Abstract
Vaccination represents the best option to protect humans against influenza virus. However, improving the effectiveness of current vaccines could better stifle the health burden caused by viral infection. Protein synthesis from individual genes can be downregulated by synthetically deoptimizing a gene’s codon usage. With more rapid and affordable nucleotide synthesis, generating viruses that contain genes with deoptimized codons is now feasible. Attenuated, vaccine-candidate viruses can thus be engineered with hitherto uncharacterized properties. With eight gene segments, influenza A viruses with variably recoded genomes can produce a spectrum of attenuation that is contingent on the gene segment targeted and the number of codon changes. This review summarizes different targets and approaches to deoptimize influenza A virus codons for novel vaccine generation.
Keywords: codon deoptimization, codon-pair bias, codon usage bias, inactivated influenza vaccines, influenza A virus, influenza reverse genetics, live attenuated influenza virus, recombinant influenza vaccine, synthetic attenuated virus engineering
Influenza A virus
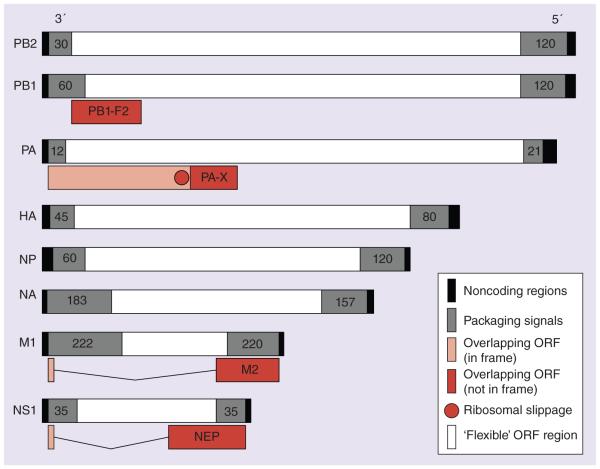
Influenza A viruses (IAVs) are enveloped viruses that belong to the Orthomyxoviridae family, and contain a genome comprised of eight segments of single-stranded negative-sense RNA that encode for 10–14 proteins (Figure 1) [1]. Influenza viruses are nearly unique among RNA viruses, in that they perform all viral RNA synthesis in the nucleus of infected cells [1]. The RNA-dependent RNA polymerase of influenza virus is a heterotrimeric complex consisting of the polymerase acidic (PA) and basic 1 and 2 (PB1, PB2) proteins, that together with the viral nucleoprotein (NP) are the minimal components for viral replication and transcription [2]. NP is associated with RNA-dependent RNA polymerase and viral RNA (vRNA) to form the viral ribonucleoprotein, which is the minimal infectious unit [2]. The eight influenza vRNA segments are flanked at both termini by noncoding regions, which possess partial fold-back complementarity between the 3′ and 5′ ends and serve as promoters for viral replication and transcription (Figure 1) [3,4]. Additionally, the noncoding regions together with nucleotide sequences located within the coding region termini are required for specific segment packaging (referred to as packaging signals) [5], albeit via an unknown mechanism (Figure 1). Defining these regions of the genome has been fundamental for studying IAV because the nucleotides, or perhaps RNA structures therein, create a ‘do not modify’ zone that needs to be conserved to reconstruct viruses with optimal fitness [5].
Figure 1. Influenza A virus genome organization and flexibility.
The eight influenza A virus segments are represented in 3′ to 5′ negative sense. Regions of flexibility are determined (white boxes) by areas inside ORFs that do not have cis-acting RNA elements (packaging signals and splice sites) or alternative overlapping ORFs. Noncoding regions are indicated in black boxes. Packaging signals are indicated in gray boxes. In frame (pink) and out of frame (red) overlapping ORFs are also indicated. Red circle indicates ribosomal slippage sequence.
ORF: Open reading frame.
The hemagglutinin (HA) and the neuraminidase (NA) glycoproteins are the major antigenic determinants of influenza virus and are essential for receptor binding and fusion, and virion release, respectively [6]. HA and NA within infected organisms and populations are driven to evolve antigenic variants via immunologic pressure, and positive selection of fit viruses occurs gradually in a process known as antigenic drift [7]. The antigenic diversity of glycoproteins is used to further classify IAV, of which there are 18 HA and 11 NA subtypes [1,8]. At least four of the eight segments encode more than one polypeptide using alternative splicing mechanisms (NEP and M2) [9,10], leaky ribosomal scanning that initiates alternative open reading frames (ORF; PB1-F2) [11] or ribosomal frame-shifting (PA-X) [12] (Figure 1). Additional gene products are being defined (M42, PB1-N40) [13] with incompletely understood expression regulation or function, and for the purpose of this review, are not discussed in further detail.
Innate immunity, coordinated mainly by the type-I interferon (IFN) response, is the first mechanism utilized by the host to control an invading viral pathogen [14]. To counteract the host response, influenza virus encodes for a potent IFN antagonist, the nonstructural protein 1 (NS1). NS1 elicits multiple effector mechanisms and RNA shielding dictated in part by its conformational plasticity [15]. Antagonism of IFN-induced genes is heightened by the ability of NS1 to limit the processing and nuclear export of host mRNA, which also contributes to virulence [16]. Taking advantage of viral immune evasion strategies, a variety of vaccine approaches modify NS1 to limit innate antagonism and attenuate the virus [17]. NS1 is produced from genome segment eight (NS), which encodes for two fundamentally distinct proteins through alternative splicing (Figure 1). The primary transcript encoded by segment eight is NS1, and a weak 5′ splice site results in a second product, the nuclear export protein (NEP) [10], which is expressed at approximately 10–15% the levels of NS1 [10]. NEP is necessary for the production of replication-competent virus and has several biologically important functions [10,18]. Segment seven (M) uses a similar strategy to produce at least two proteins, the primary transcript M1 and the alternatively spliced M2 (Figure 1) [9]. Both the M1 matrix protein and M2 ion channel are necessary for the life cycle of IAV and are major contributors to virion morphology, assembly and uncoating.
• Influenza A viruses as important human pathogens
Respiratory infections in humans caused by IAV are prevalent contributors of morbidity and mortality, and lead to significant economic impact every year [19]. Despite comprehensive vaccination programs, the WHO estimates the global disease burden from influenza results in 1 billion infections, 3–5 million cases of severe disease and between 300,000 and 500,000 deaths annually [20]. Additionally, IAV can lead to sporadic pandemics when novel viruses are introduced into humans [21]. The mechanisms involved in the emergence of seasonal epidemic and novel pandemic strains of IAV are mainly driven by antigenic drift and antigenic shift, respectively [4,7,22–23]. In the first case, which is common among RNA viruses, selected antigenic variant mutations are integrated in the viral genome. Such mutations may result in off-target changes to the virus tropism or increased levels of virus replication [7,22]. On the other hand, antigenic shift, which is common among segmented RNA viruses, results from coinfection of a host cell with two or more IAVs where vRNA in viral progeny is reassorted [4,23]. By acquiring gene constellations that confer optimal virus replication, transmissibility and immunologic stealth, reassortant IAVs can lead to a pandemic in an immunologically naive population. For instance, the first IAV pandemic of this century was declared in 2009 [24] with the emergence of a quadruple-reassortant swine-origin H1N1 IAV [25]. Within 6 months, the virus was detected in approximately 200 countries and infected >600,000 individuals worldwide, causing nearly 8000 deaths [26]. Influenza virus public health concerns are aggravated by the virus’s efficient transmission and limited antiviral therapeutic options [27]. Hence, vaccination remains the best medical intervention to protect humans against influenza virus, even though the effectiveness of current vaccines is suboptimal [28].
• The need of novel vaccines to combat influenza viruses
To date, three types of influenza virus vaccines are approved by the US FDA for human use: inactivated virus, recombinant viral HA and live attenuated virus [29–33] (Table 1). Regardless of the type of vaccine, most manufacturers strive to include three or four virus strains in each vaccine, two type A influenza strains (H1N1 and H3N2) and one or two type B influenza strains (Victoria-like and Yamagata-like) [31,34]. The most widely used influenza vaccine is the inactivated influenza vaccine (IIV), which elicits protective humoral immunity by inducing the production of neutralizing antibodies that target epitopes on HA, typically proximal to the receptor binding site [28,35]. The recombinant influenza vaccine (RIV), like IIV, is administered intramuscularly and safely elicits a protective antibody response [32]. Live attenuated viruses have been used against numerous viral diseases in the past and continue to protect people today [36]. In contrast to IIV and RIV, live attenuated influenza vaccine (LAIV) mimics natural virus infection, which consequently has risks and benefits [37]. An advantage is that LAIV provides cross-reactive, cell-mediated protection against heterotypic influenza virus strains [37,38] and, in adolescents, elicits a more efficient cellular and humoral immune response [29]. However, the tolerability of LAIV in specific populations is an important concern, and it is contraindicated in asthmatics due to wheezing [39]. Another concern is that the attenuated phenotype of LAIV is mainly conferred by just five point mutations located in PB2 (N265S), PB1 (K391E, E581G, A661T) and NP (34G) [40], and thus LAIV has a considerable chance of reverting or reassorting with circulating influenza strains to generate a novel virus.
Table 1.
Influenza vaccines.
| Characteristics | Current FDA-approved vaccines |
New vaccines |
||
|---|---|---|---|---|
| IIV | LAIV | RIV | CPB/CB | |
| Safety | ++ | + | ++ | ++ |
|
| ||||
| Immunogenicity | + | ++ | + | ++ |
|
| ||||
| Humoral response | Yes | Yes | Yes | Yes |
|
| ||||
| Cellular response | Weak | Yes | Weak | Yes |
|
| ||||
| Manufacturing method |
Egg-based production | Tissue culture (insect) | Tissue culture (mammalian) | |
CB: Codon bias; CPB: Codon pair bias; IIV: Inactivated influenza vaccine; LAIV: Live attenuated influenza vaccine; RIV: Recombinant influenza vaccine.
Although the past decades have witnessed considerable improvements in the development of influenza vaccines, much still needs to be done in order to increase the effectiveness of both seasonal and pre-pandemic influenza vaccines. Recently performed meta-analyses of vaccine studies in people found IIV and LAIV to be beneficial, where six of 17 studies found vaccination to confer significant protection against medically attended influenza infection [28]. A better comparison for a single season can be drawn for the year 2006, where RIV, IIV and LAIV vaccination was 86 [41], 77 and 53% [42] efficacious in various patient populations, despite mismatched HA antigenicity. It was surprising that LAIV had the lowest cross-protection, which may be partially due to limited cross-reactivity to the A/Ann/Arbor/6/60 virus backbone. It is also possible that IIV and RIV protect against antigenically drifted strains because of prior exposure to similar strains.
The most commonly used production methodology for seasonal inf luenza vaccines is growth in embryonated hen eggs. The WHO will improve vaccine production output by implementing a Global Action Plan on influenza vaccines [43], which has led to increased doses produced from eggs [44]. However, a significant hurdle exists in scaling up vaccine production in eggs to meet pandemic global need, as new egg sources close to vaccine facilities are difficult to create, especially since pandemic virus could easily eliminate entire chicken flocks. Perdue and colleagues provide a thorough review of the advantages and disadvantages of cell culture-based vaccines, which although have a better long-term benefit compared with the grandfathered-in egg production, can be difficult to implement due to stringent regulatory requirements and high infrastructure cost [45]. The developers of new vaccine approaches to prevent influenza viral infections must consequently be cognizant of the production, licensure and efficacy standards that currently available formulations utilize.
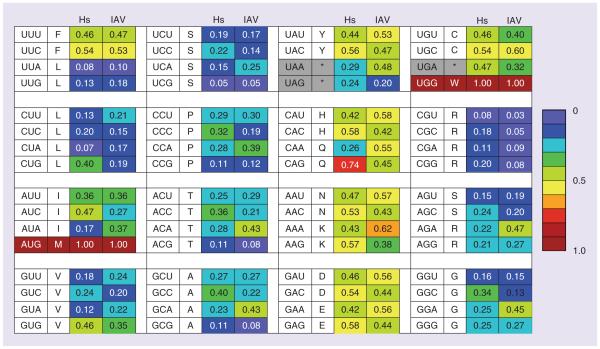
• Codon usage bias
In animals, the genetic code uses 61 codons, which encode 20 different amino acids and three stop codons (Figure 2). These codons are recognized by anticodons in complementary tRNAs that are coupled to the cognate amino acid. Consequently, the degeneracy of the genetic code allows for each amino acid to be encoded by multiple distinct codons (synonymous codons). Synonymous codons are not used with equal frequency within or between genomes [46]. Although the evolutionary pressure or consequence of codon preferences remains unclear, codon distribution could correspond with genome GC content. Also, codon biases that tend to reduce the diversity of isoacceptor tRNAs lessen the metabolic load and are therefore beneficial to organisms with rapid growth conditions [47]. Although the biological mechanism governing codon bias execution is ambiguous, these biases can control protein expression, which is a sophisticated mechanism of adaptation [47–49].
Figure 2. Codon bias of Homo sapiens and influenza A virus.
A codon chart with the relative synonymous codon usage is displayed. Relative synonymous codon usage values (data taken from [50]) and frequency per 1000 amino acids was represented as percent per amino acid. For consensus, 83,487 Homo sapiens and 40,413 influenza A virus coding sequences were evaluated.
Negative-stranded RNA viruses include a number of human and animal pathogens, such as IAV, respiratory syncytial virus (RSV), measles virus, rabies virus, Ebola virus, arenaviruses and others. These obligate intracellular pathogens all require host cell machinery to form infectious progeny, and because the virus is reliant on host cellular components for translation, the codon usage of viruses is affected by the codon bias within the host cell [51–57]. As early as 20 years ago, a correlation was detected between the prevalence of dinucleotides in viruses and their hosts [58], which suggested an active coadaptation process of viruses toward their hosts to increase the translational efficiency. Therefore, a correlation between codon usage and gene expression is expected [59].
Evidence for codon adaptation by viruses was provided by several observations. Epstein–Barr virus appears to deoptimize codon usage in latent stage genes, perhaps in order to reduce competition with host cell translation [60]. In an example to define host cell permissivity, it was shown that papillomavirus codon usage appears optimized for expression in certain cell types [61]. Experiments to show the loss of function consequence of codon adaptation successfully recoded poliovirus genes to contain disfavored synonymous codon pairs, where the synthetic poliovirus genes with underrepresented codons had correspondingly reduced protein expression levels, which led to virus attenuation [52]. Importantly, Bahir et al. demonstrated that viruses that infect humans, but not those that infect other mammals or birds, show a robust similarity to most mammalian and avian hosts, in terms of both amino acid and codon preferences [62]. Although many aspects related to virus–host codon bias adaptation are not completely understood, it is becoming more clear that viruses modify their codon usage according to the host they infect.
To date,studies of deliberate virus gene recoding have employed two specific approaches that have resulted in virus attenuation: codon usage bias [51,55,63] or codon-pair bias [52,54,57,64–65] deoptimization (Table 2). Codon usage bias refers to differences in the frequency of occurrence of synonymous codons in coding DNA/RNA sequences; therefore, to generate recombinant viruses with attenuated phenotypes, multiple codons in viral genes are substituted by the less representative codon with respect to the codon bias of the host [55]. For instance, the amino acid glutamine is encoded by two codons with different frequency in humans, CAA (27%) and CAG (73%) (Figure 2). Thus, all instances of CAG were replaced with the underrepresented CAA to deoptimize the codon usage. Codon-pair bias, on the other hand, refers to the preferential pairing of some codons over others, a phenomenon not related with codon bias, in which codons are used unequally. For example, the codon pair GCC-GAA encodes the amino acid alanine-glutamic acid, which occur together significantly less often than the pair GCA-GAG in humans. These frequencies do not take into account individual representation of codons because GCC and GAA are the most frequently used alanine and glutamic acid codons, respectively [52]. This approach was denominated ‘SAVE’ (synthetic attenuated virus engineering) and uses a computer algorithm to design codon-pair deoptimized genes, which can be applied to a wide range of viruses [52,54,57,64]. However, the mechanism and severity of viral attenuation following codon-pair bias deoptimization can be subjective by the influenza virus strain or the viral segment manipulated. Thus, after the bioinformatics approach, experimental characterization of the codon-pair deoptimized viruses needs to be performed to demonstrate viral attenuation.
Table 2.
Codon deoptimized viruses used as vaccines.
| Virus | Approach | Genes modified |
In vivo
attenuation |
Protection and immunogenicity |
Ref. |
|---|---|---|---|---|---|
| Respiratory syncytial virus |
CPB CB |
NS1, NS2, N, P, M, SH, G, F, L NS1 and NS2 |
Yes Yes |
Yes Yes |
[65] [63] |
|
| |||||
| Poliovirus | CPB | P1 capsid region |
Yes | ND | [52] |
|
| |||||
| Influenza virus | CPB CB |
PB1, HA, NP, NA NS |
Yes Yes |
Yes Yes |
[57,64] [55] |
CB: Codon bias; CPB: Codon pair bias; ND: Not determined.
It has been shown that the rearrangement of codons leads to a reduction of protein expression in tissue culture, at least at early times during infection [51–52,54–55,57,63–65]. Among the many factors that influence gene translation, the role of mRNA secondary structure has been shown to be of major importance [66]. The negative impact of mRNA structure on translation can reduce protein yield by blocking or slowing the initiation and movement of ribosomes along template mRNAs. For instance, regulation of gene expression is highly dependent on the formation of stable structures by nucleotide pairing in the mRNA strand [66]. Other factors such as tRNA expression levels, gene length composition bias (%GC content and GC skew), recombination rates and RNA stability, can also contribute to codon bias phenomena [47–49,58–59].
• Codon deoptimization to develop safe, immunogenic & effective live attenuated vaccines
RSV is a member of the Paramyxoviridae family, which contains important human pathogens that cause lower respiratory tract illness in young children, manifested as bronchiolitis and pneumonia [67]. RSV-associated lower respiratory tract illness results in approximately 66,000 to 199,000 deaths annually in children younger than 5 years old [67]. No antivirals are available yet, and prophylaxis with the humanized monoclonal antibody palivizumab to prevent RSV-associated disease is only available for infants with certain high risk factors [68]. Thus, developing safe and effective vaccines against RSV are of crucial importance. In order to develop potential vaccine candidates, codon bias or codon-pair bias deoptimization was used with RSV [63,65] (Table 2). Using codon bias, Meng et al. [63] deoptimized the nonstructural (NS1 and NS2) RSV proteins, which are key players in inhibiting IFN response [63]. The codon-deoptimized viruses generated showed attenuation in mice but replicated to high titers in FDA-approved Vero cells, also known to be deficient in IFN genes [69]. These results suggest that viral genes harboring the ability to interfere with the host IFN response are suitable candidates for codon rearrangement to generate safe live attenuated vaccines. In another study, Le Nouen et al. designed several live attenuated RSV vaccine candidates by codon-pair deoptimization [65]. The recombinant viruses were temperature-sensitive for replication in vitro, where viruses containing modifications in the G and F surface glycoproteins achieved the greatest restrictive effect. Recombinant RSV were attenuated yet immunogenic in mice and African green monkeys, exhibiting a range of restriction comparable to that of two attenuated RSV strains being tested in clinical trials [65].
Likewise, Coleman et al. engineered recombinant viruses containing different rates of codon deoptimized regions within the poliovirus capsid protein [52] (Table 2) to show that viral attenuation was directly associated with the grade of gene deoptimization that correlated with decreased rates of protein translation [52]. Importantly, polioviruses containing such amino acid-independent changes were attenuated in mice and conferred protective immunity after challenge [52].
• Rescue of influenza viruses using plasmid-based reverse genetics
Efforts by a number of research groups were fundamental in the development of influenza reverse genetics [70–73]. Established in 1999, plasmid-based reverse genetic techniques allowing for the generation of wild-type and recombinant viruses have revolutionized influenza virus research [70,71]. Since the inception of this technique, the advances in the understanding of influenza biology, vaccine candidates and therapeutic developments have been exponentially improved [72]. Initial technologies to generate recombinant infectious influenza viruses required the use of 12 plasmids, where eight polymerase I-driven plasmids encode the vRNA genes with exact 3′ and 5′ termini and four polymerase II-driven plasmids encoding the influenza viral proteins necessary for viral genome replication and gene transcription (viral ribonucleoproteins; PB2, PB1, PA and NP) [70]. A year later, plasmid-based systems for rescuing influenza viruses was reduced to eight with the use of ambisense expression plasmids, that each express both viral and messenger RNA [73]. This technology simplified the rescue of influenza viruses with modifications within independent segments, and enabled the generation of multiple recombinant viruses with a constellation of nonmodified and modified viral genes, including recombinant influenza viruses. Importantly, influenza plasmid-based reverse genetics techniques have been developed to generate recombinant influenza viruses in FDA-approved vaccine Vero [69] and Madin-Darby canine kidney (MDCK) [74] cells.
Manipulation of codon usage to develop influenza A virus vaccines
In the context of IAV, many nucleotides cannot be modified because of their role in segment packaging, splicing or ribosomal frameshifting, or because of the presence of multiple overlapping ORFs (Figure 1 & Table 3) [75–80]. To date, IAV vaccine candidates that have utilized codon-pair [57,64] or codon bias [55] deoptimization as a means of influenza virus attenuation have decreased expression levels of PB1, HA and NP [57]; NA and HA [64]; or NS1 and NEP [55] (Figure 3 & Table 4). Successful vaccine candidates must show attenuation in the host while retaining immunogenicity and must also grow well in manufacturing suitable tissue culture cells or egg platforms [37,74]. Importantly, all viruses generated by codon reorganization reported so far showed similar plaque phenotypes and viral titers in MDCK cells, a recently FDA-approved cell line for influenza vaccine production [74]. However, the ability of these recombinant viruses to replicate in eggs has not yet been evaluated, even though egg-based manufacturing is still the most common substrate for influenza vaccine production [74]. Furthermore, the primary characterization of these vaccines all used mouse models of influenza viral infection and vaccination, which do not most accurately reflect virus pathogenesis and immunology [81], are known to be more permissive to heterologous virus challenge [82], and do not represent the same codon usage bias as humans. Necessary for vaccine development will be testing other animal models (guinea pigs, ferrets, nonhuman primates) before clinical trials can begin.
Table 3.
Cis-acting elements in influenza A virus determine regions of codon ‘flexibility.’
| Viral segment |
Major transcript |
Segment length |
Primary ORF |
Secondary ORF |
3’ NCR | 3’† | Flexible | ORF 5’† | 5’ NCR | Strain | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | PB2 | 2341 | 28–2307 | 27 | 30 | 2130 | 120 | 34 | WSN | [76] | |
|
| |||||||||||
| 2 | PB1, PB1-F2 |
2341 | 25–2298 | 101–373 | 24 | 60 | 1821 | 120 | 43 | WSN | [76] |
|
| |||||||||||
| 3 | PA, PA-X |
2233 | 25–2175 | 25–784 | 24 | 12 | 1931 | 21 | 58 | WSN | [76] |
|
| |||||||||||
| 4 | HA | 1775 | 33–1730 | 32 | 45 | 1572 | 80 | 45 | PR8 | [77] | |
|
| |||||||||||
| 5 | NP | 1565 | 46–1542 | 45 | 60 | 1316 | 120 | 23 | WSN | [75] | |
|
| |||||||||||
| 6 | NA | 1409 | 20–1381 | 19 | 183 | 1021 | 157 | 28 | WSN | [78] | |
|
| |||||||||||
| 7 | M1 M2 |
1027 | 26–785 | 26–52 740–1007 |
25 | 222 | 492 | 220 | 20 | WSN | [80] |
|
| |||||||||||
| 8 | NS1 NEP |
890 | 27–720 | 27–67 540–867 |
26 | 35 | 478 | 35 | 23 | WSN | [79] |
Numbers represent nucleotide positions in the negative sense (obtained from [83]).
Packaging signals.
NCR: Noncoding regions; ORF: Open reading frame.
Figure 3. Proposed mechanism of attenuation for codon deoptimized influenza A viruses.
(A) Schematic representation of wild-type influenza infection in a permissive cell. First, vRNP-mediated replication and transcription occurs in the cell nucleus, followed by viral protein synthesis (shown here as the HA and NA glycoproteins, and the IFN antagonist NS1), export of vRNPs from the nucleus (indicated by arrow) and production of infectious progeny (black virions). (B) During PR83F infection (light gray virions), less viral genome replication and gene transcription mediated by PB1 and NP deoptimization leads to a decrease in all viral proteins and their functions, including influenza NS1, nuclear export of vRNPs and virion production. (C) A paucity of influenza glycoproteins during (NA + HA)Min infection (dark gray virions) results in ample viral protein production but minimal virion formation and release because of decreased levels of IAV HA and NA. (D) Infection with PR8 NScd (white virions) stimulates type I IFN responses because of suboptimal NS1 levels, and inefficient nuclear export of vRNPs due to low NEP levels. For simplicity, only certain stages of the life cycle are represented.
IAV: Influenza A viruses; vRNP: Viral ribonucleoprotein.
Table 4.
Characteristics of influenza A viruses with codon deoptimized genes.
| Influenza viral gene(s) |
Approach | Growth in MDCK cells | Growth in A549 cells | Attenuation in mice |
Protection in mice |
MLD50 | Ref. |
|---|---|---|---|---|---|---|---|
| PB1 | CPB | Similar to WT | ND | ND | ND | 2.7 | [57] |
|
| |||||||
| NP | CPB | Similar to WT | ND | ND | ND | 0.91 | [57] |
|
| |||||||
| HA | CPB | Similar to WT | ND | ND | ND | 1.4 | [57,64] |
|
| |||||||
| NA | CPB | Similar to WT | ND | ND | ND | 3.9 | [64] |
|
| |||||||
| PR83F | CPB | Similar to WT | ND | Yes | Yes | 4.1 | [57] |
|
| |||||||
| NA + HA | CPB | Similar to WT | Less replication | Yes | Yes | 5 | [64] |
|
| |||||||
| NS1 | CB | Similar to WT | Less replication | Yes | ND | 0.33 | [55] |
|
| |||||||
| NEP | CB | Similar to WT | Similar to WT | No | ND | 1.3 | [55] |
|
| |||||||
| NS | CB | Similar to WT | Less replication | Yes | Yes | 1.5 | [55] |
CB: Codon bias; CPB: Codon pair bias; MLD50: Fold increase in MLD50 over WT virus (log10 scale); ND: Not determined; PR83F: PB1, NP and HA were modified.
• PB1, HA & NP codon-pair deoptimization
Mueller et al. used SAVE to rationally design codon-pair bias-mutant LAIV vaccines by engineering recombinant segments that contained modifications in large regions of the coding sequence in the genes coding for PB1, HA and NP proteins of influenza virus A/Puerto Rico/8/34 H1N1 (PR8), either individually (PR8-PB1Min, PR8-HAMin and PR8-NPMin) or all together (PR83F) (Figure 3B & Table 4) [57]. Genes were engineered so that packaging signals were not modified within these segments, and because PB1-F2 is translated from an overlapping ORF within vRNA segment 2, this region was also avoided. Results in vitro showed that all mutant viruses formed plaques that were either indistinguishable from, or only slightly smaller than the wild-type virus. Although the mutant viruses did not grow as well as wild-type virus in MDCK cells, differences in peak titers were only tenfold (1 log10) lower, and protein synthesis was not affected. In vivo, the mouse lethal dose 50% (MLD50) values were 1–4 log10 higher than wild-type virus, depending on the segment deoptimized. PR83F was the most attenuated, as expected, and grew to levels 2–3 log10 lower than wild-type virus in the lung. Importantly, immunization of mice with a single dose of PR83F conferred protection against subsequent lethal challenge with PR8 wild-type virus. However, the ability of this recombinant PR83F to confer protection against a heterologous influenza A challenge was not evaluated.
• HA & NA codon-pair deoptimization
In a follow-up study, Yang et al. also used SAVE to generate recombinant PR8 viruses where codon pairs in NA (PR8-NAMin) or NA and HA ([NA + HA]Min) viral segments were deoptimized (Figure 3C & Table 4) [64]. Although deoptimization of the major antigenic determinants of the virus may seem counterproductive for viral immunogenicity, the authors rationalized that these recombinant codon-pair deoptimized influenza viruses would lack a defect in viral replication due to maintenance of the wild-type viral replication machinery (namely PB2, PB1, PA and NP) [64]. Despite reduced protein expression of NA and HA, all variants replicated well in MDCK cells as compared with wild-type PR8 virus. In mice, however, only (NA + HA)Min was tested, which displayed severe attenuation, since the MLD50 for (NA + HA) virus was >3.16 × 106 plaque-forming units (PFU) (~5 log10 times higher than wild-type PR8). Vaccinated mice were protected against homologous PR8 challenge and showed a robust humoral response as demonstrated using a hemagglutination inhibition assay. Additionally, immunization with (NA + HA)Min also protected against heterologous lethal challenges of a mouse-adapted H3N2 virus (A/Aichi/2/1968 or A/Victoria/3/75), likely due to activation of cellular immune responses. The authors demonstrated that despite the reduced expression of viral glycoproteins, which are important immunogens and responsible for virus cell entry and release, (NA + HA)Min vaccination led to a safe and protective immune response that conferred protection against both homologous and heterologous influenza viral challenges.
• NS1 & NEP codon usage deoptimization
Rather than using SAVE to recode codon pairs, Nogales et al. deoptimized the eighth (NS) segment of influenza PR8 according to codon usage bias. NS produces the IFN antagonist NS1 protein and the alternatively spliced product NEP (Figure 3D & Table 4) [55]. Because nucleotide fidelity in this segment is important for packaging signals, splice donor/acceptor activity and conserving codons in overlapping ORFs, the authors deoptimized small portions of the ORF for each viral mRNA, yielding 28 and 4% deoptimized codons for NS1 and NEP, respectively. In vitro characterization of this PR8 NS codon deoptimized virus (NScd) showed that virus fitness was not significantly decreased in MDCK cells despite reduced protein accumulation of deoptimized mRNAs. However, the phenotype of NScd virus in human alveolar epithelial (A549) cells displayed impaired growth relative to wild type. The most notable outcome of decreased NS1 expression could be a compromised ability of the codon-deoptimized virus to antagonize the host innate immune response [16]. Experiments using virus- and cell-based bioassays that evaluate the production of type I IFN showed that PR8 NScd less stringently restricted type I IFN release compared with wild-type PR8, perhaps contributing to the reduced growth phenotype in human A549 cells. Additionally, NS1 has been implicated in auto-regulating segment eight splicing to control expression [16]. This mechanism, paired with the suboptimal splice acceptor site identified for NEP [84], suggests that the splicing or differential expression balance between NS1 and NEP is tightly regulated and important for the virus. Nogales et al. also evaluated the abundance of segment eight vRNA, as well as the two resulting mRNA transcripts in infected cells and showed that mRNA accumulation was not significantly altered during PR8 NScd infection compared with wild-type PR8 viral infection. Lastly, it is interesting to note that trace amounts of NS1 have been recently shown to be specifically packaged into influenza virions [85]. The reduction of cytoplasmic NS1 protein available during PR8 NScd infection could consequently lead to decreased incorporation of NS1 into viral progeny, potentially affecting fitness.
To evaluate the potential of NScd virus as a vaccine, MLD50 values, representing tolerability, were calculated from mice infected with NS1cd, NEPcd or NScd recombinant PR8 viruses. Despite the minimal effect on virus growth in vitro, NScd was most strongly attenuated compared with wild type. The authors showed that a vaccine dose of 100 PFU of NScd that did not result in morbidity or mortality was sufficient to confer protection against lethal challenges of either 10 or 100 MLD50 of homologous PR8 and heterologous (X31, H3N2) influenza viruses. Characterization of the humoral response from vaccinated mice revealed that NScd induced protective hemagglutination inhibition titers (>1:40) and significant antibodies that reacted to purified recombinant HA or infected cell lysates. Although PR8 NScd (MLD50 of ~3 × 102 PFU) was perhaps less attenuated than PR83F (MLD50 of ~7.9 × 106 PFU) or (NA + HA)Min virus (MLD50 of ~3.16 × 106 PFU) (Table 4), provided another viral segment target for attenuation to develop influenza vaccine candidates. Importantly, introducing attenuation in an additional influenza viral segment (NS) decreases the potential generation of virus with pathogenicity in case of reassortants with circulating influenza strains. Furthermore, because the mechanism of attenuation likely coincides with an enhanced type I IFN response, PR8 NScd may be beneficial for stimulating adjuvanticity of a vaccine candidate.
Advantages & disadvantages of influenza viral segments targeted for codon deoptimization vaccine development
IAVs containing suboptimal codon arrangements in genes that constitute the viral polymerase (PB2, PB1 and PA) would likely have the most dramatic affect on virus fitness, as limiting accumulation of these viral proteins would exponentially reduce genome replication and gene transcription and therefore production of other viral proteins. MLD50 values calculated from mice infected with PR8-PB1Min, -HAMin or -NPMin (MLD50 values of ~3.2 × 104, ~1.7 × 103 and ~5 × 102 PFU, respectively) support this hypothesis, as viruses encoding PR8-PB1Min were most significantly attenuated [57]. Although IAV NP is also required for viral genomic replication, new evidence suggests that this is template-length dependent [86], thus perhaps the diminished amount of expression in NPMin is sufficient for virus growth. The virus containing all three deoptimized IAV segments (PR83F) was used as a potential vaccine in mice; however, there may be some limitations to reducing the ability of the virus to replicate its genome in terms of industrial vaccine production or vaccine immunogenicity. For example, antigen dose has been shown to directly correlate with antigenicity of vaccine immunogens [29,87]. Repeat exposure to vaccine through a prime and boost strategy is one possible way to circumvent diminished immunogenicity. The principle of decreased genome replication can be alternatively used to support development of more safe LAIV alternatives. Although the LAIV FluMist is the most effective influenza vaccine in adolescents [29], it is contraindicated in children less than 6 months of age and asthmatics due to complications that include wheezing [39]. Decreasing the replicative ability of the virus could substantially increase the therapeutic index, allowing these current risk groups to be included using the codon deoptimized attenuated approach.
HA and NA are the major antigenic determinants of IAV [37,88]. Influenza virions are coated with an approximate 6:1 ratio of HA to NA [89], and antibodies directed against the receptor binding domain of HA can neutralize antigenically matched virus [4,33]. Additionally, new strategies that induce broadly reactive neutralizing antibodies against the conserved HA regions are being explored as a means to develop a universal influenza vaccine [90]. Furthermore, antibodies that recognize NA can also neutralize influenza virus, albeit to a lesser extent than HA antibodies [91]. Thus, strategies that deliberately reduce the abundance of HA or NA may consequently limit antigen concentration in vivo and subsequent production of neutralizing antibodies. Indeed, experiments by Yang et al. showed that hemmagglutination inhibition titers were lower in (NA + HA)Min as compared with wild-type immunized mice [64]. However, both PR83F and (NA + HA)Min, which each have reduced production of IAV HA, were able to confer protection from homologous challenge [64]. These results suggest a cell-mediated component for immunogenicity, which may be attributed to the duration of antigen abundance, where infectious virus was recovered up to 7 days postinfection with both PR83F and (NA + HA)Min IAVs [64].
Early infection with influenza virus in vivo is cloaked by a blockade of innate immune responses via NS1 [16,17]. Results in vitro suggest that reduced NS1 production in NScd virus more readily trips the alarm signaling viral infection [55,92–94]. Activation of type I IFN is coupled to immune cell recruitment and pathogen clearance [95], thus NScd may more readily be cleared. Although these hypotheses were not tested directly in vivo, unpublished observations suggest a more rapid induction of type I IFN stimulated gene production in NScd compared with wild-type infected mice [55]. The consequence of this activation remains to be explored, where faster antigen clearance could limit adaptive immune magnitude, but more inflammation may have an opposite effect. In terms of human vaccination, a virus that exists for a shorter duration in vivo would have a lower opportunity to reassort with circulating IAVs, alleviating one of the caveats of LAIV vaccination.
Summary of codon deoptimized influenza A virus vaccines
Protection against persistent seasonal or potential pandemic influenza viruses of avian origin requires constant surveillance and annual reformulation of vaccines [37]. Compared with previous approaches of reassortment to generate vaccine seeds, plasmid-based reverse genetics to rescue recombinant influenza viruses significantly reduces vaccine production time [70–71,73]. However, in the advent of a pandemic, as evidenced by the H1N1 influenza outbreak in 2009, current methodologies are not rapid enough to produce sufficient vaccine doses before substantial transmission occurs [24–25,69,74]. Improvements in sequencing for surveillance coupled with gene synthesis and virus production from cell culture could significantly reduce time of vaccine manufacturing. The approaches reviewed herein provide a deliberate method of attenuation, which should be applicable for all isolates of influenza virus. However, it will be important to test various genetic backbones of influenza virus (e.g., H3N2, H5N1, influenza B) to be certain that attenuation is not limited to the as-of-yet studied IAV PR8 H1N1 backbone.
Unlike their in vitro phenotype, the codon deoptimized IAV were attenuated in vivo and were also shown to be immunogenic [55,57,64]. Although deoptimized influenza viruses replicated well in MDCK cells, the replicative abilities of codon deoptimized PR8 IAVs were impaired, with respect to wild type, in human alveolar epithelial (A549) cells, which may possibly be a better model to mimic IAV infections in vivo (in mice) or in humans [55]. However, the differences observed between both cell lines remain unclear and could be perhaps due to type I IFN signaling pathway differences [96]. Alternatively, differences in tRNA pools may elicit this phenotypic difference. Molecular evolutionary investigations suggest that codon usage bias varies both within and between genomes and may have significant relevance to understanding genome evolution among related species [59,62,97]. Therefore, the codon rearrangement could also be a powerful tool to study several aspects of virus biology, such as virus adaptation or evolution. In fact, previous studies have been performed on the general codon usage of IAV [53]. Recoding IAV, taking into account codon bias, base composition and adaptation to the host, may provide important clues to develop new and appropriate vaccines. In addition these viruses could be used to study virus–host interactions, since differences between cell lines were also observed [55].
Due to its broad species tropism, circulating IAV infect animals of agricultural (poultry and swine) and domestic (horses and dogs) importance [98]. The financial burden associated with IAVs in domesticated animals is difficult to predict, but is believed to be severe. Therefore, cost-effective and efficacious influenza vaccines that protect these susceptible animal populations are an important niche to target for future vaccine development. In 2013, losses in the poultry industry due to IAV H7N9 in China included culling of flocks, decreased sales of live poultry and market-stall rentals, which cost upward of US$1.8 billion dollars [99]. Other than the cost of losing infected populations, all IAVs are maintained in the avian reservoir, and swine serve as a ‘mixing vessel’ wherein swine, avian and human IAVs can reassort to generate novel IAV strains with pandemic potential [25]. Using similar approaches as described in this review to produce human IAV vaccines, codon usage or pair bias can be used to supply influenza vaccines for susceptible agricultural or domestic animals. Rewriting algorithms that recode genes for deoptimization in Homo sapiens to recode genes for deoptimization of other species such as Gallus gallus or Sus scrofa will provide possible IAV candidate vaccines to protect chickens or swine, respectively. Of course, initial testing of codon deoptimized LAIVs in these animals need to be performed.
With the moderate efficacy of IIV [28], approaches that better confer protection against matched strains or that induce broad immunity against drifted variant viruses are needed. Deoptimization of codon usage or pairs has the potential to replace current longstanding vaccine methodologies for several reasons: production of codon deoptimized virus is similarly efficient as wild-type virus in FDA-approved substrates like MDCK cells; attenuated segments contain a large number (hundreds) of silent nucleotide changes introduced in one or multiple viral genes or segments, making reversion to virulent wild type highly unlikely; live attenuated virus vaccines engineered by codon deoptimization express an intact viral antigenic repertoire of T- and B-cell epitopes, and consequently may induce both cellular and humoral immune responses against all viral immunogens; and safety of vaccine viruses can be titrated to target patients contraindicated for LAIV FluMist depending on deoptimized segment choice or segment numbers. Furthermore, combination of temperature sensitivity from the LAIV with codon deoptimization approaches can assure a higher safety profile for the development of safer LAIVs. Likewise, combination of both codon usage and pair bias may prove to more highly attenuate influenza viruses for LAIV development.
Conclusion
In the present work, we have reviewed the utility of codon deoptimization to alter the replicative fitness of IAV. Vaccines based on changes of codons could principally be generated rapidly in response for any of emerging, potentially pandemic, influenza viruses. To date, all studies of deliberate virus gene recoding have employed two specific approaches, codon usage bias or codon-pair bias, which have resulted in cell type-specific virus fitness loss in vitro, and attenuation in vivo. Importantly, codon deoptimized viruses will express an intact repertoire of antigenic sites because the amino acid sequence is not altered, thus conserving maximum immunogenicity for cellular and humoral immunity. Using new technologies, viral segments can be produced by de novo synthesis in a few weeks, hastening the time from surveillance of seasonal or pandemic strains to vaccine development.
Future perspective
Some virus vaccines developed in the mid 20th century have helped toward eradication of infectious diseases. Similar technology, deployed simultaneously against the influenza virus pathogen, has not nearly accomplished the same feat. Due to its natural reservoir and broad host species, the evolvability at major antigenic sites, and ability to reassort, developing the technology to extinguish or improve upon current vaccine efficacy has remained elusive. Significant progress has been made since developing plasmid-based systems to rescue recombinant virus, and there is a renewed hope for a universal influenza vaccine due to research within the past 5 years. Will the next 5 years bring society closer to taming the influenza virus? Declining cost of DNA synthesis may be the best weapon we have to more efficiently adapt to the changing influenza virus, and deoptimizing virus codons leaves a small risk for unforeseen pathogenic reversion. Regulatory and production concerns add time to vaccine roll-out, but the looming threat of the next pandemic warrants all options to limit virus spread. With more studies that demonstrate the dramatic therapeutic index of codon deoptimized viruses, it is possible that de novo synthesis of deoptimized circulating strains is a real alternative for future vaccinations.
EXECUTIVE SUMMARY.
Background
Influenza viruses are segmented, negative-sense, single-stranded RNA viruses.
Influenza viruses affect up to 500 million people annually, with children and elderly being the most vulnerable to severe illness.
Current vaccine approaches for influenza are limited to the nonreplicating inactivated influenza vaccine and recombinant influenza vaccine, and the temperature-sensitive, cold-adapted, live attenuated influenza vaccine.
The degeneracy of the genetic code has been evolved in different species such that frequencies of codon usage (codon usage bias), or their relative order (codon pair bias) can effect gene expression levels.
By deliberately deoptimizing codon usage or pairs, researchers have synthetically engineered influenza gene segments that are expressed at low levels in mammalian cells, and used plasmid-based reverse genetics to rescue recombinant deoptimized viruses.
Manipulation of codon usage to develop influenza A virus vaccine
Influenza viral segments 2 (PB1), 4 (HA), 5 (NP), 6 (NA) and 8 (NS) have been targeted for deoptimization, in a variety of combinations.
Deoptimized influenza virus segments were proven to be safe alone or in combination within viruses in mouse models of influenza virus infection.
Recombinant codon deoptimized influenza viruses have been shown to confer protection against homologous and heterologous lethal viral challenges in mice.
Advantages & disadvantages of influenza viral segments targeted for codon deoptimization vaccine development
Three major virus functions are carried out by the influenza segments targeted for deoptimization: virus replication, attachment/release, innate immune antagonism.
Future work evaluating how the functions above attribute to virus attenuation, immunogenicity or protective efficacy remain to be explored.
Summary of codon deoptimized influenza A viruses
The degree of attenuation or immunogenicity of codon deoptimized viruses can be titrated by selecting which and what percentage of viral segments to deoptimized.
Using similar approaches as described in this review for human influenza viruses, codon usage or pair bias approaches can be applied to benefit susceptible agricultural or domestic animals.
Conclusion
More effective influenza vaccines, or vaccine formulations that can be provided to a wider patient population are urgently needed for seasonal and potentially pandemic influenza viruses.
Codon deoptimization of influenza viruses represents an alternative approach for the development of live attenuated influenza vaccine.
Future perspective
Downregulating viral gene expression through de novo virus synthesis with deoptimized codons is becoming fast and less expensive.
Immunity against ‘exotic’ HAs could be achieved by vaccinating with synthesized deoptimized influenza viruses for pandemic preparedness.
Similar approaches can be developed for the generation of live attenuated viruses for other human viral pathogens.
Acknowledgments
SF Baker support was provided by the NIH Immunology Training Grant T32 AI 007285-26. Influenza virus research in L Martínez-Sobrido laboratory was partially funded by the NIAID Centers of Excellence for Influenza Research and Surveillance (CEIRS HHSN-266200700008C) and by the 2014 University of Rochester Research Award.
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- 1.Shaw ML, Palese P. Orthomyxoviridae: the viruses and their replication. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, editors. Fields Virology. 5th Lippincott Williams and WIlkins: PA, USA: 2007. [Google Scholar]
- 2.Resa-Infante P, Jorba N, Coloma R, Ortin J. The influenza virus RNA synthesis machine: advances in its structure and function. RNA Biol. 2011;8(2):207–215. doi: 10.4161/rna.8.2.14513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flick R, Neumann G, Hoffmann E, Neumeier E, Hobom G. Promoter elements in the influenza vRNA terminal structure. RNA. 1996;2(10):1046–1057. [PMC free article] [PubMed] [Google Scholar]
- 4.Baker SF, Nogales A, Finch C, et al. Influenza A and B virus intertypic reassortment through compatible viral packaging signals. J. Virol. 2014;88(18):10778–10791. doi: 10.1128/JVI.01440-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hutchinson EC, Von Kirchbach JC, Gog JR, Digard P. Genome packaging in influenza A virus. J. Gen. Virol. 2010;91:313–328. doi: 10.1099/vir.0.017608-0. Pt 2. [DOI] [PubMed] [Google Scholar]
- 6.Varghese JN, Mckimm-Breschkin JL, Caldwell JB, Kortt AA, Colman PM. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins. 1992;14(3):327–332. doi: 10.1002/prot.340140302. [DOI] [PubMed] [Google Scholar]
- 7.Carrat F, Flahault A. Influenza vaccine: the challenge of antigenic drift. Vaccine. 2007;25(39–40):6852–6862. doi: 10.1016/j.vaccine.2007.07.027. [DOI] [PubMed] [Google Scholar]
- 8.Tong S, Zhu X, Li Y, et al. New world bats harbor diverse influenza A viruses. PLoS Pathog. 2013;9(10):e1003657. doi: 10.1371/journal.ppat.1003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wise HM, Hutchinson EC, Jagger BW, et al. Identification of a novel splice variant form of the influenza A virus M2 ion channel with an antigenically distinct ectodomain. PLoS Pathog. 2012;8(11):e1002998. doi: 10.1371/journal.ppat.1002998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paterson D, Fodor E. Emerging roles for the influenza A virus nuclear export protein (NEP) PLoS Pathog. 2012;8(12):e1003019. doi: 10.1371/journal.ppat.1003019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hai R, Schmolke M, Varga ZT, et al. PB1-F2 expression by the 2009 pandemic H1N1 influenza virus has minimal impact on virulence in animal models. J. Virol. 2010;84(9):4442–4450. doi: 10.1128/JVI.02717-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jagger BW, Wise HM, Kash JC, et al. An overlapping protein-coding region in influenza A virus segment 3 modulates the host response. Science. 2012;337(6091):199–204. doi: 10.1126/science.1222213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wise HM, Foeglein A, Sun J, et al. A complicated message: identification of a novel PB1-related protein translated from influenza A virus segment 2 mRNA. J. Virol. 2009;83(16):8021–8031. doi: 10.1128/JVI.00826-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Randall RE, Goodbourn S. Interferons and viruses: an interplay between induction, signalling, antiviral responses and virus countermeasures. J. Gen. Virol. 2008;89:1–47. doi: 10.1099/vir.0.83391-0. Pt 1. [DOI] [PubMed] [Google Scholar]
- 15.Hale BG. Conformational plasticity of the influenza A virus NS1 protein. J. Gen. Virol. 2014;95:2099–2105. doi: 10.1099/vir.0.066282-0. Pt 10. [DOI] [PubMed] [Google Scholar]
- 16.Hale BG, Randall RE, Ortin J, Jackson D. The multifunctional NS1 protein of influenza A viruses. J. Gen. Virol. 2008;89(Pt 10):2359–2376. doi: 10.1099/vir.0.2008/004606-0. [DOI] [PubMed] [Google Scholar]
- 17.Richt JA, Garcia Sastre A. Attenuated influenza virus vaccines with modified NS1 proteins. Curr. Top Microbiol. Immunol. 2009;333:177–195. doi: 10.1007/978-3-540-92165-3_9. [DOI] [PubMed] [Google Scholar]
- 18.Bullido R, Gomez-Puertas P, Saiz MJ, Portela A. Influenza A virus NEP (NS2 protein) downregulates RNA synthesis of model template RNAs. J. Virol. 2001;75(10):4912–4917. doi: 10.1128/JVI.75.10.4912-4917.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 20.Girard MP, Cherian T, Pervikov Y, Kieny MP. A review of vaccine research and development: human acute respiratory infections. Vaccine. 2005;23(50):5708–5724. doi: 10.1016/j.vaccine.2005.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith GJ, Vijaykrishna D, Bahl J, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459(7250):1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 22.Kilbourne ED. Influenza pandemics of the 20th century. Emerg. Infect. Dis. 2006;12(1):9–14. doi: 10.3201/eid1201.051254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu X, Lindstrom SE, Shaw MW, et al. Reassortment and evolution of current human influenza A and B viruses. Virus Res. 2004;103(1–2):55–60. doi: 10.1016/j.virusres.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 24.WHO Influenza (Seasonal) Fact sheet No. 211. www.who.int/mediacentre/factsheets/fs211/en/
- 25.Garten RJ, Davis CT, Russell CA, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325(5937):197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maines TR, Jayaraman A, Belser JA, et al. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science. 2009;325(5939):484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynch JP, 3rd, Walsh EE. Influenza: evolving strategies in treatment and prevention. Semin. Respir. Crit. Care Med. 2007;28(2):144–158. doi: 10.1055/s-2007-976487. [DOI] [PubMed] [Google Scholar]
- 28.Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect. Dis. 2012;12(1):36–44. doi: 10.1016/S1473-3099(11)70295-X. [DOI] [PubMed] [Google Scholar]
- 29.Belshe RB, Edwards KM, Vesikari T, et al. Live attenuated versus inactivated influenza vaccine in infants and young children. N. Engl. J. Med. 2007;356(7):685–696. doi: 10.1056/NEJMoa065368. [DOI] [PubMed] [Google Scholar]
- 30.Belshe RB, Newman FK, Wilkins K, et al. Comparative immunogenicity of trivalent influenza vaccine administered by intradermal or intramuscular route in healthy adults. Vaccine. 2007;25(37–38):6755–6763. doi: 10.1016/j.vaccine.2007.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pronker ES, Claassen E, Osterhaus AD. Development of new generation influenza vaccines: recipes for success? Vaccine. 2012;30(51):7344–7347. doi: 10.1016/j.vaccine.2012.09.071. [DOI] [PubMed] [Google Scholar]
- 32.Cox MM, Patriarca PA, Treanor J. FluBlok, a recombinant hemagglutinin influenza vaccine. Influenza Other Respir. Viruses. 2008;2(6):211–219. doi: 10.1111/j.1750-2659.2008.00053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker SF, Guo H, Albrecht RA, Garcia-Sastre A, Topham DJ, Martinez Sobrido L. Protection against lethal influenza with a viral mimic. J. Virol. 2013;87(15):8591–8605. doi: 10.1128/JVI.01081-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun W. Approval Letter - Fluarix Quadrivalent (BL 125127/513) U.S. Food and 976 Drug Administration (FDA) www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm332484.htm.
- 35.Belongia EA, Kieke BA, Donahue JG, et al. Effectiveness of inactivated influenza vaccines varied substantially with antigenic match from the 2004–2005 season to the 2006–2007 season. J. Infect. Dis. 2009;199(2):159–167. doi: 10.1086/595861. [DOI] [PubMed] [Google Scholar]
- 36.Tlaxca JL, Ellis S, Remmele RL., Jr Live attenuated and inactivated viral vaccine formulation and nasal delivery: potential and challenges. Adv. Drug Deliv. Rev. 2014 doi: 10.1016/j.addr.2014.10.002. doi: 10.1016/j.addr.2014.10.002. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 37.Pica N, Palese P. Toward a universal influenza virus vaccine: prospects and challenges. Annu. Rev. Med. 2013;64:189–202. doi: 10.1146/annurev-med-120611-145115. [DOI] [PubMed] [Google Scholar]
- 38.Gorse GJ, Belshe RB, Munn NJ. Superiority of live attenuated compared with inactivated influenza A virus vaccines in older, chronically ill adults. Chest. 1991;100(4):977–984. doi: 10.1378/chest.100.4.977. [DOI] [PubMed] [Google Scholar]
- 39.Greenhawt MJ. Influenza vaccination in asthmatic patients. J. Allergy. Clin. Immunol. 2014;133(4):1233–1234. doi: 10.1016/j.jaci.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 40.Jin H, Zhou H, Lu B, Kemble G. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J. Virol. 2004;78(2):995–998. doi: 10.1128/JVI.78.2.995-998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Treanor JJ, Schiff GM, Hayden FG, et al. Safety and immunogenicity of a baculovirus-expressed hemagglutinin influenza vaccine: a randomized controlled trial. JAMA. 2007;297(14):1577–1582. doi: 10.1001/jama.297.14.1577. [DOI] [PubMed] [Google Scholar]
- 42.Ohmit SE, Victor JC, Rotthoff JR, et al. Prevention of antigenically drifted influenza by inactivated and live attenuated vaccines. N. Engl. J. Med. 2006;355(24):2513–2522. doi: 10.1056/NEJMoa061850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kieny MP, Costa A, Hombach J, et al. A global pandemic influenza vaccine action plan. Vaccine. 2006;24(40–41):6367–6370. doi: 10.1016/j.vaccine.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 44.Friede M, Palkonyay L, Alfonso C, et al. WHO initiative to increase global and equitable access to influenza vaccine in the event of a pandemic: supporting developing country production capacity through technology transfer. Vaccine. 2011;29(Suppl. 1):A2–A7. doi: 10.1016/j.vaccine.2011.02.079. [DOI] [PubMed] [Google Scholar]
- 45.Perdue ML, Arnold F, Li S, et al. The future of cell culture-based influenza vaccine production. Expert Rev. Vaccines. 2011;10(8):1183–1194. doi: 10.1586/erv.11.82. [DOI] [PubMed] [Google Scholar]
- 46.Grantham R, Gautier C, Gouy M. Codon frequencies in 119 individual genes confirm consistent choices of degenerate bases according to genome type. Nucleic Acids Res. 1980;8(9):1893–1912. doi: 10.1093/nar/8.9.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kanaya S, Yamada Y, Kinouchi M, Kudo Y, Ikemura T. Codon usage and tRNA genes in eukaryotes: correlation of codon usage diversity with translation efficiency and with CG-dinucleotide usage as assessed by multivariate analysis. J. Mol. Evol. 2001;53(4–5):290–298. doi: 10.1007/s002390010219. [DOI] [PubMed] [Google Scholar]
- 48.Knight RD, Freeland SJ, Landweber LF. A simple model based on mutation and selection explains trends in codon and amino-acid usage and GC composition within and across genomes. Genome Biol. 2001;2(4):1–13. doi: 10.1186/gb-2001-2-4-research0010. RESEARCH0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lavner Y, Kotlar D. Codon bias as a factor in regulating expression via translation rate in the human genome. Gene. 2005;345(1):127–138. doi: 10.1016/j.gene.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 50.Codon Usage Database. www.kazusa.or.jp/codon
- 51.Burns CC, Shaw J, Campagnoli R, et al. Modulation of poliovirus replicative fitness in HeLa cells by deoptimization of synonymous codon usage in the capsid region. J. Virol. 2006;80(7):3259–3272. doi: 10.1128/JVI.80.7.3259-3272.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coleman JR, Papamichail D, Skiena S, Futcher B, Wimmer E, Mueller S. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320(5884):1784–1787. doi: 10.1126/science.1155761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Goni N, Iriarte A, Comas V, et al. Pandemic influenza A virus codon usage revisited: biases, adaptation and implications for vaccine strain development. Virol. J. 2012;9:263. doi: 10.1186/1743-422X-9-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mueller S, Papamichail D, Coleman JR, Skiena S, Wimmer E. Reduction of the rate of poliovirus protein synthesis through large-scale codon deoptimization causes attenuation of viral virulence by lowering specific infectivity. J. Virol. 2006;80(19):9687–9696. doi: 10.1128/JVI.00738-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nogales A, Baker SF, Ortiz-Riano E, Dewhurst S, Topham DJ, Martinez Sobrido L. Influenza A virus attenuation by codon deoptimization of the NS gene for vaccine development. J. Virol. 2014;88(18):10525–10540. doi: 10.1128/JVI.01565-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Plotkin JB, Dushoff J. Codon bias and frequency-dependent selection on the hemagglutinin epitopes of influenza A virus. Proc. Natl Acad. Sci. USA. 2003;100(12):7152–7157. doi: 10.1073/pnas.1132114100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mueller S, Coleman JR, Papamichail D, et al. Live attenuated influenza virus vaccines by computer-aided rational design. Nat. Biotechnol. 2010;28(7):723–726. doi: 10.1038/nbt.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barrai I, Scapoli C, Barale R, Volinia S. Oligonucleotide correlations between infector and host genomes hint at evolutionary relationships. Nucleic Acids Res. 1990;18(10):3021–3025. doi: 10.1093/nar/18.10.3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Duret L. Evolution of synonymous codon usage in metazoans. Curr. Opin. Genet. Dev. 2002;12(6):640–649. doi: 10.1016/s0959-437x(02)00353-2. [DOI] [PubMed] [Google Scholar]
- 60.Karlin S, Blaisdell BE, Schachtel GA. Contrasts in codon usage of latent versus productive genes of Epstein-Barr virus: data and hypotheses. J. Virol. 1990;64(9):4264–4273. doi: 10.1128/jvi.64.9.4264-4273.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhou J, Liu WJ, Peng SW, Sun XY, Frazer I. Papillomavirus capsid protein expression level depends on the match between codon usage and tRNA availability. J. Virol. 1999;73(6):4972–4982. doi: 10.1128/jvi.73.6.4972-4982.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bahir I, Fromer M, Prat Y, Linial M. Viral adaptation to host: a proteome-based analysis of codon usage and amino acid preferences. Mol. Syst. Biol. 2009;5:311. doi: 10.1038/msb.2009.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meng J, Lee S, Hotard AL, Moore ML. Refining the balance of attenuation and immunogenicity of respiratory syncytial virus by targeted codon deoptimization of virulence genes. MBio. 2014;5(5):e01704–e01714. doi: 10.1128/mBio.01704-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang C, Skiena S, Futcher B, Mueller S, Wimmer E. Deliberate reduction of hemagglutinin and neuraminidase expression of influenza virus leads to an ultraprotective live vaccine in mice. Proc. Natl Acad. Sci. USA. 2013;110(23):9481–9486. doi: 10.1073/pnas.1307473110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Le Nouen C, Brock LG, Luongo C, et al. Attenuation of human respiratory syncytial virus by genome-scale codon-pair deoptimization. Proc. Natl Acad. Sci. USA. 2014;111(36):13169–13174. doi: 10.1073/pnas.1411290111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hall MN, Gabay J, Debarbouille M, Schwartz M. A role for mRNA secondary structure in the control of translation initiation. Nature. 1982;295(5850):616–618. doi: 10.1038/295616a0. [DOI] [PubMed] [Google Scholar]
- 67.Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hall CB, Weinberg GA, Blumkin AK, et al. Respiratory syncytial virus-associated hospitalizations among children less than 24 months of age. Pediatrics. 2013;132(2):e341–e348. doi: 10.1542/peds.2013-0303. [DOI] [PubMed] [Google Scholar]
- 69.Murakami S, Horimoto T, Ito M, et al. Enhanced growth of influenza vaccine seed viruses in vero cells mediated by broadening the optimal pH range for virus membrane fusion. J. Virol. 2012;86(3):1405–1410. doi: 10.1128/JVI.06009-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Neumann G, Watanabe T, Ito H, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl Acad. Sci. USA. 1999;96(16):9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fodor E, Devenish L, Engelhardt OG, Palese P, Brownlee GG, Garcia Sastre A. Rescue of influenza A virus from recombinant DNA. J. Virol. 1999;73(11):9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Neumann G, Kawaoka Y. Generation of influenza A virus from cloned cDNAs–historical perspective and outlook for the new millenium. Rev. Med. Virol. 2002;12(1):13–30. doi: 10.1002/rmv.332. [DOI] [PubMed] [Google Scholar]
- 73.Hoffmann E, Neumann G, Hobom G, Webster RG, Kawaoka Y. “Ambisense” approach for the generation of influenza A virus: vRNA and mRNA synthesis from one template. Virology. 2000;267(2):310–317. doi: 10.1006/viro.1999.0140. [DOI] [PubMed] [Google Scholar]
- 74.Hussain AI, Cordeiro M, Sevilla E, Liu J. Comparison of egg and high yielding MDCK cell-derived live attenuated influenza virus for commercial production of trivalent influenza vaccine: in vitro cell susceptibility and influenza virus replication kinetics in permissive and semi-permissive cells. Vaccine. 2010;28(22):3848–3855. doi: 10.1016/j.vaccine.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ozawa M, Fujii K, Muramoto Y, et al. Contributions of two nuclear localization signals of influenza A virus nucleoprotein to viral replication. J. Virol. 2007;81(1):30–41. doi: 10.1128/JVI.01434-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Muramoto Y, Takada A, Fujii K, et al. Hierarchy among viral RNA (vRNA) segments in their role in vRNA incorporation into influenza A virions. J. Virol. 2006;80(5):2318–2325. doi: 10.1128/JVI.80.5.2318-2325.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Marsh GA, Hatami R, Palese P. Specific residues of the influenza A virus hemagglutinin viral RNA are important for efficient packaging into budding virions. J. Virol. 2007;81(18):9727–9736. doi: 10.1128/JVI.01144-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fujii Y, Goto H, Watanabe T, Yoshida T, Kawaoka Y. Selective incorporation of influenza virus RNA segments into virions. Proc. Natl Acad. Sci. USA. 2003;100(4):2002–2007. doi: 10.1073/pnas.0437772100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fujii K, Fujii Y, Noda T, et al. Importance of both the coding and the segment-specific noncoding regions of the influenza A virus NS segment for its efficient incorporation into virions. J. Virol. 2005;79(6):3766–3774. doi: 10.1128/JVI.79.6.3766-3774.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ozawa M, Maeda J, Iwatsuki-Horimoto K, et al. Nucleotide sequence requirements at the 5’ end of the influenza A virus M RNA segment for efficient virus replication. J. Virol. 2009;83(7):3384–3388. doi: 10.1128/JVI.02513-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Thangavel RR, Bouvier NM. Animal models for influenza virus pathogenesis, transmission, and immunology. J. Immunol. Methods. 2014;410:60–79. doi: 10.1016/j.jim.2014.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Epstein SL. Control of influenza virus infection by immunity to conserved viral features. Expert Rev. Anti. Infect. Ther. 2003;1(4):627–638. doi: 10.1586/14787210.1.4.627. [DOI] [PubMed] [Google Scholar]
- 83.Influenza Research Database www.fludb.org
- 84.Chua MA, Schmid S, Perez JT, Langlois RA, Tenoever BR. Influenza A virus utilizes suboptimal splicing to coordinate the timing of infection. Cell. Rep. 2013;3(1):23–29. doi: 10.1016/j.celrep.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hutchinson EC, Charles PD, Hester SS, et al. Conserved and host-specific features of influenza virion architecture. Nat. Commun. 2014;5:4816. doi: 10.1038/ncomms5816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Turrell L, Lyall JW, Tiley LS, Fodor E, Vreede FT. The role and assembly mechanism of nucleoprotein in influenza A virus ribonucleoprotein complexes. Nat. Commun. 2013;4:1591. doi: 10.1038/ncomms2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Treanor JJ, Wilkinson BE, Masseoud F, et al. Safety and immunogenicity of a recombinant hemagglutinin vaccine for H5 influenza in humans. Vaccine. 2001;19(13–14):1732–1737. doi: 10.1016/s0264-410x(00)00395-9. [DOI] [PubMed] [Google Scholar]
- 88.Martinez-Sobrido L, Cadagan R, Steel J, et al. Hemagglutinin-pseudotyped green fluorescent protein-expressing influenza viruses for the detection of influenza virus neutralizing antibodies. J. Virol. 2010;84(4):2157–2163. doi: 10.1128/JVI.01433-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nayak DP, Hui EK, Barman S. Assembly and budding of influenza virus. Virus Res. 2004;106(2):147–165. doi: 10.1016/j.virusres.2004.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Krammer F, Palese P, Steel J. Advances in universal influenza virus vaccine design and antibody mediated therapies based on conserved regions of the hemagglutinin. Curr. Top. Microbiol. Immunol. 2015;386:301–321. doi: 10.1007/82_2014_408. [DOI] [PubMed] [Google Scholar]
- 91.Gulati U, Hwang CC, Venkatramani L, et al. Antibody epitopes on the neuraminidase of a recent H3N2 influenza virus (A/Memphis/31/98) J. Virol. 2002;76(23):12274–12280. doi: 10.1128/JVI.76.23.12274-12280.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kochs G, Garcia-Sastre A, Martinez Sobrido L. Multiple anti-interferon actions of the influenza A virus NS1 protein. J. Virol. 2007;81(13):7011–7021. doi: 10.1128/JVI.02581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mibayashi M, Martinez-Sobrido L, Loo YM, Cardenas WB, Gale M, Jr, Garcia Sastre A. Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J. Virol. 2007;81(2):514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Steidle S, Martinez-Sobrido L, Mordstein M, et al. Glycine 184 in nonstructural protein NS1 determines the virulence of influenza A virus strain PR8 without affecting the host interferon response. J. Virol. 2010;84(24):12761–12770. doi: 10.1128/JVI.00701-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Basler CF, Garcia Sastre A. Viruses and the type I interferon antiviral system: induction and evasion. Int. Rev. Immunol. 2002;21(4–5):305–337. doi: 10.1080/08830180213277. [DOI] [PubMed] [Google Scholar]
- 96.Dove BK, Surtees R, Bean TJ, et al. A quantitative proteomic analysis of lung epithelial (A549) cells infected with 2009 pandemic influenza A virus using stable isotope labelling with amino acids in cell culture. Proteomics. 2012;12(9):1431–1436. doi: 10.1002/pmic.201100470. [DOI] [PubMed] [Google Scholar]
- 97.Wong EH, Smith DK, Rabadan R, Peiris M, Poon LL. Codon usage bias and the evolution of influenza A viruses. Codon usage biases of influenza virus. BMC Evol. Biol. 2010;10:253. doi: 10.1186/1471-2148-10-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yoon SW, Webby RJ, Webster RG. Evolution and ecology of influenza A viruses. Curr. Top Microbiol. Immunol. 2014;385:359–375. doi: 10.1007/82_2014_396. [DOI] [PubMed] [Google Scholar]
- 99.Qi X, Jiang D, Wang H, et al. Calculating the burden of disease of avian-origin H7N9 infections in China. BMJ Open. 2014;4(1):e004189. doi: 10.1136/bmjopen-2013-004189. [DOI] [PMC free article] [PubMed] [Google Scholar]