Abstract
Background
Advanced care directives (ACDs) and end-of-life discussions are important and typically difficult to initiate because of the sensitive nature of the topic and competing clinical priorities. Resident physicians need to have these conversations but often do not in their continuity clinics.
Objective
We implemented a program to (1) increase physician opportunity to discuss end-of-life wishes with their patients, and (2) improve residents' confidence in leading discussions regarding ACDs.
Intervention
A total of 95 residents in an academic outpatient internal medicine resident continuity clinic participated in a formalized curriculum (didactic sessions, simulations, and academic detailing). Clinic workflow alterations prompted the staff to question if patients had an ACD or living will, and then cued residents to discuss these issues with the patients if they did not.
Results
Of the 77% of patients who were asked about ACDs, 74% had no ACD but were interested in discussing this topic. After our intervention, 65% (62 of 95) of our residents reported having at least 1 outpatient discussion with their patients. Residents reported increased confidence directing and discussing advanced care planning with older patients and conducting a family meeting (P < .01).
Conclusions
By delivering a formalized curriculum and creating a clinical environment that supports such discussions, resident physicians had more ACD discussions with their patients and reported increased confidence. When provided information and opportunity, patients consistently expressed interest in talking with their physician about their advanced care wishes.
What was known and gap
Discussing end-of-life care and advanced care directives (ACDs) is important to appropriate care and stewardship of resources.
What is new
A formal curriculum and changes in clinic workflow facilitated residents in an internal medicine clinic to explore end-of-life issues with patients.
Limitations
Single site, single specialty study, lack of assessment of patient response, and an intervention that consisted of multiple components limit assessment of effectiveness.
Bottom line
The curriculum and clinical environment supported end-of-life discussions; patients showed interest in talking about ACDs.
Editor's Note: The online version of this article contains a table of intervention and time estimates, and end-of-life care educational materials.
Introduction
Given the current health care environment, it is increasingly important for patients to discuss options for end-of-life care and advanced care directives (ACDs) with their health care provider. End-of-life discussions are difficult and time-consuming for providers at all levels of training, and are an uncomfortable topic for patients to discuss unless prompted. Research has demonstrated this conversation is best facilitated by a trusted provider,1 and this often is the primary care physician.
Advanced care directive discussions are particularly difficult in an academic medical setting, as residents feel uncomfortable with end-of-life issues, and a structured curriculum to educate residents about this topic is lacking.2 Residents are exposed to these discussions at a greater degree and urgency in the inpatient setting, but it has been shown that outpatient discussions regarding ACD could facilitate better decisions during inpatient hospitalizations.3,4 Residents may find it difficult to assess which patients would benefit from discussions of ACDs, unless they have a current, life-limiting illness. Residents also may perceive that patient satisfaction will be negatively affected by discussions regarding ACDs, yet data show that patient satisfaction in academic primary care general internal medicine practice improves with ACD discussions.5 A focus on older patients, application of communication tools, and development of outcome measures to assess these discussions is imperative.6 In the intensive care unit setting, a structured case-based curriculum did improve confidence in discussing acute end-of-life issues.7 Research found that a simple 1-hour education session for ambulatory care improves completion of ACD paperwork, but data are lacking regarding educational interventions for ambulatory residency training.8 We implemented a program to improve resident physician confidence to lead discussions in the outpatient setting regarding ACD, and to increase patient opportunity to discuss end-of-life care with their physician.
Methods
In 2009, the Medical University of South Carolina initiated a program to improve resident education in geriatric care and quality of life for older adults. The 5-year program, Aging Q3, was funded by a grant from the Donald W. Reynolds Foundation. End-of-life care was 1 of 16 clinical topics chosen.
A working group consisting of clinical faculty, a senior resident, and a palliative care nurse practitioner reviewed the literature on ACDs and end-of-life communication between primary care physicians and patients. We developed an evidence-based teaching curriculum, including didactic training for faculty preceptors, clinic staff, and residents rotating through our university internal medicine clinic. The curriculum used Microsoft PowerPoint presentations, role playing, and point-of-care tools.
Faculty members attended a 1-hour faculty development session that included training on specific topics, and a review of key learning points for residents. Two 1-hour role play sessions focused on discussing ACDs were also offered to all general internal medicine teaching faculty. Certified medical assistants attended a 1-hour didactic session on ACDs and systems/workflow changes. Residents were offered a 1-hour didactic session on conducting a family meeting, as well as a discussion of ACD during a scheduled noon conference, and were given the opportunity to practice scenarios through role play and simulation. Point-of-care tools included a pocket card outlining the 10 steps for leading a family conference and breaking bad news. Attendance was voluntary for all training sessions; lunch was provided at each session to encourage attendance. Attendance at each learning session was tracked manually by the project coordinator. In preparation for the clinic visit, certified medical assistants gave all patients aged 65 years or older a copy of the booklet, “Isn't It Time We Talked,”9 and asked patients if they had an ACD. The patient responses were recorded on the paperwork accompanying the patient throughout the visit, and served to prompt a discussion on ACD during the outpatient encounter. Residents were provided academic detailing on advanced directives by faculty during one-on-one precepting in their continuity clinic.10 This consisted of attending physician's review of South Carolina–specific information regarding ACD and desire for natural death documents with residents. Residents then were encouraged to compute a 4-year mortality risk for their patients and asked to discuss ACD with them.11 Resident participation in individual precepting sessions was tracked on a “check-off” sheet posted in the clinic. We tracked the residents who had participated in the individual precepting detailing.
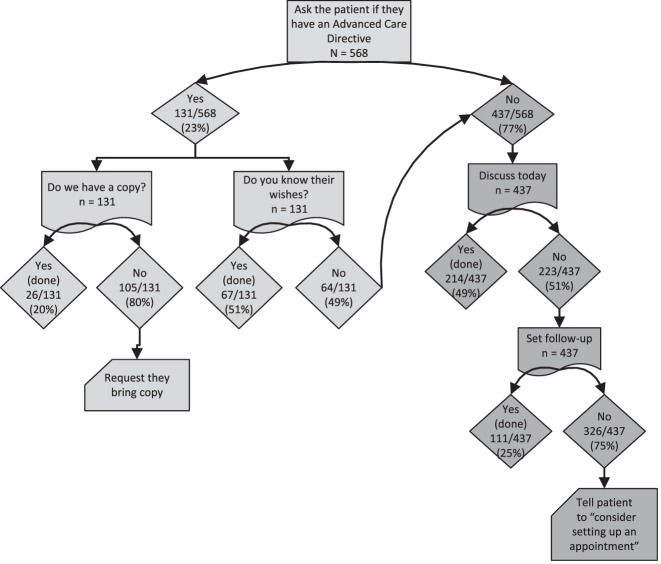
We altered the workflow in our clinic to create the opportunity to discuss ACDs by having medical assistants ask all patients about ACDs, preparing patients for the discussions with written materials, and prompting the physician to have the discussion at the visit. For patients with an ACD, residents were asked to record the patient's current advanced care wishes in the electronic health record by using a template developed by core faculty. For patients without an ACD, residents asked patients if they would like to discuss advanced directives during the appointment. If the patient was not willing to discuss, the patient was asked if he or she preferred to schedule a follow-up appointment for discussion. The resident was prompted to enter results of any discussion into the electronic health record by using a template created by the working group.
Residents completed a pretest and posttest in the 30 days before and after our intervention. The tests were delivered to residents' e-mail via SurveyMonkey and included 5 knowledge questions about end-of-life care issues, and 3 questions asking how confident they felt in discussing ACDs with their patients. Confidence items asked residents to rate on a 4-point Likert-type scale (1, not at all confident, to 4, extremely confident) their confidence in discussing ACDs, communicating bad news, and conducting a family meeting. Knowledge questions included patient scenarios assessing and calculating a patient's risk of 4-year mortality11,12; strengths and limitations of ACDs in medical decision making, including provisions of “Allow Natural Death” orders; and important considerations in conducting a family meeting.
This study was approved by the Medical University of South Carolina Institutional Review Board.
Survey results were analyzed by using the McNemar test to test the difference in correct answers to the knowledge items for matched residents (same residents pre and post), and the Wilcoxon signed rank test was used for the report of confidence items between pretests and posttests. Significance was determined at the .05 level, and SAS version 9.3 (SAS Institute Inc) was used for statistical analysis.
Results
Of the 95 residents included in the intervention, 67 (71%) residents completed the pretest, 72 (76%) completed the posttest, and 58 matched residents completed both the pretest and posttest. There was no significant difference in correct knowledge questions in pretesting and posttesting.
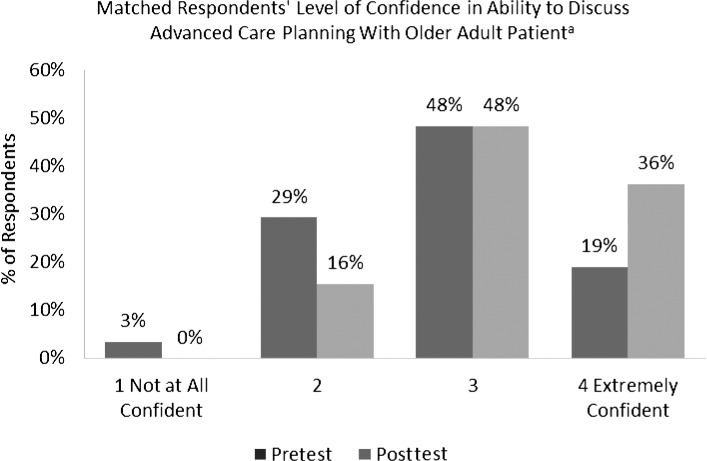
Fifty-seven percent (568 of 998) of clinic patients were asked about ACDs, and 77% reported they had no ACD. Seventy-four percent of patients without ACDs wanted to discuss ACDs with their physician either on that day or during a follow-up appointment. At the conclusion of the program, 65% (62 of 95) of residents had at least 1 discussion about ACDs with a patient in the outpatient setting (figure 1).
FIGURE 1.
Resident Confidence in Discussing Advanced Care Planning With an Older Adult Patient: Comparison of Pretesting and Posttesting
a n = 58, P = .001.
Discussion
Through education, simulation of ACD communication skills, and creation of a focused clinic environment, most residents were able to incorporate ACD communication skills into clinical practice. As compared to preintervention, residents were also more confident discussing ACDs with patients and leading a family meeting. These skills may be taught in undergraduate medical education, but it is difficult to assure continued skill development in residency. More clinical experience with end-of-life scenarios has been associated with an increased self-perceived competence with addressing these issues.13 We believe we created the opportunity in our resident clinic to initiate these discussions, and the overall program led to a greater level of resident confidence in discussing ACDs.
The older adults in our resident clinic were receptive to discussion of ACD. Our change in clinic workflow was effective in creating opportunities for medical assistants to ask patients about ACDs. With adequate training, medical assistants were able to ask about ACDs while minimizing patient visit delays.
The training and workflow changes facilitated patient-resident discussion regarding end-of-life issues, potentially overcoming 1 of the greatest hurdles to initiating these discussions: creating the opportunity for residents to broach this difficult subject with patients. Patients often wanted to discuss these issues, but without prompting during the visit, ACD would likely not have been addressed (figure 2). In busy outpatient clinics, it is important to create an environment where these discussions can occur and are not omitted because of pressing medical issues. Our study included all patients 65 years of age or older, and residents were not required to identify which patients may benefit from a discussion regarding ACD.
FIGURE 2.
Schematic of Patient and Workflow Change in Outpatient Clinic to Facilitate Advanced Care Directive Discussions
We demonstrated a change in resident behavior and an increase in resident confidence in ACD discussions. This was a multicomponent intervention targeting faculty, resident, patient, and medical assistant behaviors. Our ultimate goal was to incorporate as many opportunities to learn the skill and provide clinic workflow changes to “drive the point home” regarding the importance of learning to facilitate effective ACD discussions.
Limitations of this study include the fact that the intervention was limited to a single institution with a small sample size, and that it was not mandatory. The nature and result of the ACD discussions were not assessed, and we do not know how patients reacted to them. We used nonvalidated knowledge questions and cannot be sure how much residents learned during the intervention. Our intervention consisted of multiple components, and it was not possible to determine which of these approaches was most effective. Perhaps it would be helpful to sample future residents to determine which components most aided the implementation of practice and retention of material.
Our intervention has been sustained after the end of the Donald W. Reynolds Foundation funding period. Residents continue to be exposed to this program as part of the geriatric curriculum. This intervention can easily be scaled and replicated in other settings with modest time investment. The time for the intervention included 1 hour each for the faculty and resident lectures, 1 hour and an added 15 minutes per learner for the role play session, an average of 5 minutes for the individual precepting, and another 5 minutes for the clinic assistants to ask patients about ACDs (provided as online supplemental material (390.5KB, doc) ).
Conclusion
A combination of faculty and staff development, resident education, educational materials, brief preceptor “academic detailing,” and clinic workflow changes produced improvements in resident confidence in discussing ACDs with older clinic patients. This multicomponent intervention also increased the documentation of these discussions in the electronic health record: most residents documented at least 1 discussion. The intervention appeared to be welcomed by patients.
Supplementary Material
Acknowledgments
The authors would like to thank working group members Leigh Vaughan, Elisha Brownfield, Mary Adler, Leah Clanton, Amanda Overstreet, Yumin Zhao, and Justin Marsden.
Footnotes
All authors are in the Division of General Internal Medicine and Geriatrics, Medical University of South Carolina. Sarah Leatherman Allen, MD, is Clinical Assistant Professor; Kimberly S. Davis, MD, is Associate Professor; Paul C. Rousseau, MD, is Associate Professor; Patty J. Iverson, MA, is Program Coordinator, Project Director, Donald W. Reynolds Foundation Grant; Patrick D. Mauldin, PhD, is Professor; and William P. Moran, MD, MS, is Professor and Director.
Funding: Funding was provided by a grant from the Donald W. Reynolds Foundation.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Greutmann M, Tobler D, Colman JM, Greutmann-Yantiri M, Librach SL, Kovacs AH. Facilitators of and barriers to advance care planning in adult congenital heart disease. Congenit Heart Dis. 2013;8(4):281–288. doi: 10.1111/chd.12025. [DOI] [PubMed] [Google Scholar]
- 2.Siddiqui MF, Holley JL. Residents' practices and perceptions about do not resuscitate orders and pronouncing death: an opportunity for clinical training. Am J Hosp Palliat Care. 2011;28(2):94–97. doi: 10.1177/1049909110374599. [DOI] [PubMed] [Google Scholar]
- 3.Doll KM, Stine JE, Van Le L, Moore DT, Bae-Jump V, Brewster WR, et al. Outpatient end of life discussions shorten hospital admissions in gynecologic oncology patients. Gynecol Oncol. 2013;130(1):152–155. doi: 10.1016/j.ygyno.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Fischer SM, Sauaia A, Min SJ, Kutner J. Advance directive discussions: lost in translation or lost opportunities. J Palliat Med. 2012;15(1):86–92. doi: 10.1089/jpm.2011.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tierney WM, Dexter PR, Gramelspacher GP, Perkins AJ, Zhou XH, Wolinsky FD. The effect of discussions about advance directives on patients' satisfaction with primary care. J Gen Intern Med. 2001;16(1):32–40. doi: 10.1111/j.1525-1497.2001.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fine E, Reid MC, Shengelia R, Adelman RD. Directly observed patient-physician discussions in palliative and end-of-life care: a systematic review of the literature. J Palliat Med. 2010;13(5):595–603. doi: 10.1089/jpm.2009.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seoane L, Bourgeois DA, Blais CM, Rome RB, Luminais HH, Taylor DE. Teaching palliative care in the intensive care unit: how to break the news. Ochsner J. 2012;12(4):312–317. [PMC free article] [PubMed] [Google Scholar]
- 8.Landry FJ, Kroenke K, Lucas C, Reeder J. Increasing the use of advance directives in medical outpatients. J Gen Intern Med. 1997;12(7):412–415. doi: 10.1046/j.1525-1497.1997.00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Carolinas Center for Hospice and End of Life Care; South Carolina Bar; South Carolina Hospital Association; South Carolina Medical Association. Advance care planning: how to talk about your health care choices. https://www.scmedical.org/uploads/files/AdvanceCarePlanning(1).pdf. Accessed December 2, 2014. [Google Scholar]
- 10.Moran WP, Zapka J, Iverson PJ, Zao Y, Wiley MK, Pride P, et al. Aging Q3: an initiative to improve internal medicine residents' geriatrics knowledge, skills, and clinical performance. Acad Med. 2012;87(5):635–642. doi: 10.1097/ACM.0b013e31824d4a10. [DOI] [PubMed] [Google Scholar]
- 11.Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 12.Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285(21):2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 13.Billings ME, Curtis JR, Engelberg RA. Medicine residents' self-perceived competence in end-of-life care. Acad Med. 2009;84(11):1533–1539. doi: 10.1097/ACM.0b013e3181bbb490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.