Abstract
Background: There is no consensus on the optimal treatment for patients with complex proximal humeral fractures. A meta-analysis was performed to evaluate clinical effectiveness of plate and tension band fixation compared with conservative therapy. Methods: We systematically searched electronic databases (Pubmed, Medline, Embase, Cochrane library and Google Scholar) to identify comparative studies and randomized controlled trials in which plate and tension band fixation was compared with conservative treatment of the complex proximal humeral fractures from 1995 to 2013. The quality of the studies was assessed and effective data were pooled for meta-analysis. Results: A total of 222 patients from three RCTs and three comparative studies were included in this meta-analysis (113 fractures treated with plate and tension band and 109 with conservative treatment). The primary and secondary outcomes (Constant Score, nonunion, avascular necrosis and osteoarthritis) were compared and there was no significant difference among these different treatments of this injury. Conclusions: Compared with conservative treatment, internal fixation including plate and tension band did not find better shoulder function, higher rate avascular necrosis of humeral head, lower rate nonunion, and higher rate osteoarthritis. In further, high quality and large randomized trials should be recommended to make a choice between these treatment modalities.
Keywords: Plate fixation, tension band fixation, conservative treatment, complex proximal humeral fracture, meta-analysis
Introduction
Fracture of the proximal humerus is a common injury, especially in elderly patients with osteoporotic bone. It is accounting for 6% of all adult fractures [1] and can cause substantial pain, loss of function, and loss of independence in performance of activities of daily living. Although the vast majority of the fractures are non- or minimally displaced and can be treated conservatively [2], the complex proximal humeral fractures has a poor outcome and the optimal treatment is still controversial.
Orthopaedic surgeons searching for the best treatment of a complex proximal humeral fracture face a variety of choice. Surgical treatment options include open or closed reduction and stabilization method using wires, nails, external fixation and screws [3,4]. Prosthetic joint replacement or conservative therapies are other options [5]. Fracture type, dislocations degree and age are considered as significant predictors of functional prognosis.
Meta-analyses comparing conservative with operative management for proximal humeral fractures have been available in recent years [6-8]. Internal fixation and shoulder arthroplasty were pooled in these studies while differences in opinion existing with regard to different biomechanical stability. Very few evidence on the treatment option which comparing internal fixation with non-surgical treatment of complex proximal humeral fractures have been reported. The aim of our meta-analysis was to determine the advantages and disadvantages of internal fixation versus non-surgical treatments reported in all the related RCTs and comparative studies available. We believe such a meta-analysis will yield stronger evidence to answer the question concerning clinical treatment of complex proximal humeral fractures.
Materials and methods
Search strategy
Computer literatures search was conducted to identify publications relating to compare open reduction and internal fixation (ORIF) versus non-surgical treatment for complex proximal humeral fractures. Databases used for searches included Pubmed, Medline, Embase, Cochrane library and Google Scholar. The eligible time was from 1995 to 1st August 2013. No language restriction was made. Key words included: complex proximal humeral fracture, internal fixation, non-operation/non-surgery, conservation, comparative studies and randomized controlled trials.
Eligibility criteria
The following eligibility criteria were used to select trials.
Types of study: Randomized and quasi-randomized controlled clinical trials, prospective and retrospective comparative studies.
Types of participant: Skeletally mature patients (age > 18) with complex proximal humeral fracture. People with delayed presentation (more than 3 weeks post-injury), a history of previous humeral abnormalities (e.g. an infection or a tumor) were excluded.
Types of intervention: Internal fixation versus non-surgical treatment of complex proximal humeral fracture.
Types of outcome measure: The primary outcome measure was functional outcome as the Constant score. Secondary outcome measures were nonunion, avascular necrosis (AVN) of humeral head and osteoarthritis.
Data collection and analysis
Selection of studies
Two authors independently reviewed possible titles and abstracts and retrieved the full article if the screening criteria were met. Final eligibility was decided by consensus after discussion.
Data extraction and management
All relevant data regarding patient demographics, study design, injury characteristics, intervention, outcomes, and complications were extracted by two authors independently. Disagreements were resolved by discussion and a senior reviewer’s opinion was inquired if necessary. There was 100% agreement between the two authors.
Methodological assessment
The methodological quality of these RCTs was evaluated with the Cochrane Collaboration’s tool for assessing ‘risk of bias’ of individual studies. Assessments of five main fields including sequence generation, allocation concealment, blinding, incomplete outcome data and selective outcome reporting were made.
The comparative studies were evaluated by using MINORS score which was defined as the Methodological Index for Nonrandomized Studies score [9]. A MINORS score of more than twelve was considered the standard for inclusion.
Statistical analysis
Study data were pooled and analyzed using the Cochrane Collaboration’s REVMAN 5.0 software. Continuous variable (the Constant Score) was analyzed using the mean differences (MD) with its 95% CI, whereas dichotomous data (nonunion, avascular necrosis of humeral head, and osteoarthritis) were analyzed using the risk ratio (RR) measure and its 95% confidence interval (CI). We planned to assess heterogeneity for pooled data from comparable studies by visual inspection of the analyses along with consideration of the Q statistics test for heterogeneity and the I² statistic. Moreover, we performed prespecified subgroup analyses based on RCTs versus non-randomized studies and tension band versus plate to define source of heterogeneity.
Assessment of publication bias
Possible publication bias was evaluated by the Begg’s rank correlation test [10] and the Egger’s regression test [11]. Both analyses were performed using STATA 10.0 software.
Results
Literature search results
A total of 482 potentially relevant articles were identified. After reference to titles, abstracts and even full texts, three published RCTs [12-14], one prospective comparative study [15] and two retrospective comparative studies [16,17] with a total of 222 patients met all inclusion criteria (Figure 1). Information on general characteristics of studies and participants was listed in Table 1. The clinical outcomes of the included studies were presented in Table 2.
Figure 1.
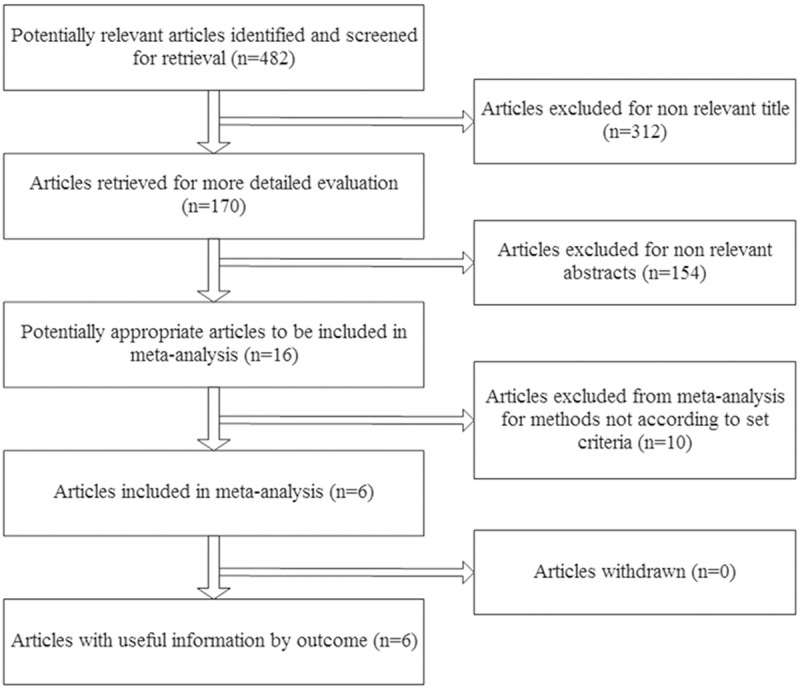
Flow chart.
Table 1.
Characteristics of included studies
| Study Type | Fracture Type | Intervention | Sample Size | Mean Age (yr) | % Female | Mean Follow-Up (month) | % Lost Follow-Up | |
|---|---|---|---|---|---|---|---|---|
| Zyto 1997 | RCT | Neer (3-, 4-part, and displaced) | Conservative | 15 | 75 | 85% | 50 | 20% |
| ORIF-tension band | 14 | 73 | 90% | |||||
| Ilchmann 1998 | R | Neer (3-, 4-part, and displaced) | Conservative | 16 | 69.8 | 81.3% | 66.3 | - |
| ORIF-tension band | 18 | 60.5 | 72.2% | 66.3 | ||||
| Kolling 2003 | PNR | Neer (3-, 4-part, and displaced) | Conservative | 9 | 52.7 | 58.5% | 74.4 | - |
| ORIF-plate | 13 | 52.5 | 82.8 | |||||
| Olerud 2011 | RCT | Neer (3-, 4-part, and displaced) | Conservative | 26 | 74.9 | 83% | 24 | 11.7% |
| ORIF-plate | 27 | 72.9 | 80% | |||||
| Sanders 2011 | R | Neer (2-, 3-, 4-part) | Conservative | 18 | 64 | 66.7% | 42 | - |
| ORIF-plate | 18 | 58 | 52.9% | 37 | ||||
| Fjalestad 2012 | RCT | OTA: B2, C2 | Conservative | 25 | 73.1 | 96% | > 12 | 4% |
| ORIF-plate | 23 | 72.2 | 80% |
RCT, randomized controlled trial; PNR, prospective non-randomized; R, retrospective.
Table 2.
Outcomes of included studies
| Constant Score | Non-union | AVN | Osteoarthritis | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| ORIF | Conservative | ORIF | Conservative | ORIF | Conservative | ORIF | Conservative | |
| Zyto 1997 | 60 ± 19 | 65 ± 15 | 1 | 0 | 1 | 0 | 4 | 2 |
| Ilchmann 1998 | - | - | 0 | 0 | 9 | 7 | - | - |
| Kolling 2003 | 72.1 ± 21.1 | 82.0 ± 15.6 | - | - | 1 | 0 | - | - |
| Olerud 2011 | 61 ± 19.2 | 58.4 ± 23.1 | 1 | 1 | 3 | 2 | 0 | 1 |
| Sanders 2011 | - | - | 0 | 1 | 1 | 0 | 11 | 6 |
| Fjalestad 2012 | 52.3 ± 20.9 | 52.2 ± 18.3 | 0 | 2 | 8 | 13 | - | - |
ORIF, Open reduction and internal fixation; AVN, Avascular necrosis.
Methodological quality
Methodological quality of each eligible study was independently assessed by two authors. The sample sizes of the three trials were ranging from 29 to 53. Table 3 described the assessments of risk of bias of the randomized trials. All studies reported baseline features of the patients, and each had a similar baseline. All trials reported a low risk of ‘selection bias’ as the sequence generation was based on the sealed envelop. All trials were judged as ‘unclear’ in the blinding field as the information of blinding of patients and care provider/outcome assessment was not provided. One [14] reported a low risk of ‘attrition bias’ with rate of loss to follow-up less than 5%. The other two trials [12,13] reported less than a 20% rate of loss to follow-up and judged the field with ‘no’.
Table 3.
Assessments of risk of bias of the randomized controlled trials
| Studies | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting |
|---|---|---|---|---|---|
| Zyto 1997 | Sealed envelope | Yes | Unclear | No | Yes |
| Olerud 2011 | Independently prepared opaque, sealed envelopes | Yes | Unclear | No | Yes |
| Fjalestad 2012 | Numbered and sealed non-translucent envelopes | Yes | Unclear | Yes | Yes |
Three studies of prospective/retrospective comparative studies were assessed with MINORS score (Table 4). Two studies [15,17] scored 18 and one [16] scored 16. All studies scored more than twelve and had a low to moderate risk of bias.
Table 4.
Methodological items for non-randomized studies
| Study | Ilchmann 1998 | Kolling 2003 | Sanders 2011 |
|---|---|---|---|
| 1. A clearly stated aim | 2 | 2 | 2 |
| 2. Inclusion of consecutive patients | 2 | 2 | 2 |
| 3. Prospective collection of data | 0 | 2 | 0 |
| 4. Endpoints appropriate to the aim of the study | 2 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 0 | 0 | 2 |
| 6. Follow-up period appropriate to the aim of the study | 2 | 2 | 2 |
| 7. Loss to follow up less than 5% | 0 | 0 | 0 |
| 8. Prospective calculation of the study size | 0 | 0 | 0 |
| 9. An adequate control group | 2 | 2 | 2 |
| 10. Contemporary groups | 2 | 2 | 2 |
| 11. Baseline equivalence of groups | 2 | 2 | 2 |
| 12. Adequate statistical analyses | 2 | 2 | 2 |
| Total score | 16 | 18 | 18 |
Publication bias
There was little evidence of publication bias with regard to the rate of AVN in relation to risk of intervention, as indicated by the Begg’s test (P = 0.602) and Egger’s test (P = 0.408).
Subgroup analysis
There were three RCTs and three comparative studies in this meta-analysis. Internal fixation in four studies [13-15,17] were treated by plate and in other two studies [12,16] were treated by tension band. Table 5 presented the results of subgroup stratified by characteristics of study design and ORIF technique. Subgroup analyses on study design and ORIF technique showed the test for interaction on the outcomes (Constant score, AVN, nonunion, and osteoarthritis) was not statistically significant. Overall, the clinical association between Constant score, AVN, nonunion, and osteoarthritis was not substantially modified by study design and ORIF technique.
Table 5.
Subgroup analysis of the included studies based on influential factors
| Factors | Constant score | AVN | Nonunion | Osteoarthritis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Subgroup | MD (95% CI) | P Interaction | Subgroup | RR (95% CI) | P Interaction | Subgroup | RR (95% CI) | P Interaction | Subgroup | RR (95%CI) | P Interaction | |
| Design | RCT (3) | -0.51 (-7.25-6.22) | 0.27 | RCT (3) | 0.86 (0.46-1.58) | 0.36 | RCT (3) | 0.78 (0.18-3.41) | 0.63 | RCT (2) | 1.34 (0.37-4.82) | 0.68 |
| Non-RCT (1) | -9.90 (-25.24-5.44) | Non-RCT (3) | 1.32 (0.65-2.67) | Non-RCT (2) | 0.33 (0.01-7.68) | Non-RCT (1) | 1.83 (0.87-3.88) | |||||
| Technique | Tension band (1) | -5.00 (-17.52-7.52) | 0.59 | Tension band (2) | 1.27 (0.62-2.59) | 0.47 | Tension band (2) | 3.20 (0.14-72.62) | 0.25 | Tension band (1) | 2.14 (0.46-9.93) | 0.69 |
| Plate (3) | -1.08 (-8.17-6.01) | Plate (4) | 0.90 (0.49-1.64) | Plate (3) | 0.41 (0.08-2.06) | Plate (2) | 1.53 (0.74-3.13) | |||||
P Interaction, Probability for interaction; CI, Confidence interval; RR, Relative risk; MD, Mean differences; AVN, Avascular necrosis.
Outcome measures
Four studies [12-15] included 152 cases provided data on Constant score. The overall results based on fixed-effect model did not support the treatment of open reduction and internal fixation to improve the functional outcome when compared with non-surgical treatment for complex proximal humeral fractures (MD = -2.03; 95% CI = -8.20, 4.14; P = 0.52; I2 = 0%) (Figure 2).
Figure 2.
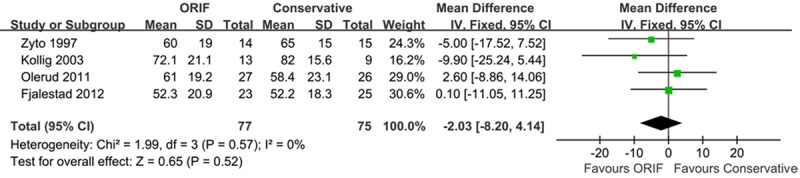
Meta-analysis of Constant-Murley scores.
AVN-risk analysis was possible across six studies with 222 cases [12-17]. As we found no statistical evidence heterogeneity (PHeterogeneity = 0.71, I2 = 0%), a fixed effect model was used. There was no significant difference in the rate of AVN comparing internal fixation with non-surgical treatment (RR = 1.02; 95% CI = 0.65, 1.62; P = 0.92; I2 = 0%) (Figure 3).
Figure 3.
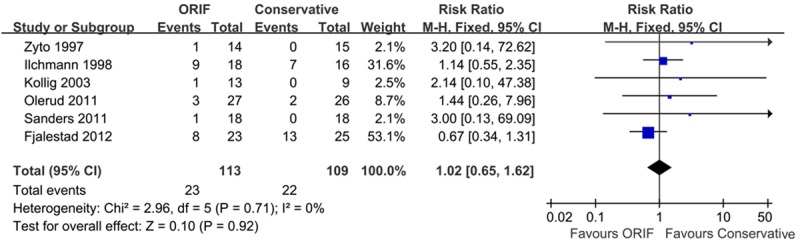
Meta-analysis of AVN.
Five studies [12-14,16,17] provided data on non-union after internal fixation or conservative treatment: 2 of 100 and 4 of 100, respectively, showing no significant difference (RR = 0.66; 95 % CI = 0.18, 2.45; P = 0.53; I2 = 0%) (Figure 4).
Figure 4.
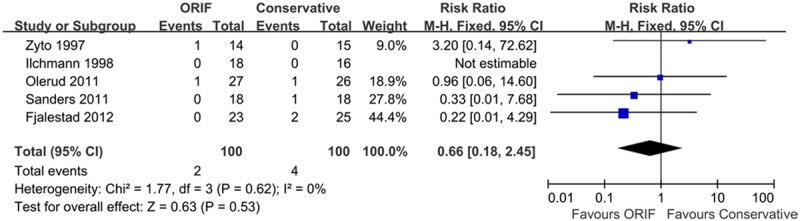
Meta-analysis of nonunion.
Three studies [12,13,17] reported data on osteoarthritis, including 118 cases. Fractures receiving internal fixation did not show more osteoarthritis than those receiving conservative treatment (RR = 1.65; 95% CI = 0.86, 3.18; P = 0.13; I2 = 0%) (Figure 5).
Figure 5.
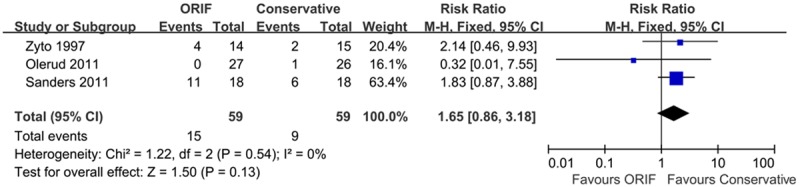
Meta-analysis of osteoarthritis.
Discussion
This systematic review was based on three RCTs and three comparative studies that included 113 cases treated with internal fixation and 109 cases treated with non-operative. The primary and secondary outcomes investigated were shoulder function (Constant Score), nonunion, avascular necrosis and osteoarthritis. In this meta-analysis, no statistically significant differences in the primary and secondary outcomes were identified following management of complex proximal humeral fracture with internal fixation or non-surgical treatment. The small sample sizes in the studies that were included left the pooled estimates underpowered to allow us to resolve the conflict and make any definitive conclusions about the optimal management of complex proximal humeral fracture-internal fixation or non-surgical treatment.
Functional outcome was a major clinical evaluation criterion in all studies assisted their comparison across patient group. The Constant Score was the most frequently used measure and can be compared across various groups and treatments [18]. A controversy against conservative management was the recognition of the impaired function. As Bertoft et al [19] indicated that after injury there was a marked tendency for the capsule of the shoulder joint to contract and for the deltoid muscle to atrophy, leading to stiffness and inferior subluxation of the humeral head respectively. It also identified that conservative treatment entails supporting the arm in a sling that neither permits early joint mobilization nor gives adequate pain relief [20]. Four studies in our meta-analysis had pooled data on the Constant Score and the combined result indicated that there were no significant differences on internal fixation versus non-surgical therapy. Misra et al [21] compared the clinical outcomes following treatment of 3-part and 4-part proximal humerus with conservative treatment, plate fixation and arthroplasty in a systematic literature review (24 studies), and found the range of motion did not show any significant differences between patients treated by conservatively and those treated by fixation.
The current studies have shown the considerable complication rate associated with surgery of above injuries [22]. Zyto et al [23] recommended that conservative treatment can be associated with nonunion, malunion and avascular necrosis with painful dysfunction as result. In our meta-analysis, we did not found a significant difference compared with internal fixation, which was in line with previous studies.
During the last two decades, to our knowledge, only three randomized controlled clinical trials [12-14] comparing option management with internal fixation versus non-surgical treatment for complex proximal humeral fracture exists. All these studies were limited with little number and small sizes. In our meta-analysis, other three comparative studies were included. The strength of this meta-analysis was its comprehensive range, with all major types of trials, and its thorough search strategy. Other the other hand, we used MINORS scores to assess the risk of bias of these including non-randomized comparative studies. Three non-randomized comparative studies were evaluated, with a score ranging from 16 to 18 and a low to moderate risk of bias, meeting the standard for inclusion with a score more than twelve. All the primary and secondary outcomes were assessed by subgroup analyses based on RCTs versus non-randomized comparative studies, and there were no statistically significant deference on the test of interaction.
There were several potential limitations in this meta-analysis. First, heterogeneity in patient age should be considered as it was impossible to match the cohorts completely for the analysis. In patients who were 65 years of age or older, surgery was an independent risk factor for inpatient adverse events and mortality when older-aged patients admitting to the hospital with an isolated fracture of the proximal humerus [24]. It was also clear that clinical results get poorer with increasing age [25]. A patient presenting with a complex proximal humeral fracture was probably not going to recover his/her pre-trauma shoulder with lower functional demands, especially when elderly. Therefore, it was most reliable and predictable to restore a range of useful mobility, improving patient comfort of daily life as rapidly as possible with increasing age [26]. We acknowledged that an additional subgroup analysis of age would have been valuable. Physiological age and functional requirements should be analyzed and discussed with the patient so as to choose the appropriate treatment. However, we failed to do a pooled analysis involving this consideration because of lack of adequate data in the analyzed studies.
Second, our inclusion criteria have been broadened to include prospective and retrospective non-randomized comparative studies. Although the inclusion of the studies increased the range of research available, it also raised the spectre of selection bias. Demand of more high quality trials has been stated previously.
Finally, we failed to analyze the performance of daily activities, vocational function and societal costs such as duration and cost of postoperative rehabilitation, time off work and ability to return to work. All these data was not concerned in the studies included, and these factors limited the outcomes when comparing the effects of treatment option.
Conclusions
In conclusion, no statistical difference between internal fixation and non-surgical treatment in outcomes for complex proximal humeral fractures could be proved on the basis of the present available evidence. Considering the limitations of included studies, a large, well designed trial is strongly required in this controversial area. We also call for a future trial that includes a specific age cut off for internal fixation versus non-surgical treatment.
Disclosure of conflict of interest
None.
References
- 1.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 2.Bahrs C, Rolauffs B, Dietz K, Eingartner C, Weise K. Clinical and radiological evaluation of minimally displaced proximal humeral fractures. Arch Orthop Trauma Surg. 2010;130:673–679. doi: 10.1007/s00402-009-0975-9. [DOI] [PubMed] [Google Scholar]
- 3.Ring D. Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures. Injury. 2007;38(Suppl 3):S59–68. doi: 10.1016/j.injury.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD. Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am. 2007;89(Suppl 3):44–58. doi: 10.2106/JBJS.G.00648. [DOI] [PubMed] [Google Scholar]
- 5.Mighell MA, Kolm GP, Collinge CA, Frankle MA. Outcomes of hemiarthroplasty for fractures of the proximal humerus. J Shoulder Elbow Surg. 2003;12:569–577. doi: 10.1016/s1058-2746(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 6.Jia Z, Li W, Qin Y, Li H, Wang D, Zhang C, He Q, Ruan D. Operative versus nonoperative treatment for complex proximal humeral fractures: a meta-analysis of randomized controlled trials. Orthopedics. 2014;37:e543–551. doi: 10.3928/01477447-20140528-54. [DOI] [PubMed] [Google Scholar]
- 7.Mao Z, Zhang L, Zeng X, Chen S, Liu D, Zhou Z, Tang P. Operative versus nonoperative treatment in complex proximal humeral fractures. Orthopedics. 2014;37:e410–419. doi: 10.3928/01477447-20140430-50. [DOI] [PubMed] [Google Scholar]
- 8.Nanidis TG, Majed A, Liddle AD, Constantinides VA, Sivagnanam P, Tekkis PP, Reilly P, Emery RJ. Conservative versus operative management of complex proximal humeral fractures: a meta-analysis. Shoulder & Elbow. 2010;2:166–174. [Google Scholar]
- 9.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 10.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. [PubMed] [Google Scholar]
- 11.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79:412–417. doi: 10.1302/0301-620x.79b3.7419. [DOI] [PubMed] [Google Scholar]
- 13.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20:747–755. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 14.Fjalestad T, Hole MØ, Hovden IAH, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26:98–106. doi: 10.1097/BOT.0b013e31821c2e15. [DOI] [PubMed] [Google Scholar]
- 15.Kollig E, Kutscha-Lissberg F, Roetman B, Dielenschneider D, Muhr G. [Complex fractures of the humeral head: which long-term results can be expected?] . Zentralbl Chir. 2003;128:111–118. doi: 10.1055/s-2003-37764. [DOI] [PubMed] [Google Scholar]
- 16.Ilchmann T, Ochsner P, Wingstrand H, Jonsson K. Non-operative treatment versus tension-band osteosynthesis in three-and four-part proximal humeral fractures. Int Orthop. 1998;22:316–320. doi: 10.1007/s002640050268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanders RJ, Thissen LG, Teepen JC, van Kampen A, Jaarsma RL. Locking plate versus nonsurgical treatment for proximal humeral fractures: better midterm outcome with nonsurgical treatment. J Shoulder Elbow Surg. 2011;20:1118–1124. doi: 10.1016/j.jse.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 18.van de Water AT, Shields N, Taylor NF. Outcome measures in the management of proximal humeral fractures: a systematic review of their use and psychometric properties. J Shoulder Elbow Surg. 2011;20:333–343. doi: 10.1016/j.jse.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 19.Bertoft ES, Lundh I, Ringqvist I. Physiotherapy after fracture of the proximal end of the humerus. Comparison between two methods. Scand J Rehabil Med. 1984;16:11–16. [PubMed] [Google Scholar]
- 20.van den Broek CM, van den Besselaar M, Coenen JM, Vegt PA. Displaced proximal humeral fractures: intramedullary nailing versus conservative treatment. Arch Orthop Trauma Surg. 2007;127:459–463. doi: 10.1007/s00402-006-0250-2. [DOI] [PubMed] [Google Scholar]
- 21.Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults--a systematic review of management. Injury. 2001;32:363–372. doi: 10.1016/s0020-1383(00)00242-4. [DOI] [PubMed] [Google Scholar]
- 22.Schliemann B, Siemoneit J, Theisen C, Kosters C, Weimann A, Raschke MJ. Complex fractures of the proximal humerus in the elderly--outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96(Suppl 1):S3–11. doi: 10.1007/s12306-012-0181-8. [DOI] [PubMed] [Google Scholar]
- 23.Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998;29:349–352. doi: 10.1016/s0020-1383(97)00211-8. [DOI] [PubMed] [Google Scholar]
- 24.Neuhaus V, Bot AG, Swellengrebel CH, Jain NB, Warner JJ, Ring DC. Treatment choice affects inpatient adverse events and mortality in older aged inpatients with an isolated fracture of the proximal humerus. J Shoulder Elbow Surg. 2014;23:800–806. doi: 10.1016/j.jse.2013.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beguin L, Adam P, Vanel O, Fessy M. Traumatologie-Indications et echecs du clou verrouille a vis auto-stables pour les fractures proximales de l’humerus: etude prospective de 50 clous Telegraph. Revue de Chirurgie Orthopedique et Reparatrice de l’Appareil Moteur. 2002;88:120–120. [Google Scholar]
- 26.Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009;95:48–55. doi: 10.1016/j.otsr.2008.09.002. [DOI] [PubMed] [Google Scholar]


