Abstract
This study describes an evaluation of a community-based psychoeducational intervention, called The Family Series Workshop, for caregivers of community-dwelling persons with Alzheimer’s disease or related dementias (ADRD). In a one-group pretest–posttest design, participants (n = 35) attended six weekly sessions. Caregiver stress, coping, and caregiving competence were evaluated along with demographic characteristics of participants. There was a significant improvement found for caregiving competence, and a marginally significant increase in coping with humor. Using regression analysis we also found that coping with humor, along with stress, were significant predictors of caregiving competence. These findings indicate that it is possible to increase caregiving competence utilizing a “grassroots” approach and that it is feasible to hold educational, group discussions on a plethora of challenging caregiving topics.
Keywords: Alzheimer’s disease, dementia, caregiving, interventions, psychoeducation, one-group pretest-posttest design
Introduction
The number of persons with Alzheimer’s disease (AD) is expected to almost triple by the year 2050 to 13.8 million people, causing a silver tsunami that will have a drastic socioeconomic impact on the US national health care system. 1 Currently, AD affects more than 5 million people in the United States, which accounts for 60% to 80% of those with progressive dementia. 1 Dementia is a cognitive disorder characterized by the loss of, or decline in memory, word recall and other cognitive abilities to the point of interfering with daily activity. 2 –5 The most common type of dementia is AD. 1 As the number of people with AD and related dementias (ADRD) increases, the number of people caring for them will also increase. Because unpaid caregivers of persons with dementia provide 60% to 70% of care in the community, ADRD impacts millions of family members and friends. 1
Caring for a person with ADRD can be an overwhelming experience. 6,7 Caregiving can be severely taxing and affect coping abilities and the well-being of the caregivers. 8,9 Providing continuous care for a person with ADRD has been associated with chronic fatigue, depression, deteriorating health, and emotional problems. 10,11 Past research has found that chronic stress, such as the stress associated with caregiving, can slow wound healing, diminish the strength of immune responses to vaccines, enhance susceptibility to infectious agents, and reactivate latent viruses. 12,13 These pathophysiological adaptations are likely related to prolonged chronic stress response, and can, in itself, be detrimental. 14 Stress results in the release of inflammatory molecules such as C-reactive protein (CRP), interleukin (IL), and tumor necrosis factor (TNF) that can cause further organ dysfunction if unchecked. 8,15,16
In spite of the negative consequences of caregiving for persons with ADRD, recent studies have documented the benefits of caregiving. 17 –19 Positive aspects of the caregiving experience may buffer caregivers from negative emotional and physical consequences of caregiving. 18 Caregivers who feel competent or self-efficacious in caring for the person with ADRD have also experienced positive thinking, improved control of negative effect, and enhanced motivation in association with self-efficacy. 18 Personal fulfillment, satisfaction from helping a family member, development of new skills and competencies regarding caregiving, and improved family relationships have also been noted in the caregiving literature. 19
A number of interventions 9,20 –23 have been published that use psychoeducation as a means to help caregivers with their caregiving situation. Psychoeducation, as described by Lukens and McFarlane, 24 is a training method to build skills in family caregivers of persons with psychiatric or mental illness. This type of intervention has been implemented with ADRD caregivers in various settings. 6,20 –23,25,26 These interventions have been found to significantly improve caregiver well-being, thereby reducing caregivers’ levels of clinical depression. 20,21,25,27 A large multicomponent intervention that included psychoeducation as part of the intervention was the Resources for Enhancing Alzheimer’s Caregiver Health II (REACH II) study. 20 Results revealed that caregiver burden or stress decreased, and their quality of life increased significantly due to the intervention. 20 Considering the number of psychoeducational interventions currently available for caregivers, the authors evaluated the impact of an ongoing community-based psychoeducational intervention that targets ADRD caregivers, called the Family Series.
The aim of this study was to evaluate the impact of a “grassroots” community-based psychoeducational intervention, named the Family Series, on caregivers of community-dwelling persons with ADRD. The study sought to determine whether caregivers who attended this intervention (Family Series) would report improved levels in caregiving competence, stress, and coping. This study also sought to examine the impact of this intervention on the relationship between caregiving competence, stress, and coping.
Methods
Caregiving for a person with ADRD is complex. Both negative and positive consequences of caregiving can have an effect on caregiver’s health or well-being as well as their care of the person with ADRD. Given this, the authors chose to use the term caregiver “stress” rather than burden, as it is commonly labeled in the literature. Some caregivers may not perceive caregiving as a burden, but rather as stressful life event. 28 Therefore, “caregiver stress” was used to refer to the negative consequences associated with providing care to a person with ADRD.
Theoretical Framework
The Stress Process Model of Alzheimer’s Caregiving was used as a framework to guide this study. Derived by Pearlin et al, 11 this model postulates that caregiver stress is a consequence of a process, which involves 4 interrelated domains including one’s (1) caregiving background and context of stress, (2) stressors, (3) mediators of stress, and (4) the outcomes or manifestations of stress. Coping is considered a mediator in which individuals employ strategies on their own behalf to help them deal with their caregiving situation. Caregiving competence measures adequacy of the caregiver’s performance as caregivers. Conditions, experiences, and activities that create stress in caregivers are those that threaten them, thwart their efforts, and fatigue them. Overtime, stressors from caregiving can have a negative effect on caregiving and lead to the preinstitutionalization of the person with ADRD and yielding of the caregiving role by the caregiver. 11,14
Community-Based Collaborative Research
The conceptual framework that guided the evaluation of the Family Series workshop intervention, which was synthesized with the current state of the science based on a literature review regarding psychoeducational interventions for caregivers, identified some important concepts. The concepts applied to the aims of the intervention (Family Series) of helping caregivers cope with their caregiving situation, as well as reducing stress (burden) related to caregiving and providing caregivers with the skills needed to adequately care for and avoid preinstitutionalization of the person with ADRD. Interdisciplinary team members of health care professionals from an Alzheimer’s nonprofit organization collaborated with the principal investigator (PI; Llanque) and agreed that these constructs would be the most appropriate constructs to evaluate for the intervention. No other additional measures were employed.
Program inception and subsequent development
The Alzheimer’s nonprofit organization had a long history of providing dementia education to caregivers. This was largely confined to general education provided in either 1 or 2 session workshops that vacillated between overloading caregivers with too much information or reducing information to fit limited time frames and leaving caregivers less prepared. The Family Series intervention breaks up the information provided in reasonable topic-specific doses and expands the amount of time of the intervention and was developed to address those challenges. Moreover, breaking the information up into 6 topic areas enables caregivers to be in more control of what information caregivers’ need or information they are ready to hear. Caregivers have the option of attending only those sessions that relate to their needs. Additionally, the extended series allows rapport building and strengthens support between the participants. Further development of the Family Series workshop’s curriculum development was shaped by clinical experiences of the staff at the Alzheimer’s nonprofit organization and past published studies of evidenced-based programs for caregivers of persons with ADRD.
Participants
Participants for this study were recruited through convenience sampling from caregivers who were interested in attending the Family Series, psychoeducational intervention. The intervention was open to all nonpaid family, friends, and significant others, who self-identified as caregivers of persons with ADRD and who met inclusion criteria for the study. Inclusion criteria limited participation to caregivers who were 18 years of age or older. Caregivers did not have to reside with the person with ADRD; however, they must have provided some support with ADLs or IADLs for a person with ADRD. Exclusion criteria involved inability to read or write English. An Alzheimer’s community service agency advertised the workshop with flyers, an educational calendar, and personal contacts with caregivers during home/office visits with care consultants.
Design and Procedures
Intervention
The Family Series workshop consisted of 6 weekly, 90-minute psychoeducational sessions designed for caregivers of persons with ADRD. Table 1 presents an overview of the workshop curriculum. Table 2 provides details with regard to how each outcome measure was tied to the sessions of this intervention. A health care professional with a minimum of a bachelor’s degree in the area of social work, nursing, gerontology, pharmacy, psychology, or related fields delivered the information and coordinated the sessions. Knowledge of the disease process as well as experience working with persons with ADRD and their caregivers were required of the health care professional. Each session of the Family Series workshop included a lecture with Power Point, discussions, educational handouts, and an open question and answer period at the end. A consulting geriatric pharmacist provided educational information and handouts for the session on medications. The series was adapted from work developed by a local social worker who used methods of community-based participatory research with staff from an Alzheimer’s community service agency. However, the impact of the Family Series workshop had not been formally evaluated.
Table 1.
The Family Series Workshop Curriculum.a
| Session | Topic | Content |
|---|---|---|
| I | What can I expect? | An overview of dementia including diagnosis, stages, and family experiences. |
| II | I don’t need any help | A discussion of managing activities of daily living including task breakdown, provision of care, and other issues associated with bathing, toileting, dressing, taking medication, and feeding. |
| III | He/she just sits around all day | Explores the role of activities and structure for the person with Alzheimer’s disease including suggestions on activities and options to maximize strengths. |
| IV | Is he/she on too many medications? | Discusses the concerns and appropriate benefits of commonly prescribed medications in the care of the person with dementia. |
| V | I can’t do this anymore | Discusses the dilemma and issues around the placement decision. Covers options, resources, and the decision-making process. |
| VI | I should, I ought, I have to… | Covers the guilt that typically goes along with the role of caregiver and the impact of guilt on caregiving. |
aThis table shows the curriculum of the Family Series Workshop psychoeducational intervention as it applies to the key concepts: coping, caregiving competence, and stress. Topics and content covered under each session were written and described by Michelle Niedens, Director of Education, Programs, and Public Policy, at the Alzheimer’s Association, Heart of America Chapter. Adapted with permission (2014) from Michelle Niedens.
Table 2.
Integration of the Stress Process Model With the Family Series Workshop Intervention.
| Session | Coping | Competence | Caregiver Stress |
|---|---|---|---|
| I | Cognitive reframing will help caregiver in their understanding of behavior and memory changes that occur as the disease progresses and will help caregivers cope with impairments caused by dementia. | Provides information regarding pathophysiology of dementia, diagnosis, stages of dementia, prognosis, genetics, risk factors of getting dementia, Alzheimer’s Association’s services, and online resources to help caregivers. | |
| II | Caregivers are able to utilize problem-solving skills while assisting the person with the disease with activities of daily living. Caregivers are able to understand cognitive processes that affect communication skills of the person with dementia. | Caregiving skills discussed regarding techniques in assisting with personal care, bathing, perineal care, pain, psychosis, boredom, paranoia, depression, visual–spatial problems, and communication. Home and community-based resources are discussed. | Caregivers are able to maintain their physical health and stress level (ie, feelings of tiredness, sleep deprivation, feeling sick, and perceived health). |
| III | Engaging in failure-free activities and structuring each day with a routine helps caregivers cope with the disease progression. | Information regarding activity/structure for the person with dementia that caregivers can do during various stages of dementia. Resources such as Adult Day Programs and In-Home Respite are discussed. | Persons with dementia experience slower progression of certain cognitive functions dementia and are able to share memories with the caregiver as they engage in activities. Resources can decrease caregiver stress via respite care, so that the caregiver gets reprieve. |
| IV | Caregivers learns about medications typically prescribed to persons with dementia, as well as the benefits vs negative effects of psychotropic medications prescribed for behavioral problems as dementia progresses. | ||
| V | Discussion on whether long-term care placement is right for the person with dementia and the caregiver. Addresses the management of the caregiving situation, leading to the need for additional care such as in-home respite, assisted living, or nursing home placement. | Information regarding the placement of the care receiver in a long-term care facility is discussed. Options for aging in place are covered. | |
| VI | Caregivers are able to manage the meaning of their caregiving situation such that feelings of guilt are reduced. | A facilitated group discussion about caregiver guilt will take place. Information about how support groups, counseling, or talking with a trusted person about caregiver guilt will be discussed. | Topics related to reducing caregiver stress and using cognitive reframing in relation to the contextual caregiving situation and cognitive status of the care receiver. |
Recruitment
Recruitment flyers were created and disseminated at support groups and other educational programs. The flyers invited and encouraged caregivers to attend the intervention. A notice of the intervention was placed in an annually disseminated education calendar, which advertised upcoming workshops and conference meetings hosted by the Alzheimer’s community agency. Caregivers who met the inclusion criteria and planned to attend the workshop for at least 4 of the 6 sessions were invited to join the study. Study participants completed questionnaires on the first and last day they attended the workshop. In addition, caregivers were asked to add a unique identifier on the pre- and posttests so that the researchers could pair each participant’s data from both assessments. Data for this study were collected March through August 2011.
Retention strategies
Caregivers received reminders regarding upcoming sessions, returning the study questionnaires, and the content that would be covered during each sessions. Another strategy used to increase retention and to express appreciation for participation was to provide caregivers with a voucher for a free book from a library that provided books on dementia.
Human subjects protection
Approval for this study was obtained from the University of Missouri-Kansas City Social Science institutional review board (IRB). A nonprofit Alzheimer’s community service agency served as a community partner for the study and provided a letter of support to the IRB.
Measures
Demographics
A demographic questionnaire was developed to obtain background information from the caregiver about their relationship to the person with ADRD, length of time providing care, living situation, race and ethnicity, age, gender, employment, and education level. Often participants are reluctant to answer questions with regard to personal finances, 29 thus the questionnaire posed the question: “Are you experiencing financial strain?” in order to assess economic status.
Coping
The Brief COPE scale, a 28-item, Likert-type scale, utilized for this study, consists of 14 subscales, with 2 questions for each subscale. Subscales measured self-distraction, active coping, denial, substance abuse, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. 30 Cronbach’s α coefficient is used as a test of internal consistency. A value of .7 to .8 is considered acceptable value for Cronbach’s α. 31,32 Cronbach’s α scores for the 14 subscales ranged from .57 to .90. Participants rated their frequency of using a particular coping style on a scale ranging from 1 (I haven’t been doing this at all) to 4 (I’ve been doing this a lot). Possible scores on this instrument range between 28 points (lowest score) and 112 points (highest score).
Caregiving competence
Caregiving competence was evaluated using the 4-item caregiving competence scale. 11 The items in the scale inquired into one’s confidence in their ability to address the demands of caregiving. The responses to each item ranged from 1 (not at all) to 4 (very much) that are summed for a possible total score that can range from 4 to 16, where a higher score indicates greater competence. Internal consistency for this instrument was α = .74 after psychometric testing. 11
Caregiver Burden Inventory
The modified Caregiver Burden Inventory (CBI) assessed the multidimensional aspects of caregiver stress. 33,34 Participants’ CBI scores may range from 0 to 96 points. Scores near or above 36 points appear to reflect caregiver burnout and the need for assistance. Psychometric testing has shown that the Cronbach’s α for this measure ranged from .69 to .87. 33 The scores for this instrument were reverse coded. Higher score for an item would reflect a low level of stress, and a low score would reflect a high level of stress.
Statistical Analysis
Data analyses were performed using the SPSS 18.0 for Windows and Statistical Analysis System (SAS) 9.2. 35,36 The α level for significance tests was set at .05. Paired t tests with random effect assessed caregiving competence, stress, and coping, from baseline to postintervention. Random effect was used to account for any differences on outcome measures due to site (ie, the 3 different recruitment sites). Missing data were imputed through mean substitution. Minimal data collected were missing, which included 2 participant cases. According to Munro, 37 mean substitution has the advantage of being easily implemented and provides all cases with complete data. An a priori power analysis determined that a power of .80, with a moderate effect size of .50 and a 1-sided, paired t test required a minimum of 34 participants for this study. 37 Additionally, regression analysis with random effect for site differences was utilized to examine the impact of the intervention on the relationship between caregiving competence, stress, and coping.
Results
Table 3 displays the demographic characteristics of the study participants. A total of 35 caregivers of persons with ADRD completed the baseline and postintervention questionnaires from the 3 workshop sites. The majority of participants were female (n = 23, 65.7%), caucasian (N = 35), middle aged (M = 62.7 years old), and had been caregiving for over 2 years (n = 21; 60%). Many of the participants self-reported experiencing no financial strain (68.6%, n = 24). Overall, the majority of participants were well-educated, wherein 83% had at least some college background, including more than half who were college graduates (terminal bachelor’s degree, n = 11, 31.4%; postgraduate, n = 8, 22.9%). Caregivers were asked to identify the current stage of dementia they believed the care receiver was at during the time of the study. This information was important to demonstrate that caregiver’s caring for a person with ADRD at any phase of dementia living in the community could benefit from this intervention. Caregivers rated the care receiver as follows: early (40%, n = 14), middle (40%, n = 14), late (17.1%, n = 6), and unknown (2.9%, n = 1), refer to Table 3. Adherence to the intervention by caregivers is depicted in Table 4. Over 82% of participants attended all 6 sessions of the intervention.
Table 3.
Participants’ Demographic Characteristics by Recruitment Site.
| Variable | f (%) |
|---|---|
| Sample size | N = 35 |
| Average age (SD) | 62.7 (13.6) |
| Ethnicity | |
| Hispanic | 1 (2.9) |
| Non-Hispanic | 34 (97.1) |
| Race | |
| Caucasian | 35 (100) |
| Gender | |
| Male | 12 (34.3) |
| Female | 23 (65.7) |
| Employment | |
| Full-time | 11 (31.4) |
| Part-time | 3 (8.6) |
| As needed | 3 (8.6) |
| Not employed | 18 (51.4) |
| Caregiver relationship to care receiver | |
| Spouse | 18 (51.4) |
| Parent | 2 (5.7) |
| Child | 9 (25.7) |
| In-law | 2 (5.7) |
| Friend | 3 (8.6) |
| Other relative | 1 (2.9) |
| Length of caregiving | |
| Less than 6 months | 7 (20.0) |
| 6 months to 1 year | 4 (11.4) |
| 1-2 years | 3 (8.6) |
| Over 2 years | 21 (60.0) |
| Residence of person with dementia | |
| Living with the caregiver | 22 (62.9) |
| Living with other family members | 4 (11.4) |
| Living with other persons | 4 (11.4) |
| Live alone | 5 (14.3) |
| Education level | |
| High school/GED | 6 (17.1) |
| Some college | 10 (28.6) |
| College graduate | 11 (31.4) |
| Graduate education | 8 (22.9) |
| Caregivers experiencing financial strain | |
| Yes | 8 (22.9) |
| No | 24 (68.6) |
| Preferred not to answer the question | 3 (8.6) |
| Dementia type | |
| Alzheimer’s disease | 26 (74.3) |
| Mild cognitive impairment | 1 (2.9) |
| Parkinson’s disease dementia | 1 (2.9) |
| Traumatic brain injury | 2 (5.7) |
| Normal pressure hydrocephalus | 1 (2.9) |
| Unknown | 4 (11.4) |
| Stage of dementia | |
| Early | 14 (40.0) |
| Middle | 14 (40.0) |
| Late | 6 (17.1) |
| Unknown | 1 (2.9) |
Abbreviations: GED, general equivalency diploma; SD, standard deviation.
Table 4.
Participation of Caregivers by Group in Each Workshop Session.
| Groups | Session 1 | Session 2 | Session 3 | Session 4 | Session 5 | Session 6 |
|---|---|---|---|---|---|---|
| Group 1 (n = 14) | 12 | 12 | 13 | 13 | 13 | 9 |
| Group 2 (n = 10) | 9 | 10 | 10 | 9 | 10 | 9 |
| Group 3 (n = 11) | 9 | 10 | 11 | 9 | 10 | 8 |
The mean scores of all measures (ie, caregiving competence, stress, and coping levels) changed in the clinically desired direction from baseline to postintervention are represented in Figure 1. Paired t test with random effect for all recruitment sites was used to examine mean changes in measures of caregiving competence and stress levels from baseline to postintervention found in Table 5. Caregiving competence scores significantly improved (P = .0358; t = 5.14) by 3 points, from an average of 11.6 at baseline to 14.6 (standard deviation [SD] = 1.9) postintervention. The mean scores of caregiver stress improved slightly from baseline at 20.7 points to 21.2 at postintervention. In spite of a 0.5 improvement in stress scores from baseline to postintervention, this improvement was not significant (P = .7081; t = 0.43).
Figure 1.
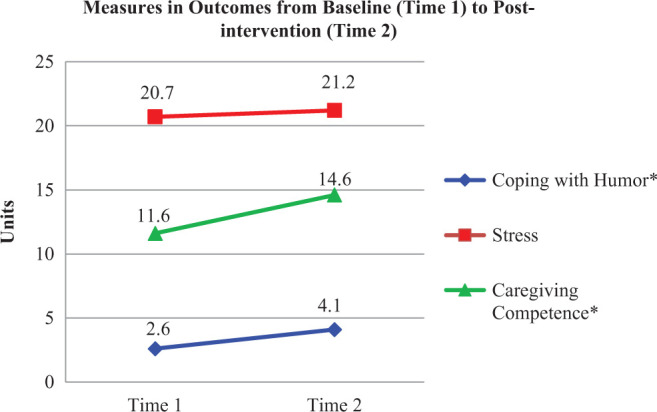
Change in mean outcome score of coping subscale humor, stress, and caregiving competence levels.
Table 5.
Summary for Paired t Tests With Random Effect Analysis Results.a
| Measures | Estimate | SE | df | t | P |
|---|---|---|---|---|---|
| Caregiving competence | 2.9429 | 0.5724 | 2 | 5.14 | .0358b |
| Stress | 0.5294 | 1.2267 | 2 | 0.43 | .7081 |
Abbreviation: SE, standard error.
aN = 35.
b P < .05.
Additionally, 14 subscales of the Brief COPE instrument were analyzed separately as recommended by Carver. 30 Using an aggregate coping mean score of all the subscales is not recommended, since there is no particular way of generating a dominant coping style for participants. 30 The coping with humor subscale consisted of a total of 2 items. For each item, the responses ranged from 1 (I haven’t been doing this at all) to 4 (I’ve been doing this a lot). Ergo, for this particular subscale, the range of possible points were from 2 to 8 points. The authors found that the coping subscale of humor produced mean scores from an average baseline of 2.6 (SD = 1.0) to 4.1 (SD = 2.2) at postintervention (P = .0493; t = 4.34). Although a change in mean total scores on the humor subscale ranged from 2.6 to 4.1 with a P value of .0493 may be statistically significant, this may not be clinically significant. Since this is a pilot study with small sample size, Bonferroni correction for multiple tests was not conducted. 38 –40 Bonferroni correction is known for being conservative and reduces statistical power. 37 However, this finding may be worth studying in future studies with a larger sample size to see whether humor does play a greater role in easing the encumbrance of caregiving. The following coping subscales approached significance: positive reframing (P = .0575; t = 3.99), religion (P = .0802; t = 3.32), self-distracting (P = .0613; t = 3.85), and venting (P = .0941; t = 3.03). Table 5 provides a visual depiction of the significant and nonsignificant changes for the outcome measures of the coping subscales.
As shown in Table 6, separate regression analyses were used to account for site differences and to analyze the relationship between the measures coping with humor subscale, caregiving competence, and stress. Since the intervention had a marginally significant effect on coping with humor subscale mean scores, the authors analyzed stress and the coping with humor subscale, separately, to see whether both stress and coping with humor were predictors of caregiving competence. As seen in Table 7, the coping subscale with humor (P = .0015; t = 3.51) in conjunction with stress (P = .0062; t = 2.95) were significant predictors of caregiving competence. Figure 2 depicts the final model illustrating intervention’s effect on caregiving competence, stress, and coping.
Table 6.
Significant Values for Coping Subscales From Baseline to Postintervention.a
| Coping Subscale | Estimate | Standard Error | df | t Value | P Value |
|---|---|---|---|---|---|
| 1. Self-distraction | 1.2000 | 0.3117 | 2 | 3.85 | .0613 |
| 2. Active coping | 1.1272 | 0.3908 | 2 | 2.88 | .1021 |
| 3. Denial | 0.9339 | 0.3347 | 2 | 2.79 | .1080 |
| 4. Substance use | −0.2286 | 0.1302 | 2 | −1.76 | .2212 |
| 5. Emotional support | 1.5170 | 0.6310 | 2 | 2.40 | .1381 |
| 6. Behavioral disengagement | 0.3143 | 0.2160 | 2 | 1.45 | .2830 |
| 7. Venting | 1.5258 | 0.5043 | 2 | 3.03 | .0941 |
| 8. Use of instrumental support | 1.4557 | 0.5827 | 2 | 2.50 | .1298 |
| 9. Positive reframing | 1.4286 | 0.3581 | 2 | 3.99 | .0575 |
| 10. Self-blame | 0.1447 | 0.2812 | 2 | 0.51 | .6581 |
| 11. Planning | 1.0936 | 0.4107 | 2 | 2.66 | .1168 |
| 12. Humor | 1.5429 | 0.3558 | 2 | 4.34 | .0493 |
| 13. Acceptance | 0.8000 | 0.2893 | 2 | 2.77 | .1097 |
| 14. Religion | 1.4086 | 0.4248 | 2 | 3.32 | .0802 |
aN = 35.
Table 7.
Caregiving Competence as Related to Caregiver Stress and Coping With Humor Subscale.a
| Effect | Estimate | Standard Error | df | t Value | P Value |
|---|---|---|---|---|---|
| Intercept | 1.5933 | 0.6111 | 2 | 2.61 | .1210 |
| Caregiver stress | 0.2038 | 0.06905 | 29 | 2.95 | .0062b |
| Coping with humor | 0.8177 | 0.2331 | 29 | 3.51 | .0015b |
aN = 35.
b P < .05.
Figure 2.
Final model.
Discussion
The aim of this study was to examine the impact of a community-based psychoeducational intervention, the Family Series workshop, involving caregivers of persons with dementia. The intervention had a significant positive effect on caregiving competence. Caregivers’ understanding of information and knowledge regarding how to provide care for the person with ADRD improved after participating in the intervention (P = .0358). Past studies that evaluated the impact of psychoeducational interventions on caregiving competence have shown mixed results as to whether caregiving competence improved postintervention. 41,42
The intervention had a marginal, positive impact on coping with humor levels of caregivers. Past findings from other caregiving interventions 43 –45 have shown mixed results with regard to whether coping significantly increased among caregivers of persons with ADRD. Moreover, further regression analysis showed that positive reframing, religion, and self-distracting and venting subscales approached significance in this study. However, since the sample size was small (N = 35), the authors were unable to determine whether these subscales for coping had a significant impact on caregiver’s coping style after participating in the intervention. Future studies should include larger samples to better determine the nature of these relationships.
Caregiver stress levels (as assessed by the CBI) did not appear to appreciably change from baseline to postintervention, based on the statistical analyses. This finding is not surprising, given that caring for a person with a chronic and incurable illness such as dementia can lead not only to acute but also to chronic stress. Although the activation of the stress response, in most cases, is a beneficial process that helps to preserve organ integrity, 46 it is now established that chronic stress leads to the accumulation of inflammatory molecules (ie, CRP, ILs, and TNF) that lead to negative physiological consequences such as hypertension, depressed immune system, and abdominal obesity, just to name a few. 47,48
The relationship between coping with humor and stress on caregiving competence was examined in this study. The authors analyzed stress and the coping subscale humor, separately, to see whether both stress and coping with humor were predictors of caregiving competence. Coping with humor, in conjunction with improved stress levels, was significant predictors of caregiving competence. This means that as stress improves by 1 point (lower stress), caregiving competence will improve (increased) by 0.2038 points. Similarly, as coping with humor improves by 1 point, caregiving competence will improve by 0.8177 points.
These findings may suggest that coping with humor and stress could be important components of the caregiving process. In hindsight, having a qualitative portion to this study would have provided more insights as to why “coping using humor” significantly improved based on this intervention study. Although there have been psychoeducation interventions studies, which have evaluated coping, 43,45 findings have not specifically evaluated coping with humor. Other studies 49 –52 have indicated that humor may be beneficial for caregiving coping with the stress of caregiving. Further research in this area could provide researchers and clinicians with an evidenced-based intervention such as using humor to assist caregivers to cope with caring for the person with ADRD.
The authors utilized Pearlin et al’s Stress Process Model of Alzheimer’s Caregiving 11 to guide this study, which purports that coping represents behaviors and practices which caregivers use in response to life’s problems. A function of coping is managing stressful caregiving situations as well as the symptoms that may rise from the situation. Coping, in this study, was considered a mediator of caregiver competence. The intervention appears to have a nominal or modest influence on 1 form of coping (using humor) on caregiving competence as seen in Figure 2. Although, the results of this study did not show a significant correlation between coping and stress, findings did suggest that improved caregiver stress levels was positively associated with an increase in caregiving competence of caregivers.
The study sample mainly consisted of caucasian, non-Hispanic caregivers. According to the Administration on Aging, 53 the number of minority elders is expected to increase exponentially, which places them at risk (due to age) of ADRD. With this increase, a greater number of minority caregivers can also be expected. Henceforward, future research should include a larger sample size that is diverse and inclusive of individuals from minority, underrepresented populations.
Caregivers in this study benefited from an intervention that provided psychoeducation about caregiving for a person with ADRD at various stages of the disease. Tailoring this community-based intervention for caregivers of those having other chronic illnesses could yield positive outcomes. Using a community-based participatory research (CBPR) methodology has been helpful in community-based and grassroots studies in implementing intervention in the community, creating community capacity, and empowering participants to take ownership of the intervention so it may continue on after researchers leave the setting. 54 Additionally, both the National Institutes of Health/National Institute of Nursing Research and the Patient Centered Outcomes Research Institute are encouraging community engagement in intervention research studies they sponsor to reduce health disparities in populations. 55,56
Limitations
Although the results of this study were encouraging, there were limitations. The study used a 1-group, pretest–posttest study design with no comparison group or long-term follow-up. Additional considerations of this study concern time constraints of participants, which may have affected participation in this study. More specifically, if there were fewer time constraints for the caregivers; more sessions may have been attended. Thus, the greater likelihood of treatment effects on stress, coping, and competence levels of the caregivers.
Although the Family Series Workshop included an interactive question and answer forum at the end of the lecture, this study did not formally evaluate ways in which participants applied newly acquired knowledge such as role playing or homework assignments. Past studies have shown that activities such as role play or homework can be effective and enhance the experience of participants partaking in psychoeducational interventions. 57,58 However, due to time, costs, and logistical issues, these cognitive-behavioral activities were not formally evaluated in this intervention.
Recruiting participants for this study was a challenge considering that each caregiver came with unique needs to the intervention and had time constraints. The sample size was small, and a convenience sampling technique was utilized. Additionally, there were few males and persons of color who participated in this study. Past research has shown that low numbers of males participate in caregiving interventions and they often drop out of studies and do not show the same evidence outcomes as females. 59 –61
It is predicted that the ADRD population will be more ethnically and racially diverse in the next 35 years, given the increased risk of acquiring ADRD in African Americans and Hispanics older adults. 1 Efforts to recruit a more diverse caregiver sample should be considered in future studies. Measures used in this study were self-report. Future studies, if practical, could use more objective assessments such as using biomarkers (eg, CRP, IL, TNF, and cortisol levels) to evaluate not only the immediate stress levels but also whether allostasis itself has been compromised.
Given that this intervention was implemented in groups, the authors did not evaluate the effects of social support on participants. Interventions conducted in a group setting are effective in increasing caregivers’ social network, which in turn could have a positive effect on social support. 24,62 Social support, in relation to the Stress Process Model of Alzheimer’s Caregiving, 11 is considered a mediator. Hence measuring social support could have provided additional insight in evaluating the success of this intervention.
Conclusion
Caregiving competence increased in participants who participated in this psychoeducational intervention, the Family Series workshop, with as little as 4 sessions. Caregiver stress was not statistically significant from baseline to postintervention. However, caregivers’ use of humor as a coping strategy was shown to have improved in terms of statistical significance, despite the small change in coping with humor scores from pre- to postintervention. The clinical significance of this result may be minute as this result may not explain existing information about the participants or provide useful direction for improving the intervention in future studies. In spite of this, other findings suggest that a community-based psychoeducational intervention framed by the Stress Process Model of Alzheimer’s Caregiving 11 has the potential to positively impact caregiver’s competence in their role as a caregiver. Such an intervention provides a resource for AD caregivers at various stages of the disease process.
Future studies should enlist a research design with added rigor and could include an additional qualitative methodological component, as well a broader model of chronic stress and its health consequences. This design could provide a better understanding of the impact of the Family Series workshop intervention and a more in-depth perspective from both the caregiver and the person with dementia. Broadening of these concepts and their understanding, together with the biological validation through the use of biomarkers, could potentially lead to more effective interventions. Furthermore, a larger sample size that is diverse and inclusive of individuals from minority and underrepresented populations is needed to strengthen the study.
There is something to be said about examining interventions that currently “work“ in the community. This study is novel in that it evaluated an on-going community-based psychoeducational program that had been implemented, since 2006, by a nonprofit Alzheimer’s agency and targeted family caregivers of persons with ADRD. This program was not formally evaluated using rigorous research methods due to time constraints and lack of research support. The first author (PI) was a doctoral student with a clinical background in the nursing care of older adults with ADRD and their caregivers. After hearing positive comments from caregivers regarding the program and talking with Alzheimer’s professionals, it was mutually agreed upon to evaluate the effects of the Family Series program on caregiver’s health. However for purposes of this study, the authors were unable to gather follow-up data and assess the existing agency’s resources to support the continued efforts.
Community agencies are a major stakeholder in the delivery of caregiving programs and providing services to community-dwelling persons with dementia and their family caregivers. Partnering with an Alzheimer’s community-based agency to evaluate this psychoeducational intervention has provided a unique way to evaluate and disseminate what “works” in the field. Although there have been a number of psychoeducation interventions targeting caregivers of persons with ADRD, 9,20,21,23,26 the literature is scant with studies that have evaluated “grassroots” community-based psychoeducational interventions. Few evidenced-based programs have been translated into the community setting. 63,64 This study provides insights into the implementation and evaluation of a community-based psychoeducational intervention. The PI and the Alzheimer’s nonprofit organization are planning on disseminating this intervention via a web site to make it available to other community-based organizations working with caregivers of persons of persons with ADRD.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a micro-grant from the Paul Ambrose Scholar’s Program, and a grant from the University of Missouri-Kansas City (UMKC) Women’s Council Fellowships, Irene Campbell Anderson Award and Mrs. Otto W. (Clara) Knutson Award. Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number T32NR013456 (PIs: Susie Beck, PhD, RN, FAAN, Ginny Pepper, PhD, RN, FAAN). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors extend gratitude to those caregivers who participated in this study. The authors would like to thank the Alzheimer’s Association, Heart of American Chapter, for their help and support with this study.
References
- 1. Alzheimer’s Association. 2014 Alzheimer’s disease facts and figures. 2014. Web site. http://www.alz.org/downloads/facts_figures_2014.pdf. Accessed January 7, 2015. [DOI] [PubMed]
- 2. Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7 (3):270–279. doi:10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jack CR, Albert MS, Knopman DS, et al. Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7 (3):257–262. doi:10.1016/j.jalz.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7 (3):263–269. doi:10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Institute of Neurological Disorders and Stroke (NINDS). Dementia: Hope through research; 2010. Web site. http://www.ninds.nih.gov/disorders/dementias/detail_dementia.htm. Accessed April 22, 2014.
- 6. Martín-Carrasco M, Martín MF, Valero CP, et al. Effectiveness of a psychoeducational intervention program in the reduction of caregiver burden in Alzheimer’s disease patients’ caregivers. Int J Geriatr Psychiatry. 2009;24 (5):489–499. doi:10.1002/gps.2142. [DOI] [PubMed] [Google Scholar]
- 7. Schulz R, Martire LM. Family caregiving of persons with dementia: prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12 (3):240–249. doi:10.1097/00019442-200405000-00002. [PubMed] [Google Scholar]
- 8. Von Känel R, Mills PJ, Mausbach BT, et al. Effect of Alzheimer caregiving on circulating levels of C-reactive protein and other biomarkers relevant to cardiovascular disease risk: a longitudinal study. Gerontology. 2012;58 (4):354–365. doi:10.1159/000334219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Parker D, Mills S, Abbey J. Effectiveness of interventions that assist caregivers to support people with dementia living in the community: a systematic review. Int J Evid Based Healthc. 2008;6 (2):137–172. doi:10.1111/j.1744-1609.2008.00090.x. [DOI] [PubMed] [Google Scholar]
- 10. Melillo KD, Houde SC. Geropsychiatric and Mental Health Nursing. 2nd ed. Sudbury, MA: Jones & Bartlett Learning; 2010. [Google Scholar]
- 11. Pearlin LI, Mullan JT, Semple SJ, Skaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist. 1990;30 (5):583–594. [DOI] [PubMed] [Google Scholar]
- 12. Kiecolt-Glaser JK, Preacher KJ, et al. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc Natl Acad Sci USA. 2003;100 (15):9090–9095. doi:10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129 (6):946–972. doi:10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 14. Brame AL, Singer M. Stressing the obvious? An allostatic look at critical illness. Crit Care Med. 2010;38 (10 suppl): s600–s607. doi:10.1097/CCM.0b013e3181f23e92. [DOI] [PubMed] [Google Scholar]
- 15. Lovell B, Wetherell MA. The cost of caregiving: endocrine and immune implications in elderly and non elderly caregivers. Neurosci Biobehav Rev. 2011;35 (6):1342–1352. doi:10.1016/j.neubiorev.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 16. Cheng K-C, Chiu Y-C, Lee Y-N, Liao S-K, Lee S-H. Relationships between stress perception and stress biomarkers in family caregivers. Hu Li Za Zhi. 2011;58 (3):43–52. [PubMed] [Google Scholar]
- 17. Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, Gallagher-Thompson D. Positive aspects of caregiving. Res Aging. 2004;26 (4):429–453. doi:10.1177/0164027504264493. [Google Scholar]
- 18. Semiatin AM, O’Connor MK. The relationship between self-efficacy and positive aspects of caregiving in Alzheimer’s disease caregivers. Aging Ment Health. 2012;16(6):683–688. doi:10.1080/13607863.2011.651437. [DOI] [PubMed] [Google Scholar]
- 19. Carbonneau H, Caron C, Desrosiers J. Development of a conceptual framework of positive aspects of caregiving in. Dementia. 2010;9(3):327–353. doi:10.1177/1471301210375316. [Google Scholar]
- 20. Belle SH, Burgio L, Burns R, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145 (10):727–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Selwood A, Johnston K, Katona C, Lyketsos C, Livingston G. Systematic review of the effect of psychological interventions on family caregivers of people with dementia. J Affect Disord. 2007;101 (1-3):75–89. doi:10.1016/j.jad.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 22. Gallagher-Thompson D, Wang P-C, Liu W, et al. Effectiveness of a psychoeducational skill training DVD program to reduce stress in Chinese American dementia caregivers: results of a preliminary study. Aging Amp Ment Health. 2010;14 (3):263–273. doi:10.1080/13607860903420989. [DOI] [PubMed] [Google Scholar]
- 23. Gonyea JG, O’Connor MK, Boyle PA. Project CARE: a randomized controlled trial of a behavioral intervention group for Alzheimer’s disease caregivers. Gerontologist. 2006;46 (6):827–832. doi:10.1093/geront/46.6.827. [DOI] [PubMed] [Google Scholar]
- 24. Lukens EP, McFarlane WR. Psychoeducation as evidence-based practice: considerations for practice, research, and policy. Brief Treat Crisis Interv. 2004;4 (3):205. doi:10.1093/brief-treatment/mhh019. [Google Scholar]
- 25. Gallagher-Thompson D, Gray HL, Dupart T, Jimenez D, Thompson LW. Effectiveness of cognitive/behavioral small group intervention for reduction of depression and stress in non-Hispanic white and Hispanic/Latino women dementia family caregivers: outcomes and mediators of change. J Ration-Emotive Cogn-Behav Ther. 2008;26 (4):286–303. doi:10.1007/s10942-008-0087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tompkins SA, Bell PA. Examination of a psychoeducational intervention and a respite grant in relieving psychosocial stressors associated with being an Alzheimer’s caregiver. J Gerontol Soc Work. 2009;52 (2):89–104. doi:10.1080/01634370802561877. [DOI] [PubMed] [Google Scholar]
- 27. Martín-Carrasco M, Martín MF, Valero CP, et al. Effectiveness of a psychoeducational intervention program in the reduction of caregiver burden in Alzheimer’s disease patients’ caregivers. Int J Geriatr Psychiatry. 2009;24 (5):489–499. doi:10.1002/gps.2142. [DOI] [PubMed] [Google Scholar]
- 28. Arevalo-Flechas LC. A hard job done with love: caregiving is neither a burden nor a carga for Hispanic caregivers. In: Interdisciplinary Research: A Road More or Less Traveled. Baltimore, MD: Southern Nursing Research Society; 2009. Web site. http://snrs.org/publications/SOJNR_articles2/Vol09Num02SupplementA.html#ArevaloFlechas. Accessed April 22, 2014. [Google Scholar]
- 29. Finlayson M. Changes predicting long-term care use among the oldest–old. Gerontologist. 2002;42 (4):443–453. [DOI] [PubMed] [Google Scholar]
- 30. Carver CS. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med. 1997;4 (1):92–100. doi:10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 31. Field A. Discovering Statistics Using IBM SPSS Statistics. 4th ed. London: SAGE Publications Ltd; 2013. [Google Scholar]
- 32. Pallant J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS. 5 Spi ed. Milton Keynes: Open University Press; 2013. [Google Scholar]
- 33. Caserta MS, Lund DA, Wright SD. Exploring the Caregiver Burden Inventory (CBI): further evidence for a multidimensional view of burden. Int J Aging Hum Dev. 1996;43 (1):21–34. [DOI] [PubMed] [Google Scholar]
- 34. Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29 (6):798–803. [DOI] [PubMed] [Google Scholar]
- 35. SAS Institute Inc. Statistical Analysis System (Version 9.2). Cary, NC: SAS Institute Inc.; 2008. [Google Scholar]
- 36. SPSS Inc. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.; 2009. [Google Scholar]
- 37. Munro BH. Statistical Methods for Health Care Research. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 38. Perneger TV. What’s wrong with Bonferroni adjustments. Br Med J. 1998;316 (7139):1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34 (5):502–508. doi:10.1111/opo.12131. [DOI] [PubMed] [Google Scholar]
- 40. Nakagawa S. A farewell to Bonferroni: the problems of low statistical power and publication bias. Behav Ecol. 2004;15 (6):1044–1045. doi:10.1093/beheco/arh107. [Google Scholar]
- 41. Hepburn KW, Lewis M, Sherman CW, Tornatore J. The Savvy caregiver program: developing and testing a transportable dementia family caregiver training program. Gerontologist. 2003;43 (6):908–915. doi:10.1093/geront/43.6.908. [DOI] [PubMed] [Google Scholar]
- 42. Morano CL, Bravo M. A psychoeducational model for Hispanic Alzheimer’s disease caregivers. Gerontologist. 2002;42 (1):122–126. doi:10.1093/geront/42.1.122. [DOI] [PubMed] [Google Scholar]
- 43. Chiverton P, Caine ED. Education to assist spouses in coping with Alzheimer’s disease. A controlled trial. J Am Geriatr Soc. 1989;37 (7):593–598. [DOI] [PubMed] [Google Scholar]
- 44. Ducharme F, Lévesque L, Lachance L, Giroux F, Legault A, Préville M. “Taking Care of Myself”: Efficacy of an intervention programme for caregivers of a relative with dementia living in a long-term care setting. Dementia. 2005;4 (1):23–47. doi:10.1177/1471301205049189. [Google Scholar]
- 45. Gallagher-Thompson D, Coon DW, Solano N, Ambler C, Rabinowitz Y, Thompson LW. Change in indices of distress among Latino and Anglo female caregivers of elderly relatives with dementia: site-specific results from the REACH national collaborative study. Gerontologist. 2003;43 (4):580–591. [DOI] [PubMed] [Google Scholar]
- 46. Dünser MW, Hasibeder WR. Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med. 2009;24 (5):293–316. doi:10.1177/0885066609340519. [DOI] [PubMed] [Google Scholar]
- 47. Kang D-H, Rice M, Park N-J, Turner-Henson A, Downs C. Stress and inflammation: a biobehavioral approach for nursing research. West J Nurs Res. 2010;32 (6):730–760. doi:10.1177/0193945909356556. [DOI] [PubMed] [Google Scholar]
- 48. McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003;43 (1):2–15. doi:10.1016/S0018-506X(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 49. Buffum MD, Brod M. Humor and well-being in spouse caregivers of patients with Alzheimer’s disease. Appl Nurs Res. 1998;11 (1):12–18. [DOI] [PubMed] [Google Scholar]
- 50. Lovelace LM. The Effect of Coping Strategies on Burden Among Male Alzheimer’s Caregivers; 2012. Web site. http://etd.lsu.edu/docs/available/etd-04262012-170458/unrestricted/Lovelace_Thesis.pdf. Accessed January 7, 2015. [DOI] [PMC free article] [PubMed]
- 51. National Institute on Aging. Coping With Emotions and Stress in Alzheimer’s Caregiving: A Resource List. Bethesda, MD: National Institute on Aging; 2011. Web site. http://www.nia.nih.gov/alzheimers/coping-emotions-and-stress-alzheimers-caregiving-resource-list. Accessed April 22, 2014. [Google Scholar]
- 52. Tan T, Schneider MA. Humor as a coping strategy for adult-child caregivers of individuals with Alzheimer’s disease. Geriatr Nurs. 2009;30 (6):397–408. doi:10.1016/j.gerinurse.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 53. Administration on Aging. Minority aging; 2011. Web site: http://www.aoa.gov/AoARoot/Aging_Statistics/Minority_Aging/index.aspx. Accessed January 7, 2015.
- 54. Kelly PJ. Practical suggestions for community interventions using participatory action research. Public Health Nurs. 2005;22 (1):65–73. doi:10.1111/j.0737-1209.2005.22110.x. [DOI] [PubMed] [Google Scholar]
- 55. Burke JG, Jones J, Yonas M, et al. PCOR, CER, and CBPR: alphabet soup or complementary fields of health research? CTS Clin Transl Sci. 2013;6 (6):493–496. doi:10.1111/cts.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cotton P. Update on health disparities; 2010. Web site. https://www.ninr.nih.gov/aboutninr/nacnr/council-minutes-sept-2010. Published September 14-15, 2010. Updated May 4, 2012. Accessed January 7, 2015.
- 57. Authier J. The psychoeducational model. Can Couns. 1977;12 (1):15–20. [Google Scholar]
- 58. Sörensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontologist. 2002;42 (3):356–372. [DOI] [PubMed] [Google Scholar]
- 59. Gitlin LN. Assessing the state of translation work in caregiving. Paper presented at: Gerontological Society of America’s 66th Annual Scientific Meeting, 2013 Caregiving Pre-Conference Workshop: Family Caregiving to Persons with Dementia; November 20, 2013; New Orleans, Louisiana. [Google Scholar]
- 60. Lloyd J. Men’s role in helping women with Alzheimer’s, dementia soars. USA Today. 2012. Web site. http://usatoday30.usatoday.com/news/health/story/2012-08-21/male-caregivers-alzheimers/57195524/1. Published August 12, 2012. Updated August 22, 2012. Accessed January 7, 2015.
- 61. Maslow K. Translating innovation to impact: evidence-based interventions to support people with Alzheimer’s disease and their caregivers at home and in the community; 2012. Web site. http://www.agingresearch.org/files/21732_file_AoA_White_Paper_Compliant_Version.pdf. Published September 2012. Accessed January 7, 2015.
- 62. Smerglia VL, Miller NB, Sotnak DL, Geiss CA. Social support and adjustment to caring for elder family members: a multi-study analysis. Aging Ment Health. 2007;11 (2):205–217. doi:10.1080/13607860600844515. [DOI] [PubMed] [Google Scholar]
- 63. Burgio LD, Collins IB, Schmid B, Wharton T, McCallum D, Decoster J. Translating the REACH caregiver intervention for use by area agency on aging personnel: the REACH OUT program. Gerontologist. 2009;49 (1):103–116. doi:10.1093/geront/gnp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Stevens AB. Example of current translational work. Paper presented at: Gerontological Society of America’s 66th Annual Scientific Meeting, 2013 Caregiving Pre-Conference Workshop: Family Caregiving to Persons With Dementia; November 2013; New Orleans, LA. [Google Scholar]



