Abstract
Objective
Cardiac rehabilitation (CR) is most often provided in a hospital setting. Home-based models of care have been developed to overcome geographic, among other, barriers in patients at lower-risk. This study assessed whether clinical and geographic factors were related to use of either a hospital- or home-based program.
Methods
Secondary analysis was undertaken within a study of 1268 cardiac outpatients recruited from 97 cardiologist practices where clinical data were extracted. Participants completed a survey including the Duke Activity Status Index. They reported CR utilization in a second survey mailed 9 months later, including CR site and program model. Geographic information systems was used to determine distances and drive times to the CR site attended from patients’ homes.
Results
Overall, 469 (37.0%) participants attended CR at one of 41 programs. Of the 373 (79.5%) participants with complete geographic data, 43 (11.5%) reported attending home-based CR. The sole clinical difference was in activity status, where patients attending hospital-based program had lower activity status (p<.01). There were no differences in model attended based on geographic parameters including urban vs. rural dwelling or drive times (p>.05).
Conclusions
Only one-tenth of outpatients participated in a home-based program, and this allocation was unrelated geographic considerations. While patients should continue to be appropriately-triaged based on clinical risk to ensure safety, more targeted allocation of patients to home-based services may be warranted. This may optimize degree of participation, and potentially patient outcomes.
Keywords: Coronary Artery Disease, Rehabilitation, Utilization, Geography, Health Services Research, Access to Care
Introduction
Cardiovascular diseases are the leading causes of mortality in the world {{5707 WHO 2011;}}. Reducing this burden can be achieved with secondary prevention measures, such as cardiac rehabilitation (CR) {{405 Taylor, R.S. 2004;305 Brown, A. 2003}}. CR is an outpatient disease management program incorporating secondary prevention measures to reduce progression, improve risk factors and prevent the recurrence of cardiac events. Composed of structured exercise, comprehensive education and counseling, CR in Ontario, Canada most-commonly entails two on-site sessions per week for approximately five months in a hospital-based setting {{5279 Stone 2009;}}.
Unfortunately, CR is grossly under-used, with rates of participation around approximately 30% {{5654 Candido 2011;}}. There are a number of reasons for these low rates, and geographic issues are key{{511 Cooper, A.F. 2002; 5328 Leung, Y.W. ;}}. In particular, greater patient distance and drive-times to CR can be a disincentive to participation {{3264 Ades, P.A. 1992; 509 Yates, B.C. 2003; 142 Cardiac Care Network. 2002; 2997 Suaya, J.A. 2007; 3601 De Angelis, C. 2008; 5288 Brual, J. 2010; }}. In order to overcome geographic barriers where there is no site available close to home, home-based CR programs have been developed. While there is no universally-recognized definition of what constitutes a home-based program {{1099 Jolly, K. 2005; }}, these are monitored programs which make similar use of graded exercise tests to develop an individualized exercise prescription, provision of exercise protocols taught by CR personnel to be performed independently, in addition to provision of reading materials on lifestyle changes, all of which is discussed during scheduled telephone calls between allied healthcare providers at CR and patients. Studies comparing the efficacy of home-based versus traditional hospital-based CR show that it is just as effective {{2711 Dalal, H.M. 2007;3322 Jolly, K. 2006;}}, and they may even be more cost-effective {{2710 Taylor, R.S. 2007; }}.
Patients frequently state that travel-time and distance are important factors influencing their decisions to choose home-based over hospital-based CR {{335 Grace, S.L. 2005;}}. Female patients in particular cite transportation barriers to CR {{2942 Grace, S.L. 2009;}}. While home-based CR participants would still be required to attend some sessions on-site for assessment and exercise prescription, the necessity to travel to and from CR two times per week would be mitigated, thus potentially increasing adherence. Other important factors influencing allocation to hospital or home-based services include patient preference (i.e., anxious about exercising unsupervised, perceive they lack motivation), return-to-work (i.e., patients working may wish to have more flexibility afforded by a home program to schedule their exercise), and clinical risk (i.e., higher-risk patients require more supervision for safety). This study aimed to assess to the role of sociodemographic, clinical, and chiefly subjective (i.e., patient perceptions of barriers) and objective (i.e., urban versus rural residence, drive-time and distance to CR) geographic factors in use of home versus hospital-based CR.
Methods
Design and Procedure
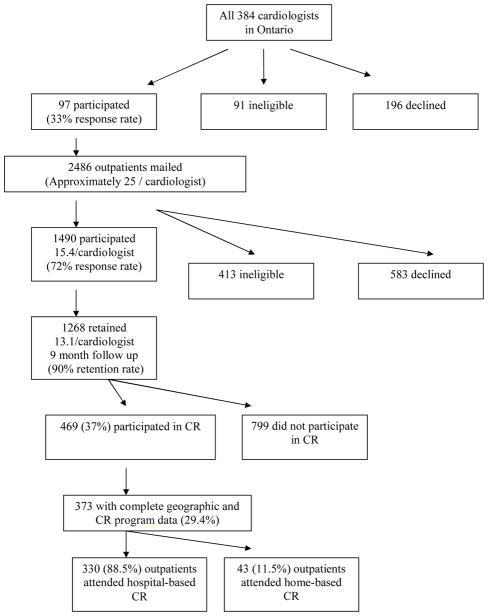
This study presents secondary analysis of a prospective study of cardiac outpatients nested within cardiologists {{2731 Grace, S.L. 2008;}}. Study flow is depicted in Figure 1. With ethics approval from participating institutions, 384 non-pediatric cardiologists from major centres in the Windsor to Ottawa corridor of Ontario were identified through a national physician registry, CMD Online (www.mdselect.com). Of the consenting cardiologists, a consecutive sample of approximately 25 of their coronary artery disease (CAD) outpatients was recruited. Patients were invited by mail to participate; cardiologists were not aware which patients were invited. Written informed consent was obtained from patients who wished to participate. Basic clinical and demographic data were extracted from the outpatient medical charts, and a self-report survey was mailed that assessed sociodemographic characteristics, including geographic factors.
Figure 1.
Participant Flow Diagram and CR Participation
Nine months later participants were mailed a follow-up survey that assessed CR utilization and subjective geographic attitudes. In particular, information regarding CR site of referral and model were assessed. This data was then verified with each CR site. The design of this sub-study is retrospective.
Participants
Cardiologists
Overall, 97 cardiologists consented to participate (33% of all), and 91 were considered ineligible. Reasons for physician ineligibility included: no CAD patients (n=57; 62.6%), no outpatient practice (n=12; 13.2%), incorrect physician address/no longer in practice (n=9; 9.9%), retired (n=2; 2.2%) or other reasons such as physician on sabbatical or maternity leave, left the country, or illness (n=11; 12.1%).
Patients
As shown in Figure 1, 2486 outpatients were mailed a consent form and a survey. CAD patients were eligible to participate in the study, but specifically confirmed acute coronary syndrome (ACS) patients were targeted or those having recently undergone revascularization for ACS. Patient inclusion criteria were eligibility for CR based on Canadian Association of Cardiac Rehabilitation guidelines, and English-language proficiency.
Of these, 1490 consented to participate (72% response rate). At the 9-month follow-up, 1268 (84.9%) outpatients were retained (90% retention rate), with 86 ineligible for participation. Reasons for exclusion included inability to locate the patient (n=37; 43.0%), patient deceased (n=24; 27.9%), orthopedic, neuromuscular, cognitive or vision impairment and non-dysphoric psychiatric comorbidities (n=6; 7.0%), and other reasons such as too ill to participate or moved out of the province/country (n=19; 22.1%). Differences in the sociodemographic and clinical characteristics of retained and unretained participants are reported elsewhere {{2731 Grace, S.L. 2008;}}.
Of retained participants, 469 (37%) enrolled and participated in CR. There were significant differences in the sociodemographic and clinical characteristics of CR participants and non-participants, such that CR participants were more likely to be younger, live in an urban area, be engaged in full-time or part-time work, have graduated from high school, have an annual family income greater than $50,000CAD, have a lower systolic blood pressure, greater functional status, have current or previous myocardial infarction, and no current or previous heart failure or valve repair compared to CR non-participants (ps<.05). For this study, 373 (79.5%) outpatients who attended either hospital or home-based CR and had complete geographic data were selected for analysis.
Measures
Sociodemographic variables were assessed in the initial survey and included marital status, ethnocultural background, family income, level of education attained and work status. Age, sex and clinical data including previous clinical events, disease severity and risk factors were extracted from outpatient charts.
The Duke Activity Status Index (DASI) {{371 Hlatky, M.A. 1989; }}was administered as an indicator of functional capacity. The DASI is a brief 12-item, self-administered survey where participants were questioned about their ability to perform common activities of daily living, such as personal care, ambulation, household tasks, sexual function, and recreational activities, which are each associated with specific metabolic equivalents. This is a valid and commonly-used tool, which correlates highly with peak oxygen uptake, such that higher scores on the DASI correspond with a greater functional capacity.
In the nine-month follow-up survey, respondents were asked whether or not they were referred and enrolled in CR by any healthcare provider (yes/no). Outpatients reporting that they were referred were asked to report the name of the site, and whether they attended hospital-based or home-based CR. This served as the dependent variable.
Respondents were asked to rate the reasons for missing sessions on the Cardiac Rehabilitation Barriers Scale {{5708 Shanmugasegaram, S. 2012;}}. Responses were made on a Likert-type scale from 1 ‘strongly disagree’ to 5 ‘strongly agree’, with higher scores indicating stronger agreement that a particular item was a barrier. The psychometric properties of the scale have been reported15. Five geographically-relevant CR barriers of the 19 administered are reported herein as subjective geographic indicators.
Objective Geographic Indicators
Patient city or town of residence was extracted from medical charts. Urban and rural categories were assigned based on a population size cut-off of 10,000 people, according to Canada’s 2006 Census community profiles (http://www12.statcan.ca/english/census06/). Regions with a population of 10,000 or greater indicated an urban area, while those with a population less than 10,000 were considered rural.
Using Microsoft MapPoint 2006 as the core Geographical Information System (GIS) software, a customized application developed by Healthcor Inc. (Toronto, Canada) was used to generate distances in kilometres and drive-times in minutes. Start-to-destination pairs were generated by geo-coding and linking outpatients’ home postal codes to the postal codes of the specific CR site where each outpatient reported attending. The distances and drive-times were derived using the Ontario Road Network file.
Statistical Analyses
A descriptive analysis of the data was performed to summarize the sociodemographic and clinical characteristics of the participants. Tests of difference by model were then computed using t-tests or chi-square as appropriate. Next, a descriptive examination of the geographic variables was performed. Differences in drive-time and distance, as well as CR barriers by model (hospital-based versus home-based) were compared using t-tests. Analyses were conducted using SPSS 15.0.
Results
Respondent Characteristics
As shown in Figure 1, 469 (37.0%) participants reported attending CR. Complete postal code, CR site and model data was available and verified for 373 (79.5%) participants. Their sociodemographic and clinical characteristics are shown in Table 1.
Table 1.
Characteristics of CR Participants by Model Attended
| Characteristic | Hospital-Based N=330 (89%) |
Home-Based N=43 (11%) |
Total N=373 |
|---|---|---|---|
| SOCIODEMOGRAPHIC | |||
| Age† (mean ± SD) | 65.9±9.9 | 64.7±10.6 | 66.0±10.0 |
| Sex (% female) | 92 (27.9) | 7 (16.3) | 99 (26.5) |
| Living status† (% alone) | 74 (22.5) | 8 (18.6) | 82 (22.0) |
| Marital status† (% married/partnered) | 244 (73.9) | 34 (79.1) | 278 (74.5) |
| Ethnocultural background† (% white) | 285 (86.4) | 38 (88.4) | 323 (86.6) |
| Family income† (% ≥ $50,000CAD) | 168 (55.4) | 25 (59.5) | 193 (55.9) |
| Education† (% ≥ high school) | 195 (60.0) | 28 (65.1) | 223 (60.6) |
| Work status† (% full or part-time) | 114 (34.9) | 19 (44.2) | 133 (35.9) |
| Regional Status (% urban) | 314 (95.2) | 42 (97.7) | 356 (95.4) |
| CLINICAL | |||
| Body Mass Index† (mean ± SD) | 27.5±5.2 | 27.7±4.7 | 27.4±5.5 |
| Smoking Status (% current smoker) | 27 (8.2) | 2 (4.7) | 29 (7.8) |
| Systolic BP, mm Hg (mean ± SD) | 130.0±18.5 | 123.7±19.1 | 129.7±18.6 |
| Diastolic BP, mm Hg (mean ± SD) | 73.9±10.5 | 73.8±9.9 | 74.0±10.3 |
| Total Cholesterol/HDL Ratio | 4.2±1.2 | 4.2±1.3 | 4.2±1.2 |
| HDL, mmol/L (mean ± SD) | 1.1±0.3 | 1.2±0.4 | 1.2±0.4 |
| LDL, mmol/L (mean ± SD) | 2.3±0.9 | 1.9±0.7 | 2.3±0.8 |
| NYHA Class, II–IV (%) | 11 (29.7) | 1 (20.0) | 12 (28.6) |
| CCS angina class, 2–4 (%) | 66 (83.5) | 7 (77.8) | 73 (83.0) |
| Multi-vessel Disease (>1 diseased coronary arteries) | 111 (81.0) | 8 (61.5) | 119 (79.3) |
| Duke Activity Status Index† (mean ± SD) | 39.5±13.8 | 44.6±14.3* | 39.8±14.1 |
| Current or Previous MI | 190 (92.2) | 26 (96.3) | 216 (92.7) |
| Current or Previous PCI | 174 (91.6) | 25 (96.2) | 199 (92.1) |
| Current or Previous CABG | 115 (84.6) | 13 (86.7) | 128 (84.8) |
| Current or Previous HF | 30 (60.0) | 3 (60.0) | 33 (60.0) |
| Current or Previous Valve repair/replacement | 30 (71.4) | 2 (100) | 32 (72.7) |
Note: Percentages take into account missing data for some variables.
p<0.01
CR, cardiac rehabilitation; CAD, Canadian dollars; SD, standard deviation; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; CCS, Canadian Cardiovascular Society; NYHA, New York Heart Association; MI, Myocardial Infarction; PCI, Percutaneous Coronary Intervention; CABG, Coronary Artery Bypass Graft; HF, Heart Failure.
Participants attended CR at 41 (70.6%) of the 58 sites known to exist in the province at the time of data collection. As shown in Table 1, the majority of outpatients attended hospital-based CR.
Factors Related to CR Model Attended
As shown in Table 1, there were no differences in participant sociodemographic characteristics by program model. This included regional status (i.e., urban vs. rural). Of the clinical characteristics, only functional capacity was found to be significantly different by program model attended. Specifically, outpatients who attended home-based CR had a higher mean DASI score indicating greater functional status, than outpatients who attended hospital-based CR.
With regard to geographic factors, overall distances and the drive-times to CR are shown in Table 2. There were no significant differences by model. Finally, CR barriers of geographic relevance assessed included distance (mean±SD=1.8±1.1), transportation (1.7±1.0), cost (1.5±0.9), time (1.8±1.1) and work obligations (2.0±1.3). There were no significant differences in barrier ratings by participants based on CR model attended (ps>.05).
Table 2.
Drive Time and Distance to the Program Attended Based on CR Model
| CR Model | |||||
|---|---|---|---|---|---|
| Hospital-Based CR | Home-Based CR | Total | p | ||
| N (%) | 330 (89%) | 43 (11%) | 373 | ||
| Drive Time, Min | |||||
| Mean ± SD | 16.5±13.8 | 17.7±16.0 | 16.7±14.1 | 0.60 | |
| Median | 12.8 | 11.4 | 12.7 | - | |
| Range | 0.0 – 102.5 | 1.9 – 76.1 | 0.0 – 102.5 | - | |
| Distance, Km | |||||
| Mean ± SD | 11.2±13.7 | 12.9±15.4 | 11.4±6.4 | 0.48 | |
| Median* | 6.4 | 5.6 | 6.4 | - | |
| Range | 0.0 – 97.5 | 0.47 – 66.5 | 0.0 – 97.4 | - | |
CR, cardiac rehabilitation; SD, standard deviation; Min, Minutes; Km, kilometers
the median number of miles for the hospital-based program was 3.98, for the home-based program was 3.48, and overall was 3.98.
Discussion
Home-based CR may be just as effective, while even more cost-efficient, than hospital-based models. Previous research has established that greater distances and drive-times negatively affect CR utilization {{3264 Ades, P.A. 1992; 509 Yates, B.C. 2003; 142 Cardiac Care Network. 2002; 2997 Suaya, J.A. 2007; 3601 De Angelis, C. 2008; 5288 Brual, J. 2010; }}. Where a patient is not considered high-risk for recurrence and a CR site is not available within a reasonable proximity to a patient’s home, allocation to home-based CR would be indicated to ensure equitable access. Results of this study showed that only approximately one-tenth of patients utilized home-based CR Model used was related to clinical, but unrelated to geographic, indicators.
The utilization of home-based CR may be lower than desired. For instance, results of the CHARMS trial revealed patients more often prefer home (57%) to hospital-based CR when given the choice {{2711 Dalal 2007;}}. Moreover, a recent survey of CR programs in Ontario where this study was conducted, revealed that approximately 70% offer home-based programs (Grace, under review), although the patient capacity in these programs is not known. This suggests that more patients could be offered and be satisfied participating in home-based CR. Providing patients the option of program model may increase their engagement in the program and ultimately their long-term management.
To our knowledge, no multifactorial triage algorithms exist to allocate patients to hospital vs. home-based CR models. While these would need to be developed based on many considerations, over and above the patient-centric considerations raise above, clearly clinical risk and safety should be foremost. For patients who are at high-risk of a recurrent event, allocation to hospital-based CR would be indicated. Indeed patients with lower functional status were more likely to be triaged to supervised programs, but no other clinical indicators differentiated model allocation. Determinations regarding patient clinical eligibility for home-based CR cannot be made within this context as a secondary analysis. Replication is warranted, using a prospective design, to ascertain the degree to which clinical factors drive program model allocation decisions in CR programs.
Arguably the second most important factor in model allocation should be geographic access. However, contrary to hypotheses, both subjectively- and objectively-assessed geographic factors were unrelated to model allocation. This could be due to several factors, including: (1) lack of awareness of their availability among referring providers and patients, (2) lack of sufficient home-based CR capacity, and (3) lack of consideration of geographic factors by CR programs when assigning patients to model. It should be investigated how clinical personnel make patient model allocation decisions, and how CR program administrators make decisions regarding capacity for hospital and home-based services.
There are limitations to this study. First, information regarding the mode of transportation that outpatients used to travel to CR such as public transportation, taxi, or carpool was not collected. Car travel was assumed. Second, there were significant differences in the characteristics of those retained in the study versus those unretained, and in the characteristics of the CR participants versus non-participants, which may introduce bias. Third, with respect to the generalizability of findings, complete geographic data was available for only approximately 80% of the sample. Moreover, study results may not be generalizable to other health care systems or regions with different CR funding systems and siting distributions. The jurisdiction where this study was conducted provides coverage for CR through a single-payer system. Fourth, the sample size by program model was unequal which may affect inferential tests. Finally, due to the nature of the study design, causal conclusions cannot be drawn.
In conclusion, home-based CR does appear to be appropriately utilized for patients at higher functional capacity, but not to overcome geographic barriers. The inappropriate selection of CR model may negatively affect patients’ degree of program adherence and completion, and thus patient outcomes. Evidence-based algorithms for CR model allocation based on not only clinical risk stratification, but also geography and patient preferences are needed. Patient outcomes and health system costs should also be considered.
Acknowledgments
We would like to acknowledge the efforts of Alan Ruth from Infoquest Technologies in providing GIS analyses.
Funding: This study was funded by Canadian Institutes of Health Research (CIHR) grant MOP-74431. Ms Brual was supported by a Heart and Stroke Foundation master’s studentship, and Dr Gravely was supported by an Ontario Women’s Health Council/CIHR Institute of Gender and Health doctoral award. Dr Grace was supported by CIHR New Investigator Award MSH-80489.
Footnotes
Conflicts of interest: None declared
Ethical approval: Ethics approval was secured at all participating institutions and at York University, Toronto, Canada.
References
- Ades PA, Waldmann ML, McCann WJ, Weaver SO. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992;152:1033–1035. [PubMed] [Google Scholar]
- Brown A, Taylor R, Noorani H, Stone J, Skidmore B. Exercise-based cardiac rehabilitation programs for coronary artery disease: A systematic clinical and economic review. Technology Report no. 34 2003 [Google Scholar]
- Brual J, Gravely-Witte S, Suskin N, Stewart DE, Macpherson A, Grace SL. Drive time to cardiac rehabilitation: at what point does it affect utilization? Int J Health Geogr. 2010;9:27. doi: 10.1186/1476-072X-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Candido E, Richards JA, Oh P, Suskin N, Arthur HM, Fair T, et al. The relationship between need and capacity for multidisciplinary cardiovascular risk-reduction programs in Ontario. Can J Card. 2011;27:200–207. doi: 10.1016/j.cjca.2011.01.008. [DOI] [PubMed] [Google Scholar]
- Cardiac Care Network. The Ontario cardiac rehabilitation pilot project:report and recommendations. Toronto, ON: Cardiac Care Network; 2002. [Google Scholar]
- Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16:541–552. doi: 10.1191/0269215502cr524oa. [DOI] [PubMed] [Google Scholar]
- Dalal HM, Evans PH, Campbell JL, Taylor RS, Watt A, Read KL, et al. Home-based versus hospital-based rehabilitation after myocardial infarction: a randomized trial with preference arms – Cornwall Heart Attack Rehabilitation Management Study (CHARMS) Int J Cardiol. 2007;119:202–211. doi: 10.1016/j.ijcard.2006.11.018. [DOI] [PubMed] [Google Scholar]
- De Angelis C, Bunker S, Schoo A. Exploring the barriers and enablers to attendance at rural cardiac rehabilitation programs. Aust J Rural Health. 2008;16:137–142. doi: 10.1111/j.1440-1584.2008.00963.x. [DOI] [PubMed] [Google Scholar]
- Grace SL, McDonald J, Fishman D, Caruso V. Patient preferences for home-based versus hospital-based cardiac rehabilitation. J Cardiopulm Rehabil. 2005;25:24–29. doi: 10.1097/00008483-200501000-00006. [DOI] [PubMed] [Google Scholar]
- Grace SL, Gravely-Witte S, Brual J, Suskin N, Higginson L, Alter D, et al. Contribution of patient and physician factors to CR referral: a prospective multi-level study. Nat Clin Pract Cardiovasc Med. 2008;5:653–662. doi: 10.1038/ncpcardio1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace SL, Gravely-Witte S, Kayaniyil S, Brual J, Suskin N, Stewart DE. A multi-site examination of sex differences in cardiac rehabilitation barriers by participation status. J Womens Health. 2009;18:209–216. doi: 10.1089/jwh.2007.0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64:651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- Jolly K, Taylor RS, Lip GY, Stevens A. Home-based cardiac rehabilitation compared with centre-based rehabilitation and usual care: a systematic review and meta-analysis. Int J Cardiol. 2006;111:343–351. doi: 10.1016/j.ijcard.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Leung YW, Brual J, Macpherson A, Grace SL. Geographic issues in cardiac rehabilitation utilization: a narrative review. Health Place. 2010;16:1196–1205. doi: 10.1016/j.healthplace.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polyzotis P, Tan Y, Prior P, Oh P, Fair T, Grace SL. Cardiac rehabilitation services in Ontario: components, models and under-served groups. J Cardiovasc Med. doi: 10.2459/JCM.0b013e32835794c1. (in press) [DOI] [PubMed] [Google Scholar]
- Shanmugasegaram S, Gagliese L, Oh P, Stewart DE, Brister SJ, Chan V. Psychometric validation of the Cardiac Rehabilitation Barriers Scale. Clin Rehab. 2012;26:152–164. doi: 10.1177/0269215511410579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone JA, Arthur HM, Suskin N. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: translating knowledge into action. 3. Winnipeg, MB: Canadian Association of Cardiac Rehabilitation; 2009. Available at http://www.cacr.ca/resources/guidelines.cfm. [Google Scholar]
- Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- Taylor R, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercisebased rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Taylor RS, Watt A, Dalal HM, Evans PH, Campbell JL, Read KL, et al. Home-based cardiac rehabilitation versus hospital-based rehabilitation: a cost effectiveness analysis. Int J Cardiol. 2007;119:196–201. doi: 10.1016/j.ijcard.2006.07.218. [DOI] [PubMed] [Google Scholar]
- WHO, World Heart Federation, World Stroke Organization. Global atlas on cardiovascular disease prevention and control. Policies, strategies and interventions. Geneva: World Health Organization; 2011. Available at http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/index.html. [Google Scholar]
- Yates BC, Braklow-Whitton JL, Agrawal S. Outcomes of cardiac rehabilitation participants and nonparticipants in a rural area. Rehab Nurs. 2003;28:57–63. doi: 10.1002/j.2048-7940.2003.tb02030.x. [DOI] [PubMed] [Google Scholar]