Abstract
Melanoma metastases to the pituitary gland are extremely rare, with only a few reported cases. We report an unusual case of pituitary metastatic melanoma in which the patient presented with pituitary apoplexy. A 68-year-old man presented general fatigue and anorexia following sudden headache. Neurological examination disclosed bitemporalhemianopsia. Computed tomography (CT) scans revealed a suprasellar mass including intratumoral hematoma. Magnetic resonance (MR) images demonstrated a circumscribed mass lesion in the intra- and suprasellar regions, compressing the optic chiasm. Surgical exploration was performed through a transsphenoidal approach, and a mixture of tumor and necrotic tissue with old hematoma was obtained. The histological examination of the specimen revealed a partly necrotic, malignant tumor with focal melanotic pigmentation. Histopathologically, the diagnosis was consistent with pituitary apoplexy caused by hemorrhage from pituitary metastatic melanoma.
Keywords: pituitary, metastasis, melanoma, pituitary apoplexy, transsphenoidal approach
Introduction
The pituitary gland is an uncommon site for metastasis. In surgical series, it is detected in less than 1% of patients subjected to transsphenoidal surgery for sellar or parasellar tumors.7,13) Breast and lung metastases demonstrate the highest affinity for the pituitary gland.7,9,10,12,13) Although malignant melanoma is known to have a high propensity to metastasize to the brain, involvement of the pituitary gland is exceedingly rare.4,8,14,18) Pituitary apoplexy is a clinical syndrome resulting from the hemorrhage, infarction, or hemorrhagic infarction of a pituitary tumor that results in its sudden and fulminant expansion.3,16) We report an unusual case of pituitary metastatic melanoma in which the patient presented with pituitary apoplexy.
Case Report
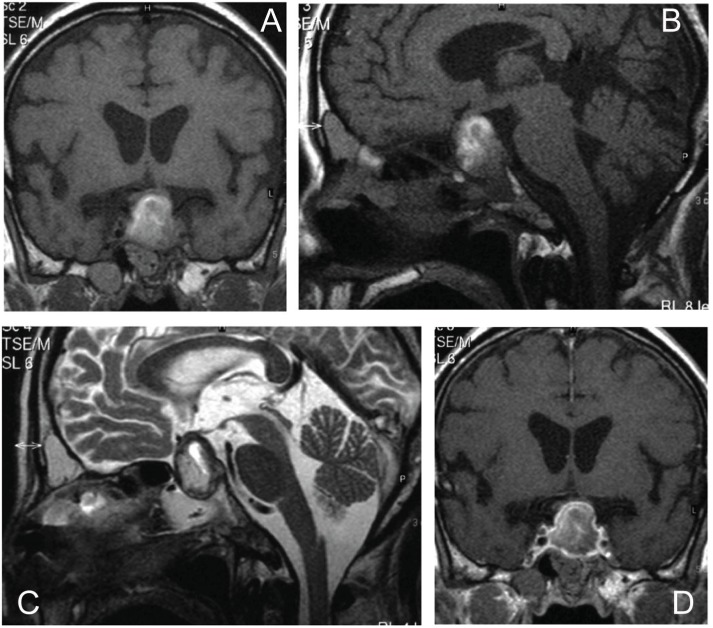
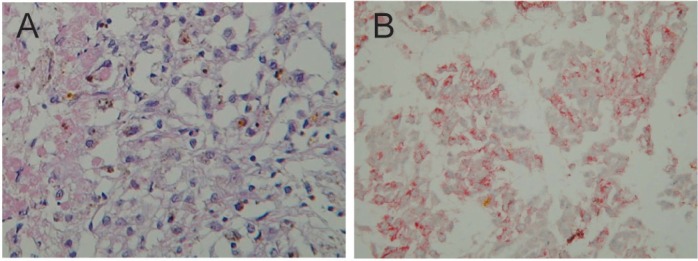
A 68-year-old man presented general fatigue and anorexia following sudden headache, which had persisted for a few days before he consulted our hospital. He was lethargic and slightly disorientated. Neurological examination disclosed bitemporalhemianopsia. Computed tomography (CT) scans revealed a suprasellar mass including intratumoral hematoma (Fig. 1). T1-weighted magnetic resonance (MR) images demonstrated a circumscribed mass lesion in the intra- and suprasellar regions, compressing the optic chiasm (Fig. 2A, B). T2-weighted image showed a hypointense rim and a heterogeneous center (Fig. 2C). After gadolinium (Gd) infusion, contrast MR image revealed marginal enhancement of the tumor and minimal inhomogeneous enhancement within the mass (Fig. 2D). There was no other cerebral lesion evident. Laboratory investigation revealed low levels of serum sodium at 128 mmol/l (normal 135–149 mmol/l). Hormone testing revealed minimal hypothyroidism (free T3 1.6 pg/ml, normal 2.5–4.5 pg/ml; free T4 0.60 ng/dl, normal 0.75–1.75 ng/dl; thyroid-stimulating hormone (TSH) 2.893 μU/ml, normal 0.47–4.14 μU/ml). The results of other endocrinological testing were as follows: adrenocorticotrophic hormone (ACTH), 29.0 pg/ml, normal 9.0–52.0 pg/ml; cortisol, 13.6 μg/dl, normal 4.5–21.1 μg/dl; and prolactin, 3.6 ng/ml, normal 3.4–16.2 ng/ml. Radiological findings and laboratory data suggested pituitary adenoma associated with hemorrhagic apoplexy or pituitary abscess.
Fig. 1.
Computed tomography (CT) scans showing a suprasellar mass including intratumoral hematoma.
Fig. 2.
Preoperative magnetic resonance (MR) imaging. A, B: T1-weighted MR images demonstrate a circumscribed mass lesion in the intra- and suprasellar regions, compressing the optic chiasm. C: T2-weighted image shows a sellar lesion with mixed signal characteristics (hypointense rim and heterogeneous center). D: After gadolinium (Gd) infusion, contrast MR image revealed marginal enhancement of the tumor and minimal inhomogeneous enhancement within the mass.
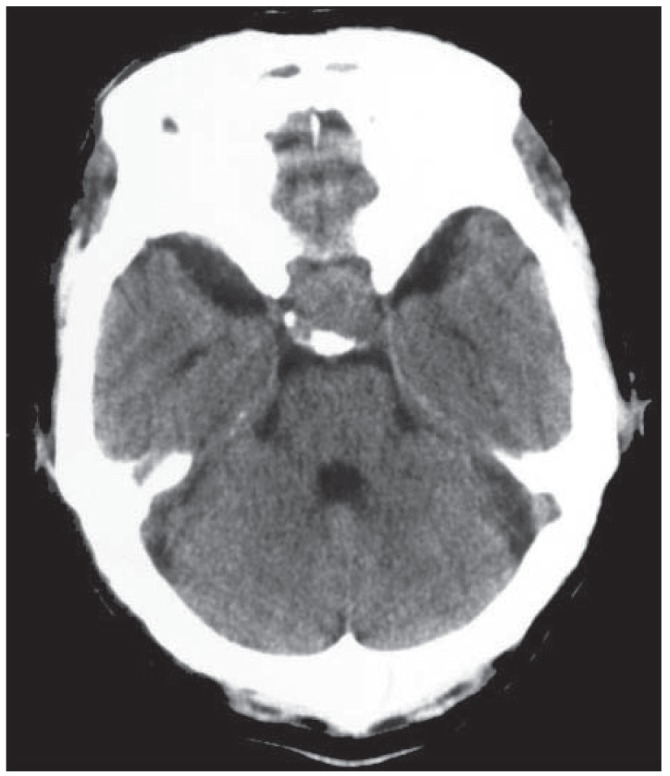
Surgical exploration was performed through a transsphenoidal approach, and a mixture of tumor and necrotic tissue with old hematoma was obtained. The yellowish gray-colored tumor occupied intra- and suprasellar regions. Gross-total tumor removal was performed. Intraoperatively, there was no macroscopically observed tumor invasion in the adjacent bone, dura, and diaphragm sellae. The histological examination of the specimen revealed a partly necrotic, malignant tumor with focal melanotic pigmentation (Fig. 3A). It was immunopositive for S-100 and HMB-45 proteins (Fig. 3B), which is indicative of a melanoma. The diagnosis was consistent with pituitary apoplexy caused by hemorrhage from pituitary metastatic melanoma.
Fig. 3.
A: The histological examination of the specimen, revealing a partly necrotic, malignant tumor with focal melanotic pigmentation. Hematoxylin and eosin stain, original magnification ×100. B: It was immunopositive for HMB-45 protein, which is indicative of a melanoma. Original magnification ×100.
Postoperatively, fatigue and anorexia were significantly improved with hydrocortisone substitution. The visual loss was completely recovered. After surgery, the patient developed diabetes insipidus despite minimal manipulation of the tumor. Presumably, the tumor had already involved the posterior lobe of the pituitary gland. The patient's diabetes insipidus required aqueous pitressin for the control of urine volume. Postoperative endocrinologic impairments and low serum sodium level were successfully treated with thyroid hormone and hydrocortisone. Endoscopic investigations were carried out and we diagnosed primary melanoma in the stomach (Fig. 4). His tumor extension had progressed markedly. Because the patient and his family refused irradiation and chemotherapy, no other adjuvant therapy had been applied. The patient was transferred to another hospital 2 months after the surgery.
Fig. 4.

Endoscopic investigation demonstrating primary melanoma in stomach.
Discussion
Metastatic tumors in the pituitary gland are well known in autopsy series, but are rare in neurosurgical practice.9,10,13) Furthermore, melanoma metastases to the pituitary gland are extremely rare, with only a few reported cases.2,5,6,8,11,15,18) In addition, cases of pituitary metastatic melanoma in which the patient presented with pituitary apoplexy have not been described.
Metastatic melanoma may appear with characteristic signal changes on MR images due to the presence of melanin. Hyperintensity on T1-weighted MR images without Gd contrast and hypointensity on T2-weighted images are characteristic of melanin.1,17) Heterogeneity in signal changes was likely due to hemorrhage. It is worth noting that other hemorrhagic metastases may show similar heterogeneous signals.1,17) Ischemic infarction of the anterior pituitary gland caused by tumor infiltration of the portal vessels may also cause diagnostic difficulties by complicating signal changes on MR images.
Pituitary apoplexy is a relatively uncommon yet potentially life-threatening clinical syndrome.3,16) The clinical features are typically sudden in onset, usually evolving in hours, and include headache, vomiting, visual disturbance, ophthalmoplegia, and altered consciousness.16) Pituitary apoplexy typically occurs in pituitary macroadenomas and may involve hyperfunctional or clinically nonfunctional tumors.3,16) However, an intratumoral hemorrhage may be associated with a pituitary metastasis. Pituitary apoplexy is a clinical syndrome resulting from the hemorrhage, infarction, or hemorrhagic infarction of a pituitary tumor that results in its sudden and fulminant expansion.3,16) In this case, CT, MR images, and histopathological findings suggested that the pathogenesis of pituitary apoplexy may have been hemorrhagic infarction of pituitary metastasis, but not pure hemorrhage.
Surgery provides effective symptomatic relief for pain and visual field deficit. As in the present case, early transsphenoidal sellar exploration facilitates the diagnosis of sellar metastasis and provides significant symptomatic improvement without the need to sacrifice longevity. The role of radiation therapy for melanoma metastases to the brain is controversial,8,14) but it does appear to provide benefit for pituitary metastases as a whole.5,11,18)
References
- 1). Atlas SW, Grossman RI, Gomori JM, Guerry D, Hackney DB, Goldberg HI, Zimmerman RA, Bilaniuk LT: MR imaging of intracranial metastatic melanoma. J Comput Assist Tomogr 11: 577– 582, 1987. [DOI] [PubMed] [Google Scholar]
- 2). Cox HH, Sloan LH: Melanoma. Report of a case apparently primary in the jejunum, the presenting symptoms resulting from metastasis in the hypophysiscerebri. J Am Med Assoc (JAMA) 82: 2021– 2025, 1924. [Google Scholar]
- 3). Furuta S, Hatakeyama T, Zenke K, Fukumoto S: Pituitary metastasis from carcinoma of the urinary bladder mimicking pituitary apoplexy—case report. Neuro Med Chir (Tokyo) 39: 165– 168, 1999. [DOI] [PubMed] [Google Scholar]
- 4). Gupta TD, Brasfield R: Metastatic melanoma. A clinicopathological study. Cancer 17: 1323– 1339, 1964. [DOI] [PubMed] [Google Scholar]
- 5). Guzel A, Maciaczyk J, Dohmen-Scheufler H, Senturk S, Volk B, Ostertag CB, Nikkhah G: Multiple intracranial melanoma metastases: case report and review of the literature. J Neurooncol 93: 413– 420, 2009. [DOI] [PubMed] [Google Scholar]
- 6). Jung SM, Hsu YY, Chuang CC, Chang CN, Hsueh C, Kuo TT: A man in his mid-70s with a sellar mass. Brain Pathol 17: 115– 116, 121, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Komninos J, Vlassopoulou V, Protopapa D, Korfias S, Kontogeorgos G, Sakas DE, Thalassinos NC: Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab 89: 574– 580, 2004. [DOI] [PubMed] [Google Scholar]
- 8). Leung GK, Chow WS, Tan KC, Fan YW, Lam KS: Metastatic melanoma of the pituitary gland. Case report. J Neurosurg 99: 913– 915, 2003. [DOI] [PubMed] [Google Scholar]
- 9). Marsh JC, Garg S, Wendt JA, Gielda BT, Turian JV, Herskovic AM: Intracranial metastatic disease rarely involves the pituitary: retrospective analysis of 935 metastases in 155 patients and review of the literature. Pituitary 13: 260– 265, 2010. [DOI] [PubMed] [Google Scholar]
- 10). Max MB, Deck MD, Rottenberg DA: Pituitary metastasis: incidence in cancer patients and clinical differentiation from pituitary adenoma. Neurology 31: 998– 1002, 1981. [DOI] [PubMed] [Google Scholar]
- 11). McCutcheon IE, Waguespack SG, Fuller GN, Couldwell WT: Metastatic melanoma to the pituitary gland. Can J NeurolSci 34: 322– 327, 2007. [DOI] [PubMed] [Google Scholar]
- 12). Morita A, Meyer FB, Laws ER: Symptomatic pituitary metastases. J Neurosurg 89: 69– 73, 1998. [DOI] [PubMed] [Google Scholar]
- 13). Nelson PB, Robinson AG, Martinez AJ: Metastatic tumor of the pituitary gland. Neurosurgery 21: 941– 944, 1987. [DOI] [PubMed] [Google Scholar]
- 14). Sampson JH, Carter JH, Friedman AH, Seigler HF: Demographics, prognosis, and therapy in 702 patients with brain metastases from malignant melanoma. J Neurosurg 88: 11– 20, 1998. [DOI] [PubMed] [Google Scholar]
- 15). Scholtz CL, Siu K: Melanoma of the pituitary. Case report. J Neurosurg 45: 101– 103, 1976. [DOI] [PubMed] [Google Scholar]
- 16). Semple PL, Webb MK, de Villiers JC, Laws ER: Pituitary apoplexy. Neurosurgery 56: 65– 72; discussion 72–73, 2005. [DOI] [PubMed] [Google Scholar]
- 17). Tüttenberg J, Fink W, Back W, Wenz F, Schadendorf D, Thomé C: A rare primary sellar melanoma. Case report. J Neurosurg 100: 931– 934, 2004. [DOI] [PubMed] [Google Scholar]
- 18). Wang YY, Norris A, Plessis D, Gnanalingham KK: Melanoma of the sellar region. J Clin Neurosci 18: 154– 156, 2011. [DOI] [PubMed] [Google Scholar]