Abstract
The integrity of the meniscal root insertions is fundamental to preserve correct knee kinematics and avoid degenerative changes of the knee. Injuries to the meniscal attachments can lead to meniscal extrusion, decreased contact surface, increased cartilage stress, and ultimately articular degeneration. Recent and well designed studies have clarified the anatomy and biomechanics of the medial and lateral meniscal roots. Although the treatment of meniscal root tears is still controversial, many different techniques have been described for root repair. The goal of this review is to summarize the existing knowledge regarding meniscal root tears, including anatomy, biomechanics and imaging. In addition, the most common surgical techniques, together with the clinical outcomes, are described.
Key words: Meniscus, knee, root, repair, sports medicine
Introduction
The menisci are two fibrocartilaginous structures essential for correct knee function and joint preservation. About 40% to 70% of the load transmitted through the knee is borne by the menisci.1 The mechanical load absorption ability of the menisci is to convert axial load into circumferential hoop stress.2 The menisci also play a major role in maintaining knee stability.3 The integrity of the meniscal root insertions is fundamental to preserve correct knee kinematics and avoid degenerative changes of the joint.4
In 1991 Pagnani et al.3 first described meniscal root tears, and during the last 20 years the importance of meniscal root integrity became evident. An injury to the meniscal attachment, especially on the medial side, can lead to meniscal extrusion. Meniscal extrusion increases stress to the cartilage, by decreasing the contact surface.4 This causes impairment of hoop stress dissipation with accelerated articular degeneration.5
The goal of this article is to report the existing knowledge regarding meniscal root tears, including: pathological anatomy, diagnosis, and treatment. The authors searched the PubMed/Medline databases for English literature regarding pathological anatomy, diagnosis, and treatment of meniscal root tears. Due to the absence of specific MeSH terms for this topic, the search strategy was as follows: meniscal root AND/OR meniscal root tear AND/OR meniscal root avulsion AND/OR meniscal root repair AND/OR meniscal root anatomy. In addition, relevant references not included in the database search, but cited by downloaded articles, were included as well. Original research and review articles (Level I to IV) regarding anatomy, pathological anatomy, diagnosis, and treatment of meniscal root tears were included. Articles regarding pathological anatomy, diagnosis, and treatment of meniscal body tears were excluded.
Anatomy
The meniscal roots are 4 strong ligaments (Figure 1) connecting the meniscal horns to the tibial intercondylar region.6
Figure 1.
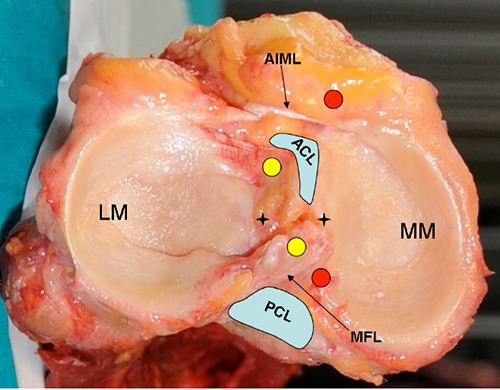
Anatomy of medial (red circles) and lateral (yellow circles) meniscal attachments. Black stars: apex of the medial and lateral intercondylar eminence. LM, lateral meniscus; MM, medial meniscus; ACL, anterior cruciate ligament tibial insertion; PCL, posterior cruciate ligament tibial insertion; AIML, anterior intermeniscal ligament; MFL, meniscofemoral ligament.
Anterior medial meniscus root
The anterior medial meniscus root (Figure 1) inserts along the anterior part of the medial intercondylar eminence, anterior to the apex. In a recent cadaveric study, the center of the tibial tuberosity and the medial tibial eminence apex were respectively 27.0 mm lateral and distal and 27.5 mm posterior to the center of the anterior medial meniscal root. The anterior medial root attachment had a mean area of 110.4 mm2 with a central attachment of 56.3 mm2.7 The intermeniscal ligament is present in 70% of knees and connects the anterior horn of the medial and lateral menisci.8 The intermeniscal ligament does not seem to be essential for tibiofemoral contact and meniscal function.9
Anterior lateral meniscus root
In the same study by LaPrade, the center of the anterior cruciate ligament (ACL) and the lateral tibial eminence apex were 5.0 mm posteromedial and 14.4 mm posterolateral to the center of the anterior lateral root, respectively (Figure 1).
The anterior lateral root attachment had a mean area of 140.7 mm2 (95% CI, 121.6-159.8) and inserted deeply beneath the ACL in all specimens. The overlap of the ACL on the anterior lateral root averaged 88.9 mm2 (95% CI, 63.3-114.6), comprising 63.2% of the anterior lateral root attachment.7
Posterior medial meniscus root
The posterior root (Figure 1) inserts just antero-medial to the posterior cruciate ligament (PCL) on the posterior aspect of the medial tibial intercondylar eminence.10 Johannsen et al.11 reported that the posterior root was approximately 9.6 mm posterior and 0.7 mm lateral to the apex of the medial tibial eminence. The root was also described as being 3.5 mm lateral to the medial tibial plateau articular cartilage inflection point and 8.2 mm anterior to the superior aspect of the PCL tibial attachment.12 The presence of shiny white fibers as a possible posterior expansion of the medial meniscus posterior root has also been described, although the role of this structure is still under debate.13
Posterior lateral meniscus root
Johannsen et al.11 described that the distance between the lateral tibial eminence apex and the center of the lateral posterior root was approximately 5.3 mm (Figure 1). Also, the root was 4.2 mm medial and 1.5 mm posterior to the lateral tibial eminence, 4.3 mm medial to the lateral tibial plateau articular cartilage margin, 12.7 mm anterior to the superior aspect of the PCL tibial attachment, and 10.1 mm posterior to the posteromedial corner of the anterior root attachment of the lateral meniscus.11,12,14
Epidemiology and risk factors
Meniscal root tears can occur chronically in degenerative knees or following acute traumas. Classically, the posterior horns of the menisci bear more load than the anterior horns, especially when the knee is flexed at 90°,15 and are more prone to lesions. No major studies are available regarding anterior roots tears. These studies describe a variety of iatrogenic injuries to the anterior roots, such as when drilling the tibial tunnel for ACL reconstruction,16 or introducing an anterograde intramedullary tibial nail.17
Medial meniscus posterior root tear (MMPRT) is the most common lesion, with a prevalence of 10 to 21% of meniscal surgeries.18 Because of its reduced mobility and significant loads, the posterior root of the medial meniscus is more prone to lesions than the posterior lateral root.19-21 Increased incidence of MMPRT has been described in those part of the world, where kneeling and squatting are common daily activities.18 However, other studies did not identify frequent lotus position or squatting as major risk factors for this condition. Increased BMI, varus mechanical axis, female sex, low activity level, together with some unknown intrinsic factors, have been associated with an increased risk of MMPRT.22
Although MMPRT could be the consequence of an acute trauma, especially in multiligamentous injuries,23 the majority of patients do not report major traumatic events.24 More frequently these are chronic injuries associated with meniscal extrusion, reduced shock absorption, joint degeneration and ultimately osteoarthritis. MMPRT results in increased peak contact pressure, with biomechanical consequences similar to meniscectomy.25,26 In addition, an higher risk of spontaneous osteonecrosis of the knee (SPONK) has been described in association with MMPRT, compared with simple radial tears of the meniscus.27 PMMRT is associated with SPONK in 80% of patients, while medial meniscal tears in 67%.28
Lateral meniscus posterior root tears (LMPRT) seem to be more frequently associated with knee sprains.29 According to De Smet et al.30 a LMPRT is identifiable in 8% of ACL injuries and in 0.8% of patients with an intact ACL.
In a finite element study,31 increased loads have been described in the lateral compartment with LMPRT. However, the integrity of the meniscofemoral ligament seemed to protect the lateral meniscus from extrusion.
Brody et al.6 in an Magnetic Resonance Imaging (MRI) study described a 14% prevalence of lateral meniscal extrusion in case of LMPRTs with intact meniscofemoral ligaments, and 60% in case of LMPRTs with disrupted meniscofemoral ligaments. At the time of injury, combined ACL- LMPRT lesions are not associated with increased risk of meniscal extrusion compared with isolated ACL injuries.32
Diagnosis
Clinical examination
The clinical examination of meniscal root tears can be difficult. The differential diagnosis with posterior horn meniscal body tear is challenging. In acute injuries, symptoms on the lateral side could not be present or hidden by associated ACL tears. In the chronic setting, patients may complain about posterior joint line pain mostly at maximum degrees of flexion or, more rarely, about locking or giving way of the knee.33 Recently, Seil et al.34 described a clinical test for medial meniscal root avulsions. The test is performed by palpating the medial meniscal extrusion when performing a varus stress in full extension. No data are available yet regarding sensitivity or specificity of this sign.
Imaging
Although the diagnosis of meniscal root tears is challenging despite the use of advanced imaging techniques, MRI is considered the gold standard in diagnosing these lesions.35 Combined ACL tears do not seem to affect the diagnostic accuracy of MRI for meniscal root avulsions.30 Controversies still exist regarding the most reliable MRI technique and image cut for detecting meniscal root tears.4 Fat-suppressed volume isotropic turbo spin echo acquisition (FS 3D VISTA) with Reader Defined Axial reconstruction has recently been described as a powerful tool in detecting radial and root tears of the menisci.36 Traditionally, 2 MRI signs have been described as pathognomonic of meniscal root tears and these are: the ghost sign and meniscal extrusion (Figure 2). The ghost sign (Figure 2A) is characterized by the absence of the posterior horn of the meniscus in sagittal cuts.4,37
Figure 2.
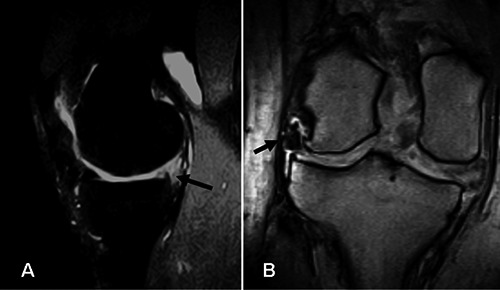
A) Sagittal magnetic resonance imaging (MRI) cut of a knee showing the ghost sign at the level of the medial meniscus posterior horn (black arrow). B) Coronal MRI of a left knee showing lateral meniscus extrusion (black arrow) and tricompartmental knee degeneration.
Meniscal extrusion (Figure 2B) is defined as an external displacement of the meniscus from the tibial articular cartilage. This is usually the result of considerable disruption of the circumferential fibers of the meniscus with loss of the ability to resist hoop strain. Meniscal extrusion has been associated with degenerative joint disease, joint effusion, and meniscal tears.18,38 Forty-two to 64% of knees with medial meniscus extrusion had associated posterior root tears on MRI.4,20 Meniscal extrusion has also been described in association with medial compartment cartilage degeneration,39,40 with a significant threshold of 3 mm displacement.12 Some authors showed that the 3 mm threshold had high specificity (98%),41 but low sensitivity (54%), and introduced the meniscal length/transverse ratio (L/T ratio) as another index for MMPRTs. The mean L/T ratio was 13% with meniscal root tears and 5% in the control groups. An extrusion ratio threshold was determined at 10% (79% sensitivity, 86% specificity). Also the presence of meniscal ossicles was described as associated with meniscal root tears.42
Subchondral marrow edema deep to the MMPRT was described as a harbinger of meniscal root failure.43 The edema usually resolved, when meniscal root tear occurs.43
Treatment
The treatment options for meniscal root avulsions include conservative management, meniscectomy and repair. Factors determining the decision making process include: age of the patient, overall condition of the cartilage, symptoms, and chronicity of the lesion. According to the existing literature,12 the authors’ decision making algorithm is as described in Figure 3. It has to be mentioned here that all studies available regarding the treatment of meniscal root tears are level III or IV studies, and therefore the grade of recommendation (A-D) of the proposed treatments is C or D, according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE). The level of evidence of the most relevant papers reporting on the outcomes of the different treatments has been reported in the results section.
Figure 3.
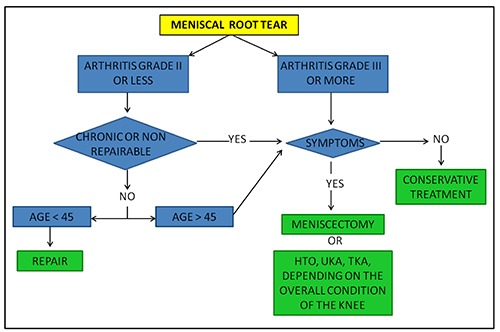
Authors’ decision making algorithm for meniscal root avulsions.
Malalignment should also be considered as a risk factor for meniscal repair failure. However, the role of osteotomy in meniscal root tears has yet to be determined.
Conservative treatment options include: rest, cryotherapy, NSAIDs, intrarticular corticosteroid injections, and physical therapy.
Surgical treatment
Although the traditional treatment of the meniscal root tears was observation or meniscectomy, concerns regarding the long term articular degeneration with these treatments increased the popularity of repair techniques.44 According to a recent cadaveric study, meniscal root repair improved contact area and decreased cartilage stress compared with untreated root tears.45,46 Whether or not meniscal root repair is able to restore normal knee biomechanics is still under debate.45,46
Meniscectomy
The patient is positioned supine after spinal or general anaesthesia. A tourniquet is positioned at the proximal thigh. The foot of the bed is dropped down and the thigh is held by an arthroscopic leg holder. An arthroscopic knee balance is performed through standard anteromedial and anterolateral portals. The lesion is debrided with a basket and arthroscopic shavers. Attention should be paid to remove only the free flap of the meniscal root and, in case of partial root avulsions, to preserve the residual tibial attachment.
Repair
Patient’s prepping, positioning, and arthroscopic knee balance is as described for meniscectomy. The tear pattern is evaluated. Depending on the tear pattern, repair techniques include pull-out (transosseous), suture anchors, and side to side repair (Figure 4).47,48 Additional posteromedial and posterolateral portals can be established to facilitate the procedure.
Figure 4.
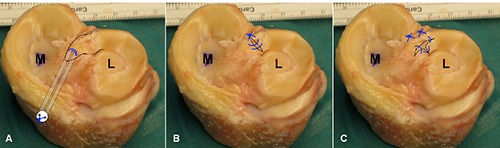
Specimens showing different repair techniques, according to different lesion patterns; A) Avulsion of the posterior root of the lateral meniscus. In this case a pull-out technique can be used. Alternatively a suture anchor technique is an equivalent option. B) Lateral meniscus posterior root radial tear, with preserved tibial attachment. In this case an all-inside side to side suture is recommended. C) Complex T shaped tear of the posterior root of the lateral meniscus. In this cases multiple stitches are required according to the preferred meniscal suturing technique (all-inside, out-in, in-out). M, medial compartment; L, lateral compartment.
Repair with pull-out (transosseous) technique
The pull-out technique (Figure 4A and 5) is generally indicated when the root is avulsed from the tibial insertion and no multiligamentous reconstruction (with multiple tibial tunnels) is planned. With this technique, 1 or 2 small tunnels (2 mm) are drilled with an ACL guide at the level of the avulsed meniscal root. A curved suture passer is generally used to arm the meniscal root with 2 n°0 non absorbable sutures. The sutures are then retrieved through the tunnels from the anteromedial tibia. In case of LMPRT combined with ACL tear, the pull-out tunnel can be drilled from the anterolateral tibia, in order to avoid interference with the ACL tibial tunnel. The sutures are then tightened distally with different fixation options, including pull-out buttons,49 screws,50 or bone bridges.51 In case of inadequate visualization, additional posteromedial or posterolateral portals can be performed.52
Figure 5.
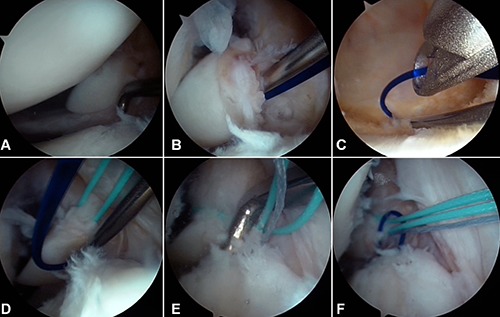
Lateral meniscus posterior root repair (pull-out technique). A) Complete detachment of the lateral meniscus posterior root (above the probe). B,C) Armature of the posterior root with a spinal needle and a non-braided shuttle suture. D) After substitution of the shuttle suture with a non resorbable n°2 braided suture, the procedure is repeated in order to have 2 stitches arming the root. Suture. E) Anterior cruciate ligament giude used to drill a 2-mm tummel at the level of the lateral meniscus posterior horn attachment. F) The sutures are retrieved through the tunnel from the anterior tibia, with a Huson suture passer, and fixed with a pull-out button.
Repair with suture anchors
In multiligamentous injuries or in previously reconstructed knees (i.e. for ACL reconstruction), transosseous fixation is not advisable, due to the risk of tunnel interference. In this case suture anchors are generally used in order to achieve stable fixation back to the tibia. Suture anchors placement usually requires posterior portals. The arthroscopic knots can be then tightened through the anterior portals.53 With this technique, an arthroscopic knot is placed directly on the meniscus root with a knot pusher and a theoretical more precise tensioning of the repair. On the other hand, anchor loosening and cartilage wear, due to the prominent knot, are possible complications.12
Repair with side to side sutures
In case of complex T shaped lesions or when the meniscus is torn close to the intact tibial insertion, a side to side suture can be performed (Figure 4). The stitches can be positioned according to the preferred meniscal suture technique, including outside-in, inside-out, and all inside methods. In case of posterior root tears, an all inside technique with possible additional posterior portals is preferred, for an easy approach to the lesion.
Biomechanics of repaired meniscal root tears
In an in vitro study on porcine knees, Stärke et al. investigated the potential effect of a nonanatomic repair of the medial meniscal horn attachment on the resultant circumferential tension and local cartilage stress. A nonanatomic position of the horn attachment had a significant effect on the resultant tension. Placing the horn attachment 3 mm medially decreased the tension at the horn attachment by 49% to 73%, depending on knee flexion angle and femorotibial load. On the other hand, fixation of the root in a lateral position resulted in a relative increase in the tension by 28% to 68%. Lower levels of meniscal hoop tension caused increased cartilage stress.54
Cerminara et al.55 quantified the time-zero displacement of the posterior medial meniscal root in response to cyclic loading after transtibial pull-out repair (2-simple suture configuration) and the individual contributions to displacement of: i) suture elongation, ii) button-bone interface, and iii) meniscussuture interface. After 1000 cycles, the meniscus-suture component displaced significantly more than the button-bone component and suture elongation component. Displacement of the button-bone and suture elongation components was not significantly different after 1000 cycles Anz et al. tested in 21 cadaveric knees the strength of the sutures arming the medial and lateral posterior roots. Four repair constructs were evaluated: 2 simple sutures, 1 inverted mattress suture, 1 double-locking loop suture, and 2 double-locking loop sutures. The double-locking loop suture repair technique had significantly higher failure loads compared with the other methods.56
Kopf et al. tested the maximum failure load of the native meniscal roots compared with 3 fixation techniques: 2 simple stitches, modified Kessler stitch, and loop stitch using a suture shuttle. None of the fixation techniques recreated the strength of the native roots. The modified Kessler stitch was the strongest technique compared with the other methods.57
Post-operative management
Although a real consensus regarding the post-operative regimen of meniscal root repair has not been established yet, a biomechanical cadaver study showed that rotations, weight bearing, and flexion increased the tensile forces on repaired MMPRTs.58 Most of the authors recommend a hinged knee brace and toe touch weight bearing for 6 weeks. The brace is locked in extension for 2 weeks and then 20° of flexion are added every week. Weight bearing and flexion over 90° are allowed at 6 weeks after surgery.
Results
Shelbourne et al. evaluated the long-term radiographic and subjective results of 33 patients with LMPRTs left in situ during ACL reconstruction at a mean of 10 years follow-up and compared the outcomes with a matched control group with no meniscal injuries (Level of evidence III). Mild lateral joint-space narrowing was noticed in the cases, but no significant differences were noted in terms of subjective and objective scores compared with the controls.59
Ozkoc et al. in a review of 67 patients with a mean follow-up of 56 months showed that arthroscopic partial meniscectomy for MMPRTs generally improved symptoms but did not arrest the progression of osteoarthritis (Level of evidence IV).35
Kim et al. in a retrospective comparison study of 58 patients (28 meniscectomies, 30 repairs) at an average follow-up of 48.5 months described significantly better clinical and radiologic results with arthroscopic pull-out repair of a MMPRT compared with partial meniscectomy (Level of evidence III). Healing and restoration of hoop tension of the meniscus was also observed on MRI and second-look arthroscopy.37
Lee et al. retrospectively evaluated 20 consecutive patients at an average 31.8 month follow-up after pullout suture repair for MMPRTs and showed a significant improvement of HSS and Lysholm knee scores after surgery (Level of evidence IV).33
Kim et al. compared the functional and radiographic results of arthroscopic suture anchor repair of the MMPRT with pullout repair (45 patients, 25.9 months of follow-up), without finding any significant difference between the groups (Level of evidence III).24
Ahn et al. evaluated the effectiveness of all-inside repair of LMPRTs, in 25 patients at a mean follow-up of 18 months. The authors reported good clinical and MRI results with reduction of sagittal plane extrusion (Level of evidence IV).48
Good outcomes have been reported for meniscal root repair, also in skeletally immature patient in a small case series of 2 patients.60
Conclusions
From a biomechanical point of view, meniscal root avulsions significantly alter the load transmission through the knee joint. The clinical implications of these biomechanical changes need to be determined with further Level I or II studies.
Some controversies exist regarding the optimal treatment of LMPRTs,59,48 when associated with ACL tears. The LMPRTs can be left untreated, with no significant clinical differences compared with arthroscopic repair at midterm follow-up (Grade of recommendation C).59 Further studies with longer follow up are needed to confirm this recommendation.
Repair of MMPRTs seems to result in better outcomes compared with partial meniscectomy, independently of the technique used (pull-out vs suture anchor) (Grade of recommendation C).24,33
Despite good initial clinical outcomes, second look arthroscopies and post operative MRI showed high rates of non healing.61
High quality (level I and II) studies are required to determine the effectiveness of meniscal root repair and the correct indications.
References
- 1.Kidron A, Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy 2002;18:254-6. [DOI] [PubMed] [Google Scholar]
- 2.Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop 1990:19-31. [PubMed] [Google Scholar]
- 3.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy 1991;7:297-300. [DOI] [PubMed] [Google Scholar]
- 4.Lerer DB, Umans HR, Hu MX, Jones MH. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 2004;33:569-74. [DOI] [PubMed] [Google Scholar]
- 5.Hein CN, Deperio JG, Ehrensberger MT, Marzo JM. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee 2011;18:189-92. [DOI] [PubMed] [Google Scholar]
- 6.Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 2006;239:805-10. [DOI] [PubMed] [Google Scholar]
- 7.LaPrade CM, Ellman MB, Rasmussen MT, et al. Anatomy of the anterior root attachments of the medial and lateral menisci: a quantitative analysis. Am J Sport Med 2014; 42:2386-92. [DOI] [PubMed] [Google Scholar]
- 8.Berlet GC, Fowler PJ. The anterior horn of the medical meniscus. An anatomic study of its insertion. Am J Sport Med 1998; 26:540-3. [DOI] [PubMed] [Google Scholar]
- 9.Poh S-Y, Yew K-SA, Wong P-LK, et al. Role of the anterior intermeniscal ligament in tibiofemoral contact mechanics during axial joint loading. Knee 2012;19:135-9. [DOI] [PubMed] [Google Scholar]
- 10.Nicholas SJ, Golant A, Schachter AK, Lee SJ. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sport Tr A 2009;17:1433-6. [DOI] [PubMed] [Google Scholar]
- 11.Johannsen AM, Civitarese DM, Padalecki JR, et al. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sport Med 2012;40:2342-7. [DOI] [PubMed] [Google Scholar]
- 12.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sport Med 2014. 42:3016-30. [DOI] [PubMed] [Google Scholar]
- 13.Anderson CJ, Ziegler CG, Wijdicks CA, et al. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am 2012;94:1936-45. [DOI] [PubMed] [Google Scholar]
- 14.Ziegler CG, Pietrini SD, Westerhaus BD, et al. Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sport Med 2011;39:743-52. [DOI] [PubMed] [Google Scholar]
- 15.Fox AJS, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health 2012;4:340-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaPrade CM, Smith SD, Rasmussen MT, et al. Consequences of tibial tunnel reaming on the meniscal roots during cruciate ligament reconstruction in a cadaveric model, part 1: the anterior cruciate ligament. Am J Sport Med 2015;43:200-6 [DOI] [PubMed] [Google Scholar]
- 17.Ellman MB, James EW, Laprade CM, Laprade RF. Anterior meniscus root avulsion following intramedullary nailing for a tibial shaft fracture. Knee Surg Sports Traumatol Arthrosc 2015;23:1188-91. [DOI] [PubMed] [Google Scholar]
- 18.Bin S-I, Kim J-M, Shin S-J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy 2004;20:373-8. [DOI] [PubMed] [Google Scholar]
- 19.Vedi V, Williams A, Tennant SJ, et al. Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br 1999;81:37-41 [DOI] [PubMed] [Google Scholar]
- 20.Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? Am J Roentgenol 2004;183:17-23 [DOI] [PubMed] [Google Scholar]
- 21.Papalia R, Vasta S, Franceschi F, et al. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull 2013;106:91-115. [DOI] [PubMed] [Google Scholar]
- 22.Hwang B-Y, Kim S-J, Lee S-W, et al. Risk factors for medial meniscus posterior root tear. Am J Sport Med 2012;40:1606-10. [DOI] [PubMed] [Google Scholar]
- 23.Mariani PP, Iannella G, Cerullo G, Giacobbe M. Avulsion of both posterior meniscal roots associated with acute rupture of the anterior cruciate ligament. J Orthop Traumatol 2014. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J-H, Chung J-H, Lee D, et al. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27:1644-53. [DOI] [PubMed] [Google Scholar]
- 25.Allaire R. Biomechanical consequences of a tear of the posterior root of the medial meniscus similar to total meniscectomy. J Bone J Surg Am 2008;90:1922-31. [DOI] [PubMed] [Google Scholar]
- 26.Guermazi A, Hayashi D, Jarraya M, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology 2013;268:814-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sung JH, Ha JK, Lee DW, et al. Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: comparison with horizontal tear. Arthroscopy 2013;29:726-32. [DOI] [PubMed] [Google Scholar]
- 28.Robertson DD, Armfield DR, Towers JD, et al. Meniscal root injury and spontaneous osteonecrosis of the knee - an observation. J Bone Joint Surg Br 2009;91:190-5. [DOI] [PubMed] [Google Scholar]
- 29.Tandogan RN, Taser O, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc 2004;12:262-70. [DOI] [PubMed] [Google Scholar]
- 30.De Smet AA, Blankenbaker DG, Kijowski R, et al. MR Diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. Am J Roentgenol 2009;192:480-6. [DOI] [PubMed] [Google Scholar]
- 31.Bao HRC, Zhu D, Gong H, Gu GS. The effect of complete radial lateral meniscus posterior root tear on the knee contact mechanics: a finite element analysis. J Orthop Sci 2013;18:256-63. [DOI] [PubMed] [Google Scholar]
- 32.Pula DA, Femia RE, Marzo JM, Bisson LJ. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury?: a case control study. Am J Sport Med 2014;42:173-6. [DOI] [PubMed] [Google Scholar]
- 33.Lee JH, Lim YJ, Kim KB, et al. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy 2009;25:951-8. [DOI] [PubMed] [Google Scholar]
- 34.Seil R, Duck K, Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 2011;19:2072-5. [DOI] [PubMed] [Google Scholar]
- 35.Ozkoc G, Circi E, Gonc U, et al. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 2008;16:849-54. [DOI] [PubMed] [Google Scholar]
- 36.Lim D, Lee YH, Kim S, et al. Fat-suppressed volume isotropic turbo spin echo acquisition (VISTA) MR imaging in evaluating radial and root tears of the meniscus: focusing on reader-defined axial reconstruction. Eur J Radiol 2013;82:2296-302. [DOI] [PubMed] [Google Scholar]
- 37.Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 2011;27:346-54. [DOI] [PubMed] [Google Scholar]
- 38.Breitenseher MJ, Trattnig S, Dobrocky I, et al. MR imaging of meniscal subluxation in the knee. Acta Radiol 1997;38:876-9. [DOI] [PubMed] [Google Scholar]
- 39.Choi C-J, Choi Y-J, Lee J-J, Choi C-H. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 2010;26:1602-6. [DOI] [PubMed] [Google Scholar]
- 40.Puig L, Monllau JC, Corrales M, et al. Factors affecting meniscal extrusion: correlation with MRI, clinical, and arthroscopic findings. Knee Surg Sports Traumatol Arthrosc 2006;14:394-8. [DOI] [PubMed] [Google Scholar]
- 41.Park H-J, Kim SS, Lee S-Y, et al. Medial meniscal root tears and meniscal extrusion transverse length ratios on MRI. Brit J Radiol 2012;85:e1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mohankumar R, Palisch A, Khan W, et al. Meniscal ossicle: posttraumatic origin and association with posterior meniscal root tears. Am J Roentgenol 2014;203:1040-6. [DOI] [PubMed] [Google Scholar]
- 43.Umans H, Morrison W, DiFelice GS, et al. Posterior horn medial meniscal root tear: the prequel. Skeletal Radiol 2014;43:775-80. [DOI] [PubMed] [Google Scholar]
- 44.Koenig JH, Ranawat AS, Umans HR, DiFelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy 2009;25:1025-32. [DOI] [PubMed] [Google Scholar]
- 45.Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med 2008;37:124-9. [DOI] [PubMed] [Google Scholar]
- 46.Kim JG, Lee YS, Bae TS, et al. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 2013;21:2121-5. [DOI] [PubMed] [Google Scholar]
- 47.Wang KH, Hwang DH, Cho JH, et al. Arthroscopic direct repair for a complete radial tear of the posterior root of the medial meniscus. Clin Orthop Surg 2011;3:332-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahn JH, Lee YS, Chang J-Y, et al. Arthroscopic all inside repair of the lateral meniscus root tear. Knee 2009;16:77-80. [DOI] [PubMed] [Google Scholar]
- 49.Padalecki JR, Jansson KS, Smith SD, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med 2014;42:699-707. [DOI] [PubMed] [Google Scholar]
- 50.Kim Y-M, Rhee K-J, Lee J-K, et al. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy 2006;22:795.e1-4. [DOI] [PubMed] [Google Scholar]
- 51.Raustol OA, Poelstra KA, Chhabra A, Diduch DR. The meniscal ossicle revisited: etiology and an arthroscopic technique for treatment. Arthroscopy 2006;22:687.e1-3. [DOI] [PubMed] [Google Scholar]
- 52.Ahn JH, Wang JH, Yoo JC, et al. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc 2007;15:1510-3. [DOI] [PubMed] [Google Scholar]
- 53.Engelsohn E, Umans H, Difelice GS. Marginal fractures of the medial tibial plateau: possible association with medial meniscal root tear. Skeletal Radiol 2007;36:73-6. [DOI] [PubMed] [Google Scholar]
- 54.Stärke C, Kopf S, Gröbel K-H, Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: a biomechanical study. Arthroscopy 2010;26:358-65. [DOI] [PubMed] [Google Scholar]
- 55.Cerminara AJ, LaPrade CM, Smith SD, et al. Biomechanical evaluation of a transtibial pull-out meniscal root repair: challenging the bungee effect. Am J Sports Med 2014;42:2988-95. [DOI] [PubMed] [Google Scholar]
- 56.Anz AW, Branch EA, Saliman JD. Biomechanical comparison of arthroscopic repair constructs for meniscal root tears. Am J Sport Med 2014;42:2699-706. [DOI] [PubMed] [Google Scholar]
- 57.Kopf S, Colvin AC, Muriuki M, et al. Meniscal root suturing techniques: implications for root fixation. Am J Sport Med 2011;39:2141-6. [DOI] [PubMed] [Google Scholar]
- 58.Stärke C, Kopf S, Lippisch R, et al. Tensile forces on repaired medial meniscal root tears. Arthroscopy 2013;29:205-12. [DOI] [PubMed] [Google Scholar]
- 59.Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sport Med 2011;39:1439-43. [DOI] [PubMed] [Google Scholar]
- 60.Sonnery-Cottet B, Mortati R, Archbold P, et al. Root avulsion of the posterior horn of the medial meniscus in skeletally immature patients. Knee 2014;21:1291-6. [DOI] [PubMed] [Google Scholar]
- 61.Petersen W, Forkel P, Feucht MJ, et al. Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg 2014;134:237-55. [DOI] [PubMed] [Google Scholar]


