Abstract
BACKGROUND
The Food and Drug Administration Amendments Act (FDAAA) mandates timely reporting of results of applicable clinical trials to ClinicalTrials.gov. We characterized the proportion of applicable clinical trials with publicly available results and determined independent factors associated with the reporting of results.
METHODS
Using an algorithm based on input from the National Library of Medicine, we identified trials that were likely to be subject to FDAAA provisions (highly likely applicable clinical trials, or HLACTs) from 2008 through 2013. We determined the proportion of HLACTs that reported results within the 12-month interval mandated by the FDAAA or at any time during the 5-year study period. We used regression models to examine characteristics associated with reporting at 12 months and throughout the 5-year study period.
RESULTS
From all the trials at ClinicalTrials.gov, we identified 13,327 HLACTs that were terminated or completed from January 1, 2008, through August 31, 2012. Of these trials, 77.4% were classified as drug trials. A total of 36.9% of the trials were phase 2 studies, and 23.4% were phase 3 studies; 65.6% were funded by industry. Only 13.4% of trials reported summary results within 12 months after trial completion, whereas 38.3% reported results at any time up to September 27, 2013. Timely reporting was independently associated with factors such as FDA oversight, a later trial phase, and industry funding. A sample review suggested that 45% of industry-funded trials were not required to report results, as compared with 6% of trials funded by the National Institutes of Health (NIH) and 9% of trials that were funded by other government or academic institutions.
CONCLUSIONS
Despite ethical and legal obligations to disclose findings promptly, most HLACTs did not report results to ClinicalTrials.gov in a timely fashion during the study period. Industry-funded trials adhered to legal obligations more often than did trials funded by the NIH or other government or academic institutions.
The human experimentation that is conducted in clinical trials creates ethical obligations to make research findings publicly available. However, there are numerous historical examples of potentially harmful data being withheld from public scrutiny and selective publication of trial results.1–3 In 2000, Congress authorized the creation of the ClinicalTrials.gov registry to provide information about and access to clinical trials for persons with serious medical conditions. In 2007, Section 801 of the Food and Drug Administration Amendments Act (FDAAA) expanded this mandate by requiring sponsors of applicable clinical trials to register and report basic summary results at ClinicalTrials.gov.4 Such trials generally include all non–phase 1 interventional trials of drugs, medical devices, or biologics that were initiated after September 27, 2007, or before that date but that were still ongoing as of December 26, 2007, have at least one U.S. research site, or are conducted under an investigational-new-drug application or an investigational-device exemption.5 The FDAAA also mandates that trial results be reported by the sponsor within 1 year after the completion of data collection for the prespecified primary outcome (primary completion date) or within 1 year after the date of early termination, unless legally acceptable reasons for the delay are evident.5
Studies have shown that compliance with the FDAAA provisions is generally poor,6–12 despite a growing consensus favoring transparent, public reporting of human trials — an enterprise whose ethical justification rests on the creation of generalizable scientific knowledge.13,14 More than 5 years after the FDAAA was enacted, we sought to determine which trial characteristics have been associated with reporting, as well as the timing of that reporting.
METHODS
DATA SOURCES
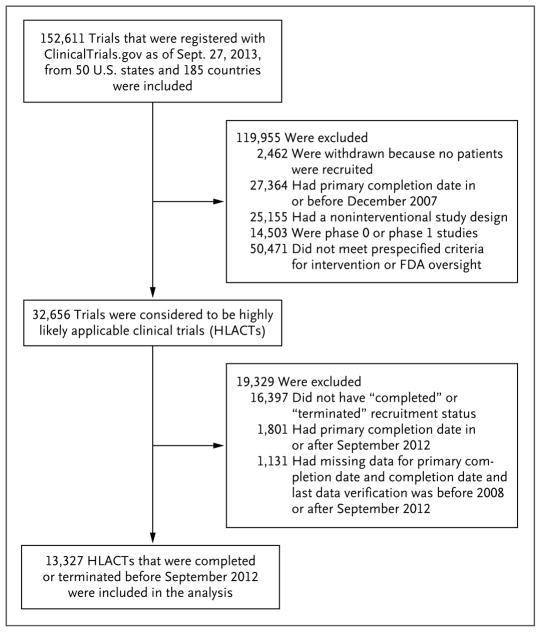
Because we could not precisely identify which applicable clinical trials are subject to FDAAA provisions using publicly available data, we used an algorithm that is based on input from the National Library of Medicine (Zarin D: personal communication) to identify 32,656 highly likely applicable clinical trials (HLACTs) from among all registered trials (Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). We further restricted our study to HLACTs with a recruitment status of “completed” or “terminated” before August 31, 2012, to allow at least 1 year of reporting for trials with a primary completion date of September 2012. We excluded 1131 trials for which dates of trial completion could not be determined and for which the date of the last data verification was either before 2008 (1078 trials) or after September 2012 (53 trials). Our final study population included 13,327 HLACTs that had been either completed or terminated between January 1, 2008, and August 31, 2012 (Fig. 1). To estimate rates of false positive and false negative findings, we also conducted a manual review of random samples of HLACTs and non-HLACTs (see Tables S15A and S15B in the Supplementary Appendix for details).
Figure 1. Clinical Trials Included in the Study.
If data regarding the date for the completion of data collection for the pre-specified primary outcome (primary completion date) were missing, the completion year was used. FDA denotes Food and Drug Administration.
To determine whether a product or indication was approved by the FDA (and if approved, the approval date), we searched Drugs@FDA, the National Drug Code Directory (for generics and supplements), the 510(k) Premarket Notification database (for devices), the Premarket Approval database (for devices), and Biologic Approvals by Year database and also conducted Web searches when necessary. Two of the authors manually reviewed uncertain cases to provide high and low estimates for false positives and false negatives.
DEFINITIONS
We specified that clinical trials had reported results if at least one primary outcome was provided. We calculated the time to reporting as the number of months from the primary completion date of the trial until the date that results were first reported to ClinicalTrials.gov. The primary completion date was defined as the date that the final trial participant was examined or received an intervention for the purpose of final data collection for the primary outcome. If the primary completion date was missing, the study completion year was used. If the study completion year was missing, the study verification date was used. We categorized a trial as having a legally acceptable period of delay to the reporting of results if a certification or extension request (as described below) was received by September 27, 2013.
A responsible party could delay the 12-month deadline for submitting results through several mechanisms, including submission of a “certification of initial use” to ClinicalTrials.gov if the medical product being studied had not been approved for market at the time of trial completion. In this case, results must be submitted 30 days after the product is approved. A “certification of new use” may be submitted if a sponsor intends to seek FDA approval, clearance, or licensure of a new use of an approved medical product. In this case, reporting may be delayed for up to 2 years or for 30 days after the FDA determines approval status or issues a complete response letter or the application is withdrawn.6 Extensions can be requested to delay the reporting of results for good cause. Data on trials that submit certification or extension requests to ClinicalTrials.gov were provided by the National Library of Medicine (Tse T: personal communication).
Trial characteristics included the type of intervention, study phase, funding source, oversight authorities, enrollment characteristics, site locations, purpose, and study-design descriptors.15–17 (Details are provided in the Supplementary Appendix.)
STATISTICAL ANALYSIS
We summarized trial characteristics overall and by the presence or absence of basic reporting of results. We also summarized the existence of a certification or extension request for a delay in results reporting. Categorical variables are reported as frequencies and percentages, and continuous variables as medians and interquartile ranges. Unless otherwise noted, missing values were excluded from the analyses.
We used the Kaplan–Meier method to estimate the cumulative percentage of trials that reported results at monthly intervals from the primary completion date, with data censored on September 27, 2013. Estimates were stratified according to funding source, trial phase, intervention, and trial status (terminated vs. completed).
We used multivariable regression modeling to examine factors associated with the time to reporting. Models included 12 prespecified trial characteristics: primary purpose, intervention group, phase, FDA oversight, funding source, total enrollment, completion status (terminated vs. completed), primary completion year, study duration, number of study groups, randomized treatment assignment, and study masking technique. Two time points were specified: reporting within 12 months after study completion and reporting within 5 years. We used logistic regression to determine factors that were associated with reporting within 12 months and Cox regression to determine factors that were associated with reporting within 5 years. Adjusted odds ratios with Wald 95% confidence intervals were reported for the logistic regression; adjusted hazard ratios with 95% confidence intervals were reported for the Cox model. In the regression analyses, we calculated P values using Wald chi-square statistics to identify unexpectedly large differences and associations. However, because of the large sample size and the number of effects tested, only differences with both large practical importance and statistical significance at the 0.001 level are highlighted in the text.
To evaluate the effect of accounting for trials with known exceptions to reporting requirements, we conducted alternative logistic-regression and Cox regression analyses (see the Supplementary Appendix for details). Statistical analyses were performed at the Duke Clinical Research Institute with the use of SAS software, version 9.2 (SAS Institute).
RESULTS
TRIAL POPULATION
Of the 13,327 HLACTs that we reviewed during the study period, 1790 (13.4%) reported results within 12 months after trial completion, and 5110 (38.3%) reported results at any time during the 5-year study period (Table 1, and Table S2 in the Supplementary Appendix). In contrast, among the 25,646 non-HLACTs, only 1287 (5.0%) reported results within 12 months, and 2473 (9.6%) reported results at any time during the 5-year study period (Table S3 in the Supplementary Appendix).
Table 1.
Characteristics of Clinical Trials That Were Completed or Terminated before September 2012.*
| Characteristic | All Trials (N = 13,327) | Trials with Results Reported by 12 Mo (N = 1790) | Trials with Results Reported by 5 Yr (N = 5110) |
|---|---|---|---|
| Primary purpose of trial — no./total no. (%) | |||
| Treatment | 10,930/12,884 (84.8) | 1509/1735 (87.0) | 4244/4954 (85.7) |
| Prevention | 990/12,884 (7.7) | 133/1735 (7.7) | 393/4954 (7.9) |
| Other† | 964/12,884 (7.5) | 93/1735 (5.4) | 317/4954 (6.4) |
| Intervention group — no. (%) | |||
| Drug | 10,309 (77.4) | 1412 (78.9) | 3992 (78.1) |
| Biologic | 1,185 (8.9) | 168 (9.4) | 492 (9.6) |
| Device | 1,586 (11.9) | 198 (11.1) | 581 (11.4) |
| Other‡ | 247 (1.9) | 12 (0.7) | 45 (0.9) |
| Phase — no. (%) | |||
| 1–2 | 867 (6.5) | 64 (3.6) | 239 (4.7) |
| 2 | 4,917 (36.9) | 466 (26.0) | 1634 (32.0) |
| 2–3 | 333 (2.5) | 20 (1.1) | 105 (2.1) |
| 3 | 3,117 (23.4) | 646 (36.1) | 1512 (29.6) |
| 4 | 1,928 (14.5) | 393 (22.0) | 919 (18.0) |
| Not applicable | 2,165 (16.2) | 201 (11.2) | 701 (13.7) |
| U.S. site — no. (%) | 11,947 (89.6) | 1652 (92.3) | 4721 (92.4) |
| U.S. FDA oversight — no. (%) | 8,640 (64.8) | 1362 (76.1) | 3449 (67.5) |
| Funding source — no. (%)§ | |||
| Industry | 8,736 (65.6) | 1483 (82.8) | 3624 (70.9) |
| NIH | 1,899 (14.2) | 153 (8.5) | 739 (14.5) |
| Other government or academic institution | 2,692 (20.2) | 154 (8.6) | 747 (14.6) |
| Recruitment completed — no. (%) | 11,128 (83.5) | 1521 (85.0) | 4286 (83.9) |
| Primary completion year — no. (%)¶ | |||
| 2008 | 3,142 (23.6) | 370 (20.7) | 1372 (26.8) |
| 2009 | 3,051 (22.9) | 373 (20.8) | 1407 (27.5) |
| 2010 | 2,853 (21.4) | 403 (22.5) | 1154 (22.6) |
| 2011 | 2,686 (20.2) | 418 (23.4) | 888 (17.4) |
| 2012 | 1,595 (12.0) | 226 (12.6) | 289 (5.7) |
Percentages may not total 100 because of rounding. FDA denotes Food and Drug Administration, and NIH National Institutes of Health.
Other primary purposes include diagnostic, screening, supportive care, health services research, and basic science.
Other interventions include radiation and genetics trials.
The funding source was derived from data about the lead sponsor and collaborators.
If data regarding the primary completion date were missing, the year of study completion was used. If the year of study completion was also missing, the verification date was used.
In our study cohort, the primary purpose was identified as treatment by 84.8% of the trials, prevention by 7.7%, and “other” (which included diagnostic, screening, supportive care, health services research, and basic science) by 7.5%. Trials were categorized according to their interventions, with drugs studied in 77.4% of the trials, devices in 11.9%, biologics in 8.9%, and “other” (including radiation and genetics) in 1.9%. The largest funding source was industry (65.6%); the National Institutes of Health (NIH) funded 14.2% of trials, and other government or academic institutions funded the remaining 20.2% (Table 1). Components of basic summary results are listed in Table S4 in the Supplementary Appendix.
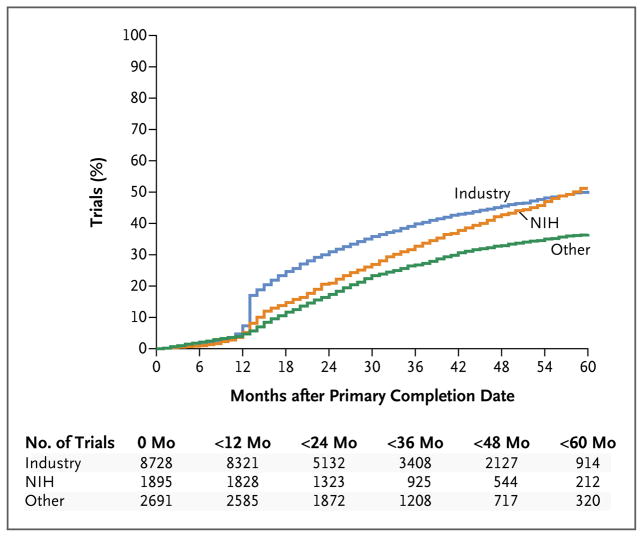
RATES OF REPORTING
At 12 months, results had been reported for 17.0% of trials that were funded by industry, 8.1% of trials funded by the NIH, and 5.7% of trials funded by other government or academic institutions. At 5 years, results had been reported by 41.5% of trials funded by industry, 38.9% of those funded by the NIH, and 27.7% of those funded by other government or academic institutions. Additional details of summary results reporting are provided in Tables S3 through S6 in the Supplementary Appendix.
By September 27, 2013, a total of 2100 of 13,327 HLACTs (15.8%) had submitted a certification or extension request to delay reporting to ClinicalTrials.gov. Of these HLACTs, 482 (23.0%) had reported results throughout the 5-year study period. At 12 months, 1790 of 13,314 trials (13.4%) that were evaluated had reported results and 818 (6.1%) had not reported results but had a legally acceptable delay because of a certification or an exemption request (Table 2). Phase 2 and phase 3 trials were more likely to have certification or exemption requests than were trials in other phases.
Table 2.
Reporting of Results to ClinicalTrials.gov.*
| Variable | All Trials (N = 13,327) | Industry Trials (N = 8736) | NIH Trials (N = 1899) | Other Trials (N = 2692) |
|---|---|---|---|---|
| Results reported by September 2013 — no. (%)† | 5110 (38.3) | 3624 (41.5) | 739 (38.9) | 747 (27.7) |
| Results reported by 12 mo after primary completion — no. (%) | 1790 (13.4) | 1483 (17.0) | 153 (8.1) | 154 (5.7) |
| Median mo until reporting of results (IQR)‡ | 17 (13–29) | 16 (13–26) | 23 (14–36) | 21 (14–30) |
| Trials with certification or extension request by September 2013 | ||||
| No. of trials (%) | 2100 (15.8) | 2015 (23.1) | 51 (2.7) | 34 (1.3) |
| Results reported by September 2013 — no./total no. (%) | 482/2100 (23.0) | 466/2015 (23.1) | 14/51 (27.5) | 2/34 (5.9) |
| Median mo until reporting of results (IQR)‡ | 26 (19–36) | 26 (19–36) | 26 (19–33) | 20 (16–23) |
| Trials without certification or extension requests by September 2013 | ||||
| No. of trials (%) | 11,227 (84.2) | 6721 (76.9) | 1848 (97.3) | 2658 (98.7) |
| Results reported by September 2013 — no./total no. (%) | 4628/11,227 (41.2) | 3158/6721 (47.0) | 725/1848 (39.2) | 745/2658 (28.0) |
| Median mo until reporting of results (IQR)‡ | 16 (13–27) | 14 (13–24) | 23 (14–36) | 21 (14–30) |
| Results reported or certification or extension request submitted by September 2013 — no. (%) | ||||
| No results reported and no certification or extension request submitted | 6599 (49.5) | 3563 (40.8) | 1123 (59.1) | 1913 (71.1) |
| No results reported but certification or extension request submitted | 1618 (12.1) | 1549 (17.7) | 37 (1.9) | 32 (1.2) |
| Results reported§ | 5110 (38.3) | 3624 (41.5) | 739 (38.9) | 747 (27.7) |
| Results reported or certification or extension request submitted by 12 mo after primary completion — no./total no. (%) | ||||
| No results reported and no certification or extension request submitted | 10,706/13,314 (80.4) | 6455/8728 (74.0) | 1719/1895 (90.7) | 2532/2691 (94.1) |
| No results reported but certification or extension request submitted | 818/13,314 (6.1) | 790/8728 (9.1) | 23/1895 (1.2) | 5/2691 (0.2) |
| Results reported§ | 1790/13,314 (13.4) | 1483/8728 (17.0) | 153/1895 (8.1) | 154/2691 (5.7) |
IQR denotes interquartile range.
The percentage of trials was not adjusted for differing lengths of time from the primary completion date until the database download in September 2013.
The median number of months was calculated for trials that had data regarding the primary completion date and the date that results were first posted at ClinicalTrials.gov. If the primary completion date was missing, then the completion date or the date when the record was last verified was used.
This category includes trials that reported results, including those that submitted certification or extension requests.
TIME TO RESULTS REPORTING
For trials with results, the median time to reporting for HLACTs was 17 months (interquartile range, 13 to 29) (Table 2). For the primary analysis, the median time to reporting was 16 months (interquartile range, 13 to 26) for industry-funded trials, 23 months (interquartile range, 14 to 36) for NIH-funded trials, and 21 months (interquartile range, 14 to 30) for other government or academic institutions (Table 2). After the exclusion of trials with certification or extension requests at any time in the secondary analysis, the median time to reporting decreased from 16 to 14 months for industry-funded trials but remained the same for NIH-funded trials and those funded by other government or academic institutions (Table 2).
REPORTING OVER TIME
Kaplan–Meier curves showing reporting of trial results during the 5-year study period according to funding source are provided in Figure 2. Industry-funded trials significantly led reporting for several years, but by 5 years, reporting rates of NIH-funded trials equaled those of industry-funded trials. Trials that were funded by other government or academic institutions had consistently lower rates of reporting over 5 years than did those funded by other sources (Fig. S1, S2, and S3 in the Supplementary Appendix).
Figure 2. Cumulative Percentage of Clinical Trials That Reported Results to ClinicalTrials.gov, According to the Time after the Primary Completion Date.
NIH denotes National Institutes of Health.
MULTIVARIABLE FACTORS ASSOCIATED WITH RESULTS REPORTING
Reporting within 12 Months
The factors that were most strongly associated with reporting by 12 months were funding source, trial phase, and FDA oversight (P<0.001 for all comparisons) (Table 3, and Table S7 in the Supplementary Appendix). As compared with NIH-funded trials, industry-funded trials were more likely to report results in a timely fashion (adjusted odds ratio, 1.62; 95% confidence interval [CI], 1.34 to 1.97), whereas trials that were funded primarily by other government or academic institutions were less likely to report on time (adjusted odds ratio, 0.58; 95% CI, 0.45 to 0.75). As compared with phase 4 trials, earlier-phase trials were significantly less likely to report on time, with an adjusted odds ratio of 0.28 (95% CI, 0.21 to 0.38) for phase 1–2 combination trials, 0.33 (95% CI, 0.27 to 0.39) for phase 2 trials, 0.22 (95% CI, 0.14 to 0.36) for phase 2–3 combination trials, 0.60 (95% CI, 0.50 to 0.71) for phase 3 trials, and 0.56 (95% CI, 0.45 to 0.70) for trials in which the phase was not applicable (e.g., trials of devices). Trials without FDA oversight were less likely to report on time than those with FDA oversight (adjusted odds ratio, 0.61; 95% CI, 0.52 to 0.71). Sensitivity analyses revealed similar associations (Tables S8 and S9 in the Supplementary Appendix).
Table 3.
Likelihood That Results of Clinical Trials Were Reported by 12 Months or 5 Years after the Primary Completion Date, According to Trial Characteristics.*
| Trial Characteristic | Results Reported by 12 Mo | Results Reported by 5 Yr |
|---|---|---|
| multivariable odds ratio (95% CI) | multivariable hazard ratio (95% CI) | |
| Type of intervention | ||
|
| ||
| Drug trial | 1.00 | 1.00 |
|
| ||
| Device trial | 0.88 (0.72–1.07) | 0.95 (0.86–1.06) |
|
| ||
| Biologic trial | 1.16 (0.95–1.44) | 1.17 (1.06–1.30) |
|
| ||
| Other | 0.48 (0.26–0.90) | 0.53 (0.39–0.71) |
|
| ||
| Trial phase | ||
|
| ||
| 4 | 1.00 | 1.00 |
|
| ||
| 1– 2 | 0.28 (0.21–0.38) | 0.46 (0.40–0.54) |
|
| ||
| 2 | 0.33 (0.27–0.39) | 0.54 (0.49–0.59) |
|
| ||
| 2–3 | 0.22 (0.14–0.36) | 0.54 (0.44–0.66) |
|
| ||
| 3 | 0.60 (0.50–0.71) | 0.80 (0.72–0.88) |
|
| ||
| Not applicable | 0.56 (0.45–0.70) | 0.71 (0.63–0.79) |
|
| ||
| FDA oversight | ||
|
| ||
| Yes | 1.00 | 1.00 |
|
| ||
| No | 0.61 (0.52–0.71) | 0.86 (0.80–0.93) |
|
| ||
| Funding source | ||
|
| ||
| NIH | 1.00 | 1.00 |
|
| ||
| Industry | 1.62 (1.34–1.97) | 0.97 (0.89–1.07) |
|
| ||
| Other government or academic institution | 0.58 (0.45–0.75) | 0.62 (0.56–0.70) |
|
| ||
| Trial terminated or completed | ||
|
| ||
| Completed | 1.00 | 1.00 |
|
| ||
| Terminated | 0.97 (0.83–1.11) | 0.94 (0.86–1.02) |
Data are for trials that were completed or terminated before September 2012. For trial results that were reported by 12 months after the completion or termination date, multivariable odds ratios were calculated by means of logistic regression. For results that were reported by 5 years, multivariable hazard ratios were calculated by means of Cox regression. Regression models included the following covariates in addition to those listed: primary purpose of study, enrollment, year of study completion, study duration, number of study groups, use of randomized assignment, and use of masking.
Reporting within 5 Years
Multivariable factors that were most strongly associated with results reporting during the 5-year study period included trial phase and funding source (P<0.001 for both comparisons) (Table 3, and Table S7 in the Supplementary Appendix). As compared with phase 4 trials, a stepwise decrease in reporting for phases was observed, with an adjusted hazard ratio of 0.46 (95% CI, 0.40 to 0.54) for phase 1–2 combination trials, 0.54 (95% CI, 0.49 to 0.59) for phase 2 trials, 0.54 (95% CI, 0.44 to 0.66) for phase 2–3 combination trials, and 0.80 (95% CI, 0.72 to 0.88) for phase 3 trials.
Industry-funded and NIH-funded trials were nearly equally likely to report results (adjusted hazard ratio, 0.97; 95% CI, 0.89 to 1.07) within 5 years, whereas trials that were funded by other government or academic institutions were less likely to report results than were NIH-funded trials (adjusted hazard ratio, 0.62; 95% CI, 0.56 to 0.70) (Table 3). After the exclusion of trials with certification or extension requests, a sensitivity analysis showed that industry-funded trials were more likely to report results within 5 years than were NIH-funded trials (Table S10 in the Supplementary Appendix). However, other sensitivity analyses that used a time-dependent covariate to account for whether reporting requirements were in effect did not change the primary finding that reporting rates over 5 years were similar for industry-funded and NIH-funded studies and were substantially lower for those funded by other government or academic institutions (Tables S11 through S14 in the Supplementary Appendix).
FINDINGS FROM SAMPLE REVIEW
We manually reviewed a sample of 205 HLACTs to determine requirements for reporting (Tables S15A and S15B in the Supplementary Appendix). By reviewing approval dates and labeling information, we determined that 44 to 45% of industry-funded HLACTs in this sample were not required to report results, as compared with 6% of NIH-funded studies and 9% of those funded by other government or academic institutions. On the basis of this review, we estimated that during the 5-year period, approximately 79 to 80% of industry-funded trials reported summary results or had a legally acceptable reason for delay. In contrast, only 49 to 50% of NIH-funded trials and 42 to 45% of those funded by other government or academic institutions reported results or had legally acceptable reasons for delay.
DISCUSSION
The reporting requirements of the FDAAA reflect the ethical obligation of researchers and sponsors to respect human trial participants through fidelity to commitments made explicit in informed consent: namely, to make results of trials available to contribute to generalizable knowledge.1,13,14,18 The FDAAA was designed to ensure timely disclosure of trial results3 and was enacted amid public concern that sponsors and investigators were selectively publishing trials that favored the interests of the sponsors and that journals were selectively reporting positive findings.1–3 However, we found that summary data are not publicly available at ClinicalTrials.gov for a majority of trials that are subject to FDAAA provisions.
Before the passage of the FDAAA, industry sponsors received particular scrutiny for selective reporting.2,3 Since the enactment of the law, many companies have developed disclosure policies and have actively pursued expanded public disclosure of data.19–22 Curiously, reporting continues to lag for trials funded by the NIH and by other government or academic institutions. Pfizer has reported that the preparation of results summaries requires 4 to 60 hours,19 and it is possible that the NIH and other funders have been unable or unwilling to allocate adequate resources to ensure timely reporting.
As expected, earlier-phase trials were consistently the least likely to report results in a timely fashion or over the 5-year study interval. Concern has been raised that earlier-phase trials are primarily focused on proof-of-concept demonstrations and as such represent valuable, closely guarded intellectual property.2 Counterarguments include the ethical obligation to volunteers who participate in early-phase experiments, which often carry unknown risks without the prospect of benefit, and concern that nondisclosure could harm participants in similar trials, because researchers and funders would remain unaware of possible risks.
Penalties that have been established by the FDAAA include publication at ClinicalTrials.gov of “failure to submit” notifications and lists of sanctions that have been imposed, including civil penalties of up to $10,000 per day and loss of funding to the NIH.4 No enforcement has yet occurred, partly because the Notice of Proposed Rulemaking for the FDAAA was released in November 2014 and the period for public comment has recently been extended to March 23, 2015.23,24 In addition, the FDA and National Library of Medicine could work together to inform sponsors of all trials that are required to report to ClinicalTrials.gov on approval of the product or new indication. Finally, the International Committee of Medical Journal Editors (ICMJE) could create policies that mandate the reporting of results, perhaps concurrent with peer-reviewed publication or FDA approval, since earlier ICMJE policies have notably improved rates of trial registration before publication.25 Other factors that could prompt increased reporting to CinicalTrials.gov include notification by the National Library of Medicine to sponsors regarding the status of all applicable clinical trials and reporting deadlines, development of internal reporting policies by sponsors, endorsement of requirements for the reporting of results by federal and nonfederal funding agencies, and enforcement of legal penalties.
We note a number of limitations to our study. Our analysis includes only registered HLACTs, and therefore some HLACTs may have been missed as a result of not being registered. The algorithm that we used to identify HLACTs cannot perfectly ascertain which trials were subject to FDAAA regulation and does not identify trials of interventions that have not been approved for marketing and therefore were not required to report results (Fig. S4 in the Supplementary Appendix). Although we examined data on certification and extension requests, not all sponsors of applicable clinical trials of unapproved or unlabeled products submitted such requests. Many of these trials may have been in the premarketing phase or may have been early negative trials for which plans for marketing were withdrawn. Finally, since trial characteristics are submitted by sponsors, we cannot independently verify their accuracy.
In conclusion, despite ethical mandates, statutory obligations, and considerable societal pressure, most trials that were funded by the NIH or other government or academic institutions and were subject to FDAAA provisions have yet to report results at ClinicalTrials.gov, whereas the medical-products industry has been more responsive to the legal mandate of the FDAAA. However, industry, the NIH, and other government and academic institutions all performed poorly with respect to ethical obligations for transparency.
Supplementary Material
Acknowledgments
Supported by the Clinical Trials Transformation Initiative and the NIH Common Fund through cooperative agreements (1U54AT007748-01 and 3U54AT007748-02S1) with the Office of Strategic Coordination in the Office of the NIH Director.
We thank Deborah Zarin, M.D., and Tony Tse, M.S., of the National Library of Medicine, NIH, for their technical assistance in using data from ClinicalTrials.gov; and Jonathan McCall, M.S., and Liz Wing, M.A., of the Duke Clinical Research Institute for assistance in the preparation of the manuscript.
Funded by the Clinical Trials Transformation Initiative and the NIH.
Footnotes
The views presented here are solely those of the authors and do not necessarily represent the official views of the Clinical Trials Transformation Initiative or the NIH.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Kesselheim AS, Mello MM. Confidentiality laws and secrecy in medical research: improving public access to data on drug safety. Health Aff (Millwood) 2007;26:483–91. doi: 10.1377/hlthaff.26.2.483. [DOI] [PubMed] [Google Scholar]
- 2.Turner EH, Matthews AM, Linardatos E, Tell RA, Rosenthal R. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–60. doi: 10.1056/NEJMsa065779. [DOI] [PubMed] [Google Scholar]
- 3.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356:2457–71. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 4.Food and Drug Administration Amendments Act of 2007. (Public Law No. 110–85 § 801;2007.)
- 5.ClinicalTrials.gov. FDAAA 801 requirements. ( http://clinicaltrials.gov/ct2/manage-recs/fdaaa)
- 6.Zarin DA, Tse T, Williams RJ, Califf RM, Ide NC. The ClinicalTrials.gov results database — update and key issues. N Engl J Med. 2011;364:852–60. doi: 10.1056/NEJMsa1012065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gill CJ. How often do US-based human subjects research studies register on time, and how often do they post their results? A statistical analysis of the Clinicaltrials.gov database. BMJ Open. 2012;2(4):e001186. doi: 10.1136/bmjopen-2012-001186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Law MR, Kawasumi Y, Morgan SG. Despite law, fewer than one in eight completed studies of drugs and biologics are reported on time on ClinicalTrials.gov. Health Aff (Millwood) 2011;30:2338–45. doi: 10.1377/hlthaff.2011.0172. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen TA, Dechartres A, Belgherbi S, Ravaud P. Public availability of results of trials assessing cancer drugs in the United States. J Clin Oncol. 2013;31:2998–3003. doi: 10.1200/JCO.2012.46.9577. [DOI] [PubMed] [Google Scholar]
- 10.Prayle AP, Hurley MN, Smyth AR. Compliance with mandatory reporting of clinical trial results on ClinicalTrials.gov: cross sectional study. BMJ. 2012;344:d7373. doi: 10.1136/bmj.d7373. [DOI] [PubMed] [Google Scholar]
- 11.Saito H, Gill CJ. How frequently do the results from completed US clinical trials enter the public domain? A statistical analysis of the ClinicalTrials.gov database. PLoS One. 2014;9(7):e101826. doi: 10.1371/journal.pone.0101826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuehn BM. Few studies reporting results at US government clinical trials site. JAMA. 2012;307:651–3. doi: 10.1001/jama.2012.127. [DOI] [PubMed] [Google Scholar]
- 13.Emanuel EJ, Wendler D, Grady C. What makes clinical research ethical? JAMA. 2000;283:2701–11. doi: 10.1001/jama.283.20.2701. [DOI] [PubMed] [Google Scholar]
- 14.Drazen JM, Morrissey S, Curfman GD. Open clinical trials. N Engl J Med. 2007;357:1756–7. doi: 10.1056/NEJMe0706501. [DOI] [PubMed] [Google Scholar]
- 15.Clinical Trials Transformation Initiative. AACT database. ( http://ctti-clinicaltrials.org/what-we-do/analysis-dissemination/state-clinical-trials/aact-database)
- 16.Tasneem A, Aberle L, Ananth H, et al. The database for aggregate analysis of ClinicalTrials.gov (AACT) and subsequent regrouping by clinical specialty. PLoS One. 2012;7(3):e33677. doi: 10.1371/journal.pone.0033677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Califf RM, Zarin DA, Kramer JM, Sherman RE, Aberle LH, Tasneem A. Characteristics of clinical trials registered in ClinicalTrials.gov, 2007–2010. JAMA. 2012;307:1838–47. doi: 10.1001/jama.2012.3424. [DOI] [PubMed] [Google Scholar]
- 18.Shalowitz DI, Miller FG. Disclosing individual results of clinical research: implications of respect for participants. JAMA. 2005;294:737–40. doi: 10.1001/jama.294.6.737. [DOI] [PubMed] [Google Scholar]
- 19.Pfizer.com. Clinical case study series: disclosure of clinical trials information. 2009 ( https://www.pfizer.com/files/research/researchclinicaltrials/DisclosureClinicalTrialsInformation030209.pdf)
- 20.GSK.com. Global public policy issues: public disclosure of clinical research. 2014 Apr; ( http://www.gsk.com/media/280827/disclosure-of-clinical-trial-information-policy.pdf)
- 21.Merck.com. Public policy statement: clinical trials data disclosure. 2014 Jul; ( http://www.merck.com/about/views-and-positions/Clinical%20Trials%20Data%20Disclosure%20-%20July%202014.pdf)
- 22.Feczko J. Clinical trials report card. N Engl J Med. 2006;354:1426–9. doi: 10.1056/NEJMc066024. [DOI] [PubMed] [Google Scholar]
- 23.Department of Health and Human Services. US Food and Drug Administration response letter to the Honorable Leonard Lance. 2014 Jul 10; ( http://nebula.wsimg.com/402766aac55d29eb46728087828d33de?AccessKeyId=B353B9F4C0E2B832754F&disposition=0&alloworigin=1)
- 24.Federal Register. Clinical trials registration and results submission: a proposed rule by the National Institutes of Health on 02/13/2015. ( https://www.federalregister.gov/articles/2015/02/13/2015-02990/clinical-trials-registration-and-results-submission)
- 25.Laine C, Horton R, DeAngelis CD, et al. Clinical trial registration — looking back and moving ahead. N Engl J Med. 2007;356:2734–6. doi: 10.1056/NEJMe078110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.