Abstract
The intent of this paper is to discuss the evolving role of the myofascial trigger point (MTrP) in myofascial pain syndrome (MPS) from both a historical and scientific perspective. MTrPs are hard, discrete, palpable nodules in a taut band of skeletal muscle that may be spontaneously painful (i.e. active), or painful only on compression (i.e. latent). MPS is a term used to describe a pain condition which can be acute or, more commonly, chronic and involves the muscle and its surrounding connective tissue (e.g. fascia). According to Travell and Simons, MTrPs are central to the syndrome—but are they necessary? Although the clinical study of muscle pain and MTrPs has proliferated over the past two centuries, the scientific literature often seems disjointed and confusing. Unfortunately, much of the terminology, theories, concepts, and diagnostic criteria are inconsistent, incomplete, or controversial. In order to address these deficiencies, investigators have recently applied clinical, imaging (of skeletal muscle and brain), and biochemical analyses to systematically and objectively study the MTrP and its role in MPS. Data suggest that the soft tissue milieu around the MTrP, neurogenic inflammation, sensitization, and limbic system dysfunction may all play a role in the initiation, amplification, and perpetuation of MPS. The authors will chronicle the advances that have led to the current understanding of MTrP pathophysiology and its relationship to MPS, and review the contributions of clinicians and researchers who have influenced and expanded our contemporary level of clinical knowledge and practice.
Introduction
Myofascial pain is a clinical problem that has generated interest and confusion for decades. The criteria for diagnosis and their relative importance have evolved over time. Myofascial pain is prevalent and a frequent cause of visits to primary care physicians and pain clinics1,2. Few people live without ever having experienced muscle pain as a result of trauma, injury, overuse, or strain. This type of pain frequently resolves in a few weeks with or without medical treatment. In some cases, however, muscle pain persists long after resolution of the injury; it may even refer to other parts of the body, usually contiguous or adjacent rather than remote. This heralds the sensitized state, one of the features of a chronic pain disorder, in which the pain itself is the pathology and requires medical intervention for its resolution.
The term “myofascial” has evolved from the view that both muscle and fascia are likely to be contributors to the symptoms. 3,4 Nomenclature from the past included “fibrositis” which implied inflammation of the connective tissue lining muscle, along with chronic muscle pain. These terms have been replaced by the term “myofascial pain.”
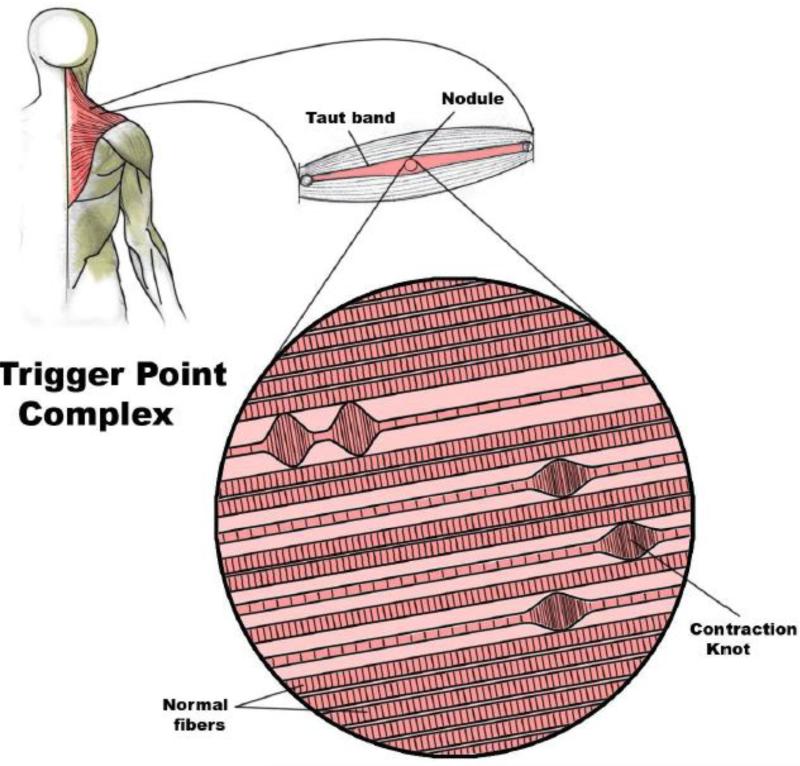
For many clinicians and investigators, the finding of one or more myofascial trigger points (MTrPs) is required to assure the diagnosis of MPS. An MTrP is a discrete, hyperirritable nodule in a taut band of skeletal muscle which is palpable and tender during physical examination (Figure 1). The pain of MPS is associated with, but may not be caused by, an active MTrP. An active MTrP is clinically associated with spontaneous pain in the immediate surrounding tissue and/or to distant sites in specific referred pain patterns. Strong digital pressure on the active MTrP exacerbates the patient's spontaneous pain complaint and mimics the patient's familiar pain experience. MTrPs can also be classified as latent, in which case the MTrP is physically present but not associated with a spontaneous pain complaint. However, pressure on the latent MTrP elicits local pain at the site of the nodule. Both latent and active MTrPs can be associated with muscle dysfunction, muscle weakness, and a limited range of motion. Over the years, the necessity of the physical presence of myofascial trigger points (MTrPs) for the definition of MPS has been hotly debated.
Figure 1.
Schematic of a trigger point complex. A trigger point complex in a taut band of muscle is composed of multiple contraction knots (Adapted from Simons, D.G., Travell, J.G. Myofascial Pain and Dysfunction: The Trigger Point Manual, vol. 1; second ed., and Användare: Chrizz., In: Shah, J. P. and E. A. Gilliams (2008). “Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome.” J Bodyw Mov Ther 12(4): 371-384, used with permission.)
Historical Perspective
Guillaume de Baillous (1538-1616) of France was one of the first to write in detail about muscle pain disorders. In 1816, the British physician Balfour associated “thickenings” and “nodular tumors” in muscle with local and regional muscle pain5. Various other publications contained differing descriptions and terminology, which reflects the slow evolution in the understanding of MTrPs. For example, Froriep in 1843 coined the term “muskelshwiele” (muscle callouses) to describe what he believed was a “callus” of deposited connective tissue in patients with rheumatic disorders6. Subsequently in 1904, Gowers suggested that inflammation of fibrous tissue (i.e., “fibrositis”), created the hard nodules7. However, the term fibrositis became discredited as biopsy data did not substantiate an inflammatory pathology. Schade (1919) later proposed that the nodules, which he called “myogeloses”, were high viscosity muscle colloids8,9. In the mid 1900s, important work was conducted independently by Michael Gutstein in Germany, Michael Kelly in Australia, and J.H. Kellgren in Britain. By injecting hypertonic saline into various anatomical structures such as fascia, tendon, and muscle in healthy volunteers, Kellgren was able to chart zones of referred pain in neighboring and distant tissue. Among others, his work influenced the U.S. physician Janet Travell, whose work on myofascial pain, dysfunction, and trigger points is arguably the most comprehensive to date. Travell and Rinzler coined the term “myofascial trigger point” in the 1950s, reflecting their finding that the nodules can be present and refer pain to both muscle and overlying fascia 10. The two-volume book, Myofascial Pain and Dysfunction: The Trigger Point Manual, which she co-authored with her colleague, David Simons, represents decades of keen observation and study of myofascial pain and MTrPs.
The manual, together with more than 40 papers Travell published on the subject, was and remains instrumental in defining and popularizing the diagnosis and treatment of MPS and MTrPs among the health care community, including physical therapists, allopathic and osteopathic physicians, chiropractors, dentists, pain specialists, massage therapists, and myofascial trigger point therapists. Among the various allopathic medical specialties, physiatrists currently have the most comprehensive working understanding of MTrPs. This is, in part, because physiatrists see MPS and the MTrP as related to muscle and musculoskeletal dysfunction. Simons, acknowledging the lack of attention paid to the muscle has stated, “Muscle is the orphan organ. No medical specialty claims it.” There are signs, however, that Simons’ comments along with Travell's myofascial pain concepts are gaining ground in mainstream medicine.
The current use of the term “MPS” implies a specific condition which is distinguished from other soft tissue pain disorders such as fibromyalgia, tendonitis, or bursitis11. It presents as regional pain, sometimes with referred pain, often accompanied by increased tension and decreased flexibility. It has been reported to coincide with other diseases and syndromes associated with pain, e.g. rheumatic diseases and fibromyalgia12. MPS has also been associated with other pain conditions including radiculopathies, joint dysfunction, disk pathology, tendonitis, craniomandibular dysfunction, migraines, tension type headaches, carpal tunnel syndrome, computer-related disorders, whiplash-associated disorders, spinal dysfunction, pelvic pain and other urologic syndromes, post-herpetic neuralgia, and complex regional pain syndrome12.
MPS has generally, but not universally, been characterized by a physical finding, the MTrP, and a symptom cluster that lacked demonstrable pathology and attracted little research attention until recently. Unlike MPS, fibromyalgia is a widespread and symmetrically-distributed pain condition associated with sleep and mood disturbances. By comparison, the pain of MPS is usually local or regional, distributed in a limited number of select quadrants of the body, and has traditionally been thought to present independently of mood or sleep abnormalities. Interestingly, recent studies indicate that MPS is associated with both mood and sleep disruptions28. However, the definition and pathogenesis of MPS is still not fully understood, and disagreement persists about whether MPS is a disease or process, rather than a syndrome.
A Contemporary Conundrum
Although the MTrP is a common physical finding, it is often an overlooked component of non-articular musculoskeletal pain because its pathophysiology is not fully understood. Besides the use of palpation, there are currently no accepted criteria (e.g., biomarkers, electrodiagnostic testing, imaging, etc.) for identifying or quantitatively describing MTrPs. In addition, diagnostic criteria are imprecise, and the full impact of MPS on life activity and function is not fully understood. To complicate this issue further, MTrPs are associated clinically with a variety of medical conditions including those of metabolic, visceral, endocrine, infectious, and psychological origin13, and are prevalent across a wide range of musculoskeletal disorders. If the MTrP is frequently associated with other musculoskeletal pain syndromes, it would make this finding non-specific—if it is not, it would make the MTrP specific for MPS.
Numerous clinicians over the past few centuries, from various countries and specialties, have encountered and described hard tender nodules in muscle. They have attempted to explain their etiology, tissue properties, and relationship to MPS. However, most investigations were hampered by a lack of objective diagnostic techniques that could record more than simply their presence or absence. As a result, theories of the MTrP pathogenesis, pathophysiology, and contribution to the diagnosis of MPS have been speculative.
As previously mentioned, MTrPs are found as discrete nodules within a taut band of skeletal muscle that may be spontaneously painful or painful only upon palpation. Although muscle pain displays unique clinical characteristics compared to cutaneous and neuropathic pain, the nature of the symptoms are highly dependent upon the individual's perception of its characteristic qualities (e.g., boring, aching, sharp, etc.), intensity, distribution, and duration. The way in which individuals report their symptoms presents a challenge for standardization and validation if these are to be used as diagnostic criteria, outcome measures of improvement, and/or in clinical trials. Characteristics like the quality of the pain, its distribution, and whether it radiates, have never been required for the diagnosis of MPS.
Some investigators are reluctant to diagnose MPS without a palpable nodule and instead rely exclusively on self-reports. MTrPs are central to the process, but are they necessary? MTrPs are commonly found in asymptomatic individuals. These latent MTrPs are nodules with the same physical characteristics as active MTrPs; however, palpation is required to elicit pain. In addition, some nodules are not tender to palpation (non-tender nodules) and may be found proximal to or remote from sites of pain. Although the term “MPS” is commonly used and generally accepted, it does not resolve the clinical dilemma of soft tissue pain in which the palpable nodule is non-tender or no nodule is palpable (and is not explained by radiculopathy, muscle strain, etc.).
In Travell and Simons’ MTrP-centered model of myofascial pain, the diagnostic criteria and relevant clinical findings can only be studied descriptively, using patient-reported outcomes. Moreover, measurements are obtained via dichotomous data (e.g., presence or absence of pain; presence or absence of MTrP) or nominal data (i.e., no nodule vs. non-painful nodule vs. latent MTrP vs. active MTrP). Since there is a bias toward objective findings, the sine qua non for this syndrome is the spontaneously painful nodule (i.e., active MTrP). Unfortunately, the role of the nodule in this process has not been determined. It remains unknown whether the nodule is an associated finding, whether it is a causal or pathogenic element in MPS, and whether or not its disappearance is essential for effective treatment.
In a survey conducted in 2000, the vast majority of American Pain Society members believed MPS to be a distinct clinical entity, characterized by the finding of MTrPs14. A growing number of pain clinics are utilizing Travell's pioneering techniques for the evaluation and treatment of muscle pain disorders. Nevertheless, the lack of consistent nomenclature, universally accepted diagnostic criteria, objective assessments, and conclusive biopsy findings has led to much controversy and generally poor acceptance by mainstream medicine.
The Role of Muscle
Travell and Simons methodically developed a working model based primarily on muscle anatomy and function, which evolved over years of observation and empirical testing. They consistently applied a descriptive approach and used the physical findings of painful nodules in taut muscle bands, along with the nature and distribution of pain, to establish the diagnosis. Their keen observational skills were also used to record natural history and treatment response as a way of further understanding mechanisms. Their model has proven to be extraordinarily useful to both clinicians and those suffering with pain by helping to identify the active MTrP.
By applying the clinical criteria developed by Travell and Simons, the diagnosis of myofascial pain has historically relied heavily on the clinical history and a careful physical examination of the soft tissue by a trained clinician. Recent published findings suggest the local milieu, as well as the nature of the tissue and whether its classification as pliable, stiff, homogeneous, or nodular may be important for evaluation and treatment response15,16. The contribution of the physical findings of the adjacent muscle is often not considered important; rather, it is only the presence and status of the MTrP. Accordingly, diagnosis of MPS has been tissue specific and anatomically based on palpation of the skeletal muscle for MTrPs. Upon examination, reproduction and/or exacerbation of the patients’ spontaneous pain complaint by firm palpation of a hard, tender nodule is classically defined as an active MTrP 17. Upon palpation, latent MTrPs show similar physical characteristics as active MTrPs but are painful only when palpated. Both active and latent MTrPs are responsible for muscle stiffness, dysfunction, and restricted range of motion, as well as autonomic dysfunction, though to a lesser degree for latent MTrPs 9,18.
There have been several theories, including Simons’ own work evolving from his Trigger Point Manual 17, published in 1983, which imply that MTrP development requires muscle overload and overuse. While Simons developed these theories by primarily working with a rabbit model, various researchers have supported his work since then with human studies9.
The Cinderella hypothesis 19 provides a possible explanation for the role of muscle in MTrP development. This hypothesis describes how musculoskeletal disorder symptoms may arise from muscle recruitment patterns during sub-maximal level exertions with moderate or low physical load. These types of exertions are typically utilized by occupational groups such as office workers, musicians, and dentists, in which myalgia and MTrPs have been commonly reported20. According to Henneman's size principle, smaller type I muscle fibers are recruited first and de-recruited last during static muscle exertions. As a result, these “Cinderella” fibers are continuously activated and metabolically overloaded, in contrast to larger motor muscle fibers that do not work as hard and spend less time being activated. This property makes the “Cinderella” fibers more susceptible to muscle damage and calcium dysregulation, key factors in the formation of MTrPs16. A study by Treaster et al. supports the Cinderella Hypothesis by demonstrating that low-level, continuous muscle contractions in office workers during 30 minutes of typing induced formation of MTrPs20.
MTrPs can also develop as a result of muscle overuse in cervical and postural muscles during the performance of low-intensity activities of daily living and sedentary work20,21. An intriguing possible mechanism involves sustained low-level muscle contractions routinely used in tasks requiring precision and postural stability of the cervical spine and shoulder. As a result of sustained low-level contractions, a decrease in intramuscular perfusion has been postulated. Thus, it is conceivable that ischemia, hypoxia, and insufficient ATP synthesis in type I motor unit fibers may occur and are responsible for increasing acidity, Ca2+ accumulation, and subsequent sarcomere contracture. This increased, sustained sarcomere contracture may lead to decreased intramuscular perfusion, increased ischemia, and hypoxia, a vicious cycle that may possibly lead to the development of MTrPs. As a result, several sensitizing substances may be released, leading to local and referred pain in addition to muscle tenderness, which are clinical hallmarks of MPS.
The Role of MTrPs
There exists a spectrum of physical findings and symptoms involving the nodule and surrounding soft tissue. From this perspective, the aim should be to characterize and measure the symptoms and physical findings associated with MPS and MTrPs more quantitatively and objectively using cardinal or non-dichotomous data. This will help investigators to elucidate the pathogenesis and pathophysiology of MPS, and develop better outcome measures for use in clinical treatment trials. Although the specific pathophysiological basis of MTrP development and symptomatology is unknown, several promising lines of scientific study (i.e., biochemical, tissue imaging, and somatosensory testing) as well as a recent systematic and comprehensive evaluative approach (including measures of range of motion; strength; and self-reports of pain, fatigue, mood, and health status) have revealed objective abnormalities15,16,22-28.
The current gold standard for the diagnosis of MPS is the physical examination as described in The Trigger Point Manual: 1) palpation of a taut band; 2) identification of an exquisitely tender nodule (MTrP) in the taut band; and 3) reproduction of the patient's symptomatic pain with sustained pressure. However, accurate diagnosis depends upon the examiner's clinical acumen, experience, index of suspicion, training, and palpation skills. Although there is no consensus regarding the physical findings associated with MPS, the clinical finding of a hard, palpable nodule identified as an active MTrP is generally accepted. While considered the “gold standard,” digital palpation has several limitations. For instance, it lacks adequate sensitivity and specificity. It is sometimes difficult to classify the pain as spontaneous. For example, an individual may have no pain at rest, but as soon as there is movement, pain begins. These limitations make it difficult to assess treatment efficacy, enable objective study of the natural history of MTrPs, and identify the presence of deep MTrPs.
Furthermore, Tough et al. reported that although many research papers on myofascial pain referenced The Trigger Point Manual for diagnostic criteria (57 out of 93 in their cohort), they were used correctly by only 12 of them29. In fact, in clinical practice, there are a variety of ways that patients presenting with a regional pain complaint (and suspected of having MPS) may be evaluated and treated depending upon the location of pain, physical findings, and results of palpation. Accordingly, beyond measuring the subjective intensity and duration of pain, the assessment of clinical outcomes is, by necessity, evolving.
One of the most important characteristics found in clinical examination that confirms the presence of an active MTrP is the local twitch response (LTR). Strumming or snapping the taut band in a direction perpendicular to muscle fibers produces a quick contraction in the muscle fibers of the taut band. The origin of the LTR is not yet fully understood, though this response may be due to altered sensory spinal processing resulting from sensitized peripheral mechanical nociceptors18.
Electromyographic studies have revealed spontaneous electrical activity (SEA) generated at MTrP loci that was not seen in surrounding tissue30. Originally attributed to dysfunctional muscle spindles, the excess electrical activity was later identified as an increase in miniature endplate potentials and excessive acetylcholine (ACh) release30. However, there is disagreement in electromyography and physiology literature on the significance of abnormal motor endplate potentials and “endplate noise.” According to Simons, investigators who lack training in examining muscles for MTrPs may misinterpret a MTrP's abnormal “endplate noise” as a normal finding31,32. Although electromyography has been used in research studies to confirm the presence of MTrPs, in clinical practice there is no advantage to using electromyography33.
The diagnosis of MPS associated with MTrPs remains controversial, especially in the medical profession, despite the methodological improvements that have been made since the first inter-rater reliability study was performed in 199234. Unfortunately, recent studies still suffer from lack of rater blinding, inadequate statistical analysis of the results, and inadequate description of the study findings35.
Other researchers emphasize the “neighborhood” of the MTrP (i.e., surrounding fascia) in order to explain the symptom complex and physical findings associated with MPS. Specifically, Stecco focuses on three anatomical layers: the deep fascia, the layer of loose connective tissue (which houses the highest concentration of hyaluronic acid), and the layer of epimysium below it. An important molecule in this system is hyaluronic acid (HA), an anionic, non-sulfated glycosaminoglycan distributed widely throughout various tissues, and one of the chief components of the extracellular matrix. Normally, HA functions as a lubricant that helps muscle fibers glide between each other without friction. However, Stecco theorizes that as a result of muscle overuse or traumatic injury, the sliding layers start to produce immense amounts of HA, which then aggregate into supermolecular structures, changing both its configuration, viscoelasticity, and viscosity. Due to its increased viscosity, HA can no longer function as an effective lubricant, which increases resistance in the sliding layers and leads to densification of fascia, or abnormal sliding in muscle fibers. Interference with sliding can impact range of motion and cause difficulty with movement, including quality of movement and stiffness. In addition, under abnormal conditions, the friction results in increased neural hyperstimulation (irritation), which then hypersensitizes mechanoreceptors and nociceptors embedded within densified fascia. This hypersensitization correlates with a patient's experience of pain, allodynia, paresthesia, abnormal proprioception, and altered movement. The fact that very few objective, repeatable studies have been conducted to elucidate these concepts demonstrates the constraints of our knowledge regarding the pathophysiology of MPS and our ability to measure what is relevant to the pathogenesis and pathophysiology of the MTrP. Further research is needed to determine not only the role of the MTrP, but also its surrounding area36,37.
Quinter and Cohen38 also disfavor the MTrP-driven hypotheses regarding MPS, arguing that circular reasoning has led to the construct of the MTrP. They suggest that viewing muscle and MTrPs as the primary source of MPS detracts from the possibility of non-muscular explanations for MPS, in which MTrPs arise secondary to an underlying condition. Since the clinical characteristics of MPS are indistinguishable from peripheral neural pain, Quinter and Cohen hypothesize that a more likely explanation for the cause of MPS involves sensitization of the nervi nervorum. They suggest that the phenomenon of the MTrP, which is a critical component of MPS, is better understood as a region of secondary hyperalgesia of peripheral nerve origin, based on anatomy and physiology. Butler supported this notion, suggesting that ectopic impulse generation or abnormal impulse-generating sites and their accompanying sensitization processes in peripheral and cutaneous sensory nerves warrant reconsideration of MTrP hypotheses38.
Although MPS is commonly thought to involve only a local muscular phenomenon of a measurably stiffer, tender nodule, the intriguing results from these studies suggest that MPS is actually a complex form of neuro-muscular dysfunction associated with functional deficits and broader symptomatology. It consists of soft-tissue and sensory abnormalities involving both the peripheral and central nervous systems. In addition, data suggest that neurogenic inflammation, wide dynamic range neurons, and limbic system structures likely play pivotal roles in muscle sensitization, pain chronification, somato-visceral interactions, and the objective physical findings of allodynia, hyperalgesia, and referred pain patterns16,39,40.
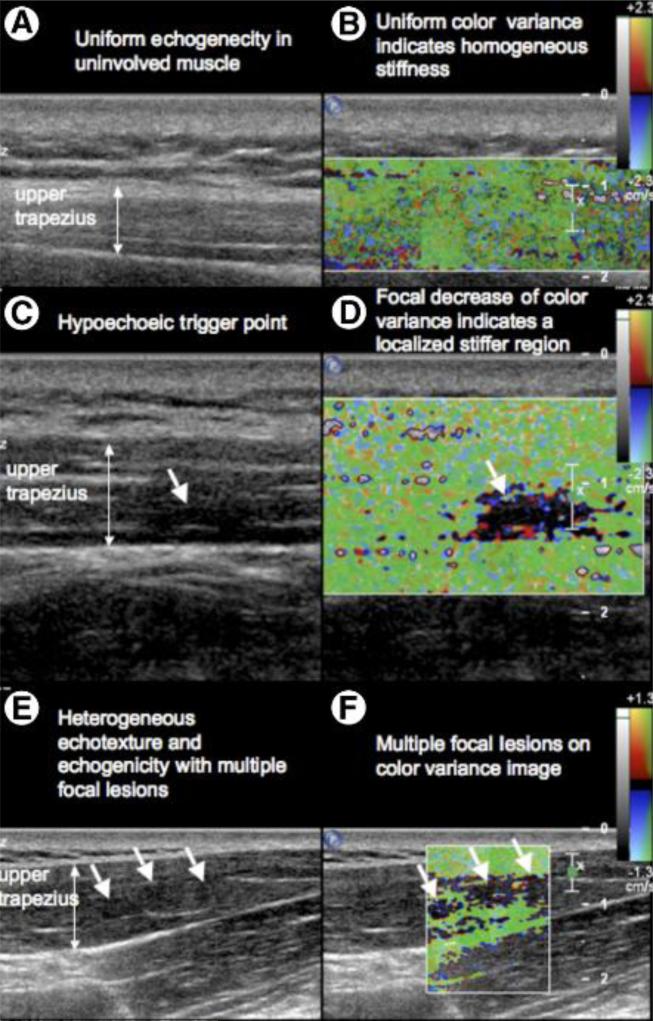
Using ultrasound imaging and elastography, Sikdar et al. demonstrated for the first time that there are abnormalities in the milieu of the muscle containing palpable MTrPs. They found nodular regions of hypoechogenicity on sonography (Figure 2)15. To investigate the mechanical properties of the muscle, an external vibration source was utilized to vibrate the muscle while imaging the distribution of vibration amplitude. This study demonstrated that MTrPs have diminished vibration amplitude on external vibration that is consistent with local regions of increased mechanical stiffness15. These images can be used to document the MTrP and track it over time to assess treatment response. Sikdar et al. have developed a number of methods for quantifying the images to better characterize the muscle milieu surrounding MTrPs. Their findings show that MTrPs are not necessarily associated with isolated nodular lesions, but active MTrPs are associated with substantial heterogeneity in the milieu of the muscle. In many cases, a number of lesions are visualized in close proximity. Quantification of the area of these lesions can distinguish between active and latent MTrPs and normal uninvolved muscle with high sensitivity and specificity41. Mechanical properties of the muscle containing MTrPs were quantitatively assessed by tracking the speed of an externally induced vibration as it propagates through tissue. This method is known as shear wave elastography. Using shear wave elastography, affected muscle in subjects with active MTrPs has been shown to be stiffer compared to palpably normal muscle42. Furthermore, the echogenicity and echotexture associated with active MTrPs can be quantified using image analysis methods such as entropy filtering, and provides a further source of image contrast and a method to differentiate between active MTrPs, latent MTrPs, and normal tissue43. Active MTrPs more often are localized near the distal fascial border of the muscle and have an irregular shape. These shapes can be characterized in 3D to reveal the complex heterogeneous nature of the muscle milieu. This lends further evidence towards an understanding of this phenomenon not just as an isolated abnormality, but rather a more pervasive process that impacts the neighborhood of the muscle and fascia. Color Doppler and spectral Doppler imaging have revealed that the neighborhood of MTrPs shows evidence of vascular remodeling that is especially pronounced in patients with acute neck pain44.
Figure 2.
Simultaneous 2D gray-scale and color variance imaging. (A and B) Normal upper trapezius muscle. The normal muscle appears isoechoic and has uniform color variance (TIS=0). (C and D) Muscle with a palpable MTrP. A hypoechoic region and a well-defined focal decrease of color variance indicating a localized stiffer region is visible (TIS=1). (E and F) Muscle with a palpable MTrP. Multiple hypoechoic regions and multiple focal nodules are visible (TIS=2). Abbreviation: TIS, tissue imaging score. (In: Sikdar S, Shah JP, Gebreab T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. Nov 2009;90(11):1829-1838, used with permission).
These findings open options for future clinical research studies that could focus on identifying the mechanisms responsible for the etiology, amplification, and perpetuation of MPS. The development of successful treatment approaches depends upon identifying and targeting the underlying mechanisms of pain and dysfunction and addressing the perpetuating factors that maintain this common pain syndrome. Accordingly, researchers have explored the dynamic interaction between the nervous system and measurable variables such as sensitizing substances found in the local milieu of active MTrPs16, the unique cortical activation observed in MPS27, and the poor functional levels associated with MPS28.
The Role of Pain: Peripheral and Central Sensitization
Until recently, researchers have largely relied upon Simons’ Integrated Trigger Point Hypothesis, introduced in 1999, to explain the role of peripheral sensitization. According to the hypothesis, the presence of an abnormal endplate activity augments the series of events leading to MTrP development. As hypothesized by Simons, during abnormal endplate activity, high levels of ACh are released, which travel down the sarcoplasmic reticulum and open calcium channels. When calcium binds to troponin on the muscle fibers, the muscle fibers contract. In order to release the contraction, ATP is needed to cause the conformational change of the muscle fibers and actively pump calcium back into the sarcoplasmic reticulum. Thus, a lack of ATP perpetuates the sustained contracture near an abnormal endplate. This leads to increased metabolic demands, compressed capillary circulation (which reduces blood flow, forming local hypoxic conditions), and a polarized membrane potential9. The increased demand for and reduced supply of ATP forms the energy crisis, which may evoke the release of neuroreactive substances and metabolic byproducts (i.e., bradykinin (BK), substance P (SP), serotonin (5-HT)) that could sensitize peripheral nociceptors45. While Simons’ hypothesis explains how sensitizing neuroreactive substances are responsible for the pain associated with active MTrPs and is the most credible theory to date, it remains conjectural. Remarkably, key tenets of Simons’ Integrated Trigger Point Hypothesis overlap with the self-sustaining cycle suggested by the Cinderella Hypothesis.
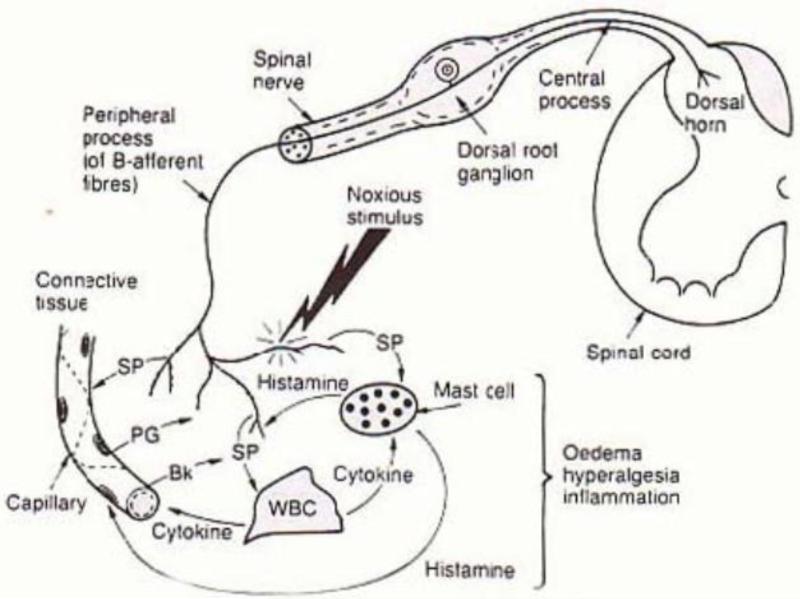
Stimulated by Simons’ work, investigators have sought to provide objective evidence underlying the role of peripheral and central sensitization by using various lines of study, including histological, neurophysiological, biochemical, and somatosensory. For example, Shah et al. hypothesize that local tissue injury (with concomitant elevation of various inflammatory mediators, catecholamines, neurogenic peptides, and cytokines) leads to sensitization of the nociceptor terminal (i.e., peripheral sensitization). In addition, small-fiber, unmyelinated afferents have been found to exhibit retrograde, neurosecretory properties similar to sympathetic fibers, involving a process known as neurogenic inflammation (Figure 3). Therefore, in the presence of persistent nociceptive bombardment (e.g., from an active MTrP), the dorsal root ganglion will release SP and calcitonin gene-related peptide (CGRP) antidromically into the peripheral tissue. The peripheral secretion of these substances can lead to a cascade of events, including the degranulation of local mast cells, local vasodilation, plasma extravasation, and the development of a sensitizing biochemical mixture, which may underlie the clinical findings of active MTrPs46. This process of neurogenic inflammation leads to the enhanced release of endogenous substances, such as BK, 5-HT, norepinephrine, nerve growth factor, and adenosine. The release of these substances will lead to local allodynia and hyperalgesia, and exacerbate local tissue tenderness, causing an active MTrP to become even more painful and tender. The continual bombardment of primary afferent activity over time can lead to abnormal function and structural changes in the dorsal root ganglia and dorsal horn neurons. This is known as central sensitization, and clinical manifestations include allodynia, hyperalgesia, temporal summation of pain47, and expansion of the receptive field of pain16.
Figure 3.
Neurogenic inflammation. In the presence of persistent nociceptive bombardment, the dorsal root ganglion will release substance P and CGRP (not shown) antidromically into the peripheral tissue. The peripheral secretion of these substances can lead to a cascade of events, including the degranulation of local mast cells, local vasodilation, plasma extravasation and the development of a sensitizing biochemical soup. This process of neurogenic inflammation leads to the enhanced release of endogenous substances, such as bradykinin, serotonin, norepinephrine, nerve growth factor, and adenosine. (In: Everett, T., Dennis M., Ricketts E,. eds. Physiotherapy in mental health : a practical approach. Oxford UK: Butterworth/Heinemann; 1995: 102-126, used with permission).
There is a biochemical basis to explain the development of peripheral and central sensitization in muscle pain. Continuous activation of muscle nociceptors leads to the co-release of L-glutamate and SP at the pre-synaptic terminals of the dorsal horn. This leads to maximal opening of calcium-permeable ion channels, which hyperexcites nociceptive neurons and causes apoptosis of inhibitory interneurons24. Consequently, a persistent noxious barrage from the periphery can create long-lasting alterations in the central nervous system. Metabolic and gene induction changes, such as cyclo-oxygenase 2 (COX-2) induction in dorsal horn neurons, are maximal at several hours after an initial noxious stimulation, and bolster functional changes after peripheral tissue injury48.
Sensitization of primary afferents is responsible for the transition from normal to aberrant pain perception in the central nervous system that outlasts the noxious peripheral stimulus. A possible explanation for expanded referral pain patterns is increased synaptic efficiency through activation of previously silent (ineffective) synapses at the dorsal horn. This concept of opening previously ineffective connections was demonstrated in a rat myositis model. Experimentally-induced inflammation unmasked receptive fields remote from the original receptive field, indicating that dorsal horn connectivity expanded beyond the original neurons involved in nociceptive transmission49. In this study, nociceptive input resulted in central hyper-excitability and this finding helps to explain referred pain patterns common to MPS.
Central sensitization may also facilitate additional responses from other receptive fields as a result of convergent somatic and visceral input at the dorsal horn50 via wide dynamic range (WDR) neurons. Furthermore, afferent fibers have the ability to sprout new spinal terminals that broaden synaptic contacts at the dorsal horn and may also contribute to expanded pain receptive fields51. This change in functional connectivity may occur within a few hours, even before metabolic and genetic alterations occur in dorsal horn neurons52. After activating WDR neurons, afferent input from active MTrPs then ascends the spinothalamic tract to reach higher brain centers. In addition to activating the thalamus, muscle afferent input preferentially activates the limbic system (i.e., the anterior cingulate gyrus, insula, and amygdala), which plays a critical role in modulating muscle pain and the emotional or affective component of persistent pain53. Increased activity in the limbic system leads to greater fear, anxiety, and stress. Furthermore, Niddam et al. demonstrated increased limbic system (i.e., anterior insula) activity in patients with upper trapezius MPS27.
Sensitization Without Pain
Latent MTrPs are not associated with spontaneous pain; however, they cause local and possibly referred pain upon deep palpation. This begs questions of their underlying pathophysiology and connectivity to the central nervous system. Do latent MTrPs play a role in central sensitization? How is it possible for these lesions to refer pain to distant locations? Two assumptions must be made to explain the mechanism of latent MTrPs. First, these latent MTrPs send nociceptive, sub-threshold signals to the dorsal horn of the spinal cord. This would effectively sensitize the central nervous system without the perception of pain, as is characteristic of latent MTrPs. Second, ineffective synapses exist within the dorsal horn. In this way, nociceptors from muscle containing the MTrP have connections to dorsal horn neurons, innervating remote muscle regions54.
Sub-threshold potentials and ineffective synapses could serve to explain the sensory phenomenon of latent MTrPs. Taken together, it could be hypothesized that the characteristics of latent MTrPs occur through a series of events. Although latent MTrPs are not spontaneously painful, they send excitatory, sub-threshold potentials that sensitize the dorsal horn. Sensitization of the dorsal horn opens previously ineffective synapses to distant muscle sites. As a result of sensitization, palpation of the latent MTrP induces pain locally and to distant sites (i.e., referred pain) upon the opening of previously ineffective synapses. Thereby, following muscle palpation, pain is experienced at the site of the palpated latent MTrP and in distant, seemingly unrelated muscle.
Human studies have shown that central sensitization can occur without the experience of acute pain. Intramuscular injection of nerve growth factor (NGF) results in allodynia and hyperalgesia, both manifestations of sensitization55. Further, rat studies demonstrated that NGF injections activate an increased proportion of muscle nociceptors. In concordance with this finding was the presence of excitatory sub-threshold potentials56,57. The thalamus and limbic system are critically involved in the subjective experience of pain. Since sub-threshold potentials provide nociceptive input without subsequent action potentials into higher brain centers, there is no perception of pain.
The Evolving Concept of Pain Perception
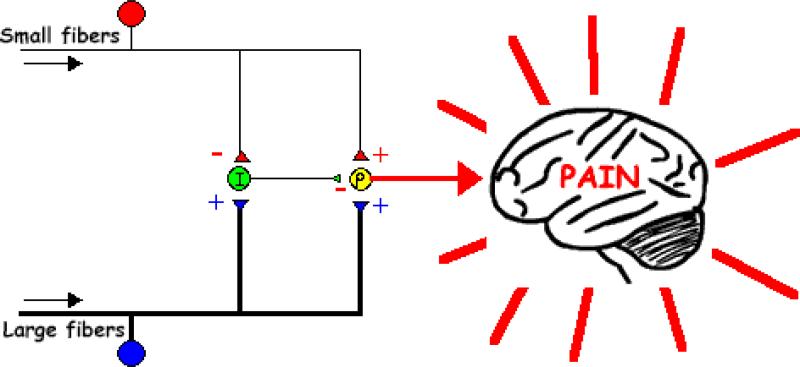
Simons’ “energy crisis” hypothesis and later his Integrated Hypothesis considered the local milieu of the MTrP, taut band, endogenous muscle contracture, and presence of sensitizing substances to explain local muscle tenderness and pain associated with active MTrPs. However, these hypotheses did not consider the prevailing theories of pain processing such as the Gate Control Theory of Pain by Melzack and Wall58 even though Simons and Travell were familiar with them. The Gate Control Theory was a breakthrough concept in pain research because it suggested that the pain experience was a dynamic one, where afferent nociceptive signaling could be modified and influenced by neurons in the CNS acting as inhibitory or excitatory gates. According to the theory, large, myelinated Aβ sensory afferents synapse on inhibitory interneurons located primarily in the substantia gelatinosa of lamina II in the dorsal horn. Specifically, activation of these sensory afferents can inhibit the activation of second-order neurons that receive input from the smaller nociceptor fibers (Figure 4). In addition, supraspinal inputs can also modulate pain perception.
Figure 4.
Gate Control Theory. Pain stimulation activates small nerve fibers. As a result, the fibers send input to the neurons to block the inhibitory interneuron (I), which is now unable to block the output of the projection neuron (P) that connects with the brain. Since the excitatory gate is open, pain is perceived. Non-painful stimulation activates large nerve fibers primarily. As a result, the projection neuron (P) and inhibitory interneuron (I) is activated. However, because the inhibitory interneuron blocks the signal in the projection neuron (P) that connects to the brain, the excitatory gate is closed, and no pain is perceived. Without any stimulation, neither large nor small nerve fibers are activated. The inhibitory interneuron (I) blocks the signal in the projection neuron (P) that connects to the brain. The excitatory gate is closed and no pain is perceived. (Accessed from https://faculty.washington.edu/chudler/pain.html).
These advances in understanding the pathophysiology of chronic pain had implications for MPS. Travell and Simons were well aware of the mechanistic aspects of the Gate Control Theory of Pain, as well as some of the implications with respect to central sensitization and gene regulation. However, the integration of this theory and their clinical observations did not occur until newer theories of pain perception and modulation were described. These involved gene regulation, receptor expression, and depolarization thresholds. In particular, more recent findings and data suggest that other processes such as neurogenic inflammation, sensitization of wide dynamic range neurons, and limbic system dysfunction may play a role in the initiation, amplification, and perpetuation of MPS.
Another important concept that Simons and Travell did not consider in their theories was the dynamic balance between supraspinal descending facilitation and inhibition, and its influence on pain perception. The relative amount of descending facilitation versus inhibition modulates the perception of pain from a normal to an aberrant state. The rostral ventral medulla (RVM) is a critical relay area between the periaqueductal gray and the spinal cord which functions in the descending pain control system. The RVM contains a population of ON cells and OFF cells, which can either increase or decrease the level of pain, respectively. It does so through projections that modulate activity in the dorsal horn. Following initial tissue injury, the ON cells serve a useful and protective purpose designed to prevent further damage. Under ordinary circumstances, tissue healing would lead to a decrease in ON cell activity and an increase in OFF cell activity. However, in chronic musculoskeletal pain conditions, there appears to be an overall shift to a decrease in inhibition, presumably due to an imbalance of ON cell and OFF cell activity59. Disrupted descending inhibition in chronic musculoskeletal pain may lead to an increased pain sensitivity of muscle tissue60.
Evaluation and Treatment
The history of soft tissue pain treatments follows the clinical trends of those physicians and soft tissue specialists (e.g., massage therapists, MTrP therapists) most likely to evaluate and treat MPS, and not necessarily researchers. Hence, early literature about therapeutics for MPS was mainly descriptive. Publications included recommendations for the use of postural exercise, heat, cold, stretch, fluoromethane spray, electrical stimulation, needling, and acupuncture, to mention a few61.
In her autobiography Office Hours: Day and Night, Travell describes her approach to the diagnosis of MPS and selection among treatment options. She demonstrates her keen clinical acumen to judge treatment effectiveness, using a trial/error empirical approach62. In The Trigger Point Manual, Travell and Simons worked together to provide a more systematic approach. They stressed the importance of the physical examination including thorough palpation of muscle and surrounding tissue in order to identify MTrPs. The MTrP requires training and experience to identify, and was the target for their treatment9. They often relied on pressure pain threshold to supplement their palpation findings in order to distinguish a latent from an active MTrP. Today, several other methods including intramuscular needling, surface electromyography-guided assessment, infrared thermography, ultrasound, and laser Doppler flowmetry are utilized in an attempt to objectify MTrP findings63. Nevertheless, palpation by an experienced clinician remains the gold standard in MTrP identification.
Travell and Simons were not the first to identify and develop a treatment for MTrPs. They were, however, among the first to recognize the relationship of the trigger point to MPS and clinical soft tissue pain syndromes. They proposed that deactivating the trigger point was an essential component to successfully treating the pain syndrome9.
One of various techniques that Travell and Simons relied on to treat MTrPs was injection with local anesthetics. Travell was greatly influenced by Kellgren's work utilizing injections with procaine to treat “myalgia”64. The injections were beneficial because they could reach muscles that could not be stretched during manual therapies (e.g., sternalis) and had the longest analgesic effect out of any treatment at the time. However, in the 1930s-1940s, the use of local anesthetics raised several concerns including muscle necrosis, fatal anaphylactic shock, and dose-related toxic effects that resulted from multiple treatments using cumulative doses. Travell and Simons stressed the importance of using a low dose and taking precautionary measures by having a tourniquet, intravenous diazepam, equipment for artificial respiration, and cardiac defibrillator available during the injection9,61. Although Travell and Simons utilized this technique, they were concerned about the risks of anaphylactic shock in a susceptible person.
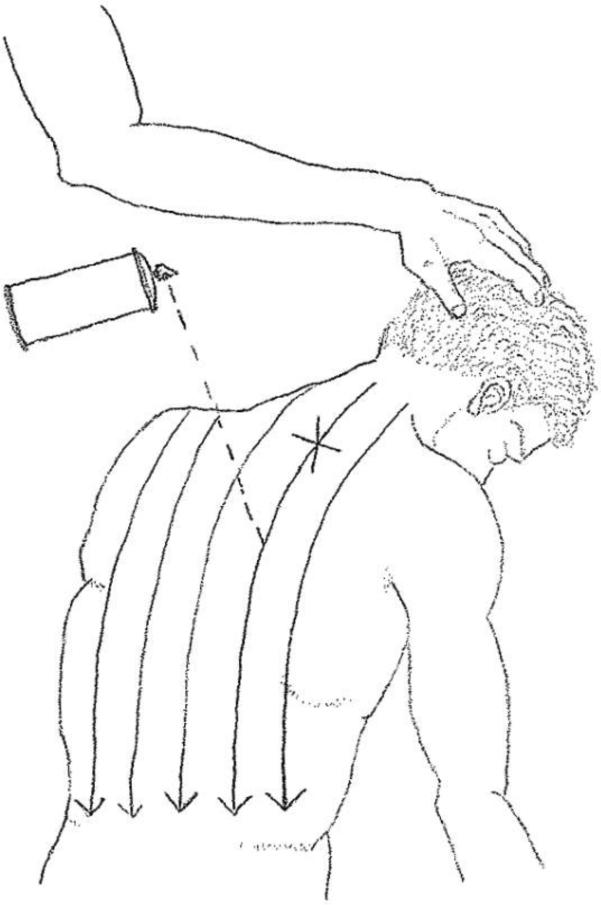
Accordingly, they often preferred to deactivate MTrPs by spray and stretch9, which involves spraying the overlying skin with ethyl chloride, introducing a sudden sensory stimulus which distracts the patient from the discomfort associated with stretching the affected muscles9 (Figure 5). One of the benefits of spray and stretch is that it allows for many muscles to be treated in a short period of time. Simons and Travell hypothesized this method was effective because it targeted an “energy crisis” in the region of the MTrP. Stretching the muscles would lengthen the sarcomere and reduce overlap between actin and myosin molecules, decreasing the need for ATP and breaking the vicious cycle of the “energy crisis”18. Simons and Travell were enthusiastic about this technique, calling it the “workhorse” of myofascial therapy. However, in the event that the MTrP was unresponsive to spray and stretch, injections with anesthetics were still used.
Figure 5.
Spray and Stretch Application. The lower posterior muscles of the upper back are stretched while the spray is applied in a downward motion, from the patient's neck to the referred pain region. (Drawn from Ferguson, L. W. and R. Gerwin (2005). Clinical mastery in the treatment of myofascial pain. Philadelphia, Lippincott Williams & Wilkins.).
In 1955, Sola and Kuitert introduced saline injections to deactivate MTrPs, which lacked the risks of local anesthetics65. Interestingly, Frost et al. (1980) discovered that in a double blinded comparison, 80 percent of patients reported pain relief with saline injections compared to 52 percent with injections of mepivacaine66.
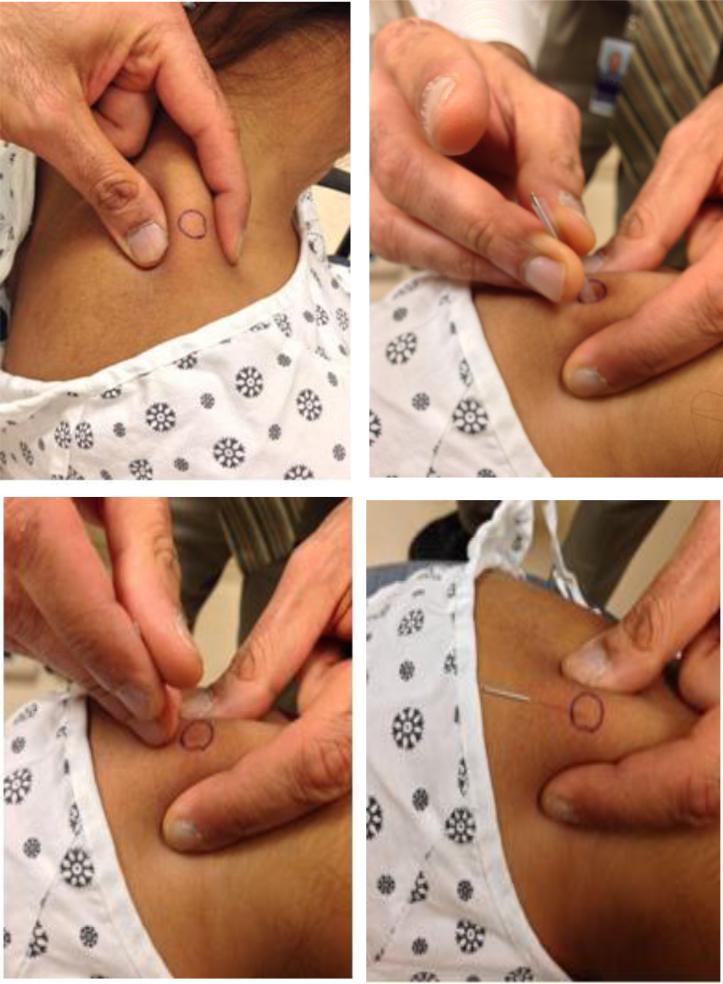
Naturally, the effectiveness of needling without anesthetics lead to the question of whether saline was even necessary for deactivating MTrPs. In 1979, Lewit was one of the first physicians to try needling without the use of anesthetic or even saline, a technique that became known as dry needling67. Given the size of the hypodermic needle and the invasive technique used, this form of dry needling was quite painful, which deterred others from using it instead of injections with procaine. However, Lewit found that the effectiveness of dry needling was related to both the severity of the pain and the precision by which the needle is inserted in relation to the MTrP67. In a study of 241 chronic myofascial pain patients with various pain sites, Lewit found that dry needling caused immediate analgesia in nearly 87% of cases. For example, in over 31% of cases, the analgesia was permanent, while 20% had several months of pain relief, 22% several weeks, and only 14% had no relief at all67. Currently, clinicians use acupuncture needles to minimize pain and tissue injury, and have found that inserting a needle into the general area of the MTrP as opposed to directly into the MTrP can have the same therapeutic effect61 (Figure 6).
Figure 6.
Dry Needling. A series of images are shown in which the MTrP is identified, the needled is inserted in the MTrP using a swift tap, the muscle and surrounding fascia are probed with an up and down motion of the needle in a clockwise direction, and the needle is left in place for 1-2 minutes for full therapeutic benefit.
In addition to dry needling, clinicians in the mid-20th century started experimenting with the use of acupuncture, after learning that the Chinese were using acupuncture analgesia to suppress surgically evoked pain61. In the 1970s, interest in acupuncture surged, and even President Nixon and his personal physician enthusiastically supported its use. While Melzack and Wall found that acupuncture points for pain and MTrP sites share a close spatial relationship (71% overall correspondence), MTrPs and acupuncture points are not the same phenomena68. For example, MTrPs, unlike acupuncture points, are not immutable, and thus MTrPs sites, as outlined in The Trigger Point Manual, mainly serve as a guide for where a clinician should start looking for MTrPs. Furthermore, MTrPs are palpable, tender nodules, whereas acupuncture points are not palpable, necessarily tender, or nodular17. Due to the lack of sound scientific studies, interest in acupuncture quickly declined, but continues to be further studied as a topic with important MTrP implications today.
In the 1980s, use of fluoromethane spray, a topical anesthetic, ceased because of its toxic effect on the ozone layer and the fact that its highly flammable properties led to accidental death69. This occurrence spurred the development of various alternative treatments. For example, the counterstrain method (see online video supplement), a positional release technique developed by Jones in 1981, is shown to be effective at reducing pain and improving function. Ischemic compression, which aims to equalize the length of the sarcomeres, has also been shown to decrease pain sensitivity. Another method is transverse friction massage which, when combined with exercise, has been shown to increase flexibility along with function63. All three of these techniques stretch the muscles, which is the aim of any manual therapy. In addition, Travell and Simons stressed the importance of moist heat to relax the underlying muscles and to diminish the tension caused by the MTrPs. They also educated patients on proper postural positioning while sitting, standing, and reading in order to avoid sustained contraction or prolonged shortening of muscles9.
During this time, Travell and Simons also explored the role of drugs with respect to pain relief (codeine, aspirin, anti-inflammatory drugs), muscular relaxation (Diazepam), sleep (anti-histamines), and post-therapy soreness (anti-inflammatory action), although their findings were largely empirical. Travell and Simons noted that many of the side effects for these drugs were often greater than symptoms of MPS. In cases where the drug seemed effective, there was always the possibility of a placebo effect9.
In the 1980s and 1990s, there was significant interest in technologies like transcutaneous electrical nerve stimulation (TENS), ultrasound, and laser for the treatment of soft tissue pain. Researchers debate the effectiveness of laser and ultrasound for the deactivation of MTrPs but generally agree that these technologies are effective for pain management. Biofeedback, introduced by Keefe in 1981, and other relaxation techniques like hypnotherapy, are also available to help patients manage their pain by training them to regain control of their pain condition.
It is important to note that clinicians have been treating MPS based on what they believe is its underlying pathophysiology and what are considered safe and effective treatments. For example, Travell and Simons primarily utilized the spray and stretch technique because they attributed MPS to muscle overload, whereas Sola and Kuitert65 and Lewit67 utilized saline injections and dry needling, respectively, because they believed their methods mechanically disrupted the dysfunctional endplates located near the MTrP. Both of these theories are still considered plausible and discussed today.
While the etiology of MPS and the pathophysiology of MTrPs are not yet fully understood, some investigators are suggesting that treatments should focus not only on the MTrP, but also the surrounding environment (e.g., fascia, connective tissue, etc.)36,54. The biochemical contributors to pain are very important. The role of muscle, fascia, and their cellular components are also important factors to both MPS and the formation of the MTrP. This thinking has led clinicians to try to reduce the size of the MTrP, correct underlying contributors to the pain, and restore the normal working relationship between the muscles of the affected functional units70.
According to Dommerholt, all treatments fall into one of these two categories or both: a pain-control phase and a deep conditioning phase. During the pain-control phase, trigger points are deactivated, improving circulation, decreasing pathological nociceptive activity, and eliminating the abnormal biomechanical force patterns. During the deep conditioning phase, the intra- and inter- tissue mobility of the functional unit is improved, which may include specific muscle stretches, neurodynamic mobilizations, joint mobilizations, orthotics, and strengthening muscle71.
Current approaches for management of MPS include pharmacological and nonpharmacological interventions. Among the pharmacological approaches are anti-inflammatory, analgesic, and narcotic medications, topical creams, and trigger point injections, which are now safer and more effective. Non-pharmacological interventions include manual therapies, which continue to include post-isometric relaxation, counterstrain method72, trigger point compression, muscle energy techniques, and myotherapy73, along with other treatments like laser therapy74, dry needling, and massage35,75.
According to Simons, stretching and strengthening of the affected muscles is important for any treatment17. While many of the manual treatment methods stay the same or are only slightly modified (all include some form of mechanical pressure), it is the underlying theory as to why they are effective that continues to evolve with further study. Modalities and manual treatments are often clinically effective for deactivating active MTrPs and desensitizing sensitized spinal segments, and are commonly employed as a first line of treatment before attempting more invasive therapies. While a number of recent reviews and meta-analyses have focused on needling, the effectiveness of manual therapy should not be overlooked and may possibly be just as effective as needling76.
Among the invasive therapies, the scientific articles report mixed results. Generally, dry needling, anesthetic injection, steroids, and botulinum toxin-A [BTA] of the trigger point have all been shown to provide pain relief70,77-81. Regardless of the method used, there is considerable agreement that elicitation of a LTR produces more immediate and long-lasting pain relief than no elicitation of LTR81-86, although some still believe that eliciting an LTR is not necessary for improvement. Nevertheless, within minutes of a single induced LTR, Shah et al. found that the initially elevated levels of SP and CGRP within the active MTrP in the upper trapezius muscle decreased to levels approaching that of normal, uninvolved muscle tissue. Though the mechanism of an LTR is unknown, the reduction of these biochemicals in the local muscle area may be due to a small, localized increase in blood flow and/or nociceptor and mechanistic changes associated with an augmented inflammatory response59,87.
While treatment options for soft tissue pain have not changed dramatically, researchers today have certainly discovered better ways of categorizing and analyzing the clinical data they collect and determining if a treatment is effective. For example, since Travell and Simons’ time, researchers have begun to utilize classifications such as latent, “non-painful palpable,” and “painful, but no nodule” to categorize MPS. Gerber et al. have also begun to assess the effect of treatment on other aspects besides pain such as quality of life and function, disability, sleep, mood, and range of motion28. Clinicians are shifting the focus from not only pain relief and increasing function, but to improving the patient's quality of life as well.
Though many practitioners can attest to improvement in pain levels of MPS, it is measured using self-reports of pain levels pre- and post-treatment. To date, the number of randomized, placebo-controlled trials is few, and most of them have small numbers of participants. Additionally, because they rely exclusively on self-reports, there remains uncertainty about the validity of the findings. Thus, while a variety of pharmacological and nonpharmacological treatments have shown efficacy, studies of proper size and quantitative outcome measures need to be performed.
Conclusion
To date, the pathogenesis and pathophysiology of MTrPs and their role in MPS remain unknown. Data have been published suggesting that MPS is a pain syndrome that can be acute or chronic, and that it involves muscle and fascia. The MTrP remains central to its diagnosis, and possibly its successful treatment. New methods of describing and imaging the MTrP as well as the milieu of the MTrP have suggested that there are a variety of objective findings associated with the syndrome and active MTrPs. Table 1 compares the contributions of Travell and Simons to the contemporary understanding of the MTrP.
Table 1.
Comparing Travell and Simons’ Contributions to the Contemporary Understanding of Myofascial Trigger Points
| Understanding of MTrPs based on Travell and Simons’ work | Contemporary understanding of MTrPs based on scientific evidence |
|---|---|
|
MTrP Characteristics A systematic description of physical and electrodiagnostic findings: • Defined MTrP as “a hyperirritable locus within a taut band of skeletal muscle . . . [that] is painful on compression and can evoke characteristic referred pain and autonomic phenomena” • Differentiated active from latent MTrPs • Codified criteria for identifying MTrPs in the evaluation of pain • Utilized electrodiagnostic studies to demonstrate abnormal activity, indicating involvement of the neuromuscular junction |
MTrP Characteristics Objective measures of abnormal physical findings suggesting MTrP pathophysiology: • Biochemical findings indicate local and remote inflammation, and local acidic milieu • Biochemical and physical findings implicate local sensitization • Oxygenation studies indicate local regions of hypoxia • Imaging studies indicate local regions of muscle stiffness • Evidence implicating abnormalities of the myofascial neighborhood beyond the MTrP |
|
Relation to MPS MTrP causes MPS symptomatology: • MTrP associates with focal pain and hyperirritability • MTrP presents with pain radiation • MTrP perturbation produces local twitch response |
Relation to MPS Relationship between MTrP and MPS has not yet been determined: • Patients may have MPS without MTrPs, and MTrPs without MPS • MTrP may or may not present with pain radiation • MTrP perturbation does not always produce local twitch response |
|
Clinical Evaluation Clinical case series propose tentative link between symptoms and physical findings: • A specific collection of symptoms is associated with MTrPs including regional pain, decreased flexibility, and clinical signs of allodynia and hyperalgesia • Stereotypical patterns of referred pain are associated with MTrPs in different muscles |
Clinical Evaluation Clinical studies and trials establish link between symptoms and physical findings: • Mechanisms of muscle nociception, sensitization, and pain have been well documented • Biochemical studies link painful MTrPs with muscle nociception, sensitization, and pain |
|
Treatment Treatments target MTrPs to reduce pain: • Spray and stretch • Deep massage • Anesthetic injections • Pharmacological agents |
Treatment Treatments target MTrP to reduce pain and improve symptoms and function: • Manual manipulation • Dry needling • Transcutaneous electrical nerve stimulation • Ultrasound |
|
Outcome Measures Treatment of MTrP leads to: • Improvement of pain • Increased flexibility (anecdotally) |
Outcome Measures Treatment of MTrP leads to: • Improvement of pain • Decreased tenderness • Increased range of motion • Improvement of quality of life |
Earlier theories for the pathogenesis of MTrPs and MPS, including muscle overuse and mechanical difficulties, remain current and have been neither proven nor disproven.
Current data suggest that active MTrPs are associated with a high symptom burden and a negative impact on function, both physical and psychosocial. Investigators also demonstrated that dry needling provides symptom relief and change in the status of the trigger point88, although the mechanism by which this works has not yet been demonstrated.
Many questions remain to be answered. For example, what is the etiology and pathophysiology of MPS? What is the role of the MTrP in the pathogenesis of MPS? Is the resolution of the MTrP required for clinical response? What is the mechanism by which the pain state begins, evolves, and persists? Though the presence of pro-inflammatory and noxious biochemicals has been established, what are the levels of anti-inflammatory substances, analgesic substances, and muscle metabolites in the local biochemical milieu of muscle with and without MTrPs? How does a tender nodule progress to a myofascial pain syndrome? Which musculoskeletal tissues are involved, what are their properties, and how do these change in response to treatment? These are some of the questions researchers must address in the future. Proper treatment of MPS requires identification and targeting of the mechanisms and pathophysiology of perpetuating factors in order to obtain sustained relief.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jay P. Shah, Rehabilitation Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD.
Nikki Thaker, Rehabilitation Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD nthaker91@yahoo.com.
Juliana Heimur, Rehabilitation Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD Juliana.heimur@gmail.com.
Jacqueline V. Aredo, Rehabilitation Medicine Department, Clinical Center, National Institutes of Health, Bethesda, MD jacqueline.aredo@gmail.com.
Siddhartha Sikdar, Departments of Electrical and Computer Engineering and Bioengineering, Volgenau School of Engineering, George Mason University, Fairfax, VA ssikdar@gmu.edu.
Lynn H. Gerber, Center for the Study of Chronic Illness and Disability, College of Health and Human Services, George Mason University, 4400 University Dr, Fairfax, VA 22030 Ngerber1@gmu.edu.
References
- 1.Skootsky S, Jaeger B, Oye R. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989 Aug;151(2):157–160. [PMC free article] [PubMed] [Google Scholar]
- 2.Gerwin RD. Classification, epidemiology, and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001 Oct;5(5):412–420. doi: 10.1007/s11916-001-0052-8. [DOI] [PubMed] [Google Scholar]
- 3.Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985 Dec;60(6):615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 4.Bennett MJ, McLaughlin S, Anderson T, McDicken WN. Error analysis of ultrasonic tissue doppler velocity estimation techniques for quantification of velocity and strain. Ultrasound in Medicine & Biology. 2007;33(1):74–81. doi: 10.1016/j.ultrasmedbio.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 5.Stockman R. The cause, pathology, and treatment of chronic rheumatism. Edinburgh Med J. 1904;15:107–116. doi: 10.1136/bmj.1.2252.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Froriep R. Ein Beitrag zur Pathologie und Therapie des Rheumatismus. 1843 [Google Scholar]
- 7.Gowers WR. Lumbago: its lessons and analogues. Br Med J. 1904;1:117–121. doi: 10.1136/bmj.1.2246.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schade H. Untersuchungen in der Erkältungstrage: III. Uber den Rheumatismus, insbesondere den Muskelrheumatismus (myogelose). Müench Med Wochenschr. 1921;68:95–99. [Google Scholar]
- 9.Travell JG, Simons DG. Myofascial pain and dysfunction : the trigger point manual. Williams & Wilkins; Baltimore: 1983. [Google Scholar]
- 10.Travell JG, Rinzler SH. The myofascial genesis of pain. Postgraduate Medicine. 1952;11:434–452. doi: 10.1080/00325481.1952.11694280. [DOI] [PubMed] [Google Scholar]
- 11.Robert B. Myofascial pain syndromes and their evaluation. Best Practice & Research Clinical Rheumatology. 2007;21(3):427–445. doi: 10.1016/j.berh.2007.02.014. [DOI] [PubMed] [Google Scholar]
- 12.Borg-Stein J, Simons DG. Focused review: myofascial pain. Arch Phys Med Rehabil. 2002 Mar;83(3 Suppl 1):S40–47. S48–49. doi: 10.1053/apmr.2002.32155. [DOI] [PubMed] [Google Scholar]
- 13.Hong C. Pathophysiology of myofascial trigger point. J Formos Med Assoc. 1996;95:93–104. [PubMed] [Google Scholar]
- 14.Harden R, Bruehl S, S SG, Niemiec C, Barbick B. Signs and symptoms of the myofascial pain syndrome: a national survey of pain management providers. Clin J Pain. 2000;16(1):64–72. doi: 10.1097/00002508-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Sikdar S, Shah JP, Gebreab T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. 2009 Nov;90(11):1829–1838. doi: 10.1016/j.apmr.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: an application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008 Oct;12(4):371–384. doi: 10.1016/j.jbmt.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction : the trigger point manual. 2nd ed. Williams & Wilkins; Baltimore: 1999. [Google Scholar]
- 18.Mense S, Simons D, Russell I. Muscle Pain: Understanding its Nature, Diagnosis and Treatment. 1st ed. Lippincott Williams and Wilkins; Philadelphia: 2001. [Google Scholar]
- 19.Hägg G, Anderson P, Hobart D, Danoff J, editors. Electromyographical Kinesiology. Elsevier; Amsterdam: 1991. Static work load and occupational myalgia: a new explanation model. pp. 141–144. [Google Scholar]
- 20.Treaster D, Marras WS, Burr D, Sheedy JE, Hart D. Myofascial trigger point development from visual and postural stressors during computer work. J Electromyogr Kinesiol. 2006 Apr;16(2):115–124. doi: 10.1016/j.jelekin.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 21.Kaergaard A, Andersen JH. Musculoskeletal Disorders of the Neck and Shoulders in Female Sewing Machine Operators: Prevalence, Incidence, and Prognosis. Occupational and environmental medicine. 2000;57(8):528–534. doi: 10.1136/oem.57.8.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reitinger A, Radner H, Tilscher H, Hanna M, Windisch A, Feigl W. Morphologische Untersuchung an Trigger punkten. Manuelle Medizin. 1996;34:256–262. [Google Scholar]
- 23.Windisch A, Reitinger A, Traxler H, et al. Morphology and histochemistry of myogelosis. Clinical Anatomy. 1999;12(4):266–271. doi: 10.1002/(SICI)1098-2353(1999)12:4<266::AID-CA5>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 24.Mense S. The pathogenesis of muscle pain. Current Pain and Headache Reports. 2003;7:419–425. doi: 10.1007/s11916-003-0057-6. [DOI] [PubMed] [Google Scholar]
- 25.Shah JP, Phillips TM, Danoff JV, Gerber LH. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol (1985) 2005 Nov;99(5):1977–1984. doi: 10.1152/japplphysiol.00419.2005. [DOI] [PubMed] [Google Scholar]
- 26.Kuan TS, Hong CZ, Chen JT, Chen SM, Chien CH. The spinal cord connections of the myofascial trigger spots. Eur J Pain. 2007 Aug;11(6):624–634. doi: 10.1016/j.ejpain.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Niddam DM, Chan RC, Lee SH, Yeh TC, Hsieh JC. Central modulation of pain evoked from myofascial trigger point. Clin J Pain. 2007 Jun;23(5):440–448. doi: 10.1097/AJP.0b013e318058accb. [DOI] [PubMed] [Google Scholar]
- 28.Gerber LH, Sikdar S, Armstrong K, et al. A systematic comparison between subjects with no pain and pain associated with active myofascial trigger points. PM R. 2013 Nov;5(11):931–938. doi: 10.1016/j.pmrj.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trough E, White A, Richards S. Variability of criteria used to diagnosis myofascial trigger point pain syndrome-evidence from a review of the literature. Clin J Pain. 2007;23:278–286. doi: 10.1097/AJP.0b013e31802fda7c. [DOI] [PubMed] [Google Scholar]
- 30.Hubbard DR, Berkoff GM. Myofascial trigger points show spontaneous needle EMG activity. Spine (Phila Pa 1976) 1993 Oct 1;18(13):1803–1807. doi: 10.1097/00007632-199310000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Wiederholt WC. “End-plate noise” in electromyography. Neurology. Mar. 1970;20(3):214–224. doi: 10.1212/wnl.20.3.214. [DOI] [PubMed] [Google Scholar]
- 32.Simons DG. Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J Electromyogr Kinesiol. 2004 Feb;14(1):95–107. doi: 10.1016/j.jelekin.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 33.Dommerholt J, Shah JP, Ballantyne JC, Rathmell JP, Fishman SM. Myofascial Pain Syndrome. 4th ed. Williams & Wilkins; Baltimore: 2010. [Google Scholar]
- 34.Wolfe F. The fibromyalgia and myofascial pain syndromes: A preliminary study of tender points and trigger points in person wiht fibromyalgia, myofascial pain syndrome and no disease. J Rheumatol. 1992;19:944–951. [PubMed] [Google Scholar]
- 35.Dommerholt J, Huijbregts P. Myofascial trigger points : pathophysiology and evidence- informed diagnosis and management. Jones and Bartlett Publishers; Sudbury, Mass: 2011. [Google Scholar]
- 36.Stecco A, Gesi M, Stecco C, Stern R. Fascial components of the myofascial pain syndrome. Curr Pain Headache Rep. 2013 Aug;17(8):352. doi: 10.1007/s11916-013-0352-9. [DOI] [PubMed] [Google Scholar]
- 37.Stecco C, Stern R, Porzionato A, et al. Hyaluronan within fascia in the etiology of myofascial pain. Surg Radiol Anat. 2011 Dec;33(10):891–896. doi: 10.1007/s00276-011-0876-9. [DOI] [PubMed] [Google Scholar]
- 38.Quintner J, Cohen M. Referred pain of peripheral nerve origin: an alternative to the ‘myofascial pain’ construct. Clinical Journal of Pain. 1994;10:243–251. doi: 10.1097/00002508-199409000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Srbely J. New trends in the treatment and management of myofascial pain syndrome. Curr Pain Headache Rep. 2010;14(5):346–352. doi: 10.1007/s11916-010-0128-4. [DOI] [PubMed] [Google Scholar]
- 40.Srbely JZ, Dickey JP, Bent LR, Lee D, Lowerison M. Capsaicin-induced central sensitization evokes segmental increases in trigger point sensitivity in humans. J Pain. 2010 Jul;11(7):636–643. doi: 10.1016/j.jpain.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Ballyns JJ, Shah JP, Hammond J, Gebreab T, Gerber LH, Sikdar S. Objective sonographic measures for characterizing myofascial trigger points associated with cervical pain. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2011 Oct;30(10):1331–1340. doi: 10.7863/jum.2011.30.10.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ballyns JJ, Turo D, Otto P, et al. Office-based elastographic technique for quantifying mechanical properties of skeletal muscle. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2012 Aug;31(8):1209–1219. doi: 10.7863/jum.2012.31.8.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Turo D, Otto P, Shah JP, et al. Ultrasonic characterization of the upper trapezius muscle in patients with chronic neck pain. Ultrasonic imaging. 2013 Apr;35(2):173–187. doi: 10.1177/0161734612472408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sikdar S, Ortiz R, Gebreab T, Gerber LH, Shah JP. Understanding the vascular environment of myofascial trigger points using ultrasonic imaging and computational modeling. Conference proceedings : ... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference. 2010;2010:5302–5305. doi: 10.1109/IEMBS.2010.5626326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huguenin L. Myofascial trigger points: the current evidence. Physical Therapy in Sport. 2004;5:2–12. [Google Scholar]
- 46.Audette J, Bailey A. The Science and Practice of Complementary and Alternative Medicine in Pain Management. California Humana Press; 2008. Integrative Pain Medicine. [Google Scholar]
- 47.Camanho L, Imamura M, Arendt-Nielsen L. Genesis of pain in arthrosis. Revista Brasileira de Ortopedia. 2011:14–17. doi: 10.1016/S2255-4971(15)30168-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Woolf CJ. Central sensitization: uncovering the relation between pain and plasticity. Anesthesiology. 2007 Apr;106(4):864–867. doi: 10.1097/01.anes.0000264769.87038.55. [DOI] [PubMed] [Google Scholar]
- 49.Hoheisel U, Koch K, Mense S. Functional reorganization in the rat dorsal horn during an experimental myositis. Pain. 1994 Oct;59(1):111–118. doi: 10.1016/0304-3959(94)90054-X. [DOI] [PubMed] [Google Scholar]
- 50.Sato A. Somatovisceral reflexes. J Manipulative Physiol Ther. 1995 Nov-Dec;18(9):597–602. [PubMed] [Google Scholar]
- 51.Sperry M, Goshgarian H. Ultrastructural changes in the rat phrenic nucleus developing within 2 h after cervical spinal cord hemisection. Experimental Neurology. 1993;120:233–244. doi: 10.1006/exnr.1993.1058. [DOI] [PubMed] [Google Scholar]
- 52.Mense S, Hoheisel U. Central nervous sequelae of local muscle pain. Journal of Musculoskeletal Pain. 2004;12:101–109. [Google Scholar]
- 53.Svensson P, Minoshima S, Beydoun A, Morrow TJ, Casey KL. Cerebral processing of acute skin and muscle pain in humans. J Neurophysiol. 1997 Jul;78(1):450–460. doi: 10.1152/jn.1997.78.1.450. [DOI] [PubMed] [Google Scholar]
- 54.Mense S. How Do Muscle Lesions such as Latent and Active Trigger Points Influence Central Nociceptive Neurons? Journal of Musculoskeletal Pain. 2010;18(4):348–353. [Google Scholar]
- 55.Svensson P, Cairns BE, Wang K, Arendt-Nielsen L. Injection of nerve growth factor into human masseter muscle evokes long-lasting mechanical allodynia and hyperalgesia. Pain. 2003 Jul;104(1-2):241–247. doi: 10.1016/s0304-3959(03)00012-5. [DOI] [PubMed] [Google Scholar]
- 56.Hoheisel U, Unger T, Mense S. Sensitization of rat dorsal horn neurons by NGF-induced subthreshold potentials and low-frequency activation. A study employing intracellular recordings in vivo. Brain Research. 2007;1169:34–43. doi: 10.1016/j.brainres.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 57.Graven-Nielsen T, Curatolo M, Mense S. Central sensitization, referred pain and deep tissue hyperalgesia in musculoskeletal pain. Proceedings of the 11th World Congress on Pain. 2006 [Google Scholar]
- 58.Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965 Nov 19;150(3699):971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 59.Willard F. Integrative Pain Medicine: The Science and Practice of Complementary and Alternative Medicine in Pain Management. Humana Press Inc; Totowa: 2008. Basic Mechanisms of Pain.” Future Trends in CAM Research. [Google Scholar]
- 60.Ge HY, Fernandez-de-Las-Penas C, Yue SW. Myofascial trigger points: spontaneous electrical activity and its consequences for pain induction and propagation. Chin Med. 2011;6:13. doi: 10.1186/1749-8546-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baldry P. Acupuncture, trigger points, and musculoskeletal pain. Churchill Livingstone; Edinburgh ; New York: 1989. [Google Scholar]
- 62.Travell JG. Office hours: day and night; the autobiography of Janet Travell. World Pub. Co.; M.D. New York: 1968. [Google Scholar]
- 63.Celik D, Mutlu E. Clinical implication of latent myofascial trigger point. Curr Pain Headache Rep. 2013;17(8):353. doi: 10.1007/s11916-013-0353-8. [DOI] [PubMed] [Google Scholar]
- 64.Kellgren J. Observations on referred pain arising from muscle. Clin Sci. 1938;3:175–190. [Google Scholar]
- 65.Sola AE, Kuitert JH. Myofascial trigger point pain in the neck and shoulder girdle; report of 100 cases treated by injection of normal saline. Northwest Med. 1955 Sep;54(9):980–984. [PubMed] [Google Scholar]
- 66.Frost FA, Jessen B, Siggaard-Andersen J. [Myofascial pain treated with injections. A controlled double-blind trial]. Ugeskr Laeger. 1980 Jun 30;142(27):1754–1757. [PubMed] [Google Scholar]
- 67.Lewit K. The needle effect in the relief of myofascial pain. Pain. 1979 Feb;6(1):83–90. doi: 10.1016/0304-3959(79)90142-8. [DOI] [PubMed] [Google Scholar]
- 68.Melzack R, Stillwell DM, Fox E. Trigger points and acupuncture points for pain: correlations and implications. Pain. 1977;3:3–23. doi: 10.1016/0304-3959(77)90032-X. [DOI] [PubMed] [Google Scholar]
- 69.Vallentyne SW, Vallentyne JR. The case of the missing ozone: are physiatrists to blame? Arch Phys Med Rehabil. 1988 Nov;69(11):992–993. [PubMed] [Google Scholar]
- 70.Majlesi J, Unalan H. Effect of treatment on trigger points. Curr Pain Headache Rep. 2010 Oct;14(5):353–360. doi: 10.1007/s11916-010-0132-8. [DOI] [PubMed] [Google Scholar]
- 71.Saal J, Saal J. Rehabilitation of the patient. In: White A, Anderson R, editors. Conservative Care of Low Back Pain. Williams and Wilkins; Baltimore: 1991. pp. 21–34. [Google Scholar]
- 72.Myers HL. Clinical application of counterstrain. Osteopathic Press; Tucson, AZ: 2006. [Google Scholar]
- 73.Cantu RI, Grodin AJ. Myofascial manipulation : theory and clinical application. 2nd ed. Aspen Publishers; Gaithersburg, Md.: 2001. [Google Scholar]
- 74.Uemoto L, Nascimento de Azevedo R, Almeida Alfaya T, Nunes Jardim Reis R, Depes de Gouvea CV, Cavalcanti Garcia MA. Myofascial trigger point therapy: laser therapy and dry needling. Curr Pain Headache Rep. 2013 Sep;17(9):357. doi: 10.1007/s11916-013-0357-4. [DOI] [PubMed] [Google Scholar]
- 75.Simons D. Understanding effective treatments of Myofascial trigger points. J Bodywork Mov Ther. 2002;6:81–88. [Google Scholar]
- 76.Rayegani SM, Bayat M, Bahrami MH, Raeissadat SA, Kargozar E. Comparison of dry needling and physiotherapy in treatment of myofascial pain syndrome. Clin Rheumatol. 2013 Dec 19; doi: 10.1007/s10067-013-2448-3. [DOI] [PubMed] [Google Scholar]
- 77.Peloso P, Gross A, Haines T, Trinh K, Goldsmith CH, Burnie S. Medicinal and injection therapies for mechanical neck disorders. Cochrane Database Syst Rev. 2007;(3):CD000319. doi: 10.1002/14651858.CD000319.pub4. [DOI] [PubMed] [Google Scholar]
- 78.Ho KY, Tan KH. Botulinum toxin A for myofascial trigger point injection: a qualitative systematic review. Eur J Pain. 2007 Jul;11(5):519–527. doi: 10.1016/j.ejpain.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 79.Lang AM. Botulinum toxin therapy for myofascial pain disorders. Curr Pain Headache Rep. 2002 Oct;6(5):355–360. doi: 10.1007/s11916-002-0076-8. [DOI] [PubMed] [Google Scholar]
- 80.Birch S, Jamison RN. Controlled trial of Japanese acupuncture for chronic myofascial neck pain: assessment of specific and nonspecific effects of treatment. Clin J Pain. 1998 Sep;14(3):248–255. doi: 10.1097/00002508-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 81.Chu J. Dry needling (intramuscular stimulation) in myofascial pain related to lumbar radiculopathy. Eur J Phys Med Rehabil. 1995;5:106–121. [Google Scholar]
- 82.Rivner M. The neurophysiology of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5:432–440. doi: 10.1007/s11916-001-0054-6. [DOI] [PubMed] [Google Scholar]
- 83.Lartigue A. Patient education and self-advocacy. Myofascial pain syndrome: treatments. J Pain Palliat Care Pharmacother. 2009;23:169–170. doi: 10.1080/15360280902901255. [DOI] [PubMed] [Google Scholar]
- 84.Simons D, Mense S. Diagnosis and therapy of myofascial trigger points [in German]. Schmerz. 2003;17:419–424. doi: 10.1007/s00482-003-0253-7. [DOI] [PubMed] [Google Scholar]
- 85.Chu J, Schwartz I. The muscle twitch in myofascial pain relief: effects of acupuncture and other needling methods. Electromyogr Clin Neurophysiol. 2002 Jul-Aug;42(5):307–311. [PubMed] [Google Scholar]
- 86.Criscoulo C. Interventional approaches to the management of myofascial pain syndrome. Curr Pain Headache Rep. 2001;5:407–411. doi: 10.1007/s11916-001-0051-9. [DOI] [PubMed] [Google Scholar]
- 87.Shah JP, Danoff JV, Desai MJ, et al. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008 Jan;89(1):16–23. doi: 10.1016/j.apmr.2007.10.018. [DOI] [PubMed] [Google Scholar]
- 88.Armstrong K, Otto PR, Turo D, Gebreab TM, Thaker N, Rosenberger W, Sikdar S, Shah JP. Dry-Needling Reduces Pain and Alters Status of Active Trigger Points in Subjects with Chronic Myofascial Pain: A Prospective Study. PM&R. 2014 Sep;6(9):S248. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.