Abstract
Introduction
To estimate the incremental cost effectiveness and cost utility of a once weekly or twice weekly resistance training intervention compared with twice weekly balance and tone classes in terms of falls prevented and quality adjusted life years (QALYs) gained.
Methods
Economic evaluation conducted concurrently with a three arm randomised controlled trial including one hundred and fifty-five community dwelling women aged 65 to 75 years, Mini Mental State Examination ≥24, and visual acuity 20/40 or better. Participants received the once weekly resistance training (n=54), the twice weekly resistance training (n=51) or the twice weekly balance and tone (the comparator) classes (n=50) for one year. Measurements included number of falls for each participant, healthcare resource utilization and associated costs over nine months; health status was assessed using the EQ-5D and SF-6D to calculate QALYs.
Results
Based on the point estimates from our base case analysis, we found that both once and twice weekly resistance training was less costly (p<0.05) and more effective than twice weekly balance and tone classes. The incremental QALYs assessed using the SF-6D were 0.003 for both the once and twice weekly resistance training groups, compared with the twice weekly balance and tone classes. The incremental QALYs assessed using the EQ-5D were 0.084 for the once and 0.179 twice weekly resistance training groups, respectively compared with the twice weekly balance and tone classes.
Conclusions
An individually tailored resistance training intervention delivered once or twice weekly provided better value for money for falls prevention than balance and tone classes.
Keywords: falls, cost-effectiveness, cost-utility, economic evaluation, resistance training, older adults
Introduction
Falls and injuries resulting from falls in older adults represent a costly and significant public health burden [1–3]. Falls are the most frequent cause of injury-related healthcare resource utilization, morbidity and mortality among older people [4, 5]. In the United Kingdom, falls result in over £981 million (at 2000 prices; US $1.6 billion at 2008 prices] in annual direct medical expenditures [6].
Progressive resistance training is a component of effective exercise programs for falls prevention in older adults [7, 8]. We previously demonstrated that progressive, high intensity resistance training significantly reduced falls risk score by 57% in older women with low bone mass [9]. Although relative risk reduction is an important step in demonstrating efficacy or effectiveness it is insufficient on its own. Hence, we need to report absolute risk reduction for the intervention compared with the control group and the subsequent number needed to treat to prevent one morbid outcome event such as a fall [10]. Resistance training also has benefits for balance, cognition, body composition, and cardiovascular health [7, 9, 11–14]. Resistance training may save money by preventing healthcare resource use by combating sarcopenia [9]. Consequences of sarcopenia include increased falls risk secondary to impaired strength, balance, and mobility. The incremental cost effectiveness ratio in terms of the cost per fall prevented has been reported for a combined program of resistance training and balance training compared with usual care [15–17]. This home-based intervention, the Otago Exercise Programme, was cost saving for those aged 80 years and older [15].
What is not known is whether there is a threshold dose of resistance training aimed at combating sarcopenia and reducing falls risk in women aged 65–75 years that will reduce total healthcare resource utilization and thus provide the best value for money. Therefore, we designed a concurrent, prospective economic analysis using individual level data on cost and effectiveness outcomes as part of the Brain Power study, a three arm randomized controlled trial [18]. The main outcome results are reported elsewhere [18]. Our primary objective for the economic evaluation was to determine the incremental cost effectiveness and cost utility ratio (cost per fall prevented and cost per quality adjusted life year gained) of once weekly or twice weekly resistance training compared with twice weekly balance and tone classes (comparator). We modeled the comparator program (twice weekly balance and tone classes, the control group activity in the Brain Power trial [18]) on a popular provincial-wide exercise program designed to reduce falls among seniors with low bone mass (the Osteofit program). The twice weekly balance and tone comparator is representative of exercise programs commonly available in the community such as Osteofit, yoga or Tai Chi. We did not use a ‘usual practice’ arm in this analysis because it would not be a reflection of current practice in the community. For communities where such classes are not offered our approach may provide an overly conservative estimate of health benefit.
Materials and methods
Overview of economic evaluation
We used a Canadian healthcare system perspective in our cost effectiveness and cost utility analyses and a nine month time horizon for the economic evaluation. We analyzed the data from the Brain Power trial on an intention to treat basis. The main outcome for our primary (cost effectiveness) analysis was the incremental cost per fall prevented and for our secondary (cost utility) analysis, the incremental cost per quality adjusted life year (QALY) gained. QALYs are defined as the benefit of a health intervention in terms of time in a series of quality-weighted health states, in which the quality weights reflect the desirability of living in the particular health state, typically anchored at “perfect” health (weighted 1.0) to dead (weighted 0.0) [19]. The quality weights spent in each state are multiplied by the time spent in each state. The total number of QALYs for that time period is the sum of all these products.
We previously reported study design, study sample, participant recruitment, randomization, demographics (including weight, height, average waist girth, average hip girth, waist to hip ratio, physiological profile assessment (PPA) and functional comorbidity index questionnaire), methods and main outcome results of the Brain Power trial [18]. Briefly, the study sample included 155 community dwelling women aged 65 to 75 years. For the study sample (n=155), we calculated the required sample size for Power study from predictions of 12-month changes in the Stroop test results base on our previous work [20]. Specifically, we predicted a 6% improvement for the once weekly resistance training and a 12% improvement for the twice weekly resistance training groups. We also estimated a 10% deterioration in the BAT group (i.e., the control group). Cognitive response to exercise differs between the sexes; therefore, our sample consisted solely of women [21]. Participants enrolled in Brain Power had a Mini Mental State Examination (MMSE) score ≥24 (i.e., were cognitively intact) and visual acuity 20/40 or better with or without corrective lenses. Participants excluded: were unable to write and speak English, were partaking in resistance training in the last six months, had a current medical condition for which exercise is contraindicated, had a neurodegenerative disease, were taking cholinesterase inhibitors, being treated currently for depression or on hormone replacement therapy during the previous 12 months. The secondary objective of Brain Power that related to our economic evaluation was to determine whether once weekly resistance training versus twice weekly resistance training significantly reduced falls compared with twice-weekly balance and tone classes. The interventions for the Brain Power study included three participant groups: once weekly resistance training, twice weekly resistance training and the control group, twice weekly balance and tone classes (comparator). The resistance training program used a progressive, high intensity protocol. The balance and tone program consisted of stretching exercises, range-of-motion exercises, basic core-strength exercises including kegels (pelvic floor exercises), balance exercises, and relaxation techniques. All classes were 60 minutes long, with a 10-minute warm-up, 40 minutes of core content, and a 10-minute cool down period.
Costs
We used a questionnaire to track total healthcare resource utilization prospectively for each participant for 9 months of the 12-month study period up. We collected these questionnaires at 3-month time intervals during the 9-month time horizon. The major resource categories were: any visits to healthcare professionals (including general practitioners, specialists, physiotherapists etc); all visits, admissions or procedures carried out in a hospital; and laboratory and diagnostic tests. We calculated the costs of delivering the once weekly resistance training, twice weekly resistance training, and twice weekly balance and tone (comparator group) interventions for nine months. Our base case analysis considered the costs of delivering the program and all healthcare resource use. Our sensitivity analyses included cost of delivering the program and fall related healthcare resource costs only. We excluded research protocol driven costs from our analysis as these do not reflect the cost of implementation in a real world setting. However, the costs of delivering the program included staff time (fitness trainer time), room use, equipment provided as part of the facility and any building overhead costs.
For each component of health resource utilization, we assigned a unit cost. All costs for admission to hospital were based on the fully allocated cost model of a tertiary care hospital, Vancouver General Hospital. For unit costs of healthcare professionals, we based costs on fee for service rates from the British Columbia Medical Services Plan 2009 price list. Unit costs for specialized services such as physiotherapy, chiropractic or naturopathic medicine were taken from the BC Association website for each specialty. We did not have access to the actual cost of each item of health resource utilization and therefore assigned a unit cost specific to the health professional seen, procedure or laboratory test performed. We inflated or deflated (where appropriate) costs to 2008 Canadian dollars using the consumer price index reported by Statistics Canada. Discounting was not relevant given our analytic time horizon was less than 12 months. We used a 2-sample t-test to determine whether there was a statistically significant difference between the total health care resource utilization costs between the twice weekly resistance training group compared with the twice weekly balance and tone group and the once weekly resistance training group, compared with the twice weekly balance and tone group.
Effectiveness outcomes
The assessors were blinded to the participants’ assignments [18]. We used monthly fall diary calendars to track all falls for each participant during the 12-month study period. We report the number of falls per participant group rather than the number of fallers. Given that we collected healthcare costs for 9 months, we calculated the total number of falls prevented at 9 months for once weekly resistance training compared with twice weekly balance and tone classes (comparator) and for the twice weekly resistance training group compared with twice weekly balance and tone classes (comparator). We calculated the total QALYs lost or gained at 6 and 12 months for each of the three participant groups using 1) the SF-36 and 2) the EQ-5D administered at baseline, 6 months and trial completion (12 months). We used linear regression to calculate the incremental QALYs for each participant adjusted for baseline utility score. All statistical analyses were carried out using STATA version 10.0.
Handling missing data
In the Brain Power study, 12.9% of participants had incomplete followup during the 52-week intervention. Missing cost data in particular can introduce substantial bias into the estimation of costs because cost data are often highly skewed [22–25]. We calculated the cost and effectiveness estimates for available cases (dropping observations with missing values), complete case sets, and an imputed data set.
We followed recommendations by Oostenbrink [24, 25] and Briggs [22, 26] for multiple imputation of missing cost and effectiveness data and the ice (Imputation by Chained Equations) program in STATA. For all discrete time points, we used a combination of multiple imputation and bootstrapping to estimate uncertainty caused by missing values. Missing data from each followup period for each participant were determined separately for both cost and effectiveness outcomes. We imputed missing EQ-5D, SF-6D and healthcare resource use values at each time point. For each missing value, we generated five possible values using multiple linear regression. Covariates included age, trial group allocation, baseline utility score, and the weight and value of the missing variable in the preceding period. The final imputed value was the mean value from the five data sets created.
Cost effectiveness analysis
We calculated the incremental cost effectiveness ratio in terms of falls prevented for both once weekly and for twice weekly resistance training compared with twice weekly balance and tone classes (comparator). We used nested imputation and nonparametric bootstrapping to model uncertainty around the estimates for costs and effectiveness. For each of the five cycles, we imputed missing values and bootstrapped the complete dataset. For each cycle of imputation and bootstrapping, we calculated the total healthcare resource use cost, fall related resource use cost and number of falls per participant by group allocation. We averaged results of each cycle of imputation for participants in each of the three participant groups. We evaluated the contribution of each cost item in relation to the total healthcare resource use estimated for each group. We used plots on the cost effectiveness plane based on 5000 iterations of nested imputation/bootstrapping using Fiellers’ method to generate 95% confidence ellipses for the joint distribution of cost and effectiveness outcomes [27].
Cost utility analysis
We also calculated the incremental cost per QALY for both once and twice weekly resistance training compared with balance and tone exercise classes (the comparator). This ratio is another expression of the differences in mean costs and health outcomes between the groups. Given that the health benefit (i.e., QALY) difference between the groups in this case was close to zero, we used 5000 bootstrapped replications of mean difference in cost and mean QALY differences [26]. These data could generate a cost utility acceptability curve to estimate the probability that once weekly resistance training or twice weekly resistance training is considered cost effective compared with twice weekly balance and tone classes over a range of willingness to pay values [28]. However, we did not report cost effectiveness acceptability curves here because both interventions were cost-saving and more effective.
Sensitivity analysis
In our sensitivity analysis we explored uncertainty surrounding the point estimate of the incremental cost-effectiveness ratios using deterministic assumptions and bootstrap methods. For example, we restricted our data to a complete case analysis, thus including only participants for whom we had complete cost and effectiveness data to eliminate uncertainty caused by missing data. We analyzed total healthcare resource utilization and fall related healthcare resource utilization costs separately in our sensitivity analysis. As mentioned above, we applied multiple imputation, bootstrapped confidence interval estimation, adjustment for imbalances in baseline utility and bootstrapped estimates of the incremental cost effectiveness and cost utility ratios.
Results
We present baseline study characteristics in Table 1. A falls histogram revealed one outlier who had a diagnosed hip condition and experienced at least eight falls over the 1-year period of observation. We report the results with and without this outlier. After 9 months there were 30 falls in the once weekly resistance training group, 38 (32 excluding the outlier) in the twice weekly training group, and 38 in the balance and tone group. After 12 months, compared with the balance and tone group the unadjusted incidence rate ratio for the once weekly resistance training group indicated a 27% (IRR: 0.73, CI: 0.44–1.23) nonsignificant reduction in falls and a 12% (IRR: 0.88, CI: 0.67–1.16) nonsignificant reduction in the twice weekly resistance training group.
Table 1.
Characteristics of participants at entry to trial
| Characteristic | Twice weekly balance and tone (comparator) (n=49) | Once weekly resistance training (n=54) | Twice weekly resistance training (n=52) |
|---|---|---|---|
|
| |||
| Mean (SD) or Frequency (%) | Mean (SD) or Frequency (%) | Mean (SD) or Frequency (%) | |
| Age, years | 70.0 (3.3) | 69.5 (0.2) | 69.4 (3.0) |
| Weight, kg | 67.0 (11.5) | 69.2 (16.2) | 72.1 (18.8) |
| Height, cm | 161.0 (6.9) | 160.9 (7.0) | 162.8 (6.5) |
| Hip girth, cm | 102.1 (9.1) | 105.4 (11.6) | 105.2 (13.8) |
| Waist girth, cm | 83.9 (10.1) | 86.8 (14.4) | 88.1 (13.7) |
| Waist to hip ratio | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) |
| PPA score | 0.2 (0.9) | 0.3 (1.0) | 0.2 (1.0) |
| Functional Comorbidity Index score | 2.2 (1.7) | 1.9 (1.7) | 2.3 (1.6) |
| Arthritis | 25 (51) | 21 (39) | 26 (50) |
| Osteoporosis | 14 (29) | 13 (24) | 19 (37) |
| Asthma | 7 (14) | 4 (6) | 6 (12) |
| Chronic Obstructive Pulmonary Disease | 2 (4) | 2 (4) | 1 (2) |
| Angina | 1 (2) | 1 (2) | 0 (0) |
| Congestive heart failure | 2 (4) | 2 (4) | 3 (6) |
| Heart attack | 0 (0) | 0 (0) | 3 (6) |
| Neurological disease | 0 (0) | 0 (0) | 0 (0) |
| Stroke or TIA | 2 (4) | 3 (6) | 1 (2) |
| Peripheral vascular disease | 1 (2) | 2 (4) | 0 (0) |
| Diabetes type I and II | 4 (8) | 2 (4) | 2 (4) |
| Upper gastrointestinal disease | 10 (20) | 15 (28) | 7 (13) |
| Depression | 6 (12) | 1 (2) | 6 (12) |
| Anxiety or panic disorders | 6 (12) | 4 (7) | 2 (4) |
| Visual impairment | 11 (22) | 10 (19) | 19 (37) |
| Hearing impairment | 4 (8) | 3 (6) | 6 (12) |
| Degenerative disc disease (back disease, spinal stenosis or severe chronic back pain) | 4 (8) | 9 (17) | 11 (21) |
| Obesity | 8 (16) | 10 (19) | 7 (13) |
Healthcare use and costs
Complete healthcare resource utilization data were provided by 50 (92%) participants at baseline, 51 (94%) at 6 months and 49 (90%) at 12 months in once weekly resistance training group; 49 (94%) participants at baseline, 50 (96%) at 6 months and 48 (92%) at 12 months in the twice weekly resistance training group; and 45 (91%) participants at baseline, 47 (95%) at 6 months and 45 (92%) at 12 months in the twice weekly balance and tone group. There were no differences in response rates or drop outs among the three participant groups. Further, there were no differences in baseline characteristics among individuals who did or did not have missing data, thus we assumed the data were missing completely at random [23]. Unit costs for healthcare cost items are provided in Table 2. The mean total healthcare costs were significantly lower for the once weekly resistance training and twice weekly resistance training groups compared with twice weekly balance and tone classes (p<0.05) (see Table 3).
Table 2.
Unit costs for each component of resource utilization
| Item | Value 2008 CAD$Ý | Unit | Reference |
|---|---|---|---|
| Cost of delivering twice weekly balance and tone classes | 706.12 | Cost per person year | Study records |
| Cost of delivering once weekly resistance training | 353.06 | Cost per person year | Study records |
| Cost of delivering twice weekly resistance training | 706.12 | Cost per person year | Study records |
| Health care professional visit, mean (standard deviation) | 111 (124) | Cost per visit | 2009 Medical services plan |
| Admissions to hospital | 606 | Cost per day | 2005 Vancouver General Hospital fully allocated cost model* |
| Emergency Department presentations | 39 | Cost per hour | 2005 Vancouver General Hospital fully allocated cost model* |
| Laboratory procedures, mean (standard deviation) | 51 (47) | Cost per procedure | 2009 Medical services plan |
The conversion rate to US dollars (USD) at 2008 purchasing power parity is $1 CAD = $0.77 USD.
Taken from the fully allocated cost model at Vancouver General Hospital
Table 3.
Results of base case analysis
| Twice weekly balance and tone (n=49) | Once weekly resistance training (n=54) | Twice weekly resistance training (n=52) | |
|---|---|---|---|
| Cost of delivering program per person (2008 CAD $¶) | 706 or | 353 | 706 |
| Mean (SD) fall related healthcare resource use cost (2008 CAD $) | 162 [158,165] | 547 [537,557] | 184 [180,188] |
| Mean incremental costs for fall related healthcare resource use (2008 CAD $) | reference | 385[375,388] | 22[12,25] |
| Total healthcare resource use costs for all participants (2008 CAD $) | 43571.23 | 42355.11 | 41408.41 |
| Mean (SD) healthcare resource use cost (2008 CAD $) | 1772 [1635,1909] | 1379* [1270,1488] | 1684* [1590,1778], 1676 [1580,1772] |
| Mean incremental costs for total healthcare resource use (2008 CAD $) | reference | −393 [−365, −421] | −88, [−45, −131] −96 [−55, −137] |
| Total number of falls in 9 months | 38 | 30 | 38, 32 excluding outlier |
| Falls rate per person over 9 months | 0.78 | 0.56 | 0.73, 0.62 |
| Incremental cost per fall prevented based on: | |||
| Total healthcare resource use costsÝ | reference|| | dominates§ | dominates§ |
| Fall related healthcare costs Ý | reference | dominates§ | dominates§ |
| Cost of program delivery Ý | reference | dominates§ | dominates§ |
| Unadjusted QALY mean (SD) based on: | |||
| SF-6D | 0.692 [0.685,0.699] | 0.699 [0.690,0.707] | 0.695 [0.687,0.703] |
| EQ-5D | 0.794 [0.771,0.816] | 0.817 [0.794,0.840] | 0.827 [0.808,0.848] |
| Unadjusted incremental QALY based on: | |||
| SF-6D ý | 0 (reference) | 0.006 [0.005,0.008] | 0.002 [0.001,0.004] |
| EQ-5Dý | 0 (reference) | 0.023 [0.023,0.024] | 0.033 [0.032,0.037] |
| Adjusted incremental QALY based on: | |||
| SF-6D ý | 0 (reference) | 0.003 [0.003,0.004] | 0.003 [0.002,0.004] |
| EQ-5Dý | 0 (reference) | 0.084 [0.084,0.085] | 0.179 [0.177,0.179] |
| Incremental cost per QALY based on: | |||
| SF-6D | reference | dominates§ | dominates§ |
| EQ-5D | reference | dominates§ | dominates§ |
p<0.05
ICER based on total HRU costs, fall related costs and cost of delivering programs
Incremental QALYs are adjusted for the baseline utility using a linear regression model
For these strategies it was not appropriate to calculate an incremental cost effectiveness ratio because the intervention strategy were less costly and more effective than the balance and tone comparator (i.e., the intervention dominates the comparator in each of these cases)
Reference indicates that the balance and tone group is the comparator
The conversion rate to US dollars (USD) at 2008 purchasing power parity is $1 CAD = $0.77 USD.
Health outcomes
Complete data for the EQ-5D were provided at all three time points (baseline, 6 months, one year) for 49 (90%) participants in the once weekly resistance training, 47 (90%) participants in the twice weekly resistance training, and 45 (91%) in the twice weekly balance and tone groups respectively. Complete data for the SF-6D were provided at all three time points by 51 (94%) in the once weekly resistance training, 49 (94%) participants in the twice weekly resistance training and 47 (95%) participants in the twice weekly balance and tone groups respectively. There were no differences in response rates or drop outs between treatment groups. Mean QALYs calculated from the EQ-5D and SF-6D scores are provided in Table 3.
Adverse events and mortality
Details on adverse events have been reported [18]. Fourteen (29.8%) women in the once weekly resistance training group developed musculoskeletal complaints, five (10.9%) in the twice weekly resistance training group, and four (9.5%) in the twice weekly balance and tone group. The one exercise related fall in the twice weekly balance and tone group did not result in healthcare resource utilization.
Adjusting QALYs for baseline utility in each group
The incremental QALYs after 12 months calculated using the EQ-5D and adjusted for baseline EQ-5D levels, were 0.084 for the once weekly resistance training group and 0.179 for the twice weekly resistance training group compared with twice weekly balance and tone classes (Table 3). Variables included in our regression model were baseline utility and group. Of note, an incremental change of 0.03 for either the EQ-5D or the SF-6D indicates a clinically significant change in the participant’s perceived health status [29].
Similarly after controlling for baseline SF-6D levels, the incremental QALY score over 12 months calculated using the SF-6D was 0.003 both for the group receiving once and the twice weekly resistance training group compared with the balance and tone group (Table 3).
Cost effectiveness analysis
Based on the point estimates from our base case cost effectiveness analysis we found that twice weekly resistance training resulted in lower healthcare costs and was more effective than twice weekly balance and tone classes (comparator) when we excluded the outlier, i.e., the twice weekly resistance training “dominates” the comparator. By definition, a new health care intervention ‘dominates’ an existing health care intervention if the new intervention results in lower health resource utilization costs and better health outcomes (i.e., falls prevented or QALYs gained) than the comparator (i.e., usual care/existing health care intervention) [30]. Based on the point estimates from our base case analysis we also found that once weekly resistance training dominated (i.e., less costly and more effective) balance and tone classes.
Cost utility analysis
Based on the point estimates from our base case analysis, we found that twice weekly resistance training was less costly and more effective than twice weekly balance and tone classes including and excluding the outlier. Figure 1a demonstrates that for twice weekly resistance training compared with twice weekly balance and tone, most of the bootstrapped cycles (100% of the 5000 cycles) were represented in the southeast quadrant. Given that all of the bootstrapped cycles yielded incremental cost effectiveness ratios within the southeast quadrant of the cost-effectiveness plane, this indicates that the intervention (twice weekly resistance training) is less costly and more effective than the comparator (twice weekly balance and tone classes). Figure 1b demonstrates that for once weekly resistance training compared with twice weekly balance and tone, most of the bootstrapped cycles (100% of the 5000 cycles) were also represented in the southeast quadrant. Thus, once weekly resistance training results in lower total health care resource utilization costs and is more effective than twice weekly balance and tone classes. Given that our cost utility acceptability curves were in the negative willingness to pay zone, we do not report them here; an incremental cost effectiveness ratio less than zero indicates the intervention is cost saving.
Figure 1.
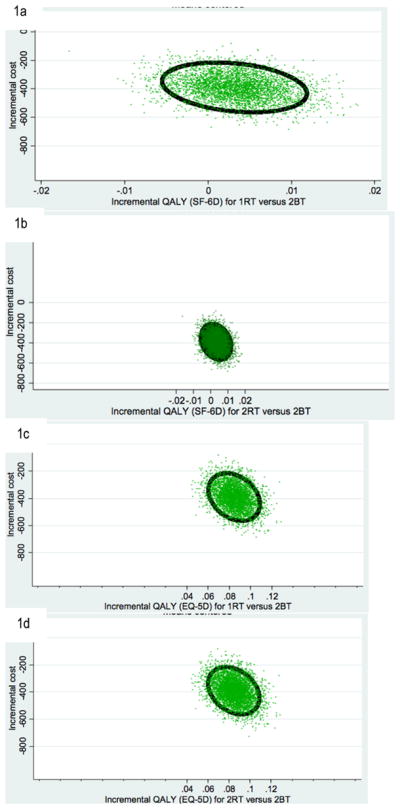
1a) Cost effective plane depicting the 95% confidence ellipses of incremental cost and effectiveness for comparison between twice weekly resistance training (2RT) and twice weekly balance and tone (2BT, comparator); 1b) Cost effective plane depicting the 95% confidence ellipses of incremental cost and effectiveness for comparison between once weekly resistance training (1RT) and twice weekly balance and tone (2BT, comparator). QALY estimates are based on utility scores from the EQ-5D. QALY estimates are based on utility score from the SF-6D for figures 1a and 1b. 1c) Cost effective plane depicting the 95% confidence ellipses of incremental cost and effectiveness for comparison between twice weekly resistance training (2RT) and twice weekly balance and tone (2BT, comparator); 1d) Cost effective plane depicting the 95% confidence ellipses of incremental cost and effectiveness for comparison between once weekly resistance training (1RT) and twice weekly balance and tone (2BT, comparator). QALY estimates are based on utility scores from the EQ-5D for figures 1c and 1d.
Sensitivity analysis
We found similar results for both our complete case analysis and our available case analysis (Table 4). For all scenarios in our sensitivity analysis, QALY estimates from the EQ-5D were in favor of the once weekly resistance training and twice weekly resistance training compared with twice weekly balance and tone classes. There were statistically significant mean cost savings for once weekly resistance training and twice weekly resistance training compared with twice weekly balance and tone classes (comparator) (Table 3). Decision makers have threshold amounts of money that they are willing to pay when comparing effective interventions with already existing community programs. Given that once weekly resistance training and twice weekly resistance training were less costly and more effective twice weekly balance and tone classes (comparator), these two resistance training options are both favorable alternatives to balance and tone classes.
Table 4.
Results of one way sensitivity analyses
| Scenario | Outcomes | Twice weekly balance and tone | Once weekly resistance training | Twice weekly resistance training |
|---|---|---|---|---|
| Available case analysis (n=103) | Mean cost* (2008 CAD $) | 1812 [1637,1987] | 1419 [1267,1571] | 1599 [1496,1701] |
|
| ||||
| This included all individuals who had complete falls and cost data | Mean incremental cost (2008 CAD $) | reference | −393 [−370, −416] | −213 [−141, −286] |
| Number of falls | 24 | 18 | 20 | |
| Cost/fall prevented | reference | dominatesý | dominatesý | |
| Available case analysis (n=99) | Mean cost (2008 CAD $) | 1812 [1637,1987] | 1443 [1289,1599] | 1659 [1552,1766] |
| This included all individuals who had complete SF-6D and cost data | Mean incremental cost (2008 CAD $) | reference | −369 [−348, −388] | −153 [−85, −221] |
| Mean unadjusted QALY | 0.702 [0.694,0.710] | 0.699 [0.689,0.710] | 0.700 [0.689,0.712] | |
| Adjusted QALYÝ | reference | 0.011 [0.000,0.016] | 0.005 [0,0.007] | |
| Available case analysis (n=84) | Mean cost (2008 CAD $) | 1880 [1681,2080] | 1522 [1350,1696] | 1665 [1542,1788] |
| This included all individuals who had complete EQ-5D and cost data | Mean incremental cost (2008 CAD $) | reference | −358 [−331, −384] | −215 [−139, −292] |
| Mean QALY (EQ-5D) | 0.816 [0.785,0.846] | 0.814 [0.777,0.850] | 0.855 [0.835,0.875] | |
| Unadjusted incremental QALY (EQ-5D) | reference | −0.002 [−0.008,0.004] | 0.039 [0.029,0.05] | |
| Adjusted incremental QALY | reference | 0.009 [−0.073,0.079] | 0.018 [0.002,0.036] | |
| Fall related healthcare costs only | Mean (SD) fall related healthcare resource use cost (2008 CAD $) | 162 [158,165] | 547 [537,557] | 184 [180,188] |
| This included only fall related costs that were check by individuals as a falls related event | Mean incremental costs for fall related healthcare resource use (2008 CAD $) | reference | 385 [375,388] | 22 [12,25] |
| Excluding 1 outlier in twice weekly balance and tone group | Mean cost (2008 CAD $) | 1772 [1635,1909] | 1380 [1270,1489] | 1676 [1581,1772] |
| This analysis excluded the outlier who fell 6 times | Mean incremental cost (2008 CAD $) | reference | −392 [−365, −420] | −96 [−54, −137] |
Total health resource utilization mean costs
Adjusted for imbalances in baseline utility between the three treatment arms of the Brain Power randomized controlled trial
For these strategies it was not appropriate to calculate an incremental cost effectiveness ratio because the intervention strategy were less costly and more effective than the balance and tone comparator (i.e., the intervention dominates the comparator in each of these cases)
Discussion
From the Canadian healthcare system perspective, the incremental cost effectiveness ratio per fall prevented indicated that both twice weekly and once weekly resistance training resulted in lower healthcare costs and were more effective than twice weekly balance and tone classes – both once or twice weekly resistance training were cost-effective alternatives. We also noted a statistically significant improvement in the adjusted incremental QALY determined from the EQ-5D in the twice weekly resistance training group compared with the twice weekly balance and tone group at trial completion. As baseline co-morbidities did not differ among groups, this seems an unlikely candidate to explain lower health care costs incurred by the resistance training groups during followup.
Rationale for Balance and Tone Comparator
Of note, the balance and tone comparator is relevant in communities where balance and tone classes such as Osteofit, aimed at reducing falls risk profile rather than falls, among community dwelling older adults are provided. Osteofit has been successful at reducing falls risk profile, but not falls [31]. The balance and tone comparator consisted of stretching, deep breathing techniques and balance exercises that are similar to some yoga, tai chi and Osteofit classes offered in the community. Thus, the balance and tone comparator is relevant at an international context where such programs are offered to older adults in the community. Further, this economic evaluation may provide an overly conservative estimate of the health benefit of the once and twice weekly resistance training classes given the already demonstrated benefits of tai chi for falls prevention [8].
Economic evaluations do not rely on a statistically significant difference in effectiveness and costs between the intervention and the comparator to drive the conclusion [32]. The key factor is the mean point estimate and the location of the greatest proportion of mean point estimates on the cost-effectiveness plane that are generated from the sensitivity analyses. The point estimates are plotted on the four quadrants of the cost-effectiveness plane (e.g. Figure 1) [32]. Exploring the uncertainty in economic evaluations uses the Bayesian perspective rather than a Frequentist perspective. Thus, rather than testing statistical significance, we conducted deterministic sensitivity analyses addressing key assumptions such as falls related versus total health resource utilization costs and we explored uncertainty using bootstrap methods. Figure 1a and 1b demonstrate that for twice or once weekly resistance training compared with twice weekly balance and tone classes, most of the bootstrapped cycles (>80% of the 4000 cycles) were located in the southeast quadrant. This indicates that resistance training is more effective and less costly than the comparator classes.
The QALY is a useful measure of health benefit because it simultaneously captures both quantity and quality of life gains or losses [30]. A key benefit of the QALY is that it enables direct comparison of patient outcomes across diseases and diverse health interventions [30]. This is important in the context of falls prevention research because the incremental cost effectiveness ratio per QALY gained for falls prevention strategies will enable comparison of value for money with other health care interventions among various chronic conditions.
Comparison with other studies
Three falls prevention strategies are cost saving in subgroups of older people. These include: (i) the home based Otago Exercise Programme in people ≥80 years [15–17], (ii) an individually customized multifactorial program in those with four or more of the eight targeted fall risk factors [33], and (iii) a home safety program in individuals who had a previous fall and were recently discharged from hospital [34]. Our economic evaluation results from the Brain Power study demonstrated that both once weekly resistance training and twice weekly resistance training dominated twice weekly balance and tone classes, a substantive finding compared with evaluations of other falls prevention strategies. The studies of falls prevention strategies listed above all used ‘usual care’ option as the comparator. This approach does not reflect that older adults may take exercise classes in the community and therefore these studies may slightly overestimate the health benefits provided by the intervention.
We also emphasize that although studies reporting relative risk reduction of falls and/or fractures provide useful information, authors should report absolute risk reduction for the intervention compared with the control group. Furthermore, the number needed to treat to prevent one morbid outcome event such as a fall is an important comparator [10].
Uncertainty in findings
We aimed to quantify uncertainty first by using multiple imputation for missing values of the EQ-5D, SF-6D and healthcare resource utilization. We then used nonparametric bootstrapping to estimate the uncertainty around the incremental cost effectiveness ratios. From both our probabilistic and selective one way sensitivity analyses, we found that the available case analysis, complete case analysis and subgroup analyses supported the conclusions that both once weekly resistance training and twice weekly resistance training dominates (i.e., more effective and less costly) twice weekly balance and tone classes (comparator). In our sensitivity analysis we used fall related health resource utilization costs rather than total health resource utilization costs which provided the base case analysis. This sensitivity analysis revealed that only the once weekly resistance training intervention was less costly and more effective than the comparator, but this may indicate that the reduced total health resource utilization was as a result of falls avoided.
Time horizon
The time horizon of our study was limited to the 9 months that healthcare resource utilization data were collected during the 12 month Brain Power study. We used falls data at nine months. Previous research demonstrates that resistance training in older adults has long term health benefits that would ideally be captured by a longer time horizon [35].
Limitations of combining an economic evaluation with a randomized controlled trial
Ideally, a gold standard economic evaluation conducted alongside a clinical trial will include the following four characteristics: 1) a comparator commonly used in standard practice, 2) adequate power to assess homogeneity of economic results (e.g., the Brain Power study was not powered to see a reduction in the number of falls), 3) sufficient followup time to assess full health benefit and 4) appropriate time frame to aid in decision making and adoption [36]. Our balance and tone comparator is not a standard ‘do nothing’ alternative. It is however consistent with programs available in the ‘real world’; the balance and tone comparator is relevant in communities where balance and tone classes such as Osteofit, not specifically aimed at fall prevention are provided. Previous research demonstrated that exercises including balance [37], resistance training [9] or balance and resistance training [8, 15] in combination may reduce falls. Consequently, our evaluation may provide an overly conservative estimate of the health benefit of the resistance training classes given that participants may also have experienced a positive health benefit from the balance and tone classes (comparator). Although once and twice weekly resistance training each dominated the twice weekly balance and tone classes, our conservative estimate should not result in any immediate change in decision making as there was no significant reduction in falls as a result of these programs because there may be difficulty in generalizing this study to other populations of men and women, given that this study was restricted to females between 65–75 years. One further limitation is that as our time horizon for this study was 9 months and we did not model life time estimates for costs and health outcomes in this study, we are unable to report long term (e.g. life time) costs and consequences of this intervention. Because we did not include a modeled analysis, we were not able to model a ‘usual care’ arm in the study for communities that may not have balance and tone classes offered.
Strengths
The strength of our study is that we collected information on cost and effectiveness outcomes prospectively and thus minimized recall and response bias. Further, we collected healthcare resource utilization every 3 months to minimize recall bias. Our analytic techniques consisted of multiple imputation and bootstrapping to estimate the uncertainty around the incremental cost effectiveness ratios as a result of the missing values and small sample size. To our knowledge, this is the first economic evaluation to examine the best value for money of two different doses of resistance training compared with commonly available balance and tone classes in the community such as Osteofit.
Conclusions and future directions
Total healthcare resource utilization costs were significantly lower for both once weekly resistance training and twice weekly resistance training compared with twice weekly balance and tone classes. Twice weekly resistance training also resulted in a statistically significant improvement in health related quality of life compared with twice weekly balance and tone classes. Among the three treatment options evaluated in the Brain Power study, both once weekly resistance training and twice weekly resistance training provide better value for money for fall prevention than balance and tone classes.
Acknowledgments
We thank the Brain Power participants. The Vancouver Foundation (BCMSF, Operating Grant to Teresa Liu-Ambrose), the Michael Smith Foundation for Health Research (MSFHR, Establishment Grant to Teresa Liu-Ambrose) and the Centre for Hip Health and Mobility provided funding for this study. Jennifer C. Davis is funded by a Michael Smith Foundation for Health Research Senior Graduate Studentship, a Canadian Institute for Health Research Canada Graduate Scholarship and the Centre for Hip Health and Mobility. Maureen C. Ashe and Teresa Liu-Ambrose are funded by a Michael Smith Foundation for Health Research Scholar Award. Carlo A. Marra is funded by a Canada Research Chair in Pharmaceutical Outcomes and a Michael Smith Foundation for Health Research Scholar Award.
Footnotes
Conflicts of Interest: None declared.
Author Contributions: Jennifer C. Davis was principal investigator for the economic evaluation, was responsible for design, data analysis, data interpretation, writing of manuscript, and is guarantor. Teresa Liu-Ambrose was principal investigator for the Brain Power study and was responsible for study concept and design, acquisition of data, data analysis and data interpretation, and reviewing of the manuscript. M. Clare Robertson, Mehdi Najafzadeh and Carlo A. Marra were responsible for study design, data interpretation and critical review of manuscript. Maureen C. Ashe, and Karim M. Khan were responsible for study design, data acquisition, and critical review of manuscript.
Conflict of Interest Statement
Jennifer C. Davis is funded by a Michael Smith Foundation for Health Research Senior Graduate Studentship, a Canadian Institute for Health Research Canada Graduate Scholarship and the Centre for Hip Health and Mobility. Maureen C. Ashe and Teresa Liu-Ambrose are funded by a Michael Smith Foundation for Health Research Scholar Award. Carlo A. Marra is funded by a Canada Research Chair in Pharmaceutical Outcomes and a Michael Smith Foundation for Health Research Scholar Award.
References
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 2.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 3.Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E. Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int. 2001;12:271–278. doi: 10.1007/s001980170116. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46:M164–170. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 6.Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57:740–744. doi: 10.1136/jech.57.9.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orr R, Raymond J, Fiatarone Singh M. Efficacy of progressive resistance training on balance performance in older adults : a systematic review of randomized controlled trials. Sports Med. 2008;38:317–343. doi: 10.2165/00007256-200838040-00004. [DOI] [PubMed] [Google Scholar]
- 8.Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, Rowe BH. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Liu-Ambrose T, Khan KM, Eng JJ, Janssen PA, Lord SR, McKay HA. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc. 2004;52:657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 7:e1000251. doi: 10.1371/journal.pmed.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrett CJ, Smerdely P. A comparison of community-based resistance exercise and flexibility exercise for seniors. Aust J Physiother. 2002;48:215–219. doi: 10.1016/s0004-9514(14)60226-9. [DOI] [PubMed] [Google Scholar]
- 12.Nelson ME, Fiatarone MA, Morganti CM, Trice I, Greenberg RA, Evans WJ. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA. 1994;272:1909–1914. doi: 10.1001/jama.1994.03520240037038. [DOI] [PubMed] [Google Scholar]
- 13.Orr R, de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Fiatarone-Singh MA. Power training improves balance in healthy older adults. J Gerontol A Biol Sci Med Sci. 2006;61:78–85. doi: 10.1093/gerona/61.1.78. [DOI] [PubMed] [Google Scholar]
- 14.Timonen L, Rantanen T, Ryynanen OP, Taimela S, Timonen TE, Sulkava R. A randomized controlled trial of rehabilitation after hospitalization in frail older women: effects on strength, balance and mobility. Scand J Med Sci Sports. 2002;12:186–192. doi: 10.1034/j.1600-0838.2002.120310.x. [DOI] [PubMed] [Google Scholar]
- 15.Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 1: Randomised controlled trial. BMJ. 2001;322:697–701. doi: 10.1136/bmj.322.7288.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robertson MC, Devlin N, Scuffham P, Gardner MM, Buchner DM, Campbell AJ. Economic evaluation of a community based exercise programme to prevent falls. J Epidemiol Community Health. 2001;55:600–606. doi: 10.1136/jech.55.8.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. 2: Controlled trial in multiple centres. BMJ. 2001;322:701–704. doi: 10.1136/bmj.322.7288.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu-Ambrose T, Nagamatsu LS, Graf P, Beattie BL, Ashe MC, Handy TC. Resistance training and executive functions: a 12-month randomized controlled trial. Arch Intern Med. 2010;170:170–178. doi: 10.1001/archinternmed.2009.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neumann PJ, Goldie SJ, Weinstein MC. Preference-based measures in economic evaluation in health care. Annu Rev Public Health. 2000;21:587–611. doi: 10.1146/annurev.publhealth.21.1.587. [DOI] [PubMed] [Google Scholar]
- 20.Liu-Ambrose T, Donaldson MG, Ahamed Y, Graf P, Cook WL, Close J, Lord SR, Khan KM. Otago home-based strength and balance retraining improves executive functioning in older fallers: a randomized controlled trial. J Am Geriatr Soc. 2008;56:1821–1830. doi: 10.1111/j.1532-5415.2008.01931.x. [DOI] [PubMed] [Google Scholar]
- 21.Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14:125–130. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- 22.Briggs A, Clark T, Wolstenholme J, Clarke P. Missing... presumed at random: cost-analysis of incomplete data. Health Econ. 2003;12:377–392. doi: 10.1002/hec.766. [DOI] [PubMed] [Google Scholar]
- 23.Manca A, Palmer S. Handling missing data in patient-level cost-effectiveness analysis alongside randomised clinical trials. Appl Health Econ Health Policy. 2005;4:65–75. doi: 10.2165/00148365-200504020-00001. [DOI] [PubMed] [Google Scholar]
- 24.Oostenbrink JB, Al MJ. The analysis of incomplete cost data due to dropout. Health Econ. 2005;14:763–776. doi: 10.1002/hec.966. [DOI] [PubMed] [Google Scholar]
- 25.Oostenbrink JB, Al MJ, Rutten-van Molken MP. Methods to analyse cost data of patients who withdraw in a clinical trial setting. Pharmacoeconomics. 2003;21:1103–1112. doi: 10.2165/00019053-200321150-00004. [DOI] [PubMed] [Google Scholar]
- 26.Briggs AH, Gray AM. Handling uncertainty when performing economic evaluation of healthcare interventions. Health Technol Assess. 1999;3:1–134. [PubMed] [Google Scholar]
- 27.Laska EM, Meisner M, Siegel C. Statistical inference for cost-effectiveness ratios. Health Econ. 1997;6:229–242. doi: 10.1002/(sici)1099-1050(199705)6:3<229::aid-hec268>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 28.Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ. 2001;10:779–787. doi: 10.1002/hec.635. [DOI] [PubMed] [Google Scholar]
- 29.Marra CA, Woolcott JC, Kopec JA, Shojania K, Offer R, Brazier JE, Esdaile JM, Anis AH. A comparison of generic, indirect utility measures (the HUI2, HUI3, SF-6D, and the EQ-5D) and disease-specific instruments (the RAQoL and the HAQ) in rheumatoid arthritis. Soc Sci Med. 2005;60:1571–1582. doi: 10.1016/j.socscimed.2004.08.034. [DOI] [PubMed] [Google Scholar]
- 30.Drummond MF, Sculpher MJ, Torrance GW, O’Brien B, Stoddart GL. Methods for the economic evaluation for health care programmes. 3. Oxford University Press; New York. United States of America: 2005. [Google Scholar]
- 31.Carter ND, Khan KM, McKay HA, Petit MA, Waterman C, Heinonen A, Janssen PA, Donaldson MG, Mallinson A, Riddell L, Kruse K, Prior JC, Flicker L. Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ. 2002;167:997–1004. [PMC free article] [PubMed] [Google Scholar]
- 32.Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ. 1999;18:341–364. doi: 10.1016/s0167-6296(98)00039-3. [DOI] [PubMed] [Google Scholar]
- 33.Rizzo JA, Baker DI, McAvay G, Tinetti ME. The cost-effectiveness of a multifactorial targeted prevention program for falls among community elderly persons. Med Care. 1996;34:954–969. doi: 10.1097/00005650-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Salkeld G, Cumming RG, O’Neill E, Thomas M, Szonyi G, Westbury C. The cost effectiveness of a home hazard reduction program to reduce falls among older persons. Aust N Z J Public Health. 2000;24:265–271. doi: 10.1111/j.1467-842x.2000.tb01566.x. [DOI] [PubMed] [Google Scholar]
- 35.McCartney N, Hicks AL, Martin J, Webber CE. Long-term resistance training in the elderly: effects on dynamic strength, exercise capacity, muscle, and bone. J Gerontol A Biol Sci Med Sci. 1995;50:B97–104. doi: 10.1093/gerona/50a.2.b97. [DOI] [PubMed] [Google Scholar]
- 36.Glick HA, Doshi JA, Sonnad SA, Polsky D. Economic Evaluation in Clinical Trials. Oxford University Press; New York USA: 2007. [Google Scholar]
- 37.Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56:2234–2243. doi: 10.1111/j.1532-5415.2008.02014.x. [DOI] [PubMed] [Google Scholar]


