Abstract
Objective: To investigate the therapeutic effect and safety of cerclage placed in pregnancy via laparoscopy (CPL) in the first trimesteror in non-pregnant phase (CNL). Methods: A total of 134 cervical insufficiency patients who were treated with cervical cerclage were included. All the patients were divided into 3 groups. CPL group: 43 cases were treated with cerclage placed in pregnancy via laparoscopy in the first trimester, of which 26 cases received termination of pregnancy. CNL group: 58 cases were treated with cerclage placed via laparoscopy in the non-pregnant phase, of whom 34 received termination of pregnancy. TVC group: 33 cases received traditional vaginal cerclage placed in second trimester, of whom 33 cases received termination of pregnancy. Results: All patients received a successful operation without any complications during or after surgery. The post-operative hospitalization duration in CPL group was significantly shorter than that in TVC group. In 3 groups, for all patients who received termination of pregnancy, the postoperative full term delivery rate, fetal salvage rate (if pregnancy lasted ≥ 14 weeks), mean gestational weeks (if pregnancy lasted ≥ 14 wk) after operation, post-operation gestational age for all patients, and weeks of pregnancy gained were observed and analyzed. There were no significant differences of every index between CPL group and CNL group. Every index in TVC group was lower than that in both CNL group and CPL group. Conclusion: CPL or CNL for treatment of cervical insufficiency is safe and effective, with a better therapeutic effect than that of TVC in the second trimester.
Keywords: Cerclage placed via laparoscopy, cervical insufficiency, pregnancy outcome
Introduction
In pregnant women, the incidence of cervical insufficiency is 1%, with a high recurrence rate of 30%, and it will mainly result in abortion or premature delivery in the second and third trimester [1,2]. Traditional vaginal cerclage in the second trimester was the main treatment of cervical insufficiency [3], which would partly solve the problem [4,5]. However, it failed to achieve an ideal effect in some patients, especially in patients with uterus deformity, uterus laceration and a failed TVC treatment. In recent years, there have been some reports about treating cervical insufficiency with cerclage placed via laparoscopy in non-pregnant phase [6-8]. We searched the literature about laparoscopic cervical cerclage in PubMed, EMBASE, and Cochrane database, and concluded that most cases received a better prognosis to some extent (Table 1) [9,10]. There were still some problems remained unsolved: what are the advantages of cerclage placed via laparoscopy compared to TVC; should cerclage placed via laparoscopy be operated before or after pregnancy; will fertilization be affected if cerclage placed via laparoscopy is operated before pregnancy; and what is the appropriate time of fertilization if cerclage placed via laparoscopy is operated before pregnancy? Compared with traditional vaginal cerclage in the second trimester, this study was aimed to investigate the therapeutic effect and safety of CPL and CNL, in order to solve the problems above.
Table 1.
Cumulative results of laparoscopic cervical cerclage
| Cerclage by laparoscopy: study and year | Patient no. | The time of surgery | Pregnancy no. | Intraoperative complication rate (%) | Fetal survival rate (%) | Mean GA at birth |
|---|---|---|---|---|---|---|
| Lesser KB et al., 1998 | 1 | During pregnancy | 1 | 0 | 100 | Not reported |
| Mingione MJ et al., 2003 | 11 | Before pregnancy | 12 | 9 | 83 | 37.1 |
| Cho CH et al., 2003 | 20 | During pregnancy | 21 | 0 | 95 | 36.2 |
| Gallot D et al., 2003 | 3 | Before pregnancy | 2 | 0 | 100 | 38 |
| Ghomi A et al., 2006 | 1 | Before pregnancy | 1 | 0 | 100 | 38.4 |
| Aboujaoude R et al., 2007 | 1 | During pregnancy | Not reported | 0 | Not reported | Not reported |
| Agdi M et al., 2008 | 1 | Before pregnancy | 1 | 0 | Not reported | Not reported |
| Reid GD et al., 2008 | 3 | During pregnancy | 3 | 0 | Not reported | Not reported |
| Liddell HS and Lo C., 2008 | 11 | Before pregnancy | 10 | 0 | 100 | Not reported |
| Whittle WL et al., 2009 | 65 | 34 not pregnant, 31 pregnant | 67 | 10.7 | 80 | 35.8 |
| Fechner AJ et al., 2009 | 1 | During pregnancy | 1 | 0 | 100 | 37 |
| Carter JF et al., 2009 | 12 | 7 not pregnant, 5 pregnant | 12 | 0 | 75 | Not reported |
| Pereira RM et al., 2009 | 1 | Before pregnancy | 2 | 0 | 100 | 38 |
| Pawlowicz P et al., 2009 | 2 | Before pregnancy | Not reported | 0 | Not reported | Not reported |
| Murray A et al., 2011 | 1 | Before pregnancy | 1 | Not reported | 100 | 28 |
| DaCosta V et al., 2011 | 3 | Before pregnancy | 2 | 0 | 100 | 37 |
| Riiskjaer M et al., 2012 | 52 | Before pregnancy | 45 | 0 | 83.3 | 37.4 |
| El-Nashar SA et al., 2013 | 4 | During pregnancy | 4 | Not reported | 100 | 37.3 |
| Salmeen KE and Parer JT., 2013 | 66 | Before pregnancy | 36 | 4.5 | 90 | 37.2 |
| Ades A et al., 2014 | 64 | 61 not pregnant, 3 pregnant | 35 | 1.6 | 95.8 | 35.8 |
| Shin JE et al., 2014 | 1 | During pregnancy | 1 | 0 | 100 | 35 |
| Luo L et al., 2014 | 19 | Before pregnancy | 15 | 0 | 90 | 36.4 |
| Current study | 101 | 58 not pregnant, 43 pregnant | 93 | 0 | 95 | 36.2 |
Materials and methods
General data
A total of 134 cervical insufficiency patients who had fertility will and required cervical cerclage treatment were included. Briefly, 96 cases of them never received any cervical cerclage treatment, and 38 cases of them received TVC treatment before. None of the patients received cerclage placed via laparoscopy before. All patients have signed the informed consent, and this study was approved by institutional research ethics committee. General conditions of all patients in three groups are shown in Table 2.
Table 2.
Demographic variable linked with the three groups [x ± SD or Cases (%)]
| Group | For all patients | For patients of termination pregnancy | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| CPL (n = 43) | CNL (n = 58) | TVC (n = 33) | CPL (n = 26) | CNL (n = 34) | TVC (n = 33) | |
| Mean maternal age at cerclage | 29.07 ± 3.76 | 29.28 ± 3.28 | 29.94 ± 4.04 | 29.85 ± 4.29 | 29.00 ± 3.26 | 29.94 ± 4.04 |
| Mean gravidity | 2.42 ± 1.01 | 2.14 ± 0.91 | 1.97 ± 0.85 | 2.42 ± 0.95 | 2.12 ± 1.01 | 1.97 ± 0.85 |
| Patient with previous term pregnancy | n = 2 (4.65%) | n = 1 (1.72%) | n = 0 | n = 0 | n = 0 | n = 0 |
| No. of previous living children | n = 2 (4.65%) | n = 2 (3.35%) | n = 0 | n = 0 | n = 0 | n = 0 |
| Mean GA prior to cerclage | 22.25 ± 3.67 | 21.36 ± 3.64 | 22.08 ± 3.04 | 21.91 ± 1.77 | 20.80 ± 4.06 | 22.08 ± 3.04 |
| No. of prior T1 SA | n = 1 | n = 0 | n = 1 | n = 0 | n = 0 | n = 0 |
| No. of prior T1 SA | n = 43 | n = 58 | n = 33 | n = 26 | n = 34 | n = 33 |
Footnote: There were no statistically differences between each two groups. CPL, cerclage placed in pregnancy via laparoscopy; CNL, cerclage placed nonpregnant via laparoscopy; TVC, traditional vaginal cerclage; GA, gestational age.
Inclusion criteria and indication of operation
Medical history of spontaneous abortion or preterm delivery in second or third trimester, diagnosed cervical insufficiency, and fertility will.
Exclusion criteria of cerclage placed via laparoscopy
1). A complication of intrauterine adhesion or uterus myoma in septum and submucosa
2). Medical history of pelvic surgery, a possibility of pelvic comprehensive adhesion
3). Patients with cervical cerclage in first trimester, before this operation, had a medical history of threatened abortion, or a medical history of diagnosed inevitable abortion, or a medical history of missed abortion.
Exclusion criteria of TVC treatment in second and third trimester
1). Vaginitis, acute or sub-acute amniotitis, pelvic inflammation
2). Premature rupture of fetal membranes.
Appropriate operation type was chosen according to patients’ conditions and wills after they were fully informed: If patients were in the second or third trimester, TVC was recommended; if patients were in the first trimester, CPL in the first trimester and TVC in the second or third trimester were recommended; if patients were not pregnant, CNL in non-pregnant phase, CPL in the first trimester, and TVL in the second or third trimester, were all appropriate.
Of all the 134 patients included, 43 cases were treated with CPL in the first trimester (< 14 gestational weeks) (CPL group), 58 cases were treated with CNL in non-pregnant phase (CNL group), 33 cases were treated with TVC in the second or third trimester (TVC group). Cohort study was conducted.
Cervical cerclage via laparoscopy
Tracheal general anesthesia was applied.
CNL: Operating levers was put into uterine cavity to support uterus, and peritoneum covering bladder and uterus was incised using ultrasonic scalpel. Uterus isthmus and blood vessels were exposed after bladder was push down. On the two sides of uterus isthmus, cervical muscular tissue in the medial side of uterus blood vessels (close to the cervical inner orifice) was chosen as the needle insertion point (Figure 1A). A Mersilene encircling band, 5 mm in width, with needles on both ends, was used. Straight needle was inserted from anterior at the point chosen above, and left from the posterior of ipsilateral uterus isthmus (Figure 1B). The knot was tied on the dorsal surface of uterus to prevent possible irritation sign of bladder (Figure 1C). The encircling band was strained till the cervical inner orifice could only contain 6-gauge cervical dilator. The second encircling band was placed right a little upper to the first one the same way as above. Laparoscopic tubal perfusion was performed to confirm that the ovarian ducts remained unobstructed. At last, hysteroscopy examination was performed to make sure that encircling band was in muscular layer, without piercing out of cervix or cervical mucosa (Figure 1D).
Figure 1.
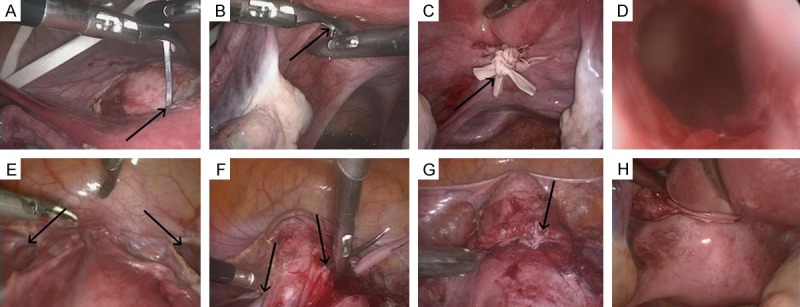
A: Straight entry point of needle in the non-pregnant state; B: Straight exit point of needle in the non-pregnant state; C: Cerclage location in the non-pregnant state; D: Hysteroscopy; E: Surgical approach in the pregnant state with opened broad ligament; F: Straight entry and exit points of needle in the pregnant state; G: Cerclage location in the pregnant state; H: Dorsal surface of the uterus in the pregnant state.
CPL: Because it is impossible to support the uterus with operating levers during pregnancy, ultrasonic scalpel was used to cut up bilateral round ligaments and broad ligaments peritoneum. Cervical isthmus and uterus vessels were exposed after uterovesical peritoneal reflection was cut up (Figure 1E). On the two sides of uterus isthmus, the medial side of uterus blood vessels was chosen as the withdrawing needle points. Straight needle carrying one end of Mersilene suture was inserted from posterior of cervix (Figure 1F) and left from the point chosen above. The other end of the suture was hauled to the other side of cervix from the posterior of uterus, and the same process was performed as before. The Mersilene band was strained as tight as possible, and the knot was tied in the anterior of cervix (Figure 1G, 1H). The second Mersilene band was placed right a little upper to the first one the same way as above. Hysteroscopy examination was not needed.
Treatment after operation: At the end of the operation, laparoscopy was removed and the air in enterocoelia was evacuated. Abdominal wall and skin were repaired. Antibiotics was given only once during perioperative period. After 2 days of observation, patients were allowed to leave hospital if there were no signs of fever, abdominal pain or vaginal bleeding. Cesarean delivery was recommended. Encircling band was not needed to be removed.
TVC
Cervical local anesthesia was applied. Bivalve speculum was used to expose cervix. After vagina and cervix were disinfected, regional anesthesia was performed to cervix. Carrying 10-gauge suture, great curve needle was inserted from the 11-10 o’clock of cervix, where bladder was attached to. The suture went through muscularis mucosae to draw the cervix a little higher, and continued to make purse string at 8-7 o’clock, 5-4 o’clock, and 2-1 o’clock of cervix. A double button ligation was tied on the cervical front lip till the cervix can only contain a fingertip. Patients received fully rest after operation till the delivery. Suture could be removed when the labor was onset. Vaginal delivery was also recommended. All operations were accomplished by a same chief physician with high qualification.
Statistical analysis
SPSS 13.0 software was used in the analysis. Measurement data were documented with means ± standard deviation (SD), and quantitative data were documented with cases (%). With comparison of quantitative data between multiple groups, one-way analysis of variance was conducted if the data showed a normal distribution with an equal variance, and Post Hoc was conducted if a multiple comparison was needed. If the conditions above were not met, Kruskal-Wallis H test would be used to conduct multiple comparisons between groups. In that case, Rank cases were used for coding rank, and then rank orders were used to conduct multiple comparisons of variance analysis. As for quantitative data, chi-square test or continuous corrected chi-square test was conducted for the analysis. If the conditions for chi-square test or continuous corrected chi-square test were not met, Fisher exact propability would take the role. If double variants accorded with normal distribution, the correlation analysis would be conducted using Person analysis, and will be replaced by Spearman analysis if the normal distribution was not shown. P < 0.05 was considered significantly different.
Results
General conditions after operation
All operations were successful without assistance of open operations. There were no complications such as bleeding, infection, and injury of peripheral organs. Patients treated with laparoscopic operation were allowed to leave hospital one week after this surgery. Hospitalization time after operation showed a significant difference between 3 groups (F = 80.488, df = 2, P = 0.000) and was recorded respectively as following: CPL group 3.15 ± 1.41 d, CNL group 1.53 ± 0.66 d, TVC group 5.73 ± 4.15 d.
Outcomes of post-operation pregnancy
In CPL group, 26 cases received termination of pregnancy, and 1 case presented a spontaneous abortion with an unclear reason. In CNL group, 8 patients didn’t show any signs of pregnancy. 50 patients were pregnant, of which 34 cases received termination of pregnancy. Onecase presented a spontaneous abortion due to chromosome abnormalities at 4 weeks of pregnancy, and treated with complete curettage of uterine cavity. Onecase received drug-induced abortion because of stagnation of embryonic development at 14 weeks of pregnancy. In TVC group, 24 cases had a successful vaginalbirth while 9 cases presented a spontaneous abortion in the third trimester. The outcomes of post-operation pregnancy in three groups were showed in Table 3. In CPL and CNL group, all patients were treated with caesarean section, without encircling band removed. For the neonates in three groups, there were no needs of intensive care, no neonatal death, and no sequelae of prematurity.
Table 3.
Main outcome of patients among three groups (Cases)
| Variable | CPL (n = 43) | CNL (n = 58) | TVC (n = 33) |
|---|---|---|---|
| Not pregnant | - | n = 8 | - |
| Still being pregnant | n = 17 | n = 16 | n = 0 |
| Abortion | n = 1 | n = 2 | n = 10 |
| Delivery | n = 25 | n = 32 | n = 23 |
For patients who were pregnant and received termination of pregnancy successfully in three groups, the comparisons of the outcomes are shown in Table 4. Among three groups, significant difference was shown in full term delivery rate (χ2 = 18.678, df = 2, P = 0.000), in mean gestational weeks (if pregnancy lasted ≥ 14 wk) after operation (F = 17.771, df = 2, P = 0.000), in post-operation gestational age for all patients (F = 14.898, df = 2, P = 0.000), in weeks of pregnancy gained (F = 12.678, df = 2, P = 0.000).
Table 4.
Comparison of pregnant outcomes among three groups [x ± SD or Cases (%)]
| Data | CPL group (n = 26) | CNL group (n = 34) | TVC group (n = 33) | χ2 or F (df) | P | P value (CPL vs CNL) | P value (CPL vs TVC) | P value (CNL vs TVC) |
|---|---|---|---|---|---|---|---|---|
| T1 SA | n = 1 | n = 1 | n = 1 | |||||
| T2 SA | n = 0 | n = 1 | n = 9 | |||||
| Premature delivery | n = 1 | n = 4 | n = 8 | |||||
| Term delivery | n = 24 | n = 28 | n = 15 | 18.678 (2) | 0.000 | 0.459 | 0.000 | 0.002 |
| Fetal salvage rate | 25/25 | 32/33 | 23/32 | 0.569 | 0.012 | 0.014 | ||
| GA if pregnancy lasted ≥ 14 wk* | 37.88 ± 0.83 | 36.67 ± 4.51 | 32.91 ± 7.20 | 17.771 (2) | 0.000 | 0.434 | 0.000 | 0.000 |
| GA for all patients* | 36.73 ± 5.92 | 35.71 ± 7.15 | 31.30 ± 7.88 | 14.898 (2) | 0.000 | 0.521 | 0.000 | 0.000 |
| Birth weight (g)* | 3006.00 ± 402.94 | 2885.94 ± 437.41 | 2762.50 ± 591.10 | 0.197 (2) | 0.821 | 0.713 | 0.553 | 0.767 |
| Weeks of pregnancy gained | 16.00 ± 1.96 | 14.58 ± 5.63 | 10.69 ± 5.93 | 12.678 (2) | 0.000 | 0.065 | 0.000 | 0.001 |
Footnote: T1 SA, first trimester spontaneous abortion; T2 SA, second trimester spontaneous abortion;
Values are average (range).
Fetal salvage rate (if pregnancy lasted ≥ 14 wk) was defined as the ratio of live fetus number and the total number of pregnancy (excluding the number of continuous pregnancy and the number of abortions within 14 wk). Weeks of pregnancy gained were the differences between the weeks of first abortion or delivery after surgery and the average weeks of all spontaneous abortions or deliveries before surgery (excluding abortions within 14 wk).
Multiple comparison between every two groups
CPL group and CNL group: there were not significant differences in every index of post-operation pregnancy (P > 0.05).
CPL group and TVC group: significant differences were shown in indexes such as full term deliveryrate (24/26 VS 15/33, P = 0.000), fetalsurvival rate (25/25 VS 23/32, P = 0.000), mean gestational weeks (if pregnancy lasted ≥ 14 wk) (37.88 ± 0.83 VS 32.91 ± 7.20, P = 0.000), post-operation gestational age for all patients (35.71 ± 7.15 VS 31.30 ± 7.88, P = 0.000), and weeks of pregnancy gained (16.00 ± 1.96 VS 10.69 ± 5.93, P = 0.000).
CNL group and TVC group: significant differences were shown in indexes such as full term delivery rate (28/34 VS 15/33,P = 0.000), neonatal survival rate (32/33 VS 23/32,P = 0.000), mean gestational weeks (if pregnancy lasted ≥ 14 wk) (36.67 ± 4.51 VS 32.91 ± 7.20, P = 0.000), post-operation gestational age for all patients (36.73 ± 5.92 VS 31.30 ± 7.88, P = 0.000), and weeks of pregnancy gained (16.00 ± 1.96 VS. 10.69 ± 5.93, P = 0.000).
Analysis of correlation between pregnancy and operation
In CPL group, for the 25 patients who received termination of pregnancy, the correlation between gestational time before CPL and gestational weeks at delivery was demonstrated (Figure 2A). The correlation coefficient was rs = -0.121, P = 0.555, showing no significant correlation.
Figure 2.
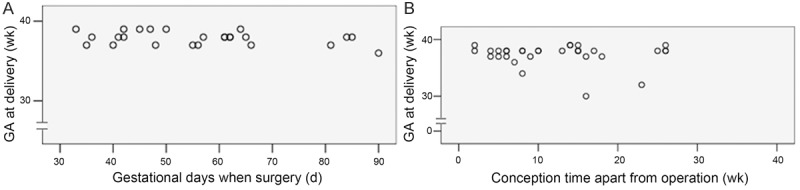
A: Relationship between gestational days when surgery and GA at delivery; B: Relationship between conception time apart from operation and GA at delivery.
In CNL group, for the 32 patients who received termination of pregnancy, the correlation between interval time before fertilization and gestational weeks at delivery was demonstrated (Figure 2B). The correlation coefficient was rs = 0.130, P = 0.464, showing no significant correlation.
Discussion
Cervical insufficiency was caused by defects in cervical structure or function. If pregnancy cannot be maintained to full term, in the second or the third trimester, there will be premature rupture of fetal membranes or pregnant capsule intruding into vagina or even pregnant capsule discharged out of the uterine. Cervical insufficiency has become one of the leading causes of recurrent abortion and premature labor in the second or the third trimester [2,4]. TVC, as a traditional method, was usually placed in the second and the third trimester or used as an emergency treatment for threatened abortion and premature labor in the second and the third trimester [4,11]. Because the operation was performed in vagina and in pregnancy, bladder was not push down, in order to prevent the stretching of cervix. The position of knot was located below cervical inner introitus, close to the cervical outer orifice and 10-gauge suture was used. However, what really supports the pregnant uterine was only the encircling string and the cervical tissue beneath it, which resulted in an insufficient power and a high rate of failure.
It is still a problem how the full term labor rate could be improved. We placed laparoscopic cervical cerclage in non-pregnant phase and the first trimester (< 14 gestational weeks), showing that CPL and CNL could shorten the hospitalization time and prolong the gestational weeks compared with TVC. In CPL group and CNL group, the indexes such as the full term deliveryrate, fetal salvage rate (if pregnancy lasted ≥ 14 weeks), mean gestational weeks (if pregnancy lasted ≥ 14 wk) after operation, post-operation gestational age for all patients, and weeks of pregnancy gained, were all significantly higher than those in TVC group (P < 0.05) (Table 3). It has been proved that CPL and CNL have advantages compared with TVC [1,6,12-17], probably the reason could be shown as following: 1). With laparoscope, cervix could be fully exposed after bladder was pushed down. Therefore the encircling band could be sutured above the cervical inner orifice accurately (Figure 1G). 2). Two relative wide encircling bands could be used in the operation so that the problem of cervical anatomic defects was fundamentally solved, with the mechanical requirement of a pregnant uterine well satisfied [9]. 3). Stable encircling band and the enough cervical tissue beneath it could well support the pregnant uterine during the whole pregnancy, enhance the bearing capacity of cervix and prevent the cervical orifice from dilating with gestational weeks increasing. Therefore, abortion or premature delivery could be avoided effectively with gestational weeks prolonged and outcomes of pregnancy obviously improved.
Should the CPL and CNL be placed during non-pregnant phase or the first trimester? We concluded from this study that, every index (including full term delivery rate, fetal salvage rate (if pregnancy lasted ≥ 14 weeks), mean gestational weeks (if pregnancy lasted ≥ 14 wk) after operation, post-operation gestational age for all patients, and weeks of pregnancy gained) of CPL and CNL was similar, without a significant difference (Table 3), indicating CPL is as safe as CNL.
Frankly, there was risk of abortion if laparoscopic cervical cerclage was placed in pregnancy. In order to improve the safety and success rate, patients with gestational weeks less than 14 weeks were chosen. Uterus was less sensitive with less gestational weeks, therefore risk of uterus contraction decreased. Using laparoscope, there was no need of drawing the cervix when push down the bladder and suture the cervical inner orifice, so the pregnant uterus received less irritation. There was no incisions in vagina, which reduced the risk of abortion and infection. In addition, there was some technical improvement in CPL compared with CNL: 1). In order to reduce the irritation uterine got, operational levers were not used. 2). The straight needle carrying the encircling band was inserted from posterior to anterior (Figure 1F), and the knot was tied in the anterior of uterus. Uterus was swayed as less as possible to reduce the irritation. At the same time, the knot was fully exposed making it easier to tie the knot and examine whether the knot was strained tight without swaying the uterus. 3). Hysteroscopy examination was not needed after operation.
Compared with CNL, CPL may increase the hospitalization time, but patients could still leave hospital within one week after operation, which were both shorter than that of TVC. For patients received CPL, the normal life and work would not be affected, and long term of bedding to recover is not necessary. Progesterone injection through muscle would be enough for tocolytic effect. Antibiotic treatment was given before and after operation respectively for perioperative prevention of infection. The correlation analysis between CPL placed time and gestational weeks at delivery (Figure 1) showed that there was not an obvious correlation. So for cervical insufficiency patients, CPL placement was recommended at any time within 14 weeks of pregnancy. While in the third trimester, laparoscopic vision field was blocked by a bigger uterus, CPL was not recommended. Whether CPL could be placed in the second trimester is worthy of further investigation.
What we are really concerned about is whether CNL will affect the fertilization after operation. In the CNL operation, after the encircling band was placed, not only tubal perfusion was performed to make sure the oviduct was unblocked, but also the hysteroscopy examination was performed to make sure the encircling band was not piercing out of uterine endometrium. Theoretically, in cervical cerclage placement, encircling band was embed in the cervical muscular tissue of isthmus (close to the cervical inner orifice) without piercing out of cervix or endometrium to become foreign bodies, and it would not affect the sperm passing through the cervix or the capacity of uterus. The encircling band was used to tight the cervix instead of ovaries or its vessels, so the ovaries’ function was not affected. A minimally invasive laparoscope was used with a low possibility of pelvic adhesion. Therefore, CNL is considered to have no influence on fertilization. There was no significant correlation between fertilization time in CNL patients and gestational weeks at delivery. Any time of fertilization after operation would be appropriate, and there is no need of waiting.
In summary, compared with TVC in the second or third trimester, laparoscopic cervical cerclage is a safe and effective treatment. For cervical insufficiency patients, it can effectively prolong the gestational weeks, and improve the full term labor rate and fetal lavage rate, with a shorted time to recover. The operation would be safe and effective both in non-pregnant phase and the first trimester. A longer and larger-scale follow-up visit remains worthy and necessary.
Acknowledgements
This study was funded by Guangzhou Science Project 12A022061820 and Guangdong Province Science Project 2013B021800237 and 2012B040304007.
Disclosure of conflict of interest
None.
References
- 1.Shin JE, Kim MJ, Kim GW, Lee DW, Lee MK, Kim SJ. Laparoscopic transabdominal cervical cerclage: Case report of a woman without exocervix at 11 weeks gestation. Obstet Gynecol Sci. 2014;57:232–235. doi: 10.5468/ogs.2014.57.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ACOG Practice Bulletin No. 142: Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123:372–379. doi: 10.1097/01.AOG.0000443276.68274.cc. [DOI] [PubMed] [Google Scholar]
- 3.McDonald IA. Suture of the cervix for inevitable miscarriage. J Obstet Gynaecol Br Emp. 1957;64:346–350. doi: 10.1111/j.1471-0528.1957.tb02650.x. [DOI] [PubMed] [Google Scholar]
- 4.Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68:379–388. doi: 10.1097/OGX.0b013e31828737c7. [DOI] [PubMed] [Google Scholar]
- 5.Abbott D, To M, Shennan A. Cervical cerclage: A review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52:220–223. doi: 10.1111/j.1479-828X.2012.01412.x. [DOI] [PubMed] [Google Scholar]
- 6.Luo L, Chen Sq, Jiang Hy, Niu G, Wang Q, Yao SZ. Successful treatment of cervical incompetence using a modified laparoscopic cervical cerclage technique: a cohort study. Eur J Obstet Gynecol Reprod Biol. 2014;179:125–129. doi: 10.1016/j.ejogrb.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 7.Riiskjaer M, Petersen OB, Uldbjerg N, Hvidman L, Helmig RB, Forman A. Feasibility and clinical effects of laparoscopic abdominal cerclage: an observational study. Acta Obstet Gynecol Scand. 2012;91:1314–1318. doi: 10.1111/aogs.12001. [DOI] [PubMed] [Google Scholar]
- 8.Nicolet G, Cohen M, Begue L, Reyftmann L, Boulot P, Déchaud H. [Laparoscopic cervico-isthmic cerclage evaluation] . Gynecol Obstet Fertil. 2009;37:294–299. doi: 10.1016/j.gyobfe.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 9.El-Nashar SA, Paraiso MF, Rodewald K, Muir T, Abdelhafez F, Lazebnik N, Bedaiwy MA. Laparoscopic cervicoisthmic cerclage: technique and systematic review of the literature. Gynecol Obstet Invest. 2012;75:1–8. doi: 10.1159/000343036. [DOI] [PubMed] [Google Scholar]
- 10.Burger NB, Brölmann HAM, Einarsson JI, Langebrekke A, Huirne JAF. Effectiveness of abdominal cerclage placed via laparotomy or laparoscopy: systematic review. J Minim Invasive Gynecol. 2011;18:696–704. doi: 10.1016/j.jmig.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Berghella V, Ludmir J, Simonazzi G, Owen J. Transvaginal cervical cerclage: evidence for perioperative management strategies. Am J Obstet Gynecol. 2013;209:181–192. doi: 10.1016/j.ajog.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Ades A, May J, Cade TJ, Umstad MP. Laparoscopic transabdominal cervical cerclage: A 6-year experience. Aust N Z J Obstet Gynaecol. 2014;54:117–120. doi: 10.1111/ajo.12156. [DOI] [PubMed] [Google Scholar]
- 13.Carter JF, Soper DE, Goetzl LM, Van Dorsten JP. Abdominal cerclage for the treatment of recurrent cervical insufficiency: laparoscopy or laparotomy? Am J Obstet Gynecol. 2009;201:111.e111–111.e114. doi: 10.1016/j.ajog.2009.05.033. [DOI] [PubMed] [Google Scholar]
- 14.Whittle WL, Singh SS, Allen L, Glaude L, Thomas J, Windrim R, Leyland N. Laparoscopic cervico-isthmic cerclage: surgical technique and obstetric outcomes. Am J Obstet Gynecol. 2009;201:364.e361–364.e367. doi: 10.1016/j.ajog.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Reid GD, Wills HJ, Shukla A, Hammill P. Laparoscopic transabdominal cervico-isthmic cerclage: A minimally invasive approach. Aust N Z J Obstet Gynaecol. 2008;48:185–188. doi: 10.1111/j.1479-828X.2008.00835.x. [DOI] [PubMed] [Google Scholar]
- 16.Gallot D, Savary D, Laurichesse H, Bournazeau JA, Amblard J, Lémery D. Experience with three cases of laparoscopic transabdominal cervico-isthmic cerclage and two subsequent pregnancies. BJOG. 2003;110:696–700. [PubMed] [Google Scholar]
- 17.Mingione MJ, Scibetta JJ, Sanko SR, Phipps WR. Clinical outcomes following interval laparoscopic transadominal cervico-isthmic cerclage placement: Case series. Hum Reprod. 2003;18:1716–1719. doi: 10.1093/humrep/deg345. [DOI] [PubMed] [Google Scholar]


