Abstract
Granular cell tumors are rare soft tissue neoplasms, among which only 2% are malignant, arising from nervous tissue. Here we present a case of a large esophageal granular cell tumor with benign histopathological features which metastasized to the liver, but showing on positron emission tomography-computerized tomography standardized uptake value suggestive of a benign lesion.
Key words: Granular cell tumor, esophagus, malignant
Introduction
Granular cell tumor (GCT) is a rare, mostly benign, soft tissue neoplasm, arising from nervous tissue. It can occurs anywhere in the body but, most commonly in the skin, tongue, subcutaneous tissue and skeletal muscle.1 About 5-11% of these tumors are found in the gastrointestinal (GI) tract and 1/3 of these are seen in the esophagus.2 From the time the first GCT was described in the esophagus in 1931,3 till date, approximately 350 cases have been reported.4 Out of these, 20% were in the middle of esophagus.5 Malignant lesions are rare, about 1-2%.6 Our knowledge of these rare tumors and the present treatment recommendations are based on individual case reports or small series studies because of the rarity of these tumors. Here we are presenting a case of large esophageal GCT with metastatic liver lesions.
Case Report
Mrs. B.N., a 60-year-old lady, presented to our outpatient department with a history of progressive dysphagia of 1 year duration, cough and hoarseness of voice for 3 months. She was evaluated at our center and was found to have a large mediastinal mass compressing on the esophagus and underwent an endoscopic examination and biopsy which was reported as doubtful of malignant pathology. No intraluminal mass or ulceration of mucosa was found on upper gastrointestinal endoscopy (UGIE). Contrast enhanced computerized tomography (CECT) chest and abdomen done, showed a large well defined intramural enhancing mass lesion arising from the right posterolateral wall of the esophagus measuring approximately 9.1×4.8×4.8 cm with areas of necrosis within, involving the middle third of esophagus (T3-T7) with complete luminal compromise (Figure 1). Enlarged subcentimetric lymph nodes were seen in the celiac axis and bilateral axillary regions. Multiple centrilobular pulmonary nodules and ground glass opacities in bilateral lung fields and a hypodense lesion in segment VII of liver were visualized. In view of the inconclusive histopathology a repeat biopsy was done, the histopathological examination of which revealed, fragments of hyperplastic stratified squamous epithelium along with a tumor composed of sheets of polygonal cells with abundant granular eosinophilic cytoplasm. The nuclei were round to irregular with non-descript chromatin and inconspicuous nucleoli. No mitosis could be identified. On immunohistochemistry (IHC), the tumor showed a low Ki67 proliferative index. S-100, CD 68 and Desmin were positive while myf-4 was negative. The histopathological features supported a diagnosis of benign granular cell tumor. In view of the indeterminate lung nodules and a solitary lesion on segment Vll of right lobe of liver, a positron emission tomography-computerized tomography (PET-CT) scan was performed. It showed the esophageal mass to be metabolically active with 18-fluoro deoxy glucose (FDG) uptake suggestive of a benign tumor and the liver lesions to be non FDG avid. Ultrasound guided fine needle aspiration cytology (FNAC) of the liver lesion was performed which revealed metastatic granular cell tumor.
Figure 1.
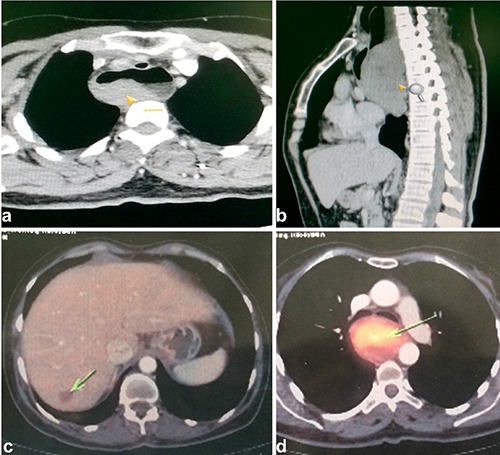
a,b) Contrast enhanced computed tomography (CT) chest images showing the intramural mass (arrow) in the right posterolateral wall of esophagus in axial and sagittal sections respectively. c) Positron emission CT (PET CT) showing non 18-fluoro deoxy glucose avid lesion (arrow) in segment Vll of liver. d) PET CT showing the FDG avid esophageal mass (arrow) of standardized uptake value 2.
Patient did not pursue treatment at our center and opted for alternative medicine elsewhere.
Discussion
Granular cell tumors are also referred to as Arbikossoff tumors, after Arbikossoff first described these tumors in the tongue in 1926 and called them myoblastomas.7 Now, it is known that they arise from Schwann cells. These are uncommon in the GI tract, where 8% of these tumors are found. The esophagus is the commonest site in the GI tract with most of these developing in the distal esophagus.8 Overall, 1% of all reported cases of GCT were in the esophagus.9 Tumors of 2 cm or less are usually asymptomatic and are found incidentally during UGI endoscopy or imaging studies.10 Tumors more than 2 cm in size are usually symptomatic, the commonest symptom being dysphagia. Less commonly patients present with gastro esophageal reflux disease, dyspepsia, chest pain, cough, nausea, and hoarseness.1 Our patient presented with dysphagia and respiratory symptoms secondary to airway obstruction owing to extrinsic compression by the large tumor measuring 9.1×4.8×4.8 cm. Multifocal tumors have also been reported in literature.11 On endoscopy, they typically show yellowish smooth surface with an underlying mass. Sometimes the surface may appear white or red. This tumor does not ulcerate the mucosa. In case of superficial lesions endoscopic biopsy can be done.1 Our patient had a reddish mucosal surface with a mass arising from the posterolateral wall causing luminal narrowing with almost complete obstruction of the lumen. Endoscopic ultrasound (EUS) is very useful in the diagnosis and assessment of size, location and the layers infiltrated by these tumors. On EUS these tumors appear as hypoechoic, homogenous, and smooth-edged lesions located commonly in mucosa or submucosa.1 In a series of 15 patients with 21 mucosal lesions with a pathological diagnosis of esophageal granular cell tumor, Palazzo et al., reported endosonographic features of: i) tumor size of less than 2 cm in 95% of cases; ii) hypoechoic solid pattern in 100% of cases, and iii) tumor arising in the inner layers (second echo-poor layer) in 95%. They concluded that: when a granular cell tumor of the esophagus is suspected, EUS can show the inner layer location of the tumor and thus contribute to planning the endoscopic resection or follow up. When the tumor also invades the outer layers, EUS can contribute to planning the surgical resection.12
Though endosonography can suggest a GCT, there are other differential diagnosis like leiomyoma from which we cannot differentiate by imaging. Histopathology with immunohistochemistry studies is the diagnostic procedure for the tumors. On gross examination, these are solid, firm, and non-enveloped tumors with a yellow or yellowish cross section usually located in the mucosa or submucosa. Characteristic microscopic picture is that of sheets or nests of round or polygonal large cells with abundant eosinophilic granular cytoplasm and small, round, central uniform nuclei (Figure 2).13 Histological criteria for diagnosing a malignant GCT as proposed by Fanburg-Smith et al. are: i) necrosis, ii) spindling, iii) vesicular nuclei with large nucleoli, iv) high nuclear-to-cytoplasmic ratio, v) increased mitotic activity (more than 2 mitoses per 10 high-power fields at 200× magnification), vi) pleomorphism. Those tumors which meet atleast 3 of these criteria are classified as malignant. Those that meet one or two are atypical. If there is only focal pleomorphism and none of the other criteria are satisfied, then they are classified as benign.14 So our patient fits into the criteria of a benign tumor, immunohistologically supported by a low Ki67 proliferative index. On PET-CT scan the FDG uptake of the esophageal tumor was suggestive of a benign pathology with a maximum standardized uptake value (SUV) of 2.21 and the liver lesion was non FDG avid. Hoess et al. have reported on the PET evaluation of breast GCT and according to them, in a population of 51 patients at their centre, a threshold SUV of 2.5 was able to best differentiate benign from malignant lesions.15 But there is not sufficient data on PET evaluation of esophageal GCT.
Figure 2.
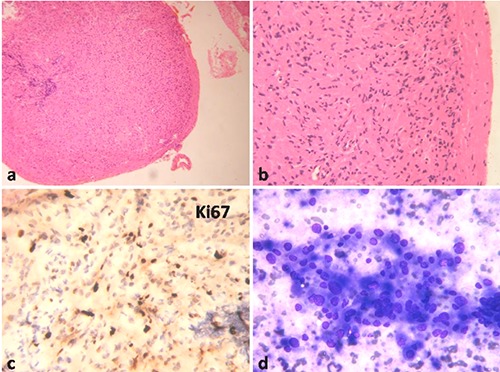
a) Esophageal tumor nodule at low magnification, Hematoxylin & Eosin (H&E, 100×). b) High magnification showing tumor composed of sheets of polygonal cells with eosinophilic cytoplasm, H&E 400×. c) Low Ki67 proliferative fraction, DAB chromogen 400×. d) Liver aspirate showing loose clusters of polygonal cells with variation in nuclear size and abundant cytoplasm, MGG 400×.
Conclusions
In this case report, our patient presented with a granular cell tumor of mid esophagus, which appeared benign on histology and PET imaging; however, it showed metastatic deposit in the liver which to our knowledge has not been reported before. Malignant GCT are rare and constitute only 2% of these tumors. Differentiating a benign from a malignant GCT is a challenge, even with the existing histopathological, immunohistochemical and clinical criteria for differentiation. Moreover, most of the clinical data we have on GCT are based on individual case reports or small series studies. Information on the role of PET-CT in esophageal GCT is unfortunately lacking.
References
- 1.Chen WS, Zheng XL, Jin L, et al. Novel diagnosis and treatment of esophageal granular cell tumor: report of 14 cases and review of the literature. Ann Thorac Surg 2014;97:296-302. [DOI] [PubMed] [Google Scholar]
- 2.Johnston MJ, Helwig EB. Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Dig Dis Sci 1981;26:807-16. [DOI] [PubMed] [Google Scholar]
- 3.Abrikossoff AI. Further studies on myoblasts fibroids. Virchows Arch Pathol Anat 1931;280:723-40. [Google Scholar]
- 4.Zhong N, Katzka DA, Smyrk TC, et al. Endoscopic diagnosis and resection of esophageal granular cell tumors. Dis Esophagus 2011;24:538-43. [DOI] [PubMed] [Google Scholar]
- 5.De Rezende L, Lucendo AJ, Alvarez-Arguelles H. Granular cell tumors of the esophagus: report of five cases and review of diagnostic and therapeutic techniques. Dis Esophagus 2007;20:436-43. [DOI] [PubMed] [Google Scholar]
- 6.Ordonez NG. Granular cell tumor: a review and update. Adv Anat Pathol 1999;6:186-203. [DOI] [PubMed] [Google Scholar]
- 7.Abrikossoff A. Übermyome, ausgehend von der quegestreiften willkurlichen muskulatur. Virchows Arch Pathol Anat 1926;260:215-33. [Google Scholar]
- 8.Lack EE, Worsham GF, Callihan MD, et al. Granular cell tumors: a clinicopathologic study of 110 cases. J Surg Oncol 1980;13:301-16. [DOI] [PubMed] [Google Scholar]
- 9.Wang JF, Repertinger-Fisher S, Mittal SK, Deng C. A large esophageal granular cell tumor with review of literature. J Cancer Sci Ther 2011;3:213-5. [Google Scholar]
- 10.Huang AT, Dominguez LM, Powers CN, Reiter ER. Granular cell tumor of the cervical esophagus: case report and literature review of an unusual cause of dysphagia. Head Neck Pathol 2013;7:274-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.John BK, Dang NC, Hussain SA, et al. Multifocal granular cell tumor presenting as an esophageal stricture. J Gastrointest Cancer 2008;39:107-13. [DOI] [PubMed] [Google Scholar]
- 12.Palazzo L, Landi B, Cellier C, et al. Endosonographic features of esophageal granular cell tumors. Endoscopy 1997;29:850-3. [DOI] [PubMed] [Google Scholar]
- 13.Percinel S, Savas B, Yilmaz G, et al. Granular cell tumor of the esophagus: three case reports and review of the literature. Turk J Gastroenterol 2008;19:184-8. [PubMed] [Google Scholar]
- 14.Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol 1998;22:779-94. [DOI] [PubMed] [Google Scholar]
- 15.Hoess C, Freitag K, Kolben M, et al. FDG PET evaluation of granular cell tumor of the breast. J Nucl Med 1998;39:1398-401. [PubMed] [Google Scholar]


