Abstract
Stigma is a prevalent risk factor challenging the health and well-being of children from marginalized groups. One potential protective factor for such children is resilience—one’s capability to adapt flexibly, persistently, and resourcefully to stressful situations. This study investigated the associations among stigma, resilience, and hypothalamic-pituitary-adrenal (HPA) axis function in a sample of 645 youth affected by parental HIV. Perceived stigmatization was associated with lower cortisol levels at awakening and flatter cortisol slopes, whereas resilience was independently associated with higher levels of salivary cortisol at awakening and steeper cortisol slopes. We found evidence for an indirect effect of resilience on diurnal cortisol through lower perceived stigma. These associations remained significant after controlling for demographic and health factors and stressful life events. Our findings demonstrate that perceived stigma and resilience are associated with HPA axis functioning in childhood. Broadly, the data suggest that resilience-promoting and stigma-reducing efforts should be considered to improve the health of children from disadvantaged groups.
Keywords: Stigma, Resilience, Salivary Cortisol, Children, Parental HIV
Stigma has negative and far-reaching effects on those who experience it. In the short term, stigma can adversely affect people’s feelings, thoughts, and behaviors. Cumulatively, it can negatively influence one’s mental and physical health (Benetti & Kambouropoulos, 2006; Pascoe & Richman, 2009; Schmitt, Branscombe, Postmes, & Garcia, 2014). For children whose parents are living with HIV, perceived stigma is a salient stressor (Chi & Li, 2013). Although many studies have demonstrated the deleterious effect of stigma on the psychosocial well-being of these children (e.g., Chi, Li, Zhao, & Zhao, 2014), little is known about how perceived stigma may influence underlying physiologic processes that are associated with health. Conversely, resilience, defined as an individual’s capability to adapt flexibly, persistently, and resourcefully to adverse situations (Connor & Davidson, 2003), is suggested to be associated with better health outcomes. The purpose of this investigation is to examine the associations among perceived stigma, resilience and diurnal cortisol in children whose parents are living with HIV.
Stigma against people living with HIV involves physical rejection and social exclusion derived from the fear of infection and moral judgments on behaviors perceived to be associated with HIV infection such as drug use, commercial sex, and homosexual behaviors (Chi et al., 2014). These stigmatizing perceptions are not just limited to HIV patients, but also extend to their children. Children of parents with HIV report experiencing humiliation, rejection by peers, neglect from family members, and reduced social support (Cluver, Gardner, & Operario, 2008). Further, perceived stigma is associated with internalizing and externalizing problems among these children (Chi et al., 2014; Cluver et al., 2008). However, the extent to which the negative impact of perceived stigma “gets under the skin” to affect children’s physical health and health-related biology is unknown.
People in stigmatized groups are at a greater risk for mental and physical health problems, including depression, hypertension, and coronary heart disease (Major & O’Brien, 2005). Prior work suggests that stigma affects health by exposing individuals to physical and social settings that are more disadvantageous. For example, stigmatized individuals may suffer from limited educational opportunities and may be deprived of access to quality health care (Schmitt et al., 2014). Stigma can also affect health through engagement in unhealthy behaviors as maladaptive responses to coping with stigma (Klonoff, 2014). In addition, various cognitions and emotions associated with stigma such as being excluded, avoided, ignored and treated with less respect may lead to negative health outcomes (Fuller-Rowell, Doan, & Eccles, 2012). It has been argued that the subjective perception and interpretation of stigma—compared with objective encounters with stigma—may have unique consequences for an individual’s health (Schmitt et al., 2014). Indeed, individuals experiencing high perceived stigma show greater cardiovascular reactivity to and slower recovery from an acute laboratory stressor (Richman, Bennett, Pek, Siegler, & Williams, 2007), and have unhealthy diurnal cortisol profiles, including greater overall cortisol output, higher cortisol awakening response, and flatter diurnal cortisol slope (Fuller-Rowell et al., 2012; Zeiders, Doane, & Roosa, 2012). While these associations have been extensively examined among adults and adolescents of ethnic minorities, they have not been studied among children.
A substantial literature has documented the significance of trait resilience in ameliorating people’s psychological distress in response to a wide range of life adversities, such as maltreatment, poverty, parental illness, violence exposure, and other stressful life events (Cicchetti & Rogosch, 2007; Gewirtz & Edleson, 2007; Werner, 1993). In the current research, we view resilience as a psychological trait that is shaped by both genetic and environmental factors. It can present as early as birth and emerges in part from the socialization process of child development. It accounts for significant individual differences in the capacity to adapt in the face of trauma and stress (e.g., parental HIV). Recently, a few studies have directly examined the effects of resilience on health-related processes and outcomes in the context of various environmental threats. For example, among five-year old children, greater resilience was associated with attenuated cortisol reactivity to negative parental interactions (Smeekens, Riksen-Walraven, & van Bakel, 2007). Resilience was also linked to lower risk for cardiovascular problems such as metabolic syndrome, inflammation, and sleep disturbance among children in adverse environments (Matthews, McGrath, Chen, & Miller, 2013).
We propose that resilience may be especially protective among children of parents living with HIV in helping to shape a healthy biological stress response system. Cortisol is a hormone sensitive to psychological stress, released by the hypothalamic-pituitary-adrenal (HPA) axis. It demonstrates a strong basal diurnal rhythm, typically with levels peaking approximately 30–45 minutes after waking, then declining to its nadir around midnight. There is significant variability between people in the profiles of their diurnal cortisol rhythms (Adam, Hawkley, Kudielka, & Cacioppo, 2006). Flatter diurnal cortisol slope is viewed as a marker of a dysregulated HPA axis, because it indicates that stress hormones are remaining high as the day progresses (McEwen, 1998). Dysregulation of the HPA axis is associated with a number of poor health outcomes, including compromised immune functioning, inflammation, diabetes, lung disease, and cardiovascular disease (Miller, Chen, & Zhou, 2007). Existing evidence suggests that flatter cortisol slopes are indicative of poorer future health, with links to mortality in at least four recent studies of adults (Cohen et al., 2012; Kumari, Shipley, Stafford, & Kivimaki, 2011; Sephton et al., 2013; Sephton, Sapolsky, Kraemer, & Spiegel, 2000). It has been suggested that HPA dysregulation during childhood may be a pathway through which early life adversity may negatively influence future health outcomes in adulthood (Miller, Chen, & Parker, 2011; Slatcher & Robles, 2012).
Less known is how resilience may serve as a salutary factor in daily life against the physiological wear and tear of stressors such as having a parent with HIV. Intuitively, and in line with some theoretical reasoning (e.g., Shih, 2004), one would expect that resilience should moderate the negative impact of stigma on diurnal cortisol. From this perspective, the association between perceived stigma and diurnal cortisol might be weaker or absent for children high in resilience compared to those low in resilience. However, resilience may instead influence diurnal cortisol indirectly through perceived stigma. Given that resilience is characterized by a person’s ability to adapt to adversity in flexible and resourceful ways (Connor & Davidson, 2003), it follows that one resourceful (and self-protective) way to adapt to potentially stigmatizing situations is by perceiving lower levels of stigma. Following this logic, youth affected by parental HIV who are more resilient may perceive lower levels of stigma, and, in turn, show healthier diurnal cortisol profiles. We explored these two possible ways in which resilience might positively affect diurnal cortisol—as either a moderator of the effects of perceived stigma or indirectly through lower perceived stigma.
The current study examined the associations among perceived stigma, resilience and diurnal cortisol rhythm in a large sample of children aged 8 to 15 years of parents living with HIV. We hypothesized that perceived stigma would be associated with lower wakeup cortisol and flatter diurnal cortisol slopes, whereas resilience would be associated with higher wakeup cortisol and steeper cortisol slopes. Additionally, although the links between physical health and total cortisol secretion—assessed via area under the curve analysis—are less well established than the links between physical health and cortisol slope, we conducted ancillary analyses using this approach. Finally, we tested whether resilience buffers the negative effect of stigma on diurnal cortisol (a moderation model) or influences diurnal cortisol indirectly through perceived stigma (a mediation model).
Method
Participants
This study used the baseline data from a randomized controlled trial of a psychological intervention project1. Our sample included a subset of 746 children aged 8 to 15 years (from the total study sample of 790 children aged 6–17 years), based on the age range for which the self-report measures used in present analyses were normed. Among those, 645 children (51.9% boys) provided valid saliva specimens for cortisol analysis and they composed the sample in the current study. Approximately 12.6% of the children in our sample had one or both parents who had died from AIDS. The average age of the children was 10.67 years (SD = 1.79). The children and their primary caregivers were recruited from five administrative villages in a HIV endemic area in central China. The paternal education levels were as follows: never attended school (2.3%), elementary school (32.4%), middle school (24.8%), high school (7.2%), and post-secondary education (5.8%). The maternal education levels were as follows: never attended school (6.3%), elementary school (33.5%), middle school (18.4%), high school (8.2%), and post-secondary education (6.0%). The household income levels in Chinese Yuan were as follows: 0–999 (58.0%), 1,000–1,999 (29.9%), 2000–2999 (7.7%), 3000–3999 (2.5%), 4000–4999 (1.0%), 5000 and above (0.8%). Out of the range of education levels (1–5), the mean of paternal education level is 2.64 (SD = 1.06) and the mean of maternal education level is 2.75 (SD = 0.97). Out of the range of income levels (1–6), the mean of the sample is 1.61 (SD = 0.91). The participants in the study had a lower household income level and parental education level in comparison with the broader population in the province or in the country, according to the census data at the year of data collection (National Bureau of Statistics of China, 2013).
Procedure
Children and their primary caregivers were recruited through the village social welfare and local school system. We obtained village-level HIV surveillance data and identified villages with the highest rates of HIV infection and then generated a list of families caring for children affected by HIV/AIDS in each village. Based on the eligible criteria of the intervention study, children with known HIV infection were not included in the study. Children’s HIV-infection status (along with age eligibility and parent’s viral status) was verified through the current caregivers or local community leaders. We then randomly selected families on the lists and invited one child and his/her primary caregiver to participate in the study, until the target sample size (i.e., a total of 800 children of parents living with HIV) was achieved. Appropriate informed consent/assent was obtained prior to participation. Data were collected in 2012 using a research protocol that was approved by the Institutional Review Boards at Wayne State University in the United States and Henan University in China.
Both children and caregivers answered a survey questionnaire, including demographic information and several psychosocial scales. The survey was self-administrated individually or in a small group in the presence of two interviewers. For a few children (2% of the sample) who had reading difficulties, interviewers read the survey items and recorded their responses in a private room. If such a room was not available, the reviewer read the survey items to the child and asked the child to indicate their response directly on the questionnaire without saying the answer. Children were instructed to collect their saliva samples at wakeup, 30 minutes after awakening, before dinner and at bedtime across 3 days (Thursday-Saturday). Each child received age-appropriate gifts at completion of the survey and saliva collection as tokens of appreciation.
Measures
Perceived stigma
Perceived Stigma was measured with the Stigma Against Children Affected by AIDS Scale (Zhao et al., 2010). The scale consists of 15 items assessing three dimensions of subjective awareness of social stigma: social exclusion (e.g., “people think children of parents living with HIV should leave their villages”), purposive avoidance (e.g., people do not want their children to play with children of parents living with HIV”), and perceived inferiority (e.g., “people think children of parents living with HIV are unclean”). The children were asked to indicate their perception on a 4-point Likert scale (“strongly disagree” to “strongly agree”). The Cronbach’s alpha of the scale was .93.
Resilience
The 25-item Connor-Davidson Resilience Scale (CD-RISC) was used to evaluate children’s resilience (Connor & Davidson, 2003). The scale taps various personality characteristics such as tenacity, tolerance of negative effect, positive acceptance of change, sense of control, optimism, recognition of limits to control, and viewing stress as a challenge or opportunity. The scale has been translated and validated among Chinese youths who survived an earthquake and demonstrated good reliability and validity (Yu, Lau, Mak, Zhang, & Lui, 2011). The participants were asked to rate each item with reference to the previous month. If a particular situation (e.g., stressor, change, and challenge) described in the items had not happened within the time frame, the participants were asked to respond to how they would react if such a situation occurred. A 5-point scale was used (0 = not true at all, 4 = true all the time). Cronbach’s alpha of CD-RISC in this study was .88.
Socioeconomic status (SES)
An SES index was created by z-scoring family income, maternal education, and paternal education and then averaging those three components together to form a single composite.
Daily sleep quality
The children were asked to answer the question, “How did you sleep last night?” on a four-point scale (“Terrible” to Great”) for each day of saliva collection.
Perceived health status
The children were asked to rate their overall health status on a 5-point scale (“Very poor” to “Very good”).
Other stressful life events
Based on a stressful life events checklist used in our previous work among this population (Li et al., 2009), we used 15 items to assess children’s experience of a number of stressful life events (in addition to HIV-related parental illness and death). Children reported whether these events occurred in their life in the past six months. Sample items included being in a traffic accident, being a witness to violence, hospitalization, natural disaster, severe sickness or death of friends, involuntary family relocation, and death of family members.
Parental death from HIV/AIDS
The information on parental HIV/AIDS-related death was acquired from village welfare registration offices. The villages are responsible for issuing monthly subsidies for families affected by HIV and AIDS. Thus, they have the updated and accurate information on the health and mortality status of parents in the household.
Salivary cortisol assessment and analysis
Children self-collected saliva samples using Salivettes (Sarstedt, Rommelsdorft, Germany) from Thursday morning through Saturday evening. The children were instructed to collect saliva samples and record the collection times at four time points on each of the three days: immediately upon waking, thirty minutes later to assess cortisol awakening response (CAR), one hour before dinner time, and then right before bedtime. The timing of saliva collection was determined based on the recommendations on assessing salivary cortisol in large-scale studies (Adam & Kumari, 2009). Each child was provided with a wristband to remind them of the timing of saliva collection. Children were asked to place the Salivette samples in plastic bags at the end of day, then returned them to the local research team the following Monday. Salivettes were refrigerated until they were assayed at Huaihe Hospital, an affiliated hospital of Henan University. Cortisol levels were determined via chemiluminescent immunoassay (Access Cortisol kit YZB/USA 2802, Beckman Coulter, Inc, Fullerton, CA). Compliance with the saliva collection procedures was excellent, with 96% of participants providing at least eight of the 12 possible saliva samples across the three days.
Data Analysis
To correct for positive cortisol skewness and kurtosis, a log10 transformation was performed and constant of 1 was added before transformation so that all values would be positive. Because of the strong circadian rhythm of cortisol, a 3-level multilevel modeling (MLM) growth curve approach was used for diurnal cortisol analyses. MLM allows researchers to simultaneously estimate multiple cortisol parameters (e.g. wakeup level, slope, and CAR), and to predict individual differences in diurnal cortisol parameters from individual difference variables of interest as well as covariates (Hruschka, Kohrt, & Worthman, 2005). In line with previous diurnal cortisol research (Adam et al., 2006), Time Since Waking, Time Since Waking2, and CAR (dummy coded 0 or 1) were modeled at Level-1 to provide estimates of each child’s diurnal cortisol rhythm. This approach is optimal because it simultaneously estimates all three cortisol parameters of interest (wakeup levels, CAR, and slope) as well as the curvilinear effect of Time Since Waking2 (e.g., it estimates cortisol slope while taking into account a person’s wakeup cortisol level and CAR, rather than estimating these parameters separately). Second, we estimated Level-3 (person-level) effects of perceived stigma and resilience on cortisol. Third, we controlled for potential confounds, including effects of weekdays vs. weekends (dummy-coded 0 and 1, respectively), daily sleep quality and daily wake time at Level-2 (day level) and gender, socioeconomic status, parental death, other stressful life events, average wake time, average sleep quality and perceived health status at Level-3. Cortisol intercept, slope (effect of Time) and CAR were all allowed to vary randomly at Level-3 (i.e., treated as random effects), while Time Since Waking2 was treated as a fixed effect with no Level-2 or Level-3 predictors. Next, we tested whether perceived stigma mediated the association between resilience and diurnal cortisol. Finally, we tested whether the association between perceived stigma and diurnal cortisol was moderated by resilience. Person-level variables were all grand mean centered, with the exception of gender. All significance tests were 2-tailed with robust standard errors. In addition to examining diurnal cortisol profiles, we also examined the effects of perceived stigma and resilience on cortisol area under the curve (AUC) with respect to ground across the three days of cortisol sampling for each participant. We used standard formulae for computing AUC described in Pruessner et al. (2003). We then used linear regression to regress AUC on perceived stigma and resilience, along with the previously described covariates.
Results
Intercorrelations among study variables are shown in Table 1.
Table 1.
Intercorrelations among predictor variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Perceived stigma | ------- | |||||||||
| 2. Resilience | −.11** | ------- | ||||||||
| 3. Age | −.22** | .13** | ------- | |||||||
| 4. Boy | −.05 | −.02 | −.10** | ------- | ||||||
| 5. Socioeconomic status | .08* | −.03 | −.24** | .05 | ------- | |||||
| 6. Average wake time | .03 | −.05 | .01 | .06 | .06 | ------- | ||||
| 7. Average sleep quality | .01 | −.03 | −.14** | .04 | .03 | −.14** | ------- | |||
| 8. Life events | .13** | .05 | .05 | −.04 | −.01 | .04 | −.14** | ------- | ||
| 9. Parental death | .10* | −.05 | .03 | −.04 | .00 | .09* | .00 | .10** | ------- | |
| 10. Perceived health status | −.02 | .03 | −.10** | .05 | .03 | .01 | .15** | −.18** | −.06 | ------- |
| Mean/Percentage | 1.70 | 2.02 | 10.67 | 51.9% | 0.00 | 6.51 | 3.40 | 2.46 | 12.6% | 4.25 |
| SD | 0.64 | 0.63 | 1.79 | ------- | 0.68 | 1.16 | 0.49 | 2.11 | ------- | 1.05 |
Note.
p < .01,
p < .05, two-tailed.
In initial MLM analyses, we entered perceived stigma and resilience separately as predictors of diurnal cortisol parameters at Level-3 without any other covariates. Perceived stigma was associated with lower wakeup cortisol (β001 = −.034, SE = .009, p < .001; 95% CI = −.052, −.016) and with a flatter cortisol slope (β201 = .004, SE = .001, p < .001; 95% CI = .002, .006). Additionally, resilience was significantly associated with higher wakeup cortisol (β001 = .036, SE = .010, p < .001; 95% CI = .004, .056) and a steeper cortisol slope (β201 = −.002, SE = .001, p = .021; 95% CI = −.004, .000). Neither stigma nor resilience was related to CAR (p’s > .82); thus, CAR was set as a fixed effect with no predictors in subsequent analyses. The diurnal cortisol slopes of youth high (+1 SD) and low (−1 SD) in perceived stigma are depicted in Panel A of Figure 1; cortisol slopes of youth high and low in resilience are depicted in Panel B.
Figure 1.
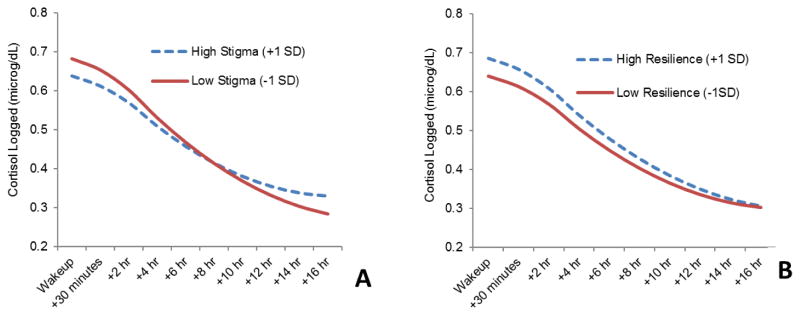
Effects of perceived stigma and resilience on logged diurnal cortisol. The effects of perceived stigma are displayed in Panel A; the effects of resilience are displayed in Panel B. High values for stigma and resilience are plotted at +1 standard deviation and low values are plotted at −1 standard deviation from the mean.
We then examined whether the associations among perceived stigma, resilience and cortisol remained significant when controlling for potential confounds. As displayed in the left half of Table 2 (Model 1), the associations between stigma, wakeup cortisol and cortisol slope remained significant after controlling for age, gender, socioeconomic status, daily and average wake time, daily and average sleep quality, stressful life events, parental death, perceived health status and weekend vs. weekday. By contrast, greater resilience significantly predicted higher cortisol levels at awakening but not cortisol slope, possibly because the effects of resilience on cortisol levels at awakening and cortisol slope were mediated by perceived stigmatization.
Table 2.
Time of Day, Perceived Stigma, Resilience, Stigma × Resilience and Covariates
| Model 1
|
Model 2
|
|||
|---|---|---|---|---|
| Fixed effect (independent variable) | Coefficient (SE) | p-value | Coefficient (SE) | p-value |
| Intercept (average cortisol at wakeup), β000 | 0.687 (0.010) | <.001 | 0.699 (0.010) | <.001 |
| Perceived Stigma, β001 | −0.027 (0.009) | 0.005 | −0.027 (0.009) | 0.004 |
| Resilience, β002 | 0.029 (0.010) | 0.004 | 0.031 (0.010) | 0.002 |
| Perceived Stigma × Resilience β003 | 0.013 (0.014) | 0.341 | ||
| Age, β004 | 0.007 (0.003) | 0.048 | 0.007 (0.003) | 0.052 |
| Gender, β005 | 0.020 (0.012) | 0.077 | 0.021 (0.011) | 0.069 |
| Socioeconomic status, β006 | 0.009 (0.010) | 0.230 | 0.009 (0.007) | 0.218 |
| Average wake time, β007 | −0.002 (0.010) | 0.825 | −0.003 (0.010) | 0.774 |
| Average sleep quality, β008 | 0.001 (0.014) | 0.969 | 0.000 (0.014) | 0.980 |
| Life events, β009 | −0.004 (0.002) | 0.090 | −0.004 (0.002) | 0.087 |
| Parental death, β0010 | 0.002 (0.009) | 0.823 | 0.002 (0.009) | 0.822 |
| Perceived health status, β0011 | −0.000 (0.006) | 0.960 | −0.000 (0.006) | 0.965 |
| Weekend, β010 | −0.111 (0.009) | <.001 | −0.111 (0.009) | <.001 |
| Daily wake time, β020 | −0.023 (0.007) | 0.002 | −0.023 (0.007) | 0.002 |
| Daily sleep quality, β030 | −0.004 (0.009) | 0.669 | −0.004 (0.009) | 0.670 |
| Average CAR, β100 | −0.011 (0.006) | 0.081 | −0.011 (0.006) | 0.080 |
| Average slope of time since waking, β200 | −0.039 (0.002) | <.001 | −0.039 (0.002) | <.001 |
| Perceived Stigma, β201 | 0.004 (0.001) | <.001 | 0.004 (0.001) | <.001 |
| Resilience, β202 | −0.002 (0.001) | 0.093 | −0.002 (0.001) | 0.055 |
| Perceived Stigma × Resilience β203 | −0.002 (0.001) | 0.124 | ||
| Age, β204 | −0.000 (0.000) | 0.134 | −0.000 (0.000) | 0.151 |
| Gender, β205 | −0.000 (0.001) | 0. 699 | −0.000 (0.001) | 0.640 |
| Socioeconomic status, β206 | −0.000 (0.000) | 0.695 | −0.000 (0.001) | 0.651 |
| Average wake time, β207 | −0.002 (0.001) | 0.097 | −0.001 (0.000) | 0.119 |
| Average sleep quality, β208 | −0.000(0.001) | 0.693 | −0.000(0.001) | 0.703 |
| Life events, β209 | 0.000 (0.000) | 0.429 | 0.000 (0.000) | 0.414 |
| Parental death, β2010 | 0.001 (0.001) | 0.451 | 0.001 (0.001) | 0.453 |
| Perceived health status, β2011 | −0.000(0.000) | 0.972 | −0.000(0.000) | 0.962 |
| Weekend, β210 | 0.008 (0.001) | <.001 | 0.008 (0.001) | <.001 |
| Daily wake time, β220 | 0.000 (0.001) | 0.802 | 0.000 (0.001) | 0.810 |
| Daily sleep quality, β230 | 0.001 (0.001) | 0.588 | 0.001 (0.001) | 0.588 |
| Average slope of time since waking2 β300 | 0.000 (0.000) | <.001 | 0.001 (0.000) | <.001 |
Note. Intercepts indicate average cortisol values at wakeup; average slopes of time since waking indicate change in cortisol per 1-hour change in time; average slopes of time since waking2 indicate change in cortisol per 1-hour change in time2; CAR = Cortisol Awakening Response, indicating amount of change in cortisol during the 30 minutes after waking. For gender, Female = 0, Male = 1. Weekday = 0, Weekend = 1.
We next test whether the associations between resilience and diurnal cortisol were mediated by perceived stigma. Confidence intervals (95%) for indirect effects were estimated using the Monte Carlo method for multilevel modeling with 20,000 repetitions (Selig & Preacher, 2008, June). We first used simple regression and found that perceived stigma was significantly predicted by resilience (b = −.132, SE = .040, p = .001; 95% CI: −.210, −.054). Next, when perceived stigma and resilience were entered into the MLM model together in predicting diurnal cortisol parameters, controlling for covariates, the effect of resilience on wakeup cortisol was reduced but still remained significant, whereas the effect of resilience on cortisol slope was no longer significant. The indirect effects of resilience on wakeup cortisol (95% CI: .001, .008) and cortisol slope (95% CI: − .0010, − .0002) via perceived stigma were both found to be significant, suggesting a mediating effect of perceived stigma in the association between resilience and a healthier diurnal cortisol rhythm.
Next, we explored whether the negative effect of perceived stigma on diurnal cortisol might be moderated by resilience. Perceived stigma, resilience and the Perceived Stigma × Resilience interaction term were entered together with the control variables to predict diurnal cortisol. As shown in the right half of Table 2 (Model 2), the interaction effect between stigma and resilience was not significant. Together, these results, along with the previously described findings, suggest that the effect of perceived stigma on diurnal cortisol is not dependent on the level of resilience; rather, children higher in resilience perceive lower levels of stigma, and those lower levels of stigma, in turn, are associated with healthier HPA functioning in daily life.
We then conducted AUC analyses, regressing AUC on perceived stigma and resilience. Initial simple regression models without covariates showed that perceived stigma was not associated with AUC (b = −.152, SE = .106, p = .154; 95% CI: −.360, .056). Resilience was significantly associated with higher AUC (b = .291, SE = .109, p = .008; 95% CI: .077, .505), indicating that higher resilience was associated with higher daily output of cortisol. We next tested whether the associations between stigma, resilience and cortisol AUC were significant when controlling for demographic and health covariates. To test this, we entered both perceived stigma and resilience together in a regression model, along with all of the person-level covariates described previously in the MLM diurnal cortisol analyses, predicting AUC. Controlling for the effects of perceived stigma and covariates, resilience remained a significant predictor of higher AUC (b = .211, SE = .107, p = .049; 95% CI: .001, .421). Controlling for the effect of resilience and covariates, perceived stigma remained a nonsignificant predictor of AUC (b = −.077, SE = .107, p = .470; 95% CI: −.287, .133). Finally, we tested possible interaction effects between perceived stigma and resilience on cortisol AUC. The interaction term of perceived stigma and resilience was not significantly associated with AUC (p = .906).
We conducted further analyses to examine whether the effect of resilience on AUC might be driven by higher wakeup cortisol levels. Using regression, we found that the effect of resilience on AUC became nonsignificant (p = .565) when controlling for average wakeup cortisol, together with stigma and all the person-level covariates. In contrast, the effect of resilience on wakeup cortisol remained significant (b = .023, SE = .009, p = .011; 95% CI: .005, .041) when controlling for AUC together with stigma and all the person-level covariates. These results suggest that the effect of resilience on higher AUC may be driven by the robust effect of resilience on higher wakeup cortisol, mirroring the findings from the MLM analyses described previously.
Discussion
In a large sample of children affected by parental HIV, we found that greater perceived stigma was associated with lower wakeup cortisol and flatter diurnal cortisol slopes. Resilience did not moderate the relationship between perceived stigma and cortisol slopes; rather, it showed a salutary effect on diurnal cortisol via decreased perceived stigma. That is, children with higher resilience tend to perceive lower stigma, and, in turn, show a “healthier” diurnal cortisol rhythm. The positive association between resilience and wakeup cortisol was mirrored in additional analyses assessing total daily cortisol output. Our findings suggest that HIV stigmatization can impact children’s stress physiology in daily life and that resilience is a potentially promotive factor for such children. Notably, the relationships among perceived stigma, resilience and diurnal cortisol remained strong after controlling potential confounds such as child’s age and gender, family socioeconomic status, self-rated health status, parental death, daily and average wake time and sleep quality, and other stressful life events.
This is, to the best of our knowledge, the first study to show that HIV-related stigma is associated with diurnal cortisol patterns. Our findings corroborate existing research on the relationship between stigmatization stress and psychological health (Pascoe & Richman, 2009), and extend these previous findings to a child population and show the potential physical health consequences of perceiving stigmatization towards having parents infected with HIV. Prior studies suggest that activation of the HPA axis is sensitive to stressors that are socially evaluative and uncontrollable (Schmitt et al., 2014). Naturalistic studies have found that uncontrollable stressors and/or stressors that pose a threat to the individual’s social standing are related to flattened diurnal cortisol slopes, lower morning values, and higher afternoon values (Miller et al., 2007; Zeiders et al., 2012). Perceived stigma against children affected by HIV could be considered both socially evaluative and uncontrollable. It is socially evaluative because such an experience threatens children’s social standing in their peer group and their immediate context (e.g., school) and uncontrollable because stigma has nothing to do with children’s actions, but rather their parents’ HIV infections.
Notably, we found an indirect effect of resilience via decreased perceived stigma on steeper cortisol slope. The findings are consistent with previous evidence generally derived from youth from low socioeconomic environments and racial minority backgrounds (Chen, 2013). To our knowledge, this is the first published study in any population to examine how resilience is associated with HPA axis function. Our findings suggest that children higher in resilience generally may have greater internal resources to cope with the multiple stressors in their lives. Children with a resilient mindset may generally perceive the world more positively and perceive fewer external stressors such as stigma, thus enjoying better health outcomes. Our findings echo prior evidence emphasizing the importance of subjective interpretation of objective encounters with stigmatizing behaviors. Indeed, objective discrimination encounters may not inevitably be perceived or interpreted as stigma, even for those in a disadvantaged group (Schmitt et al., 2014). Resilience appears to partially determine the extent to which others’ discrimination behaviors are perceived as stigma. Children are not simply passive targets of adverse environments, but rather active participants in society as they may seek to understand their social world and create their own lives. Therefore, in trying to reduce stigmatization at the socio-structural level and promote supportive communities (Hatzenbuehler & McLaughlin, 2014), future research should also focus on identifying and fostering resilience factors that may help children to achieve healthy outcomes.
Resilience was also found to be associated with higher daily cortisol output using AUC analysis. This finding, at first, seems counterintuitive because higher daily cortisol output is generally assumed to be related to poorer health (Pruessner et al., 2003). However, our findings suggest that the positive association between resilience and higher daily cortisol output is, in fact, driven by higher wakeup cortisol—which is considered to be an indicator of healthy HPA axis functioning in childhood. Previous research among maltreated or abused children have showed similar results, suggesting that chronic stress is associated with blunted diurnal cortisol, particularly lower cortisol early in the morning (Fisher, Van Ryzin, & Gunnar, 2011) and positive psychological factors are associated with higher morning cortisol (Cicchetti & Rogosch, 2007).
There are some limitations of this study. First, the data are cross-sectional; we cannot rule out the reverse causality interpretation that HPA axis dysregulation may lead to lower resilience and higher perceived stigma. Second, most of the parents of the sampled children were infected with HIV via unhygienic blood-collection practices associated with sale of blood for income rather than other highly stigmatized behaviors, such as drug use and commercial sex, which limits the representativeness of the sample. This unique, largely poverty-driven, cause of HIV infection may have reduced the range and severity of stigma experienced or perceived by the current sample. Third, the large sample size made it impossible (both financially and logistically) to closely monitor individual children’s compliance with the timing of salivary sample collection. The absence of a statistically significant CAR in this sample may suggest possible problems in compliance with the timing of saliva collection (e.g., some participants might have collected their saliva samples substantially more or less than 30 minutes after waking). An alternative explanation is that our sample differs from other population in showing a non-significant CAR. Prior research shows that adverse early life experiences may result in a blunted CAR response (Quevedo, Johnson, Loman, LaFavor, & Gunnar, 2012). However, both of these possible explanations necessitate further research.
Despite these limitations, this work makes important advances in generating evidence of associations among perceived stigma, resilience and health-related biology during childhood. These findings indicate that children’s perception of being stigmatized is associated with what is considered a less healthy diurnal cortisol rhythm, whereas resilience is a predictive of a healthier diurnal cortisol rhythm. The naturalistic assessment of saliva collection over multiple days from a large sample of children lends confidence to our findings. Future intervention research should focus on reducing stigma and promoting resilience to cope with the stress associated with parental HIV-related illness and death.
Acknowledgments
This research was supported by NIH grant R01NR13466. The authors want to thank Heidi Kane, Ledina Imami, George Tam and others from the Close Relationships Lab at Wayne State University for their comments on this manuscript.
Footnotes
Published findings from this project include analyses of links between coping and diurnal cortisol (Slatcher et al., in press). None of the findings from that paper—with the exception of covariates included in the MLM models—overlap with those reported here. Further, the findings reported in this paper all remain significant when controlling for coping (both positive and negative coping).
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience–cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam EK, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34(10):1423–1436. doi: 10.1016/j.psyneuen.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Benetti C, Kambouropoulos N. Affect-regulated indirect effects of trait anxiety and trait resilience on self-esteem. Personality and individual differences. 2006;41(2):341–352. [Google Scholar]
- Chen E. Psychological resilience among low socioeconmic status youth and implications for cardiovascular risk profiles. Paper presented at the 71st Annual Scientific Meeting of the American PsychosomaticSociety.2013. Apr, [Google Scholar]
- Chi P, Li X. Impact of parental HIV/AIDS on children’s psychological well-being: A systematic review of global literature. AIDS and behavior. 2013;17(7):2554–2574. doi: 10.1007/s10461-012-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P, Li X, Zhao J, Zhao G. Vicious circle of perceived stigma, enacted stigma and depressive symptoms among children affected by HIV/AIDS in China. AIDS and behavior. 2014;18(6):1054–1062. doi: 10.1007/s10461-013-0649-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Personality, adrenal steroid hormones, and resilience in maltreated children: A multilevel perspective. Development and Psychopathology. 2007;19(3):787–809. doi: 10.1017/s0954579407000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver LD, Gardner F, Operario D. Effects of stigma on the mental health of adolescents orphaned by AIDS. Journal of Adolescent Health. 2008;42(4):410–417. doi: 10.1016/j.jadohealth.2007.09.022. [DOI] [PubMed] [Google Scholar]
- Cohen L, Cole SW, Sood AK, Prinsloo S, Kirschbaum C, Arevalo JM, Wei Q. Depressive symptoms and cortisol rhythmicity predict survival in patients with renal cell carcinoma: Role of inflammatory signaling. PloS one. 2012;7(8):e42324. doi: 10.1371/journal.pone.0042324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Van Ryzin MJ, Gunnar MR. Mitigating HPA axis dysregulation associated with placement changes in foster care. Psychoneuroendocrinology. 2011;36(4):531–539. doi: 10.1016/j.psyneuen.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Doan SN, Eccles JS. Differential effects of perceived discrimination on the diurnal cortisol rhythm of African Americans and Whites. Psychoneuroendocrinology. 2012;37(1):107–118. doi: 10.1016/j.psyneuen.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Edleson JL. Young children’s exposure to intimate partner violence: Towards a developmental risk and resilience framework for research and intervention. Journal of Family Violence. 2007;22(3):151–163. doi: 10.1007/s10896-007-9065-3. [DOI] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA. Structural Stigma and Hypothalamic-Pituitary-Adrenocortical Axis Reactivity in Lesbian, Gay, and Bisexual Young Adults. Annals of Behavioral Medicine. 2014;47(1):39–47. doi: 10.1007/s12160-013-9556-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruschka DJ, Kohrt BA, Worthman CM. Estimating between-and within-individual variation in cortisol levels using multilevel models. Psychoneuroendocrinology. 2005;30(7):698–714. doi: 10.1016/j.psyneuen.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Klonoff EA. Introduction to the Special Section on Discrimination. Health Psychology. 2014;33(1):1–2. doi: 10.1037/hea0000070. [DOI] [PubMed] [Google Scholar]
- Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. The Journal of Clinical Endocrinology & Metabolism. 2011;96(5):1478–1485. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Barnett D, Fang X, Lin X, Zhao G, Zhao J, Stanton B. Lifetime incidence of traumatic events and mental health among children affected by HIV/AIDS in rural China. Journal of Clinical Child and Adolescent Psychology. 2009;38(5):731–744. doi: 10.1080/15374410903103601. [DOI] [PubMed] [Google Scholar]
- Major B, O’Brien LT. The social psychology of stigma. Annual Review of Psychology. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- Matthews KA, McGrath J, Chen E, Miller G. Childhood roots of adult cadiovascular risk: Focus on ealry resilience. Paper presented at the 71st Annual Scientific Meeting of the American-Psychosomatic-Society.2013. Apr, [Google Scholar]
- McEwen BS. Protective and Damaging Effects of Stress Mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137(6):959. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133(1):25. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics of China. China Statistical Yearbook 2013. Beijing, China: China Statistics Press; 2013. [Google Scholar]
- Pascoe EA, Richman LS. Perceived discrimination and health: A meta-analytic review. Psychological Bulletin. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28(7):916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Quevedo K, Johnson AE, Loman ML, LaFavor TL, Gunnar M. The confluence of adverse early experience and puberty on the cortisol awakening response. International journal of behavioral development. 2012;36(1):19–28. doi: 10.1177/0165025411406860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richman LS, Bennett GG, Pek J, Siegler I, Williams RB. Discrimination, dispositions, and cardiovascular responses to stress. Health Psychology. 2007;26(6):675–683. doi: 10.1037/0278-6133.26.6.675. [DOI] [PubMed] [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychological Bulletin. 2014 doi: 10.1037/a0035754. doi: http://dx.doi.org/10.1037/a0035754. [DOI] [PubMed]
- Selig JP, Preacher KJ. Monte Carlo method for assessing Mediation: An interactive tool for creating confidence intervals for indirect effects. 2008 Jun; Available from http://quantpsy.org/
- Sephton SE, Lush E, Dedert EA, Floyd AR, Rebholz WN, Dhabhar FS, Salmon P. Diurnal cortisol rhythm as a predictor of lung cancer survival. Brain, Behavior, and Immunity. 2013;30:S163–S170. doi: 10.1016/j.bbi.2012.07.019. [DOI] [PubMed] [Google Scholar]
- Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. Journal of the National Cancer Institute. 2000;92(12):994–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- Shih M. Positive stigma: Examining resilience and empowerment in overcoming stigma. The ANNALS of the American Academy of Political and Social Science. 2004;591(1):175–185. [Google Scholar]
- Slatcher RB, Chi P, Li X, Zhao J, Zhao G, Ren X, Stanton B. Associations between coping and diurnal cortisol among children affected by parental HIV/AIDS. Health Psychology. doi: 10.1037/hea0000169. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher RB, Robles TF. Preschoolers’ everyday conflict at home and diurnal cortisol patterns. Health Psychology. 2012;31(6):834. doi: 10.1037/a0026774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeekens S, Riksen-Walraven JM, van Bakel HJA. Cortisol reactions in five-year-olds to parent-child interaction: the moderating role of ego-resiliency. Journal of Child Psychology and Psychiatry. 2007;48(7):649–656. doi: 10.1111/j.1469-7610.2007.01753.x. [DOI] [PubMed] [Google Scholar]
- Werner EE. Risk, Resilience, and Recovery - Perspectives from the Kauai Longitudinal-Study. Development and Psychopathology. 1993;5(4):503–515. [Google Scholar]
- Yu X, Lau JTF, Mak WWS, Zhang J, Lui WWS. Factor structure and psychometric properties of the Connor-Davidson Resilience Scale among Chinese adolescents. Comprehensive Psychiatry. 2011;52(2):218–224. doi: 10.1016/j.comppsych.2010.05.010. [DOI] [PubMed] [Google Scholar]
- Zeiders KH, Doane LD, Roosa MW. Perceived discrimination and diurnal cortisol: Examining relations among Mexican American adolescents. Hormones and Behavior. 2012;61(4):541–548. doi: 10.1016/j.yhbeh.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Li X, Fang X, Hong Y, Zhao G, Lin X, Stanton B. Stigma Against Children Affected by AIDS (SACAA): Psychometric evaluation of a brief measurement scale. AIDS and behavior. 2010;14(6):1302–1312. doi: 10.1007/s10461-009-9629-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


