Abstract
There is much uncertainty about levels and trends in infant mortality in the former Soviet republics of Central Asia. As a result, the impact of the break-up of the Soviet Union on infant mortality in the region is not known, and proper monitoring of mortality levels is impaired. In this paper, we use a variety of data sources and methods to assess infant mortality levels and trends in one Central Asian republic, Kyrgyzstan, between 1980 and 2010. We find that, contrary to what the registration data indicate, infant mortality abruptly stopped declining during the decade following the break-up of the Soviet Union. We also find that infants of Central Asian ethnicity or born in rural areas remain considerably more at risk, in contrast with what the reported levels show. We discuss the implication of these findings for health policy and for understanding the nature of the health crisis in this understudied part of the former Soviet Union.
Keywords: Infant Mortality, Kyrgyzstan, Central Asia, Former Soviet Union, Indirect Estimation Techniques, Data Quality
Introduction
Countries of the former Soviet Union have experienced a severe health crisis in recent decades (Meslé et al. 1996; Shkolnikov et al. 1998; Brainerd 1998; Cornia and Paniccia 2000; Stuckler et al. 2011). The severity of the crisis has varied greatly by country, but all of them have experienced substantial declines in life expectancy following the break-up of the Soviet Union in 1991. To this day, most of these countries have not recovered their 1991 life expectancy levels.
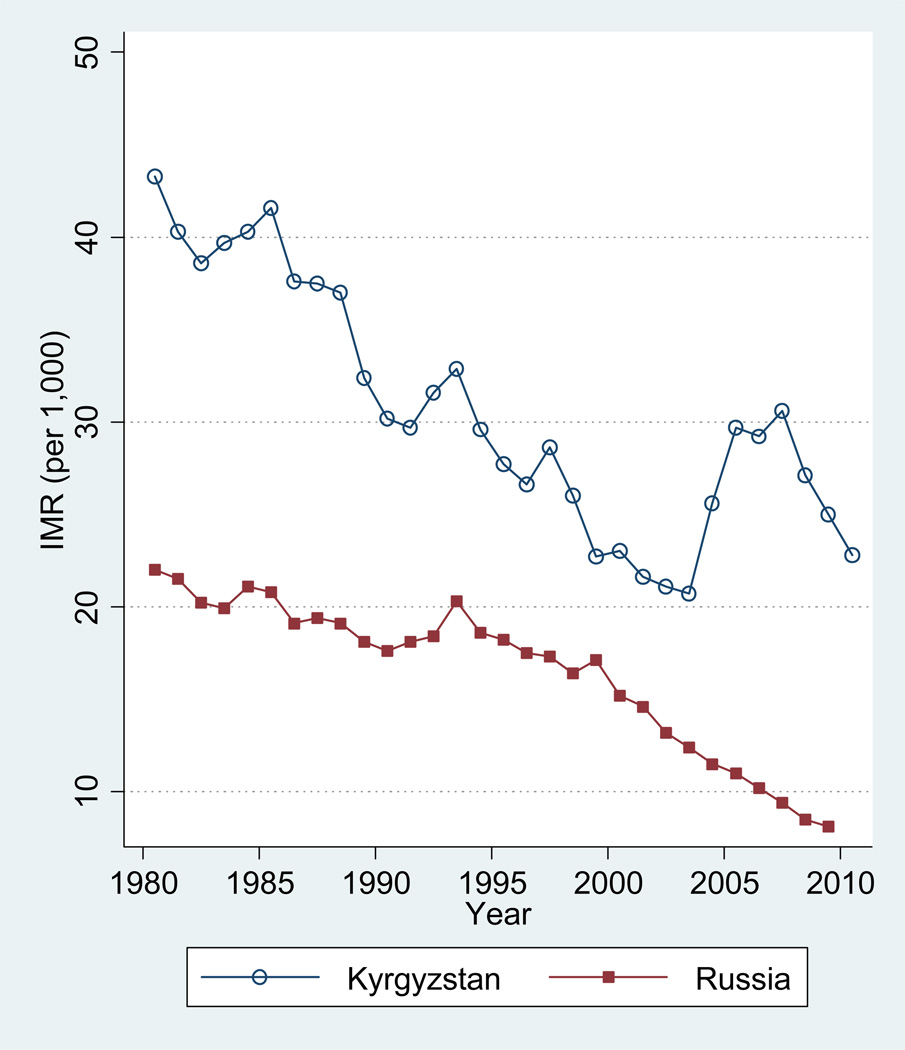
Trends in reported infant mortality in the region contrast greatly with these negative trends in overall mortality. In most former Soviet republics, reported infant mortality rates (IMR), calculated as the ratio of infant deaths to births the same year, have not increased substantially during the post-independence period, and today’s reported levels are substantially lower than they were in 1991. In Russia, for example, after a stalling of progress in the early 1990s, the reported IMR shows an impressive trajectory of decline, as shown in Figure 1. The IMR value for 2009 is 8.16 per thousand, more than half the 1991 value of 17.1 per thousand. This contrasts with life expectancy at birth, which in 2009 was still lower than the 1991 value. Declines in life expectancy in Russia, which actually pre-dated the break-up of the Soviet Union (Shkolnikov et al. 2004), have been overwhelmingly due to increases in adult mortality, especially in the 20–59 age range, rather than to changes in infant mortality (Vallin and Meslé 2001).
Figure 1.
Registration-based infant mortality rate (IMR), Russia and Kyrgyzstan, 1980–2010
Source:
Kyrgyzstan: Official registration data;
Russia: European Health for All Database, available at http://data.euro.who.int/hfadb/
The contrast between decreases in infant mortality and increases in adult mortality has led researchers to conclude that, in Russia at least, the health crisis may not have been directly linked to a deterioration in curative medical care or public health (Chen et al. 1996; Shkolnikov et al. 1998; Anderson 2002). Indeed, a deterioration in medical care or public health services would have generated increases in communicable diseases, to which infants are particularly vulnerable, and substantial IMR increases would have been observed.
The reported data from the former Soviet republics of Central Asia indicate a somewhat similar pattern in that region. Figure 1 shows the IMR trend in one Central Asian republic, Kyrgyzstan, together with Russia. Although IMR levels have been higher in Kyrgyzstan, there is no sustained increase in the reported IMR since 1991. There is a small increase between 1991 and 1993, but this increase is short term and followed by substantial declines thereafter. In fact, the reported data indicate a narrowing of the gap between Russia and Kyrgyzstan during the 1990s, both in absolute and relative terms. (The sharp increase in the IMR between 2003 and 2005 is not real but reflects Kyrgyzstan’s adoption of WHO’s standard with regards to the definition of live births and stillbirths. We will discuss this pattern later in the paper.)
Although the overall pattern of IMR change in Kyrgyzstan is somewhat similar to that observed in Russia (albeit at a different level), it has been regarded with much doubt in the case of Kyrgyzstan. Indeed it has been argued that reported IMR decreases in the 1990s in Kyrgyzstan and in other Central Asian republics are likely to be artifactual, due to possible declines in the completeness of vital registration during the years following the collapse of the Soviet Union (Becker et al., 1998; Hohmann and Garenne, 2005).
In addition to uncertainty about trends (decrease vs. increase vs. stagnation), there is much uncertainty about levels of infant mortality in Central Asian republics. While there is consensus that the reported rates are too low overall (Anderson and Silver 1986, 1997; Velkoff and Miller 1995; Aleshina and Redmond 2005), there is uncertainty about the actual amount of underestimation and how it might have changed over time. This is obviously related to uncertainty about trends. If the magnitude of the underestimation was constant over time, trends in reported rates would still be informative. However, as shown later in the paper, it is likely that the magnitude of the biases has changed over time, and that reported trends, in addition to levels, are misleading.
In this study, we used a number of data sources and methodological approaches to assess levels and trends in infant mortality in one Central Asian republic, Kyrgyzstan. The data include detailed vital registration data, census data, and survey data. Many of these sources are not publicly available and are used for the first time in a former Soviet republic.
We focused on the period 1980–2010, which includes a number of years before and after the break-up of the Soviet Union in December 1991. This gave us ample room to assess whether the break-up of the Soviet Union coincided with a marked deviation from earlier trends. (Before 1980, the reported IMR was increasing in Kyrgyzstan and other Central Asian republics (Guillot 2007). These reported increases, which affected IMR trends at the Soviet level, have been the topic of a lively debate among scholars (Davis and Feshbach 1980; Eberstadt 1981; Anderson and Silver 1986; Velkoff and Miller 1995). The study of this issue is beyond the scope of this paper.)
We focused on infant mortality rather than under-five mortality for both substantive and empirical reasons. The substantive reason is that infant mortality is more responsive to changes in annual mortality conditions, because it involves a shorter lag between the timing of mortality exposures and the timing of corresponding births. The empirical reason is that the national statistical office of Kyrgyzstan collects more detailed information on infant mortality than on under-five mortality. Although infant mortality has a long tradition in demography, the international health community now seems to prefer under-five mortality, because in retrospective surveys measures of under-five mortality are less subject to age misreporting errors. It is also argued that the correlation between infant mortality and under-five mortality is high, making under-five mortality an adequate measure. However, surveys are only one of many data sources that we use in this paper. Thus the advantage of using under-five mortality is less clear.
Assessing levels and trends in infant mortality in Central Asia has obvious policy relevance. For health policy purposes, a precise monitoring of infant mortality is paramount. The broader relevance of this assessment pertains to understanding the nature of the health crisis in former Soviet republics and how it might vary by republic. In the case of Russia, as we said earlier, a deterioration of health services has not been identified as the most important factor of the health crisis, because of the observed decreases in infant mortality since the mid-1990s. The extent to which this conclusion also applies to Central Asian republics remains to be determined, due to the large amount of uncertainty regarding reported trends in infant mortality.
In this paper, we first review the errors and biases that have been identified as relevant in the former Soviet context in general, and in Central Asia in particular. Second, we present uncorrected trends in infant mortality, based on official vital registration data, and discuss patterns that seem implausible on the basis of internal comparisons. Third, we present results based on a variety of data sources, including census data, vital registration data, and survey data, with the purpose of addressing possible deficiencies in reported infant mortality. Finally, we propose corrected levels and trends in infant mortality, and discuss the implication of these corrected trends for understanding the health crisis in this understudied part of the former Soviet Union.
This article builds on a number of recent studies that have produced corrected trends in infant mortality in former Soviet republics, including Armenia (Hakokyan and Yepiskoposyan 2006; Duthé et al. 2010), Georgia (Duthé et al. 2010), Ukraine (Vallin and Meslé 2012), Uzbekistan (Hohmann and Garenne 2005), and Moldova (Penina et al. 2010). Central Asia remains an understudied region in this literature, a gap we seek to address with this article.
Sources of errors in reported infant mortality in Kyrgyzstan
In the demographic literature on infant mortality in former Soviet republics, there is consensus that the reported levels are too low, and that the underestimation is particularly severe in Central Asian republics (Anderson and Silver 1997; Aleshina and Redmond 2005). The underestimation of infant mortality, which existed throughout the Soviet period, appeared clearly when independent estimates of infant and child mortality, produced by Demographic and Health Surveys (DHS), became available for Central Asian republics. In Kyrgyzstan, for example, the 1997 DHS estimated an average infant mortality rate of 66.2 per thousand for the period 1988-97 (Macro International 1998: 97). By contrast, the official mortality rate for the same period was 30.8 per thousand.
There are several reasons for the underestimation of infant mortality in the former Soviet Union. The first reason stems from differences between the Soviet and the World Health Organization’s (WHO) definitions of a live birth and a stillbirth (Anderson and Silver 1986). Some births that would be counted as live births under the WHO standard are counted as stillbirths or miscarriages under the Soviet standard, and receive neither a birth certificate nor a death certificate. Specifically, under the WHO standard, births showing any sign of life should be counted as live births, while the Soviet definition only considers breathing as a sign of life justifying the recording of a live birth. Moreover, among babies who breathed, those who are born before the end of the 28th week of gestation (or with weight under 1000 grams, or with length less than 35 cm) and who die in the first seven days are considered miscarriages rather than live births under the Soviet definition. These differences in definition produce a downward bias in the infant mortality rate calculated in Soviet republics. Anderson and Silver (1986) estimated that infant mortality rates in Soviet republics would be higher by 22–25 percent if they were calculated according to international standards. After the break-up of the Soviet Union, newly-independent republics progressively adopted the international standard. In Kyrgyzstan, the change occurred in 2004. As shown in Figure 1, this change generated a 43% increase in the reported IMR between 2003 and 2005, from 20.7 to 29.7 per 1,000.
Anderson and Silver (1999) and Aleshina and Redmond (2005) discuss additional sources of bias which make reported rates in the former Soviet Union too low. These sources of bias include: the misreporting of live births as stillbirths, even for cases that would meet the Soviet definition of a live birth; the misreporting of late infant deaths as deaths occurring after the child’s first birthday, generating an unusually high number of reported deaths at the age of 12 completed months and beyond; and underregistration of infant deaths. These problems, which occur to some degree in all former Soviet Republics, are believed to be particularly severe in Central Asian republics.
Patterns of uncorrected infant mortality
In a first set of analyses, we examined the raw vital registration data. These analyses were made possible by a data collection effort that we undertook in Kyrgyzstan. This data collection consisted of gathering unpublished aggregate tables of births and deaths from the archives of the National Statistical Committee (NSC) of the Kyrgyz Republic. The tables used in this study were distributions of annual births and infant deaths by urban/rural residence and ethnicity (Forms No. 3 and A03), and distributions of deaths below age two by age at death in months (Forms No. 4a, 4z, S40 and S45). Raw distributions of reported births and infant deaths by urban/rural residence and ethnicity are provided in the Annex.
Annex Table.
Registered births and deaths below age one, Kyrgyzstan, 1980–2010, by urban/rural residence and ethnicity
| Births |
Deaths below age 1 |
Percent of Births |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Total | Urban | Rural | Central Asian |
Slavic | Other ethn. |
Total | Urban | Rural | Central Asian |
Slavic | Other ethn. |
Urban | Slavic |
| 1980 | 107278 | 34450 | 72828 | 79690 | 18985 | 8603 | 4643 | 1107 | 3536 | 3839 | 515 | 289 | 32,1% | 17,7% |
| 1981 | 113434 | 36046 | 77388 | n/a | n/a | n/a | 4577 | 1022 | 3555 | n/a | n/a | n/a | 31,8% | n/a |
| 1982 | 117235 | 35670 | 81565 | 89147 | 18544 | 9544 | 4523 | 1036 | 3487 | 3711 | 495 | 317 | 30,4% | 15,8% |
| 1983 | 120708 | 36597 | 84111 | 93034 | 17975 | 9699 | 4788 | 1062 | 3726 | 3982 | 501 | 305 | 30,3% | 14,9% |
| 1984 | 126075 | 39289 | 86786 | 97147 | 18676 | 10252 | 5086 | 1118 | 3968 | 4233 | 477 | 376 | 31,2% | 14,8% |
| 1985 | 128460 | 39352 | 89108 | 100477 | 17901 | 10082 | 5346 | 1181 | 4165 | 4522 | 491 | 333 | 30,6% | 13,9% |
| 1986 | 133728 | 40796 | 92932 | 105006 | 18241 | 10481 | 5034 | 1154 | 3880 | 4343 | 399 | 292 | 30,5% | 13,6% |
| 1987 | 136588 | 41732 | 94856 | 107757 | 18371 | 10460 | 5122 | 1300 | 3822 | 4359 | 464 | 299 | 30,6% | 13,4% |
| 1988 | 133710 | 40803 | 92907 | 106773 | 16983 | 9954 | 4952 | 1252 | 3700 | 4249 | 401 | 302 | 30,5% | 12,7% |
| 1989 | 131508 | 38943 | 92565 | 107321 | 15238 | 8949 | 4258 | 1114 | 3144 | 3631 | 381 | 246 | 29,6% | 11,6% |
| 1990 | 128810 | 37404 | 91406 | 106846 | 13845 | 8119 | 3889 | 1033 | 2856 | 3367 | 305 | 217 | 29,0% | 10,7% |
| 1991 | 129536 | 37616 | 91920 | 109558 | 12598 | 7380 | 3848 | 1007 | 2841 | 3369 | 291 | 188 | 29,0% | 9,7% |
| 1992 | 128352 | 35599 | 92753 | 110828 | 10744 | 6780 | 4058 | 1097 | 2961 | 3583 | 267 | 208 | 27,7% | 8,4% |
| 1993 | 116795 | 31070 | 85725 | 102542 | 8285 | 5968 | 3839 | 1127 | 2712 | 3416 | 226 | 197 | 26,6% | 7,1% |
| 1994 | 110113 | 29327 | 80786 | 97711 | 6976 | 5426 | 3262 | 956 | 2306 | 2948 | 186 | 128 | 26,6% | 6,3% |
| 1995 | 117340 | 30081 | 87259 | 104410 | 7143 | 5787 | 3250 | 980 | 2270 | 2933 | 177 | 140 | 25,6% | 6,1% |
| 1996 | 108007 | 28700 | 79307 | 95990 | 6571 | 5446 | 2871 | 866 | 2005 | 2620 | 124 | 127 | 26,6% | 6,1% |
| 1997 | 102050 | 25919 | 76131 | 90967 | 5984 | 5099 | 2920 | 847 | 2073 | 2644 | 166 | 110 | 25,4% | 5,9% |
| 1998 | 104183 | 28494 | 75689 | 92921 | 6232 | 5030 | 2708 | 821 | 1887 | 2445 | 136 | 127 | 27,3% | 6,0% |
| 1999 | 104068 | 28328 | 75740 | 92490 | 6217 | 5361 | 2360 | 756 | 1604 | 2118 | 127 | 115 | 27,2% | 6,0% |
| 2000 | 96770 | 28193 | 68577 | 85778 | 5943 | 5049 | 2225 | 836 | 1389 | 1973 | 143 | 109 | 29,1% | 6,1% |
| 2001 | 98138 | 28491 | 69647 | 87505 | 5684 | 4949 | 2123 | 785 | 1338 | 1902 | 112 | 109 | 29,0% | 5,8% |
| 2002 | 101012 | 30195 | 70817 | 90301 | 5535 | 5176 | 2128 | 870 | 1258 | 1908 | 130 | 90 | 29,9% | 5,5% |
| 2003 | 105490 | 31866 | 73624 | 94578 | 5609 | 5303 | 2186 | 880 | 1306 | 1960 | 115 | 111 | 30,2% | 5,3% |
| 2004 | 109939 | 37381 | 72558 | 98586 | 5829 | 5524 | 2812 | 1427 | 1385 | 2552 | 140 | 120 | 34,0% | 5,3% |
| 2005 | 109839 | 35600 | 74239 | 99020 | 5691 | 5128 | 3258 | 1617 | 1641 | 2977 | 163 | 118 | 32,4% | 5,2% |
| 2006 | 120737 | 39414 | 81323 | 108858 | 5892 | 5987 | 3526 | 1802 | 1724 | 3219 | 158 | 149 | 32,6% | 4,9% |
| 2007 | 123251 | 41402 | 81849 | 111683 | 5752 | 5816 | 3771 | 1963 | 1808 | 3442 | 173 | 156 | 33,6% | 4,7% |
| 2008 | 127332 | 43974 | 83358 | 115594 | 5924 | 5814 | 3453 | 1852 | 1601 | 3152 | 167 | 134 | 34,5% | 4,7% |
| 2009 | 135494 | 46924 | 88570 | 123795 | 5584 | 6115 | 3393 | 1893 | 1500 | 3150 | 135 | 108 | 34,6% | 4,1% |
| 2010 | 146123 | 49905 | 96218 | 134203 | 5473 | 6447 | 3337 | 1888 | 1449 | 3080 | 143 | 114 | 34,2% | 3,7% |
Source: Official registration data
The IMR was calculated using the conventional approach (annual deaths below age one divided by annual births). This conventional IMR provides an approximation of 1q0, the period probability of dying before age one. We used this approach because it has fewer data requirements; it does not require information on infant deaths by year of birth, which in Kyrgyzstan is not available for all the subgroups studied in this paper, including ethnic subgroups. In the absence of large fluctuations in the annual number of births, the conventional IMR provides a close approximation of period 1q0 (Preston, Heuveline and Guillot 2001, p.36). (A comparison of the conventional IMR vs. period 1q0 in Kyrgyzstan at the national level shows that discrepancies are negligible.)
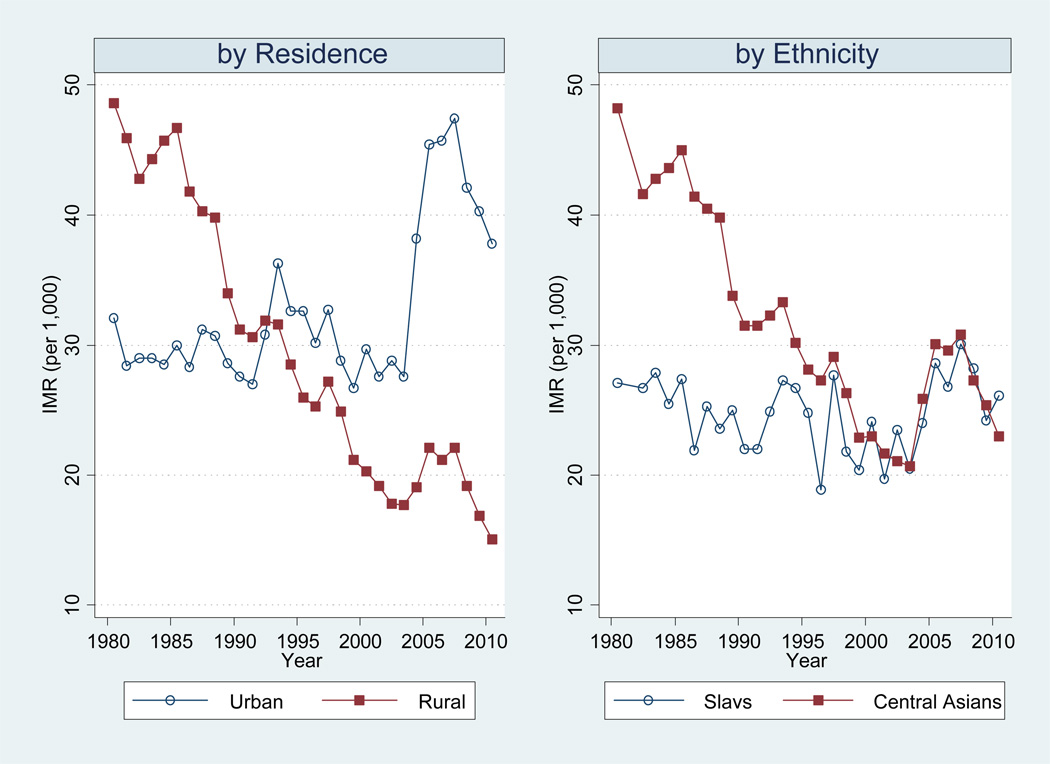
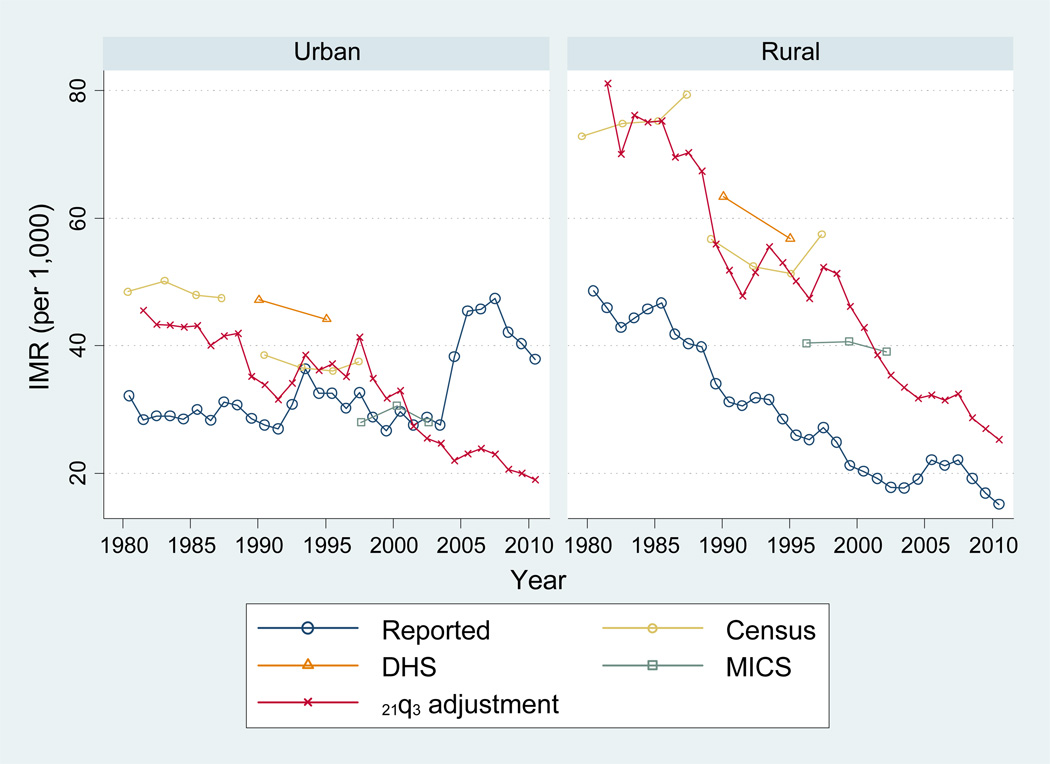
Infant mortality by urban/rural residence
Internal comparisons of uncorrected vital registration data largely confirmed the problems mentioned in the previous section. In Figure 2 (left panel), we show the reported IMR in urban and rural areas. Around the world, infant mortality rates tend to be higher in rural areas (United Nations 1982; Preston and Haines 1991; Bocquier et al. 2011), due in part to lower levels of socio-economic status and more difficult access to health facilities. This is the case in most former Soviet Republics (Kingkade and Arriaga 1997), including Kyrgyzstan in the early 1980s, as shown in Figure 2. However, the urban/rural differential decreased during the 1980s, and in 1992, we observe a cross-over. By the late 1990s, the reported rural IMR is substantially lower than the urban one. This is highly implausible. The sources of error that we mentioned earlier are likely to be particularly prominent in rural areas, potentially creating a spurious rural advantage. An additional source of error potentially affecting this trend is the misreporting of residence on birth and death certificates. The literature on Soviet mortality mentions the possibility that many rural deaths are reported as urban, perhaps because they sometimes occur in urban hospitals and might lack information about the deceased person’s actual place of residence (Anderson and Silver 1997). This problem does not affect the trends at the national level, but it does affect trends by residence, potentially contributing to the implausible urban/rural differential observed in Kyrgyzstan since 1992.
Figure 2.
Registration-based infant mortality rate (IMR) by residence and ethnicity, Kyrgyzstan, 1980–2010
Source: Official registration data.
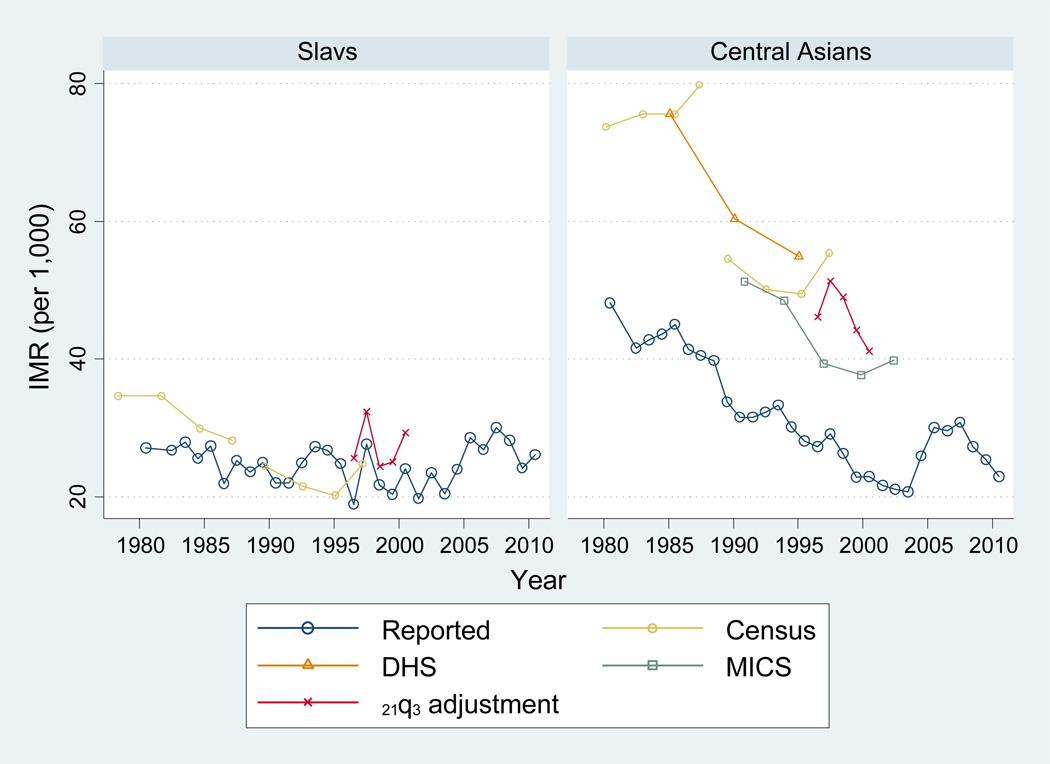
Infant mortality by ethnicity
Comparing reported IMRs by ethnicity is useful for our purpose, because Kyrgyzstan is a multi-ethnic country in which different ethnic groups have different urban/rural residence patterns, different educational levels, different standards of living, and, probably, different levels of data quality. Therefore, internal comparisons of ethnic groups can help distinguish real trends from spurious ones.
Figure 2 (right panel) shows patterns of infant mortality by ethnicity. We show here results for two broad ethnic groups: “Central Asians” (Kyrgyz, Uzbeks, Kazakhs, Tajiks and Turkmens), and “Slavs” (Russians, Ukrainians and Byelorussians). These two broad ethnic groups cover between 92% and 96% of annual births during our period of analysis. (The distribution of registered births by ethnicity is provided in the Annex.)
The estimation of IMR by ethnicity also reveals some implausible patterns. In the early 1980s, Central Asians had substantially higher infant mortality. This is consistent with well-established patterns of social stratification between Slavs and native ethnic groups in the region (Kahn 1993). During the 1990s, however, reported infant mortality among Central Asians continued declining, while it stayed more or less constant among Slavs. As a result, by the late 1990s, the excess infant mortality of Central Asians disappeared. This is also implausible, given the persistent economic disadvantage of Central Asians relative to Slavs during the 1990s and beyond, documented in several poverty surveys (Ackland and Falkingham 1997; World Bank 1999, 2007).
The pattern of infant mortality by ethnicity is related to patterns by urban/rural residence, because Central Asians live disproportionately in rural areas. These implausible patterns make us suspect that the extent of underestimation of infant mortality is particularly large among rural Central Asians. The timing of these implausible trends makes us also suspect that the extent of underestimation worsened during the 1990s.
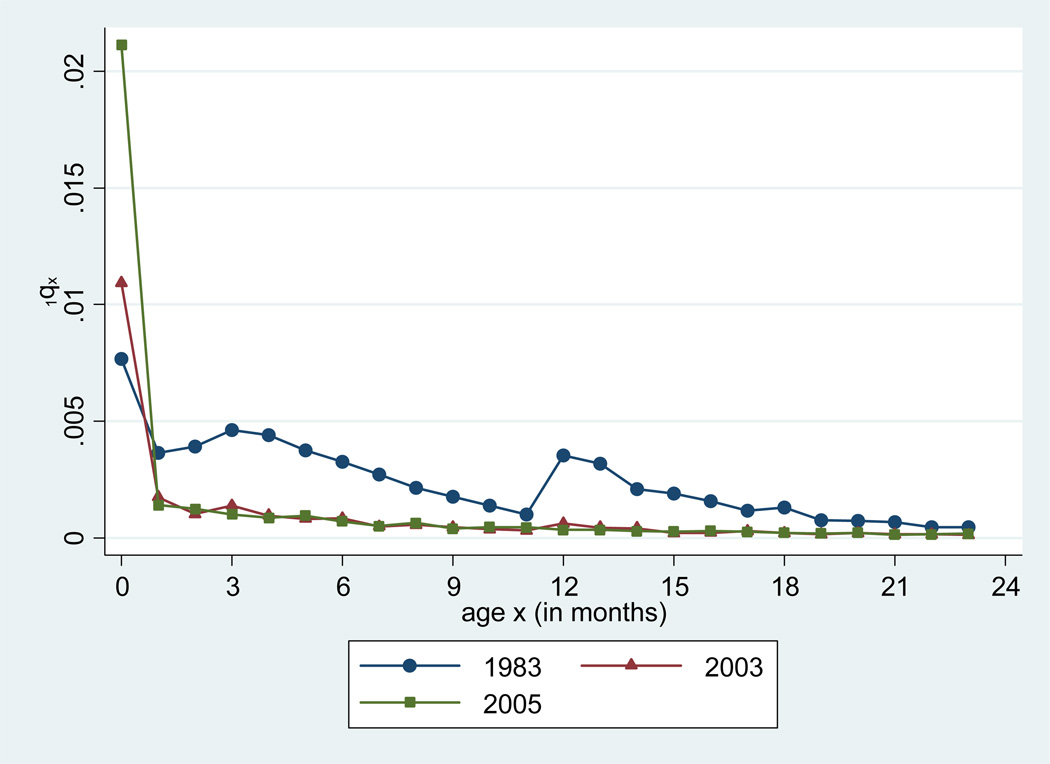
Infant mortality by month of age
Age patterns of infant mortality reveal some more specific deficiencies in the vital registration data. Figure 3 shows an approximation of the probability of that a baby aged x months will die before age x+1 months (1qx in life table notation, with subscripts expressed in months) in Kyrgyzstan in 1983 (the earliest year for which we have data on deaths below age 2 years by age in months). (Since it is not possible to calculate an actual period or cohort life table by age in months with the available data, we approximated period 1qx by combining deaths below age 2 in 1983 with births in 1983. This approximation is acceptable as long as births do not vary greatly over three consecutive years. Calculations for years where it was possible to relate deaths by age in months to the actual size of the corresponding cohorts show that this approximation made virtually no difference.) It appears that reported mortality in 1983, while highest during the first month of life, increases between the second and fourth months, and then increases again between the 12th and 13th months. This pattern is highly implausible. Typically, mortality decreases with age starting from birth until reaching a minimum around 10 years. A few instances in which mortality increases with age following an initial decline during the first few months of life have been documented in the literature, but these instances seem limited to some high-mortality sub-Saharan African populations (Garenne 1982; Pison and Langaney 1985; Delaunay et al. 2001; Sankoh et al. 2006), including populations with high prevalence of malaria (Abdullah et al. 2007) or HIV (Marinda et al. 2007). These epidemiological contexts have little in common with Kyrgyzstan. A more likely explanation for the age pattern shown in Figure 3 is data errors, because this pattern is consistent with the types of errors mentioned earlier. Specifically, the mortality increase between the second and fourth months is probably due to a combination of misclassification of infant deaths as stillbirths and incompleteness of registration of infant deaths during the first three months, which both contribute to underestimation of mortality at ages 0–2 months relative to ages 3–11 months. Similarly, the mortality increase between the 12th and 13th month is probably due to a misreporting of deaths occurring during the later months of the first year as deaths occurring during the early months of the second year of life, a misreporting perhaps used with the purpose of artificially deflating the reported infant mortality rate (Ksenofontova 1994, Aleshina and Redmond 2005). Figure 3 also shows monthly death probabilities in 2003 and 2005. By the year 2005, the mortality peaks around ages 3 and 12 months have disappeared, and reported mortality presents a more classic pattern of age-wise decrease.
Figure 3.
Reported monthly death probabilities (1qx), by age in months, Kyrgyzstan, 1983, 2003 and 2005
Source: Official registration data.
This examination of the raw vital registration data shows clear patterns of errors and calls for corrections. We will see later in this paper how we can use these detailed vital registration data to make adjustments. Such adjustments will be complemented by corrections based on additional sources of information, which we discuss in the next section.
Data and methods
In this paper, we use three main sources of information: (1) sample surveys (DHS and MICS); (2) 1989 and 1999 censuses; and (3) detailed vital registration information. These data sources are analyzed using various estimation methods, as detailed below.
Sample surveys
Two sample surveys containing relevant mortality information have been conducted in Kyrgyzstan: a Demographic and Health Survey (DHS) in 1997, and a Multiple Indicator Cluster Surveys (MICS) in 2006.
The DHS contains full birth histories, from which direct estimates of infant and child mortality can be derived. We are aware, however, that in the DHS direct estimates of infant mortality are more subject to errors than estimates of under-five mortality, in part because of misreporting of children’s age at death, in particular age heaping around age 1.00, i.e., a critical age for determining whether a death should be counted as an infant death or not. Therefore, in this study, rather than directly estimating the IMR, we directly estimated under-five mortality from the DHS, and then converted this indicator into infant mortality using model life tables. We used the Coale and Demeny West family for this procedure, because for the most recent years in our data series, the age pattern of under-five mortality (1q0 vs. 4q1) as observed in official registration data conformed best to this family. (As we will see later, the quality of the vital registration data has improved considerably in recent years, and therefore these data provided a strong basis for determining which family of model life tables was the best model for this conversion.)
For information at the national level, we followed DHS practice of estimating mortality estimates for three five-year periods preceding the survey date, which we recalculated from the raw data. However, for estimates by urban/rural residence, we calculated estimates for only two five-year periods. This is because residence status in the DHS is determined on the basis of the mother’s residence at the time of the survey, and we wanted to ensure that this variable was reasonably applicable to retrospective information on child survival. For estimates by ethnicity, we were not able to reliably estimate mortality for Slavs, because the sample size was too small (the number of unweighted deaths for Slavs for each five-year period varied between 3 and 8). However, this problem was not present among Central Asians, for whom we show estimates for the three five-year period preceding the survey.
The MICS survey was conducted in 2006. Rather than full birth histories, MICS collected only summary birth histories (number of children ever born and number of children surviving). This information was converted into IMR estimates using the Brass method. Here also, we rely on Coale and Demeny’s West model for this procedure. We ignored mortality information based on women in the first two age groups (15–19 and 20–24), because these estimates were implausibly high and out-of-line with the estimates from the older age groups (as is usually the case with the Brass method). For the same reason as in the DHS, we present MICS-based IMR estimates by urban/rural residence only for periods up to 10 years preceding the survey. Here also, because of sample size issues, we were not able to use the MICS data for estimating mortality among Slavs.
Census-based estimates of infant mortality
The 1989 Soviet census included a question on the number of children ever born and the number of children surviving, asked to women aged 15 and above who received the census long form (25% sample). This question was also asked in the 1999 census in Kyrgyzstan (to all women aged 15 and above). As with the MICS data, this information can be used to estimate levels and trends in infant mortality, using the Brass method. Official tabulation of these variables in the 1989 and 1999 censuses was very limited. Fortunately, thanks to the existence of the original individual-level databases for these two censuses, we were able to obtain more detailed tabulations of this information from NSC, including tabulations by urban/rural residence and ethnicity.
These census data usefully complement the estimates derived from sample surveys. First, the census databases were considerably larger than the sample surveys, which allowed us to estimate mortality among Slavs. Second, the 1989 census provided the only data that could produce indirect estimates of mortality before the break-up of the Soviet Union. The availability of both the 1989 and 1999 censuses allowed us to make useful pre- and post-independence comparison in a way that sample surveys do not. As with the MICS data, we used Coale and Demeny’s West model, ignored mortality information based on younger women’s age groups, and present information by urban/rural residence only up to 10 years before the time of the census.
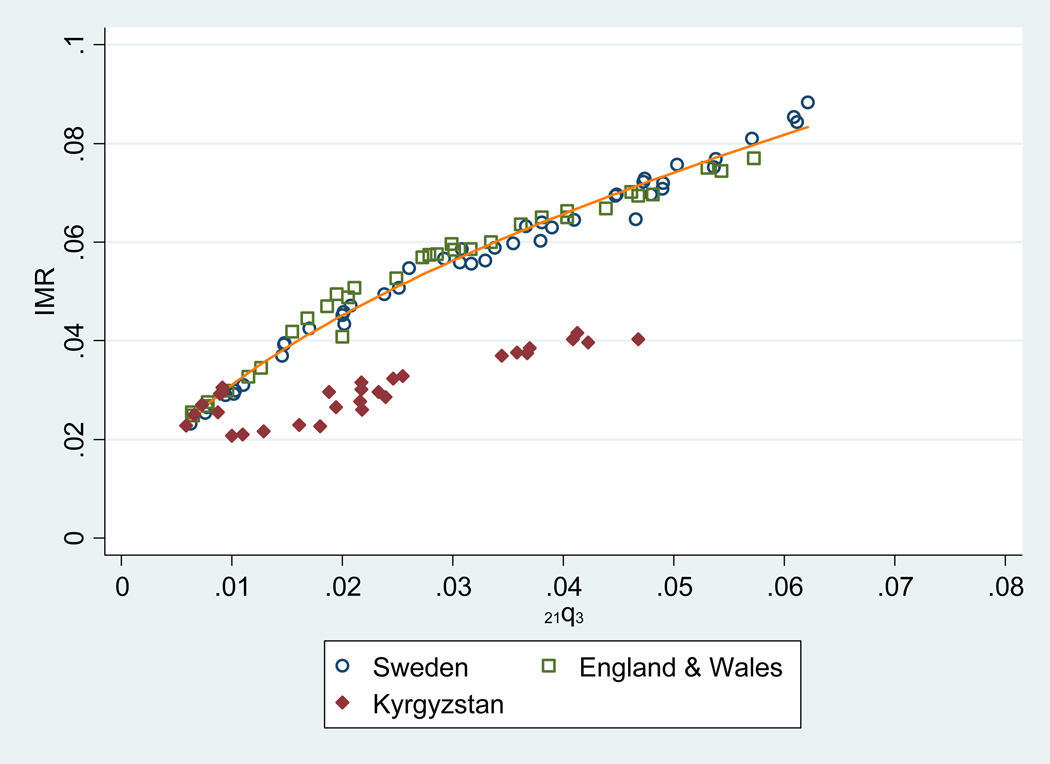
Registration information by month of age
In this study, we used an alternative procedure based on vital registration data, taking into consideration the patterns of error shown in Figure 3. Indeed, in Figure 3, two major problems can be detected: (1) underestimation of mortality at ages 0–2 months, relative to ages 3–11 months; (2) overestimation of mortality during months 12–23, relative to months 3–11. An interesting feature of these two types of errors is that they do not affect the reported probability that a child aged 3.0 months will die before age 24.0 months. Indeed, a death below age three months, if not registered, does not affect the reported number of survivors at age 3.0 months if the corresponding birth was not registered either. Therefore the denominator of the death probability will be unaffected. Similarly, a death occurring between ages 3.0 and 12.0 months, if misreported as occurring between age 12.0 and 24.0 months, will not affect the numerator of the death probability between 3.0 and 24.0 months. We term the probability that a baby aged 3.0 months will die before age 24.0 months “21q3”, using traditional demographic notation with subscripts referring to age in months.
21q3 is not totally free of data errors either. In particular, undercount of deaths in the age range 3.0–24.0 months will bias 21q3 downwards. Nonetheless, the patterns of errors shown in Figure 3 suggest that the most serious errors occur during the first three months and around the first birthday, and that 21q3, as reported in the vital registration data, is less biased than the traditional IMR. (Undercount of deaths below the age of 3.0 months, if the corresponding births were actually recorded, would bias 21q3 downwards. Such undercount affects the denominator, rather than the numerator, of the probability, and has a small impact on 21q3 relative to undercount of deaths in the age range 3.0–24.0 months. As in the case of 1qx in Figure 3, we approximate period 21q3 by relating deaths below age 2 years to births the same year.)
Levels and trends in 21q3 are useful for our purpose, because there exists a strong relationship between 21q3 and the IMR. This relationship is illustrated in Figure 4, which presents data from Sweden (1904–1948) and England & Wales (1922–1955), together with the fitted log-log linear relationship between the two indicators. (In the absence of more general models of the relationship between 21q3 and IMR, we relied here on data from two countries known for their high data quality and their long time series. The years were chosen such that the observed levels of 21q3 in Sweden and England & Wales are in the same range as in Kyrgyzstan during our period of interest. As in Kyrgyzstan, period 21q3 in Sweden and England & Wales was approximated by relating deaths below age 2 years to births the same year.) Figure 4 also presents points based on Kyrgyzstan’s registration data. In Kyrgyzstan, the reported IMR is much lower than what we would expect on the basis of the reported level of 21q3, given the patterns seen in Sweden and England & Wales.
Figure 4.
Relationship between 21q3 (probability that a child aged 3.0 month will die before reaching age 24.0 months) and infant mortality rate (IMR), in Sweden, England & Wales, and Kyrgyzstan (registration data) 1
Source: Official registration data.
1 This figure includes years 1904–1948 for Sweden; 1922–1955 for England & Wales; and 1981–2010 for Kyrgyzstan. The fitted series is based on a log-log linear model estimated using the Sweden and England & Wales data.
Because 21q3 appeared as a more reliable indicator of mortality levels and trends, we used it as a basis for calculating corrected estimates of IMR in Kyrgyzstan. The correction was made using the log-log relationship between 21q3 and IMR as observed in Sweden and England & Wales. This correction appears reasonable, because in Figure 4, data points for the years with the lowest levels of 21q3 (which correspond to years 2006–2010) conform well to the pattern observed in Sweden and England & Wales. This change towards the modeled pattern coincides with Kyrgyzstan’s adoption of WHO’s standard for classifying live births, i.e., an important improvement in the way infant mortality information is collected. (The 21q3 procedure proposed here is similar to the one developed by Kingkade and Arriaga (1997) for Soviet republics in 1990, except that these authors did not take into account observed mortality during the second year of life. Instead, they used 6q4 (with subscripts expressed in months) as the basis for their correction. Therefore, their procedure did not take into account errors arising from the misreporting of infant deaths as deaths above age one.)
Results
Infant mortality at the national level
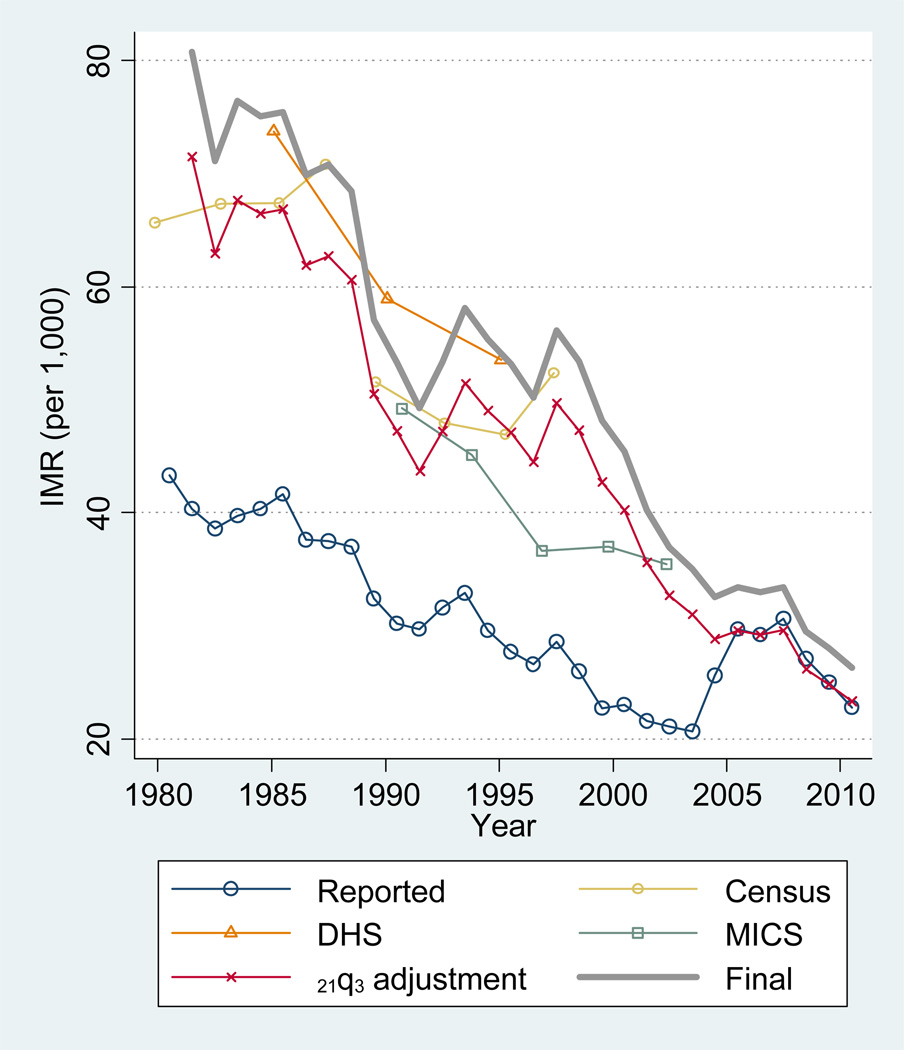
Figure 5 compares the reported IMR trend with various IMR estimates based on the data and methods described above. Although these estimates are based on completely different data sources and methods, they all lie within a rather narrow range, by comparison with the reported trend. The DHS estimates are somewhat higher than the 21q3-based IMR estimates for the years when they overlap, and the MICS estimates are somewhat lower, but on the whole these various estimates provide a similar picture of the evolution of infant mortality in Kyrgyzstan. This agreement increases our confidence that the corrected estimates bring us closer to truth. Among all the corrected indicators, the series that appears as the most informative is the one based on the 21q3 adjustment. Indeed, this series provides us with annual estimates and is based on a consistent data source and methodology for the entire period of analysis. This is in contrast with the other approaches which are meant to provide only a broad indication of levels and trends for rather limited time periods. Since the 21q3 adjustment series agrees overall with the other approaches for the years when they overlap, we find it reasonable to privilege it in the discussion. In this section we focus on the period up to 2004, the year of the change of standard for classifying live births. The period 2004–2010 will be discussed in a separate section later in the paper. (Figure 5 also presents a final adjustment which we discuss later in the paper.)
Figure 5.
Comparison of various infant mortality rate (IMR) estimates, Kyrgyzstan, 1980–2010
Source: Various primary data sources (see text for details).
The adjusted IMR estimates all confirm that the reported estimates are largely underestimated during the 1980s and the 1990s. Beyond this general assessment, however, we find that the amount of underestimation has changed overtime. During the 1980s, when looking at the 21q3 adjustment, we see a progressive diminution of the gap between the reported and adjusted indicators, suggesting a decline in the extent of underestimation in the registration-based IMR. During the 1990s, however, the gap between the two indicators increases, suggesting an increase in the underestimation of the registration data. A consequence of this change in the extent of underestimation is that the trend in the adjusted IMR is quite different from the trend in the reported IMR. While the reported IMR does not depart substantially from the earlier trends and continues to decline during the 1990s, the adjusted IMR abruptly stops declining in the 1990s. Only in 1999 does the adjusted IMR reach again the level observed in 1991, resuming its decline thereafter. The apparent decline in the reported IMR in the 1990s appears to be spurious, due to a deterioration of data quality following the break-up of the Soviet Union.
However, in none of the estimates do we find evidence for a large surge in infant mortality in the 1990s. On the whole, we find that the IMR levels of the 1990s were lower than the levels of the 1980s.
Infant mortality by urban/rural residence
Figure 6 presents results by urban/rural residence. Here also, there is broad agreement between the different data sources and methodologies, with the 21q3 series providing us with the longest times series. According to these corrected estimates, infant mortality in urban areas remains systematically lower than in rural areas, both before and after 1991, and the cross-over disappears. This is consistent with expectations of urban/rural differentials, and supports the hypothesis that the urban/rural cross-over in the registered data is artifactual. Similarly, these results indicate that the underestimation of infant mortality in the reported data is much larger in the rural areas. This is also consistent with expectations. We also observe in the corrected estimates that the stalling of mortality decline in the 1990s occurs in both urban and rural areas.
Figure 6.
Comparison of various infant mortality rate (IMR) estimates by urban/rural residence, Kyrgyzstan, 1980–2010
Source: Various primary data sources (see text for details).
Infant mortality by ethnicity
Corrected IMR estimates by ethnicity are shown in Figure 7. Ethnic-specific deaths by month of age were only available for the years 1996–2000, so unfortunately the 21q3 adjustment is presented only for those years, and we lack corrected estimates altogether for recent years. Nonetheless, for the years covered by these estimates, we find that infant mortality remains consistently higher among Central Asians. There is no evidence that the ethnic differential has narrowed over time. Also, the gap between reported and corrected estimates is much larger among Central Asians, indicating that the amount of mortality underestimation in the reported data is greater among them.
Figure 7.
Comparison of various infant mortality rate (IMR) estimates by ethnicity, Kyrgyzstan, 1980–2010
Source: Various primary data sources (see text for details).
The impact of the change of standard for classifying live births
One premise of our correction based on 21q3 is that it should largely correct for the bias arising from differences in the definition of a live birth. Therefore, if the increase in the IMR between 2003 and 2005 is due to this change of definition, and if the premise of our correction is adequate, no increase in the 21q3-based IMR estimates should be observed, and differences between reported and corrected IMRs should decrease during that period.
Figure 5 confirms that this is indeed the case. In fact starting in 2005 there is virtually no difference between the reported and 21q3-adjusted IMRs. The impact of the adoption of the WHO standard also appears in Figure 3, which shows, as expected, that most of the increase in reported mortality below age one between 2003 and 2005 takes place below age one month. Changes in age heaping around the age of 12 months plays a negligible role in this increase, because the scale of heaping has gradually decreased since the early 1980s, and also because mortality around the age of 12 months has substantially declined, reducing the impact on the IMR of any remaining age heaping.
A puzzling pattern following the change in definition, though, is that the reported increase in 2003–2005 is much larger in urban areas than in rural areas, as shown in Figure 2 (left panel). This is puzzling, because in theory the impact of the change in definition should not be so different in various population subgroups. Interestingly, in Figure 2 (right panel), Slavs and Central Asians happen to be equally affected by this definitional change. This makes the urban/rural comparison even more puzzling; since Slavs live predominantly in urban areas and Central Asians live predominantly in rural areas, there should be some parallel between the patterns by urban/rural residence and the patterns by ethnicity. In this case, patterns by ethnicity are consistent with expectations, while patterns by residence are not.
We mentioned earlier that urban/rural comparisons are likely to be confounded in part by misreporting of residence on birth and death certificates. The extent of this phenomenon, however, has never been fully explored. The comparison of reported and 21q3-adjusted IMRs in urban and rural areas for the period 2003–2005, shown in Figure 6, confirms the existence of this problem in the case of Kyrgyzstan. Following the change of definition, the reported IMR in urban areas exhibits a large increase, to the point that it reaches a level above the one that we predict on the basis of 21q3. In rural areas, however, the reported IMR increases only slightly and remains significantly below the corrected ones. At the national level, however, no such pattern occurs – the increase in the reported IMR is large but does not go above the corrected level, which is what we expect given the change of definition. A plausible explanation for this overreporting of infant mortality in urban areas (relative to what is predicted on the basis of 21q3), while underreporting remains large in rural areas, is that many rural deaths are misreported as urban deaths.
It is likely that this misreporting of residence in the registration data occurred before 2004 as well. It does not appear as clearly during these years, because, with the old standard of live births vs. stillbirths, the reported IMR in urban areas is sufficiently underestimated to remain lower than the 21q3-adjusted IMR, even with the additional misclassified rural deaths. In fact, given the role played by differences in definition, we would expect the gap between reported and corrected rates to be somewhat larger, in the absence of this misreporting of residence, before 2004 in urban areas (Figure 6). Interestingly, the gap between reported and corrected IMRs suddenly decreases in urban areas during the early 1990s (a pattern that does not appear in the national data). It is quite likely that the misclassification of rural deaths as urban deaths worsened in the early 1990s, contributing to the observed cross-over and the implausible excess infant mortality in urban areas during the post-Soviet period.
Using data for the period 2006-10, we estimate that about 36% of actual rural infant deaths are misclassified as occurring in urban areas. This estimate is based on the assumption that, in the absence of misclassification, the rural/urban IMR ratio in the reported data would be equal to the rural/urban ratio in the 21q3-adjusted IMR for that time period.
It is also noteworthy that the 21q3-adjusted IMR estimates present a surprising stagnation between the years 2004 and 2007, both at the national level and by residence. It is possible that the adoption of the WHO standard has had an impact on the quality of vital registration data beyond the mere issue of classifying live births and still births, and that following this change of standard the overall coverage of death registration improved, generating a spurious stagnation in infant mortality.
Final IMR estimates at the national level
While the 21q3 adjustment provides us with the most informative time series, we recognize that this procedure is still subject to underestimation as a result of possible undercount of deaths in the age range 3.0–24.0 months. Therefore, the near perfect agreement between the reported and 21q3-adjusted IMR for the years 2005–2010 in Figure 5 should not be interpreted as an indication that the reported IMR information is now perfectly accurate in Kyrgyzstan.
We have little information to provide a correction for such undercount. However, one reason for the fact that the DHS estimates are a bit higher than the 21q3 adjustment for the years when they overlap is probably that the reported levels of 21q3, which is the basis for the 21q3 adjustment, are probably still somewhat underestimated. Therefore, we made a final adjustment in the national level estimates, such that the average corrected IMR for the period 1982–1997 matches the DHS-based average for that period (i.e., the 15-year period prior to the survey). This produces an adjustment factor of 1.129, which we apply to the entire series of 21q3-based IMR estimates. This appears to be a reasonable combination of the useful information respectively contained in these two sources. (Although the amount of underestimation in 21q3 may have changed in recent years, we lack a recent source of information for this evaluation.) This adjustment produces our final and preferred adjusted IMR estimates for the period 1980–2010. These final estimates, which are included in Figure 5, are also presented in Table 1, along with other IMR estimates.
Table 1.
Reported and adjusted infant mortality rate (IMR), Kyrgyzstan, 1980–2010
| Infant Mortality Rate (IMR), per 1,000 |
|||
|---|---|---|---|
| Year | Registration |
21q3-based adjustment |
Final estimates |
| 1980 | 43.3 | n/a1 | n/a1 |
| 1981 | 40.3 | 71.5 | 80.7 |
| 1982 | 38.6 | 63.0 | 71.1 |
| 1983 | 39.7 | 67.7 | 76.4 |
| 1984 | 40.3 | 66.5 | 75.0 |
| 1985 | 41.6 | 66.8 | 75.4 |
| 1986 | 37.6 | 61.9 | 69.9 |
| 1987 | 37.5 | 62.7 | 70.8 |
| 1988 | 37.0 | 60.6 | 68.4 |
| 1989 | 32.4 | 50.5 | 57.1 |
| 1990 | 30.2 | 47.2 | 53.3 |
| 1991 | 29.7 | 43.7 | 49.3 |
| 1992 | 31.6 | 47.3 | 53.4 |
| 1993 | 32.9 | 51.5 | 58.1 |
| 1994 | 29.6 | 49.0 | 55.4 |
| 1995 | 27.7 | 47.1 | 53.2 |
| 1996 | 26.6 | 44.5 | 50.2 |
| 1997 | 28.6 | 49.7 | 56.2 |
| 1998 | 26.0 | 47.3 | 53.4 |
| 1999 | 22.7 | 42.7 | 48.2 |
| 2000 | 23.0 | 40.2 | 45.4 |
| 2001 | 21.6 | 35.6 | 40.2 |
| 2002 | 21.1 | 32.7 | 36.9 |
| 2003 | 20.7 | 31.0 | 35.0 |
| 2004 | 25.6 | 28.8 | 32.6 |
| 2005 | 29.7 | 29.6 | 33.4 |
| 2006 | 29.2 | 29.2 | 33.0 |
| 2007 | 30.6 | 29.6 | 33.4 |
| 2008 | 27.1 | 26.2 | 29.5 |
| 2009 | 25.0 | 24.8 | 28.0 |
| 2010 | 22.8 | 23.3 | 26.3 |
Source: Official registration data.
The data needed for calculating 21q3 were not available in 1980. Therefore our adjusted series starts in 1981.
Discussion
We can summarize our findings as follows. First, we confirm the large underestimation of the IMR in the registration data due to a combination of errors. The national-level reported IMR is systematically lower than the adjusted one. Comparing the final estimates to registration estimates in Table 1, we find that, for the period 1980–2010, the reported IMR is 41% lower, on average, than the corrected IMR. However, we also find that the amount of mortality underestimation has varied greatly overtime. While we detect improvements in the registration data in the 1980s, we find a deterioration in the 1990s, following the break-up of the Soviet Union. As a result of these patterns of errors, we find that the reported decreases in infant mortality in the 1990s are spurious, and that in reality, infant mortality abruptly stalled following the break-up of the Soviet Union. We estimate that actual decreases in infant mortality resumed only in 1999. However, we find no evidence for a large surge in infant mortality in the 1990s.
Second, we find that the amount of underestimation in the reported data is disproportionately large in rural areas and among Central Asian ethnic groups. Consistently with these patterns of errors, we find that the reported cross-over between urban and rural areas is spurious, likely due to greater undercount in rural areas, as well as misreporting of residence. In reality, we find that the actual IMR stays consistently higher in rural areas during the period. Similarly, we find that the reported decrease in the gap between Slavs and Central Asians is spurious. Our estimates indicate that the actual IMR stays consistently higher among Central Asians.
Third, we find that the quality of the reported data has improved recently, following the adoption in 2004 of the international standard for classifying live births and stillbirths. Nonetheless, some underestimation is probably still taking place. Comparing estimates in Table 1, we estimate that, for the 2006–2010 period, the reported IMR is still lower than the true values by about 11%, on average. In spite of these improvements, misclassification of urban/rural residence continues to generate spurious urban/rural comparisons. We estimate that, in 2006–2010, about 36% of actual rural infant deaths are misclassified as occurring in urban areas.
The implication of these findings is that health policy would be largely misguided if it was based on the reported levels and trends. Infants of Central Asian ethnicity or born in rural areas remain considerably more at risk, contrary to what the reported levels indicate. Resources should be allocated or reallocated to address these differentials.
In light of these findings, it is useful to contrast mortality patterns in Kyrgyzstan with those observed in Russia. As we said in the introduction, the health crisis in Russia has been characterized by a large surge in mortality at adult ages, while infant mortality remained low and continued declining. These patterns, together with information on causes of deaths, have led researchers to emphasize the role of adult behaviors, such as alcohol consumption and violence, and to relate these behaviors to the stark decline in the country’s economic and social conditions (Shkolnikov et al. 1998). In the case of Kyrgyzstan, a much poorer country where the economic crisis has been even more severe than in Russia, adult mortality has paradoxically exhibited stronger resilience, in part because of cultural differences influencing patterns of alcohol consumption (Guillot et al. 2011). However, this conclusion does not hold for children. Our corrected estimates show that the relative gap in infant mortality between Russia and Kyrgyzstan remains more or less constant during the 1990s, as both countries experience a stalling of progress. In Kyrgyzstan and other Central Asian republics, access to health care (which was virtually free during the Soviet period), became more expensive during the 1990s, due to increases in both official costs and under-the-table costs. This happened during a period when poverty levels increased dramatically, leaving many unable to afford health care (Falkingham 2002). At the same time, quality of care declined substantially (McKee, Healy, and Falkingham 2002). In view of these changes, it is not surprising that infant mortality stalled, rather than declined, in the 1990s. However, as said earlier, we find no evidence for a large surge in infant mortality in Kyrgyzstan in the 1990s. As in Russia, reported declines in life expectancy in Kyrgyzstan are mostly due to mortality increases at adult ages, even after accounting for the underestimation of infant mortality.
While this paper deals with Kyrgyzstan only, our findings have some implications for other Central Asian republics as well. Indeed, many of the patterns found in the registration data in Kyrgyzstan are also present in the reported data in other Central Asian republics. For example, reported infant mortality has declined in all Central Asian republics during the 1990s. In the case of Uzbekistan, an analysis of the DHS data questions the veracity of these declines and even suggests the possibility of increases in the 1990s (Hohmann and Garenne 2005). In view of these results, declines in reported infant mortality in Kazakhstan, Tajikistan, Turkmenistan in the 1990s should also be regarded with much doubt.
This paper also has some methodological implications. In spite of the deficiencies in the vital registration sources, the most informative findings come from a procedure that uses vital registration data. Indirect methods and survey data are useful and provide broad indications of levels, but they often fail to provide precise information on short-term trends and differentials. Vital registration data remain underused in many less-developed countries, in part because they are more difficult to access, but also because of the premise that they are too unreliable to be used as a basis for mortality estimation. This premise, while true in many populations, does not apply to all less-developed contexts. Our study of the different data sources in Kyrgyzstan shows that, while the registration data have a number of deficiencies, the extent of errors varies substantially by age and population subgroup. With this more nuanced evaluation, we believe that much can be learned about real mortality patterns from official registration data.
Acknowledgments
We would like to thank Zarylbek Kudabaev, former chairman of the National Statistical Committee (NSC) of the Kyrgyz Republic, and Orozmat Abdykalykov, its current chairman, for giving us access to much of the data used in this paper. We are also grateful to Larissa Mimbaeva and Elena Komandirova for supervising the data collection in Kyrgyzstan. Jane Falkingham provided useful comments on an earlier draft. This project was supported by grants from NICHD, R03 HD38752 and R01 HD045531.
Contributor Information
Michel Guillot, University of Pennsylvania, USA.
So-jung Lim, University of Wisconsin-Madison, USA.
Liudmila Torgasheva, National Statistical Committee of the Kyrgyz Republic.
Mikhail Denisenko, Higher School of Economics, Moscow, Russia.
References
- Abdullah S, Adazu K, Masanja H, Diallo D, Hodgson A, Ilboudo-Sanogo E, Nhacolo A, Owusu-Agyei S, Thompson R, Smith T, Binka FN. Patterns of age-specific mortality in children in endemic areas of sub-Saharan Africa. American Journal of Tropical Medicine and Hygiene. 2007;77(Suppl 6):99–105. [PubMed] [Google Scholar]
- Ackland R, Falkingham J. A profile of poverty in Kygyzstan. In: Falkingham J, Klugman J, Marnie S, Micklewright J, editors. Household Welfare in Central Asia. Houndmills, Basingstoke [England]: Macmillan Press; 1997. pp. 81–99. New York, St. Martin’s Press. [Google Scholar]
- Aleshina N, Redmond G. How high is infant mortality in central and eastern Europe and the commonwealth of independent states? Population Studies. 2005;59(1):39–54. doi: 10.1080/0032472052000332692. [DOI] [PubMed] [Google Scholar]
- Anderson BA. Russia faces depopulation? Dynamics of population decline. Population and Environment. 2002;23(5):437–464. [Google Scholar]
- Anderson BA, Silver Brian D. Infant mortality in the Soviet Union: regional differences and measurement issues. Population and Development Review. 1986;12(4):705–738. [Google Scholar]
- Anderson BA, Silver Brian D. Issues of data quality in assessing mortality trends and levels in the New Independent States. In: Bobadilla José Luis, Costello Christine A, Mitchell Faith., editors. Premature Death in the New Independent States. Washington: National Academy Press; 1997. pp. 120–155. [Google Scholar]
- Anderson BA, Silver Brian D. The geodemography of infant mortality in the Soviet Union, 1950–1990. In: Demko GJ, Ioffe G, Zayonchkovskaya Zh, editors. Population Under Duress: The Geodemography of Post-Soviet Russia. Boulder: Westview Press; 1999. pp. 73–103. [Google Scholar]
- Becker Charles M, Bibosunova Damira I, Holmes Grace E, Ibragimova Margarita M. Maternal care vs. economic wealth and the health of newborns: Bishkek, Kyrgyz Republic and Kansas City, USA. World Development. 1998;11:2057–2072. [Google Scholar]
- Bocquier P, Madise N, Zulu E. Is there an urban advantage in child survival in sub-Saharan Africa? Evidence from 18 countries in the 1990s. Demography. 2011;48(2):531–558. doi: 10.1007/s13524-011-0019-2. [DOI] [PubMed] [Google Scholar]
- Brainerd R. Market Reform and Mortality in Transitions Economics. World Development. 2007;26:2013–2027. [Google Scholar]
- Chen L, Wittgenstein F, McKeon E. The upsurge of mortality in Russia: causes and policy implications. Population and Development Review. 1996;22(3):517–530. [Google Scholar]
- Cornia GA, Paniccia R. The mortality crisis in transitional economies. Oxford: Oxford University Press; 2000. [Google Scholar]
- Davis C, Feshbach M. Rising Infant Mortality in the U.S.S.R. in the 1970’s. Washington, DC: US Bureau of the Census; 1980. Series P-95, No 74. [Google Scholar]
- Delaunay V, Etard JF, Préziosi MP, Marra A, Simondon F. Decline of infant and child mortality rates in rural Senegal over a 37-year period (1963–1999) International Journal of Epidemiology. 2001;30:1286–1293. doi: 10.1093/ije/30.6.1286. [DOI] [PubMed] [Google Scholar]
- Duthé G, Badurashvili I, Kuyumjyan K, Meslé F, Vallin J. Mortality in the Caucasus: An attempt to re-estimate recent mortality trends in Armenia and Georgia. Demographic Research. 2010;22(23):691–732. [Google Scholar]
- Eberstadt Nick. The health crisis in the USSR. New York Review of Books. 1981;28(2):23–31. [Google Scholar]
- Falkingham J. Poverty, affordability and access to health care. In: McKee M, Healy J, Falkingham J, editors. Health Care in Central Asia. Open University Press; 2002. pp. 42–56. [Google Scholar]
- Garenne Michel. Variations in the Age Pattern of Infant and Child Mortality with Special Reference to a Case Study in Ngayokheme (Rural Senegal) 1982 Ph.D. dissertation (University of Pennsylvania) [Google Scholar]
- Guillot Michel. Mortality in Kyrgyzstan since 1959: real patterns and data artifacts. Espace-Populations-Sociétés. 2007;1:113–126. [Google Scholar]
- Guillot M, Gavrilova N, Pudrovska T. Understanding the ‘Russian mortality paradox’ in Central Asia: evidence from Kyrgyzstan. Demography. 2011;48:1081–1104. doi: 10.1007/s13524-011-0036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakobyan M, Yepiskoposyan L. Infant mortality in Armenia, 1992–2003. Economics & Human Biology. 2006;4(3):351–358. doi: 10.1016/j.ehb.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Hohmann S, Garenne M. Enjeu politique des indicateurs de santé en Ouzbékistan soviétique et post-soviétique: l’exemple de la mortalité infantile; Paper presented at the XV IUSSP International Population Conference; Tours, France. 2005. Jul 18–23, 2005. [Google Scholar]
- Kahn M. Les russes dans les ex-républiques soviétiques. Le Courrier des Pays de l’Est. 1993;376:3–20. [Google Scholar]
- Kingkade W. Ward, Arriaga Eduardo E. Mortality in the New Independent Sates: patterns and impacts, in. In: Bobadilla José Luis, Costello Christine A, Mitchell Faith., editors. Premature Death in the New Independent States. Washington: National Academy Press; 1997. pp. 156–183. [Google Scholar]
- Ksenofontova N. Trends in infant mortality in the USSR. In: Lutz Wolfgang, Sherbov Sergei, Volkov Andrei., editors. Demographic Trends and Patterns in the Soviet Union Before 1991. London: Routledge; 1994. pp. 359–378. [Google Scholar]
- Macro International. Kyrgyz Republic Demographic and Health Survey. Calverton, Maryland; 1998. [Google Scholar]
- Marinda E, Humphrey JH, Iliff PJ, Mutasa K, Nathoo K, Piwoz EG, Moulton L, Salama P, Ward B, and the ZVITAMBO Study Group Child mortality according to maternal and infant HIV status in Zimbabwe. The Pediatric Infectious Disease Journal. 2007;26(6):519–526. doi: 10.1097/01.inf.0000264527.69954.4c. [DOI] [PubMed] [Google Scholar]
- McKee M, Healy J, Falkingham J. Poverty Health care systems in the Central Asian republics: an introduction. In: McKee M, Healy J, Falkingham J, editors. Health care in central Asia. Open University Press; 2002. pp. 3–11. [Google Scholar]
- Meslé F, Shkolnikov VM, Hertrich V, Vallin J. Tendances récentes de la mortalité en Russie par cause. Paris: INED; 1996. [Google Scholar]
- Meslé France, Vallin Jacques. Mortality and Causes of Death in 20th-Century Ukraine. Springer; 2012. p. 279. Demographic Research Monographs. [Google Scholar]
- Penina O, Meslé F, Vallin J. Correcting for under-estimation of infant mortality in Moldova. Population-E. 2010;65(3):499–514. [Google Scholar]
- Pison G, Langaney A. The level and age pattern of mortality in Bandafassi (Eastern Senegal): results from a small-scale and intensive multi-round survey. Population Studies. 1985;39:387–405. [Google Scholar]
- Preston SH, Haines M. Fatal Years: Child Mortality in Late Nineteenth-Century America. Princeton: Princeton University Press; 1991. [Google Scholar]
- Preston SH, Heuveline P, Guillot M. Demography: Measuring and Modeling Population Processes. London: Blackwell; 2001. [Google Scholar]
- Sankoh Osman A, Ngom Pierre, Clark Samuel J, Don de Savigny , Binka Fred. Levels and patterns of mortality at INDEPTH demographic surveillance sites. In: Feachem R, Jamison D, Makgoba WM, Rogo K, Hofman K, Bos E, editors. Disease and Mortality in sub-Saharan Africa. 2nd Edition. Oxford: Oxford University Press, for the World Bank; 2006. [PubMed] [Google Scholar]
- Shkolnikov VM, Cornia GA, Leon DA, Meslé F. Causes of the Russian mortality crisis. World Development. 1998;26:1995–2011. [Google Scholar]
- Shkolnikov VM, Andreev EM, Leon DA, McKee M, Meslé F, Vallin J. Mortality Reversal in Russia: The story so far. Hygiea Internationalis. 2004;4(1):29–80. [Google Scholar]
- Stuckler D, King L, McKee M. Mass privatization and the post-communist mortality crisis: a cross-national analysis. Lancet. 2011;373:399–407. doi: 10.1016/S0140-6736(09)60005-2. [DOI] [PubMed] [Google Scholar]
- United Nations. Levels and trends of mortality since 1950. New York: United Nations; 1982. [Google Scholar]
- Vallin J, Meslé F. Trends in mortality in Europe since 1950: Age-, sex-, and cause-specific mortality. In: Vallin J, Meslé F, Valkonen T, editors. Trends in Mortality and Differential Mortality. Strasbourg, France: Council of Europe Publishing; 2001. pp. 31–186. [Google Scholar]
- Velkoff VA, Miller JE. Trends and differentials in infant mortality in the Soviet Union, 1970-90: how much is due to misreporting? Population Studies. 1995;49(2):241–58. doi: 10.1080/0032472031000148496. [DOI] [PubMed] [Google Scholar]
- World Bank. Kyrgyz Republic: Update on Poverty in the Kyrgyz Republic. Washington, D.C: The World Bank; 1999. Report No. 19425-KG. [Google Scholar]
- World Bank. Kyrgyz republic Poverty Assessment. Washington, D.C: The World Bank; 2007. Report No. 40864-KG. [Google Scholar]