Abstract
The stability of screw constructs is of considerable importance in determining the outcome, especially in spinal osteoporosis. Polymethylmethacrylate (PMMA) has been proven as an effective material for increasing the pullout strength of pedicle screws inserted into the osteoporotic bones. However, PMMA has several disadvantages, such as its exothermic properties, the risk of neural injury in the event of extravasation, and difficulties in performing revision surgery. In the current study, we used hydroxyapatite (HA) cement for screw augmentation in spinal osteoporosis. We conclude that HA cement is a useful tool for screw augmentation and recommend it as a promising option for spinal instrumentation in osteoporotic patients.
Keywords: pedicle screw, osteoporosis, screw augmentation, hydroxyapatite, fusion
Introduction
Over the last decade, internal stabilization using a pedicle screw system has been used as the gold standard for the treatment of an unstable spine. This method has three main advantages over other internal spinal fixation constructs: the ability to (1) provide 3-column fixation, (2) facilitate the instrumentation of short segments, and (3) maintain anatomic or desired sagittal alignment.9) Rigid internal fixation reflects the strength of the screw attachment to the spine, which is directly related to the quality of bone into which the pedicle screw is placed. The stability of the instrumentation is also of considerable importance in determining the outcomes.
In industrial countries, the increase in the number of elderly population is a well-known problem for the society and health services. Advanced countries have been officially labeled as “aging societies,” which means that the elderly constitute 7% or more of the country's total population. Consequently, many types of spine operations are performed in elderly people who have osteopenia or osteoporosis. Attaining a rigid internal fixation can be extremely difficult in these cases and may sometimes be precluded. The augmentation of pedicle screw fixation with various materials has been studied.3,4,6,7,9,13) Among these materials, polymethylmethacrylate (PMMA) augmentation is a widely accepted and efficient method to enhance screw strength in osteoporotic bones.3,4) However, there are concerns over the exothermic properties of PMMA and the risk of neural injury in the event of extravasation. In addition, PMMA is non-degradable and may hamper revision surgery.12) Therefore, the use of bioabsorbable bone cements, such as hydroxyapatite (HA), has been suggested because these compounds are not exothermic during polymerization and are safe in the event of extravasation. However, the clinical use of HA cement as a screw augmentation technique in spinal surgery has not been proven. In the current study, we determined the efficacy of HA cement for screw augmentation in osteoporotic patients.
Materials and Methods
This study was designed as a retrospective, cohort study. Thirty-four patients treated from March 2002 to December 2005 were included in the study. Patients were divided into two groups: a screw augmentation group (Group A) and a control group (Group B). Patients from both groups had been diagnosed with spondylolisthesis grade I or II at L4–5 and concomitant osteoporosis. The demographic data of each group are summarized in Table 1. Osteoporosis was diagnosed through the assessment of dual-energy X-ray absorptiometry (DEXA) scans of the femur and lumbar spine. Osteoporosis was defined as a loss of trabecular bone with an average bone mineral density (BMD) at the lumbar levels of less than 0.8 g/cm2 or a T-score of −2.5 or less.1) The treatment method used for spondylolisthesis was transforaminal lumbar interbody fusion (TLIF) with the polyethyetherketone (PEEK) cages. In Group A, additional screw augmentation was performed with HA cement. In Group B, conventional TLIF was carried out. All operations were performed by one surgeon (H.Y.L.). After lumbar interbody fusion, the entry point of the pedicle screw was prepared with a 4 mm burr. The screw path was created using a gear shift. The absence of pedicle violation was confirmed with a ball tip probe. In Group A, 2 mL BoneSource® (Stryker Howmedica Osteonics, Mississippi, Kalamazoo, USA) HA cement was inserted through a poverty needle (Kyeongwon Medical, Seoul, South Korea) which has an outer diameter of 3 mm and an inner diameter of 2.2 mm. HA cement consisted of a liquid to powder ratio of 5 cc to 10 g. Proper space for HA cement was made by withdrawing a poverty needle by 1 cm. After hardening of the HA cement, a 6.5 mm diameter by 45 ± 5 mm long Diapason® (Stryker Osteonics, Allendale, New Jersey, USA) screw was inserted at each level. Standing lateral radiographs were taken at postoperative day 1 and during every follow-up visit (1 month, 3 months, 6 months, and annually). The following are the radiologic parameters assessed during the procedure (Fig. 1):
Segmental lordosis (SL): the angle between the superior endplate of L4 and the inferior endplate of L5.
Disc height (DH): the distance between the inferior endplate of L4 and the superior endplate of L5.
Screw angle (SA): the mean angle between the mid-axial line of the bilateral L4 and L5 screws.
L4 screw angle (4A): the angle between the L4 screw and the inferior endplate of L4.
L5 screw angle (5A): the angle between the L5 screw and the inferior endplate of L5.
Table 1.
Demographic data of patients in Group A and Group B
| Group A | Group B | |
|---|---|---|
| Age | 67.6 ± 5.0 | 68.2 ± 5.1 |
| Gender (M:F) | 1:16 | 2:15 |
| BMD (T score) | –3.5 ± 0.6 | –3.3 ± 0.7 |
| Meyerding G I:II | 15:2 | 16:1 |
| Operation | L4–5 | L4–5 |
F: female, M: male.
Fig. 1.
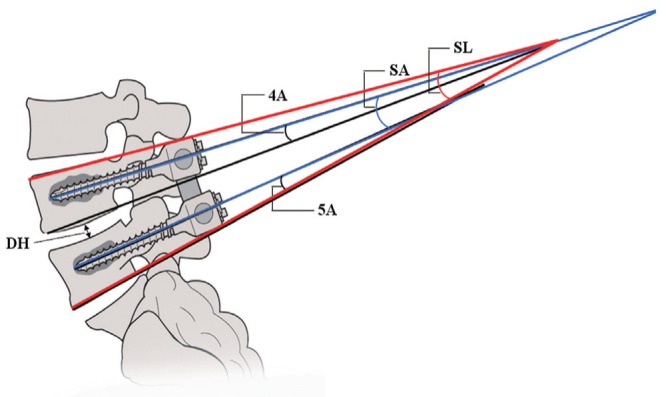
Radiologic parameters measured included segmental lordosis (SL), disc height (DH), screw angle (SA), L4 screw angle (4A), and L5 screw angle (5A).
All radiologic data were digitized and analyzed using a custom software (Piview; Infinitt Co., Seoul, Korea). They were measured by a single observer (S.H.J.) who was not involved in patient selection, surgery, or follow-up. Radiologic parameters were compared between postoperative day 1 and the 3-month follow-up, and between postoperative day 1 and the 2-year follow-up in each group. Clinical outcome was assessed according to the visual analog scale (VAS) at 3-month follow-up. All data were analyzed using the Statistical Package for the Social Sciences software version 17.0K (SPSS, Inc., Chicago, Illinois, USA). Clinical and radiological results were compared using the paired t-test and the Wilcoxon signed-rank test.
Results
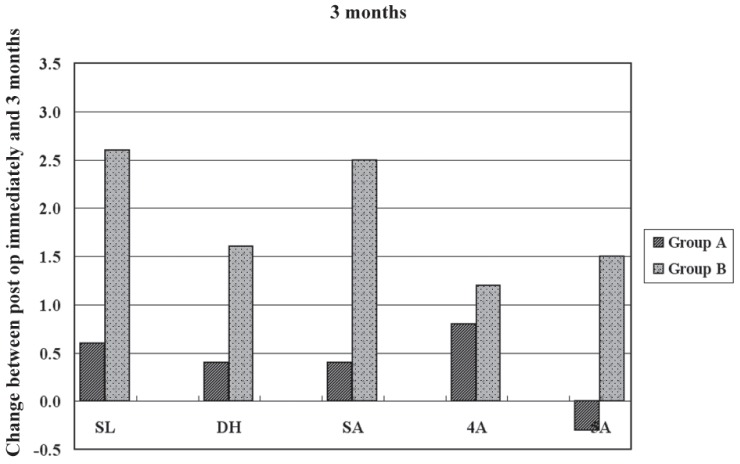
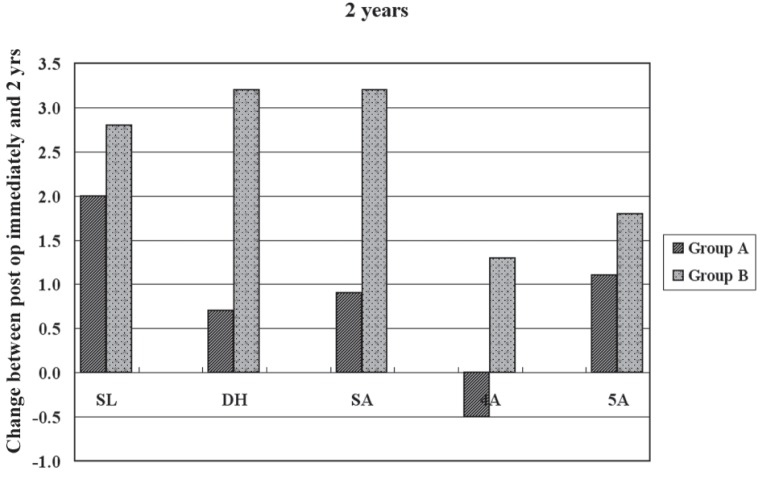
The mean age was 67.6 years in Group A and 68.2 years in Group B. The mean T score of Group A and Group B was −3.5 ± 0.6 and −3.3 ± 0.7, respectively (Table 1). There was no major perioperative complication in both the groups. But few minor complications occurred: 1 patient (Group A) underwent revision surgery for the removal of a drainage tube that was tightly anchored to the fascia, and 1 patient from (Group B) underwent revision surgery because of subcutaneous fluid collection. The mean improvement in the VAS pain score for back pain during the follow-up period was slightly higher in Group A than in Group B, but the difference was not statistically significant (Table 2). Radiologic parameters were analyzed by measuring the change between postoperative day 1 and the 3-month follow-up (Table 3, Fig. 2), and postoperative day 1 and the 2-year follow-up (Table 4, Fig. 3) in both groups.
Table 2.
Visual analogue scale (VAS) pain score for back pain during the follow-up period
| Group A | Group B | p | |
|---|---|---|---|
| Postop immediately | 8.9 ± 2.91 | 8.2 ± 3.23 | 0.373 |
| 3 months follow-up | 1.51 ± 1.16 | 1.49 ± 1.01 | 0.082 |
| 2 years follow-up | 1.01 ± 1.42 | 2.19 ± 1.23 | 0.107 |
Mean ± standard deviation,
p < 0.05.
Table 3.
Changes in radiologic parameters between postoperative day 1 and 3 months
| Group A | p | Group B | p | |
|---|---|---|---|---|
| SL | 0.6 ± 4.3 | 0.106 | 2.6 ± 3.4 | 0.019* |
| Disc height | 0.4 ± 3.2 | 0.622 | 1.6 ± 2.0 | 0.061 |
| Screw angle | 0.4 ± 3.7 | 0.718 | 2.5 ± 2.1 | 0.005* |
| L4 Screw angle | 0.8 ± 2.4 | 0.899 | 1.2 ± 2.6 | 0.164 |
| L5 Screw angle | –0.3 ± 2.5 | 0.613 | 1.5 ± 2.5 | 0.084 |
SL: segmental lordosis, mean ± standard deviation,
p < 0.05.
Fig. 2.
Changes of radiologic parameters during 3 months. There were no statistically significant changes in radiologic parameters in Group A. However, in Group B, there was a significant change in SL and SA. (*p < 0.05). SA: screw angle, SL: segmental lordosis, .
Table 4.
Changes in radiologic parameters between postoperative day 1 and 2 years
| Group A | p | Group B | p | |
|---|---|---|---|---|
| SL | 2.0 ± 5.4 | 0.707 | 2.8 ± 2.1 | 0.003* |
| Disc height | 0.7 ± 3.6 | 0.558 | 3.2 ± 1.7 | 0.003* |
| Screw angle | 0.9 ± 3.3 | 0.385 | 3.2 ± 2.5 | 0.005* |
| L4 Screw angle | –0.5 ± 2.2 | 0.482 | 1.3 ± 1.7 | 0.044* |
| L5 Screw angle | 1.1 ± 5.4 | 0.501 | 1.8 ± 1.8 | 0.019* |
SL: segmental lordosis, mean ± standard deviation,
p < 0.05.
Fig. 3.
Changes of radiologic parameters during 2 years. There were no statistically significant changes in radiologic parameters in group A. However, in group B, there was a significant change in all radiologic parameters. (*p < 0.05).
In Group A, SL at the operated level (L4–5) changed to 0.62 ± 1.15° during 3 months (p = 0.106) and 2.01 ± 1.61° during 2 years (p = 0.707). In Group B, SL changed to 2.57 ± 1.03° (p = 0.109) during 3 months and 2.78 ± 0.67° (p = 0.003) during 2 years. A statistically significant change in SL was seen only in Group B (Figs. 2, 3).
DH changed to 0.43 ± 0.86 mm during 3 months (p = 0.622) and 0.65 ± 1.07 mm during 2 years (p = 0.55) in Group A, and to 1.58 ± 0.71 mm during 3 months (p = 0.061) and 3.15 ± 0.65 mm during 2 years (p = 0.003) in Group B. Statistically significant changes in DH were also seen in Group B (Figs. 2, 3).
SA changed to 0.36 ± 0.97° during 3 months (p = 0.718) and 0.89 ± 0.98° during 2 years (p = 0.385) in Group A, and it changed to 2.50 ± 0.67° during 3 months (p = 0.005) and 3.20 ± 0.84° during 2 years (p = 0.005) in Group B. SA changed significantly in Group B (Figs. 2, 3).
The 4A changed to 0.84 ± 0.65° during 3 months (p = 0.899) and 0.49 ± 0.67° during 2 years (p = 0.482) in Group A, and it changed to 1.24 ± 2.60° during 3 months (p = 0.164) and 1.34 ± 0.56° during 2 years (p = 0.044) in Group B. The 5A changed to 0.34 ± 0.67° during 3 months (p = 0.613) and 1.13 ± 1.63° during 2 years (p = 0.501) in Group A, and it changed to 1.52 ± 0.78° during 3 months (p = 0.84) and 1.75 ± 0.60° during 2 years (p = 0.019) in Group B. Both 4A and 5A showed significant change in Group B (Figs. 2, 3). Fusion rate at final follow-up (2 years) was 93.8% in Group A and 76.2% in Group B, but the difference was not statistically significant (p = 0.089).
Case 1:
A 78-year-old woman underwent TLIF at L4–5 with HA screw augmentation. The T-score was found to be −3.8. Arrow shows well-visualized HA at each level. Over a 2-year period, the segmental lordosis (SL) angle, disc height (DH), screw angle (SA), L4 screw angle (4A), and L5 screw angle (5A) changed by 1.56°, 2.34 mm, 0.23°, 0.15°, and 0.79°, respectively. Except for the DH and SL, all other radiologic parameters did not change significantly. The SL angle changed by only 1.56° because of subsidence of disc space during the follow-up period. Each radiologic parameter represents mean value of bilateral pedicle screw.
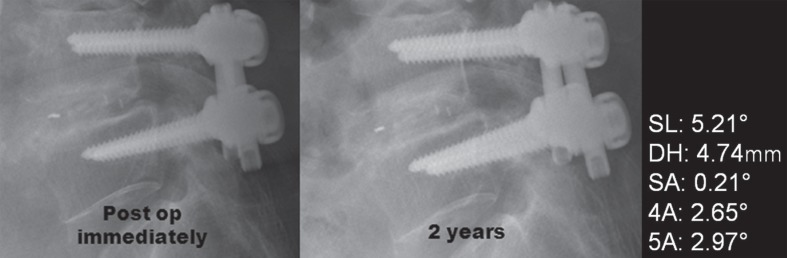
Case 2:
A 70-year-old woman underwent TLIF at L4–5 without screw augmentation. The T-score was found to be −3.5. Over a 2-year period, the segmental lordosis (SL) angle, disc height (DH), screw angle (SA), L4 screw angle (4A), and L5 screw angle (5A) changed by 5.21°, 4.74 mm, 0.21°, 2.65°, and 2.97°, respectively. Except for the SA, all other parameters changed significantly after the 2-year period. Each radiologic parameter represents mean value of bilateral pedicle screw.
Discussion
Rigid internal fixation relates to the ability of a screw to attach to the spine. The stability of the instrumentation used is of considerable importance in determining the outcome. Naturally, the quality of the bone into which the screw is placed is also an important factor. Several studies have confirmed that screws placed in osteoporotic spines have a significantly lower screw strength with more frequent screw movements within the vertebra than those placed in normal spines, and thus have overall higher failure rates of up to 12%.2,9) Therefore, the augmentation of pedicle screw fixation with various materials has been studied.3,4,6,7,9,13)
Frankel et al. reported that pullout strength increased after PMMA augmentation in primary and salvage procedures by 119% and 162%, respectively.3) Although PMMA has proven to be an effective material for increasing the pullout strength of pedicle screws inserted into osteoporotic bones, it also has several disadvantages, such as its exothermic properties, the risk of neural injury in the event of extravasation, and difficulties in performing revision surgery.12) As a consequence, the use of bioabsorbable bone cements has been suggested. Wittenberg et al. evaluated a biodegradable mixture of tricalcium phosphate, calcium carbonate, and methylmethacrylate monomer and found a significant improvement in pullout strength when using this augmentation.14) Moore et al. reported the results of using a calcium phosphate cement for augmentation of pedicle screw fixation and found an increase of 200% in pullout strength compared to native bone.8) Wuisman et al. reported satisfactory results of in vitro screw augmentation with calcium apatite cement.13) HA cement has also been suggested as a biodegradable material for use in screw fixation. Hasegawa et al. performed an animal study showing that the resistance to pullout force of HA augmented screws was 1.6 times that of non-augmented screws.5) Sandén et al. performed a clinical study comparing the extraction torque between HA-coated screws and non-coated screws in 23 consecutive patients.10) They showed that use of HA-coated screws resulted in improved screw fixation with a reduced risk of loosening.10) However, HA-coated screws are somewhat different compared to augmentation with HA cement. HA cement can be injected or packed into an irregular bony defect and can enable augmentation of only the distal tip of the screw. Renner et al. reported that the average pull-out strength for the screws was 1617 N after injection of calcium phosphate cement only to the distal tip of the screw hole. This was not significantly different from the 1852 N measured after injection of calcium phosphate cement along the entire length of the screw hole in a cadaveric model.9) Although HA-coating along the entire screw length creates higher extraction torque, and if this torque exceeds the range of the torque wrench it would be harmful, especially in case of revision surgery.11)
In the current study, 2 mL of HA cement paste was used for screw augmentation, and before each augmentation a poverty needle (Kyeongwon Medical, Seoul, South Korea) was drawn back about 1 cm. This method can enable the augmentation of only the distal tip of the pedicle screw and not along the entire length, which can prevent extravasation of HA cement into the central canal and/or pedicle fracture. Radiologic parameters were measured at postoperative day 1, 3 months, and 2 years for indirect comparison of biomechanical properties between groups A and B. The results were interesting. There were no statistically significant changes in radiologic parameters in Group A. However, in Group B, there was significant change in several radiologic parameters (Figs. 2, 3). In particular, SL changed to 2.57 ± 1.03° (p = 0.109) during 3 months and 2.78 ± 0.67° (p = 0.003) during 2 years. SA also changed to 2.50 ± 0.67° during 3 months (p = 0.005) and 3.20 ± 0.84° during 2 years (p = 0.005). In addition, DH changed 1.58 ± 0.71 mm during 3 months (p = 0.061) and 3.15 ± 0.65 mm during 2 years (p = 0.003). Although the differences were not statistically significant, fusion rate was higher in Group A than Group B at final follow-up (2 years), and the mean improvement in the VAS pain score for back pain during the follow-up period was slightly higher in Group A than Group B (Table 2).
These findings show that screw augmentation with HA results in an improved screw-bone interface, reduces the risk of angular displacement of screw constructs, and prevents subsidence at the operative level. Furthermore, as shown in a previous report,9) in osteoporotic patients, augmentation at the proximal end of the screw was sufficient to attain rigid internal fixation and avoid unnecessary morbidities like extravasation or pedicle fracture, which are associated with augmentation of the entire screw length. Although measuring the biomechanical properties is an indirect method, it highlights the superiority of screw augmentation with HA over native spine in osteoporotic patients. However, the present study has several limitations, including a small sample size, single observer, a retrospective design, and no direct comparison between HA-coated screws and HA cement augmentation.
In spite of these limitations, we believe that HA cement may be a useful tool for screw augmentation and should be recommended as a promising option for spinal instrumentation in osteoporotic patients.
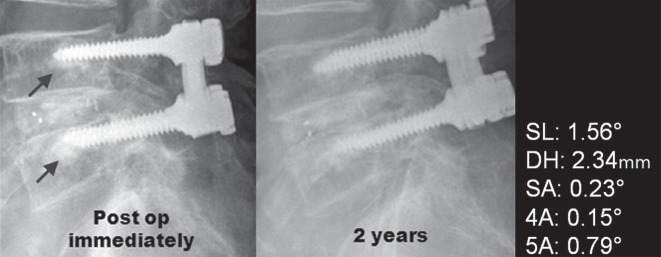
Case 1 A 78-year-old woman underwent TLIF at L4–5 with HA screw augmentation. The T-score was found to be −3.8. Arrow shows well-visualized HA at each level. Over a 2-year period, the segmental lordosis (SL) angle, disc height (DH), screw angle (SA), L4 screw angle (4A), and L5 screw angle (5A) changed by 1.56°, 2.34 mm, 0.23°, 0.15°, and 0.79°, respectively. Except for the DH and SL, all other radiologic parameters did not change significantly. The SL angle changed by only 1.56° because of subsidence of disc space during the follow-up period. Each radiologic parameter represents mean value of bilateral pedicle screw.
Case 2 A 70-year-old woman underwent TLIF at L4–5 without screw augmentation. The T-score was found to be −3.5. Over a 2-year period, the segmental lordosis (SL) angle, disc height (DH), screw angle (SA), L4 screw angle (4A), and L5 screw angle (5A) changed by 5.21°, 4.74 mm, 0.21°, 2.65°, and 2.97°, respectively. Except for the SA, all other parameters changed significantly after the 2-year period. Each radiologic parameter represents mean value of bilateral pedicle screw.
References
- 1). Burval DJ, McLain RF, Milks R, Inceoglu S: Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine 32: 1077– 1083, 2007. [DOI] [PubMed] [Google Scholar]
- 2). Coe JD, Warden KE, Herzig MA, McAfee PC: Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine 15: 902– 907, 1990. [DOI] [PubMed] [Google Scholar]
- 3). Frankel BM, D'Agostino S, Wang C: A biomechanical cadaveric analysis of polymethylmethacrylate-augmented pedicle screw fixation. J Neurosurg Spine 7: 47– 53, 2007. [DOI] [PubMed] [Google Scholar]
- 4). Frankel BM, Jones T, Wang C: Segmental polymethylmethacrylate-augmented pedicle screw fixation in patients with bone softening caused by osteoporosis and metastatic tumor involvement: a clinical evaluation. Neurosurgery 61: 531– 537; discussion 537–538, 2007. [DOI] [PubMed] [Google Scholar]
- 5). Hasegawa T, Inufusa A, Imai Y, Mikawa Y, Lim TH, An HS: Hydroxyapatite-coating of pedicle screws improves resistance against pull-out force in the osteoporotic canine lumbar spine model: a pilot study. Spine J 5: 239– 243, 2005. [DOI] [PubMed] [Google Scholar]
- 6). Lapresle P, Missenard G: Hydroxylapatite-coated Diapason screws: first clinical report. J Spinal Disord 8 ( Supple 1): S31– 39, 1995. [PubMed] [Google Scholar]
- 7). Lotz JC, Hu SS, Chiu DF, Yu M, Colliou O, Poser RD: Carbonated apatite cement augmentation of pedicle screw fixation in the lumbar spine. Spine 22: 2716– 2723, 1997. [DOI] [PubMed] [Google Scholar]
- 8). Moore DC, Maitra RS, Farjo LA, Graziano GP, Goldstein SA: Restoration of pedicle screw fixation with an in situ setting calcium phosphate cement. Spine 22: 1696– 1705, 1997. [DOI] [PubMed] [Google Scholar]
- 9). Renner SM, Lim TH, Kim WJ, Katolik L, An HS, Andersson GB: Augmentation of pedicle screw fixation strength using an injectable calcium phosphate cement as a function of injection timing and method. Spine (Phila Pa 1976) 29: E212– E216, 2004. [DOI] [PubMed] [Google Scholar]
- 10). Sandén B, Olerud C, Johansson C, Larsson S: Improved extraction torque of hydroxyapatite-coated pedicle screws. Eur Spine J 9: 534– 537, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Sandén B, Olerud C, Petrén-Mallmin M, Larsson S: Hydroxyapatite coating improves fixation of pedicle screws. A clinical study. J Bone Joint Surg Br 84: 387– 391, 2002. [DOI] [PubMed] [Google Scholar]
- 12). Wilkes RA, Mackinnon JG, Thomas WG: Neurological deterioration after cement injection into a vertebral body. J Bone Joint Surg Br 76: 155, 1994. [PubMed] [Google Scholar]
- 13). Wuisman PI, Van Dijk M, Staal H, Van Royen BJ: Augmentation of (pedicle) screws with calcium apatite cement in patients with severe progressive osteoporotic spinal deformities: an innovative technique. Eur Spine J 9: 528– 533, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Wittenberg RH, Lee K-S, Shea M, White AA, Hayes WC: Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop 296: 278– 287, 1993. [PubMed] [Google Scholar]