Abstract
To add a further contribution to the literature supporting the relationship between previous head trauma and the development of glioma. We present the first case of pregnancy-related post-traumatic malignant glioma in a 29-year-old female who was admitted because of left sided hemiplegia and epilepsy due to a malignant glial tumor. She had been operated for a right frontal hematoma caused by a motorbike accident 9 years before. Neuroimaging showed a large neoplasia in the right frontal region beneath the material used for cranialplasty, and postoperative pathological revealed a glioblastoma multiforme (GBM) in continuity with the scar resulting from the trauma. While epidemiologic studies may not be conclusive, a pathologic basis has been suggested which show that trauma act as a cocarcinogen in the presence of an initiating carcinogen. Our case fulfilled the widely established criteria for brain tumors of traumatic origin. We believe that in specific cases it is reasonable to acknowledge an etiological association between head trauma and glioma. And additional factors such as pregnancy may promote the manifestation of the clinical symptoms.
Keywords: head injury, glioblastoma multiforme, posttraumatic glioma, pregnancy
Introduction
The relationship between traumatic brain injury and the development of brain tumors has been a topic of controversy since the last century. There is as yet no clear evidence regarding a causative relationship between head injury and brain tumor so far. Here we report another case of glioma that developed in patients during pregnancy with a previous head trauma, which adds further support to the relationship between trauma and glioma.
Case presentation
In 2003, a 20-year-old girl met with a motorbike accident in which she received a moderate head injury. An emergency computed tomography (CT) scan showed a right frontal bone fracture with intracerebral hematoma that caused significant mass effect. Hematoma evacuation and fracture plasty were performed. Further details of the procedure were not available. The postoperative course was entirely uneventful.
In 2012, a 29-year-old G2P1A0 patient (G2P1A0: gravida 2, para 1, abortion 0) was admitted to our hospital at the 16th week of gestation. She complained of a persistent frontal headache associated with left-sided weakness, vomiting and anorexia for 2 weeks. After admission, the patient complained of worsening left-sided weakness and presented of generalized seizure. About 4 h later, after a second fit, the patient was referred to us. An emergency CT scan revealed a large right frontal mass with hyperdense center with perilesional finger-like edema (Fig. 1A). The mass was just under the old operative field extending anteriorly up to the pole, medially up to the falx, and posteriorly up to the ganglionic region. Magnetic resonance imaging (MRI) showed a large mixed necrotic and hemorrhagic lesion in the right frontal region, likely to be high-grade glioma or malignant tumor which had a broad dural base and displaying irregularly circular enhancement (Fig. 1B–D). A multidisciplinary approach is clearly indicated with comprehensive discussion of the risks with patient and their families. The patient and her family declined the option of term pregnancy and opted for termination of pregnancy with a view to postoperative chemoradiotherapy. At surgery, a rich vascular tumor with cystic lesion and necrotic center was found; the tumor was localized precised beneath the material used for cranialplasty (Fig. 1A). Intraoperative frozen section revealed high-grade glioma, and the tumor was subtotal excised. Histological examination disclosed pleomorphic features with multiple atypical mitoses, atypical vascular proliferation, and acellular areas of necrosis were delineated by atypical classic pseudopalisading consistent with the tissue pattern of a glioblastoma multiforme (GBM). Immunohistochemical result: glial fibrillary acidic protein (GFAP) (+), Vim (+), Ki-67 (30%), IDH-1 (+), NF (−) (Fig. 2). After surgery the patient was treated with radiotherapy and chemotherapy.
Fig. 1.
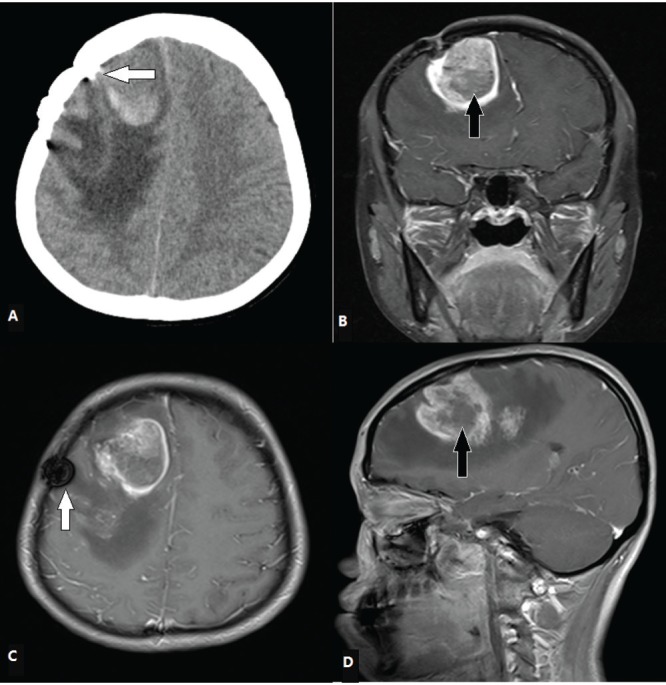
Radiological pictures of the lesion. A: Computed tomography (CT) scan showed a large irregular heterogenous density area in the right frontal lobe under the old operative field and skull fix system (white solid arrow). B–D: Magnetic resonance imaging (MRI) revealed a two-centric large mixed intensity lesion in the right frontal lobe that showed rim-like irregular contrast enhancement with gadolinium at the site of the previous intracerebral hematoma. Hemorrhage and necrosis in lesions were also evident (black arrows).
Fig. 2.
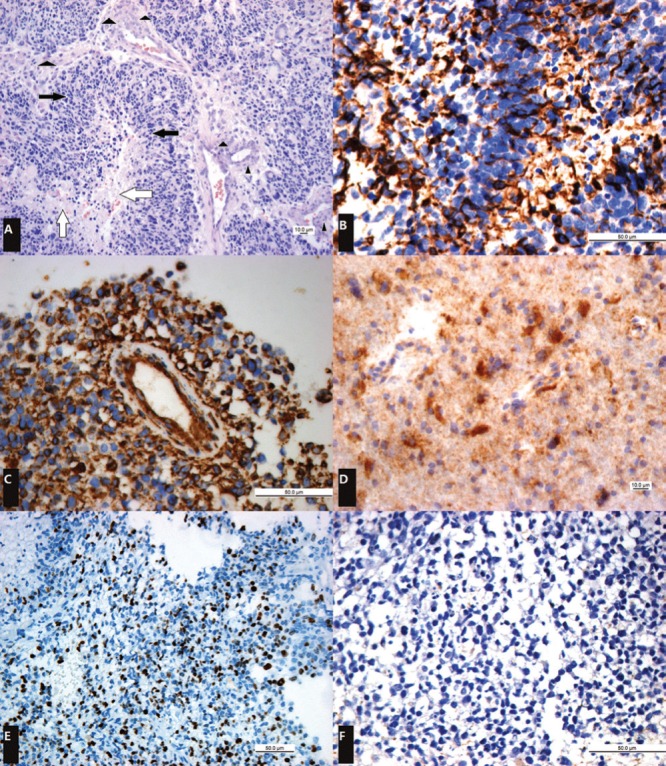
Photomicrographs of the lesion. A: [original magnification, ×200; hematoxylin-eosin stain] demonstrate regions of necrosis (white arrows) surrounded by rings of pseudopalisading tumor cells (black arrows), which are in turn surrounded by abundant microvascular hyperplasia (arrowheads). B: [original magnification, ×400; glial fibrillary acidic protein (GFAP) stain] demonstrate diffuse positivity. C: [original magnification, ×400; Vimentin stain] demonstrate strongly positive expression. D: [original magnification, ×400; IDH-1 stain] showed diffuse positive expression. E: [original magnification, ×200; Ki-67 stain] note a high Ki-67 proliferation index with about 30% of the tumor cells showing nuclear staining. F: [original magnification, ×400; neurofilament (NF) stain] showing negative result.
Discussion
Views on the correlation between head trauma and glioma range from complete acceptance to total rejection. Various approaches such as population studies, animal investigations, and individual case reports have been used in an attempt to answer this question.
1. Trauma as an etiologic factor by means of epidemiology
Regarding prior head injury some case-control studies reported an elevated risk for primary malignant brain tumors.4,9,10) However, these retrospective case control studies may have serious epidemiological drawbacks. Patients with brain tumor may be motivated to recall and report previous head injuries more completely than do controls (“recall bias”).
Most epidemiological studies have failed to show a definite association between head trauma and glioma. Annegers et al.,1) who followed 2,953 survivors of head trauma, did not find any difference between the actual and expected number of brain tumors. A large cohort study of Danish found no excess risk of glioma on average for 8 years following injury except during the first year following injury.11) A multicenter case-control study18) involving 1,509 patients concluded that evidence for elevated brain tumor risk after head trauma is strongest for meningiomas compared to other cerebral neoplasms.
Although epidemiological data do not allow a definite statement on the matter, a few cases of trauma-related gliomas were reported since 1948 (Table 1).
Table 1.
Reported cases of post-traumatic gliomas
| Authors | No. of cases | Histology | Type of trauma | Time interval (years) |
|---|---|---|---|---|
| Hallervorden (1948) | 1 | Oligodendroglioma | Head injury | 38 |
| Diezel (1949) | 1 | Oligodendroglioma | Head injury | 30 |
| Heyck (1954) | 1 | Glioblastoma | Leukotom | 5 |
| Finkemeyer (1956) | 1 | Glioblastoma | Shell injury | 13 |
| 1 | Astrocytoma | — | * | |
| Manuelidis (1971) | 1 | Glioblastoma | Leukotom | 12 |
| Mrowka (1978) | 1 | Glioblastoma | Shell injury | 30 |
| Annegers (1979) | 1 | Astrocytoma | Head injury | 12 |
| Troost et al. (1984) | 1 | Astrocytoma grade III | Shell injury | 40 |
| Perez-Diaz et al. (1985) | 2 | Oligodendroglioma | Contusion | 28 & 7 |
| Janda et al. (1987) | 1 | Mixed pilocytic and fibrillary astrocytoma | Contusion | 20 |
| Di Trapani et al. (1996) | 1 | Mixed glioma | Head injury | * |
| Stendel (1997) | 1 | Glioblastoma multiforme | Shell injury | 48 |
| 1 | Anaplastic oligodendroglioma | After clippiing aneurysm | 10 | |
| Sabel et al. (1999) | 1 | Glioblastoma | Splinter injury | 37 |
| Henry and Rajshekhar (2000)8) | 1 | Astrocytoma grade IV | Contusion | 2 |
| Henderson et al. (2000) | 1 | Anaplastic astrocytoma | Intracerebral hematoma | 19 |
| Magnavita et al. (2003) | 1 | Polytypic glioblastoma | Contusion | 4 |
| Moorthy and Rajshekhar (2004)15) | 1 | Glioblastoma | Contusion | 5 |
| Salvati et al. (2004) | 1 | Glioblastoma | Intracerebral hematoma | 7 |
| 1 | Malignant astrocytoma | Contusion | 5 | |
| 1 | Glioblastoma | Contusive focus | 4 | |
| 1 | Malignant astrocytoma | Intracerebral hematoma | 7 | |
| Anselmi et al. (2006)2) | 1 | Glioblastoma multiforme | Intrathecal hematoma | 20 |
| 1 | Glioblastoma multiforme | Contusion | 15 | |
| Hebert-Blouin (2010) | 1 | Spinal cord anaplastic astrocytoma | Brachial plexus injury | 5 |
| Zhou (2010) | 1 | Glioblastoma multiforme | Intracerebral hematoma | 10 |
| Present | 1 | Glioblastoma multiforme | Intracerebral hematoma | 9 |
not given, data from abstract.
2. Trauma as a risk factor from the point of view of the morphological study
A pathologic basis for development of post-traumatic gliomas has been suggested while controversial data also have been compiled in experimental studies.
Morantz and Shain16) and Schiffer et al.20) have demonstrated that intracerebral trauma may act as a cocarcinogen and enhance the rate of glioma formation in rats exposed to a potent neurocarcinogen. In contrast, Mennel and Zulch14) reported similar studies with the opposite result. However, the two studies are not directly comparable, because in the latter study trauma was applied 12 days after birth as opposed to 30 days in the investigation by Morantz and Shain.16)
Recent study by Hasegawa and Grumet7) indicated that trauma can induce tumorigenesis using implantation of genetically modified cells suggesting that trauma-induced factors caused alterations in the expression of various genes. The case reported by Sabel et al.,19) in which persisting splinters were demonstrated in a glioma 37 years after penetrating injury, is a pointer to it being responsible for an ongoing proliferating stimulus.
The histopathological examination in Table 1 showed heterogenous populations of glioma which provides corroborative evidence for the hypothesis that cells damaged by the initiating carcinogen or predisposing genetic alteration proliferated as a natural result of the trauma, leading to tumor formation.
3. Interactions between pregnancy and glioma
Although interactions with pregnancy remain poorly documented, it has been suggested that pregnancy can have a positive impact on glioma growth.17,21) The acceleration of tumor growth during pregnancy may depend on multiple factors, including hormone,6) growth factor,5) and hemodynamic changes.3) Possibly the enhanced growth rate of gliomas is related to the activation of specific receptors by these hormones especially progesterone which enhances cell growth in human gliomas via progesterone receptor (PR)-B while inhibiting the growth via PR-A.6) Further, secretion of placental growth hormone at the maternal-placental interface stimulates secretion of growth factors.5) The increase in systemic and cerebral blood volume that occurs during pregnancy may increase peritumoral edema and absolute tumor blood volume.
In our case, pregnancy-related tumor edema and tumor growth made the clinical symptom more notable. According to the authors' knowledge, this is the first case reported in the literature concern these two factors in the development of glioma.
4. Criteria for diagnosing post-traumatic glioma
Zulch22) and Manuelidis13) presented criteria for the diagnosis of a traumatic etiology for a brain tumor. The proposed criteria are the following: (1) the patient must have been in good health before suffering the head injury; (2) the injury must be severe enough to cause brain contusion and a secondary reparative process; (3) the location of the impact and the tumor should correspond exactly one to the other; (4) there should be a time interval between trauma and the appearance of the tumor of at least 1 year, a longer latent period increasing the likelihood of a causal relationship; (5) the presence of the tumor must be proved histologically; (6) trauma should consist of an external force; (7) tumor tissue should be in direct continuity with the traumatic scare, not merely in its vicinity or separated by a narrow zone of healthy or slightly altered brain tissue.
Our case seems to fulfill these conditions. The patient lived in good health for 9 years after a traumatic frontal hematoma due to a right bone fracture. If there were a brain malignant tumor at the site and time of the trauma, she would not have been asymptomatic for 9 years. We think that the development of GBM in our patient originated from a cerebral laceration.
Conclusion
The fact that epidemiological studies have not supported a definite connection between head injury and glioma may reflect the fact that the association, if it exists, is not a direct one, which means that there must be an additional agent involved in the etiology of glioma. Experimental data have shown that trauma can act as a cocarcinogen in the presence of an initiating carcinogen. This corresponds to the “Two Hit Theory” of Knudson.12)
We believe that in specific cases (like our case) it is reasonable to acknowledge an etiological association between head trauma and glioma. And additional factors such as pregnancy may be a promotor which enhances the tumor growth and manifests the clinical symptoms. Future studies of head trauma and brain tumor risk should evaluate the role as cocarcinogen of various factors such as hereditary predisposition, hormone, chronic irritation due to the presence of foreign bodies and tissue debris, and granulomatous reaction.
Acknowledgments
The authors thank Mr. Tai-li Li and Mr. Cai-ling Li who helped to perform the immunochemistry and Mrs. Zi-hui Wang (pathologist) who helped in distinguishing the tumor from the merely gliosis and other types of glioma.
References
- 1). Annegers JF, Laws ER, Kurland LT, Grabow JD: Head trauma and subsequent brain tumors. Neurosurgery 4: 203– 206, 1979. [DOI] [PubMed] [Google Scholar]
- 2). Anselmi E, Vallisa D, Bertè R, Vanzo C, Cavanna L: Post-traumatic glioma: report of two cases. Tumori 92: 175– 177, 2006. [DOI] [PubMed] [Google Scholar]
- 3). Blumenthal DT, Parreño MG, Batten J, Chamberlain MC: Management of malignant gliomas during pregnancy: a case series. Cancer 113: 3349– 3354, 2008. [DOI] [PubMed] [Google Scholar]
- 4). Bunin GR, Buckley JD, Boesel CP, Rorke LB, Meadows AT: Risk factors for astrocytic glioma and primitive neuroectodermal tumor of the brain in young children: a report from the Children's Cancer Group. Cancer Epidemiol Biomarkers Prev 3: 197– 204, 1994. [PubMed] [Google Scholar]
- 5). Fuglsang J, Ovesen P: Aspects of placental growth hormone physiology. Growth Horm IGF Res 16: 67– 85, 2006. [DOI] [PubMed] [Google Scholar]
- 6). González-Agüero G, Gutiérrez AA, González-Espinosa D, Solano JD, Morales R, González-Arenas A, Cabrera-Muñoz E, Camacho-Arroyo I: Progesterone effects on cell growth of U373 and D54 human astrocytoma cell lines. Endocrine 32: 129– 135, 2007. [DOI] [PubMed] [Google Scholar]
- 7). Hasegawa K, Grumet M: Trauma-induced tumorigenesis of cells implanted into the rat spinal cord. J Neurosurg 98: 1065– 1071, 2003. [DOI] [PubMed] [Google Scholar]
- 8). Henry PT, Rajshekhar V: Post-traumatic malignant glioma: case report and review of the literature. Br J Neurosurg 14: 64– 67, 2000. [DOI] [PubMed] [Google Scholar]
- 9). Hochberg F, Toniolo P, Cole P: Head trauma and seizures as risk factors of glioblastoma. Neurology 34: 1511– 1514, 1984. [DOI] [PubMed] [Google Scholar]
- 10). Hu J, Johnson KC, Mao Y, Guo L, Zhao X, Jia X, Bi D, Huang G, Liu R: Risk factors for glioma in adults: a case-control study in northeast China. Cancer Detect Prev 22: 100– 108, 1998. [DOI] [PubMed] [Google Scholar]
- 11). Inskip PD, Mellemkjaer L, Gridley G, Olsen JH: Incidence of intracranial tumors following hospitalization for head injuries (Denmark). Cancer Causes Control 9: 109– 116, 1998. [DOI] [PubMed] [Google Scholar]
- 12). Knudson AG: Mutation and cancer: statistical study of retino-blastoma. Proc Natl Acad Sci USA 68: 820– 823, 1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Manuelidis EH: Glioma in trauma, in Minckler J. (ed): Pathology of the Nervous System, New York, McGraw-Hill, 1972, Vol 2, 2237– 2240, and Vol 3, p 291 [Google Scholar]
- 14). Mennell HD, Zülch KJ: [Morphology of transplacentally induced neurogenic tumors in Syrian hamsters]. Acta Neuropathol 21: 194– 203, 1972. (German) [DOI] [PubMed] [Google Scholar]
- 15). Moorthy RK, Rajshekhar V: Development of glioblastoma multiforme following traumatic cerebral contusion: case report and review of literature. Surg Neurol 61: 180– 184; discussion 184, 2004. [DOI] [PubMed] [Google Scholar]
- 16). Morantz RA, Shain W: Trauma and brain tumors: an experimental study. Neurosurgery 3: 181– 186, 1978. [DOI] [PubMed] [Google Scholar]
- 17). Pallud J, Mandonnet E, Deroulers C, Fontaine D, Badoual M, Capelle L, Guillet-May F, Page P, Peruzzi P, Jouanneau E, Frenay M, Cartalat-Carel S, Duffau H, Taillandier L, Club de Neuro-Oncologie de la Société Française de Neurochirurgie (SFNC) Association des Neuro-Oncologues d'Expression Française (ANOCEF) : Pregnancy increases the growth rates of World Health Organization grade II gliomas. Ann Neurol 67: 398– 404, 2010. [DOI] [PubMed] [Google Scholar]
- 18). Preston-Martin S, Pogoda JM, Schlehofer B, Blettner M, Howe GR, Ryan P, Menegoz F, Giles GG, Rodvall Y, Choi NW, Little J, Arslan A: An international case-control study of adult glioma and meningioma: the role of head trauma. Int J Epidemiol 27: 579– 586, 1998. [DOI] [PubMed] [Google Scholar]
- 19). Sabel M, Felsberg J, Messing-Jünger M, Neuen-Jacob E, Piek J: Glioblastoma multiforme at the site of metal splinter injury: a coincidence? Case report. J Neurosurg 91: 1041– 1044, 1999. [DOI] [PubMed] [Google Scholar]
- 20). Schiffer D, Giordana MT, Vigliani MC, Cavalla P: Relationship between glial reaction to a stab wound and tumor development after receiving transplacental ethylnitrosourea in the rat. Acta Neuropathol 83: 30– 38, 1991. [DOI] [PubMed] [Google Scholar]
- 21). Tewari KS, Cappuccini F, Asrat T, Flamm BL, Carpenter SE, Disaia PJ, Quilligan EJ: Obstetric emergencies precipitated by malignant brain tumors. Am J Obstet Gynecol 182: 1215– 1221, 2000. [DOI] [PubMed] [Google Scholar]
- 22). Zulch KJ: Brain Tumors: Their Biology and Pathology, ed 2 New York, Springer-Verlag, 1965, pp 51– 58 [Google Scholar]


