Abstract
Although the importance of the anterolateral stabilizing structures of the knee in the setting of anterior cruciate ligament (ACL) injuries has been recognized since many years, most of orthopedic surgeons do not take into consideration the anterolateral structures when performing an ACL reconstruction. Anatomic single or double bundle ACL reconstruction will improve knee stability, but a small subset of patients may experience some residual anteroposterior and rotational instability. For this reason, some researchers have turned again towards the anterolateral aspect of the knee and specifically the anterolateral ligament. The goal of this review is to summarize the existing knowledge regarding the anterolateral ligament of the knee, including anatomy, histology, biomechanics and imaging. In addition, the most common anterolateral reconstruction/tenodesis techniques are described together with their respective clinical outcomes.
Key words: Anterolateral ligament, knee, anterior cruciate ligament, reconstruction
Introduction
Anterior cruciate ligament (ACL) reconstruction is a very common procedure all over the world, with almost 130,000 surgeries performed in the US in 2006.1 In most ACL deficient athletes involved in pivoting sports, ACL reconstruction is the only way to achieve pre-injury level of performance.2,3 During the past decades a significant improvement in ACL reconstruction techniques has been observed, evolving from extra-articular to intra-articular techniques, from open to arthroscopic procedures, and from non anatomic to anatomic reconstructions.4 However, the ideal ACL reconstruction technique is still under debate and residual anterior and rotational instability can be found in a small subset of patients also after anatomic ACL reconstruction.5-7 In 1879 Segond described the existence of an anterolateral capsular thickening in human knees that can cause a small avulsion fracture at the level of the anterolateral tibia, also known as Segond’s fracture, and pathognomonic of ACL rupture.8 With the boom of arthroscopic ACL reconstruction, the importance of the anterolateral knee capsule thickening, also known as anterolateral ligament (ALL), has been often disregarded. However, the high incidence of ALL lesions in ACL-injured knees and its causative relationship with a high-grade pivot-shift, recently stimulated researchers to better investigate the anatomy and function of the ALL.5,9-11 The aim of this review is to report the current knowledge regarding the anatomy and biomechanics of the ALL, along with the diagnosis and treatment of patients with injury to the ALL. The authors searched the PubMed/Medline database for publications specifically addressing the ALL and anterolateral tenodesis/reconstruction techniques. Only the English literature was included. The references of the papers included were also analyzed, in order to add any missing relevant article. Data extraction related to the anatomy, morphometry, biomechanics, and histology of the ALL was performed. In addition, a historical perspective of lateral tenodesis techniques was provided, together with the results of the procedures combining ACL reconstruction and anterolateral tenodesis/reconstruction.
Anatomy of the anterolateral ligament
In 1879, the French surgeon Paul Segond described a pearly, resistant, fibrous band inserting on the anterolateral aspect of the proximal tibia.8 This can be considered the first description of the ALL, which was referred to with different names in the subsequent years, including: anterior band of the lateral collateral ligament for Irvine et al. in 1987,12 (mid-third) of the lateral capsular ligament for different authors,12-15 anterior oblique band for Campos et al.16 and anterolateral ligament for Vieira et al. and Claes et al.10,17 Recently, different studies were performed on cadaveric knees in order to identify anatomical and histological features of the ALL (Figure 1).
Figure 1.
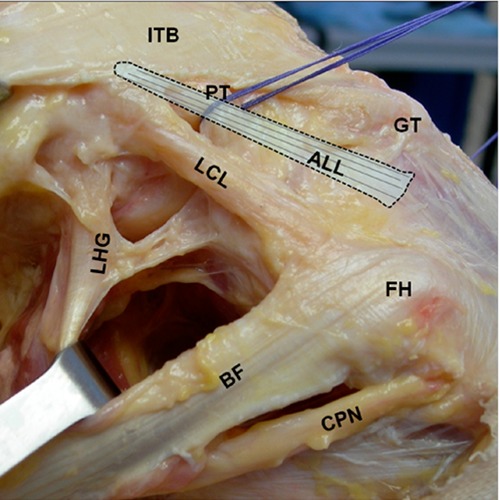
Anatomy of the lateral aspect of the knee. ALL, anterolateral ligament; ITB, iliotibial band. LCL, lateral collateral ligament; LHG, lateral head of the gastrocnemius; PT, popliteus tendon; CPN, common peroneal nerve; BF, biceps femoris; GT, gerdy’s tubercle; FH, fibular head.
Anatomy of the femoral origin
In 2012, Vincent et al. identified an anatomical variation of the ALL origin near or on the popliteus tendon.18 In 2013, with a larger number of specimens, Claes et al. described the origin of the ALL on the prominence of the lateral femoral epicondyle, anterior to the socket from which the lateral collateral ligament (LCL) originated, and proximal and posterior to the insertion of the popliteus tendon.10 In a similar study, Dodds et al. identified the ALL origin on average 8 mm proximal and 4.3 mm posterior to the most prominent point of the lateral epicondyle. The femoral attachment was described as complex, with a fan-like blending of fibers at the lateral aspect of the lateral femoral condyle.11 Caterine et al. described the proximal fibers of the ALL fanned over the top of the LCL origin. However, the main body of both the ALL and LCL were easily separable. The ALL originated either anterior-distal or posterior–proximal to the LCL femoral insertion, with two anatomical variations.19
Anatomy of the distal insertion
While Vincent et al. reported as macroscopically impossible to assess whether some fibers of the ALL actually inserted onto the meniscus,18 Claes et al. identified a strong connection between the ALL and the periphery of the middle third of the lateral meniscal body, and suggested to divide the ALL into a meniscofemoral and a meniscotibial band.10 Similarly to Vincent et al., Dodds et al. described the ALL as superficial and distinct from the capsule of the knee, with only branching attachments to the lateral meniscus.11 Caterine et al. identified the attachments of the ALL to the lateral meniscus in all the specimens.19 All the above mentioned anatomical studies described the ALL tibial insertion as a thick capsular fold, broader than its main body, between fibular head and Gerdy’s tubercle.10,11,18,19
Quantitative anatomy of the anterolateral ligament
Quantitative anatomical characterization about length, width and thickness of the ALL were also reported by Caterine et al. The mean length, with the knee extended, was 40.3±6.2 mm. The width of the ALL increased from proximal to distal, beginning as a more tubular, narrow structure at the femoral origin with a mean attachment width of 4.8±1.4 mm. The ALL then widened distally, with a mean tibial insertion width of 11.7±3.3 mm. The mean thickness was 1.4±0.6 mm.19 Dodds et al. also identified an isometric behavior of the ALL from 0° to 60° of flexion. With flexion >60° and with external rotation, the ALL tension and length decreased. An opposite effect was noted with internal rotation. Both internal and external rotations significantly affected the ALL length, but only with the knee flexed.11
Histology
Caterine et al. also investigated the ALL from a histological point of view. In the Hematoxylin and Eosin stained specimens, the body of the ALL had a dense regularly organized collagenous structure, similar to other ligamentous tissues. In longitudinal sections, the collagen pattern of the ALL was described as organized into individual bundles, indicating that the structure may be a combination of multiple thickenings of the lateral joint capsule. However, a clear distinction of the ALL in cross section compared with the joint capsule was described, as the joint capsule resembled a loose connective tissue. Immunohisto-chemistry analysis showed a peripheral nervous innervation together with mechanoreceptors.19
Biomechanics
Monaco et al. in 2012 investigated the knee kinematics on 10 fresh-frozen cadaver knees with a computer navigation system. The knee kinematics was evaluated with: i) ACL intact, ii) after cutting the posterolateral (PL) bundle of the ACL, iii) after cutting the anteromedial (AM) bundle, and iv) after cutting of the ALL. Cutting the PL bundle did not increase anterior translation and rotation of the knee. Cutting the AM bundle significantly increased the anteroposterior (AP) translation at 30° and 60° (P=0.01), but did not increase rotation of the knee. Cutting the ALL increased anterior translation at 60° (P=0.04) and internal rotation at 30°, 45°, and 60° (P=0.03). The authors concluded that cutting the ALL increased tibial rotation and could be related to the pivot shift phenomenon.9
In 2015, Pearsons et al. studied the in situ forces of the ALL, ACL, and LCL on 11 cadaveric knees, subjected to 134 N of anterior drawer at flexion angles between 0° and 90° and separately to 5 N·m of internal rotation at the same flexion angles. The authors noted that the ALL is an important stabilizer of internal rotation at flexion angles >35°. The ACL is the primary restraint during anterior drawer at all flexion angles and during internal rotation at flexion angles less than 35°.20
Epidemiology
In 2014, Claes et al. retrospectively reviewed 271 MRIs of unilateral ACL-injured knees. Of these MRIs, the ALL was considered as non-visualized in 65 cases (24.0%), leaving 206 knees (76.0%) for further analysis. Out of 206 knees, the ALL was considered uninjured in 44 knees (21.3%) and torn in 162 (78.8%). The majority of ALL abnormalities were found in the distal portion of the ligament (77.8%). Three (1.8%) knees were diagnosed with a bony ALL avulsion (Segond fracture).21
Diagnosis
Radiographs
Anteroposterior, lateral and Merchant X ray views of the knee should be obtained to rule out fractures (including Segond Fracture, tibial eminence avulsions, etc) (Figure 2).
Figure 2.
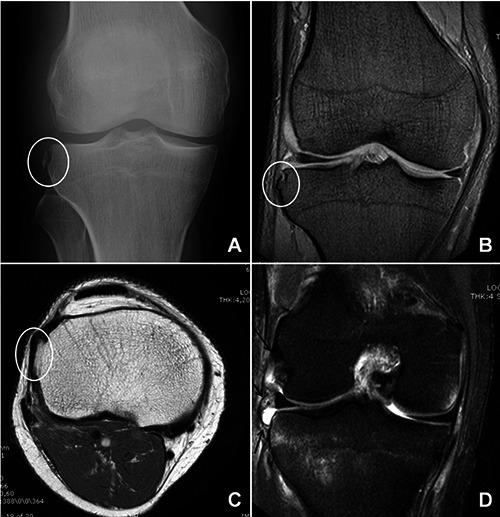
Imaging. A) Anteroposterior knee radiograph, showing Segond fracture (white circle). B) Coronal magnetic resonance imaging (MRI) showing sequelae of Segond fracture (white circle). C) Sagittal T1 MRI showing sequelae of Segond fracture (white circle). D) Coronal fat suppression MRI showing anterolateral ligament rupture (black arrows).
Magnetic resonance imaging
According to the anatomical location of the ALL, this can be better visualized with coronal images (Figure 2). Visibility of the ALL seemed to be easier on MRI of patients with ruptured ACL. This is due to the joint effusion and tissue edema separating the anatomical structures.22 Caterine et al. reported that identification of the ALL is easier at the meniscal and tibial attachment compared with the proximal attachment, due to the ALL’s close relationship with the insertion of the LCL and popliteus tendon proximally.19 A 3.0 T study with 0.4 mm slice thickness and fat suppression images is recommended to better identify the ALL (Figure 2).19,22
In 2015, Porrino et al. evaluated 53 routine knee MRI studies interpreted as normal to characterize the ALL, and 20 knee MRI studies with a Segond fracture to determine the relationship between the fracture and the ALL. In all 53 cases the ALL was visualized. This structure was somewhat ill defined and sheet-like, inseparable from the adjacent LCL proximally and iliotibial band distally. Almost all cases with a Segond fracture showed attachment of the ALL to the fracture fragment (19/20 cases).23
In 2015, De Maeseneer et al. retrospectively reviewed the MRI of 13 cases of Segond fracture. The authors noted that the mean size of the Segond bone fragment was 8×10×2 mm. The ACL was torn in all cases, the medial collateral ligament in 8, the posterolateral corner was involved in 5, and the posterior horn of the medial meniscus was torn at the meniscocapsular junction in 5 knees. The iliotibial band (11/13) and ALL (10/13) inserted on the Segond bone fragment.24
Arthroscopy
Sonnery-Cottet et al. described an arthroscopic surgical technique to identify the ALL. With the knee at 90° of flexion, using the anterolateral portal, the arthroscope is introduced into the lateral gutter of the knee joint and a shaver is introduced in an accessory superolateral portal to debride the synovial tissue. This allows visualization, from proximal to distal, of the femoral attachments of LCL, ALL and popliteus tendon.25
Surgical procedures
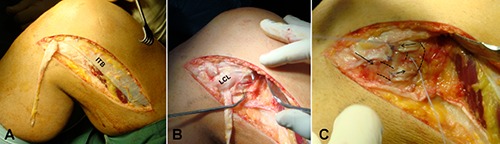
Over the years, several different techniques of ALL reconstruction have been described either as an extra-articular procedure isolated or combined with intra-articular ACL reconstruction. In 1967, Lemaire described a completely extra-articular procedure to treat chronic ACL deficient knees.26 With the Lemaire’s procedure, the purpose is to span the outside lateral portion of the knee joint with a soft tissue band, which controls the rotational instability. A 1-cm wide band of fascia lata is harvested, maintaining its distal insertion on the tibia (Figure 3). A semi-circular tunnel is created on the lateral aspect of the distal femur. The fascia lata band is passed under the LCL and through the tunnel. The fascia lata band is then tightened and stitched back to itself (Figure 3).
Figure 3.

Lemaire Technique. A) A 1 cm wide band of fascia lata is harvested, maintaining its distal insertion. B) The fascia lata band is passed under the LCL and a semi-circular tunnel is created on the lateral aspect of the distal femur. C) The graft is passed through the tunnel and stitched back to itself.
A modified Lemaire’s procedure, performed with a free gracilis tendon, has been described by Dejour et al. The gracilis tendon is harvested, detached from its tibial insertion, and prepared on the back table. Through a lateral incision, the graft is then passed into a semicircular tunnel located at the isometric point just above the LCL femoral insertion. The two ends are passed under the LCL. One end is passed into a tunnel at the level of the Gerdy’s tubercle and then sutured back to the other end.27
In 1979, MacIntosh described a different anterolateral tenodesis.28 A 20-cm long, 3-cm wide strip of iliotibial band (ITB) was harvested, preserving the distal insertion. The strip was passed deep to the LCL, through a subperiostal tunnel (posterior to the proximal LCL insertion), through the distal intermuscular septum, deep to the LCL again, and then anchored to the anterolateral tibia (Figure 4A).
Figure 4.
A) MacIntosh technique (see text). B) Christel and Dijan technique.
This technique has been slightly modified by Arnold et al.,29 Losee et al.,30 Andrews and Sanders,31 Frank and Jackson,32 as well as Christel and Dijan.33 These variations mainly involve the femoral fixation of the ITB strip. According to Losee et al., the ITB is passed through an extrarticular femoral tunnel, through the lateral gastrocnemius tendon and under the LCL.30 Similarly to Losee et al., Frank and Jackson passed the ITB under the LCL, though the lateral gastrocnemius tendon and secured it with stitches to both structures (LCL and gastrocnemius).32 Andrews and Sanders described an isometric lateral plasty with two ITB strips (one tight in flexion, the other tight in extension), both fixed at the lateral femur.31 Christel and Dijan described the use of a short (12×75 mm) ITB strip left attached distally (Figure 4B).33 The strip was then twisted 180° and fixed with an interference screw in a femoral bone tunnel, drilled at the isometric point. Ellison described a dynamic lateral reconstruction with the ITB detached distally and preserved proximally.34 The strip was then passed under the LCL and fixed back to the anterolateral tibia. Ellison hypothesized that the contraction of the tensor fascia lata would stabilize the knee during activity. With the increasing renewed interest in anterolateral stabilizing structures, different authors recently described combined intra- and extra-articular reconstruction techniques.27,35-38 According to Marcacci et al. the gracilis and semitendinosus tendons are harvested preserving the distal insertion (Figure 5). The graft is then passed through a tibial tunnel and in an over the top position on the femoral side using a lateral incision to the distal femur. The graft is fixed proximally with 2 Richard’s staples, with the knee flexed at 90° and the foot externally rotated. The remnant of the graft is then passed under the iliotibial band and fixed with 1 staple at the level of the Gerdy’s tubercle (Figure 5).37
Figure 5.
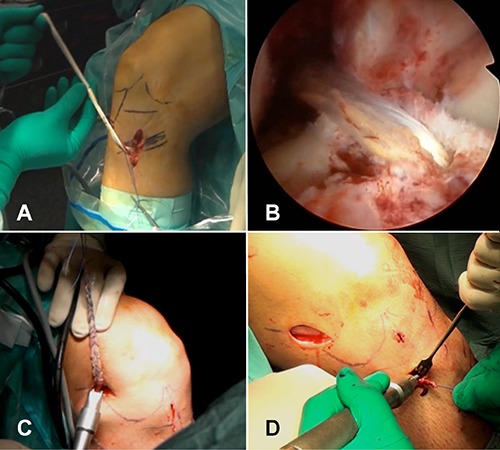
Marcacci technique. A) The hamstrings are harvested, preserving the tibial insertion. B) An anatomic tibial tunnel is created and the graft is passed in an over the top position on the femur, through a lateral approach. C) The graft is fixed proximally with 2 staples. D) The remnant of the graft is then passed under the fascia lata and fixed to the anterolateral tibia with another staple.
Yamaguchi et al. described an ITB ACL reconstruction procedure with combined lateral plasty.39 A 25-cm longitudinal incision was performed on the lateral femur. A 22-cm-long strip of the ITB was harvested, leaving the tibial insertion attached. A 7.5-mm femoral hole was then drilled in an outside-in fashion. A 7.5-mm tibial tunnel was drilled. With forceps, the graft was passed deep to the LCL and through the femoral and tibial tunnels. With the knee at 90° of flexion and the foot externally rotated, the graft was sutured to the LCL and the periosteum of the lateral femoral condyle. Then, with the knee at 30° of flexion and the foot externally rotated the graft was sutured to the periosteum around the outlet of the tibial tunnel.
In 2013, Saragaglia et al. published their technique. The hamstrings are harvested and left attached distally. At the level of the intrarticular portion, the semitendinosus is doubled. The tibial and femoral full tunnels are drilled with an out-in technique. The graft is passed into the knee through the tunnels, exiting the lateral femur. A second anterolateral lateral skin incision allows for the lateral plasty.38
Recently, Verdonk et al. described in VuMedi the Antwerp Monoloop procedure for the anatomical reconstruction of the ALL [https://www.vumedi.com/video/the-antwerp-monoloop-for-reconstruction-of-the-anterolateral-ligament-all/]. The procedure starts with an anatomical ACL reconstruction, without tibial fixation. With the knee at 60° of flexion, a 10 cm hokey stick incision is made on the lateral side. Then, a 1 cm ITB strip is harvested, preserving the tibial attachment. A 10-15 cm ITB strip is created. Then the ITB strip is passed deep to the LCL. The free end of the ITB strip is tunneled towards the proximal femur underneath the lateral gastrocnemius head. With the knee ever at 60° of flexion and the foot in slight external rotation, the ITB strip is fixed with an 8 mm staple. Then, tibial fixation of the ACL graft is performed with knee in 20° of flexion.
Results
Biomechanical and clinical outcomes have been reported regarding extra-articular procedures, both isolated and combined with ACL reconstruction.
Biomechanical results
In 2007, Monaco et al. compared lateral tenodesis (Arnold-Coker procedure) plus single bundle ACL reconstruction (Group A) with anatomic double bundle ACL reconstruction (Group B), in terms of internal tibial rotation. A computer navigation system was used to evaluate the global kinematic of the knee in twenty patients. No differences were found in terms of anteroposterior tibial displacement and external rotation; however a significant reduction in internal rotation of the tibia was found in group A compared with group B (P=0.0001).40
Similarly, Zaffagnini et al. quantitatively assessed in vivo static and dynamic biomechanics of the knee before and after ACL reconstruction, comparing the Marcacci technique with anatomic double-bundle technique in thirty-five consecutive patients. The Marcacci technique showed statistically better laxity reduction in varus/valgus stress test at full extension and in internal/external rotation at 90° of flexion; the lateral plasty better controlled the lateral compartment during drawer test and varus/valgus stress test both at 0° and 30° of flexion and both the compartments during internal/external rotation at 90° of flexion. On the other hand, pivot-shift phenomenon was better controlled by anatomic double-bundle reconstruction.5
In 2014, Monaco et al. evaluated the role of lateral tenodesis on the pivot shift effect. Twenty patients underwent anatomic single-bundle ACL reconstruction with the addition of extra-articular reconstruction. In group A, intra-articular reconstruction was performed first and lateral tenodesis thereafter; in group B, lateral tenodesis was performed first. Maximum anterior tibial translation (ATT) and axial tibial rotation (ATR) at 30° of flexion and during the pivot-shift test were measured. The authors showed that extra-articular reconstruction had little effect in reducing ATT at 30° of flexion, but it was more effective than intra-articular reconstruction in reducing ATR. The authors concluded that anatomic ACL reconstruction and lateral tenodesis were synergic in controlling the pivot-shift phenomenon.41
Clinical results
Clinical outcomes have been reported for extra-articular procedures, both isolated and combined with ACL reconstruction. Being isolated extra-articular reconstruction obsolete, in this paper only the relevant literature regarding combined intra and extra-articular ACL reconstruction techniques has been reported.
In 2006, Yamaguchi et al. described the long term results of their technique with iliotibial tract at 6, 13, and 24-year longitudinal follow-up. Twenty-six (60%) patients of the original ACL reconstruction cohort participated in all three follow-up assessments. The mean Lysholm score was 96.2, 93.8, and 87.8 at 6-, 13-, and 24-year follow-up, respectively. A significant decrease in mean Lysholm score was found between 13- and 24- year follow-up. The mean KT-1000 side-to-side difference was 3.5 mm at 24-year follow-up. At 24-year follow-up, 17 (71%) patients had moderate or severe degenerative changes on radiographs.39
In 2006, Zaffagnini et al. clinically compared the Marcacci technique with the single bundle patellar tendon (PT) and 4 strand hamstring (HS) techniques at 5 years of follow-up. The authors described significant kneeling pain in the PT with respect to the other groups. Subjective IKDC evaluation for PT and Marcacci technique groups had significantly higher scores than the HS group (P=0.04). There was a trend to less pathologic laxity in PT and Marcacci group (Pivot and Lachman tests) compared to the HS group. The Pivot shift test was negative in 88% in PT group and 92% in Marcacci group, and these scores were significantly higher (P=0.03) with respect to the HS group (64%). Regarding the Lachman test 88% had no laxity in PT group, 78% in HS group and 92% in Marcacci group. The KT 2000 arthrometer revealed a significant laxity (P=0.049) in the HS group compared with the other groups. Time to return to sport was shorter for the Marcacci group compared with the other two. Tibial tunnel enlargement was significantly higher in the HS group (P=0.03). The authors concluded that patellar tendon and Marcacci techniques can be equivalent options for ACL reconstruction.42
In 2009, Marcacci et al. evaluated the outcomes of 54 consecutive high-level athletes operated with their technique at a 10 to 13 year follow-up. After 11 years, the IKDC score demonstrated good or excellent results in 90.7% of patients. Ligament arthrometry showed that only 2 patients had >5 mm manual maximum side-to-side difference in laxity. The mean Tegner activity score was 4.5, while the mean Lysholm score was 97.3 and the mean subjective score was 90.0%. Radiographic evaluation demonstrated progressive joint narrowing only for the 20 patients having concomitant medial meniscal surgery. The authors concluded that the technique showed satisfactory results, with maintenance of knee stability at long-term. Knee osteoarthritis after the Marcacci technique does not appear to be greater than after conventional ACL reconstruction procedures.43
In 2012, Dejour et al. compared three groups of patients treated with double bundle ACL reconstruction (DB), bone-patellar tendonbone (BPTB) and bone-patellar tendon-bone in addiction with a modified Lemaire’s procedures (BPTB + L) at 2 years minimum of follow up. Clinical data included IKDC objective and subjective forms together with the pivot shift test. All patients were evaluated for the anterior tibial translation (ATT) for the medial and lateral compartments. No significant differences were noted between the groups in terms of absolute values of medial and lateral ATT. However, when comparing the lateral compartment ATT reduction mean values, the BPTB + L group was superior to the other two (P=0.0001). There was no statistical difference between the groups in terms of pivot shift and subjective/objective IKDC.27
In 2013, Saragaglia et al. described the results of their technique at an average follow-up of 76±12 months in 68 patients. The Lachman test was performed using the KT1000™ and compared with the contralateral side. Two patients had recurrent instability The average anterior drawer near extension (Lachman test) was 9.5±2.8 mm and the differential (side to side difference) was 2.5±3.4 mm representing statistically significant improvements. With regard to pivot shift, a statistically significant improvement with no pivot was found in 75% of the cases, pivot shift + in 21%, ++ in 4% and +++ in none of the patients. The average IKDC subjective score was 90±9. Ninety percent of patients had a score greater than 80 and 63% greater than 90.38
No clinical results are yet available for the Antwerp Monoloop procedure.
Discussion
The history of ALL starts in 1879, even before the invention of radiographs with Dr. Segond. In 1936 the Segond fracture was recognized on radiographs in the first clinical cases presented by Milch.44 In 1979, Woods et al. showed the correlation between the lateral capsular sign on radiographs and the tear of the ACL.45 This finding was also subsequently confirmed by Goldman et al.46 and Hess et al.47 Although the current literature is clearly lacking large series, some studies suggest that Segond fractures occur in 9% to 12% of all ACL injuries.48
The concept of anterolateral laxity is old as well as the use of anterolateral tenodesis for ALL injuries and these techniques were disregarded by most surgeons after the boom of arthroscopic surgery. Although controversies still exist regarding the ALL, a better understanding of its anatomy, function, and role in the pivot shift of the knee renewed the popularity of this structure.
Although isolated lateral plasties are obsolete, many surgeons are currently combining a lateral tenodesis with traditional ACL reconstruction. Whether or not these techniques produce better outcomes compared with isolated ACL reconstruction is still under debate. No randomized controlled trials are available comparing the traditional ACL reconstruction techniques isolated and combined with lateral plasties; randomized trials are required to determine if the ALL needs to be reconstructed or not.
Senior authors recommendation for combined anterior cruciate and anterolateral ligament injuries
In the light of these considerations, the authors add a lateral plasty to traditional ACL reconstruction in case of: i) marked rotational instability; ii) In some cases of high level athletes; iii) in case of revision ACL surgery. In case of revision ACL surgery, the author’s preferred procedure is the Marcacci technique. This technique is easy, inexpensive (using only 3 staples for fixation), can be performed with autologous hamstrings or allografts, and the surgeon does not have to worry about previous tunnels or graft fixation both proximally and distally. However, this technique is non anatomic (at least for the femoral graft position). In addition, discomfort at the proximal staples is common and frequently requires hardware removal.
It has to be mentioned that lateral tenodesis is not an alternative option to posterolateral corner reconstruction. In case of double varus or posterolateral corner lesion, these need to be addressed separately.
References
- 1.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014;42:2363-70. [DOI] [PubMed] [Google Scholar]
- 2.Bonasia DE, Dettoni F, Bruzzone M, et al. Single bundle anatomic anterior cruciate ligament reconstruction: Indications, technique and results. OA Sports Med 2013;1:13. [Google Scholar]
- 3.Andersson C, Odensten M, Gillquist J. Knee function after surgical or nonsurgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. Clin Orthop Relat Res 1991:255-63. [PubMed] [Google Scholar]
- 4.Chambat P, Guier C, Sonnery-Cottet B, et al. The evolution of ACL reconstruction over the last fifty years. Int Orthop 2013; 37:181-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zaffagnini S, Signorelli C, Lopomo N, et al. Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 2012;20:153-9. [DOI] [PubMed] [Google Scholar]
- 6.Snook GA. A short history of the anterior cruciate ligament and the treatment of tears. Clin Orthop Relat Res 1983:11-3. [PubMed] [Google Scholar]
- 7.Kocher MS, Steadman JR, Briggs KK, et al. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 2004;32:629-34. [DOI] [PubMed] [Google Scholar]
- 8.Segond PF. Recherches cliniques et experimentales sur les epanchements sanguins du genou par entorse. Prog Med 1879; 7:297-9, 319,-21, 40-1. [Google Scholar]
- 9.Monaco E, Ferretti A, Labianca L, et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc 2012; 20:870-7. [DOI] [PubMed] [Google Scholar]
- 10.Claes S, Vereecke E, Maes M, et al. Anatomy of the anterolateral ligament of the knee. J Anatomy 2013;223:321-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodds AL, Halewood C, Gupte CM, et al. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J 2014; 96B:325-31. [DOI] [PubMed] [Google Scholar]
- 12.Haims AH, Medvecky MJ, Pavlovich R, Jr., Katz LD. MR imaging of the anatomy of and injuries to the lateral and posterolateral aspects of the knee. AJR Am J Roentgenol 2003;180:647-53. [DOI] [PubMed] [Google Scholar]
- 13.Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 1976;58:173-9. [PubMed] [Google Scholar]
- 14.Johnson LL. Lateral capsualr ligament complex: anatomical and surgical considerations. Am J Sports Med 1979;7:156-60. [DOI] [PubMed] [Google Scholar]
- 15.Moorman CT, 3rd, LaPrade RF. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg 2005;18: 137-45. [DOI] [PubMed] [Google Scholar]
- 16.Campos JC, Chung CB, Lektrakul N, et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 2001;219:381-6. [DOI] [PubMed] [Google Scholar]
- 17.Vieira EL, Vieira EA, da Silva RT, et al. An anatomic study of the iliotibial tract. Arthroscopy 2007;23:269-74. [DOI] [PubMed] [Google Scholar]
- 18.Vincent JP, Magnussen RA, Gezmez F, et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 2012;20:147-52. [DOI] [PubMed] [Google Scholar]
- 19.Caterine S, Litchfield R, Johnson M, et al. A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc 2014. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 20.Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am j sports med 2015;43:669-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Claes S, Bartholomeeusen S, Bellemans J. High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belgica 2014;80:45-9. [PubMed] [Google Scholar]
- 22.Gossner J. The anterolateral ligament of the knee. Visibility on magnetic resonance imaging. Rev Bras Ortop 2014;9:98-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Porrino J, Jr., Maloney E, Richardson M, et al. The anterolateral ligament of the knee: MRI appearance, association with the segond fracture, and historical perspective. AJR Am J Roentgenol 2015;204:367-73. [DOI] [PubMed] [Google Scholar]
- 24.De Maeseneer M, Boulet C, Willekens I, et al. Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skeletal Radiol 2015;44:413-21. [DOI] [PubMed] [Google Scholar]
- 25.Sonnery-Cottet B, Archbold P, Rezende FC, et al. Arthroscopic identification of the anterolateral ligament of the knee. Arthrosc Tech 2014;3:e389-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lemaire M. Rupture ancienne du ligament croisé antérieur du genou; fréquence, clinique, traitement (46 cas). J Chirurgie 1967:311-20. [Google Scholar]
- 27.Dejour D, Vanconcelos W, Bonin N, Saggin PR. Comparative study between monobundle bone-patellar tendon-bone, double-bundle hamstring and mono-bundle bone-patellar tendon-bone combined with a modified Lemaire extra-articular procedure in anterior cruciate ligament reconstruction. Int Orthop 2013;37:193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ireland J, Trickey EL. Macintosh tenodesis for anterolateral instability of the knee. J Bone Joint Surg Br 1980;62:340-5. [DOI] [PubMed] [Google Scholar]
- 29.Arnold JA, Coker TP, Heaton LM, et al. Natural history of anterior cruciate tears. Am J Sports Med 1979;7:305-13. [DOI] [PubMed] [Google Scholar]
- 30.Losee RE, Johnson TR, Southwick WO. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am 1978;60:1015-30. [PubMed] [Google Scholar]
- 31.Andrews JR, Sanders R. A mini-reconstruction technique in treating anterolateral rotatory instability (ALRI). Clin Orthop Relat Res 1983:93-6. [PubMed] [Google Scholar]
- 32.Frank C, Jackson RW. Lateral substitution for chronic isolated anterior cruciate ligament deficiency. J Bone Joint Surg Br 1988;70:407-11. [DOI] [PubMed] [Google Scholar]
- 33.Christel P, Djian P. [Anterio-lateral extra-articular tenodesis of the knee using a short strip of fascia lata]. Rev Chir Orthop Reparatrice Appar Mot 2002;88:508-13. [Article in French]. [PubMed] [Google Scholar]
- 34.Ellison AE. Distal iliotibial-band transfer for anterolateral rotatory instability of the knee. J Bone Joint Surg Am 1979;61:330-7. [PubMed] [Google Scholar]
- 35.Roth JH, Kennedy JC, Lockstadt H, et al. Intra-articular reconstruction of the anterior cruciate ligament with and without extra-articular supplementation by transfer of the biceps femoris tendon. J Bone Joint Surg Am 1987;69:275-8. [PubMed] [Google Scholar]
- 36.Strum GM, Fox JM, Ferkel RD, et al. Intraarticular versus intraarticular and extraarticular reconstruction for chronic anterior cruciate ligament instability. Clin Orthop Relat Res 1989:188-98. [PubMed] [Google Scholar]
- 37.Marcacci M, Zaffagnini S, Iacono F, et al. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 1998;6:68-75. [DOI] [PubMed] [Google Scholar]
- 38.Saragaglia D, Pison A, Refaie R. Lateral tenodesis combined with anterior cruciate ligament reconstruction using a unique semitendinosus and gracilis transplant. Int Orthop 2013;37:1575-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamaguchi S, Sasho T, Tsuchiya A, et al. Long term results of anterior cruciate ligament reconstruction with iliotibial tract: 6-, 13-, and 24-year longitudinal follow-up. Knee Surg Sports Traumatol Arthrosc 2006;14:1094-100. [DOI] [PubMed] [Google Scholar]
- 40.Monaco E, Labianca L, Conteduca F, et al. Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthrosc 2007;15:1168-74. [DOI] [PubMed] [Google Scholar]
- 41.Monaco E, Maestri B, Conteduca F, et al. Extra-articular ACL reconstruction and pivot shift: in vivo dynamic evaluation with navigation. Am j Sports Med 2014;42:1669-74. [DOI] [PubMed] [Google Scholar]
- 42.Zaffagnini S, Marcacci M, Lo Presti M, et al. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 2006;14:1060-9. [DOI] [PubMed] [Google Scholar]
- 43.Marcacci M, Zaffagnini S, Giordano G, et al. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med 2009;37:707-14. [DOI] [PubMed] [Google Scholar]
- 44.Milch H. Cortical avulsion fracture of the lateral tibial condyle. J Bone Joint Surg Am 1936;18:159-64. [Google Scholar]
- 45.Woods GW, Stanley RF, Tullos HS. Lateral capsular sign: x-ray clue to a significant knee instability. Am J Sports Med 1979;7:27-33. [DOI] [PubMed] [Google Scholar]
- 46.Goldman AB, Pavlov H, Rubenstein D. The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol 1988; 151:1163-7. [DOI] [PubMed] [Google Scholar]
- 47.Hess T, Rupp S, Hopf T, et al. Lateral tibial avulsion fractures and disruptions to the anterior cruciate ligament. A clinical study of their incidence and correlation. Clin Orthop Relat Res 1994:193-7. [PubMed] [Google Scholar]
- 48.Claes S, Luyckx T, Vereecke E, Bellemans J. The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 2014;30:1475-82. [DOI] [PubMed] [Google Scholar]


