Abstract
The Merci retrieval system is a useful modality for the recanalization of acute cerebral artery occlusion. However, it remains unclear whether the tortuosity of the middle cerebral artery (MCA) plays a role in successful recanalization. In this study, we investigated the association between the shape of the horizontal MCA segment (M1) and successful recanalization using the Merci retrieval system with or without adjunctive treatments. Twenty-three patients with M1 occlusion underwent thrombectomy using the Merci retrieval system with or without adjunctive treatments between July 2010 and July 2012. The anteroposterior view of final angiograms was used to measure the M1 curve angles. M1 with a curve angle measuring < 100° was defined as arch-type M1, whereas that with a curve angle measuring ≥ 100° was defined as straight-type M1. Angiographic findings were evaluated on the basis of the thrombolysis in cerebral infarction grade; grade 2B or 3 corresponds to successful recanalization. Eight patients had arch-type M1 and 15 patients had straight-type M1. Successful recanalization was achieved in 2 patients (25%) with arch-type M1 and 12 patients (80%) with straight-type M1 (p = 0.023). The mean M1 curve angle was significantly greater in the 14 patients in whom successful recanalization was achieved than in the 9 patients in whom it was not achieved (129 ± 21° vs. 93 ± 29°, p = 0.002). Arch-type M1 was an independent predictive factor of unsuccessful recanalization (odds ratio, 0.045; 95% confidence interval, 0.03–0.696). A tortuous M1 was associated with unsuccessful recanalization by the Merci retrieval system, even when adjunctive treatments were used.
Keywords: Merci retrieval system, middle cerebral artery, recanalization
Introduction
The Merci retrieval system has been established as a useful modality for the recanalization of acute cerebral artery occlusions,1–4) and successful recanalization is the most important factor influencing a good postoperative clinical course.5) Although a previous study demonstrated that systolic blood pressure (SBP)5) and M2 occlusion5,6) were independent predictors of revascularization using the Merci retrieval system, it remains unclear whether the tortuosity of the middle cerebral artery (MCA) influences the success of recanalization. In this study, we investigated the association between the shape of the horizontal MCA segment (M1) and successful recanalization using the Merci retrieval system with or without adjunctive treatments.
Materials and Methods
Sixty-five consecutive patients underwent endovascular treatment for acute ischemic stroke with large artery occlusion at the Stroke Center of Kobe City Medical Center General Hospital (Kobe) between July 2010 and July 2012. Of these 65 patients, 23 who were treated for M1 occlusion using the Merci retrieval system (Concentric Medical Inc., Mountain View, California, USA) with or without adjunctive treatments were included in this study.
All patients were examined by magnetic resonance imaging (MRI) before endovascular treatment. Diffusion-weighted imaging (DWI) using a 1.5-T scanner with single-shot echoplanar imaging (b = 1000 s/mm2, 5-mm slices) was performed and the Alberta Stroke Program Early Computed Tomography Score (0–10 points) was evaluated.7) Angiography was performed before treatment, and patients were divided into two groups on the basis of the location of the M1 occlusion, i.e., proximal and distal.
Thrombolysis in cerebral infarction (TICI) grades8) were used to evaluate the angiographic findings obtained after treatment using the Merci retrieval system and after all the adjunctive endovascular treatments. Grades 2B or 3 corresponded to successful recanalization. Vessel injury such as dissection was also evaluated.
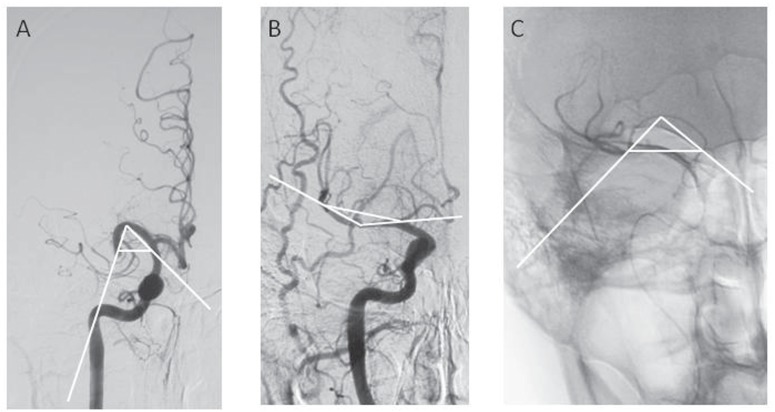
M1 curve angles were measured on the anteroposterior view of final angiograms. When M1 was curved in the cranial direction, the M1 curve angle was measured as the angle formed by its endpoint, vertex, and the internal carotid artery (ICA) at the level of the M1 endpoint (Fig. 1A). When M1 was curved in the caudal direction, the M1 curve angle was measured as the angle formed by the endpoint, bottom, and origin of M1 (Fig. 1B). When the distal portion of M1 was not recanalized, the microcatheter tracts created during treatment were employed to evaluate the endpoint and vertex or bottom portions of M1 (Fig. 1C). M1 with a curve angle of < 100° was defined as arch-type M1, while that with a curve angle ≥ 100° was defined as straight-type M1.
Fig. 1.
Analysis of the curve angle of the horizontal MCA segment (M1). A: M1 is curved in the cranial direction in Case 2. The M1 curve angle is measured as the angle formed by its endpoint, vertex, and internal carotid artery at the level of the M1 endpoint. B: M1 is curved in the caudal direction in Case 5. The M1 curve angle is measured as the angle formed by the endpoint, bottom, and origin of M1. C: The microcatheter tract created during treatment is employed to evaluate the endpoint and vertex portion of M1 because the distal portion of M1 is not recanalized in Case 3.
All patients were examined by computed tomography (CT) within an hour of endovascular treatment. The development of intracranial hemorrhage, including subarachnoid hemorrhage (SAH), hemorrhagic infarction (HI), and/or parenchymal hematoma (PH), was evaluated.9) If the clinical deterioration score on the National Institutes of Health Stroke Scale increased by > 4 after treatment in patients with intracranial hemorrhage, the intracranial hemorrhage was defined as symptomatic.10)
Statistical analysis
Fisher's exact test and Student's t-test were used to statistically analyze categorical variables and continuous variables, respectively. Subsequently, all covariates with a p value of < 0.2 were entered into a multi-variate logistic regression model. A p value of < 0.05 was considered to indicate statistical significance. Statistical Package for the Social Sciences (SPSS) for Windows version 11.0 (SPSS, Inc., Chicago, Illinois, USA) was used to perform all statistical analyses.
Results
Of the 102 consecutive patients who underwent endovascular treatment for acute ischemic stroke with large artery occlusion, 23 patients with M1 occlusion (16 men, 7 women; mean age, 68 years; range, 40–84 years) underwent treatment using the Merci retrieval system. Table 1 shows the clinical features and treatments of these 23 patients. Eighteen patients were ineligible for intravenous tissue-type plasminogen activator (iv-tPA) treatment, and prompt recanalization failed in 5 patients after treatment with iv-tPA. Sixteen patients received adjunctive treatment, including percutaneous transluminal angioplasty (n = 11), intra-arterial urokinase (n = 2), intracranial stent placement (n = 2), carotid artery stenting (n = 2), and Penumbra system treatment (n = 2). Five patients developed M1 occlusion after recanalization of ICA occlusion during endovascular treatment.
Table 1.
Clinical features and treatments
| Case | Age (y.o.) | Sex | Onset-Needle (hr) | NIHSS | DWI-ASPECTS | Occlusion site | Merci size/type | iv-tPA | Adjnctive treatments |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 66 | M | 10.0 | 19 | 8 | M1 d | 2.0F | Ineligible | Extracranial stent |
| 2 | 54 | M | 2.3 | 30 | 4 | M1 p | 2.0F | Ineligible | None |
| 3 | 52 | M | 3.5 | 18 | 6 | M1 p | 2.0F | Failed | PTA |
| 4 | 78 | M | 37.5 | 22 | 5 | M1 p | 2.0F | Ineligible | PTA |
| 5 | 64 | M | 7.7 | 10 | 8 | M1 p | 2.0F | Failed | None |
| 6 | 40 | M | 16.3 | 12 | 8 | M1 p | 2.5S | Ineligible | PTA, intracranial stent |
| 7 | 76 | M | 3.0 | 18 | 6 | M1 p | 2.5F, 2.0F, 2.5F | Ineligible | None |
| 8 | 82 | F | 16.0 | 23 | 6 | M1 d | 2.0F | Ineligible | ia-UK |
| 9 | 81 | M | 2.0 | 29 | 9 | M1 d | 2.0F, 2.5S | Ineligible | PTA |
| 10 | 67 | M | 2.8 | 10 | 9 | M1 p | 2.5S, 2,0F | Ineligible | PTA |
| 11 | 67 | M | 5.8 | 7 | 7 | M1 d | 2.5F | Failed | PTA |
| 12 | 68 | F | 4.2 | 12 | 8 | M1 d | 2.0F | Ineligible | PTA |
| 13 | 48 | F | 2.9 | 22 | 4 | M1 p | 2.5S | Ineligible | ia-UK |
| 14 | 59 | M | 11.7 | 26 | 4 | M1 p | 2.5S | Ineligible | PTA |
| 15 | 84 | M | 3.8 | 16 | 6 | M1 p | 2.0S, 2.0F | Failed | PTA |
| 16 | 73 | M | 2.9 | 34 | 4 | M1 p | 2.0S, 2.5S | Ineligible | PTA |
| 17 | 74 | M | 3.7 | 20 | 5 | M1 p | 2.0F, 2.5F, 2.0F | Failed | extracranial stent |
| 18 | 60 | M | 11.1 | 23 | 4 | M1 p | 2.0F, 2.0S | Ineligible | None |
| 19 | 59 | F | 2.7 | 26 | 5 | M1 p | 2.0S, 2.5F | Ineligible | None |
| 20 | 81 | M | 4.3 | 18 | 7 | M1 d | 2.0S, 2.0F | Failed | None |
| 21 | 83 | F | 10.7 | 19 | 5 | M1 p | 2.0S, 2.0F | Ineligible | Penumbra, PTA, intracranial stent |
| 22 | 82 | F | 11.3 | 10 | 6 | M1 d | 2.0S, 2.0F | Ineligible | None |
| 23 | 72 | F | 10.3 | 23 | 6 | M1 d | 2.0S, 2.0F | Ineligible | Penumbra |
If onset-time was unknown, the onset-time was defined as the time at which the patient was last known to be without any neurological deficit. ASPECTS: Alberta Stroke Program Early Computed Tomography, DWI: diffusion-weighted imaging, hr: hour, ia-UK: intra-arterial urokinase, M1 d: M1 distal, M1 p: M1 proximal, NIHSS: National Institutes of Health Stroke Scale, PTA: percutaneous transluminal angioplasty, y.o.: years old.
Of the 23 patients with M1 occlusion, 15 (65%) had straight-type M1 while 8 (35%) had arch-type M1. Successful recanalization using the Merci retrieval system alone was achieved in 6 patients with straight-type M1 and in none with arch-type M1 (40% vs. 0%, p = 0.058, Table 2). However, successful recanalization was achieved in 12 patients with straight-type M1 and 2 with arch-type M1 (80% vs. 20%, p = 0.023, Table 2) when adjunctive treatments were used in addition to the Merci retrieval system. There were no significant differences in the incidence of dissection, SAH, HI/PH, and any intracranial hemorrhage between the 2 groups (Table 2). All intracranial hemorrhages were asymptomatic.
Table 2.
M1 shapes and recanalization/complication
| M1 shapes |
p | ||
|---|---|---|---|
| Straight-type (n = 15) | Arch-type (n = 8) | ||
| TICI 2B/3 after Merci | 6 (40%) | 0 (0%) | 0.058 |
| TICI 2B/3 after all procedures | 12 (80%) | 2 (25%) | 0.023 |
| Dissection | 1 (6.6%) | 0 (0%) | 1.000 |
| SAH | 4 (27%) | 3 (38%) | 0.657 |
| HI/PH | 8 (53%) | 3 (38%) | 0.667 |
| Any intracranial hemorrhage | 10 (67%) | 4 (50%) | 0.657 |
Fisher's exact test. HI: hemorrhagic infarction, PH: parenchymal hematoma, SAH: subarachnoid hemorrhage, TICI: thrombolysis in cerebral infarction.
Univariate analysis showed that the M1 curve angle was significantly greater in patients who exhibited successful recanalization after all endovascular treatments than in those who did not (129° ± 21° vs. 93° ± 29°, p = 0.002, Table 3). Multivariate analysis for arch-type M1, age, and SBP, which had p values of < 0.2 in univariate analysis, showed that arch-type M1 was an independent predictive factor for unsuccessful recanalization (odds ratio, 0.045; 95% confidence interval, 0.03–0.696, Table 4).
Table 3.
Univariate analysis for successful recanalization
| Successful recanalization |
p | ||
|---|---|---|---|
| Yes (n = 14) | No (n = 9) | ||
| Age (y.o.) | 66 ± 13 | 72 ± 11 | 0.198 |
| Onset-needle (hr) | 7.3 ± 5.1 | 9.3 ± 11 | 0.566 |
| SBP (mmHg) | 159 ± 31 | 138 ± 29 | 0.124 |
| DBP (mmHg) | 83 ± 16 | 83 ± 27 | 0.916 |
| NIHSS | 20 ± 6.7 | 19 ± 8.1 | 0.730 |
| DWI-ASPECTS ≥ 7 | 6 (43%) | 2 (22%) | 0.400 |
| M1 proximal occlusion | 9 (64%) | 6 (67%) | 1.000 |
| M1 curve-angle (degrees) | 129 ± 21 | 93 ± 29 | 0.002 |
Student's t test/Fisher's exact test. ASPECTS: Alberta Stroke Program Early Computed Tomography, DBP: diastolic blood pressure, DWI: diffusion-weighted imaging, hr: hour, NIHSS: National Institutes of Health Stroke Scale, SBP: systolic blood pressure, y.o.: years old.
Table 4.
Multivariate analysis for successful recanalization
| OR (95% CI) | p | |
|---|---|---|
| Age (/1y) | 0.924 (0.819–1.042) | 0.198 |
| SBP (/1 mmHg) | 1.032 (0.991–1.075) | 0.129 |
| Arch-type M1 | 0.045 (0.030–0.696) | 0.027 |
CI: confidence interval, OR: odds ratio, SBP: systolic blood pressure, y: year.
Discussion
To the best of our knowledge, this is the first study to directly demonstrate that an elongated tortuous M1 can be associated with unsuccessful recanalization. However, we could not elucidate whether or not M1 shape was related to the development of hemorrhagic complications after endovascular therapy.
In a large population study, Nogueira et al. reported that low SBP and M2 occlusion were independent predictors of revascularization.5) In addition, Shi et al. reported that higher revascularization rates were achieved in cases of M2 occlusion than in cases of M1 occlusion.6) However, associations between the shape of MCA and successful recanalization were not investigated.
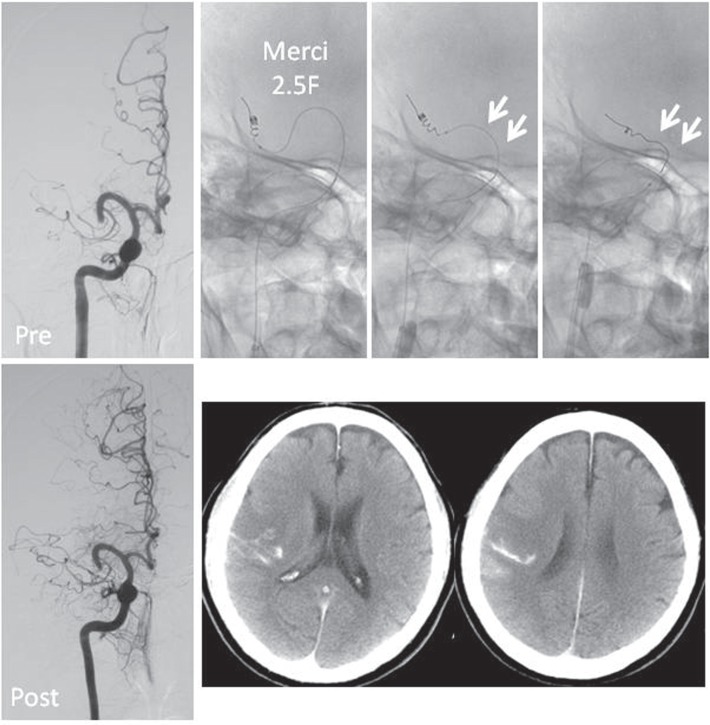
On the other hand, Zhu et al. reported that a curved M1 detected on T2*-weighted gradient-echo MRI decreased the technical success of Merci thrombectomy and suggested that mechanical force applied during retriever pullback would be dispersed radially in a tortuous M1, whereas mechanical forces could be exerted on the target thrombus with less impedance in a straight M1.11) When the Merci retriever is delivered and withdrawn, M1 is pulled down entirely. Vertical tension is exerted on the microcatheter if M1 is severely elongated. Subsequently, a thrombus tends to evade capture because the retriever loops are stretched. In Case 13 with arch-type M1, recanalization was not achieved, and CT performed after the procedures showed the development of SAH (Fig. 2).
Fig. 2.
Right-sided occlusion in an arch-type horizontal middle cerebral artery (MCA) segment (M1; Case 11). When the Merci retriever is withdrawn, M1 is entirely pulled down and vertical pressure is applied to the microcatheter (white arrows). Subsequently, the retriever loops are stretched. In this case, recanalization was not achieved, and computed tomography performed after the procedures showed the development of subarachnoid hemorrhage.
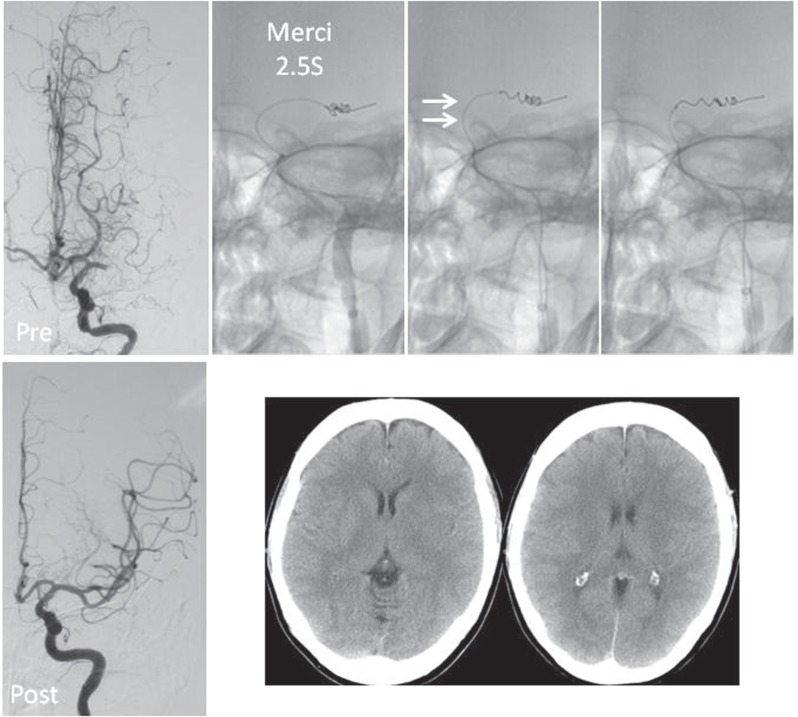
In contrast, straight M1 segments are not vertically pulled down to the same extent as curved M1 segments, even when horizontal tension is applied to the microcatheter in the terminal portion of ICA. Successful recanalization was achieved in Case 15 who had a straight-type M1 (TICI grade 3), with no complication of intracranial hemorrhage (Fig. 3).
Fig. 3.
Left-sidedocclusion in a straight-type horizontal middle cerebral artery (MCA) segment (M1; Case 13). When the Merci retriever is withdrawn, the entire M1 segment is not pulled down vertically, although horizontal pressure is applied to the microcatheter in the terminal portion of the internal carotid artery (white arrows). In this case, successful recanalization (thrombolysis in cerebral infarction grade 3) was achieved, and computed tomography performed after the procedures demonstrated no intracranial hemorrhage.
In Case 13, the Outreach Distal Access Catheter (DAC; Concentric Medical Inc., Mountain View, California, USA),12) which was designed to provide distal access, support, and stability in tortuous anatomy during treatment with the Merci system, may have been useful. However, we could not use DAC because it has not been approved in Japan. In addition, we could not use the Penumbra system (Penumbra Inc., Alameda, California, USA)13) until July 2011 for the same reason.
In our study, the rate of successful recanalization using the Merci retrieval system was higher in patients with straight-type M1 than in those with arch-type M1, but the difference was not significant (p = 0.058). However, the rate of successful recanalization using adjunctive treatments after the use of the Merci retrieval system was significantly higher in patients with straight-type M1 than in those with arch-type M1 (Table 2). Univariate analysis showed that the M1 curve angle was the most significant factor associated with final successful recanalization (Table 3), while multivariate analysis showed that arch-type M1 was a predictor of final unsuccessful recanalization. The association between an elongated M1 and unsuccessful recanalization may not solely reflect the efficacy of the Merci retriever system itself, because 16 patients (70%) underwent other adjunctive treatments in our study. The results of this study may not have been device specific because poor results were obtained for patients with elongated tortuous MCAs even when adjunctive treatments were used. Although a recent study showed the superiority of stent-retriever systems such as the Solitaire (ev3 Inc., Irvine, California, USA)14) and the Trevo (Concentric Medical Inc.)15) over the Merci retrieval system, the usefulness of these systems in cases of elongated tortuous arteries should be explored.
We also investigated association between M1 shape and development of hemorrhagic complications after endovascular procedures. However, the incidence of all types of hemorrhagic complications was not significantly different between patients with arch-type and straight-type M1 (Table 2). In addition, we evaluated the association between Merci sizes/types and complications such as vessel dissections, SAH, HI/PH, and any intracranial hemorrhage; however, there was no correlation.
This study had several limitations. First, it was performed in a very small population. Second, we measured the M1 curve angle angiographically from the anteroposterior view of final angiograms to evaluate M1 elongation, but this angle varied depending on the radiographic exposure angle. Three-dimensional imaging is required for precise evaluation of the M1 curve angle. Third, although ICA elongation may also be associated with unsuccessful recanalization, this factor was not evaluated in the present study. Finally, the variable selection of Merci sizes and types in this series may make it difficult to conclude that straight-type M1 is easier to treat than arch-type M1.
In conclusion, the results of this study suggest that a tortuous M1 may be associated with unsuccessful recanalization using the Merci retrieval system, even when and adjunctive treatments are used, although this finding should be confirmed in a larger population.
Acknowledgments
The auhtors thank the staff of the Department of Radiology, Kobe City Medical Center General Hospital for their technical support in performing cerebral angiography and endovascular treatments.
References
- 1). Gobin YP, Starkman S, Duckwiler GR, Grobelny T, Kidwell CS, Jahan R, Pile-Spellman J, Segal A, Vinuela F, Saver JL: MERCI 1: a phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke 35: 2848– 2854, 2004. [DOI] [PubMed] [Google Scholar]
- 2). Smith WS: Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I. AJNR Am J Neuroradiol 27: 1177– 1182, 2006. [PMC free article] [PubMed] [Google Scholar]
- 3). Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, Lutsep HL, Rymer MM, Higashida RT, Starkman S, Gobin YP, Multi MERCI Investigators. Frei D, Grobelny T, Hellinger F, Huddle D, Kidwell C, Koroshetz W, Marks M, Nesbit G, Silverman IE: Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke 39: 1205– 1212, 2008. [DOI] [PubMed] [Google Scholar]
- 4). Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, Lutsep HL, Nesbit GM, Grobelny T, Rymer MM, Silverman IE, Higashida RT, Budzik RF, Marks MP, MERCI Trial Investigators : Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 36: 1432– 1438, 2005. [DOI] [PubMed] [Google Scholar]
- 5). Nogueira RG, Liebeskind DS, Sung G, Duckwiler G, Smith WS, MERCI, Multi MERCI Writing Committee : Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI Trials. Stroke 40: 3777– 3783, 2009. [DOI] [PubMed] [Google Scholar]
- 6). Shi ZS, Loh Y, Walker G, Duckwiler GR, MERCI and Multi-MERCI Investigators : Clinical outcomes in middle cerebral artery trunk occlusions versus secondary division occlusions after mechanical thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI trials. Stroke 41: 953– 960, 2010. [DOI] [PubMed] [Google Scholar]
- 7). Singer OC, Kurre W, Humpich MC, Lorenz MW, Kastrup A, Liebeskind DS, Thomalla G, Fiehler J, Berkefeld J, Neumann-Haefelin T, MR Stroke Study Group Investigators : risk assessment of symptomatic intracerebral hemorrhage after thrombolysis using DWI-ASPECTS. Stroke 40: 2743– 2748, 2009. [DOI] [PubMed] [Google Scholar]
- 8). Tomsick T, Broderick J, Carrozella J, Khatri P, Hill M, Palesch Y, Khoury J, Interventional Management of Stroke II Investigators : Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol 29: 582– 587, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, Ringleb AP, Lorenzano S, Manelfe C, Bozzao L: Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke 30: 2280– 2284, 1999. [DOI] [PubMed] [Google Scholar]
- 10). Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, ECASS Investigators : Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359: 1317– 1329, 2008. [DOI] [PubMed] [Google Scholar]
- 11). Zhu L, Liebeskind DS, Jahan R, Starkman S, Salamon N, Duckwiler G, Vinuela F, Tateshima S, Gonzalez N, Villablanca P, Ali LK, Kim D, Ovbiagele B, Froehler M, Tenser M, Saver JL: Thrombus branching and vessel curvature are important determinants of middle cerebral artery trunk recanalization with Merci thrombectomy devices. Stroke 43: 787– 792, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Spiotta AM, Hussain MS, Sivapatham T, Bain M, Gupta R, Moskowitz SI, Hui FK: The versatile distal access catheter: the Cleveland Clinic experience. Neurosurgery 68: 1677– 1686; discussion 1686, 2011. [DOI] [PubMed] [Google Scholar]
- 13). Penumbra Pivotal Stroke Trial Investigators : The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 40: 2761– 2768, 2009. [DOI] [PubMed] [Google Scholar]
- 14). Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO, SWIFT Trialists Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 380: 1241– 1249, 2012. [DOI] [PubMed] [Google Scholar]
- 15). Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, Liebeskind DS, Smith WS, TREVO 2 Trialists : Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 380: 1231– 1240, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]