studies have highlighted depression and burnout in resident physicians, resulting in an enhanced focus on resident wellness.
What is new
A study of residents found a small majority of respondents had a score indicating poor well-being.
Limitations
Single institution study, response rate, and respondents significantly younger than the overall group, and a survey tool lacking validity evidence all reduce generalizability.
Bottom line
Despite finding low well-being in a significant proportion, the results do not suggest residency-related burnout as a significant predictor of well-being after adjusting for other variables.
Editor's Note: The online version of this article contains measures used in the study, stratified by demographic variables, and themes from open-ended questions pertaining to sleep and nutrition arrangements as well as overall well-being.
Introduction
Resident physicians suffering from burnout often report suboptimal patient care practices, more perceived medical errors, and a need to distance themselves from their patients.1,2 Burnout is defined as a syndrome composed of emotional exhaustion, cynicism, and inefficacy occurring in response to chronic emotional and interpersonal work-related stressors.1,3 In contrast, well-being is a broad term used to describe a holistic sense of confidence, energy, empathy, enjoyment, and purpose. Resident physicians wish to thrive during residency and beyond. Yet, there are aspects of residency that may threaten their well-being. Aspects of residency that have been considered in efforts to reduce burnout include sleep deprivation, nutrition management, and overall work/job satisfaction.
Sleep deprivation may contribute to residents' decreased well-being.4 Individuals with diminished opportunities for sleep tend to have significantly increased rates of procedural complications such as infection, hemorrhage, organ injury, wound failure, and other failed procedures.5 While we know that sleep deprivation can be a problem for residents, the results are mixed with regard to the effect of duty hour restrictions.6,7 Nutritional habits of resident physicians also can impact sleep and well-being. Appropriate workplace nutrition may improve physician cognition, while a high glycemic index from unhealthy food choices may result in lethargy and need for sleep.8,9
Burnout and decreased well-being can also have profound effects on work satisfaction. This is defined as multidimensional psychological responses to an individual's job, which includes cognitive (evaluative), affective (or emotional), and behavioral components.10 Dissatisfaction with work can influence behaviors, including burnout, anxiety, and depression, as well as absenteeism and decisions to resign.11–13 Duty hour restrictions have improved residents' satisfaction with their personal lives but not satisfaction with work.6,14,15 It is important to describe the characteristics of well-being in residents to develop resident wellness initiatives.
We sought to characterize the predictors of well-being in residents by assessing personal and work-related burnout, work dissatisfaction, nutritional needs while on call, sleep needs while on call, along with demographics.
Methods
Measures and Data Collection
Well-Being
An online survey was set up to collect data from residents at the University of Calgary, Alberta, Canada. We used the WHO-Five Well-Being Index (WHO-5) to minimize response burden. While the WHO-5 has never been used in residents, there is validity evidence from other groups.16,17 WHO-5 scores are based on a maximum of 25, and scores below 13 suggest poor mental well-being.16,17
Burnout
The personal burnout and work-related burnout subscales of the Copenhagen Burnout Inventory (CBI) were chosen because they address deficiencies in a previous widely used scale, and they have been used in practicing physicians and residents.18 Higher scores on burnout scales correspond to higher burnout, and possible scores range from 0 to 100.
Work Satisfaction
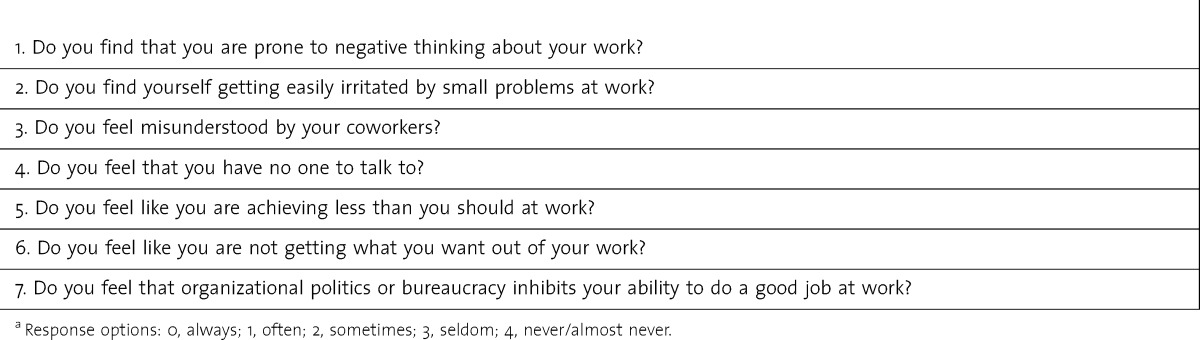
No measure of work dissatisfaction is considered a “gold standard” in residents,13 and we included 7 questions previously found that relate to work dissatisfaction (table 1).19 We used the same Likert scale for the work dissatisfaction questions as the CBI, with higher scores indicating greater satisfaction. Scores range from 0 to 100.
TABLE 1.
Work Dissatisfaction Scalea
Sleep and Nutrition Needs While on Call
As scales to measure nutrition needs of residents do not exist, multiple-choice and open-ended questions were developed to assess sleep, nutritional, and overall wellness needs. Our questionnaire was reviewed by residents with input from the Resident Wellness Committee to ensure that questions were clear and relevant to residents, as well as feasible for use as an online survey with minimal response burden.
Forced choice responses were paired with open-ended questions asking residents to list any barriers contributing to residents' nutritional needs not adequately being met, inadequate sleep arrangements, and to include any other aspects of resident wellness that were of concern.
Residents were recruited by e-mail through the Office of Postgraduate Medical Education. Recruitment took place during 3 weeks with an e-mail that included the online survey link. Residents provided an informed consent online, and were encouraged to contact the researchers if they had concerns. All residents in training at the University of Calgary were eligible to participate.
The study was approved by the University of Calgary Conjoint Health Research Ethics Board.
Analysis
Data were analyzed by using Stata 12.0 (StataCorp) after the final deadline. Age was dichotomized by using the mean age of residents from this sample, and postgraduate years (PGYs) above 4 were collapsed into a PGY-4 category. We analyzed personal burnout, work-related burnout, and work dissatisfaction with respect to 50th percentiles, as scores were based on a 0 to 100 scale.
We computed linear regression models, and used mean scores stratified by sex, age, and PGY. We conducted t tests to determine if any differences existed between the scores and the age and sex variables. Analysis of variance was used to determine if there were differences across the PGY groups. Given the number of t tests needed, a multiple comparison correction was also applied by dividing the α level (α = 0.05). We also conducted a factor analysis using Varimax rotation of the work satisfaction tool to ensure construct validity.
Additionally, we analyzed the open-ended questions pertaining to nutrition, sleep, and overall wellness needs, looking for recurrent themes.20 Data were analyzed manually, and independently, by 2 of the authors (A.K. and J.H.).
Results
We obtained a response rate of 45% (317 of 706 eligible residents). Eleven of the 317 residents had missing data. The instruments showed internal reliability with a Cronbach α value of 0.7 or greater (table 2).21 Our assessment of construct validity for the work dissatisfaction questions was also satisfactory. The factor analysis showed a 1-factor solution, which accounted for 53.3% of the variance by the work satisfaction questions and factor loadings of greater than 0.6 for each of the 7 questions.21
TABLE 2.
Internal Reliability of Measures
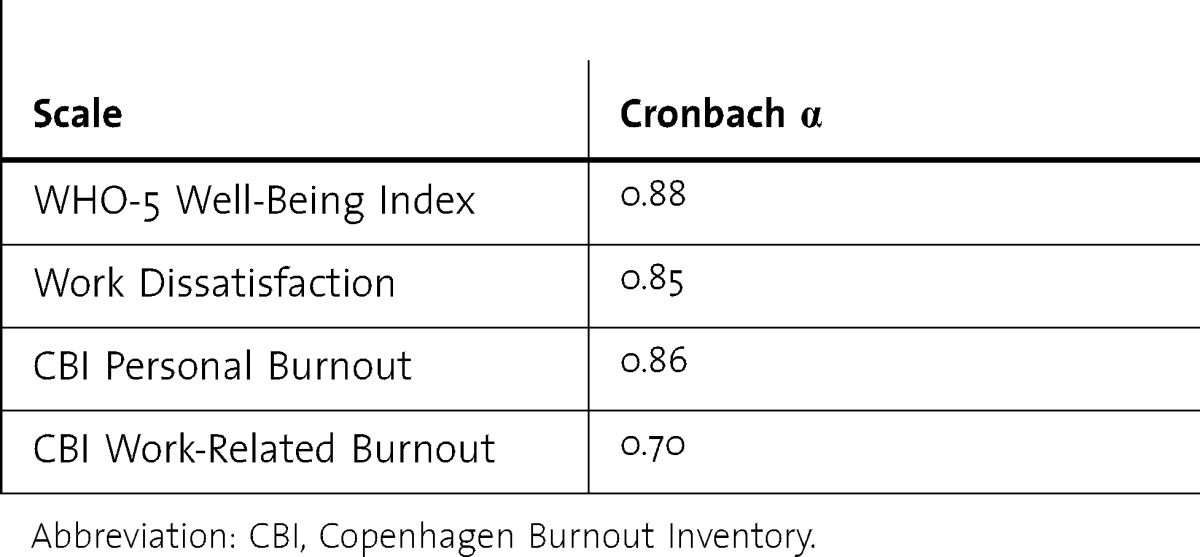
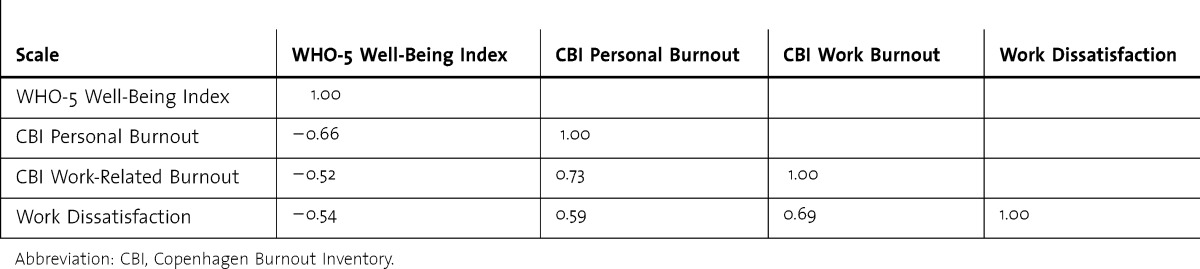
table 3 shows the Pearson correlation coefficients between measures. Personal and work-related burnout, and work dissatisfaction scores, were negatively correlated with well-being. There was a strong correlation between personal and work-related burnout, and work dissatisfaction and work-related burnout.
TABLE 3.
Pearson Correlation Coefficients Between Measures
Our sample consisted of 60.6% women and 39.4% men. When compared to the 706 eligible residents, respondents were significantly younger (30.9 versus 32.4 years, P < .001). There was no significant difference in the proportions of men and women in the overall group and our sample.
Of responding residents, 27% (85 of 317) were in PGY-1, 25% (78 of 317) were in PGY-2, 23% (73 of 317) were in PGY-4, and 25% (81 of 317) were in PGY-4 or higher. The total mean score of well-being was 13.3 (SD = 4.6), and 53% (168 of 317) of respondents had a well-being score of 13 or less, which suggests poor well-being.
In looking at the scores of personal burnout, work-related burnout, and work satisfaction (which were scored by using a 0-to-100 scale), residents showed a substantial level of burnout and work dissatisfaction. The mean score of personal burnout was 51.6 (SD = 17.0), and the mean score of work burnout was 48.9 (SD = 12.7). The mean score of work satisfaction was 37.0 (SD = 17.6).
Univariate Analysis
The scores for well-being, burnout (personal and work-related), and work dissatisfaction, stratified by demographic variables, are shown in the online supplemental material (20.2KB, docx) . There were no significant differences by sex in overall well-being; however, significant differences were detected between men and women with respect to personal burnout (P = .002) and work-related burnout (P = .008). There were no significant differences between those residents younger than 30 years, those 30 years and older, or between residents in their respective PGY of residency.
Thirty-nine percent (122 of 311) of residents reported that their sleeping needs while on call were never, seldom, or only sometimes adequately met, and 81% (250 of 310) reported that their nutritional needs while on call were only never, seldom, or only sometimes adequately met. There were no significant differences between residents whose sleep needs were never, sometimes, or always met. There were, however, significant differences between the residents whose nutrition management needs were never, sometimes, or always met with respect to well-being. Residents whose nutrition management needs were never met had significantly lower well-being scores (12.5) than residents whose nutrition needs were sometimes (14.0, P = .007) or always (14.8, P = .002) met. There also was a significant difference between residents who never and always (55.0 versus 45.6, P = .001) had their nutritional needs met with respect to personal burnout (provided as online supplemental material (20.2KB, docx) ).
Multivariate Analysis (Linear Regression)
Personal burnout and work dissatisfaction were the only significant predictors of well-being after adjusting for sex, age, PGY, work-related burnout, nutrition, and sleep needs as well as interaction variables. The personal burnout (b = –0.14, P < .001) and work dissatisfaction (b = –0.06, P < .001) subscales were significantly negatively correlated with well-being.
Narrative Data
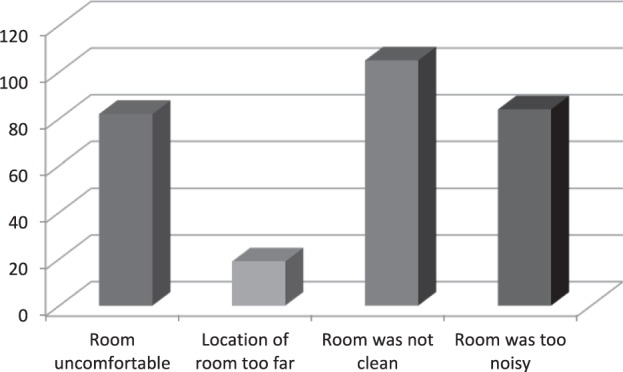
Content analyses of the responses to open-ended questions pertaining to sleep and nutrition and overall well-being are presented in the online supplemental material (20.2KB, docx) . figures 1 and 2 show perceived barriers of sleep arrangement needs and nutritional needs while on call.
FIGURE 1.
Frequency of Residents Reporting Barriers to Sleep Arrangement Needs Being Met While on Call
FIGURE 2.
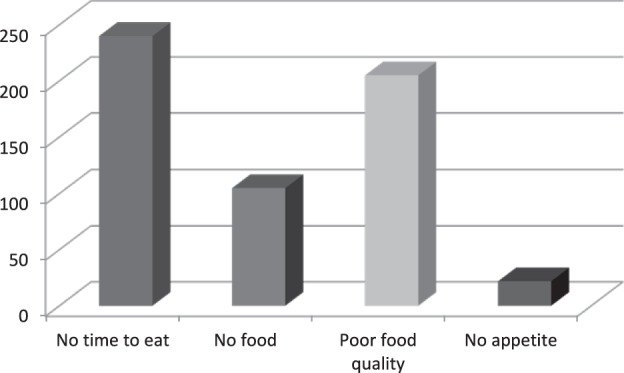
Frequency of Residents Reporting Barriers to Nutritional Needs Being Met While on Call
Discussion
Our findings showed that personal and work-related burnout was higher in female residents compared to male residents, which is consistent with prior research.22–25 Being a female resident, however, may be more difficult given family roles, ability to deal with stress, and cultural factors. In contrast, a study of internal medicine residents demonstrated persistent burnout was more prevalent in male residents.26
Our study did not find work-related burnout to be associated with well-being, after adjustment for other variables. Most studies of resident burnout and well-being have focused on work-related rather than personal factors.27–29 Factors outside of work may contribute to personal burnout and work dissatisfactions, which may lead to overall decreased well-being. In addition, the relationship between these variables is complex and may depend on other residency-related, non–residency-related, and individual factors. Our study suggested that low well-being was prevalent in slightly more than half of our sample. If none of the nonresponders (55% of total) had a similar low sense of well-being, our findings would still suggest burnout in a large proportion of residents at this site. Our findings suggest that personal and work-related burnout scores were more than 10 points higher than those of Canadian academic pediatricians in another study that used the same tool.29
While sleeping arrangement needs were met by more than half of residents, call room conditions, such as noise and cleanliness, are added factors that may play a role in burnout and work dissatisfaction. Well-being and personal burnout varied significantly among residents who had their nutritional needs met and those who did not. We do not know if this correlation is spurious, or whether personal burnout makes a resident more likely to be dissatisfied with other work and life conditions. The analysis of open-ended survey responses suggests that there may be an erosion of boundaries with work-life balance, with work encroaching into personal time. For example, residents reported feeling unable to care for themselves or their family when ill.
Our study has several limitations. The results are derived from a single site, and the sample consisted of significantly younger residents than the group of eligible residents. This suggests sampling bias, as younger residents may be more affected by the stress of new training situations, and may respond differently to threats to well-being. The survey design precluded analysis of whether respondents are representative of the overall population by specialty distribution. Our response rate of 45% also limits generalizability. The survey consisted of questions from several previously used instruments and additional questions on sleep and nutrition; therefore, the instrument lacks validity evidence for this population and setting.
Conclusion
Our findings suggested that a high proportion of residents at a single institution report low well-being. However, we did not find work-related burnout to be a significant predictor of well-being, after adjustment for other variables. Future research should look at evaluating interventions targeting personal burnout, and how this relates to dissatisfaction with training, and to resident well-being.
Supplementary Material
Acknowledgments
The authors would like to thank the University of Calgary Resident Wellness Committee, the University of Calgary Office of Postgraduate Medical Education, The Stadium Keg Restaurant in Calgary, and all study participants.
Footnotes
All authors are at the University of Calgary, Alberta, Canada. Aliya Kassam, PhD, is Assistant Professor, Office of Postgraduate Medical Education, Department of Community Health Sciences; Joan Horton, MD, is Family Physician, Department of Family Medicine; Ilya Shoimer, MD, is Resident Physician, Division of Dermatology, Department of Internal Medicine; and Scott Patten, MD, PhD, is a Professor and Psychiatrist, Departments of Psychiatry & Community Health Science.
Funding: The authors report no external funding sources for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Prins JT, van der Heijden FM, Hoekstra-Weebers JE, Bakker AB, van de Wiel HB, Jacobs B, et al. Burnout, engagement and resident physicians' self-reported errors. Psychol Health Med. 2009;14(6):654–666. doi: 10.1080/13548500903311554. [DOI] [PubMed] [Google Scholar]
- 2.Beckman TJ, Reed DA, Shanafelt TD, West CP. Resident physician well-being and assessments of their knowledge and clinical performance. J Gen Intern Med. 2012;27(3):325–330. doi: 10.1007/s11606-011-1891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eckleberry-Hunt J, Lick D, Boura J, Hunt R, Balasubramaniam M, Mulhem E, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269–277. doi: 10.1097/ACM.0b013e3181938a45. [DOI] [PubMed] [Google Scholar]
- 4.Ripp J, Fallar R, Babyatsky M, David R, Reich L, Korenstein D. Prevalence of resident burnout at the start of training. Teach Learn Med. 2010;22(3):172–175. doi: 10.1080/10401334.2010.488194. [DOI] [PubMed] [Google Scholar]
- 5.Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302(14):1565–1572. doi: 10.1001/jama.2009.1423. [DOI] [PubMed] [Google Scholar]
- 6.Choi D, Dickey J, Wessel K, Girard DE. The impact of the implementation of work hour requirements on residents' career satisfaction, attitudes and emotions. BMC Med Educ. 2006;6:53. doi: 10.1186/1472-6920-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Papp KK, Stoller EP, Sage P, Aikens JE, Owens J, Avidan A, et al. The effects of sleep loss and fatigue on resident-physicians: a multi-institutional, mixed-method study. Acad Med. 2004;79(5):394–406. doi: 10.1097/00001888-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Lemaire JB, Wallace JE, Dinsmore K, Roberts D. Food for thought: an exploratory study of how physicians experience poor workplace nutrition. Nutr J. 2011;10(1):18. doi: 10.1186/1475-2891-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lemaire JB, Wallace JE, Dinsmore K, Lewin AM, Ghali WA, Roberts D. Physician nutrition and cognition during work hours: effect of a nutrition based intervention. BMC Health Serv Res. 2010;10:241. doi: 10.1186/1472-6963-10-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hulin CL, Judge TA. Job attitudes. In: Borman WC, Iigen DR, Klimoski RJ, editors. Handbook of Psychology: Industrial and Organizational Psychology. Vol. 2004. Hoboken, NJ: Wiley; pp. 255–276. [Google Scholar]
- 11.Faragher E, Cass M, Cooper C. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62(2):105–112. doi: 10.1136/oem.2002.006734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rouleau D, Fournier P, Philibert A, Mbengue B, Dumont A. The effects of midwives' job satisfaction on burnout, intention to quit and turnover: a longitudinal study in Senegal. Hum Resour Health. 2012;10(1):9. doi: 10.1186/1478-4491-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Saane N, Sluiter JK, Verbeek JH, Frings-Dresen MH. Reliability and validity of instruments measuring job satisfaction—a systematic review. Occup Med (Lond) 2003;53(3):191–200. doi: 10.1093/occmed/kqg038. [DOI] [PubMed] [Google Scholar]
- 14.Arora V, Meltzer D. Effect of ACGME duty hours on attending physician teaching and satisfaction. Arch Intern Med. 2008;168(11):1226–1228. doi: 10.1001/archinte.168.11.1226. [DOI] [PubMed] [Google Scholar]
- 15.Bailit JL, Weisberger A, Knotek J. Resident job satisfaction and quality of life before and after work hour reform. J Reprod Med. 2005;50(9):649–652. [PubMed] [Google Scholar]
- 16.Henkel V, Mergl R, Kohnen R, Allgaier AK, Moller HJ, Hegerl U. Use of brief depression screening tools in primary care: consideration of heterogeneity in performance in different patient groups. Gen Hosp Psychiatry. 2004;26(3):190–198. doi: 10.1016/j.genhosppsych.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Henkel V, Mergl R, Kohnen R, Maier W, Möller HJ, Hegerl U. Identifying depression in primary care: a comparison of different methods in a prospective cohort study. BMJ. 2003;326(7382):200–201. doi: 10.1136/bmj.326.7382.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kristensen T, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192–207. [Google Scholar]
- 19.Mind Tools Ltd. Burnout self test. 2012. http://www.mindtools.com/pages/article/newTCS_08.htm. Accessed November 25, 2014. [Google Scholar]
- 20.Weber RP. Basic Content Analysis. 2nd ed. Iowa City, IA: Sage; 1990. [Google Scholar]
- 21.Nunnaly J. Psychometric Theory. New York, NY: McGraw-Hill; 1978. [Google Scholar]
- 22.Prins JT, Hoekstra-Weebers JE, Gazendam-Donofrio SM, Dillingh GS, Bakker AB, Huisman M, et al. Burnout and engagement among resident doctors in the Netherlands: a national study. Med Educ. 2010;44(3):236–247. doi: 10.1111/j.1365-2923.2009.03590.x. [DOI] [PubMed] [Google Scholar]
- 23.Prins JT, Gazendam-Donofrio SM, Tubben BJ, van der Heijden FM, van de Wiel HB, Hoekstra-Weebers JE. Burnout in medical residents: a review. Med Educ. 2007;41(8):788–800. doi: 10.1111/j.1365-2923.2007.02797.x. [DOI] [PubMed] [Google Scholar]
- 24.Cohen JS, Leung Y, Fahey M, Hoyt L, Sinha R, Cailler L, et al. The happy docs study: a Canadian Association of Internes and Residents well-being survey examining resident physician health and satisfaction within and outside of residency training in Canada. BMC Res Notes. 2008;1:105. doi: 10.1186/1756-0500-1-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ. 2005;5:21. doi: 10.1186/1472-6920-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell J, Prochazka AV, Yamashita T, Gopal R. Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med. 2010;85(10):1630–1634. doi: 10.1097/ACM.0b013e3181f0c4e7. [DOI] [PubMed] [Google Scholar]
- 27.Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4(2):e004185. doi: 10.1136/bmjopen-2013-004185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lue BH, Chen HJ, Wang CW, Cheng Y, Chen MC. Stress, personal characteristics and burnout among first postgraduate year residents: a nationwide study in Taiwan. Med Teach. 2010;32(5):400–407. doi: 10.3109/01421590903437188. [DOI] [PubMed] [Google Scholar]
- 29.Wright JG, Khetani N, Stephens D. Burnout among faculty physicians in an academic health science centre. Paediatr Child Health. 2011;16(7):409–413. doi: 10.1093/pch/16.7.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


