Abstract
Infantile hemangiomas as frequent infancy tumors have been a controversial issue of medical scientists worldwide. Their clinical aspects are various and their physiopathology is yet to be fully understood. Numerous publications outline the characteristics, causes, evolution possibilities and therapeutic approaches. Deciding whether to treat or not is the main question of this kind of pathology. Hemangiomas that have complications or can cause irreversible damage need therapy. This is a brief review of up-to-date information regarding the presentation of infantile hemangiomas and target-therapies.
Keywords: infantile hemangiomas, etiopathogenesis, therapy
Introduction
Infantile hemangiomas represent the most common type of benign tumors of the infancy, with a prevalence estimated at 1–10% of the infants worldwide [1]. Even though the disorder is mostly harmless [2], there are some specific situations in which treatment is necessary, even urgent [1].
These tumors develop in the period of infancy, only 20% [3] of them being present at birth, with an increased frequency in the female gender, the white race [4] and in low birth weight infants [5]. An increased incidence of hemangiomas is also noted in twins [6]. Some studies reported the disorder in many siblings of the same family, with non-affected parents, pointing out a possible genetic immixture [7].
The hypothesis of pathogenesis supports the idea that hemangiomas develop by cellular hyperplasia and by the proliferation of endothelial cells [8]. Important research has shown that angiogenic and vasculogenic factors stimulate their proliferation [8,9,10,11] and these markers influence all the evolutionary phases of hemangiomas.
To date, the most used therapeutic agents were represented by corticotherapy, either systemic or topical. Their effects on the evolution of hemangioma are beneficial, but the side-effects are significant [8]. Since the discovery in 2008 by Laute-Labreze, Propranolol has been used in infantile hemangioma therapies, with good results and few adverse effects, which are of minimal severity [12]. Still, there are multiple possibilities of therapeutic approaches that include surgery, radiotherapy, laser therapy, embolization, Imiquimod or Vincristine, therapies that need to be individualized.
Infantile hemangiomas remain a current challenge for the medical science, raising constant questions about risk factors, prognostic factors, pathogenesis, evolution and treatment.
Ethiopathogenesis
The pathogenesis of infantile hemangiomas is still vague. Researchers worldwide presently consider the disorder a pressing issue, and that is why several studies have been conducted in order to elucidate the exact mechanism of developing infantile hemangioma. Multiple theories have been outlined, but there are still more to be discovered.
The clonality of endothelial cells of the hemangioma [4,8]. Hypoxia and acidosis are known to create a disturbance of the equilibrium between proangiogenic and antiangiogenic factors. These situations stimulate endothelial cell proliferation and thereafter growth of the infantile hemangioma [10].
The theory of hypoxia and the successive angiogenesis [10,13,14]. In addition to the proliferation of endothelial cells, intrauterine or perinatal hypoxia and acidosis, both stimulate angiogenesis by increasing the secretion of VEGF (vascular endothelial growth factor). HIF1- alpha (hypoxia-inducible factor 1 alpha) induces the gene-transcription of VEGF, which is the most powerful angiogenic factor.
Placental hypothesis:
The injury of placenta is supposed to cause the embolization of endothelial cells and the consecutive overflow of these into the fetal circulation. Through the POF (patent foramen ovale) the cells penetrate to the tissues, and abide throughout gestation. The placenta releases angiostatic factors (sFLT1), but after birth these inhibitory factors are wasted, which allows the development of the infantile hemangioma by endothelial cell proliferation [8,15].
The vasculogenesis theory:
This theory supports the idea that hemangiomas form from undifferentiated progenitor stem cells. A high number of CD133+, CD34+ endothelial cells have been detected in the blood of children with proliferative infantile hemangiomas [16].
The hormonal theory:
High levels of 17-beta-estradiol were noted in several studies, simultaneously with high numbers of estradiol receptors at hemangioma tissue-surfaces in their proliferative phase [9,17].
Clinical aspects and evolution
Infantile hemangiomas present as one or more tumors of variable dimensions and aspects, with predilection in the head and neck area [17]. Other areas, as well as organs, can be affected.
In the majority of cases they are singular, only in 10–25% of cases they are multiple tumors [4]. Multiple hemangiomas always question simultaneous organ involvement. Even without clear proof, a tight connection between these has been observed, a proportion of 83% cases with multiple hemangiomas are with concurrent visceral involvement [4].
Superficial hemangiomas present as round or oval tumors, lobulated or with a fine surface, more often in the head-neck area [17], 1 to 25 cm in size. They are the most frequent type, being encountered in 50–60% of cases [4].
Deep hemangiomas come as soft, bluish masses, some with superficial telangiectasia, and are the rarest type - 15% [4].
Mixed hemangiomas combine aspects of the two above mentioned. (see Tab. I)
Tabel I.
Infantile hemangioma types.
In most of the cases, hemangiomas develop in the first 2–4 weeks of life, but 20% of them can be present at birth. The lesion is at first a pale-white to blue-grey macula, depending on its profoundness, or a papule with the same characteristics. They grow during a variable period of time until 6–9 months, after which they involute, following the characteristic evolution. Thus 50% regress by the age of 5 years and 90% regress by the age of 9 [3]. The regression is established by the reduction of dimensions, the colour intensity; the skin comes back to normal, or remains with a residue of telangiectasia, hypopigmentation, scars or fiber-fatty deposits [3].
Symptoms vary with the location. An airway hemangioma is accompanied by feeding difficulty, stridor, loud breathing and a typical cry, all of them representing signs of airway obstruction [19]. Subglottis hemangiomas are life-threatening [19]. Chin hemangiomas are frequently associated with hemangiomas in the upper airway system [3]. Visceral hemangiomas, for example hepatic ones, present with hepatomegaly and an abdominal compartment syndrome [4]. Concurrent thyroid damage, often seen in hepatic hemangiomatosis, manifests with the specific symptoms of hypothyroidism, and is a high-mortality risk emergency. Usually, with the resolution of the hemangioma hypothyroidism also subsides [4], but in some cases intravenous substitute thyroid hormones are necessary. Dorsal hemangiomas always question the existence of spinal cord malformations [3]. Eyelid or periocular hemangiomas express with low visual acuity, amblyopia or strabismus [20]. Facial hemangiomas associate with CNS malformations or ophthalmic vessel anomalies [3]. Anogenital hemangiomas associate with malformations in the area, such as the absence of small or big labia, hemiclitoris or the absence of the anal canal [21]. Hemangiomas of the auditory canal lead to obstructive hearing loss and can destroy the helix or the auricular pavilion [4].
Aproximately 10% of infantile hemangiomas develop complications in their evolution and need individualized therapy [2,22]. Of this sort are especially the perineal, periocular and airway hemangiomas [2]. The most common complications are ulceration, infection and hemorrhage. Systemic complications come with Kassabach Meritt syndrome, characterized by the association of cutaneous and visceral lesions of variable aspects and dimensions, and with extracutaneous manifestations, such as consumption coagulopathy [4]. Consumption coagulopathy is accompanied by thrombocytopenia, hypofibrinogenemia, low D-dimmers and low coagulation factors [4]. PHACE syndrome (posterior fossa abnormalities, hemangiomas, arterial lesions, cardiac abnormalities, eye abnormalities) or Lumber syndrome are also disorders seen with infantile hemangiomas and are characterized by the association with several other anomalies in the upper or lower part of the body [23].
Treatment
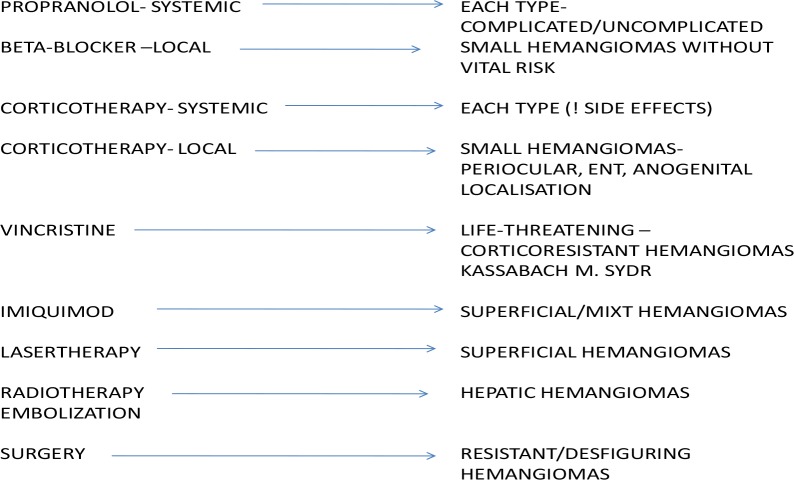
Most of the infantile hemangiomas lend themselves to the “wait-and-see” therapy, but some of them need immediate treatment [18]. Their localization is one of the essential elements of the therapy approach. Hemangiomas in the periocular, eyelid, airway or ano-genital area, are at high risk of complications and need an early individualized therapy approach [14] (see Fig. 1).
Figure 1.
Treatment options for infantile hemangiomas.
Systemic corticotherapy has been used as a first-line therapy for a long time, using its inhibitory effects on angiogenesis [8]. Prednisolone is of choice, in a dose of 2–5mg/kg/day, once a day, for 4–8 weeks [8]. If no effect is seen in the first 4 weeks, the hemangioma is considered corticoresistant and other options are taken into consideration [8]. Betamethasone is another option, in doses of 0.10–0.30 mg/kg/day. Responses to steroids are in most cases good, 84% with healing evidence [14]. An important aspect of steroid therapy is that of adverse reactions, which are frequent and significant. Growth retardation, gastro-esophageal reflux [24], vomiting [4], behavior disorders [25], high blood pressure [25,4], acne, cushingoid facies, increased appetite which leads to weight gain [4, 24], obstructive hypertrophic cardiomyopathy [22] are some of the adverse effects of steroids. This highlights the importance of follow-up of patients taking this kind of treatment. Topical steroids or intralesional steroids can also be used in order to avoid systemic effects, but these can only be used in small hemangiomas and without serious complications [14].
Nowadays, the therapeutic options are multiple and can be individualized based on the hemangioma characteristics. Since 2008, therapy with Propranolol has been a first-option therapy in most of the situations. Several studies have pointed out its use in infantile hemangiomas treatment, even in situations with complications. It may be used in every type of hemangioma, even in big, complicated ones [26,27,28]. The usual dose starts with 0.5 mg/kg/day with a possibility to increase the dose up to 2 mg/kg/day [14]. The duration is based on dimensions, location and complications, but on average is of 1 year [29]. As with corticotherapy, if there are no responses in the first 4 weeks, they are considered to be non-responsive to Propranolol. However, there are studies suggesting that there might be a slow rhythm of healing and propose a longer period of therapy until declaring a hemangioma non-responsive [30]. The mean response rate is about 98% [29]. Adverse reactions are possible, but are rare and mostly mild. The most frequent ones are bradycardia, hypoglycemia and bronchospasm [31,32]. Severe allergic reactions are rarely seen, and present themselves as lingual edema, dyspnea and angina pectoris [32]. Conversely, blood pressure and heart rate variations are considered markers of good response to the treatment [33]. In some cases, topical beta-blockers can be used to avoid systemic effects. Timolol ointment has been used in some studies with good responses [34,35]. Used once or twice a day by applying it on the surface of the lesion, it has increased compliance to the treatment [34,35].
Severe life-threatening hemangiomas, corticoresistant ones or Kassabach Meritt syndrome sometimes need a more aggressive therapy, such as Vincristine [17,4,36]. This an antineoplastic agent with antiangiogenic actions, that leads to tumoral cell apoptosis [8,14]. It is administered orally, a dose a week of 0.5–2mg/m2 [8] for 15 weeks. Adverse reactions consist of peripheral neuropathy, mandibular pain, anemia, leucopenia or constipation [4] and an inadequate secretion of ADH [22].
Other therapeutic options for small, superficial and uncomplicated hemangiomas are Imiquimod [37], an immune mediator or laser-therapy of different types (e.g. laser-argon, Nd-YAG laser, CO2 laser, fractionate photothermolisis or dye-pulsed laser [14]. Both types can present with disfiguring side effects, such as disfiguring scars, or ulceration [37,38]. Laser therapy can also be used for residual hemangiomas with fibro-fatty tissue remnants [38].
Surgery is indicated in disfiguring hemangiomas or multiple-therapy resistant ones [17]. Hemangiomas localized periocularly can cause serious damage to vision, disorders like amblyopia, caused by deprivation or astigmatism [20]. If surgery is not indicated early, these disorders become permanent [20]. The most important advantage is that it leads to nearly the complete resolution of the hemangioma, but entails risks of bleeding [14].
Radiotherapy and embolization are used in hepatic hemangiomas [17,4].
Each type of therapy has its indications, contraindications, side effects and risks; therefore, the treatment of hemangiomas remains a challenge. Because the exact mechanisms of action of several therapies remain unknown, the subject is of great interest for researchers. Therefore a high number of studies are performed and more are need to be conducted in order to achieve target-therapies.
References:
- 1.Ma X, Zhao T, Xiao Y, Yu J, Chen H, Huang Y, et al. Preliminary experience on treatment of infantile hemangioma with low-dose propranolol in China. Eur J Pediatr. 2013;172(5):653–659. doi: 10.1007/s00431-012-1928-9. [DOI] [PubMed] [Google Scholar]
- 2.Melo JN, Rotter A, Rivitti-Machado MC, Oliveira ZN. Propranolol for treatment of infantile hemangiomas. An Bras Dermatol. 2013;88(6 Suppl 1):220–223. doi: 10.1590/abd1806-4841.20131699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weston WL, Lane AT, Morelli JG. Lesiones vasculares. In: Weston WL, Lane AT, Morelli JG, editors. Dermatologia pediatrica. 4ed. Spain: Elsevier; 2008. pp. 237–255. [Google Scholar]
- 4.Lucky AW. Lesiones cutaneas benignas transitorias en el recien nacido. In: Eichenfield LF, Frieden IJ, Esterly NB, editors. Dermatologia neonatal. 2ed. Spain: Elsevier; 2009. pp. 85–97. [Google Scholar]
- 5.Drolet BA, Swanson EA, Frieden IJ, Hemangioma Investigator Group Infantile hemangiomas: an emerging health issue linked to an increased rate of low birth weight infants. J Pediatr. 2008;153(5):712–715. 715.e1. doi: 10.1016/j.jpeds.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 6.Chen XD, Ma G, Chen H, Ye XX, Jin YB, Lin XX. Maternal and perinatal risk factors for infantile hemangioma: a case-control study. Pediatr Dermatol. 2013;30(4):457–461. doi: 10.1111/pde.12042. [DOI] [PubMed] [Google Scholar]
- 7.Couto RA, Hassanein AH, Maclellan RA, Greene AK. Infantile hemangioma in four siblings. Pediatr Dermatol. 2013;30(3):e14–15. doi: 10.1111/j.1525-1470.2012.01779.x. [DOI] [PubMed] [Google Scholar]
- 8.Leaute-Labreze C, Sans-Martin V. [Infantile hemangioma] Presse Med. 2010;39(4):499–510. doi: 10.1016/j.lpm.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 9.Casanova D, Norat F, Bardot J, Magalon G. [Cutaneous hemangioma: clinical aspects] Ann Chir Plast Esthet. 2006;51(4–5):287–292. doi: 10.1016/j.anplas.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Przewratil P, Sitkiewicz A, Andrzejewska E. Local serum levels of vascular endothelial growth factor in infantile hemangioma: intriguing mechanism of endothelial growth. Cytokine. 2010;49(2):141–147. doi: 10.1016/j.cyto.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Przewratil P, Sitkiewicz A, Wyka K, Andrzejewska E. Serum levels of vascular endothelial growth factor and basic fibroblastic growth factor in children with hemangiomas and vascular malformations--preliminary report. Pediatr Dermatol. 2009;26(4):399–404. doi: 10.1111/j.1525-1470.2009.00910.x. [DOI] [PubMed] [Google Scholar]
- 12.Lynch M, Lenane P, O’Donnell BF. Propranolol for the treatment of infantile haemangiomas: our experience with 44 patients. Clin Exp Dermatol. 2014;39(2):142–145. doi: 10.1111/ced.12210. [DOI] [PubMed] [Google Scholar]
- 13.Chen XD, Ma G, Huang JL, Chen H, Jin YB, Ye XX, et al. Serum-level changes of vascular endothelial growth factor in children with infantile hemangioma after oral propranolol therapy. Pediatr Dermatol. 2013;30(5):549–553. doi: 10.1111/pde.12192. [DOI] [PubMed] [Google Scholar]
- 14.Callahan AB, Yoon MK. Infantile hemangiomas: A review. Saudi J Ophthalmol. 2012;26(3):283–91. doi: 10.1016/j.sjopt.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun ZY, Yi CG, Zhao H, Yin GQ, Gao M, Liu YB, et al. Infantile hemangioma is originated from placental trophoblast, fact or fiction? Med Hypotheses. 2008;71(3):444–448. doi: 10.1016/j.mehy.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Zou HX, Jia J, Zhang WF, Sun ZJ, Zhao YF. Propranolol inhibits endothelial progenitor cell homing: a possible treatment mechanism of infantile hemangioma. Cardiovasc Pathol. 2013;22(3):203–210. doi: 10.1016/j.carpath.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Champion RH, Burtoon JL, Burns DA, Breathnach SM. Rook’s Textbook of Dermatology. 6th ed. Oxford Blackwell Science; 1998. [Google Scholar]
- 18.Talaat AA, Elbasiouny MS, Elgendy DS, Elwakil TF. Propranolol treatment of infantile hemangioma: clinical and radiologic evaluations. J Pediatr Surg. 2012;47(4):707–714. doi: 10.1016/j.jpedsurg.2011.10.058. [DOI] [PubMed] [Google Scholar]
- 19.Truong MT, Chang KW, Berk DR, Heerema-McKenney A, Bruckner AL. Propranolol for the treatment of a life-threatening subglottic and mediastinal infantile hemangioma. J Pediatr. 2010;156(2):335–338. doi: 10.1016/j.jpeds.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Mawn LA. Infantile hemangioma: treatment with surgery or steroids. Am Orthopt J. 2013;63:6–13. doi: 10.3368/aoj.63.1.6. [DOI] [PubMed] [Google Scholar]
- 21.Dompmartin A, Boon LM, Labbe D. [Infantile hemangiomas: differential diagnosis and associated anomalies] Ann Chir Plast Esthet. 2006;51(4–5):300–309. doi: 10.1016/j.anplas.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 22.Hasan M, Rahman M, Hoque S, Zahid Hossain AK, Khondker L. Propranolol for hemangiomas. Pediatr Surg Int. 2013;29(3):257–262. doi: 10.1007/s00383-012-3220-5. [DOI] [PubMed] [Google Scholar]
- 23.Lee KC, Bercovitch L. Update on infantile hemangiomas. Semin Perinatol. 2013;37(1):49–58. doi: 10.1053/j.semperi.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Haider KM, Neely DE, Plager DA. Hemangiomas treated with propranolol: do the rewards outweigh the risks? Am Orthopt J. 2013;63:2–5. doi: 10.3368/aoj.63.1.2. [DOI] [PubMed] [Google Scholar]
- 25.Nieuwenhuis K, de Laat PC, Janmohamed SR, Madern GC, Oranje AP. Infantile hemangioma: treatment with short course systemic corticosteroid therapy as an alternative for propranolol. Pediatr Dermatol. 2013;30(1):64–70. doi: 10.1111/j.1525-1470.2012.01846.x. [DOI] [PubMed] [Google Scholar]
- 26.Hermans DJ, van Beynum IM, Schultze Kool LJ, van de Kerkhof PC, Wijnen MH, van der Vleuten CJ. Propranolol, a very promising treatment for ulceration in infantile hemangiomas: a study of 20 cases with matched historical controls. J Am Acad Dermatol. 2011;64(5):833–838. doi: 10.1016/j.jaad.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 27.Kim LH, Hogeling M, Wargon O, Jiwane A, Adams S. Propranolol: useful therapeutic agent for the treatment of ulcerated infantile hemangiomas. J Pediatr Surg. 2011;46(4):759–763. doi: 10.1016/j.jpedsurg.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Saint-Jean M, Leaute-Labreze C, Mazereeuw-Hautier J, Bodak N, Hamel-Teillac D, Kupfer-Bessaguet I, et al. Propranolol for treatment of ulcerated infantile hemangiomas. J Am Acad Dermatol. 2011;64(5):827–832. doi: 10.1016/j.jaad.2010.12.040. [DOI] [PubMed] [Google Scholar]
- 29.Marqueling AL, Oza V, Frieden IJ, Puttgen KB. Propranolol and infantile hemangiomas four years later: a systematic review. Pediatr Dermatol. 2013;30(2):182–191. doi: 10.1111/pde.12089. [DOI] [PubMed] [Google Scholar]
- 30.Causse S, Aubert H, Saint-Jean M, Puzenat E, Bursztejn AC, Eschard C, et al. Propranolol-resistant infantile haemangiomas. Br J Dermatol. 2013;169(1):125–129. doi: 10.1111/bjd.12417. [DOI] [PubMed] [Google Scholar]
- 31.Dalby TK, Lester-Smith D. Propranolol for the treatment of infantile haemangioma. J Paediatr Child Health. 2013;49(2):148–151. doi: 10.1111/jpc.12076. [DOI] [PubMed] [Google Scholar]
- 32.Martin K, Blei F, Chamlin SL, Chiu YE, Frieden IJ, Frommelt PC, et al. Propranolol treatment of infantile hemangiomas: anticipatory guidance for parents and caretakers. Pediatr Dermatol. 2013;30(1):155–9. doi: 10.1111/pde.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puttgen KB, Summerer B, Schneider J, Cohen BA, Boss EF, Bauman NM. Cardiovascular and blood glucose parameters in infants during propranolol initiation for treatment of symptomatic infantile hemangiomas. Ann Otol Rhinol Laryngol. 2013;122(9):550–4. doi: 10.1177/000348941312200903. [DOI] [PubMed] [Google Scholar]
- 34.Sorrell J, Chamlin SL. Topical timolol 0.5% gel-forming solution for small deep facial infantile hemangiomas. Pediatr Dermatol. 2013;30(5):592–594. doi: 10.1111/pde.12209. [DOI] [PubMed] [Google Scholar]
- 35.Moehrle M, Leaute-Labreze C, Schmidt V, Rocken M, Poets CF, Goelz R. Topical timolol for small hemangiomas of infancy. Pediatr Dermatol. 2013;30(2):245–249. doi: 10.1111/j.1525-1470.2012.01723.x. [DOI] [PubMed] [Google Scholar]
- 36.Leaute-Labreze C. [Infantile hemangioma: update and treatment] Arch Pediatr. 2013;20(5):517–522. doi: 10.1016/j.arcped.2013.01.052. [DOI] [PubMed] [Google Scholar]
- 37.Qiu Y, Ma G, Lin X, Jin Y, Chen H, Hu X. Treating protruding infantile hemangiomas with topical imiquimod 5% cream caused severe local reactions and disfiguring scars. Pediatr Dermatol. 2013;30(3):342–347. doi: 10.1111/pde.12002. [DOI] [PubMed] [Google Scholar]
- 38.Alcantara-Gonzalez J, Boixeda P, Truchuelo-Diez MT, Perez-Garcia B, Alonso-Castro L, Jaen Olasolo P. Infantile hemangiomas treated by sequential application of pulsed dye laser and Nd:YAG laser radiation: a retrospective study. Actas Dermosifiliogr. 2013;104(6):504–511. doi: 10.1016/j.ad.2012.12.010. [DOI] [PubMed] [Google Scholar]