Abstract
Medullary thyroid carcinoma (MTC) is a rare malignancy that may metastasize to liver, lungs and bones. Breast is an unusual metastatic site for MTC and only 20 female cases have been reported in the literature. We present a male patient in whom histological examination and immunohistochemistry of a breast mass were indicative of breast metastasis from MTC. A 67-year-old man with recent diagnosis of MTC and metastases to cervical and upper mediastinum lymph nodes was referred to our department for further treatment. At first evaluation, diagnostic imaging techniques showed lung and bone metastases and three months later the presence of liver metastases. Due to the extension of the disease, treatment with vandetanib was decided, but serious adverse events led to its interruption after two weeks. During follow-up, patient developed a painful swelling in the right breast. Ultrasound and mammography showed the presence of multiple masses to the right breast suspicious for malignancy. Core needle biopsy and histological examination of the specimen confirmed the presence of metastatic MTC. Palliative external beam irradiation was used to relieve local pain and, after one month, the patient died. Consequently, breast masses should be cautiously evaluated, mainly in the presence of a known primary malignancy. Histological and/or cytopathological examination are requisite diagnostic tools, while external beam irradiation and tyrosine kinase inhibitors may be used as palliative therapies in the concurrent presence of breast metastases from MTC.
Key words: Medullary thyroid cancer, breast metastasis, tyrosine kinase inhibitor
Introduction
Medullary thyroid carcinoma (MTC) is a rare malignancy which originates from parafollicular C cells of the thyroid gland. Survival rates vary according to the extent of disease at diagnosis with a 10-year disease-specific survival about 75%.1 Liver, lungs and bones represent the most common metastatic sites of the disease.
Breast metastases are a relatively rare condition in both genders and account for about 0.5-2% of all breast tumors. Most frequently, these metastases are observed in lymphoma and malignant melanoma, while metastases from lung cancer, ovarian carcinoma and gastrointestinal tumors are seldom described. Among men, prostate cancer is the most prevalent primary tumor which metastasizes to the breast.2 Regarding breast metastases from MTC, only few female cases are reported in the literature.
Herein we i) present a patient with MTC who developed breast metastasis seven months after the initial diagnosis of the disease, ii) discuss possible pathogenetic mechanisms of this rare metastatic site and iii) present the results of an extensive review of the literature regarding breast metastases from MTC. To our knowledge, this is the first reported male case with breast metastasis from MTC.
Case Report
A 67-year-old man was referred to our department with a recent histological diagnosis of MTC without any family history of MTC or multiple endocrine neoplasia (MEN). Fractionated metanephrines measured preoperatively were found within the normal limits. Two months prior the patient underwent total thyroidectomy with central compartment and bilateral cervical lymph node dissection, followed by lymph node dissection of the superior upper mediastinum under thoracotomy. Primary tumor was multifocal and bilateral. The major lesion was measured 8.5 cm in its maximum diameter, invaded small intrathyroid vessels and presented extrathyroidal extension to the perithyroidal soft tissue. The majority of the dissected lymph nodes contained metastasis. Invasion of the lymph node capsule as well extension of the metastatic tissue to the adjacent adipose tissue was observed, too. At this point the patient was referred to our department for further evaluation and treatment.
At first evaluation, hoarseness due to post-surgical right vocal-fold paresis, diarrhea and fatigue were the most prominent symptoms, aggravating his quality of life. Biochemical tests revealed postoperative hypoparathyroidism, other serum electrolytes were normal and electrocardiogram showed the presence of chronic atrial fibrillation. Both MTC serum tumor markers, calcitonin and carcinoembryonic antigen (CEA), were measured.1 Calcitonin levels were elevated to 613.6 pg/mL (normal range <10 pg/mL), compatible with the presence of local and/or distant metastases. CEA was 17.88 ng/mL (normal range <5.1 ng/mL). Chest and upper abdomen computed tomography (CT) showed the presence of lung metastases and bone scintigraphy was indicative of lesions in lumbar spine, ilium and left hip. No liver metastases were noted at that time. All the known mutations in exons 8, 10, 11, 13, 14, 15, 16 of rearranged during transfection protooncogene were tested and no mutation was confirmed. The absence of any mutation in accordance with the negative family history is highly indicative that the patient did not belong to MEN 2 syndrome or familial MTC.
Three months later a new spiral CT of the liver was done. The presence of four metastatic lesions measuring 10 to 27 mm was confirmed for first time. Moreover, increase in the size of lung metastases was observed as well as pressure of the spinal cord at level of 8th vertebra. Despite the metastatic disease, no clinical paraneoplastic syndrome was identified. Due to the progression and the extension of the disease, administration of vandetanib, a tyrosine kinase inhibitor (TKI), was decided in the dose of 300 mg daily. Unfortunately, two weeks later, the drug was discontinued as serious adverse events appeared (decrease of creatinine clearance, thrombocytopenia, severe nasal bleeding). Nevertheless, the combination of antimotility agents (loperamide) with somatostatin analogues (octreotide LAR 20 mg) reduced the amount and frequency of diarrhea.
Breast metastasis
During follow-up, the patient presented a painful swelling in the right breast. He had a diagnostic mammography. Both craniocaudal and mediolateraloblique views showed bilateral breast enlargement and the presence of well circumscribed lesions mainly in the right breast (Figure 1). Ultrasound examination of the breast revealed a hypoechoic, almost homogeneous mass, with lobular appearance and well defined borders. The mass had hyperechoic diaphragms and occupied most of the right breast. No calcifications or acoustic shadowing were found (Figure 2).
Figure 1.
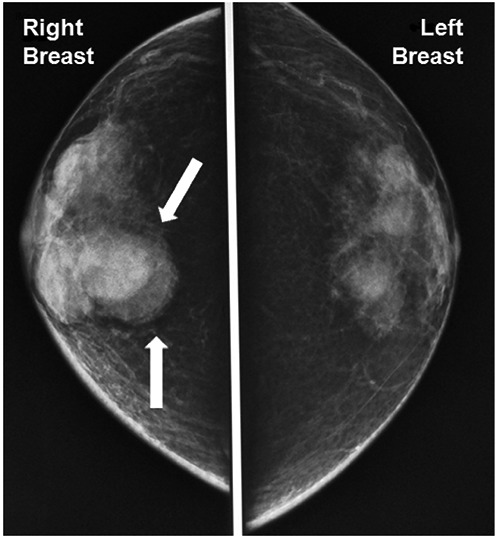
Craniocaudal mammographic view shows well circumscribed lesions mainly in the right breast.
Figure 2.
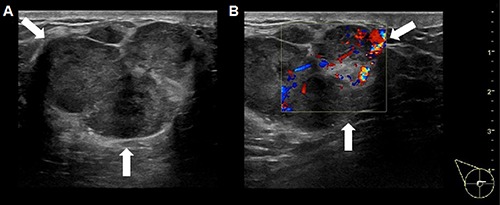
A hypoechoic mass with lobular appearance and hyperechoic diaphragms on ultrasound examination (A). Doppler examination reveals internal vascularity of the mass (B).
Core needle biopsy of the mass revealed metastatic disease from the known MTC. The neoplasm was characterized by sheets and nests of round or slightly spindle cells in a fibrous tissue. Amyloid deposits have been identified with the Congo red histochemical stain. Tumor cells contained round to oval, regular hyperchromatic nuclei with occasional nucleoli. Mitosis was scant (Figure 3). Immunohistochemistry showed that the neoplastic cells were positive for calcitonin, chromogranin, synaptophysin, thyroid transcription factor-1 (TTF-1), low molecular weight keratins and negative for thyroglobulin (Figure 4).
Figure 3.
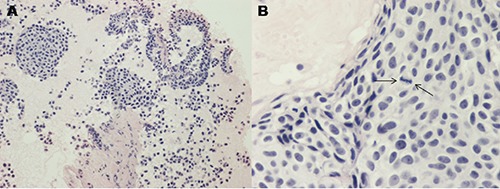
Nests of uniform round to slightly spindle cells (100×) in a fibrous tissue (A). Tumor cells (600×) contain round to oval hyperchromatic nuclei with occasional nucleoli. A mitosis is evident (B).
Figure 4.
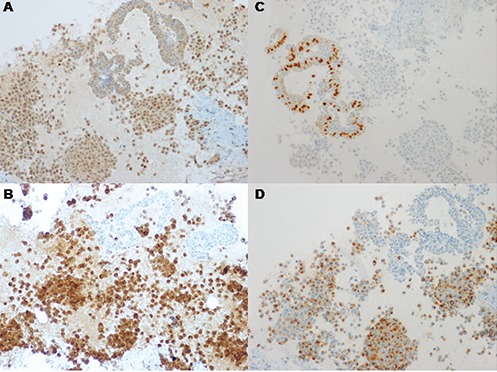
Neoplastic cells (100×) stain positively for thyroid transcription factor-1 (TTF-1) (A). Neoplastic cells (200×) show strong reactivity for calcitonin (B). Neoplastic cells (100×) are negatively stained for estrogen receptor. The adjacent epithelial cells of a mammary duct show estrogen receptor reactivity and is considered as an internal positive control (C). Neoplastic cells (100×) are positively stained for chromogranin (D).
Palliative external beam irradiation was decided resulting in mild relief of pain. Unfortunately, during the following month, the patient’s health deteriorated due to a right ulnar fracture and septic fever and, few days later, he died.
Literature search method
Two reviewers (SM and EM) performed computerized literature search in the PubMed electronic database, Wiley Online Library and the Cochrane Library. The initial search included the query: medullary thyroid carcinoma and breast metastasis, metastatic medullary thyroid carcinoma and breast, medullary thyroid cancer and breast metastasis» and «metastatic medullary thyroid cancer and breast last updated on June 2014. The selection of the articles was based subsequently on the title, abstract or full-text basis. Literature search was extended to the Related Articles link next to each selected. The selection criterion was the presence of MTC with breast metastasis confirmed by cytological staining or histopathological examination. The publication time was not an exclusion criterion. Patients with unknown or other variants of thyroid cancer were excluded.
Literature search results
In summary, 20 cases of MTC metastatic to the breast have been documented. All patients were female and the mean age at diagnosis of breast metastasis was 42.5 years. The interval between thyroidectomy and the detection of breast metastasis varied significantly (mean time 6 years, range 0-28 years). In two patients breast was the first site of metastasis, while the concurrent presence of other distant metastases was detected in the majority of them. MEN 2 syndrome was identified in five cases. Seven patients succumbed to their disease.
Breast metastases were presented as a solitary (eight cases) or multiple nodules (eleven cases). The diagnosis relied on fine needle aspiration cytology (FNAC) (eight patients), core biopsy (five) and tumor excision (four).
Therapeutically, the excision of metastasis was performed in seven patients, mastectomy in three, chemotherapy and administration of tyrosine kinase inhibitor (sorafenib) in one patient. In contrary, three patients did not receive any further therapy. Results are summarized in Table 1.2-19
Table 1.
Demographic and radiology characteristics, presence of metastases and alive status of patients with metastatic medullary thyroid carcinoma to the breast (20 cases)
| First author, year | Age | MEN 2 | Breast affected and number of metastatic nodules | Mammography-U/S | Metastases | Deceased/alive |
|---|---|---|---|---|---|---|
| Martinez-Rodriguez, 20136 | 51 | No | R-1 | No-No | Liver, bones, thoracic wall | A |
| Rodriguez-Gil, 20125 | 43 | No | Bilateral-3 | Yes-No | Bone | D |
| Basu, 20107 | 32 | NR | L-1 | NR-NR | NR | NR |
| Ricciato, 20103 | 54 | No | L-1 | Yes-Yes | Cervical lymph nodes, liver, lungs, rib | A |
| Andreiuolo, 20098 | 57 | No | Bilateral-2 | Yes-Yes | NR | NR |
| Marcy, 20094 | 43 | No | Bilateral-M | No-Yes | Cervical lymph nodes, tracheal wall | D |
| Nofech-Mozes, 20082 | 50 | No | L-1 | Yes-Yes | Cervical lymph nodes, liver | A |
| Kim, 20089 | 39 | No | R-2 | No-No | Cervical lymph nodes, liver | A |
| Kang, 200810 | 38 | No | Bilateral-2 | Yes-Yes | Cervical lymph nodes | A |
| Vaughan, 200711 | 35 | Yes | L-1 | Yes-Yes | Unknown distant metastases | D |
| Vaughan, 200711 | 29 | Yes | L-1 | Yes-No | Unknown distant metastases | D |
| Vaughan, 200711 | 30 | Yes | Bilateral-2 | Yes-Yes | Unknown distant metastases | A |
| Lee, 200712 | 48 | NR | NR-M | NR-NR | Cervical lymph nodes | NR |
| Ishitobi, 200413 | 54 | No | Bilateral-M | Yes-Yes | NR | NR |
| Pritchett, 199814 | 42 | No | R-1 | No-No | Cervical lymph nodes, lungs, brain | D |
| Kiely, 199515 | 64 | No | L-1 | Yes-Yes | Cervical lymph nodes | A |
| Soo, 199516 | 40 | Yes | L-2 | Yes-No | Cervical lymph nodes, liver | NR |
| Ali, 199417 | 28 | Yes | NR-NR | NR-NR | NR | NR |
| Ahuja, 199118 | 32 | NR | NR-M | NR-NR | Cervical lymph nodes, lungs, bones | D |
| Ordonez, 198819 | 72 | No | R-2 | No-No | Cervical lymph nodes, skin | D |
MEN, multiple endocrine neoplasia; NR, not reported; M, multiple; A, alive; D, deceased.
Discussion
In the present work we refer to a male patient with MTC who developed breast metastases. Moreover, the patient had metastases to lung, liver and bone and he died ten months after the diagnosis of MTC. To our knowledge this is the first male case reported in the literature. Considering the present case, the arising question is if breast metastasis is really too rare in men or underestimated. Unfortunately, the answer is not easy as information about metastatic MTC to the breast comes exclusively from some case reports which till now refer only to women. The possibility of an underestimated condition is low, as breast masses in males are more easily recognized due to the small size of the gland and the pain that usually accompanies their development. Therefore, it seems that the breast metastatic disease is extremely rare, in accordance with the scarcity of primary breast cancer in men.
Based on the present literature review, we could conclude that the majority of female patients had already distant metastases in other sites at the time of diagnosis of breast involvement. This fact enhances the hypothesis that breast metastases may be a late manifestation of widely MTC metastatic disease caused by hematogenous dissemination of cancer cells.3 On the other hand, there were two female cases in which the presence of breast malignant nodules was the first site of distant metastasis. This could be the result of a lymphatic retrograde dissemination from supraclavicular to subclavicular axillary lymph nodes and then to the breast, secondary to postoperative radiotherapy blockage of lymphatic pathways as reported elsewhere.4 The fact that, almost all patients had been submitted to neck dissection, six women had previously received neck irradiation therapy and, in two women, breast involvement was the first metastatic manifestation, favors the second causative factor. For that reason, neither hematogenous diffusion nor lymphatic retrograde dissemination could be completely ignored.
Breast ultrasonography and mammography are useful diagnostic tools albeit the absence of pathognomonic criteria to establish the diagnosis of breast metastasis.2 Metastatic nodule is mostly superficial, solitary, firm and adherent to skin.5 Other ultrasound characteristics are the rapid growth and the lack of tumor-associated acoustic shadowing. Mammographically, the mass is well-defined and usually multiple with other deep nodules or axillary involvement.2 In any case, FNAC or/and core biopsy should be advocated. The two methods had been used in any patient from the review apart from 4 patients in whom excision of tumor or modified radical mastectomy were firstly selected. Differential diagnosis of breast metastasis from primary breast tumor is very crucial as it may alter the therapy and prevent unnecessary surgery.20
Therapeutically metastasectomy could be indicated in the absence of any other metastatic lesion.11 This option was not chosen in the present case as the patient presented extensive metastatic disease. Instead, external beam irradiation therapy as a palliative therapy was offered.1 In few cases, chemotherapy or targeted therapy (TKIS) was applied. Despite their side effects, TKIs were proved to be a promising therapeutic tool with efficacy in a phase III trial of patients with advanced MTC.21 Based on the recent approval of vandetanib for the treatment of progressive metastatic MTC, we decided to prescribe it. Unfortunately, its use was interrupted as grade IV adverse events soon appeared.
Conclusions
In summary, we present a male with breast metastasis from MTC and we reviewed the literature for similar cases. FNAC and core biopsy are requisite diagnostic tools due to the scarcity of these metastases and the ambiguous diagnostic criteria using ultrasound and mammography. When a breast mass is present in patients with MTC, the possibility of metastasis may be considered.
References
- 1.Kloos RT, Eng C, Evans DB, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. The American Thyroid Association Guidelines Task Force. Thyroid 2009;19:565-612. [DOI] [PubMed] [Google Scholar]
- 2.Nofech-Mozes S, Mackenzie R, Kahn HJ, et al. Breast metastasis by medullary thyroid carcinoma detected by FDG positron emission tomography. Ann Diagn Pathol 2008;12:67-71. [DOI] [PubMed] [Google Scholar]
- 3.Ricciato MP, Lombardi CP, Raffaelli M, et al. Metastatic breast involvement from medullary thyroid carcinoma: a clue to consider the need of early diagnosis and adequate surgical strategy. Thyroid 2010;20:831-2. [DOI] [PubMed] [Google Scholar]
- 4.Marcy PY, Thariat J, Peyrottes I, Dassonville O. Bilateral breast involvement in medullary thyroid carcinoma. Thyroid 2009;19:197-9. [DOI] [PubMed] [Google Scholar]
- 5.Rodríguez-Gil Y, Pérez-Barrios A, Alberti-Masgrau N, et al. Fine-needle aspiration cytology diagnosis of metastatic non-haematological neoplasms of the breast: a series of seven cases. Diagn Cytopathol 2012;40:297-304. [DOI] [PubMed] [Google Scholar]
- 6.Martínez-Rodríguez I, Banzo I, Carril JM. Metabolic response demonstrated by 18F-FDG-PET/CT in metastatic medullary thyroid carcinoma under sorafenib therapy. Endocrine 2012;44:264-5. [DOI] [PubMed] [Google Scholar]
- 7.Basu S, Shet T. Unilateral solitary breast metastasis from medullary carcinoma of thyroid detected by FDG-PET. Clin Nucl Med 2010;35:512-3. [DOI] [PubMed] [Google Scholar]
- 8.Andreiuolo F, Suciu V, Bayou EH, et al. Bilateral breast lesions in a patient with medullary thyroid carcinoma. Cytopathology 2009;20:403-5. [DOI] [PubMed] [Google Scholar]
- 9.Kim JH, Lee SW, Kim WS, et al. Metastatic medullary thyroid carcinoma to the breast. Basic Appl Pathol 2008;1:149-51. [Google Scholar]
- 10.Kang M, Hazarika D, Ghosal S, et al. Metastatic medullary thyroid carcinoma to the breast: Radiological features. Eur J Radiol Extra 2008;65:47-9. [Google Scholar]
- 11.Vaughan A, Dietz JR, Moley JF, et al. Metastatic disease to the breast: the Washington University experience. World J Surg Oncol 2007;5:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee Y, An J, Kim CH, et al. Metastatic medullary carcinoma of thyroid to breast; a case initially diagnosed as primary invasive lobular carcinoma – a case report. Korean J Pathol 2007;41:412-5. [Google Scholar]
- 13.Ishitobi M, Tamaki Y, Yamamura J, et al. Bilateral breast metastases of medullary thyroid cancer. Breast J 2004;10:162. [DOI] [PubMed] [Google Scholar]
- 14.Pritchett DD, Ali SZ. Metastatic medullary thyroid carcinoma in a breast fine needle aspirate: cytopathologic findings. Acta Cytol 1998;42:446-8. [PubMed] [Google Scholar]
- 15.Kiely N, Williams N, Wilson G, Williams RJ. Medullary carcinoma of the thyroid metastatic to breast. Postgrad Med J 1995;71:744-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soo MS, Williford ME, Elenberger CD. Medullary thyroid carcinoma metastatic to the breast: mammographic appearance. AJR Am J Roentgenol 1995;165:65-6. [DOI] [PubMed] [Google Scholar]
- 17.Ali SZ, Teichberg S, Attie JN, Susin M. Medullary thyroid carcinoma metastatic to breast masquerading as infiltrating lobular carcinoma. Ann Clin Lab Sci 1994;24:441-7. [PubMed] [Google Scholar]
- 18.Ahuja S, Ernst H. Dormant metastases in medullary thyroid carcinoma. A case report. Exp Clin Endocrinol 1991;98:37-41. [DOI] [PubMed] [Google Scholar]
- 19.Ordóñez NG, Katz RL, Luna MA, Samaan NA. Medullary thyroid carcinoma metastatic to breast diagnosed by fine-needle aspiration biopsy. Diagn Cytopathol 1988;4:254-7. [DOI] [PubMed] [Google Scholar]
- 20.Yeh CN, Lin CH, Chen MF. Clinical and ultrasonographic characteristics of breast metastases from extramammary malignancies. Am Surg 2004;70:287-90. [PubMed] [Google Scholar]
- 21.Wells SA, Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol 2012;30:134-41. [DOI] [PMC free article] [PubMed] [Google Scholar]


