Abstract
A 70-year-old man presented with acute coronary syndrome 3 weeks after plastic stent insertion for hilar biliary stricturing secondary to IgG4-related sclerosing cholangitis (IgG4-SC). Imaging demonstrated haemopericardium due to proximal migration of the plastic biliary stent through the liver capsule and diaphragm into the pericardial sac. The stent was endoscopically removed and a pericardiocentesis was performed. The patient's clinical condition rapidly improved. We illustrate an unusual but potentially serious complication that may arise from migration of a biliary stent and discuss a management strategy.
Introduction
IgG4-related disease is a steroid-responsive, multi-system inflammatory disorder. The most frequent extra-pancreatic manifestation of IgG4-related disease is IgG4-related sclerosing cholangitis (IgG4-SC), present in over 70% of patients with IgG4-related autoimmune pancreatitis (AIP).1 Endoscopic retrograde cholangiopancreatography (ERCP) is often required in such cases to obtain a tissue diagnosis and to treat strictures requiring a biliary stent.2
Case Report
A 70-year-old Chinese man with a past medical history of hepatitis B virus infection (HBsAg negative) and glaucoma presented with pruritis and painless obstructive jaundice (bilirubin 300 µmol/L). Cross-sectional imaging revealed a 3-cm mass in the head of the pancreas abutting the superior mesenteric vein, portal lymphadenopathy, and a hilar liver mass with associated intrahepatic duct dilatation. ERCP revealed a long biliary stricture extending to the hilum, which was treated with a straight plastic biliary stent. Histological sampling from the ampulla, common bile duct (CBD), and the liver lesion all showed a lymphoplasmacytic infiltrate with a high expression of IgG4-positive plasma cells (>100 cells per high-powered field), consistent with a diagnosis of IgG4-related disease. Serum IgG4 was elevated at 4.36 g/L (normal: 0-1.3 g/L).
He started a tapering course of oral steroids and had an excellent biochemical and clinical response. His biliary stent was removed. After 6 months, steroid treatment was stopped. Three months later, he presented with jaundice and chills. Repeat ERCP demonstrated 2 short, dominant biliary strictures in the distal CBD and at the liver hilum (Figure 1), and a long, irregular, thin pancreatic duct (Figure 1). A 15-cm, 10-French, straight plastic biliary stent was placed across the liver hilum into the left main intrahepatic duct (Figure 1). The length of this stent was necessary to traverse both strictures and provide adequate biliary drainage. Steroids were restarted with intent of starting second-line long-term maintenance immunosuppression.
Figure 1.

ERCP showing (A) a cholangiogram with areas of biliary structuring at the liver hilum (red arrow) and distal common bile duct (blue arrow), (B) a pancreatogram with a thin, irregular main pancreatic duct (arrow) in the head/body of pancreas with some relative dilation towards the tail, and (C) the 15-cm, 10-French straight biliary stent (arrow) sited across the hilum into the left main intrahepatic duct.
Twenty days following biliary stent insertion, he developed acute chest pain. An electrocardiogram showed widespread ST segment elevation; coronary angiography was normal. The following day, he developed a fever with dyspnea and supraventricular tachycardia. Chest radiography showed left lower lobe consolidation with air bronchograms and blunting of the left costophrenic angle. A biliary stent was noted on the inferior aspect of the film; its superior end was overlying the cardiac silhouette (Figure 2). He was treated with antibiotics for suspected pneumonia. A CT scan confirmed a large pericardial effusion, with the proximal tip of the plastic stent extending through the liver capsule and diaphragm into the pericardial sac (Figure 3). ERCP showed that the distal end of the stent was within the distal bile duct. The stent was mobilized with traction using a biliary extraction balloon and removed with stent grabbers. He remained hemodynamically stable during the procedure, but the pericardial effusion later enlarged and was successfully treated with percutaneous pericardial drainage of approximately 300 mL of blood.
Figure 2.
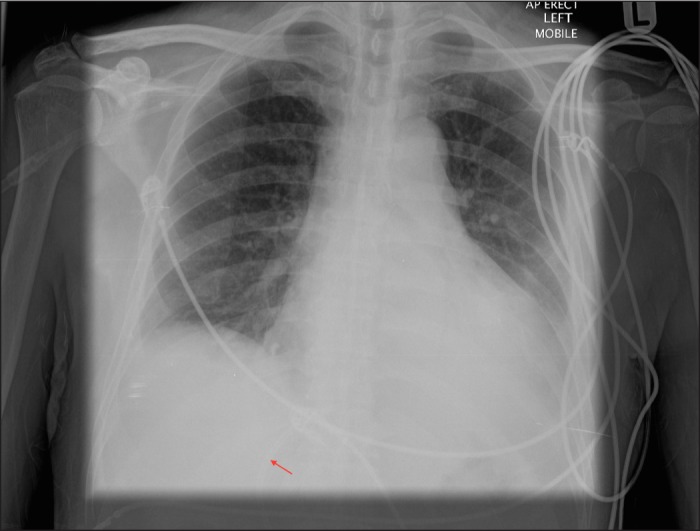
Chest radiograph 3 weeks after biliary stent insertion showing the tip of the biliary stent (arrow) overlying the cardiac silhouette.
Figure 3.
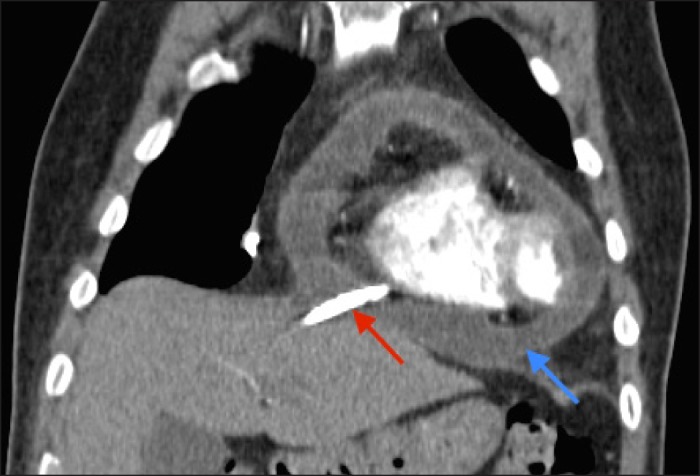
CT showing the biliary stent (red arrow) within the pericardial space and free pericardial fluid (blue arrow).
He made a swift recovery and his IgG4-related disease has since been remission with azathioprine and low dose prednisolone. Eighteen months later, no further biliary intervention has been required and he remains clinically well with normalization of his liver function tests and radiological improvement in biliary stricturing.
Discussion
IgG4-related disease is a multi-system inflammatory disorder and an emerging disease entity of unknown etiology. It comprises a collection of conditions that share clinical, serological, histopathological, and radiological features.3 It is characterized by a lymphoplasmacytic tissue infiltration with a predominance of IgG4-positive plasma cells and T-lymphocytes.4 Multiple organs may be involved, including the pancreas and biliary tree.5 Although the optimal treatment for IgG4-related disease has not been established, clinical and radiological response to steroids usually occurs within weeks of starting therapy.1
Our patient had an established diagnosis of IgG4-related disease with biliary and pancreatic involvement. We hypothesize that rapid improvement in biliary stricturing in response to steroids reduced the traction force on the biliary stent, allowing it to migrate proximally, and that the 15-cm length of the stent may have been an additional factor influencing migration. An argument could be made for steroid treatment without biliary stenting, but there is not sufficient evidence at this stage to support that approach.
Proximal or distal migration of plastic biliary stents is a recognized complication of ERCP in 5-7% of patients.6 Migration frequency is higher in patients with benign disease.7 Proximally migrated biliary stents can be removed successfully using an endoscopic retrieval technique, the choice of which depends on several factors including biliary duct dilation, depth of stent migration, distal stent impaction, and biliary stricture distal to the migrated stent. Common retrieval techniques include biliary baskets, extraction balloons, snares, forceps, and cholangioscopic stent retrieval.8
Traumatic bronchopleurobiliary, hepaticogastric, and other extrahepatic bile duct fistulae following migration of a plastic biliary stent through the liver capsule have previously been described, but we could find no previous case reports of intrapericardial migration.9-11 Our case illustrates the need for clinical awareness and early recognition of this condition if a patient presents with otherwise unexplained cardiorespiratory symptoms following biliary stent insertion.
Disclosures
Author contributions: B. Paranandi wrote the manuscript and is the article guarantor. D. Joshi contributed to the discussion. GJ Johnson and GJ Webster provided endoscopic images, and reviewed and edited the final manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Acknowledgement: We thank Dr. Pascal Meier and Dr. John Yap from University College London Hospitals for their advice and technical support on the interventional procedures for this patient.
References
- 1. Khosroshahi A, Stone JH. Treatment approaches to IgG4-related systemic disease. Curr Opin Rheumatol. 2011;23(1):67–71. [DOI] [PubMed] [Google Scholar]
- 2. Kalaitzakis E, Levy M, Kamisawa T, et al. Endoscopic retrograde cholangiography does not reliably distinguish IgG4-associated cholangitis from primary sclerosing cholangitis or cholangiocarcinoma. Clin Gastroenterol Hepatol. 2011;9(9):800–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012;366(6):539–51. [DOI] [PubMed] [Google Scholar]
- 4. Cheuk W, Chan JK. IgG4-related sclerosing disease: A critical appraisal of an evolving clinicopathologic entity. Adv Anat Pathol. 2010;17(5):303–32. [DOI] [PubMed] [Google Scholar]
- 5. Okazaki K, Uchida K, Koyabu M, et al. Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. J Gastroenterol. 2011;46(3):277–88. [DOI] [PubMed] [Google Scholar]
- 6. Johanson JF, Schmalz MJ, Geenen JE. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest Endosc. 1992;38(3):341–6. [DOI] [PubMed] [Google Scholar]
- 7. Arhan M, Odemis B, Parlak E, et al. Migration of biliary plastic stents: Experience of a tertiary center. Surg Endosc. 2009;23(4):769–75. [DOI] [PubMed] [Google Scholar]
- 8. Pohl J. Cholangioscopic retrieval of a proximally migrated biliary plastic stent. Vid J Encyclopedia Gastrointest Endosc. 2013;1(2):440–41. [Google Scholar]
- 9. Dasmahapatra HK, Pepper JR. Bronchopleurobiliary fistula: A complication of intrahepatic biliary stent migration. Chest. 1988;94(4):874–5. [DOI] [PubMed] [Google Scholar]
- 10. Mahadeva S, Ranjeev P, Goh KL. Hepaticogastric fistulation from a proximally migrated biliary stent. Gastrointest Endosc. 2003;58(2):295–7. [DOI] [PubMed] [Google Scholar]
- 11. Sinha S, Wardle A, Kalidindi V, et al. Erosion and perforation of the biliary tree by plastic biliary endoprostheses. Endoscopy. 2010;42(9):760–3. [DOI] [PubMed] [Google Scholar]


